Abstract
Objective
A system for measuring posterior-to-anterior spinal stiffness (PAS) was developed for use in clinical trials of manipulation for low back pain (LBP). The current report is an analysis of the baseline PAS data, with particular emphasis on relationships between PAS and clinical and demographic characteristics.
Methods
Posterior-to-anterior spinal stiffness measurements were recorded over the spinous processes of the lumbar spines from patients who had LBP. The system uses electronic sensors to record displacement and force, whereas a human operator provides the force of indentation. Clinical and outcome measures were compared with spinal stiffness.
Results
We recruited 192 patients (89 female and 103 male; average age, 40.0 years; SD, 9.4 years). The average Roland-Morris score was 9.7 (SD, 3.2) on a 24-point scale. The Visual Analog Scale pain scores were 55.7 (SD, 20.9) on a 100-mm scale. Stiffness values ranged from 4.16 to 39.68 N/mm (mean, 10.80 N/mm; SD, 3.72 N/mm). Females’ lumbar spines were, on the average, 2 N/mm more compliant than males (P < .001).
Conclusions
The PAS system of computer-monitored equipment with human operation performed well in this clinical study of LBP. Spinal stiffness was found to be different between males and females, and age and body mass index were related to PAS. We found no significant relationship between the severity or chronicity of the LBP complaint and spinal stiffness. There was little agreement between the stiff or tender segments identified by the clinicians using palpation and the segment that measured most stiff using the PAS device.
Key Indexing Terms: Chiropractic, Lumbar Spine, Biomechanics, Low Back Pain, Stiffness, Tests and Measurement, Manipulation, Spinal
Spinal stiffness assessments are frequently performed as part of patient evaluation in chiropractic, osteopathy, and physical therapy. Often referred to as posterior-to-anterior spinal stiffness (PAS), in chiropractic, the method might be called motion palpation or joint end-play assessment. The clinician typically will use the palm of his or her hand to press on the spine and feel for restricted movement.
Studies of spinal stiffness or motion palpation in chiropractic and physical therapy most often find limited interexaminer reliability of the assessment.1,2 Because these are commonly used clinical tests, researchers have attempted to develop instruments to help improve the objectivity of the measures. Over the past 20 years, several devices have been reported in the literature.3–11 Such devices typically use a computer-controlled motor to indent the spine or adjacent tissues while monitoring the amount of displacement of the skin surface and the amount of force developed. These devices report very good reliability and accuracy.6
Posterior-to-anterior spinal stiffness measurement is a more complex task than it might seem at first. Investigators have identified a host of variables that can influence the measurement. Relative to the patient, variables include patient positioning and the support surface,12,13 respiration and abdominal pressure,14,15 paraspinal muscle activity,16,17 and the thickness of soft tissue between the indenter and the underlying bones.5,10,18 Lee et al18 suggested that PAS measures may have more to do with the supporting structures than the intrinsic properties of the spine. Relative to the indentation process itself, the variables include the location and direction of load application,8,10,19–22 the rate of loading,23,24 the magnitude of the peak load used,25 and the size of the indenter.24 Any system of PAS measurement must control or account for as many of these variables as possible to provide valid measurements. A model has been developed, which includes elements of soft tissue compression at the points of contact between the patient and the supporting surface and under the indenter, as well as skeletal movements.18,26
Interpretation of PAS measurements is also complex. Although clinicians conceive of the test as being indicative of intersegmental motion, particularly at the level of the segment being directly contacted during the test, studies have shown that the movements associated with PAS testing are distributed throughout the lumbodorsal spine and pelvis. When pressing on the midlumbar spine, the whole lumbar spine extends, and there is also rotation of the ribcage and pelvis.27–30 Imaging studies with radiography30 and magnetic resonance imaging (MRI)31,32 have shown that all of the lumbar vertebrae are involved in motion during PAS testing. The movements are generally rotational in nature, producing relative extension of the segments, although flexion can be seen at the lowest lumbar levels when loading is directed to the upper lumbar segments. Powers et al32 and Kulig et al31 applied posterior to anterior loads to each of the lumbar segments and found that the greatest amount of intersegmental rotations did occur at the segment contacted. These investigators used manually applied loads estimated at between 20- and 25-lb force (9–11 kg).
