Abstract
Objective
The current paper aims to: (1) examine clinical practice guidelines in suicide prevention across fields, organizations, and clinical specialties and (2) inform emerging standards in clinical practice, research, and training.
Methods
The authors conducted a systematic literature review to identify clinical practice guidelines and resource documents in suicide prevention and risk management. The authors used PubMed, Google Scholar, and Google Search, and keywords included: clinical practice guideline, practice guideline, practice parameters, suicide, suicidality, suicidal behaviors, assessment, and management. To assess for commonalities, the authors reviewed guidelines and resource documents across 13 key content categories and assessed whether each document suggested validated assessment measures.
Results
The search generated 101 source documents, which included N=10 clinical practice guidelines and N=12 additional resource documents (e.g., non-formalized guidelines, tool-kits). All guidelines (100 %) provided detailed recommendations for the use of evidence-based risk factors and protective factors, 80 % provided brief (but not detailed) recommendations for the assessment of suicidal intent, and 70 % recommended risk management strategies. By comparison, only 30 % discussed standardization of risk-level categorizations and other content areas considered central to best practices in suicide prevention (e.g., restricting access to means, ethical considerations, confidentiality/legal issues, training, and postvention practices). Resource documents were largely consistent with these findings.
Conclusions
Current guidelines address similar aspects of suicide risk assessment and management, but significant discrepancies exist. A lack of consensus was evident in recommendations across core competencies, which may be improved by increased standardization in practice and training. Additional resources appear useful for supplemental use.
Keywords: Suicide, Curriculum development
Suicide represents a complex but preventable public health problem and global disease burden. Although rates and prevalence vary cross-culturally by a diverse array of social, psychological, and biological factors, suicide currently accounts for nearly 1 million deaths annually [1, 2], and 57 % of all violent deaths worldwide. The Institute of Medicine (IOM) further estimates that an additional 25 suicide attempts (up to 100 for youth) occur for every death by suicide [2]. Given the profound impact of suicidal behaviors on the individual, family, community, economy, and society as a whole, the prevention of suicide has emerged as a global imperative, motivating unprecedented efforts designed to improve awareness, advance research, and enhance access to care.
Despite such advancements, suicide remains a leading cause of death with inherent challenges in its prevention. Although a host of well-researched screening and assessment measures are available to clinicians, researchers, and educators, a lack of consensus in gold-standard suicide risk assessment and management, as well as a lack of standardized nomenclature, challenges the accurate detection of risk and ability to prevent suicide outcomes [3]. As a result, a number of health agencies have called for standardized terminology in the assessment and monitoring of suicidal behaviors. The US Food and Drug Administration (FDA) now mandates administration of a standardized instrument to assess suicide risk across all central nervous system (CNS) drug trials [4, 5], and the Centers for Disease Control and Prevention (CDC) recently published a suggested, uniform nomenclature for self-directed violence [6]. Even so, the use of such nomenclature, and the number of existing clinical practice guidelines for suicide prevention across fields, is unknown.
Suicide cuts across both psychiatric and medical illness, yet detection of risk continues to challenge prevention and intervention. The majority of suicide decedents visit their primary care physician in the year prior to death (45 % in the past month)—considerably higher than the number of visits to a mental health care practitioner [7]. This highlights the need for easily-accessible best practice guidelines, adaptable to diverse fields of medicine and clinical specialties, that may be the first point of contact for risk detection, intervention, and prevention.
The aim of the current paper was to conduct a systematic review of multidisciplinary clinical practice guidelines and related resource documents in suicide risk assessment and management. The authors aimed to: (1) assess for the presence and accessibility of practice guidelines and related resource documents, (2) evaluate commonalities across these documents, and (3) identify the extent to which each addressed specific content areas, consistent with emerging standards in suicidology and relevant to clinical practice. The overarching aim of the review was to identify areas of consensus, as well as practice gaps, that may guide emerging standards in suicide prevention clinical practice, research, and training.
