Abstract
Sustained parental involvement in diabetes management has been generally advised to counteract the deteriorating adherence and glycemic control often seen during adolescence, yet until recently, little attention has been given to the optimal amount, type, and quality of parental involvement to promote the best health outcomes for adolescents with type 1 diabetes (T1D). This review synthesizes research regarding the involvement of caregivers—primarily mothers and fathers—of youth with T1D, with a focus on biopsychosocial outcomes. The recent literature on parental involvement in diabetes management highlights a shift in focus from not only amount but also the types (e.g., monitoring, problem-solving) and quality (e.g., warm, critical) of involvement in both mothers and fathers. We provide recommendations for ways that both parents can remain involved to facilitate greater collaboration in shared direct and indirect responsibility for diabetes care and improve outcomes in youth with T1D.
Keywords: Adolescence, Type 1 diabetes, Parenting, Involvement, Responsibility, Monitoring, Collaboration, Quality, Adherence, Maternal, Paternal
Introduction
Type 1 diabetes (T1D) is a chronic condition that redefines the lives of the entire family upon diagnosis due to the demanding treatment regimen recommended to achieve and maintain glycemic control [1]. In pediatric populations, parental involvement in diabetes management is essential to the maintenance of psychological health, glycemic control, and the development of self-care behaviors in youth [2]. Youth typically take on more responsibility for diabetes care as they reach adolescence, but if this increase in responsibility is not accompanied by a growth in maturity and self-efficacy, adherence and glycemic control may deteriorate [3, 4••]. Sustained parental involvement in the management of diabetes throughout adolescence has been generally advised to counteract these declines, yet identifying the optimal amount, type, and interpersonal quality of involvement is necessary for more precise recommendations and interventions.
While caregivers can include biological, foster, adoptive, stepparents, grandparents, or other relatives, previous research in pediatric diabetes has focused mainly on mothers as the primary caregiver (i.e., the parent who is directly involved in the routine tasks of caring for a child with T1D) [5]. Recent studies in children with T1D and other chronic illnesses have begun to include fathers as well, who play a different, but still vital, role in their children’s care [6]. For example, fathers may affect health outcomes indirectly by offering support and stability to the family as a whole [6]. In T1D specifically, fathers’ helpfulness and amount of involvement have been linked to better treatment adherence and quality of life in children [7] as well as fewer psychiatric symptoms in mothers [8]. It is important to consider the role of different types of caregivers in relation to diabetes outcomes and psychological adjustment in youth, but the literature on alternative caregivers is quite limited. Therefore, we concentrate our review primarily on studies with mothers or fathers.
The purpose of this narrative review is to synthesize recent empirical evidence regarding the involvement of mothers and fathers of youth with T1D, with a focus on adolescents’ biopsychosocial outcomes. We explore recent literature on the amount, type, and quality of parental involvement in diabetes care, along with the risks and benefits of sustained involvement throughout adolescence. In addition, we discuss how being a part of a single-parent family may impact parental involvement and diabetes-related outcomes. In many families, parents take on a role of “good cop” or “bad cop” depending on the type and quality of their involvement. While the police metaphor may not be appropriate for all families, the image of good cop/bad cop in popular culture is one to which many parents can relate. Parenting a child with T1D requires vigilant monitoring, regulation, and enforcement of certain care behaviors with the goal of protection from negative health outcomes, just as police monitor, regulate, and enforce the laws of the community. In this paper, good cop refers to a parent whose involvement is supportive and collaborative and bad cop refers to a parent whose involvement is critical and intrusive. However, educating families on the importance of both parents’ high-quality involvement—rather than each parent taking on a separate good cop or bad cop role—may facilitate greater collaboration in shared responsibility for diabetes care and improve outcomes in youth with T1D. Studies included in this review were categorized into several broader constructs of involvement in diabetes management: parental responsibility for diabetes management tasks, monitoring, and the interpersonal quality of involvement (see Table 1).
Table 1.
Studies included in review of parental involvement
| Study (year) | Study design | Sample size | Child Age (Years) |
Caregiver involved | Type of Parental Involvement |
Measure(s) of Involvement |
|---|---|---|---|---|---|---|
| Helgeson et al. [2] (2008) | Longitudinal | 132 | 10–14 | Caregivers (92 % mothers) | Parental responsibility | Diabetes Family Responsibility Questionnaire (DFRQ) |
| Wysocki et al. [3] (2009) | Cross-sectional | 309 | 9–14 | Primary caregivers (87 % mothers/stepmothers, 12 % fathers/stepfathers, 1 % other) and secondary caregivers (82 % fathers/stepfathers, 13 % mothers/stepmothers, 3 %grandmothers, 2 % aunts) | Parental responsibility; Collaborative involvement | DFRQ; Collaborative Parent Involvement Scale (CPI) |
| Wiebe et al. [4••] (2014) | Longitudinal | 252 | 10–14 | Mothers (n=252) and fathers (n=188) | Parental responsibility | Diabetes Responsibility Scale |
| King et al. [9] (2014) | Longitudinal | 252 | 10–14 | Mothers (n=252) and fathers (n=188) | Diabetes monitoring; behavioral involvement in diabetes care; Quality of parent-adolescent relationship | Diabetes-Specific Monitoring Scale; adolescent report of parents' behavioral involvement in diabetes management (2 items); acceptance subscale of the Mother-Father-Peer Scale (MFP) |
| Berg et al. [10] (2013) | Longitudinal | 180 | 10–15 | Mothers (n=176) and fathers (n=139) | Parental monitoring, parental responsibility, intrusive support | Diabetes-Specific Monitoring Scale; Diabetes Responsibility and Conflict Scale—revised (DRC-R); Daily Diary measure; Intrusive Support Scale; |
| Hilliard et al. [11] (2011) | Cross-sectional | 136 | 9–12 | Fathers | Helpfulness and frequency of paternal involvement | DADS |
| Hansen et al. [12•] (2012) | Cross-sectional | 89 | 7–14 | Fathers | Helpfulness and frquency of paternal involvement | Dads’ Active Disease Support Scale (DADS) |
| Hilliard et al. [13••] (2014) | Longitudinal | 136 | 9–12 | Fathers | Helpfulness and frequency of paternal involvement | DADS |
| Berg et al. [14•] (2011) | Cross-sectional | 252 | 10–14 | Mothers father* | Relationship quality quality (parental acceptance and independence encouragement); Monitoring; Behavioral involvement | MFP; General monitoring and diabetes monitoring scales; Intrusive Support Scale and two items assessing frequency of parental assistance with diabetes tasks |
