Abstract
Purpose
The purpose of the current study was to pilot-test a positive psychology intervention to improve adherence to diabetes management in adolescents with type 1 diabetes.
Methods
A total of 39 adolescents (ages, 13–17 years) with type 1 diabetes and their caregivers were randomized to a positive psychology intervention (n = 20) or an attention control (education) intervention (n = 19). The intervention condition used positive psychology exercises (eg, gratitude, self-affirmation), small gifts, and parent affirmations to boost positive affect. Outcomes included frequency of blood glucose monitoring, quality of life, and glycemic control.
Results
No main effects for treatment were observed at the 6-month follow-up. However, there was a significant association between adolescents’ levels of positive affect and measures of adherence, including self-report and meter downloads of glucose monitoring.
Conclusions
The results from the current study support the assertion that positive affect in the context of diabetes education is an important factor to consider in adolescents with type 1 diabetes.
Type 1 diabetes is one of the most common chronic childhood illnesses, affecting 1 in 400 youth, with a peak onset in adolescence.1 The adolescent and his or her family is responsible for the majority of treatment management, which is complex and demanding and can include checking blood sugar several times a day, administering insulin with shots or insulin pump multiple times a day, monitoring carbohydrate intake and activity levels, and making adjustments as necessary.2 During adolescence, glycemic control often deteriorates as a result of growth, hormonal changes, and problems with adherence. At a time of increasing independence from parents and desire to fit in with peers, the majority of adolescents (93%) report problems with adherence.3 Previous studies aimed at improving adherence in youth with type 1 diabetes have focused on problem solving,4 parent-child communication,5 and reminders,6 with modest to moderate effects. Novel approaches are needed; therefore, and a positive psychology intervention may be effective for this population.
There has been a recent focus on the effects of positive affect (PA) on health, and a review of the literature found that PA—or feelings that reflect pleasurable engagement with the environment—is related to favorable health outcomes.7 Furthermore, increases in PA have been shown to improve intrinsic motivation. For example, participants of an experimental study who experienced increased PA were willing to forgo enjoyable activities to engage in necessary tasks.8 One of the only studies to describe affect in relation to diabetes self-management found that adolescents’ reports of higher levels of PA were associated with greater perceived self-efficacy for diabetes tasks.9 Thus, PA has been associated with adolescents’ perceptions of their ability to perform diabetes tasks, such as blood glucose monitoring (BGM). The broaden-and-build hypothesis posits that increased PA offers a respite from chronic stress and allows individuals to use more complex coping strategies.10 Since coping is related to diabetes self-management in adolescents,11 increased PA may help them to apply more coping strategies to improve their self-management.
A recent meta-analysis of 51 intervention studies—including several with adolescents—demonstrated that positive psychology interventions are effective for enhancing well-being and reducing depressive symptoms,12 but none of these studies examined adherence to medical regimen as an outcome. Furthermore, none of the studies included youth with type 1 diabetes or any other pediatric health condition. Positive psychology interventions have been effective in improving adherence to medical regimens in adult populations; Charlson et al have conducted several clinical trials demonstrating that positive psychology interventions that induced PA improved adherence to treatment recommendations in adults with hypertension13 and cardiovascular disease,14 and these improvements were sustained over time.14 However, a positive psychology intervention has not been tested in a pediatric population. Based on the literature in adults, it is hypothesized that a positive psychology intervention to increase PA could improve adherence in adolescents with type 1 diabetes.
BGM, or testing blood sugar, is one of the best indicators of adherence to the intensive treatment regimen recommended for type 1 diabetes; these tests provide the information needed to make decisions about insulin adjustments, carbohydrate intake, and exercise.15 Frequency of BGM is also strongly related to glycemic control.16 Therefore, BGM represents a specific behavior that may be targeted by adherence interventions in youth with type 1 diabetes. Using positive psychology exercises to induce PA, the current study was aimed at improving adherence to treatment recommendations—specifically, increased BGM—in adolescents with type 1 diabetes.
