Abstract
Dance-based therapy has the potential to slow the progression of functional limitations in older adults. The purpose of this study was to explore the feasibility of measuring the impact of dance-based therapy on the nighttime restfulness patterns of older adults in an aging-in-place facility using passive bed sensors. A secondary data analysis of the continuous 2-month nighttime bed sensor data was reviewed for measurable change during a dance study. A measurable variation in nighttime restfulness level was detected between the dancers and nondancers, and no high or very high restlessness was detected during this period for the dance-based therapy group. Although these exploratory variations are modest, the findings suggest that bed sensors can be used to measure nighttime restfulness following a therapeutic dance intervention. More research is needed in this emerging area.
Keywords: gerontology, population focus, exercise, health behavior, symptom focus, sleep
Dance-based therapy as an intervention to maintain function, promote well-being, and improve the quality of life in older adults is an emerging area. A sedentary lifestyle can negatively impact the health and well-being of older adults and expedite functional decline. Regular exercise, in a form that engages the older adult and is therefore sustainable over time, such as dance, has the potential to increase overall functional capacity, thus slow the progression of decline (Keough, Kilding, Pideon, Axhey, & Gillis, 2009).
The association between exercise, sleep, and optimal health has been studied over the past several decades (Millman, 2012). What is not known is whether exercise in the form of dance therapy has an effect on the nighttime restfulness on older adults and if this can be monitored, measured, and reported using nighttime passive bed sensors.
The findings reported in the literature are scant and mixed related to the correlation of exercise and sleep disorders in the older adult population. Many research reports focus on sleep disorders and sleep quality, rather than interventions to impact well-being (Neikrug & Ancoli-Israel, 2010; Wolkove, Elkholy, Baltzan, & Palayew, 2007). Buman, Heckler, and Bliwise (2011) reported the complexity of measuring sleep quality following exercise in older adults includes consideration of the initial physical fitness level and baseline sleep quality. The purpose of this study was to explore the feasibility of measuring the effect of dance-based therapy on the nighttime restfulness patterns of older adults in an aging-in-place facility using passive bed sensors.
Dancing is a mode of physical activity that may allow older adults to improve their physical function, health, and well-being (Keough et al., 2009). Dance-based exercise is a new area of research that has the capacity to be transitioned to practice with older adults in multiple settings, facilitated by trained instructors and sustained for several years (Krampe, 2011; Krampe et al., 2010; Sandel et al., 2005). A specific type of dance-based therapy, The Lebed Method™, also known as Healthy-Steps, was used for this study (Lebed, 2002, 2008). Healthy-Steps was recently recognized as having an intermediate level of evidence in the category of Disease Prevention and Health Promotion Services (Older Americans Act Title IIID) by the Administration on Aging (2012).
Healthy-Steps is a medically based therapeutic exercise and movement program that uses uplifting age-appropriate music and props. This low-impact aerobic program, founded in 1980 by a professional dancer and her physician brothers, was one of the first programs to do clinical trials and continues to be studied as an evidence-based dance method (Krampe, 2011; Molinaro, Kleinfeld, & Lebed, 1986; Sandel et al., 2005). Initially developed to help breast cancer survivors after treatment regain range of motion and flexibility and decrease depression, it now has also been found effective with older adults to increase range of motion and mobility (Krampe, 2011; Krampe et al., 2010). Previous pilot research on dance therapy with older adults has established and reported a mild effect on walking speed and moderate effect in forward, right, and left reach after fourteen, 45-minute sessions of dance therapy conducted over a 6-week period (Krampe, 2011).
The benefits of early detection using passive sensors for older adults have been established and include the capacity to augment traditional health care and improve nurse care coordination (Rantz et al., 2012; Rantz, Skubic, & Miller, 2009). Furthermore, emerging research using passive sensors has been able to establish an early warning detection system for illness, cardiovascular events, urinary tract infections, and falls (Rantz et al., 2012; Rantz, Skubic, Miller, & Krampe, 2008).