| King et al. [15••] (2012) | Longitudinal | 252 | 10–14 | Mothers and fathers* | Diabetes monitoring; Acceptance; Behavioral involvement in diabetes management | Diabetes-specific monitoring; acceptance subscale of the MFP; adolescent-report of parents' behavioral involvement in diabetes management (2 items); |
| Hsin et al. [16] (2010) | Cross-sectional | 111 | 10–17 | Caregiver (83 % mothers) | Parental responsibility; Diabetes-specific family support | DRFQ; Diabetes Social Support Questionnaire-Family (DSSQ-Fa) |
| Ingerski et al. [17] (2010) | Longitudinal | 147 | 13–18 | Caregiver (83 % mothers) | Parental responsibility; Diabetes-specific family conflict | DFRQ; Diabetes Family Conflict Scale (DFCS) |
| Vesco et al. [18] (2010) | Cross-sectional | 261 | 13–18 | Caregivers (78% mothers) | Diabetes responsibility sharing (direct and indirect management tasks) | DFRQ |
| Palmer et al. [19] (2009) | Cross-sectional | 185 | 10–14 | Mothers (N=185) and fathers (N=145) | Diabetes responsibility sharing | The responsibility items of the DRCS |
| Berg et al. [21] (2008) | Cross-sectional | 84 | 10–14 | Mothers (n=185) and fathers (n=145) | Parental monitoring Acceptance, | Parental Monitoring Scale; acceptance subscale of the MFP |
| Horton et al. [22] (2009) | Cross-sectional | 252 | 10–14 | Mothers and fathers* | General and diabetes related monitoring | Scale of general parental monitoring; Diabetes specific scale of parental monitoring |
| Hilliard et al. [23•] (2013) | Cross-sectional | 257 | 11–14 | Caregiver (91 % mothers) | Monitoring; Diabetes-specific family conflict | 24 Hour Diabetes Interview (DI) and Parental Monitoring of Diabetes Care scale (PMDC); DFCS-R DFRQ; PMDC and DI |
| Robinson et al. [24] (2011) | Longitudinal | 255 | 11–14 | Caregiver (92% mothers) | Parental responsibility; Monitoring | DFRQ; PMDC and DI |
| Palmer et al. [25] (2011) | Cross-sectional | 252 | 10–14 | Mothers and fathers* | Relationship quality (acceptance, independence encouragement, communication); Behavioral involvement (intrusive support, frequency of help); Monitoring | (MFP) and the communication subscale of parent and peer attachment; Intrusive Support Scale and two items assessing frequency of parental assistance with diabetes tasks; General parental monitoring scale adapted for diabetes care behavior |
| Jaser et al. [26] (2010) | Observational | 30 | 10–16 | Mothers | Quality of parent-child communication | Videotaped interactions coded using the Iowa Family Interaction Rating Scales (IFIRS) for hostility, parental influence; sensitive/child centered, positive reinforcement |
| Lloyd et al. [27] (2009) | Cross-sectional | 50 | 13–17 | Mothers* | Maternal empathy | Child Empathy Questionnaire |
| Mlynarczyk et al. [28] (2013) | Cross-sectional | 102 | 12–18 | Mothers and fathers* | Parental support; Parenting style | Diabetes-Specific Parental Support for Adolescents’ Autonomy Scale; Parenting Style Index-II |
| Geffken et al. [29] (2008) | Cross-sectional | 100 | 7–18 | Caregivers (unspecified) | Diabetes-specific family support; Parental responsibility | Diabetes Family Behavior Scale (DFBS); Diabetes Family Behavior Checklist (DFBC); |
| Shorer et al. [30] (2011) | Cross-sectional | 100 | 11–18 | Mothers (N=79) and fathers (N=63) | Parenting style | Parental Authority Questionnaire |
| Greene [31] (2010) | Cross-sectional | 29 | 10–18 | Mothers (n=29) and fathers (n=29) | Parenting style | Parenting Practices Report |
| Nansel et al. [32] (2009) | Cross-sectional | 122 | 9–14.5 | Primary caregivers (87% mothers) and Secondary caregivers (82% fathers) | Collaborative involvement; Parental responsibility | Authoritative Parenting Index; DFRQ |
| Weissberg-Benchell et al. [33] (2009) | Cross-sectional | 121 | 9–14 | Primary caregiver (92% mothers) | Parenting style; Parent-child Conflict; Parental responsibility; collaborative parent involvement; Qulity of parent-child communication** | Authoritative Parenting Index; Parental authority scale; Diabetes Conflict Scale; DFRQ; CPI Videotaped interactions coded using the Interaction Behavior Code (IBC) |
| Butner et al. [34] (2009) | Cross-sectional | 185 | 10–14 | Mothers (n=185) and fathers (n=145) | Parental encouragement of adolescents’ independence; parental responsibility | Independence–encouragement subscale from the MFP; DRC |
| Osborn et al. [35] (2013) | Longitudinal | 183 | 10–14 | Mothers (N=178) and fathers (N=134) | Parental knowledge | Diabetes-Specific Monitoring Scale |
| Weinger et al. [36] (2001) | Qualitative | 24 | 13–15 | Mothers and fathers* | Diabetes-related conflict; Parental support | Qualitative analysis of focus group data |
| Hood et al. [37] (2007) | Cross-sectional | 202 | 8–18 | Caregiver 76% mothers | Diabetes-related conflict | DFCS |
| Lewin et al. [38] (2006) | Cross-sectional | 109 | 8–18 | Caregiver (82% mothers) | Adolescents’ perceived family support; Quality of parental behaviors; Parental Responsibility | DFBS; DFBC; DFRQ; |
| Cameron et al. [39] (2008) | Cross-sectional | 2,062 | 11–18 | Caregiver (77% mothers) | Adolescents’ perceived over-involvement; Parental responsibility | Parental involvement scale from the Diabetes Quality of Life for Youth-Short Form (DQOLY-SF); DFRQ |
| Duke et al. [40] (2008) | Cross-sectional | 120 | 8–18 | Caregivers (78 % mothers | Adolescents’ Perceived family support; Quality of parental behaviors | DFBS; DFBC |
| Sweenie et al. [41] (2014) | Cross-sectional | 86 | 9–11 | Primary Caregiver (93 % mothers) | Critical parenting behaviors | DFBC |
| Seiffge-Krenke et al. [42] (2013) | Longitudinal | 109 | 14–16 | Mothers and fathers* | Family restrictiveness; Parental support | Family Environment Scale (FES); Network of Relationships Inventory (abbreviated) |
| Butler et al. [43] (2007) | Cross-sectional | 78 | 11–17 | Mothers | Parenting style (psychological control, firm control, acceptance) | Parent Behavior Inventory |
| Armstrong et al. [44•] (2011) | Cross-sectional | 84 | 9–11 | Mothers and fathers* | Critical parenting behaviors | (DFBC) |
| Ivey et al. [45] (2,009) | Qualitative | 28 | 11–15 | Mothers and fathers | Quality of parent adolescent communication | Content analysis of interaction transcripts |
| Dashiff et al. [50] (2011) | Qualitative | 23 | 16–18 | Mothers, fathers, stepparents | Support for adolescent’s self-management | Qualitative analyses of interviews |
Note.
Adolescent report of caregiver involvement.
Parental Responsibility for Diabetes Management Tasks
Parental responsibility refers to the extent to which parents assist with diabetes care behaviors either directly (e.g., assisting with administering insulin injections) or indirectly (e.g., remembering clinic appointments, checking expiration dates). This type of parental involvement typically declines throughout adolescence, which may contribute to the problems with adherence [9] and deteriorating glycemic control often observed during this developmental stage [2].