Methods
The authors performed a web-based, systematic literature search [October 25, 2013] to identify clinical practice guidelines as well as related resource documents using PubMed, Google Scholar, and Google Search. Citation search keywords included clinical practice guideline, practice guideline, suicide, suicidality, suicidal behaviors, assessment, and management. PubMed generated 101 search results, 3 of which were clinical practice guidelines, and Google Scholar and Google Search located 7 additional clinical practice guidelines. The authors used the same keywords to internally search the websites of specialty organizations to locate organization-specific guidelines and/or resource documents. To verify the accuracy and existence of guidelines, the authors made efforts to communicate via email and/or phone with a representative from each organization.
The authors next assessed source documents according to the extent to which they addressed the following content areas: (1) evidence-based risk and protective factors, (2) standardized risk categorization levels, (3) assessment of degree of suicidal intent, (4) recommended standardized risk assessment measures, (5) recommended treatments, (6) outpatient management strategies, (7) safety planning procedures, (8) restricting access to means, (9) confidentiality issues, (10) ethical considerations in suicide risk assessment and management, (11) postvention practices, (12) legal issues, and (13) training of clinicians. Authors generated tables to summarize findings across these areas and by source document type (i.e., clinical practice guideline or additional resource document).
Results
Search criteria generated a total of 101 source documents, with authors identifying 22 documents as guidelines for practice. Of these, N=10 were formalized clinical practice guidelines or practice parameters (see Table 1) [8–17], whereas N= 12 reflected additional resource documents (i.e., specialized recommendations for work with individuals at elevated risk, but not representing clinical practice guidelines; e.g., non-formalized clinical guidelines, abbreviated recommendations, assessment standards, and toolkits) (see Table 2) [18–28].
Table 1.
Summary of clinical practice guidelines
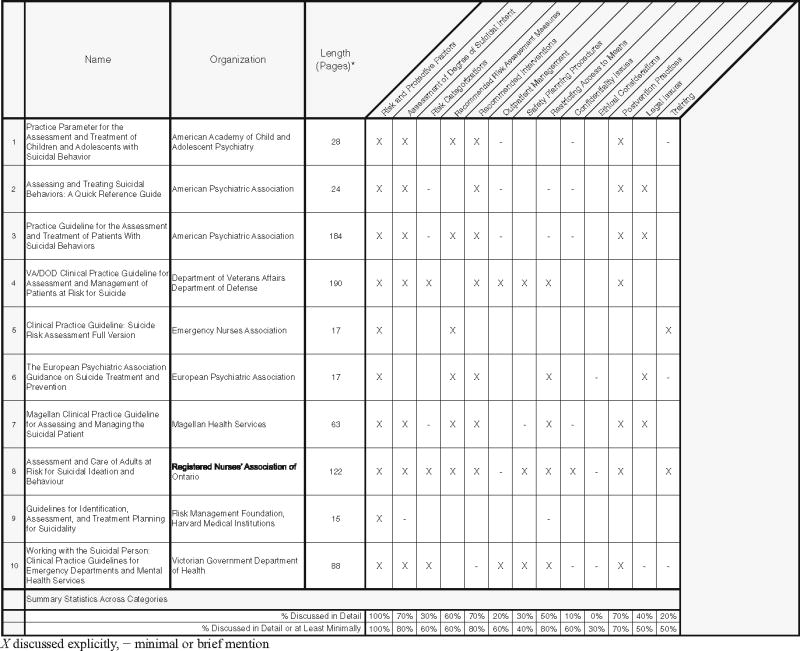
|
Table 2.
