Abstract
Objective
In the context of scientific uncertainty, treatment choices for localized prostate cancer vary, but reasons for this variation are unclear. We explored how black and white American men made their treatment decision.
Methods
Guided by conceptual model, we conducted semistructured interviews of 21 American (14 black and 7 white) men with recently diagnosed localized prostate cancer.
Results
Physician recommendation was very important in the treatment decision, but patient self-perception/values and attitudes/beliefs about prostate cancer were also influential. Patients who chose surgery believed it offered the best chance of cure and were more concerned that the cancer might spread if not surgically removed. Patients who chose radiation therapy believed it offered equal efficacy of cure but fewer side effects than surgery. Fear of future consequences was the most common reason to reject watchful waiting. Anecdotal experiences of family and friends were also important, especially in deciding “what not to do.” The new technology of robotic-assisted prostatectomy provided optimism for men who wanted surgery but feared morbidity associated with traditional open surgery. Few men seemed aware that treatment did not guarantee improved survival.
Conclusion
Most men reported making “the best choice for me” by taking into account medical information and personal factors. Perceptions of treatment efficacy and side effects, which derived mainly from physicians’ descriptions and/or anecdotal experiences of family and friends, were the most influential factors in men’s treatment decision. By understanding factors that influence patients’ treatment decisions, clinicians may be more sensitive to individual patients’ preferences/ concerns and provide more patient-centered care.
Keywords: prostate cancer, treatment, racial disparities
INTRODUCTION
Approximately 1 in 6 US men are diagnosed with prostate cancer and 1 in 34 die from it each year.1 As a result of increased prostate-specific antigen (PSA) screening, most cancers are detected while they are localized to the gland.2 For localized prostate cancer, current primary treatment options include surgery, radiation, and watchful waiting. Rigorous evidence is still lacking regarding which option offers the best long-term survival, and each is associated with significant morbidity.3 Therefore, when diagnosed with localized prostate cancer, men face complex and often inconclusive information regarding treatment options and associated outcomes.
Treatment choices for localized prostate cancer appear to vary widely, although it is unclear whether this variation is a result of patient values or other factors such as information received or emotional feelings about a cancer diagnosis.4 Furthermore, considerable variation exists in prostate cancer treatment by racial/ ethnic groups,5,6 with black men more likely to receive radiation therapy and white men to receive surgery.7 Watchful waiting is the least used treatment option, chosen by fewer than 10% of men overall, with blacks more likely to choose it than whites.8,9
Few qualitative studies10,11 conducted near the time of initial diagnosis and treatment have elicited patients’ perspectives about the reasons for their treatment choices. Such studies included few minority participants and lacked variability in treatment selected10 and most often studied only patients of urologists.11 There is little research regarding how patients’ personal values shape and influence their individual treatment decision.4,12 In this qualitative interview study, we explored how black and white American men who selected a variety of treatment options made their prostate cancer treatment decision shortly after their diagnosis. The purpose of the study was to gain an in-depth understanding of men’s perspectives on selecting their prostate cancer treatment.
METHODS
Study Sample
Patients with newly diagnosed localized prostate cancer were recruited through referrals from 3 urology offices and 1 radiation oncology office in metropolitan Detroit, Michigan, and also through recruitment flyers in hospitals and doctors’ offices. The sampling aim was to select information-rich cases representing each of the main treatment strategies for prostate cancer (ie, surgery, radiation, and watchful waiting) and to maximize the likelihood that a broader range of experiences could be obtained. Purposeful sampling strategy is able to do just that, ie, providing us with a diverse study sample in terms of treatment choice, race, age, social class, and income.13
We had no problems recruiting men who chose surgery or radiation, and data saturation was reached for these groups. However, we had some difficulty finding and recruiting men who chose watchful waiting; we were only able to recruit 2 and may not have reached saturation.
Eligibility criteria were: age younger than 75 years, recently diagnosed localized prostate cancer, a treatment consultation with either an urologist and/or radiation oncologist, and self-identification as either black or white. Excluded were patients who were not given a treatment choice due to medical contraindications or those unable to communicate in English. The study protocol was reviewed and approved by the Wayne State University institutional review board.