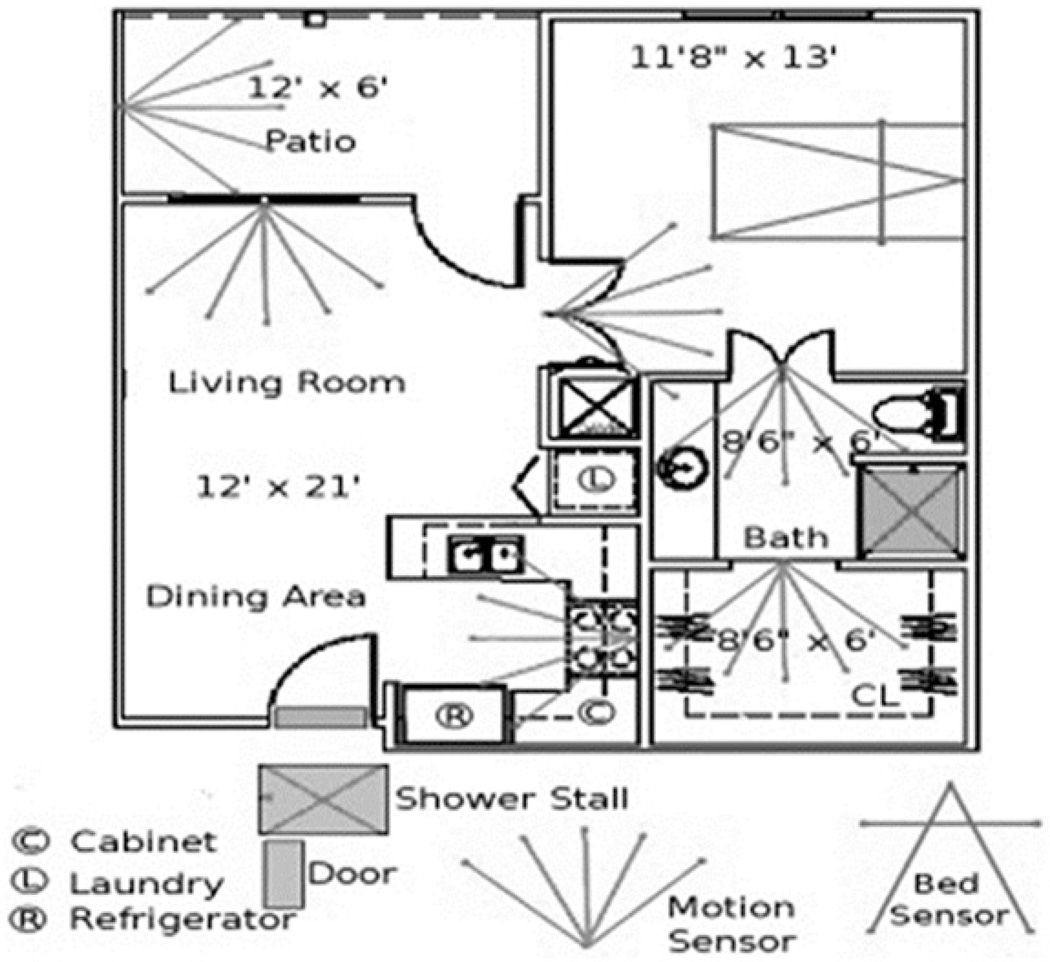
A network of passive sensors was installed in the apartments of volunteers at the Midwest aging-in-place facility where this study was conducted as displayed in Figure 1. The sensor suite included motion sensors and a bed sensor.
Figure 1.
Sensor network.
Because this is a preliminary feasibility work using passive sensor technology for monitoring nighttime restfulness following dance-based therapy, the focus of this study is the bed sensor. The bed sensor was developed by collaborators at the University of Virginia using a passive, ballistocardiography-based sleep-monitoring system (Mack, Patrie, Suratt, Felder, & Alwan, 2009). A bed sensor detects presence in bed as well as restlessness, breathing, and pulse rates while sleeping. The bed sensor is a pneumatic strip that lies on top of the mattress and under linens. The pneumatic tube displaces air as a person lies in bed. Displacement varies for movement, breathing, and pulse; with signal processing, the bed sensor distinguishes between different levels of restlessness, breathing, and pulse. The sensor measures four levels of restlessness (based on time of continuous movement) as well as three levels of qualitative pulse and respiration rates (low, normal, and high). The sensor signals are date and time stamped, and then stored in a database to analyze potential patterns of decline or change (Skubic, Alexander, Popescu, Rantz, & Keller, 2009).
A common change associated with aging is a disruption to the daily sleep−wake cycle. It has been estimated that as many as 50% of older adults complain about difficulty initiating or maintaining sleep (Neikrug & Ancoli-Israel, 2010). Poor sleep quality results in an increased risk of significant morbidity and mortality. In younger adults, poor sleep quality had a consistent effect on cognitive function, which may suggest that sleep problems contribute to the cognitive changes that accompany old age. The multifactorial nature of variables affecting sleep in old age cannot be overstated.