Current Study
The purpose of the current study was to pilot-test the feasibility and acceptability of a positive psychology intervention to improve adherence to diabetes management in adolescents with type 1 diabetes. In addition, the preliminary efficacy of the intervention on family conflict, quality of life, and glycemic control was evaluated. Finally, the association between changes in PA and adherence was explored.
Methods
Participants
Adolescents were eligible for the study if they were between the ages of 13 and 17 years, able to speak and read English, had no other major medical conditions, and had been diagnosed with type 1 diabetes for at least 6 months. The adolescents’ parents or guardians were eligible to participate if they lived with the adolescent and were able to speak and read English.
Procedure
Participants were recruited from an outpatient pediatric diabetes clinic during regularly scheduled visits. In line with university institutional review board requirements, consent and assent forms were completed by the parent and adolescent, respectively.
Research Design
After completing baseline data, adolescents and their parents were randomly assigned to either the PA or attention control–education (EDU) condition. The randomization scheme was determined by a computer program in 4 blocks of 10.
PA Intervention
Following the protocol that has been successful in adults with chronic illness,17 the PA intervention was designed to increase PA through gratitude, self-affirmation, small gifts, and parental affirmations. At the time of enrollment, adolescents in the PA condition completed a PA interview, consisting of a series of questions to identify topics for positive psychology exercises, including gratitude (“What are some things that make you happy, even for a moment?”) and self-affirmation (“What’s something that you are proud of?”). Adolescents also selected their preference from a list of small gifts worth about $3 (eg, drawstring bag, water bottle), and one preferred gift was mailed every 2 weeks during the 8-week intervention. Adolescents’ parents were instructed to provide weekly affirmations to adolescents on topics other than diabetes self-care by writing a short note or sending a text message (eg, “Great job in your soccer game last night”). Adolescents were given instructions to take a moment to notice things that made them happy (gratitude) and to remember something that they were proud of (self-affirmation) when it was time to check their blood sugar. They were reminded to use gratitude and self-affirmation during phone calls (every 2 weeks during the 8-week intervention).
EDU Intervention
Adolescents randomized to the attention control (EDU) group were mailed diabetes educational materials every 2 weeks for 8 weeks (on the same schedule as PA group mailings). The educational materials consisted of brief (3-page) packets with developmentally appropriate information from the American Diabetes Association website, on topics such as hypoglycemia, hyperglycemia, driving and diabetes, and exercise.
Measures
Adolescents and their parents completed questionnaires at baseline, 3 months, and 6 months. Parents completed the demographics form at baseline only. In addition, all adolescents were called every 2 weeks for 8 weeks, during which they completed validated measures of affect and diabetes management over the phone.
The Positive and Negative Affect Scale18 was used to measure participants’ affect. The measure consists of two 10-item scales: a positive construct (interested, excited, strong, enthusiastic, proud, alert, inspired, determined, attentive, active) and a negative construct (distressed, upset, guilty, scared, hostile, irritable, ashamed, nervous, jittery, afraid). Participants were asked to rate to what extent they experienced each emotion over the past week, on a scale of 1 (very slightly or not at all) to 5 (extremely). Scores range from 10 to 50, with higher scores indicating higher levels of affect. In the current study, internal consistency was α = .77 for PA and .85 for negative affect in adolescents.
Because adolescent or parent depression could have a confounding effect on participation or response to the intervention, data were collected on depressive symptoms. The Children’s Depression Inventory19 was used to measure adolescents’ current depressive symptoms. The inventory consists of 27 items, with scores ranging from 0 to 54, and higher scores indicate higher levels of depression. In the current study, internal consistency was α = .88 for adolescents. The Center for Epidemiologic Studies of Depression Scale20 was used to measure depressive symptoms in parents. This questionnaire consists of 20 items scored on a scale of 0 to 3. Similar to the Children’s Depression Inventory, as the score increases, the likelihood of current levels of depression increases, with a range from 0 to 60. In the current study, internal consistency was α = .90 for parents.