Summary of additional resource documents
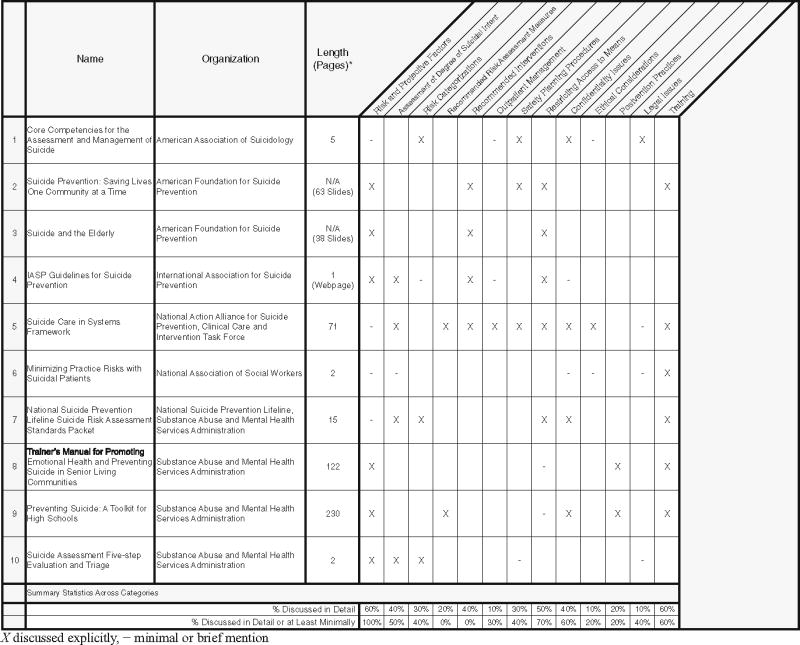
|
In total, the authors identified and contacted 22 organizations for confirmation of guidelines: the American Academy of Child and Adolescent Psychiatry (AACAP), American Association of Suicidology (AAS), American Foundation for Suicide Prevention (AFSP), American Medical Association (AMA), American Nurses Association (ANA), American Psychiatric Association (APA), American Psychological Association (APA), Centers for Disease Control and Prevention (CDC), Department of Veterans Affairs and Department of Defense (VA/DOD), Emergency Nurses’ Association (ENA), European Psychiatry Association (EPA), International Association for Suicide Prevention (IASP), Magellan Health Services, National Action Alliance for Suicide Prevention, National Association of Social Workers (NASW), National Institutes of Health (NIH), National Suicide Prevention Lifeline (NSPL), Registered Nurses Association of Ontario (RNAO), Substance Abuse and Mental Health Services Administration (SAMHSA), Suicide Prevention Action Network (SPAN), Suicide Prevention Resource Center (SPRC), and the Victorian Department of Health.
Of the 22 organizations, N=18 (81.8 %) responded and verified findings. Four organizations (18.2 %) did not respond; however, all four of these guidelines were unambiguous of categorization as clinical practice guidelines based on the title. In one case, an organization [the American Psychological Association (APA)] noted that they have clinical practice guidelines in development but not yet published. Finally, the Suicide Prevention Resource Center (SPRC) publishes multiple resource documents that address highly specific core competencies within suicide prevention and postvention. A representative from this agency verified that these are intended to be resource documents versus formal clinical practice guidelines. Based on their highly specialized nature (e.g., media recommendations), these documents are consolidated into a single SPRC category.
For results and summary statistics of key content areas addressed, please see Tables 1 and 2. Table 3 provides a summary of assessment measures that are recommended within clinical practice guidelines and resource documents.
Table 3.
Summary of recommended measures
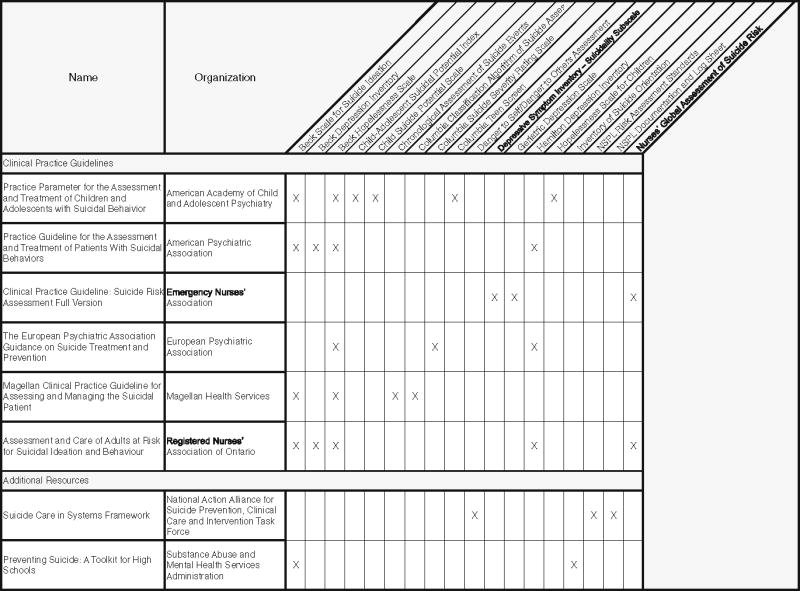
|
Discussion
The current review identified a total of 10 formalized clinical practice guidelines and 12 additional resources. Although the high number of guidelines and resources reflect a great strength (22 total resources), this can also reflect a limitation, as a larger number of resources (1,353 pages total) may be cumbersome and introduce potential for confusion. This was also evident in the relative length of each clinical practice guideline, which ranged from 15 pages (i.e., Harvard Medicine) to 190 pages (i.e., DOD/VA Clinical Practice Guideline). Although the breadth and depth of material increases within a longer set of guidelines, a clear strength of a brief source document is its brevity and usability. Consistent with this, documents categorized as additional resources were shorter in average length than the practice guidelines. These took the form of more abbreviated, pocketbook-style resource documents, slides, or webpages.