Research shows that parents may take over responsibility for diabetes care for a number of reasons, some of which differ between mothers and fathers. For example, a recent study determined that parents’ direct involvement in daily diabetes management was associated with the number of problems their adolescents experienced with diabetes tasks, and this association was mediated in both mothers and fathers by increased worry and diminished confidence in their child’s ability to manage diabetes effectively [10]. In terms of parents’ differing motivations for involvement, mothers generally serve as the primary caregivers and are more directly involved in daily diabetes care activities (e.g., reminding the child to check his/her blood sugar) while fathers are often more likely to get involved only as need arises [11, 12•]. For example, poorer self-management in pre-adolescent youth (age 9–12) predicted an increased amount of paternal involvement over 3 years [13••], suggesting that fathers may become involved as a “relief” or “backup” in response to suboptimal control.
Furthermore, paternal and maternal involvement may impact diabetes outcomes in different ways. In a study that examined the relative influence of maternal and paternal involvement over time, mothers’ involvement predicted 37.6 % variance in adherence, 17.5 % variance in diabetes self-efficacy, and 13.9% variance in adolescent HbA1c,while fathers’ involvement predicted 27.4 % variance in adherence, 22.1 % variance in self-efficacy, and 16.6% variance in HbA1c [14•]. In another longitudinal study, lower levels of paternal involvement predicted deteriorating HbA1c across adolescence, while maternal involvement was not a significant predictor of trajectories of glycemic control [15••]. These findings suggest that paternal involvement may be uniquely important to the development of autonomy in diabetes management during adolescence.
While current treatment standards encourage continued involvement throughout adolescence, previous research on the effects of parental responsibility on diabetes-related has produced heterogeneous findings. Some studies have shown that lower levels of parental responsibility were associated with poorer adherence [16–18] and glycemic control [17], while others reported no associations with adherence [19] or glycemic control [18, 19]. Additionally, longitudinal studies have revealed that declines in parental responsibility were related to declines in adherence [17] and that adherence deteriorated more rapidly in youth who did not report a concurrent growth in self-efficacy [4••]. One study found, for example, that direct parental involvement in response to diabetes problems improved self-efficacy for adolescents who were not confident in their abilities to manage their diabetes, but parental involvement lowered self-efficacy the next day for children already confident in their management skills [14•]. Cross-sectional studies have linked the transfer of diabetes responsibility with both age and pubertal development [19, 20]; however, these developmental factors are imperfect indicators of the psychosocial maturity necessary for youth to manage diabetes independently. Taken together, these findings suggest that it is difficult to isolate the effects of parental responsibility from the other factors associated with age, puberty, and self-efficacy.
Parental Monitoring
Parental monitoring involves regular contact with adolescents regarding their daily activities as well as knowledge about and supervision of those activities. Monitoring of the adolescent with T1D can be general (e.g., knowing when child’s homework is due) or diabetes specific (e.g., knowledge of child’s blood sugar levels) [21]. Monitoring can also be direct (e.g., parent and child performing a task together with the parent supervising) or indirect (parent questioning/reminding the child about the task performed (or to be performed)) [22, 23]. While diabetes-specific parental monitoring is associated with greater parental responsibility for diabetes tasks, monitoring occurs mainly when parents begin to relinquish direct responsibilities [21].
General monitoring has been indirectly related to diabetes outcomes through lower levels of externalizing behaviors [24] and directly related to glycemic control by restricting adolescents’ behavior (e.g., diet restrictions [14•]). Diabetes-specific parental monitoring has been directly associated with better diabetes self-care, less family conflict, and lower HbA1c in adolescents [25•, 26]. Several studies revealed that mothers’ and fathers’ general and diabetes-specific monitoring predicted adolescents’ adherence to their recommended diabetes care regimen [14•, 21, 24, 25•, 27]. Notably, only fathers’ monitoring has emerged as a significant predictor of glycemic control [14•, 21, 24, 27]—a finding that was consistent when both parents were examined longitudinally [15••]. While paternal monitoring may have a more direct effect on adolescents’ glycemic control, maternal monitoring (general and diabetes specific) may be indirectly associated with HbA1c through better adherence [14•, 24] and self-efficacy for diabetes management [9]. As adolescents begin to manage diabetes tasks independently, it appears important for both parents—and especially fathers—to continue to monitor their children’s adherence in order to ensure optimal glycemic control [21, 26].
Quality of Involvement
Inconsistent findings for the effects of parental involvement on adolescent adjustment may be explained by how involvement is executed by the parent and perceived by the adolescent. Parents may feel obligated to be either the good cop or bad cop when regulating, assisting with, and monitoring their child’s diabetes. However, the literature on parenting practices (i.e., specific parental behaviors while interacting with their children [28]) indicates that some approaches are more helpful than others.
Good Cop
High-quality parental involvement (good cop) enables collaboration (i.e., parent–adolescent partnership) and is characterized by open communication, emotional support, and independence encouragement. Maternal and paternal parent–child relationships characterized by warmth, support, sensitivity, acceptance, and independence encouragement are associated with greater quality of life [29], adherence [21, 27, 30, 31], glycemic control [19, 21, 29, 30], and self-efficacy [14•] as well as lower frequency of diabetic ketoacidosis [32] and lower levels of externalizing behaviors [14•] in adolescents. Several studies have indicated that children of parents who are both warm and sensitive while maintaining high expectations for adolescents’ behavior were in better glycemic control [33, 34] and displayed more self-care behaviors (e.g., BGM, giving insulin shots, not skipping meals) [34]. Additionally, adolescents of parents who balanced rule setting with granting freedom reported lower stress and were in better glycemic control [35].
Similarly, collaborative involvement, defined as the parent–adolescent partnership in diabetes management that occurs when the parent offers the amount and type of support the adolescent feels is needed [3], has been associated with better general quality of life [3, 36], health-related quality of life [3, 37], improved self-efficacy [3], better adherence [3, 36], and lower HbA1c [3]. It is important to consider adolescents’ perception of involvement, as one study found that more frequent involvement was only related to better adjustment and adherence when the adolescent enjoyed and needed it [21]. However, discrepancies often exist between parent–child views of the adolescents’ competence level; one study found that both mothers and fathers perceived lower adolescent competence than the adolescents themselves [38], and these discrepancies were related to increased adolescent autonomy and poorer glycemic control [38]. Thus, a collaborative approach to diabetes management acts as scaffolding for youth’s current ability to self-manage, providing necessary expertise and support without taking over and reducing adolescents’ confidence in their own ability to manage.
Additionally, open communication is particularly important in facilitating efficient diabetes responsibility sharing. One study found that higher levels of adolescent disclosure to parents regarding diabetes management were associated with better adherence, while greater secrecy was associated with poorer adherence [39]. Therefore, open channels of communication are likely to improve daily parental monitoring and ultimately aid providers in preventing long-term complications. For parents experiencing difficulty relinquishing responsibility for the majority of the child’s diabetes care, open communication may establish trust in this collaborative partnership.