The Self Care Inventory (SCI)21 was used to assess adolescents’ and parents’ perceptions of how well adolescents were adhering to treatment recommendations for their diabetes care. The overall adherence score is based on the average of 7 of the 14 items administered, which include the items most strongly linked to better diabetes management and control. A mean score is created, ranging from 1 (never do it) to 5 (always do this as recommended without fail). In the current study, internal consistency was α = .75 for adolescents’ self-report and α = .79 for parents’ report. The Blood Glucose Regulation subscale was also used, which consists of 3 items (glucose testing, glucose recording, and adjusting insulin intake based on blood glucose values). Internal consistency for the Blood Glucose Regulation subscale was α = .62 for adolescents and α = .60 for parents.
The Diabetes Family Conflict scale,22 a 15-item instrument, was completed by adolescents and parents to evaluate parent-child conflict related to diabetes management. It is based on a scale of 1 (almost never) to 3 (almost always), with a range of 15 to 45; higher scores indicate greater conflict between the adolescent and parent. In the current study, internal consistency was α = .97 for adolescents and α = .87 for parents.
The Pediatric Quality of Life Inventory Type 1 Diabetes Module23 was used to determine the adolescents’ quality of life in relation to diabetes. It consists of 28 items, with a standardized score ranging from 0 to 100. Higher scores indicate better quality of life. In the current study, internal consistency was α = .86 for adolescents.
The mean frequency of BGM over the previous week was used as a measure of adherence.24 The American Diabetes Association recommends that adolescents with type 1 diabetes check blood glucose at least 4 times a day.2 The mean BGM was obtained by downloading the adolescents’ glucose meter at the time of enrollment (if possible) and at 3- and 6-month follow-up visits. If adolescents did not bring their meters to the clinic, self-report was used in 3% (n = 1) at 3 months and 5% (n = 2) at 6 months. As an added incentive, adolescents were compensated with $10 gift cards if they remembered to bring their meters to each clinical visit.
Glycemic control was determined by glycosylated hemoglobin (A1C) levels, which is an average of blood glucose levels over the prior 8 to 12 weeks. The goal range for adolescents with type 1 diabetes is < 7.5%.2 Analyses were performed with the Bayer Diagnostics DCA2000® machine, which provides results in 6 minutes on a fingerstick blood sample (normal range = 4.2%–6.3%).
Data Analysis
To determine if there were significant differences between groups, the PA and EDU groups were compared on baseline measures via t tests or chi-square analyses as appropriate (see Table 1). To determine the effect of the intervention, mixed-effects models were used to take into account correlation among outcomes repeatedly measured within the same subject. The models included the baseline measurement for each outcome, family income, adolescent depressive symptoms at baseline, and time variable, to adjust for their potential confounding effects in the analysis. In addition, bivariate correlations were used to examine the association between PA (as reported at the end of the 8-week intervention) and measures of adherence (SCI and BGM) and glycemic control (ie, A1C) at 3- and 6-month follow-up. As this was a pilot study, there was not enough power to detect significant effects; however, results provide estimates of preliminary efficacy and the variability of outcome measurements that will be extremely useful to design a larger study with adequate power.
Table 1.