The decreased ability to maintain high sleep quality results from factors that accompany aging, such as comorbidities, medical and psychiatric illness, increased medication use, and a higher prevalence of specific sleep disorders. Given the large number of older adults with sleep complaints and sleep disorders, there is a need for health care professionals to have an increased awareness of these sleep disturbances to better enable them to assess and intervene with these patients (Neikrug & Ancoli-Israel, 2010).
Aging is associated with several well-described normal changes in patterns of sleep. Typically, there is a phase advance in the normal sleep cycle: Older people tend to go to sleep earlier in the evening but also wake earlier. They may also wake more frequently during the night and experience fragmented sleep (Wolkove et al., 2007).
Given that changes in sleep quality and quantity in later life have implications for quality of life and level of functioning, it is important to explore this issue further. It has been established that passive sensor technology has the capacity to detect early signs of illness onset in older adults (Rantz et al., 2012). This study uses a secondary data analysis methodology to investigate if this same passive sensor technology can detect measurable changes in nighttime restfulness, following a therapeutic dance-based movement intervention. To the authors’ knowledge, no previous research has been reported using bed sensors to continuously monitor the nighttime restfulness of older adults for a 2-month period of low-impact aerobic dance-based therapeutic exercise.
The research questions are as follows:
Research Question 1: Can passive bed sensors be used over a continuous 2-month period to measure nighttime restfulness patterns of older adults participating in a dance-based therapy study?
Research Question 2: Do the aggregate patterns of dance study subjects’ sleep movement patterns change (defined as bed restlessness) over an 8-week period compared with the no-dance group?
Method
Design
Following approval by the University of Missouri, Columbia Institutional Review Board, a secondary data analysis methodology was used. Bed sensor data were compared with individual subjects’ 2-month (January–February, 2010) dance-therapy intervention attendance records (Krampe, 2011). Dayto-day, week-to-week, and 1-month pre−post intervention nighttime restlessness patterns were reviewed for overall changes, resulting in the total data analysis period of December 2009–March 2010. A standard formatting process previously established by the research engineering team at the aging-in-place facility was used for the bed sensor data collected between December 2009 and March 2010 (Skubic et al., 2012). The process to analyze the bed sensor data and translate the findings to compare an individual’s baseline nighttime restlessness data to a measurable change is described further in the “Analysis” section. All data were provided with no patient identifiers linked to the subjects.
Sample
The sample was a subset of subjects who were simultaneously participating in two research studies during December 2009–March 2010 at the aging-place facility: (a) Study 1—A randomized control trial: Dance-Based Therapy to Decrease Fall Risk in Older Persons and (b) Study 2—A Passive Sensor Networks study in progress by the Eldercare Research Team.
The inclusion criteria for this study were (a) having bed sensors installed during the 4-month study time frame and (b) sleeping in the bed. Of the 14 eligible subjects who met the criterion, 5 were excluded from final analysis because they only had the room motion sensors installed in their apartment and no bed sensors, or did not sleep in bed. All participants reported no physical problem limiting them from participating in mild low-impact, slow rhythmic dance movements.