Bad Cop
Low-quality parental involvement (bad cop) is often referred to as intrusive support and is characterized by controlling, critical, and restrictive parenting behaviors that can create family conflict and reduce adolescents’ self-efficacy. Intrusive parental involvement in diabetes management occurs when the parent takes over responsibilities without the adolescent expressing a need or desire for assistance [40], which manifests as lecturing, nagging, blaming, scolding, asking too many questions, or giving orders [41]. Intrusive involvement is not only associated with lower adherence and suboptimal glycemic control [42–44] but has also been linked with poorer health-related quality of life [37] and greater family conflict [37, 44]. These critical parenting practices may be especially harmful in older adolescents [45, 46] or adolescents with externalizing behavior problems (e.g., aggression, disobedience, defiance) [45].
In addition, parent–child relationships characterized by overprotection, strict rules/limits, harshness, and low emotional support are associated with poorer glycemic control [47] and greater depressive symptoms in youth [48, 49•]. Rather than fostering partnership and collaboration, poor quality involvement (i.e., being the bad cop) creates conflict in parent–adolescent relationships. This is a significant concern, given that even small increases in family conflict can negatively impact glycemic control [11, 42]. A qualitative study revealed that adolescents’ anger and frustration stemmed from their desire to be included in decision-making and to receive recognition for the positive aspects of their diabetes management [50]. Similarly, adolescents in another qualitative study reported that parental intrusiveness, blame, and lack of understanding were the main sources of diabetes-related conflict [41]. Finally, qualitative analysis revealed that parental actions such as scolding, judging, nagging, and getting emotional hindered self-management in adolescents [51].
Factors Affecting Parental Involvement
Several factors may influence the type, degree, and quality of parental involvement in diabetes management, and these are important to consider in developing a more comprehensive understanding of parental involvement during adolescence.
Demographic Variables
Over the past few decades, the prevalence of single parenthood in the USA has increased from 23 to 36 % [52], and more than half of today’s children will spend at least part of their childhood in a single-parent home [53, 54]. Recent studies have consistently linked single-parent households with poorer glycemic control in youth with T1D [55–57]. When examined longitudinally, youth living in single-parent and blended families exhibit significantly higher HbA1c levels than those living with biological parents [58], and glycemic control has been shown to deteriorate three times faster among adolescents from single-parent households than those from intact families [59]. Single parenthood has also been linked with poor diabetes management behaviors (e.g., less frequent blood glucose monitoring, missed clinic appointments), and single parents have reported more difficulty managing their adolescents’ T1D than married parents [60]. Although these studies support that children of single parents are at increased risk for poor diabetes-related outcomes, few studies have explicitly measured parental involvement in single parents of youth with T1D.
Single parenthood often overlaps with other demographic risk factors, such as low income and minority race/ethnicity, which are also associated with suboptimal glycemic control and parental involvement [61, 62]. In one study, for example, the relationship between low income and glycemic control was explained by lower levels of parental acceptance [63]. Parents of minority youth have also demonstrated lower levels of monitoring than parents of white youth [22]. In addition, race/ethnicity has been related to observed parenting behaviors; white mothers’ have been observed to exhibit higher levels of collaborative parenting behaviors, while non-white mothers exhibit higher levels of over involved, or intrusive, behaviors [64]. However, higher levels of parental involvement and family support in Hispanic families have been associated with better adherence in adolescents [16]. Given that the majority of research on parental involvement has been conducted with predominantly white samples, more research is needed to determine if the same associations between different types of involvement and youth outcomes reported here are evident in minority youth with T1D. Although minority parents may exhibit higher levels of critical or permissive parental involvement, the most optimal outcomes in these populations are facilitated by high expectations for adherence along with high levels of warmth and sensitivity [65].
Parental Stress and Distress
The relationship between parental involvement and distress is complex and bidirectional; greater responsibility for diabetes management has been linked with higher levels of parenting stress and distress [66], which, in turn, may compromise the level and quality of parents’ further involvement [1]. For example, parents who are more involved in diabetes management report higher levels of caregiver strain, which may lead to depression and anxiety [66]. Similarly, increases in fathers’ involvement have been linked to higher levels of anxiety in fathers as well as elevated parenting stress in both mothers and fathers [12•]. Parental distress, including symptoms of anxiety and depression, has been associated with lower levels of warmth, involvement, and monitoring [67] as well as more intrusive parenting behaviors, such as nagging [68]. Studies also support that fathers’ adjustment to chronic illness is linked to mothers’ adjustment, and mothers who are unsupported by fathers are less able to support their children [69–71]. This finding suggests that fathers may become involved when mothers are overwhelmed and stressed to offer emotional support [12•]. Providers should be aware of the impact of caregiver distress, which may limit the parents’ involvement in T1D care or diminish the quality of their involvement. When encouraging greater involvement from caregivers, therefore, providers should consider assessing sources of support and promoting a balance of responsibility between both parents (in two-parent households) and/or other family members.
Child Behavior
Finally, the child’s behavior is important to consider as it may affect the type, amount, and quality of involvement. For example, problematic child behaviors (e.g., disruptive or defiant behaviors) have been linked with critical parenting, and this association was mediated by parenting stress [46]. In addition, as noted above, child secrecy has been associated with poorer adherence [39], which may in turn impact parental involvement. Although longitudinal studies help us to understand the direction of effects, these findings suggest a bidirectional relationship between child behavior and parental involvement [9], whereby adolescents engaging in secretive, argumentative, or hostile behavior may impede parents’ ability to be involved in diabetes management in a productive and collaborative manner.