Data Collection
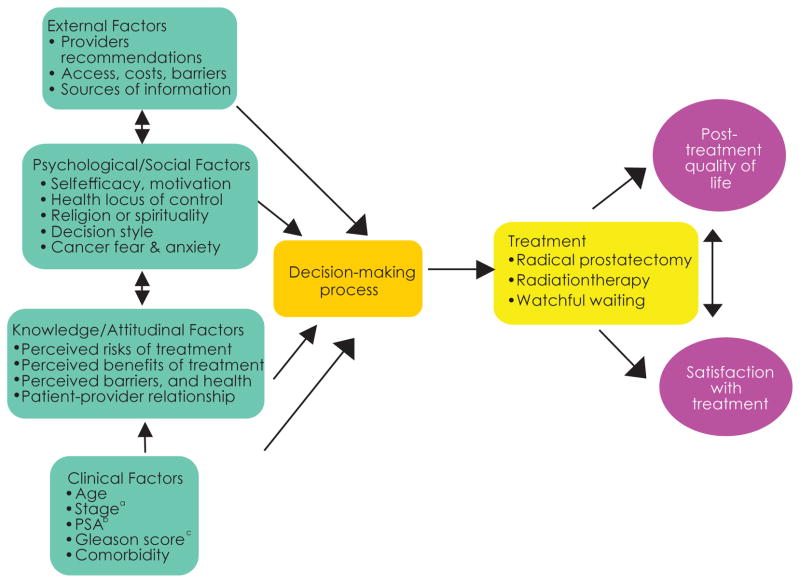
The semistructured interview guide (Appendix) included multiple cognitive (eg, a rational weighing of the pros and cons of a specific treatment option) and affective (eg, fear of cancer and death) domains of health behavior, based on the Health Belief Model (HBM) and the Cognitive-Social Health Information Processing (C-SHIP) Model14,15 (Figure). Interviews took place either in the participant’s home or in a research office, according to the participant’s preference. Interviews lasted approximately 60 to 120 (median 90) minutes and were audiotaped and transcribed. Most of the interviews were conducted by R.D., an African American researcher, and others by J.X., a Chinese American family physician and researcher. Both were trained and experienced in qualitative research.
Figure. Conceptual Model.
aStaging describes the extent or severity of an individual’s cancer based on the extent of the original tumor and the extent of spread in the body. The stage can be used to estimate the person’s prognosis.
bProstate-specific antigen (PSA) is a protein produced by cells of the prostate gland. The PSA test measures the level of PSA in the blood. The higher a man’s PSA level, the more likely his prostate cancer is aggressive.
cGleason score is based upon microscopic appearance of tumor pattern. Higher number represents more aggressive tumor. The Gleason score ranges from 2 to 10, with 10 having the worst prognosis.
The interviews began with a general, open-ended question eliciting participants’ perceptions of their health status prior to their diagnosis of prostate cancer and their general beliefs about cancer and cure. Participants were then asked to describe their experiences learning about the diagnosis, their treatment decision-making process, and their beliefs about the efficacy and side effect profile of each treatment option. Perceptions of influential information sources and barriers and facilitators of decision making were also elicited. Patient clinical factors (eg, PSA level, Gleason score, tumor stage) and comorbidities were provided by the referral physician and/or from self-report during interview.
Data Analysis
Verbatim transcripts were checked against audio-tapes to verify accuracy and entered into Atlas.ti V5.0, qualitative analysis software. Analysis was ongoing during data collection.16 The theoretical preconceptions from our model were used to build a preliminary skeleton, or axis, of codes.16 Three authors (J.X., R.D., and S.E.) independently read the transcripts to look for recurring emergent themes, using immersion/crystallization analysis technique.13,16 After the team agreed we had captured the relevant themes, we developed operational definitions of the themes. Each transcript was then independently coded by at least 2 reviewers. When disagreement occurred, the transcripts were reviewed again and consensus was reached by discussion. Once all transcripts were coded, analyses of the themes, such as patterns of development and frequencies of occurrence, were compared across participants. Memos and notes were written to preserve ideas throughout data collection and analysis regarding emerging theory.16 Main findings were presented to 10 interviewees for their feedback and confirmation of the findings.
RESULTS
Twenty-one newly diagnosed localized prostate cancer patients were interviewed. They consulted a total of 12 urologists and 6 radiation oncologists in the local metropolitan area. Sociodemographics, tumor characteristics, and treatment selected are summarized in Table 1. Most men were otherwise healthy and none had a previous cancer diagnosis.
Table 1.