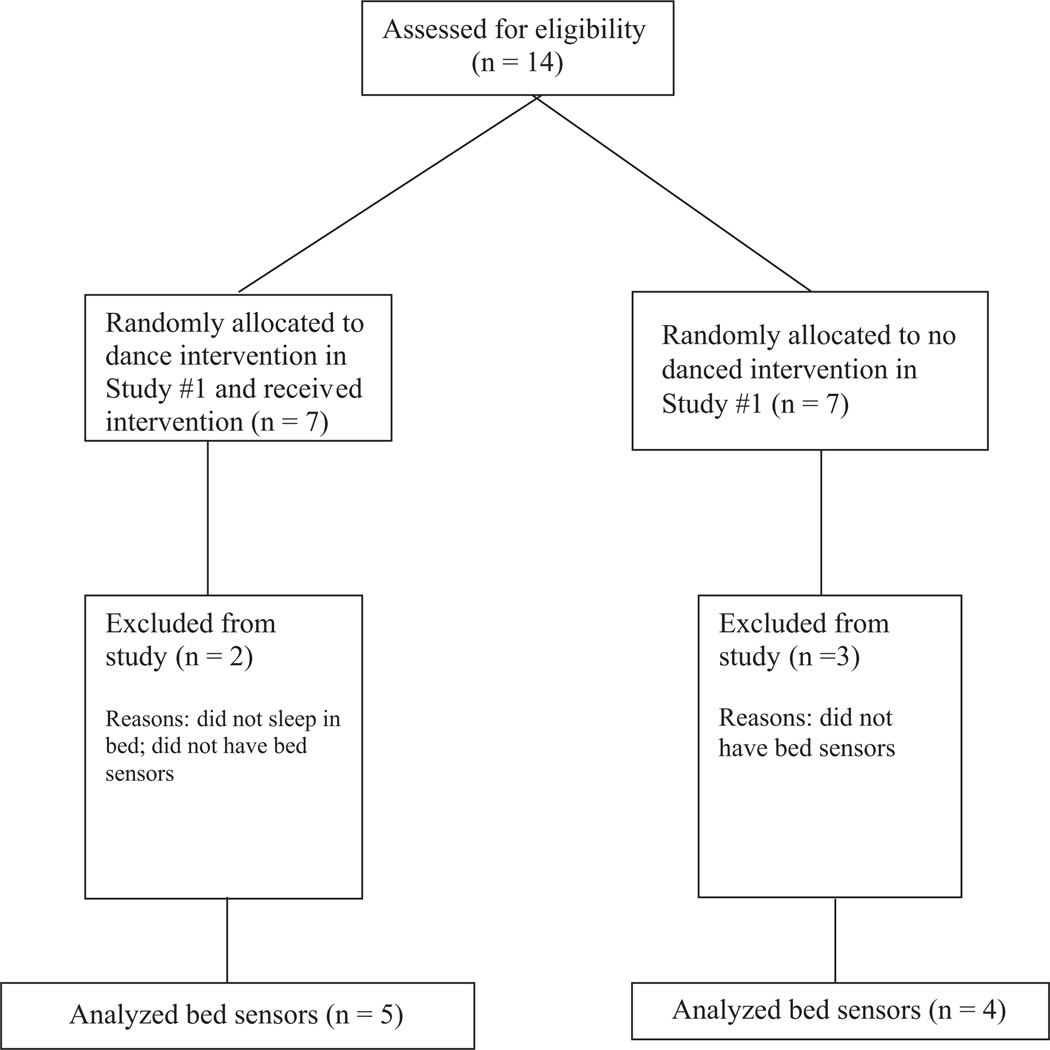
The remaining total (n = 9) included dance (n = 5) and no-dance (n = 4) subjects. The individual bed sensor data were compiled, aggregated, and then analyzed for each group. The subject flow diagram in Figure 2 displays the eligibility analyses.
Figure 2.
Consolidated standards of reporting trials (consort) flow diagram: Eligibility analyses.
Intervention
The dance group was asked to attend 18 dance sessions, three times each week for 6 weeks. The sessions included 10 min of warm-up movements, 30 min of dance-based therapy, and 5 min of cool down. The dance-therapy protocol included low-impact aerobics and stretching mixed with dance movements. The dance movements were based on simple jazz and ballet steps. Choreographed specifically for older adults, they included movements to shift weight, reach arms in every direction, lift legs, march, and flex feet. Both seated and standing options were offered at each session (Krampe, 2011).
Measures
Bed restlessness parameters transmitted by bed sensors
The bed sensor technology used for this study was the restlessness component. Four levels of bed restlessness are captured. The sensor generates a Level 1 (low) restlessness event if there is 1 to 3 seconds of continuous movement; 4 to 6 seconds of movement creates a Level 2 event; 6 to 9 seconds is a Level 3 event; and more than 9 seconds of continuous movement generates a Level 4 event (Rantz et al., 2010). The subject’s total number of events per day and week were analyzed to determine if patterns of change could be identified during the 2-month period of the dance-based study intervention.
Analysis
The variables used for the bed sensor analysis were the restlessness levels (level of activity in bed recorded every 3 seconds). These values were then recorded separately over a 6-hr period from midnight to 6:00 a.m. For each variable, a monthly (December 2009 to March 2010) average per subject was generated excluding the days the resident was away from home. The Eldercare Research Team at this facility has defined one night as 6:00 p.m. to 6:00 a.m. for ongoing sensor technology research in progress and data analysis. Although 8:00 p.m. to 8:00 a.m. would be a more specific time frame to monitor nighttime restfulness for this study, the previously standardized time frame was used rather than cross a 24-hr boundary. Thus, the period from midnight to 6 am was used.