Discussion
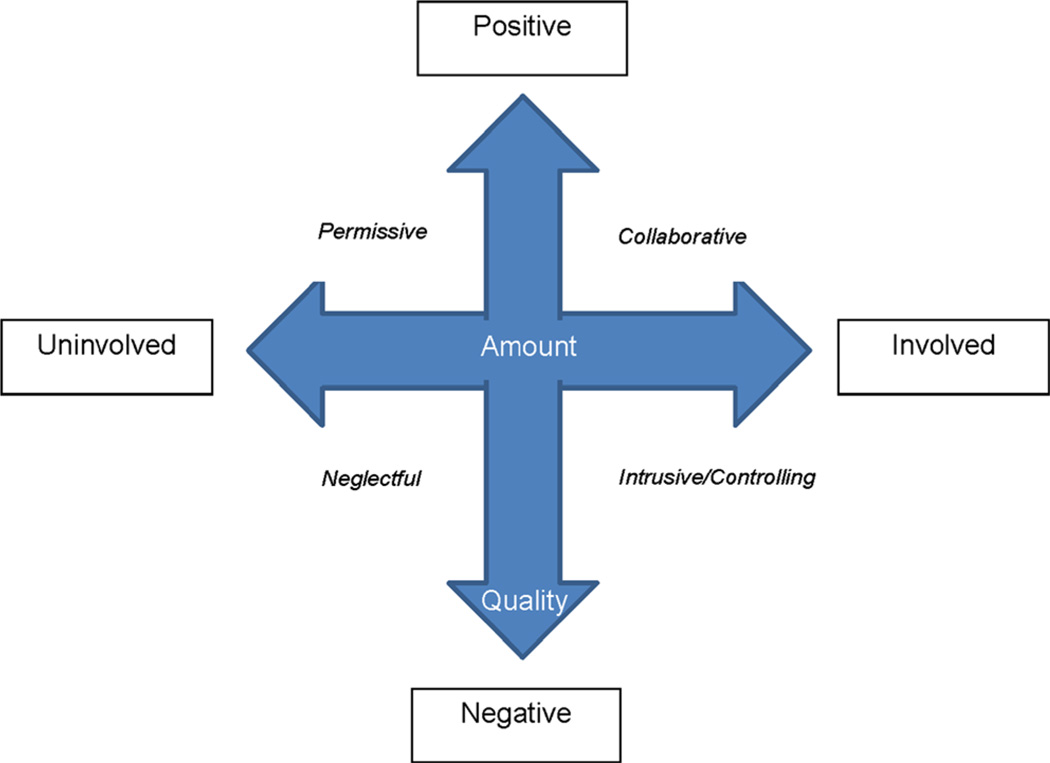
Taken together, the recent literature in parental involvement in diabetes management highlights the shift in focus from the amount of involvement to include the types (e.g., monitoring, behavioral involvement) and quality (e.g., warm, critical) of involvement in diabetes management by both mothers and fathers. We have integrated recent work in adults with type 2 diabetes [72] with the literature on youth with T1D to illustrate a model of parental involvement that incorporates all aspects (see Fig. 1). As described above, the amount of involvement alone does not predict outcomes. For example, if a parent is highly involved in diabetes management, but the involvement is of a harmful quality (e.g., criticizing, nagging, lecturing), diabetes outcomes could be negatively affected. Findings from this review also highlight the importance of adolescents’ perceptions of parental involvement; the same type of involvement may occur in different ways and be perceived differently by adolescents. For example, blood glucose monitoring could happen in the context of a regular weekly check-in, with praise for frequent monitoring (good cop), or it could occur in the context of an argument (e.g.,“I don’t trust you, show me your meter!”; bad cop). Therefore, parents need to balance the type, amount, and quality of parental involvement.
Fig. 1.
Integrated model of parental involvement in diabetes management
Uninvolved/No Cop
While past research has primarily focused on the effects of parental over-involvement on children with chronic conditions, more attention to parents who are uninvolved or under-involved is warranted. Adolescents are at the highest risk for poor diabetes outcomes when both parents display low levels of involvement (i.e., “no cop”), implicating the importance of both caregivers’ contributions to adolescent outcomes [3]. Parents’ motivation for their lack of involvement may be important to understand, however. For example, uninvolved parents may be neglectful (e.g., “He’s old enough to manage on his own.”) or permissive (e.g., “She needs to learn from her mistakes”). These different motivations need to be identified and addressed in future research (see Fig. 1).
Recommendations
The hormonal, metabolic, and behavioral changes that occur throughout adolescence can be especially challenging and frustrating for families trying to adapt and adjust diabetes care. Providers can help adolescents adapt to the physiological changes by increasing insulin requirements and adjusting management plans, yet parents receive little support for addressing the behavioral changes (e.g., establishing autonomy, rebellious and pleasure-seeking behaviors, and increased desire for privacy) that also contribute to deteriorating diabetes control. In the following sections, we highlight several strategies that may help parents promote better adherence through involvement.
Recommendations for Improving Parental Responsibility for Diabetes Management
During the transition from childhood to adolescence, youth seek greater independence, which offers parents an opportunity to share the responsibility for diabetes management. However, parents should be encouraged to shift the responsibility of care incrementally and work collaboratively with adolescents as they assume more autonomy in self-care. Some examples of this parent–teen partnership may include meal planning, non-verbal communication (e.g., regularly texting blood glucose numbers), setting goals, giving positive feedback when possible, and being available to offer guidance or advice when problems occur. No universal guideline (e.g., adolescents take on certain responsibilities at a specific age) can be applied, and responsibility for diabetes care activities should be shared and transferred with the individual adolescent’s level of self-efficacy and maturity in mind. By partnering with adolescents and continuing to maintain some direct involvement in management [18], parents can gradually shift more responsibility to their child, while also monitoring the completion of tasks. Sharing responsibilities and sustaining involvement during the transition to adolescence allows parents to foster protective factors that enable better self-care (e.g., self-efficacy, quality of life) while preventing risk factors linked to poor glycemic control (e.g., depressive symptoms, family conflict, internalizing, and externalizing behaviors) [3, 14•, 73]. Providers can help parents in the task of shifting responsibility by assessing the child’s ability to self-manage and encourage parents to step in as needed.
Recommendations for Improving Parental Monitoring
Ideally, parental monitoring should increase as parents begin to relinquish control of diabetes care to the adolescent, ensuring that the child is both equipped to take on these added tasks and accountable for his/her behaviors. However, as adolescents mature, monitoring techniques may change. For example, instead of directly watching the adolescent check his/her blood sugar, the parent may ask how many times the adolescent checked at the end of the day or check his/her logbook (or meter) weekly. Reminders can also be used as a monitoring technique, but these must be balanced with being perceived as intrusive, hovering, or giving too much guidance, which could compromise adolescents’ self-efficacy. Some families may find that using notes to remind the child to complete diabetes care instead of asking or telling the child in person may be more acceptable to both adolescents and parents. Monitoring should also be used as a tool for the assessment of adolescents’ readiness to assume more independence in management tasks, and direct supervision may still be needed to ensure good diabetes management [4••].
Recommendations for Improving Quality of Involvement
Good cops establish a collaborative partnership with their child that encourages independence and thrives on open, honest communication. Good cops balance setting boundaries and clear expectations, with emotional support (i.e., warmth, sensitivity, and acceptance). In contrast, bad cops do not attempt to understand or solicit the child’s point of view; they are in control of diabetes management in a way that is demanding and rigid, offering little emotional support or acceptance for the child. While parents should be encouraged to maintain high expectations for diabetes care, this needs to occur within a supportive context. The use of behavioral contracts may be an effective method for parents to communicate expectations and establish consequences for lack of diabetes care [74]. Parental guidance delivered in a non-coercive manner may also improve health outcomes in adolescents [43]. These findings demonstrate that parents should avoid nagging and lecturing, but instead provide clear and consistent rewards and consequences for diabetes management.
Limitations
Several limitations within the studies reviewed must be acknowledged. First, researchers have conceptualized parental involvement in a variety of ways, including behavioral involvement, monitoring, responsibility for disease management, and relationship quality, and the field has not reached consensus on these constructs (see Table 1). Researchers have often created new measures to examine parental involvement, despite the existence of numerous well-established measures for examining family functioning in pediatric samples [75]. Also, the measures of parental involvement differ across studies and particularly between studies of mothers and fathers, which prevent comparison between parents. Similarly, some studies failed to specify which parent provided data, further inhibiting comparisons between mothers and fathers. Finally, several of the studies included in this review came from a few research groups that have been particularly active in this area, and therefore, these findings need to be replicated in other populations.