Medical and Demographic Characteristics of Participants
| Patient No. | Age | Marital Status | Education | Race/Ethnicity | Income | Insurance | Gleason Scorea | PSAb | Initial Treatment Chosen/Received | Second Opinion |
|---|---|---|---|---|---|---|---|---|---|---|
| P1 | 60 | Married | College graduate | White | ≥$90 000 | Private | 6 | 7.5 | Surgery (robotic) | Yes |
| P2 | 68 | Married | Some college | White | ≥$90 000 | Private | 6 | 4.5 | Radiation (external) | Yes |
| P3 | 59 | Married | College graduate | Black | ≥$90 000 | Private | 6 | 2.7 | Radiation (external) | Yes |
| P4 | 49 | Married | Some college | White | ≥$90 000 | Private | 6 | 2.4 | Surgery | Yes |
| P5 | 57 | Married | Some college | Black | $30 000–$39 999 | Private | 6 | 1 | Radiation (seed) | No |
| P6 | 55 | Single | Some high school | Black | $10 000–$19 999 | Private + Medicare | 6 | 2.6 | Radiation (seed) | No |
| P7 | 59 | Divorced | College graduate | White | $50 000–$69 999 | Private | 7 | 9.9 | Radiation (external + hormone) | Yes |
| P8 | 55 | Separated | Some college | Black | <$9999 | Medicaid | 6 | 4.2 | Surgery | Yes |
| P9 | 56 | Separated | High school graduate | Black | $10 000–$19 999 | Medicare | – | – | Surgery | No |
| P10 | 62 | Divorced | Some college | Black | $20 000–$29 999 | Private | – | 5 | Cryotherapy | Yes |
| P11 | 57 | Single | College graduate | White | $20 000–$29 999 | Private | 7 | 6.7 | Radiation (external) | Yes |
| P12 | 63 | Divorced | College graduate | Black | – | Private | – | 5.8 | Watchful waiting | Yes |
| P13 | 68 | Married | College graduate | White | ≥$90 000 | Private | 6 | 5.8 | Radiation (external) | Yes |
| P14 | 53 | Married | College graduate | White | ≥$90 000 | Private | 6 | 4.8 | Radiation high-dose brachytherapy | Yes |
| P15 | 60 | Widowed | Some college | Black | $10 000–$19 999 | Private | 6 | 5 | Surgery (robotic) | Yes |
| P16 | 48 | Married | High school graduate | Black | $20 000–$29 999 | Private | 6 | 3.7 | Surgery | Yes |
| P17 | 57 | Single | Some college | Black | ≥$90 000 | Private | 6 | 7 | Surgery | Yes |
| P18 | 51 | Cohabited | Some college | Black | $70 000–$89 999 | Private | – | 9.4 | Surgery | Yes |
| P19 | 53 | Divorced | College graduate | Black | $50 000–$69 999 | Private | 6 | – | Radiation (external) | Yes |
| P20 | 53 | Divorced | Some college | Black | <$9999 | Medicare +Medicaid | – | – | Watchful waiting | No |
| P21 | 70 | Divorced | High school graduate | Black | <$9999 | Medicaid | 6 | 3 | Radiation (external) | Yes |
Gleason score is based upon microscopic appearance of tumor pattern. Higher number represents more aggressive tumor. The Gleason score ranges from 2 to 10, with 10 having the worst prognosis.
Prostate-specific antigen (PSA) is a protein produced by cells of the prostate gland. The PSA test measures the level of PSA in the blood. The higher a man’s PSA level, the more likely his prostate cancer is aggressive.
The time elapsed between diagnosis and interview ranged from 1 to 6 months, with the exception of 1 man, who chose watchful waiting and had been diagnosed 2 years previously. Among the men who chose active treatment (n = 19), 7 had not yet been treated at the time of interview, 10 had been treated within the previous 2 months, 1 had been treated within 3 months of and another 5 months prior to interview.
Decision-making Process and Influencing Factors
For most men, both black and white, treatment decision making occurred within an emotional context of fear and uncertainty and without systematic use of information. Most men reported coping with the distress by attempting to take control of the decision-making process. They sought information from a variety of sources, including second opinions from physicians and informal social networks. A complex interaction of internal and external factors influenced the treatment decision. Internal factors included personal attributes, attitudes/ beliefs about cancer, and perceptions of treatment options. External factors included influential individuals, including physicians, family and friends, particularly other prostate cancer survivors.
Guided by our conceptual model, below are more detailed descriptions of the major themes that emerged during the interviews as factors that influenced men’s treatment decision. Men’s perceptions and specific reasons as to why they chose or did not choose each of the main treatment options are provided in Tables 2 to 4.