Data were graphically displayed and tests of inference were inappropriate in this exploratory work.
Results
Participant Characteristics
Fourteen aging-in-place older adult subjects ranging in age between 63 and 96 (10 females; M age = 85 years; SD = 8.96) met the criteria and were assessed for eligibility: n = 7, dance intervention; n = 7, no-dance intervention. All of the subjects were Caucasian. The baseline characteristics of the groups were similar with the dance group ranging in age from 71 to 96 (7 females; M age = 86.57 years, SD = 8.19) and control group ranging in age from 63 to 93 (5 females; M age = 83.43 years; SD = 3.44). See Figure 2: Flow Diagram.
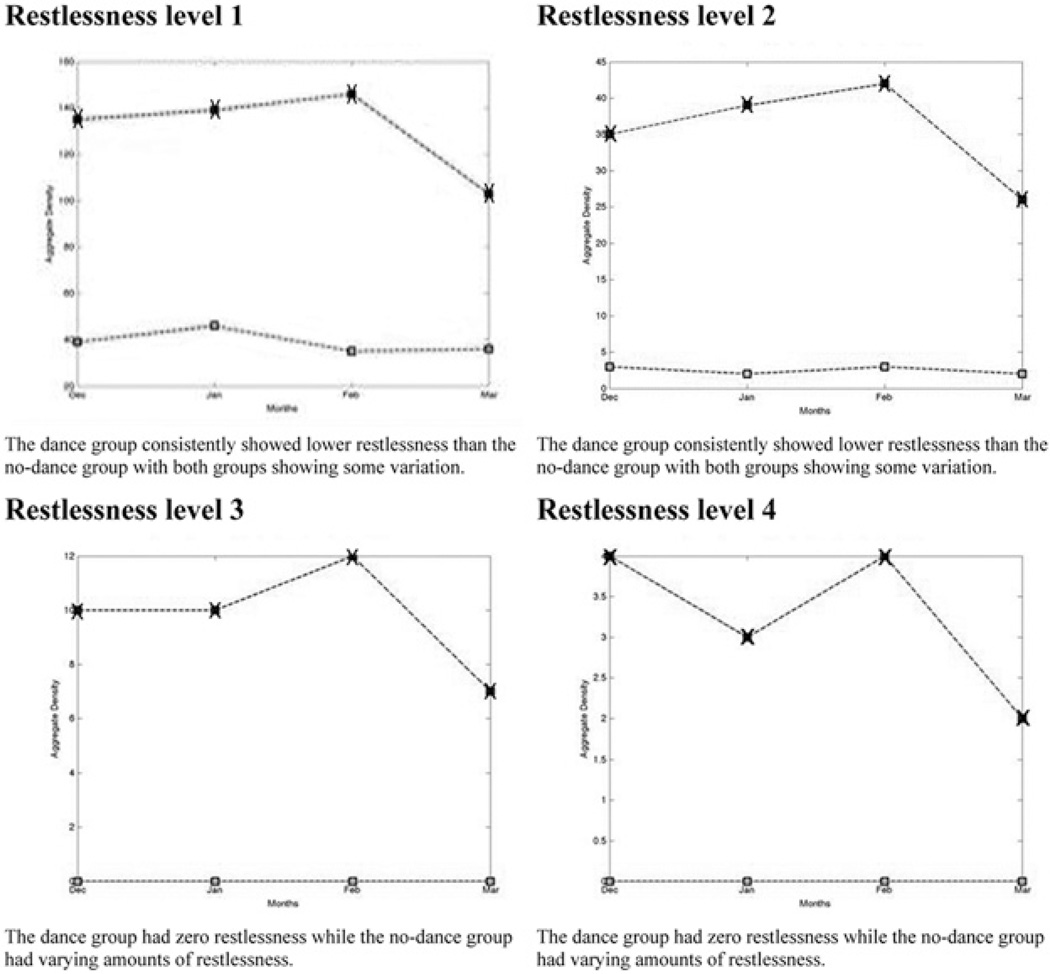
Nighttime Restlessness
All bed data graphs shown here are for nighttime activity from midnight to 6:00 a.m. The pulse and respiration data were not inclusion measures in this preliminary feasibility study. Figure 3 displays the restlessness parameters transmitted by the bed sensors. A reduced level of nighttime restlessness is noted in each level for the dance group versus no dance. Of note is the zero restlessness Levels 3 and 4 for the dance group. These results can be interpreted as the restlessness periods during the hours of midnight and 6:00 a.m. for the subjects completing the dance intervention, measured by the passive bed sensors, was reduced, compared with the no-dance group during the same period.