Comparison of Demographic and Baseline Clinical Characteristics by Group
| Variables | Positive Affect (n = 20)
|
Education (n = 19)
|
||
|---|---|---|---|---|
| No. | % | No. | % | |
| Sex | ||||
| Male | 8 | 40.0 | 11 | 58.0 |
| Female | 12 | 60.0 | 8 | 42.0 |
| Race/ethnicity | ||||
| White | 13 | 65.0 | 17 | 94.0a |
| Non-white | 7 | 35.0 | 1 | 6.0a |
| Annual family income, US$ | ||||
| < 79 000 | 11 | 42.0a | 14 | 78.0a |
| > 80 000 | 8 | 58.0a | 4 | 22.0a |
| Therapy type | ||||
| Pump | 13 | 68.0a | 16 | 84.0 |
| Injection | 6 | 32.0a | 3 | 16.0 |
|
| ||||
| Mean ± SD | Range | Mean ± SD | Range | |
|
| ||||
| Age, y | 15.3 ± 1.4 | 13–17 | 15.0 ± 1.6 | 13–17 |
| Duration, y | 7.3 ± 4.3 | 0–14 | 6.5 ± 3.5 | 0–12 |
| A1C at baseline, % | 8.5 ± 1.1 | 7.0–11.0 | 8.2 ± 1.0 | 7.0–11.0 |
| CDI score | 8.6 ± 6.8 | 0.0–21.0 | 3.0 ± 4.4 | 0.0–16.0 |
| CES-D score | 10.7 ± 9.7 | 0.0–32.0 | 6.4 ± 5.0 | 0.0–16.0 |
| PedsQL score DFC score | 53.6 ± 13.7 | 30.0–82.0 | 66.7 ± 14.7 | 36.0–91.0 |
| Adult | 25.5 ± 10.1 | 15.0–51.0 | 24.9 ± 6.3 | 18.0–40.0 |
| Teen | 36.8 ± 18.6 | 15.0–72.0 | 29.9 ± 20.1 | 15.0–74.0 |
| SCI | ||||
| Total score | ||||
| Adult | 3.40 ± 0.77 | 1.0–5.0 | 4.0 ± 0.41 | 3.0–4.0 |
| Teen | 3.46 ± 0.65 | 2.0–5.0 | 4.0 ± 0.70 | 2.0–5.0 |
| Blood glucose regulation | ||||
| Adult | 3.38 ± 0.92 | 1.0–5.0 | 3.94 ± 0.54 | 3.0–5.0 |
| Teen | 3.34 ± 0.89 | 2.0–5.0 | 3.72 ± 0.79 | 2.0–5.0 |
| Mean BGM | 3.76 ± 1.47 | 1.0–6.0 | 4.36 ± 1.79 | 2.0–8.0 |
Abbreviations: BGM, blood glucose monitoring; CDI, Children’s Depression Inventory; CES-D, Center for Epidemiologic Studies of Depression Scale; DFC, Diabetes Family Conflict scale; PedsQL, Pediatric Quality of Life Inventory Type 1 Diabetes Module; SCI, Self Care Inventory.
Valid percentage accounting for missing values.
Results
In total, 73 families were approached: 9 did not meet the eligibility criteria; 16 refused to participate (most common reasons were time and lack of interest); 8 expressed interest in participating at a future date; and 40 were enrolled in the study. One adolescent was later determined not to be eligible due to an additional medical condition; therefore, the number of participants included in analyses was 39 (see Figure 1). There were no demographic differences between adolescents who did and did not choose to participate.
Figure 1.

CONSORT diagram.
As seen in Table 1, the sample was predominantly white, non-Hispanic, and of moderate-high income, with an adolescent mean age of 15 and mean A1C of 8.3%. Adolescents reported good adherence overall, with a mean overall adherence score of 3.7 (indicating that they usually follow the treatment regimen as recommended, with occasional lapses), and a range of daily BGM from 1 to 8 (mean = 4 times/day).
Feasibility
Participation in all components of the intervention was high: 90% of adolescents in the PA group reported receiving all 4 gifts, and 89% of adolescents in the EDU group reported receiving all 4 packets. Furthermore, participation in phone call data collection was good: 75% (n = 15) of adolescents in the PA group and 90% (n = 17) of adolescents in the EDU group completed at least 3 of 4 phone calls. Overall, retention was excellent in both groups: 19 of 20 participants in the PA group (95%) completed follow-up data at 3 and 6 months, and 18 of 19 participants in the EDU group (95%) completed follow-up data at 3 and 6 months.