Table 2.
Men’s Perceptions Regarding Surgery (Radical Prostatectomy)
| Reasons Why Chosen | Reasons Why Not Chosen |
|---|---|
|
|
Table 4.
Men’s Perceptions Regarding Watchful Waiting
| Reasons Why Chosen | Reasons Why Not Chosen |
|---|---|
|
|
Self-perception, Values and Preferences
Most men described their personality and temperament, life stages and goals, and occupation to provide a context to their decision-making process. This self-perception appeared to be the most fundamental part of the experience of cancer and the lens through which all else was interpreted. For example, one man described himself in the following way:
I am a planner, thinker and worrier … I’d like to get it over with and move on with life and not have to worry about it. Something that doesn’t result in a cure is not a viable option in my mind. [60, white, surgery]
All men mentioned their age as influencing their decision. Being “young” was a justification for rejecting watchful waiting by men with a range of ages, based on their belief that watchful waiting is more appropriate for “older men.” Other justifications for rejecting watchful waiting were self-perception as having good general health and the longevity of their relatives.
Although survival was a goal of treatment for most men, some emphasized valuing quality of life over survival. Many men stated their initial goal was to “take it out” through surgery but later changed their minds after learning the possible side effects of this treatment.
I went there with the attitude, this is a no-brainer … Just take it [prostate] out. So then a surgeon comes in, and he says … “You’ll have a catheter for 2 weeks. You’ll be wearing a bag for about a month” … I can’t do it … And he said, “There’s a slight, slight chance you’ll be wearing a diaper.” Well, God bless people who wear a diaper, but that’s not me. To me, it’s the quality of life not the quantity of life. I’d rather be gone than that.” [57, white, external radiation]
On the other hand, fear of cancer progression caused some men to choose surgery, despite potential side effects. One man who witnessed his father’s death from prostate cancer was very anxious about his cancer and wanted it “out” as soon as possible. When asked if side effects such as impotence influenced his decision on surgery, he explained:
Well, I didn’t think about that stuff…I would rather live than have sex… I don’t look at myself not being a man because I can’t have sex. [55, black, surgery]
Personality traits and education also played a major role in decision-making style. For example, men who described themselves as “I am a self-reliance type of guy” were more active in the decision-making process, searching for information from different sources and social networks. These individuals were more likely to seek second, third, or even more professional opinions. Similarly, some highly educated men sought additional opinions and had a harder time selecting a treatment because the information was “too general” and there was a “lack of consensus among experts.”
Attitudes/Beliefs About Cancer, Treatment, and Cure
Treatment decisions were affected by prior beliefs about cancer and cure, perceptions of efficacy and side effects of treatments, aggressiveness of the cancer, coping styles, and religion/faith. Most men believed surgery was the best option for cure by “taking the cancer out,” as other treatments “leave the cancer in” the body, potentially leading to recurrence. Furthermore, radiation was considered “nasty stuff,” possibly damaging other organs and causing suffering (skin burns and hair loss).
Most men who chose radiation stated that either radiation or surgery could cure their cancer, but radiation was less invasive, thus leading to fewer side effects than surgery. Prioritizing quality-of-life issues, some chose radiation despite their belief that surgery may provide better chance of cure.
I know for this early-stage disease, if I take surgery, which probably gives me maximum chance of it never occurring again. So if I was older, I’d probably take surgery, but you know, I’m not. I don’t want to be [impotent]…I want to enjoy myself for a few more years, hell. [53, white, brachytherapy]
Other men believed surgery and radiation would have similar side effects, thus minimizing the role of side effects in their decision.
I know there was a chance, no matter what treatment I had, that after 2 years, your odds of impotence or incontinence is going to be about the same. [49, white, surgery]
Others believed that their cancer was so small and nonaggressive they did not need active treatment at all:
If it’s not bothering you, don’t mess with it. If it’s bothering me real bad, yeah, I might do something, but if it’s not bothering me, why mess with it. [53, black, watchful waiting]
Some men who wanted surgery but feared the side effects of traditional open surgery were pleased to learn of the option of robotic-assisted prostatectomy (RAP). Half of the participants (4/8) who chose surgery were aware of this option. These men described the new technology as “less invasive and more precise, and able to better protect the nerve,” leading to fewer side effects, especially sexual dysfunction. However, only 2 men actually received the newer procedure. The other 2 men received traditional surgery because they were comfortable with their urologists who did not perform RAP and who reassured their patients that the outcomes were about the same.