In the majority of cases, practice guidelines comprehensively addressed a number of key content areas in suicide risk assessment and management. The authors reviewed a total of 13 content areas across guidelines and resource documents. The majority (>70 %) of guidelines consistently addressed five of these categories, with at least minimal mention of category-specific recommendations: assessment of evidence-based suicide risk factors (100 %), assessment of suicidal intent (80 %), recommended treatments (80 %), restricting access to means (80 %), and postvention practice recommendations (70 %). The assessment of evidence-based risk factors for suicide was the only category addressed across all guidelines, consistent with evidence-based practices in suicidology. This appears to reflect consensus that a starting point to suicide risk management involves assessment of risk factors and warning signs known be associated with risk (i.e., both static and dynamic risk factors, including diagnostic, demographic, and psychosocial factors, as well as protective factors). Next, the majority (80 %) of guidelines addressed the assessment of the degree of suicidal intent and planning. This is considered a great strength of the guidelines, as this informs risk level in risk assessment frameworks [29, 30]. Similarly, nearly all guidelines reviewed and recommended evidence-based treatments for suicidal behaviors, including psycho-pharmacological and psychotherapy treatments shown to be effective in the management of suicide risk. However, guidelines provided this in varying detail and with few recommendations regarding the selection of treatment. Next, all but two guidelines addressed restricting access to means, though few guidelines provided explicit recommendations. Given the effectiveness of this intervention strategy in suicide prevention [31, 32], this appears to represent an important gap between science and practice. Finally, most guidelines (70 %) provided explicit recommendations for postvention practices (i.e., suicide bereavement recommendations for family survivors as well as clinicians following a suicide)—a clinically important, yet often neglected area of research and training [33–35].
By comparison, a number of content areas were not addressed across guidelines (<70 % of guidelines providing at least minimal mention of the category). These included: suicide risk level categorizations (60 %), recommended risk assessment measures (60 %), tools for outpatient management (60 %), safety planning (40 %), confidentiality issues (60 %), training recommendations (50 %), ethical considerations (30 %), and legal issues (50 %). A diverse array of ethical considerations, considered fundamental to suicide prevention, exist in suicide risk assessment and management [36, 37], including informed consent (i.e., to the process of risk assessment in clinical practice, with a discussion of safety planning procedures and treatment ground rules—typically occurring at the outset of treatment), confidentiality limits, legal issues, and safety concerns. However, less than half of all guidelines addressed ethical considerations. Four of the 12 additional resources (i.e., National Action Alliance Report, AAS Core Competencies, Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment, SPRC Resource Library) addressed the importance of legal and ethical issues, as well as standardized risk assessment, safety planning, confidentiality issues, and training. These documents may thus be helpful, alongside current guidelines, for adaptation of future practice parameters.
Although most guidelines recognized the need to assess risk level, a relative few (<60 %) offered recommendations regarding standardized risk level categorizations or decision-tree rules; this is an important practice gap since such procedures may routinize risk assessment, referral, and management procedures [29, 30, 37]. In addition, few guidelines or additional resources recommended established screening measures and inventories. Those that do, generate a total count of 36 possible measures (see Table 3). Such measures importantly aid a clinician in establishing risk level, which routinizes assessment, clinical decision-making, and risk management procedures; yet an excess of options (for review, see Brown 2002) [38] makes it unclear which measure one should select or use based on the setting, population, and circumstances. This suggests that increased consensus regarding gold standard assessment techniques, across or within specific clinical populations, as well as a narrowing of recommended measures, may be helpful. Consensus in risk assessment may impact science and clinical practice, improving comparability in nomenclature and risk management, and may critically inform training. Next, both guidelines and additional resources only minimally discussed outpatient risk management techniques. This includes safety planning procedures, a patient-driven approach [39], adopted by the VA by memorandum [40], involving the identification of emergency resources and internal coping strategies to be utilized during a suicidal crisis. Outpatient settings are the most likely point of intervention for suicide prevention, which highlights their importance and need for incorporation into future guidelines. We thus recommend that safety planning procedures and other outpatient intervention strategies, such as restricting access to means, be thoroughly described in all future guidelines and resources.