Adherence
In terms of adherence, there was a significant mean difference in adolescents’ self-report of regulating blood glucose (on the SCI) (mean difference = −.56; 95% confidence interval [CI] = −.87, −.25; P < .001) such that the adolescents in the EDU group reported significantly greater BGM over 6 months. There was no significant difference between groups in the average of adolescent and parent reports on the Blood Glucose Regulating subscale (mean difference = −.19; 95% CI = −.47, .09; P = .193). However, there was greater variability in the PA group than in the EDU group; as seen in Figure 2, improvements in blood glucose regulation leveled off after the active phase of the intervention.
Figure 2.
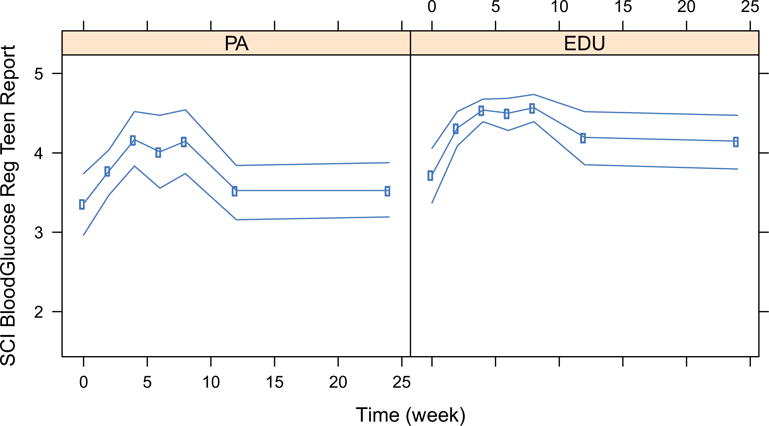
Self-reported blood glucose regulation by week. Circles represent the means and upper and lower lines represent the corresponding 95% confidence limits obtained using nonparametric bootstrap without assuming normality.
There was no significant difference in the means of average daily BGM (based on meter download) between the 2 groups (mean difference = −0.5; 95% CI = −1.5, to 0.5; P = .324).
Family Conflict, Quality of Life, and Glycemic Control
There was no significant difference in the means of diabetes-related family conflict between the 2 groups (mean difference = .01; 95% CI = −0.20, 0.22 for parent and adolescent report; P = .924), diabetes quality of life (mean difference = 4.1; 95% CI = −4.3, 12.5; P = .336), or glycemic control (mean difference = .02; 95% CI = −0.04, 0.08; P = .472).
PA and Adherence Measures
Bivariate correlations were conducted to examine the association between PA and measures of adherence (SCI, mean BGM) and A1C. Higher rates of PA (reported in the final week of the intervention) were related to better self-reported overall adherence (SCI) and better self-reported glucose monitoring (SCI-BGM) in the PA group, as well as greater frequency of BGM, obtained from glucose meter (see Table 2).
Table 2.
Bivariate Correlations of Positive Affect Postintervention With Adherence Measures
| Outcome Variables | Positive Affect Groupa | Education Group |
|---|---|---|
| SCI | ||
| 3 mo | .51** | .50* |
| 6 mo | .62* | .54* |
| SCI BGM | ||
| 3 mo | .52* | .19 |
| 6 mo | .51** | .39 |
| Mean BGMb | ||
| 3 mo | .25 | .42 |
| 6 mo | .61* | .22 |
Abbreviations: BGM, blood glucose monitoring; SCI, Self Care Inventory.
Positive affect intervention was measured in the last week of the 8-week intervention.
Meter download.
P < .05.
P < .01.