In addition, although sample sizes were generally large, the majority of the studies focused on Caucasian, intact families, and findings may differ in minority and non-traditional families (e.g., blended, single/or divorced parents, adoptive/foster, grandparents raising grandchildren). It is important to note that parental beliefs about autonomy and diabetes management are likely to differ by culture and family structure, which may impact the parents’ involvement. For example, Hispanic families may emphasize greater family responsibility sharing over adolescent autonomy [16]. Asking about parental beliefs can create opportunities for providers to encourage positive involvement. For example, if parents think a child is skipping blood glucose checks due to laziness, their response is likely different than if they think the child is overwhelmed or depressed. Further, creative approaches are needed to recruit and retain more diverse samples, including different minority groups, single parents, and non-traditional caregivers so that providers can give more culturally competent and informed clinical recommendations.
Future Directions
Interventions aimed at improving parent–child collaboration around diabetes management and addressing the quality of parent–child communication have been successful [76, 77]. Still needed are interventions that include a focus on parental monitoring, assess adolescents’ ability to self-manage, and address parental distress. In addition, strengths of recent studies include longitudinal designs (e.g.,[9, 15••, 13••, 17]) and the use of multiple informants and measures to create latent variables of parental involvement (e.g., [9, 14•, 25]). More of these rigorous study designs are needed, and researchers need to report on the numbers of mothers, fathers, and single parents included in studies as well.
Conclusions
Parental involvement can serve as a risk or protective factor for youth with T1D [73]. Optimal parenting across the transition from pre-adolescence to adolescence is characterized by a shift from a directive to a more collaborative role, which may help adolescents to better understand the rationale for diabetes self-care tasks. Collaborative involvement requires some flexibility and fluidity from parents when adjusting the type and level of their involvement, not only over time but also in day-to-day parenting practices. Furthermore, findings from this review indicate that parental monitoring should not decrease during adolescence and may in fact need to increase depending on the child’s self-efficacy and current abilities. Providers should be aware of the factors that may compromise parental involvement, including marital status, income, parental stress and distress, and child behavior, while working to recognize and encourage optimal parental involvement.
Acknowledgments
Sarah S. Jaser has received grants from the National Institutes of Health.
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent This article does not contain any studies with animal subjects performed by any of the authors. With regard to the authors’ research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Conflict of Interest
Mackenzie T. Young, Jadienne H. Lord, Niral J. Patel, and Meredith A. Gruhn declare that they have no conflict of interest.
Contributor Information
Mackenzie T. Young, Email: mackenzie.t.young@vanderbilt.edu.
Jadienne H. Lord, Email: jadienne.h.lord@vanderbilt.edu.
Niral J. Patel, Email: niral.patel@vanderbilt.edu.
Meredith A. Gruhn, Email: meredith.a.gruhn@vanderbilt.edu.
Sarah S. Jaser, Email: sarah.jaser@vanderbilt.edu.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Whittemore R, et al. Psychological experience of parents of children with type 1 diabetes a systematic mixed-studies review. The Diabetes Educ. 2012;38(4):562–579. doi: 10.1177/0145721712445216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helgeson VS, et al. Parent and adolescent distribution of responsibility for diabetes self-care: links to health outcomes. J Pediatr Psychol. 2008;33(5):497–508. doi: 10.1093/jpepsy/jsm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wysocki T, et al. Collaborative involvement of primary and secondary caregivers: associations with youths’ diabetes outcomes. J Pediatr Psychol. 2009;34(8):869–881. doi: 10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wiebe DJ, et al. Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. J. Pediatr Psychol. 2014 doi: 10.1093/jpepsy/jsu006. p. jsu006. This study provides some of the first longitudinal evidence of the association between declines in parental responsibility and deteriorating adolescent adherence, while emphasizing the important role of adolescent self-efficacy.
- 5.Kovacs M, et al. Psychological functioning among mothers of children with insulin-dependent diabetes mellitus: a longitudinal study. J Consult Clin Psychol. 1990;58(2):189. doi: 10.1037//0022-006x.58.2.189. [DOI] [PubMed] [Google Scholar]
- 6.Swallow V, et al. Fathers’ contributions to the management of their child’s long-term medical condition: a narrative review of the literature. Health Expect. 2012;15(2):157–175. doi: 10.1111/j.1369-7625.2011.00674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wysocki T, Gavin L. Paternal involvement in the management of pediatric chronic diseases: associations with adherence, quality of life, and health status. J Pediatr Psychol. 2006;31(5):501–511. doi: 10.1093/jpepsy/jsj042. [DOI] [PubMed] [Google Scholar]
- 8.Gavin L, Wysocki T. Associations of paternal involvement in disease management with maternal and family outcomes in families with children with chronic illness. J Pediatr Psychol. 2006;31(5):481–489. doi: 10.1093/jpepsy/jsj043. [DOI] [PubMed] [Google Scholar]
- 9.King PS, et al. Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents’ adherence. Health Psychol. 2014;33(5):424–432. doi: 10.1037/a0032804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berg CA, et al. Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychol. 2013;32(7):719. doi: 10.1037/a0029427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hilliard ME, et al. Fathers’ involvement in preadolescents’ diabetes adherence and glycemic control. J Pediatr Psychol. 2011;36(8):911–922. doi: 10.1093/jpepsy/jsr020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hansen JA, et al. Paternal involvement in pediatric type 1 diabetes: fathers’ and mothers’ psychological functioning and disease management. Fam Syst Health. 2012;30(1):47. doi: 10.1037/a0027519. This study offers evidence that increased paternal support is related to better maternal and child adjustment outcomes, but findings suggest that fathers may only become involved in response to poor glycemic control.
- 13. Hilliard ME, et al. Patterns and predictors of paternal involvement in early adolescents’ type 1 diabetes management over 3 years. J Pediatr Psychol. 2014;39(1):74–83. doi: 10.1093/jpepsy/jst067. This study provides longitudinal evidence that different aspects of paternal involvement can predict youths’ diabetes self-management and extends previous findings that fathers may become more involved as need arises.
- 14. Berg CA, et al. Parental involvement and adolescents’ diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. J Pediatr Psychol. 2011;36(3):329–339. doi: 10.1093/jpepsy/jsq088. This study offers evidence indicating that both monitoring and a high quality parent-child relationship are important in promoting adherence and glycemic control in adolescents through better self-efficacy for diabetes management.
- 15. King PS, et al. Longitudinal trajectories of metabolic control across adolescence: associations with parental involvement, adolescents’ psychosocial maturity, and health care utilization. J Adolesc Health. 2012;50(5):491–496. doi: 10.1016/j.jadohealth.2011.09.007. This study provides longitudinal evidence demonstrating that adolescents with rapidly deteriorating glycemic control reported lower parental monitoring and frequency of help with diabetes care, lower levels of autonomy and greater number of hospitalizations.