Findings were generally similar across guidelines and additional resource documents with a few notable exceptions. Additional resources demonstrated a greater overall focus on training (i.e., explicit recommendations were provided in 67 vs. 20 % of guidelines), and in many cases, appeared designed for this purpose. Resources often devoted more time to describing what aspects of suicide risk assessment and management should be emphasized in training, and several outlined helpful training case examples or vignettes. Additionally, they typically described topics in greater detail, such as ethical considerations in suicide risk assessment and management, legal issues, and how to discuss confidentiality with patients. Additional resources were, however, less likely to include recommended treatment modalities, standardized risk assessment measures, and postvention practices, likely because they were not intended to serve as formal clinical practice guidelines. Finally, across all guidelines and resource documents, only one document addressed all content areas: the SPRC Resource Library. Given this, and its easy-to-use format, this resource may be helpful in guiding refinements to future documents and guidelines. Given the strengths and weaknesses of the guidelines and additional resources, a merging of the two, emphasizing more user friendly, pocket-style recommendations or resource libraries—is an additional recommendation of this review.
Considering that training predicts practice in this important clinical area, we recommend an increased focus on training in clinical practice guidelines. Across guidelines and resource documents, only 50–57 % addressed training, respectively. This demonstrates the acute need for formalized training recommendations in future practice parameters and guidelines. A national survey of psychiatry residency training directors demonstrated results consistent with this recommendation. Survey findings indicated that, while the majority of programs provided some degree of training in the assessment and management of suicidal patients, little was known about both whether trainees felt adequately prepared to work with individuals at elevated risk and what specific practices were being used [35]. Similarly, a national survey of chief residents showed that, although the majority of programs offered formalized training in suicide risk management, individuals desired additional support for supervision and teaching in this area [34]. In particular, the survey identified a lack of teaching materials (audio or visual) and relevant texts as barriers to teaching or areas of suggested improvement. In general, although suicide prevention training is provided in medical education, little appears known about its content, structure, and perceived adequacy. This, therefore, is a suggested future direction of the current review. Finally, the extent to which clinical practice guidelines and/or additional resources are being utilized by providers and clinician educators, and their perceived utility, remains largely unknown. Research is thus warranted to examine training and education further, across disciplines, building on the current study.
Limitations and Future Directions
This report primarily evaluated the content and structure of existing clinical practice guidelines, but not the extent to which clinicians, educators, and trainees are actively using these guidelines. The authors recommend future research to explore the degree to which various guidelines are being used to inform clinical practice and training, as well as to investigate their perceived strengths and weakness in the context of medical education. This may guide improvements and advancements in the development of future guidelines and resources, adaptable to diverse clinical and research settings. A merging of practice guidelines—with additional resource documents—is a final recommendation of the present review, as this may narrow formalized recommendations, suggested techniques and measures, and in so doing, standardize clinical practice and training education in suicide risk assessment and management.
Implications for Educators.
Efforts should be made to routinize clinical decision making, referral, and risk management practices and to evaluate the lack of consensus across core competency areas of suicide risk assessment and management. A merging of clinical practice guidelines with briefer, and more user-friendly additional resource documents is recommended.
There is a need for increased research of standardized suicide risk assessment measures used across disciplines and their evidence-base. This should be incorporated into existing guidelines to result in increased uniformity in training and use, and a narrowing of recommended measures.
A thorough evaluation regarding the use of current clinical practice guidelines and tools within clinical practice and training—including perceived strengths and weaknesses of existing resources—is recommended to inform future refinements of clinical practice guidelines.
Acknowledgments
This work was supported by the following grant funding: NIH K23MH093490, DOD MSRC004 (Bernert).