Discussion
Adolescents with type 1 diabetes are at risk for suboptimal glycemic control, and novel approaches are needed to improve their adherence to the complex treatment regimen.3 The current study is believed to be the first to use a positive psychology intervention aimed at improving adherence in a pediatric population. The high rates of participation and retention indicate that the study was feasible and acceptable to adolescents with type 1 diabetes and their parents. Contrary to the hypothesis, the PA intervention did not result in significant improvements in glucose monitoring. However, a significant association was found between adolescents’ level of PA with measures of adherence, including both self-report and meter downloads, supporting the assertion that PA is an important factor to consider in adolescents with type 1 diabetes.
As illustrated in Figure 2, both groups improved BGM initially, but this waned over time. This finding is in line with results from an intervention for adolescents with type 1 diabetes consisting of text-messaging reminders to check blood glucose, in which adolescents showed initial improvements in BGM that were not sustained over time (3 months).6 Interventions that provide more contact over time may therefore be needed to sustain improvements and demonstrate differences between groups.
Frequency of BGM has been shown to decrease with age in adolescents,25 and parental reminders to check blood glucose are a frequent source of conflict between adolescents and their parents.26 This positive psychology intervention was aimed at increasing frequency of BGM in adolescents without requiring additional reminders from parents. In this way, the intervention was designed to minimize parent-child conflict around this necessary task and improve quality of life. There was not a significant change in diabetes-related family conflict, but this may be due to the fact that diabetes-related conflict was relatively low at baseline.
Surprisingly, the adolescents in the attention control group, who received EDU packets, improved on measures of self-reported adherence. These findings suggest that adolescents may benefit from developmentally appropriate diabetes EDU, and it may be important to include EDU in addition to PA to enhance adherence. In previous studies with adults, the PA interventions also included EDU to promote adherence to the treatment regimen.27 However, the improvement in self-reported adherence may be an artifact of the study design. The adolescents were contacted biweekly to complete a measure of adherence over the phone, and it is possible that they were inflating estimates of adherence. Alternatively, the phone calls may have been an active part of the intervention. Since adolescents knew that they would be reporting about diabetes management, it may have had an effect on their behavior.
Another important consideration is that, despite random assignment, there were differences between groups on several key variables at baseline, including adolescent and parental depressive symptoms, income, and race/ethnicity. Although depressive symptoms were controlled for in the analyses, it is still likely that some of the baseline differences had a confounding effect on the impact of the intervention. It is possible that PA inducement is not effective for adolescents who are depressed. A larger sample size with greater variability is needed to determine if these results will generalize. Based on results from the current study, the intervention protocol may need to be revised to include EDU, more frequent contact to remind youth to use PA exercises (weekly instead of biweekly), and a longer follow-up period to determine if improvements can be sustained over time.
Limitations
The current study was a pilot study, so the sample size does not allow for a robust test of efficacy. It is limited by the demographics of the diabetes clinic, with fairly high socioeconomic status and good glycemic control, and results may not generalize to other populations. Finally, despite random assignment, there were significant demographic and clinical differences between the groups, including family income and depressive symptoms in parents and adolescents. These variables were controlled for in the analyses, but baseline depressive symptoms may have limited the effects of the interventions.
Implications
Despite study limitations, further development and evaluation of positive psychology interventions for youth with type 1 diabetes are indicated. Significant associations between PA and measures of adherence were demonstrated. In addition, the high levels of participation and retention indicate that adolescents and their parents were receptive to a positive psychology approach,26 which places an emphasis on positive emotions and strengths, rather than problems. While many diabetes educators may already incorporate principles of positive psychology, the current study supports that providers should consider asking about positive aspects of adolescents’ lives (eg, “What makes you happy? What are you proud of?”), in addition to the typical focus on diabetes-related challenges and glycemic control. In summary, adolescents with type 1 diabetes were receptive to the intervention and may demonstrate improved diabetes-related outcomes from a positive psychology intervention in the context of diabetes EDU.
Acknowledgments
Funding: This research was supported in part by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (DP3DK097678, K23DK088454) and the Yale School of Nursing.
Footnotes
For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav.