Posterior-to-anterior spinal stiffness testing shows some promise as either a diagnostic tool or an outcome measure in low back pain (LBP) studies. Neither area has been well investigated. Lumbar PAS over the spinous process has been assessed in nonspecific patients with LBP and found to have no substantial difference with the measure in pain-free controls.9,33 These were small studies, however, and did not use matched pairs of patients with LBP and pain-free controls. Using a different type of PAS measuring system, with the PA load contacting the paraspinal muscles rather than the spinous process, Brodeur and DelRe3 found a difference in lumbar spine stiffness between male patients with LBP and pain-free male controls. In an animal model of lumbar spine degeneration, Kawchuk et al34 have found that PAS measurement is sensitive to disk lesions. Kawchuk’s device is somewhat different from other testing systems in that it uses an ultrasound sensor at the point of contact with the loading probe to detect changes in soft tissue thickness during the test.5,35 Hence, the method is better able to detect skeletal movement independent of soft tissue indentation. In a cadaver model, PAS measurements in the thoracic spine correlated with direct measurement of intersegmental flexibility in flexion/extension movements.36 Thus, although PAS does seem to provide information about deep lumbar structure, now, the sensitivity and specificity of the measure for detecting spinal joint dysfunction related to LBP in humans are unknown.
Posterior-to-anterior spinal stiffness testing has not been widely used as an outcome measure in clinical trials. In a longitudinal study, spinal stiffness was found to decrease by 8% (1.2 N/mm) when patients were no longer in pain.33 However, studies in asymptomatic participants have not shown any changes in PAS in the short term in response to mobilization,37,38 and the only study to measure PAS in patients with LBP also failed to show any change with a single session of mobilization.39 There is a need for studies comparing the results of a course of therapy to changes in biomechanical parameters, such as PAS.
We developed a hand-held device to take measurements of spinal stiffness of patients with nonspecific LBP in a clinical study of the relationship between those patients’ baseline biomechanical and demographic characteristics and their response to spinal manipulation. In earlier studies, we found that the instrument exhibits substantial intraexaminer reliability, with an intraclass correlation coefficient of 0.790.40 Repeated testing showed a standard error of measurement of 1.62 N/mm. The current report is an analysis of the PAS data from that clinical study, with particular emphasis on relationships between PAS and clinical and demographic characteristics.
Methods
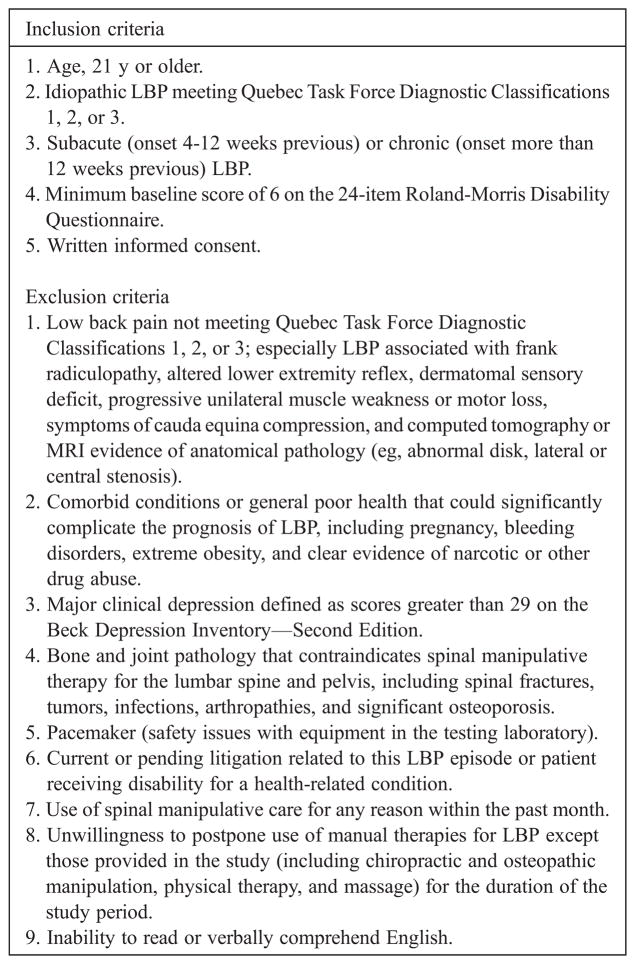
The project was approved by the college’s institutional review board. Patients were recruited from the local population using print ads, radio announcements, and direct mail. On their initial visit, prospective patients signed an informed consent form and completed a packet of enrollment forms and baseline outcomes surveys including the Roland-Morris Questionnaire (RMQ), Medical Outcomes Trust 36-Item Short-Form Survey, Visual Analog Scale (VAS) for pain, Pain Disability Index, and Beck Depression Inventory. Patients were screened for inclusion and exclusion criteria (Fig 1) by a study coordinator and examining doctor of chiropractic. The 2 inclusion criteria were that the LBP was of at least 4 weeks’ duration and the severity was at least 6 on the 24-point RMQ. The physical examination was performed over the course of the study by 3 chiropractors with a minimum of 10 years of experience. The examination included range of motion (ROM) tests, orthopedic tests, and palpatory tenderness and stiffness tests. Range of motion was performed with