Footnotes
Disclosures: On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- 1.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R. World report on violence and health. Geneva: World Health Organization; 2002. [Google Scholar]
- 2.Institute of Medicine (IOM) Reducing suicide: a national imperative. Washington: National Academic Press; 2002. [Google Scholar]
- 3.Silverman MM, Berman AL, Sanddal ND, O'Carroll PW, Joiner TE. Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide Life Threat Behav. 2007;37(3):248–63. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- 4.Food and Drug Administration (FDA); U.S. Department of Health and Human Services. Suicidal ideation and behavior: prospective assessment of occurrence in clinical trials. Silver Spring, MD: 2012. [Google Scholar]
- 5.Meyer RE, Salzman C, Youngstrom EA, Clayton PJ, Goodwin FK, Mann JJ, et al. Suicidality and risk of suicide—definition, drug safety concerns, and a necessary target for drug development: a brief report. J Clin Psychiatry. 2010;71(8):1040–6. doi: 10.4088/JCP.10cs06070ablu. [DOI] [PubMed] [Google Scholar]
- 6.Crosby AE, Ortega L, Melanson C. Self-directed violence surveillance: uniform definitions and recommended data elements, Version 1.0. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2011. [Google Scholar]
- 7.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159(6):909–16. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Academy of Child and Adolescent Psychiatry (AACAP). . Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2001;40(7 Suppl):24s–51. doi: 10.1097/00004583-200107001-00003. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association (APA) Practice guideline for the assessment and treatment of patients with suicidal behaviors. American Psychiatric Association; 2003. [PubMed] [Google Scholar]
- 10.American Psychiatric Association (APA) Assessing and treating suicidal behaviors: a quick reference guide. American Psychiatric Association; 2003. [Google Scholar]
- 11.The Assessment and Management of Risk for Suicide Working Group. VA/DOD Clinical Practice Guideline (CPG) for the assessment and management of patients at risk for suicide. 2013. pp. 1–190. Version 1.0. [Google Scholar]
- 12.ENA Emergency Nursing Resources Development Committee. Clinical practice guideline: suicide risk assessment full version. Emergency Nurses Association (ENA); 2012. [Google Scholar]
- 13.Wasserman D, Rihmer Z, Rujescu D, Sarchiapone M, Sokolowski M, Titelman D, et al. The European Psychiatric Association (EPA) guidance on suicide treatment and prevention. Eur Psychiatry. 2012;27(2):129–41. doi: 10.1016/j.eurpsy.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Magellan Clinical Practice Guideline Task Force. Magellan Clinical Practice guideline for assessing and managing the suicidal patient. Magellan Health Services; 2000. [Google Scholar]
- 15.Registered Nurses' Association of Ontario (RNAO) Assessment and care of adults at risk for suicidal ideation and behaviour. Toronto, Canada: Registered Nurses' Association of Ontario; 2009. [Google Scholar]
- 16.Committee SRA. Guidelines for the identification, assessment, and treatment planning for suicidality. Cambridge: Risk Management Foundation of the Harvard Medical Institutions; 1996. [Google Scholar]
- 17.State of Victoria Department of Health. Working with the suicidal person: clinical practice guidelines for emergency departments and mental health services. Melbourne, Victoria: Mental Health, Drugs, & Regions Branch, Victorian Government; 2010. [Google Scholar]
- 18.American Association for Suicidology (AAS) Assessing and Managing Suicide Risk (AMSR) Education Development Center, Inc. (EDC); Core competencies for the assessment and management of individuals at risk for suicide. [Google Scholar]
- 19.Clayton PJ. Suicide prevention: saving lives one community at a time. American Foundation for Suicide Prevention; [Accessed 18 April 2014]. http://www.afsp.org/index.php/content/download/9544/169597/file/Saving_Lives_One_Community_at_a_Time.pptx. [Google Scholar]
- 20.Clayton PJ. Suicide and the elderly. American Foundation for Suicide Prevention; [Accessed 18 April 2014]. http://www.afsp.org/index.php/content/download/3015/54627/file/Suicide_and_the_Elderly.pptx. [Google Scholar]
- 21.International Association for Suicide Prevention (IASP) [Accessed 18 April 2014];IASP guidelines for suicide prevention. http://www.iasp.info/suicide_guidelines.php.