For some, prayer and faith in a higher being helped determine their approach to treat the cancer; this seemed especially true for black men. For example, one black man chose watchful waiting primarily based on his faith that “God will take care of me.” On the other hand, watchful waiting was often referred to as “do nothing.” Although many participants believed that their prostate cancer was slow growing, they still thought it eventually would “kill” if not actively treated:
If you watch and do nothing it’s going to obviously progress. It’s like, well, you’re waiting for the time bomb to explode. [57, black, brachytherapy]
Influence of Physicians
Most participants remembered that their diagnosing urologist presented them with several treatment options, but only half recalled being told the option of watchful waiting. Some men were initially frustrated by the fact that the urologist did not recommend any one treatment over others but later thought it showed professionalism and appreciated it.
Many men talked about the influence of a direct recommendation from their physician. They frequently cited urologists as saying “at your age I would recommend surgery because it offers the best chance for cure,” whereas others spoke of radiation oncologists advising them to choose radiation over surgery because “radiation can get rid of the cancer with fewer side effects.” However, more men were influenced by their physician’s description of treatment options, even when the physician did not offer a specific recommendation. For example, many recalled their urologist stating that surgery was no longer an option after initial radiation, and this information strongly influenced their decision.
What he [urologist] told me is that if you do radiation to treat this cancer, there is no plan B. That is, if something comes back later, you’ve got a problem. You can’t do radiation again; you can’t do surgery, because there’s so much fibrosis. I thought it over and said, boy, I don’t like the sound of that. That’s not a good plan. You always need a plan B. [60, white, surgery]
Another common influencing remark made by urologists was that the only way to confirm the extent of the cancer is by performing surgery. For some men, the uncertainty of their cancer stage was intolerable and they chose surgery to be more certain.
He [urologist] didn’t say it was the best procedure but he was saying that it had a greater outlook for things and make sure that it hasn’t gone through your body. [51, black, surgery]
Although most men were concerned about impotence, many who chose surgery seemed to be influenced by their urologist’s positive attitudes about treating impotence with drugs. In addition, they were reassured by their urologist that impotence could be avoided by a competent surgeon: “It’s just a matter of who does it.”
On the other hand, respondents who rejected surgery due to concerns about side effects stated that they had to get over the negative biases against radiation, referring to reassurance by their radiation oncologist that current therapy “is technologically improved and not your grandfather’s radiation.”
Most men (17/21) reported seeking at least 1 professional second opinion; 4 men did not and all were black. Three of these 4 also did not seek additional reading information beyond the brochure given by their urologist, saying they had enough information, or had confidence and trust in their urologist or trust in God, or concern about possible delay in treatment. One man indicated that different opinions would make it harder for him to make the decision. Financial cost was denied as a factor for not seeking second opinion.
Some men sought additional opinions at their urologist’s suggestion, while others obtained a second opinion because they disagreed with the initial treatment recommendation. The median number of urologists men consulted for advice was 2 (range, 1–8); most also consulted a radiation oncologist (range, 1–3). Some sought help from their primary care physicians or physician acquaintances. Many times, the second opinion conflicted with the first opinion.
I was seriously considering having the surgery, the way the urologist made it sound like, “oh, my goodness, you know, you’ve got do this [surgery] as soon as possible.” Then I went to [different hospital], and they recommended watchful waiting. [63, black, watchful waiting]
Agreement among physicians regarding the most appropriate treatment was a powerful influence. For example, one man initially chose brachytherapy based on his friend’s experience, despite his urologist’s recommendation of surgery. Then he sought out this friend’s physician (an urologist) as a second opinion. To his surprise, this physician recommended surgery for him, which he chose despite his initial reluctance.
Conflicting recommendations caused more confusion and anxiety for some men. For example, one man stated:
My urologist recommended that I undergo radiation. When I talked to my primary care physician, he thought I should do surgery. So it was like, these are the experts, now I have to decide which one I do. [60, black, external radiation]
In the process of seeking second opinions, many men noted that physicians tended to emphasize the positive aspects of their own method of treatment, while minimizing the side effects or even withholding some of the information.