Figure 3.
Aggregate nighttime restlessness: Dance group (lower line) versus no dance (upper line).
These preliminary data confirm that (a) passive bed sensors can be used over a continuous 2-month period to measure nighttime restfulness patterns of older adults participating in dance-based therapy study and (b) the aggregate patterns of dance study subjects’ sleep movement patterns changed (defined as bed restlessness decreasing) in the desired direction over an 8-week period, compared with the no-dance group.
Discussion
The results of this exploratory study are promising. It is feasible to capture patterns of nighttime bed movement and a comparative control group movement continuously during an 8-week dance study. Although this health promotion application of bed sensor technology is at an exploratory stage, this study confirmed that a ballistocardiography-based sleep-monitoring system previously used to detect signs of early illness can also be used to monitor desirable change in sleep patterns over an 8-week dance study period.
The sensor network generates a large volume of data that make identifying the relevant changes in the data challenging. The early detection of illness methodology that was adapted for this study used trends over time to estimate changes in health status. A highly researched and established network of passive sensors installed in the subject’s apartment is used in the early detection of illness research to measure changes in health status (Rantz et al., 2013). This study only used the bed sensor restlessness component. In addition, the bed sensor generates three levels (low, normal, and high) of breathing and pulse data, not measured in this study. A more sensitive bed sensor that produces quantitative data is needed to identify the small differences associated with dance therapy-related changes in sleep quality and possibly changes on pulse or respirations. A new sensor developed by the research team is currently being tested and could be considered for use in future dance-therapy studies (Rosales, Skubic, Heise, Devaney, & Schaumburg, 2012).
Another challenge with this study is linking changes in the sensor data to changes in health and sleep quality. Many factors including changes in medications, physical therapy, and illnesses could affect the nighttime restlessness, restfulness, and overall sleep quality of older adults. Additional research is needed to account for these factors.
Although this pilot was exploratory, the small sample size limits generalization of findings to the general population. The population recruited was Caucasian, which does not provide a representative sample of older adults. All of the subjects were female, posing an additional limitation. Future studies should include diversity in race and gender.
Given the small sample size, the relative short duration of the study, and modest variations, the restlessness level findings should be interpreted cautiously. However, using the bed sensor methodology established for early detection of illness (Rantz et al., 2013; Skubic et al., 2012), the findings of no high (Level 3) or very high (Level 4) restlessness (over 9 min) in the dance subjects during the dance study time frame is considered a positive finding. As stated earlier, it is difficult to measure improved sleep quality following exercise for this population. Thus, using passive bed sensors may be an option to consider when evaluating future exercise interventions. This objective passive methodology may be useful to include as a second measure of sleep quality, along with established subjective methods when evaluating exercise benefits.
The methodology used in this exploratory study does not account for related and existing sleep disorders, or baseline level of exercise activity with the subjects in each group. These factors may affect the amount of change expected following an exercise intervention. This study does not include sleep diaries or any self-report verification to determine if the subjects perceived to have sleep restlessness issues. Future research should include measures to establish perceived restfulness.
Research on dance-based therapy as an intervention to maintain function, promote well-being, and improve the quality of life in older adults is an emerging area. Passive bed sensors can be used to extend the knowledge of the benefit of dance-based therapy and measure optimal nighttime restfulness. More research is needed.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Administration on Aging. Disease prevention and health promotion services (OAA Title IIID): Intermediate criteria. 2012 Retrieved from http://www.aoa.gov/AoARoot/AoA_Programs/HPW/Title_IIID/index.aspx.