an electronic dual inclinometer system (Jtech Medical, Salt Lake City, Utah). The clinician located the lumbar spinous processes by palpation with respect to the crest of the ilia and the posterior inferior iliac spines (PSIS). The clinician pressed on each of the 5 spinous processes and rated each joint as stiff or not stiff. The clinician pressed on the PSIS to judge the sacroiliac joint stiffness on each side. Tenderness on palpation was scored on a 0 to 10 scale by asking the patient to rate their pain when the clinician pressed on each spinous process or PSIS (0 indicates no pain, 10 indicates the most severe pain).
Fig 1.
Inclusion and exclusion criteria for the clinical study
Enrolled patients had a baseline biomechanics assessment on their second visit to the research clinic, which included a postural sway test, ROM, and PAS. This report describes the PAS results only. The PAS measurement methods and equipment are described fully in a previous report.40 Briefly, the PAS device consisted of a plastic rod with an inline force transducer (Omegadyne, Inc, LC201-50, Sunbury, Ohio) mounted at the lower end and a position tracking sensor mounted at the upper end. A Polhemus Liberty motion tracking system (Virtalis Group, Manchester, UK) monitored the location of the rod, while a Motion Monitor (Innovative Sports Training, Chicago, Ill) software recorded data on both rod location and force. In use, the device was pressed manually into the soft tissue overlying the lumbar spinous processes of patients, while force and displacement data were recorded. The computer provided audible feedback to the operator when the target force was reached. The lumbar spinous processes were located by palpation and marked with a skin marker. We tested each spinal level from L1 through L5 with 5 cycles of 80 N of compression. If the patient was unable to tolerate 80 N, the target force was decreased to 5 N below his/her pain tolerance; no testing was performed when a patient could not tolerate more than 50 N. The 5-cycle test on one lumbar segment was completed within 5 seconds. Patients were prone on a hard wooden table for the testing and were asked to exhale fully and suspend their breathing during the test.
Data Reduction
Biomechanics technicians who performed the testing and data reduction were blinded to the demographic and clinical data. During data reduction, linear regression was used to calculate the slope of the force-displacement relationship resulting in a stiffness value in newtons per millimeter (N/mm). The regression was only performed on the data in the 20-N range 5 N below the maximum testing load used (eg, for a test load of 80 N, linear regression was performed on the segment from 55 to 75 N). During data reduction, we rejected the stiffness value on a cycle-by-cycle basis if the regression coefficient (R2) was less than 0.90. The data for the first depression were ignored, and an average stiffness value for the test was calculated from cycles 2 to 5. Posterior-to-anterior spinal stiffness testing also resulted in variables related to the performance of the test, including the patient’s most tender lumbar segment, the threshold force that produced pain at that level (if less than 80 N), and the maximum load that was used in the test.
Statistical Analysis
A complete data set was compiled from outcomes surveys, demographic, clinical, and biomechanical data sets, and ported to SPSS for Windows (version 12; SPSS, Inc, Chicago, Ill). Descriptive statistics were tabulated on the PAS variables, particularly the spinal stiffness at each segment and the threshold sensitivity. Bivariate correlations were explored between the segmental stiffness values and a selection of patient characteristics, including age, sex, and body mass index (BMI), and clinical findings including, RMQ score, VAS, chronicity of complaint, and lumbar ranges of motion in flexion and extension.