References
- 1.Liese AD. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118:1510–1518. doi: 10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Standards of medical care in diabetes: 2013. Diabetes Care. 2013;35:S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borus JA, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22:405–411. doi: 10.1097/MOP.0b013e32833a46a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mulvaney SA, Rothman RL, Wallston KA, Lybarger C, Dietrich MS. An Internet-based program to improve self-managmenet in adolescents with type 1 diabetes. Diabetes Care. 2010;33:602–604. doi: 10.2337/dc09-1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wysocki T, Harris MA, Buckloh LM, et al. Randomized trial of behavioral family systems therapy for diabetes: maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30:555–560. doi: 10.2337/dc06-1613. [DOI] [PubMed] [Google Scholar]
- 6.Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11:99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131:925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 8.Isen AM, Reeve J. The influence of positive affect on intrinsic and extrinsic motivation: facilitation enjoyment of play, responsible work behavior, and self-control. Motiv Emotion. 2005;29:297–325. [Google Scholar]
- 9.Fortenberry KT, Butler JM, Butner J, Berg CA, Upchurch R, Wiebe DJ. Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Ann Behav Med. 2009;37:1–9. doi: 10.1007/s12160-009-9086-7. [DOI] [PubMed] [Google Scholar]
- 10.Fredrickson BL. The role of positive emotions in positive psychology: the broaden-and-build hypothesis of positive emotions. Am Psychol. 2001;56:218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaser SS, Faulkner MS, Whittemore R, et al. Coping, self-management, and adaptation in adolescents with type 1 diabetes. Ann Behav Med. 2012;43:311–319. doi: 10.1007/s12160-012-9343-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol. 2009;65:467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- 13.Ogedegbe GO, Boutin-Foster C, Wells MT, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 2012;172:322–326. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson JC, Charlson ME, Hoffman Z, et al. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med. 2012;172:329–336. doi: 10.1001/archinternmed.2011.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silverstein JH, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes. Diabetes Care. 2005;28:184–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 16.Haller MJ, Stalvey MS, Silverstein JH. Predictors of control of diabetes: monitoring may be the key. J Pediatr. 2004;144:660–661. doi: 10.1016/j.jpeds.2003.12.042. [DOI] [PubMed] [Google Scholar]
- 17.Charlson ME, Boutin-Foster C, Mancuso CA, et al. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: rationale, trial design, and methods. Contemp Clin Trials. 2007;28:748–762. doi: 10.1016/j.cct.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Watson D, Clark LA. Development and validation of a brief measure of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 19.Kovacs M. The Children’s Depression Inventory (CDI) Psychopharm Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 21.La Greca A. Manual for the Self Care Inventory. Miami, FL: University of Miami; 2004. [Google Scholar]
- 22.Rubin RR, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38(suppl 2):28A. [Google Scholar]
- 23.Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The PedsQL in type 1 and type 2 diabetes: reliability and validity of the Pediatric Quality of Life Inventory Generic Core Scales and Type 1 Diabetes Module. Diabetes Care. 2003;26:631–637. doi: 10.2337/diacare.26.3.631. [DOI] [PubMed] [Google Scholar]
- 24.Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatr. 2010;124:1171–1179. doi: 10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- 25.Ingerski LM, Anderson BJ, Dolan LM, Hood KK. Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. J Adolesc Health. 2010;47:191–197. doi: 10.1016/j.jadohealth.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schilling LS, Knafl KA, Grey M. Changing patterns of self-management in youth with type 1 diabetes. J Pediatr Nurs. 2006;21:412–424. doi: 10.1016/j.pedn.2006.01.034. [DOI] [PubMed] [Google Scholar]
- 27.Charlson ME, Boutin-Foster C, Mancuso CA, et al. Three randomized controlled trials of positive affect and self-affirmation to facilitate health behavior changes in patients with cardiopulmonary diseases; Paper presented at: Society of Behavioral Medicine Annual Meeting; 2009; Montreal, Canada. [Google Scholar]