- 16.Hsin O, et al. Adherence and glycemic control among Hispanic youth with type 1 diabetes: role of family involvement and acculturation. J Pediatr Psychol. 2010;35(2):156–166. doi: 10.1093/jpepsy/jsp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ingerski LM, et al. Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. J Adolesc Health. 2010;47(2):191–197. doi: 10.1016/j.jadohealth.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vesco AT, et al. Responsibility sharing between adolescents with type 1 diabetes and their caregivers: importance of adolescent perceptions on diabetes management and control. J Pediatr Psychol. 2010;35(10):1168–1177. doi: 10.1093/jpepsy/jsq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmer DL, et al. Mothers’, fathers’, and children’s perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. J Pediatr Psychol. 2009;34(2):195–204. doi: 10.1093/jpepsy/jsn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanna KM, Decker CL. A concept analysis: assuming responsibility for self-care among adolescents with type 1 diabetes. J Specialists Pediatr Nurs. 2010;15(2):99–110. doi: 10.1111/j.1744-6155.2009.00218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berg CA, et al. Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care. 2008;31(4):678–683. doi: 10.2337/dc07-1678. [DOI] [PubMed] [Google Scholar]
- 22.Ellis DA, et al. Toward conceptual clarity in a critical parenting construct: parental monitoring in youth with chronic illness. J Pediatr Psychol. 2008;33(8):799–808. doi: 10.1093/jpepsy/jsn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cemeroglu AP, et al. Comparison of the expectations of caregivers and children with type 1 diabetes mellitus for independence in diabetes care-related tasks. Endocrine Practice. 2014:1–22. doi: 10.4158/EP13472.OR. [DOI] [PubMed] [Google Scholar]
- 24.Horton D, et al. The role of parental monitoring in metabolic control: effect on adherence and externalizing behaviors during adolescence. J Pediatr Psychol. 2009;34(9):1008–1018. doi: 10.1093/jpepsy/jsp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hilliard ME, et al. Disentangling the roles of parental monitoring and family conflict in adolescents’ management of type 1 diabetes. Health Psychol. 2013;32(4):388. doi: 10.1037/a0027811. This study offers evidence that the risk of poorer glycemic control associated with decreasing parental monitoring is greater than that of elevated family conflict, supporting the importance of maintaining sufficient levels of monitoring, even with the possibility of increased conflict.
- 26.Robinson EM. Assessing parental involvement in type 1 diabetes management during adolescence. Richmond, VA: Virginia Commonwealth University; 2011. [Google Scholar]
- 27.Palmer DL, et al. The structure of parental involvement and relations to disease management for youth with type 1 diabetes. J Pediatr Psychol. 2011;36(5):596–605. doi: 10.1093/jpepsy/jsq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spera C. A review of the relationship among parenting practices, parenting styles, and adolescent school achievement. Educ Psychol Rev. 2005;17(2):125–146. [Google Scholar]
- 29.Jaser SS, Grey M. A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. J Pediatr Psychol. 2010;35(7):738–747. doi: 10.1093/jpepsy/jsp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lloyd SM, et al. Brief report: Hope, perceived maternal empathy, medical regimen adherence, and glycemic control in adolescents with type 1 diabetes. J Pediatr Psychol. 2009;34(9):1025–1029. doi: 10.1093/jpepsy/jsn141. [DOI] [PubMed] [Google Scholar]
- 31.Mlynarczyk SM. Adolescents’ perspectives of parental practices influence diabetic adherence and quality of life. Pediatr Nurs. 2013;39(4):181–189. [PubMed] [Google Scholar]
- 32.Geffken GR, et al. Family functioning processes and diabetic ketoacidosis in youths with type I diabetes. Rehabil Psychol. 2008;53(2):231. [Google Scholar]
- 33.Shorer M, et al. Role of parenting style in achieving metabolic control in adolescents with type 1 diabetes. Diabetes Care. 2011;34(8):1735–1737. doi: 10.2337/dc10-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Greene MS, et al. Metabolic control, self-care behaviors, and parenting in adolescents with type 1 diabetes a correlational study. Diabetes Educ. 2010;36(2):326–336. doi: 10.1177/0145721710361270. [DOI] [PubMed] [Google Scholar]
- 35.Céspedes-Knadle YM, Munoz CE. Development of a group intervention for teens with type 1 diabetes. J Specialists Group Work. 2011;36(4):278–295. [Google Scholar]
- 36.Nansel TR, et al. Development and validation of the collaborative parent involvement scale for youths with type 1 diabetes. J Pediatr Psychol. 2009;34(1):30–40. doi: 10.1093/jpepsy/jsn058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weissberg-Benchell J, et al. Generic and diabetes-specific parent–child behaviors and quality of life among youth with type 1 diabetes. J Pediatr Psychol. 2009;34(9):977–988. doi: 10.1093/jpepsy/jsp003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Butner J, et al. Parent–adolescent discrepancies in adolescents’ competence and the balance of adolescent autonomy and adolescent and parent well-being in the context of type 1 diabetes. Dev Psychol. 2009;45(3):835. doi: 10.1037/a0015363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Osborn P, et al. What mom and dad don’t know can hurt you: adolescent disclosure to and secrecy from parents about type 1 diabetes. J Pediatr Psychol. 2013;38(2):141–150. doi: 10.1093/jpepsy/jss102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pomerantz EM, Eaton MM. Maternal intrusive support in the academic context: transactional socialization processes. Dev Psychol. 2001;37(2):174. doi: 10.1037/0012-1649.37.2.174. [DOI] [PubMed] [Google Scholar]
- 41.Weinger K, O’Donnell KA, Ritholz MD. Adolescent views of diabetes-related parent conflict and support: a focus group analysis. J Adolesc Health. 2001;29(5):330–336. doi: 10.1016/s1054-139x(01)00270-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hood KK, et al. Updated and revised diabetes family conflict scale. Diabetes Care. 2007;30(7):1764–1769. doi: 10.2337/dc06-2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lewin AB, et al. The relation between family factors and metabolic control: the role of diabetes adherence. J Pediatr Psychol. 2006;31(2):174–183. doi: 10.1093/jpepsy/jsj004. [DOI] [PubMed] [Google Scholar]
- 44.Cameron F, et al. Are family factors universally related to metabolic outcomes in adolescents with type 1 diabetes? Diabet Med. 2008;25(4):463–468. doi: 10.1111/j.1464-5491.2008.02399.x. [DOI] [PubMed] [Google Scholar]
- 45.Duke DC, et al. Glycemic control in youth with type 1 diabetes: family predictors and mediators. J Pediatr Psychol. 2008;33(7):719–727. doi: 10.1093/jpepsy/jsn012. [DOI] [PubMed] [Google Scholar]
- 46.Sweenie R, Mackey ER, Streisand R. parent–child relationships in type 1 diabetes: associations among child behavior, parenting behavior, and pediatric parenting stress. Families, Systems, & Health. 2014;32(1):31. doi: 10.1037/fsh0000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seiffge-Krenke I, et al. Declining metabolic control and decreasing parental support among families with adolescents with diabetes: the risk of restrictiveness. J Pediatr Psychol. 2013;38(5):518–530. doi: 10.1093/jpepsy/jst006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Butler JM, et al. Maternal parenting style and adjustment in adolescents with type I diabetes. J Pediatr Psychol. 2007;32(10):1227–1237. doi: 10.1093/jpepsy/jsm065. [DOI] [PubMed] [Google Scholar]
- 49. Armstrong B, Mackey ER, Streisand R. Parenting behavior, child functioning, and health behaviors in preadolescents with type 1 diabetes. J Pediatr Psychol. 2011;36(9):1052–1061. doi: 10.1093/jpepsy/jsr039. This study offers evidence for the association between parenting behaviors, particularly critical parenting behaviors, and child depressive symptoms and self-efficacy, both factors linked to diabetes outcomes.