The palpation data on stiffness and tenderness were evaluated in an attempt to identify which lumbar segment was found to be most stiff or most tender. Likewise, the PAS data were used to identify which segment had the greatest measured stiffness.
Results
We recruited 192 patients (89 female and 103 male; average age, 40.0 years; SD, 9.4 years) for the study. The average Roland-Morris score was 9.7 (SD, 3.2) on a 24-point scale. Initial VAS for pain scores were 55.7 (SD, 20.9) on a 100-mm scale, where 100 is the worst pain the patient could imagine. Table 1 shows these baseline descriptive statistics, along with weight, BMI, chronicity of complaint, and lumbar ROM. Most of the variables were normally distributed and could be well represented by mean values and SDs. Chronicity, however, was significantly skewed with nearly half of the patients having had their complaint from between 4 weeks and 4 years. Chronicity is represented by a frequency distribution in Table 1.
Table 1.
Descriptive statistics on selected baseline measures (n = 192)
| Variable | Mean (SD) |
|---|---|
| Age (y) | 40 (9.41) |
| Weight (lb) | 195.85 (43.71) |
| Weight (kg) | 89.02 (19.87) |
| BMI | 29.84 (6.69) |
| VAS (0–100) | 55.65 (20.90) |
| Roland-Morris score (0–24) | 9.68 (3.20) |
| LS active flexion (°) | 56.18 (30.72) |
| LS active extension (°) | 18.28 (8.70) |
| Chronicity a (y) | No. of patients |
| <1 | 39 |
| 1–4 | 50 |
| 5–8 | 26 |
| 9–12 | 24 |
| 13–16 | 26 |
| >16 | 27 |
Presented as a frequency distribution due to skewness.
Not all patients could tolerate the PAS test because of spinous process sensitivity. Posterior-to-anterior spinal stiffness measures were recorded for 173 patients; however, 11 patients had incomplete tests, where one or more segments were not recorded because of extreme sensitivity or equipment malfunction. Seventy-four percent of patients could withstand 80 N of load without pain. The average time for indentation and retraction of the probe was not the same; indentation averaged 1.16 seconds (SD, 0.39 seconds) and retraction 0.50 seconds (SD, 0.20 seconds). The average rate of loading, although varying across patients, was consistent across all segments, averaging 0.65 cycles/s (SD, 0.18 cycles/s).
Stiffness values ranged from 4.16 to 39.68 N/mm (mean, 10.80 N/mm; SD, 3.72 N/mm). There was a significant difference in spinal stiffness values between females and males (Table 2). Females’ lumbar spines were, on average, 2 N/mm more compliant than males’ (P <.001).
Table 2.
Posterior-to-anterior stiffness measures by lumbar segment and sex
| Mean (SD) of PA stiffness (N/mm)
|
|||
|---|---|---|---|
| Segment | All patients (n = 162) | Female (n = 64) | Male (n = 98) |
| L1 | 10.25 (2.98) | 9.26 (2.82) | 10.97 (2.91)* |
| L2 | 10.45 (3.72) | 9.29 (3.62) | 11.30 (3.58)* |
| L3 | 10.82 (3.85) | 9.38 (2.99) | 11.83 (4.07)* |
| L4 | 10.81 (4.24) | 9.86 (4.97) | 11.48 (3.51)* |
| L5 | 11.12 (3.73) | 9.55 (2.74) | 12.14 (3.93)* |
Significant differences between sex (P < .001).
There was no difference in PAS with respect to lumbar levels when considering the group as a whole (Table 2). Many patients did, however, exhibit differences of more than 2 N/mm between segments. The mean difference between patients’ maximum and minimum recorded PAS was 5.00 N/mm (SD, 3.97 N/mm). The fifth lumbar had the highest stiffness in 25% of cases, with the other segments each comprising between 11% and 17% (Table 3). Only 17% of patients exhibited less than 2 N/mm difference across the lumbar spine.
Table 3.
The frequency with which stiffness occurred at each lumbar segment as measured with PAS
| Lumbar segment | % of Patients (n = 173) |
|---|---|
| <2 N/mm difference | 16.8 |
| L1 | 15.6 |
| L2 | 13.9 |
| L3 | 17.3 |
| L4 | 11.6 |
| L5 | 24.9 |
The lumbar segment with the highest PAS measure was ranked as stiffest when there was more than 2 N/mm difference between the patient’s most and least stiff segment.