- 22.Clinical Care and Intervention Task Force. Suicide care in systems framework. National Action Alliance; 2011. [Google Scholar]
- 23.Coleman M. Minimizing practice risks with suicidal patients. [Accessed 18 April 2014];Clinical Social Work. 2002 2(4) http://www.naswdc.org/practice/clinical/csw0204.pdf. [Google Scholar]
- 24.National Suicide Prevention Lifeline (NSPL) Suicide risk assessment standards and recommendations for an approach to asking lifeline callers about suicidality. National Suicide Prevention Lifeline; 2007. [Google Scholar]
- 25.Joiner T, Kalafat J, Draper J, Stokes H, Knudson M, Berman AL, et al. Establishing standards for the assessment of suicide risk among callers to the national suicide prevention lifeline. Suicide Life Threat Behav. 2007;37(3):353–65. doi: 10.1521/suli.2007.37.3.353. [DOI] [PubMed] [Google Scholar]
- 26.Substance Use and Mental Health Services Administration (SAMHSA) Promoting emotional health and preventing suicide: a toolkit for senior living communities. Rockville: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- 27.Substance Use and Mental Health Services Administration (SAMHSA) Preventing suicide: a toolkit for high schools. Rockville: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2012. [Google Scholar]
- 28.Substance Use and Mental Health Services Administration (SAMHSA) Suicide Assessment Five-step Evaluation and Triage (SAFE-T) Substance Abuse and Mental Health Services Administration; 2009. [Google Scholar]
- 29.Joiner TE, Walker RL, Rudd DM, Jobes DA. Scientizing and routinizing the assessment of suicidality in outpatient practice. Prof Psychol Res Proj. 1999;30(5):447–53. [Google Scholar]
- 30.Rudd DM, Joiner TE, Rajab H. Treating suicidal behavior: an effective time-limited approach. New York: Guilford Press; 2001. [Google Scholar]
- 31.Beautrais AL. Effectiveness of barriers at suicide jumping sites: a case study. Aust N Z J Psychiatry. 2001;35(5):557–62. doi: 10.1080/0004867010060501. [DOI] [PubMed] [Google Scholar]
- 32.Mott JA, Wolfe MI, Alverson CJ, Macdonald SC, Bailey CR, Ball LB, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988–95. doi: 10.1001/jama.288.8.988. [DOI] [PubMed] [Google Scholar]
- 33.Coverdale JH, Roberts LW, Louie AK. Encountering patient suicide: emotional responses, ethics, and implications for training programs. Acad Psychiatry. 2007;31(5):329–32. doi: 10.1176/appi.ap.31.5.329. [DOI] [PubMed] [Google Scholar]
- 34.Melton BB, Coverdale JH. What do we teach psychiatric residents about suicide? A national survey of chief residents. Acad Psychiatry. 2009;33(1):47–50. doi: 10.1176/appi.ap.33.1.47. [DOI] [PubMed] [Google Scholar]
- 35.Ellis TE, Dickey TO, Jones EC. Patient suicide in psychiatry residency programs: a national survey of training and postvention practices. Acad Psychiatry. 1998;22(3):181–9. doi: 10.1007/BF03341922. [DOI] [PubMed] [Google Scholar]
- 36.Rudd MD, Joiner T, Brown GK, Cukrowicz K, Jobes DA, Silverman M, et al. Informed consent with suicidal patients: rethinking risks in (and out of) treatment. Psychotherapy. 2009;46(4):459–68. doi: 10.1037/a0017902. [DOI] [PubMed] [Google Scholar]
- 37.Jobes DA. Managing suicide risk: a collaborative approach. New York: Guilford Press; 2006. [Google Scholar]
- 38.Brown GK. A Review of suicide assessment measures for intervention research with adults and older adults. Bethesda: National Institute of Mental Health; 2002. [Google Scholar]
- 39.Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62(2):185–200. doi: 10.1002/jclp.20222. [DOI] [PubMed] [Google Scholar]
- 40.Stanley B, Brown GK, Karlin B, Kemp JE, VonBergen HA. Safety Plan treatment manual to reduce suicide risk: veteran version. U.S. Department of Veterans Affairs; 2008. [Google Scholar]