- 50.Ivey JB, Wright A, Dashiff CJ. Finding the balance: adolescents with type 1 diabetes and their parents. J Pediatr Health Care. 2009;23(1):10–18. doi: 10.1016/j.pedhc.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 51.Dashiff C, et al. Parents’ experiences supporting self-management of middle adolescents with type 1 diabetes mellitus. Pediatr Nurs. 2011;37(6) [PubMed] [Google Scholar]
- 52.Bureau, U.S.C. America’s children: key national indicators of well-being, 2013. Family Structure and Children’s Living Arrangements. 2013 [cited 2014; Available from: http://www.childstats.gov/americaschildren/famsoc1.asp.
- 53.Blau DM, Van der Klaauw W. What determines family structure? Econ Inq. 2013;51(1):579–604. [Google Scholar]
- 54.Blau DM, Van der Klaauw W. A demographic analysis of the family structure experiences of children in the United States. Rev Econ Househ. 2008;6(3):193–221. [Google Scholar]
- 55.Thompson SJ, Auslander WF, White NH. Comparison of single-mother and two-parent families on metabolic control of children with diabetes. Diabetes Care. 2001;24(2):234–238. doi: 10.2337/diacare.24.2.234. [DOI] [PubMed] [Google Scholar]
- 56.Urbach SL, et al. Predictors of glucose control in children and adolescents with type 1 diabetes mellitus. Pediatr Diabetes. 2005;6(2):69–74. doi: 10.1111/j.1399-543X.2005.00104.x. [DOI] [PubMed] [Google Scholar]
- 57.Johns C, Faulkner MS, Quinn L. Characteristics of adolescents with type 1 diabetes who exhibit adverse outcomes. Diabetes Educ. 2008;34(5):874–885. doi: 10.1177/0145721708322857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Swift EE, et al. Demographic risk factors, mediators, and moderators in youths’ diabetes metabolic control. Ann Behav Med. 2006;32(1):39–49. doi: 10.1207/s15324796abm3201_5. [DOI] [PubMed] [Google Scholar]
- 59.Frey MA, et al. Predicting metabolic control in the first 5 yr after diagnosis for youths with type 1 diabetes: the role of ethnicity and family structure. Pediatr Diabetes. 2007;8(4):220–227. doi: 10.1111/j.1399-5448.2007.00260.x. [DOI] [PubMed] [Google Scholar]
- 60.Edmonds-Myles S, Tamborlane WV, Grey M. Perception of the impact of type 1 diabetes on low-income families. Diabetes Educ. 2010;36(2):318–325. doi: 10.1177/0145721709349219. [DOI] [PubMed] [Google Scholar]
- 61.Gallegos-Macias AR, et al. Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and white non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes. 2003;4(1):19–23. doi: 10.1034/j.1399-5448.2003.00020.x. [DOI] [PubMed] [Google Scholar]
- 62.Jacobsen JJ, et al. Race/ethnicity and measures of glycaemia in the year after diagnosis among youth with type 1 and type 2 diabetes mellitus. J Diabetes Complicat. 2014 doi: 10.1016/j.jdiacomp.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 63.Drew LM, et al. Depleted parental psychological resources as mediators of the association of income with adherence and metabolic control. J Fam Psychol. 2011;25(5):751. doi: 10.1037/a0025259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lord JH, et al. Effect of race and marital status on mothers’ observed parenting and adolescent adjustment in youth with type 1 diabetes. J Pediatr Psychol. doi: 10.1093/jpepsy/jsu078. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Anderson BJ. Parenting styles and parenting practices in pediatric diabetes. Diabetes Care. 2011;34:1885–1886. doi: 10.2337/dc11-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carcone AI, Ellis DA, Naar-King S. Linking caregiver strain to diabetes illness management and health outcomes in a sample of adolescents in chronically poor metabolic control. J Dev Behav Pediatr. 2012;33(4):343–351. doi: 10.1097/DBP.0b013e31824eaac8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eckshtain D, et al. The effects of parental depression and parenting practices on depressive symptoms and metabolic control in urban youth with insulin dependent diabetes. J Pediatr Psychol. 2010;35(4):426–435. doi: 10.1093/jpepsy/jsp068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams L, Laffel L, Hood K. Diabetes-specific family conflict and psychological distress in paediatric type 1 diabetes. Diabet Med. 2009;26(9):908–914. doi: 10.1111/j.1464-5491.2009.02794.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rodrigues N, Patterson JM. Impact of severity of a child's chronic condition on the functioning of two-parent families. J Pediatr Psychol. 2007;32(4):417–426. doi: 10.1093/jpepsy/jsl031. [DOI] [PubMed] [Google Scholar]
- 70.Soliday E, Kool E, Lande MB. Family environment, child behavior, and medical indicators in children with kidney disease. Child Psychiatry Hum Dev. 2001;31(4):279–295. doi: 10.1023/a:1010282305881. [DOI] [PubMed] [Google Scholar]
- 71.Worrall-Davies A, et al. The effect of parental expressed emotion on glycaemic control in children with type 1 diabetes: parental expressed emotion and glycaemic control in children. J Psychosom Res. 2002;52(2):107–113. doi: 10.1016/s0022-3999(01)00293-8. [DOI] [PubMed] [Google Scholar]
- 72.Mayberry LS, Osborn CY. Family members’ supportive and obstructive behaviors are associated with the self-care behaviors of adults with diabetes. Philadelphia, PA: 2014. [Google Scholar]
- 73.Hilliard ME, Harris MA, Weissberg-Benchell J. Diabetes resilience: a model of risk and protection in type 1 diabetes. Curr Diabetes Rep. 2012;12(6):739–748. doi: 10.1007/s11892-012-0314-3. [DOI] [PubMed] [Google Scholar]
- 74.Carroll AE, et al. Contracting and monitoring relationships for adolescents with type 1 diabetes: a pilot study. Diabetes Technol Ther. 2011;13(5):543–549. doi: 10.1089/dia.2010.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alderfer MA, et al. Evidence-based assessment in pediatric psychology: family measures. J Pediatr Psychol. 2008;33(9):1046–1061. doi: 10.1093/jpepsy/jsm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Anderson BJ, et al. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care. 1999;22(5):713–721. doi: 10.2337/diacare.22.5.713. [DOI] [PubMed] [Google Scholar]
- 77.Wysocki T, et al. Randomized, controlled trial of behavioral family systems therapy for diabetes: maintenance and generalization of effects on parent-adolescent communication. Behav Ther. 2008;39(1):33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]