Palpatory stiffness and tenderness measures were collected on all 192 patients in the study. Most patients exhibited stiffness and tenderness at multiple segments (Table 4). Although only 11 patients (5.7%) had no segment that the clinician judged as stiff, an almost equal number exhibited stiffness at all 5 lumbar segments. The most frequent finding was stiffness at 2 segments (69, 35.9%). Tenderness to palpation was also found in most patients, except many more had tenderness at several (or all) segments.
Table 4.
The number and frequencies of segments that were found either stiff or tender on palpation
| No. of segments | Palpably stiff, n (%) | Tender on palpation, n (%) |
|---|---|---|
| 0 | 11 (5.7) | 5 (2.6) |
| 1 | 45 (23.4) | 7 (3.6) |
| 2 | 69 (35.9) | 18 (9.4) |
| 3 | 44 (22.9) | 16 (8.3) |
| 4 | 13 (6.8) | 23 (12.0) |
| 5 | 10 (5.2) | 123 (64.1) |
| Total | 192 | 192 |
Because clinicians only used a 2-level scale to assess spinal joint stiffness (yes or no), it is not possible to derive a correlation to the PAS measure. Instead, we attempted to see if the clinicians were identifying as stiff the same segments as the PAS system measured. First, we examined the clinical data to find the particular segment that showed increased stiffness or tenderness by palpation. In those few cases where only one segment was noted on palpation, the choice was clear. An attempt was made to reduce the palpation findings to only one segment in those cases where positive findings were found in only 2 or 3 segments and when those segments were contiguous (ie, L3 and L4 or L2–L4 were all found tender). When 2 contiguous segments were found, the most distal was selected as the stiffest segment, and when 3 segments were found, the middle of the 3 was designated. With this method, a single segment was designated as palpably most stiff in 112 patients and as palpably most tender in 166 patients.
The amount of agreement between the PAS and palpation findings was found by subtracting the segment number found by each method for each patient. Hence, we calculated the distance (in segments) between the 3 determinations (Table 5). For example, if a patient was found to be most tender at L1, most stiff by palpation at L5, and had greatest PAS at L4, the PAS vs palpable stiffness would be −1 (4–5), the PAS vs palpable tenderness would be 3 (4 –1), and the palpable tenderness vs Palpable Stiffness would be 4 (5 –1). There was very little agreement between the segmental determinations by PAS and those by palpation; however, both palpation methods were within 2 segments of each other in 80% of the 99 cases where both methods found a segment.
Table 5.
Agreement on designated segment by PAS instrument measurement and manual palpation for stiffness and tenderness
| Distance (no. of segments away) | PAS vs Palpatory stiffness
|
PAS vs Palpatory tenderness
|
Palpatory tenderness vs palpatory stiffness
|
|||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| −4.00 | 8 | 9.8 | 7 | 5.8 | 0 | 0 |
| −3.00 | 19 | 23.2 | 17 | 14.0 | 0 | 0 |
| −2.00 | 16 | 19.5 | 22 | 18.2 | 0 | 0 |
| −1.00 | 10 | 12.2 | 15 | 12.4 | 13 | 13.1 |
| .00 | 18 | 22.0 | 26 | 21.5 | 50 | 50.5 |
| 1.00 | 10 | 12.2 | 16 | 13.2 | 19 | 19.2 |
| 2.00 | 1 | 1.2 | 9 | 7.4 | 8 | 8.1 |
| 3.00 | 0 | 0 | 8 | 6.6 | 6 | 6.1 |
| 4.00 | 0 | 0 | 1 | .8 | 3 | 3.0 |
| Total | 82 | 100.0 | 121 | 100.0 | 99 | 100.0 |
Cases were included only if both methods being compared determined a positive finding at least one lumbar segment.
Significant correlations were seen for demographic factors: age, sex, weight, and BMI. However, none of the following clinical factors correlated with spinal stiffness: chronicity of complaint, Roland-Morris score, VAS for pain, or lumbosacral (LS) ROM (Table 6). The weight and BMI correlation was most significant at the lowest lumbar segments.
Table 6.