When you go to one doctor, they tell you about what the other doctor hasn’t told you, by both sides. The radiologists would tell you something about surgery that the surgeon didn’t tell you. The surgeon would tell you something about radiation that the radiologists didn’t know. I’m not saying they did on purpose. [59, white, external radiation plus hormone]
Distrust of physicians and the health care system was mentioned by 3 black men but none of the white men. One man questioned the financial motivation of surgeons who may recommend unnecessary surgery. General distrust of the health care system contributed to another’s decision for watchful waiting. The third black participant also mentioned the physician’s race as an important consideration regarding trust of the advice.
It [race] made a big difference. You know, I had more confidence in his opinion because he was a black man. I don’t have complete confidence in white people being concerned about us, and so yeah, it had a big factor on it, and that’s why I wanted black doctor. [60, black, surgery]
Influence of Family and Friends
Most men sought information and advice from friends or family, particularly those with personal experience with prostate cancer. Only 2 men did not talk to other prostate cancer patients. The experience of others often exerted strong sway over patients’ final decisions.
A good friend of mine had surgery. He was a young man going in and he has nothing now. He dribbles, he’s incontinent, and he doesn’t have sexual function. I couldn’t imagine myself in that way. [59, white, external radiation plus hormone]
I talked to people and they all had different treatment. Some had surgery, some had radiation and each one swore by the treatment that they had, with the exception of my friend, who had undergone the latest surgical technique, the robotic surgery. My friend said, “After having gone through the surgery, I would do radiation,” which was very helpful. [60, black, external radiation]
My friend got [external] radiation and he said it hurts, he lost his hair and his sex drive. Other friends told me surgery is painful. [55, black, brachytherapy]
Wives or partners were not typically reported as influential in the men’s final decision. The typical roles for wives were as information gatherers, processors, and supporters. However, some men reported feeling pressure to accept aggressive treatment. One who initially chose watchful waiting plus natural supplements decided on radiation due to family pressure.
DISCUSSION
In our sample, men with localized prostate cancer reported making “the best choice for me” by taking into account medical information gained from all sources and personal factors while personally framing the meaning of the diagnosis and treatment. Cancer eradication was nearly every patient’s initial goa, and for many men it remained the primary factor in their decision, but for some, quality-of-life issues were almost equally important. A direct recommendation from a physician influenced men’s decisions. However, when physicians did not directly recommend a treatment, their description of efficacy and side effects of the different options was influential. Anecdotal experiences of family and friends were also important, especially in deciding “what not to do.” The new technology of RAP provided optimism for men who wanted surgery but feared the morbidity associated with the traditional open surgery. However, the final treatment decision was influenced by opinions and expertise of their trusted urologist. Fear of future consequences was the most common reason to reject watchful waiting. Few men seemed aware of uncertainty and the notion that active treatment may not improve survival any better than watchful waiting.
Comparison with Existing Literature
Our study supports previous findings that patients often have an incomplete or inaccurate understanding of treatment options, do not use information systematically, and need patient-centered information to facilitate their decision making.10,11,17,18 In addition, processing medical information is influenced by previous beliefs about cancer and cure, and personal history factors.12,18
Consistent with Denberg et al,11 the anecdotal experiences of prostate cancer survivors among family and friends played an important role in the men’s treatment decisions. Contrary to previous reports that few patients sought a second opinion,10–12,17 a majority of our participants sought a second opinion. The different results may be related to the fact that most other study samples were from urology clinics only,10,11,17 while our sample included men recruited from radiation oncology offices as well. We found that men seeking a second opinion expressed the recognition that physicians were not infallible, whereas having faith and trust in doctors was associated with not seeking a second opinion.
Men who were aware of RAP believed it to be minimally invasive and more precise, thus reducing complications such as impotence and incontinence as compared with conventional open radical prostatectomy (ORP). Currently, there is lack of evidence to support these beliefs.19 Furthermore, the emerging literature suggests that the more costly RAP may result in more incontinence and impotence and lead men to regret their decision more than men who received ORP.20,21 Further research is particularly relevant because of soaring treatment costs of new, unproven technologies.
Little research has addressed racial/cultural differences in the treatment decision-making process.4 Blacks are known to report less trust in the health care system, which may contribute to health disparities.22 In our study, some black men mentioned their distrust of physicians or the health care system influenced their treatment decision. Some black men also emphasized the role of God/religion in helping them cope with the distress of their diagnosis and treatment decision making. Personality and education seem to have an effect on the decision-making process, such as in information gathering and the deliberation of treatment choices. Given the greater prostate cancer incidence and mortality among black men,1,7 studies are greatly needed to explore the decision- making process in black communities, especially those with lower socioeconomic status.