- Buman M, Heckler E, Bliwise D. Moderators and mediators of exercise-induced objective sleep improvements in midlife and older adults with sleep complaints. Health Psychology. 2011;30:579–587. doi: 10.1037/a0024293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keough J, Kilding A, Pideon P, Axhey L, Gillis D. Physical benefits of dance for healthy older adults: A review. Journal of Aging and Physical Activity. 2009;17:1–23. doi: 10.1123/japa.17.4.479. [DOI] [PubMed] [Google Scholar]
- Krampe J. Exploring the effects of dance-based therapy on balance and mobility in older adults. Western Journal of Nursing Research. 2011;35:39–56. doi: 10.1177/0193945911423266. [DOI] [PubMed] [Google Scholar]
- Krampe J, Rantz MJ, Dowell L, Schamp R, Skubic M, Abbott C. Dance-based therapy in a program of all-inclusive care for the elderly: An integrative approach to decrease fall risk. Nursing Administration Quarterly. 2010;34:156–161. doi: 10.1097/NAQ.0b013e3181d91851. [DOI] [PubMed] [Google Scholar]
- Lebed S. Thriving after breast cancer: Essential healing exercise for body and mind. New York, NY: Broadway Books; 2002. [Google Scholar]
- Lebed S. The Lebed Method: Focus on dance and healing movement. 2008 Available from http://www.gohealthysteps.com/ [Google Scholar]
- Mack DC, Patrie JT, Suratt PM, Felder RA, Alwan M. Development and preliminary validation of heart rate and breathing rate detection using a passive, ballistocardiography-based sleep monitoring system. IEEE Transactions on Information Technology in Biomedicine. 2009;13:111–120. doi: 10.1109/TITB.2008.2007194. [DOI] [PubMed] [Google Scholar]
- Millman RP. Sleep and aging. Medicine Health/Rhode Island. 2012;95(3):88–90. [PubMed] [Google Scholar]
- Molinaro J, Kleinfeld M, Lebed S. Physical therapy and dance in the surgical management of breast cancer: A clinical report. Physical Therapy. 1986;66:967–969. doi: 10.1093/ptj/66.6.967. [DOI] [PubMed] [Google Scholar]
- Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult—A mini-review. Gerontology. 2010;56(2):181–189. doi: 10.1159/000236900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Alexander G, Aud M, Wakefield B, Koopman R, Miller S. Improving nurse care coordination with technology. Computers, Informatics, Nursing. 2010;28:325–332. doi: 10.1097/NCN.0b013e3181f69838. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Koopman RJ, Alexander G, Phillips L, Musterman KI, Miller SJ. Automated technology to speed recognition of signs of illness in older adults. Journal of Gerontological Nursing. 2012;38(4):18–23. doi: 10.3928/00989134-20120307-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Miller SJ. Using sensor technology to augment traditional healthcare; Proceedings from 31st Annual International Conference of the IEEE EMBS; Minneapolis, MN. 2009. pp. 6159–6162. [DOI] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Miller SJ, Galambos C, Alexander G, Keller J, Popescu M. Sensor technology to support aging in place. Journal of the American Medical Directors Association. 2013;14:386–391. doi: 10.1016/j.jamda.2013.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rantz MJ, Skubic M, Miller SJ, Krampe J. Using technology to enhance aging in place; Proceedings from International Conference on Smart Home and Health Telematics; Ames, IA. 2008. pp. 169–176. [Google Scholar]
- Rosales L, Skubic M, Heise D, Devaney MJ, Schaumburg M. Heartbeat detection from a hydraulic bed sensor using a clustering approach; Proceedings of the 34th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; San Diego. CA. 2012. pp. 2383–2387. [DOI] [PubMed] [Google Scholar]
- Sandel S, Judge J, Landry N, Faria L, Ouellette R, Majczak M. Dance movement improves quality-of-life measures in breast cancer survivors. Cancer Nursing. 2005;28:301–309. doi: 10.1097/00002820-200507000-00011. [DOI] [PubMed] [Google Scholar]
- Skubic M, Alexander G, Popescu M, Rantz MJ, Keller J. A smart home application to eldercare: Current status and lessons learned. Technology and Health Care. 2009;17(3):183–201. doi: 10.3233/THC-2009-0551. [DOI] [PubMed] [Google Scholar]
- Skubic M, Rantz MJ, Miller SJ, Guevara RD, Koopman RJ, Alexander GL, Phillips LL. Non-wearable in-home sensing for early detection of health. In: Schultz R, editor. Quality of life technology for the disabled and elderly. Boca Raton, FL: CRC Press; 2012. pp. 227–244. [Google Scholar]
- Wolkove N, Elkholy O, Baltzan M, Palayew M. Sleep and aging: Sleep disorders commonly found in older people. Canadian Medical Association Journal. 2007;176:1299–1304. doi: 10.1503/cmaj.060792. [DOI] [PMC free article] [PubMed] [Google Scholar]