The above study findings are consistent with our conceptual model. This model describes a process whereby a combination of factors unique to each individual contributes to decisions regarding health behaviors, such as decisions about which treatment is most appropriate for localized prostate cancer. These decisions, in turn, influence their satisfaction with treatment and subsequent quality of life. Based on findings from this study, we suggest that, ultimately, treatment decisions are determined by the way an individual processes health information at the cognitive level (eg, a rational weighing of the pros and cons of a specific treatment option) and at the affective level (eg, fear of cancer progression and death). Furthermore, multiple cognitive and affective domains of health behavior, from attitudes and beliefs to self-efficacy and health locus of control, are all influential in individual men’s choice of treatment. These factors, along with the clinical factors (eg, tumor aggressiveness/prognosis, age, and comorbidity) on which clinicians generally base their treatment recommendations, 23 are all salient for men with prostate cancer.
Strengths and Limitations
Although small, our study provides new insights about the salient aspects of prostate cancer treatment decision-making experiences with a focus on black men. First, our interviews were conducted before or shortly after the men received treatment for localized prostate cancer, thus reducing the potential for recall bias that may occur based on a man’s experience with treatment outcomes. Second, our sample includes participants with a range of education and socioeconomic backgrounds who consulted primary care physicians and radiation oncologists in addition to urologists, in contrast to previous studies focusing on patients from urologist offices only.10,11 In addition, data saturation was reached for men who chose surgery and radiation, which suggests that all important factors were identified in these groups. Finally, our data collection and data analysis were guided by theoretical model, which provided us a comprehensive framework to accomplish our research aim by enhancing the breadth and completeness of our data.
However, generalizing these findings is limited by the exploratory nature of the study, the small sample size, and the sample characteristics. Although we reached saturation regarding the decision for surgery and radiation, it is possible that another sample drawn from older men may report a different experience. In addition, the study sample was drawn from English-speaking volunteers from one geographic area and may not be representative of other areas. However, the study aimed to contribute to theory development, questionnaire design, and hypothesis generation rather than seek “empirical generalizations.” Finally, there were only 2 men in our sample who chose watchful waiting; thus, we may not have reached data saturation with this group. Our study sample is younger (mean age, 58 years) than reported previously,10–12,17 which may explain the small number of men choosing watchful waiting. Despite these limitations, emergent themes from this research are likely to have universal applicability.
CONCLUSIONS
Here we report one of the first studies to include black men’s descriptions of their prostate cancer treatment decision-making process. While multiple factors influence men’s treatment decision, perceptions of efficacy and likely treatment side effects (either from physicians’ description or anecdotal experience of family and friends) are the most influential. Making “the best choice for me” takes into account the medical information gained from all sources plus the personal factors that men bring to the decision process.
In addition to providing evidence-based medical information, clinicians should assist patients to select a treatment choice that encompasses their individual concerns, values, and preferences regarding cancer recurrence and potential side effects. By understanding the factors that influence patients’ decision making, clinicians may be more sensitive to individual patients’ preferences and provide more patient-centered care.
Table 3.
Men’s Perceptions Regarding Radiation (External Radiation and Brachytherapy)
| Reasons Why Chosen | Reasons Why Not Chosen |
|---|---|
|
|
Acknowledgments
Funding/Support: This study was funded by American Cancer Society grant MRSGT-06-133-01-CPPB.
Role of the Sponsor: The funder had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Appendix. Interview Guide
|
References
- 1.American Cancer Society. Detailed Guide: Prostate Cancer. [Accessed March 16, 2010];What are the key statistics about prostate cancer? www.cancer.org/docroot/CRI/content/CRI_2_4_1X_What_are_the_key_statistics_for_prostate_cancer_36.asp?sitearea=
- 2.Welch HG, Albertsen PC. Prostate cancer diagnosis and treatment after the introduction of prostate-specific antigen screening: 1986–2005. J Natl Cancer Inst. 2009;101:1325–1329. doi: 10.1093/jnci/djp278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilt TJ, MacDonald R, Rutks I, Shamliyan TA, Taylor BC, Kane RL. Systematic review: comparative effectiveness and harms of treatments for clinically localized prostate cancer. Ann Intern Med. 2008;148:435–448. doi: 10.7326/0003-4819-148-6-200803180-00209. [DOI] [PubMed] [Google Scholar]
- 4.Zeliadt SB, Ramsey SD, Penson DF, et al. Why do men choose one treatment over another?: a review of patient decision making for localized prostate cancer. Cancer. 2006;106:1865–1874. doi: 10.1002/cncr.21822. [DOI] [PubMed] [Google Scholar]
- 5.Zeliadt SB, Potosky AL, Etzioni R, Ramsey SD, Penson DF. Racial disparity in primary and adjuvant treatment for nonmetastatic prostate cancer: SEER-Medicare trends 1991 to 1999. Urology. 2004;64:1171–1176. doi: 10.1016/j.urology.2004.07.037. [DOI] [PubMed] [Google Scholar]
- 6.Underwood W, III, Jackson J, Wei JT, et al. Racial treatment trends in localized/regional prostate carcinoma: 1992–1999. Cancer. 2005;103:538–545. doi: 10.1002/cncr.20796. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz K, Powell IJ, Underwood W, III, George J, Yee C, Banerjee M. Interplay of race, socioeconomic status, and treatment on survival of patients with prostate cancer. Urology. 2009;74:1296–1302. doi: 10.1016/j.urology.2009.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harlan SR, Cooperberg MR, Elkin EP, et al. Time trends and characteristics of men choosing watchful waiting for initial treatment of localized prostate cancer: results from CaPSURE. J Urol. 2003;170:1804–1807. doi: 10.1097/01.ju.0000091641.34674.11. [DOI] [PubMed] [Google Scholar]
- 9.Shavers VL, Brown ML, Potosky AL, et al. Race/ethnicity and the receipt of watchful waiting for the initial management of prostate cancer. J Gen Intern Med. 2004;19:146–155. doi: 10.1111/j.1525-1497.2004.30209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Rourke ME. Narrowing the options: the process of deciding on prostate cancer treatment. Cancer Invest. 1999;17:349–359. doi: 10.3109/07357909909032877. [DOI] [PubMed] [Google Scholar]
- 11.Denberg TD, Melhado TV, Steiner JF. Patient treatment preferences in localized prostate carcinoma: The influence of emotion, misconception, and anecdote. Cancer. 2006;107:620–630. doi: 10.1002/cncr.22033. [DOI] [PubMed] [Google Scholar]
- 12.Berry DL, Ellis WJ, Woods NF, Schwien C, Mullen KH, Yang C. Treatment decision-making by men with localized prostate cancer: the influence of personal factors. Urol Oncol. 2003;21:93–100. doi: 10.1016/s1078-1439(02)00209-0. [DOI] [PubMed] [Google Scholar]
- 13.Miller WL, Crabtree BF. Clinical research: a multimethod typology and qualitative roadmap. In: Crabtree BF, Miller WL, editors. Doing qualitative research. 2. Thousand Oaks, CA: Sage Publications; 1999. pp. 3–30. [Google Scholar]
- 14.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 15.Miller SM, Diefenbach MA. The Cognitive-Social Health Information Processing (C-SHIP) model: A theoretical framework for research in behavioral oncology. In: Krantz D, editor. Perspectives in Behavioral Medicine. Mahwah, NJ: Lawrence Erlbaum; 1998. pp. 219–244. [Google Scholar]
- 16.Strauss A, Corbin J. Basics of qualitative research: grounded theory - procedures and techniques. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- 17.O’Rourke ME, Germino BB. Prostate cancer treatment decisions: a focus group exploration. Oncol Nurs Forum. 1998;25:97–104. [PubMed] [Google Scholar]
- 18.Steginga SK, Occhipinti S, Gardiner RA, Yaxley J, Heathcote P. Making decisions about treatment for localized prostate cancer. BJU Int. 2002;89:255–260. doi: 10.1046/j.1464-4096.2001.01741.x. [DOI] [PubMed] [Google Scholar]
- 19.Murphy DG, Challacombe BJ, Costello AJ. Outcomes after robot-assisted laparoscopic radical prostatectomy. Asian J Androl. 2009;11:94–99. doi: 10.1038/aja.2008.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302:1557–1564. doi: 10.1001/jama.2009.1451. [DOI] [PubMed] [Google Scholar]
- 21.Schroeck FR, Krupski TL, Sun L, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2008;54:785–793. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- 22.Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health. 2009;99:1293–1299. doi: 10.2105/AJPH.2007.123927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thompson I, Thrasher JB, Aus G, et al. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007;177:2106–2131. doi: 10.1016/j.juro.2007.03.003. [DOI] [PubMed] [Google Scholar]