Pearson’s correlation coefficient and level of significance for selected demographic and clinical factors vs PAS value by segment
| Correlation coefficient (P)
|
|||||
|---|---|---|---|---|---|
| L1 | L2 | L3 | L4 | L5 | |
| Age | 0.23 (.002) | 0.21 (.007) | 0.13 (.080) | 0.18 (.02) | 0.06 (.439) |
| Weight (lb) | −0.04 (.646) | −0.07 (.341) | −0.22 (.004) | −0.24 (.002) | −0.26 (.001) |
| BMI | −0.13 (.087) | −0.17 (.028) | −0.33 (<.001) | −0.33 (<.001) | −0.40 (<.001) |
| Chronicity * | 0.05 (.529) | −0.04 (.613) | 0.12 (.108) | 0.03 (.682) | −0.08 (.298) |
| VAS | 0.04 (.592) | −0.07 (.344) | 0.01 (.913) | 0.01 (.977) | 0.07 (.409) |
| Roland-Morris score | 0.09 (.225) | 0.03 (.667) | 0.06 (.470) | 0.08 (.333) | 0.03 (.733) |
| LS active flexion | 0.08 (.280) | 0.05 (.517) | 0.02 (.763) | 0.12 (.109) | 0.15 (.059) |
| LS active extension | −0.11 (.159) | −0.01 (.919) | −0.10 (.216) | 0.01 (.849) | 0.04 (.649) |
Spearman ρ was used because of skewness of chronicity variable.
Discussion
The average PAS stiffness measured in our patient population was 3 to 5 N/mm lower than that measured in previous studies that used a fully mechanized testing apparatus.33,39 A number of factors could have accounted for this difference, including patient factors and testing methods. Our system does not use a motor to drive the indenter, and so, despite examiner training, there was variability in the rate of loading and inconsistency between loading and unloading rates. The rate of loading in our study, 0.65 cycles/s, was close to the speed (0.50 Hz) used by several investigators in Australia.8,10,38 Their testing showed that rates between 0.5 and 1 Hz produced very similar PAS results.23,24 Also, our method of data reduction, using a linear region of the force-displacement curve near the peak load, was styled after that used by Latimer and Lee.7
There was, however, a significant difference in the size of the indenting tip used in our study. Our indenter tip is a contoured round shaft with cross-sectional area 314 mm,2 whereas the device most commonly reported had a rectangular tip 720 mm2 in area. Squires et al24 found that a smaller tip (300 mm2) tended to produce larger PAS measures. Some other factor must have been responsible for our generally lower PAS measures.
Our method of PAS measurement uses the force and displacement data of the indenting rod to calculate a stiffness value. Unfortunately, we cannot distinguish the displacement that results from spinal displacement from that due to compression of soft tissue overlying the spinal contact point. The effect of overlying soft tissue is evident in our data as a correlation between BMI and PAS. Patients with a greater BMI are thicker in constitution, which is quite likely a sign of thicker tissues overlying the spine. Compression of tissues between the table and the patient can also contribute to displacement. Increased BMI may have resulted in the lower PAS values seen in our patient population. Lee et al18 reported a lower mean BMI value in their study (23.8 vs 29.8 in our sample) but did not suggest a relationship between BMI and PAS. They did, however, note a decrease in PAS at L4 with increasing skinfold thickness over the ilium, a more direct indicator of body fat thickness than BMI.
It is interesting that weight and BMI correlated most strongly with PAS in the lower lumbar segments. Weight is a component of the calculation of BMI, so there should be some correspondence. The greater effect of BMI on lower lumbar PAS scores, though, is probably related to the distribution of body fat. The lower lumbar segments most often have a thicker covering of body fat. It was commonly noted during palpation of spinal landmarks in our study that the L4 and L5 spinous processes were difficult to palpate through the overlying tissues.
Our findings underscore the importance of being able to discriminate the sources of tissue displacement during PAS testing. The ultrasonic indentation system developed by Kawchuk et al5,35 has the advantage of being able to measure tissue thickness changes under the indenting head.
The correlation between sex and PAS might be explained by considering BMI. However, BMI was not different between the males and females on our study sample. The correlation between age and PAS was slight but statistically significant, most notably in the upper lumbar spine. It would be interesting to compare the findings in this study with an elderly population to determine if the PAS-age relationship holds true over a wide age range as well.
Active ranges of motion in LS flexion and extension were not related to spinal stiffness. We thought they might be because the action of the PAS test itself induces mild extension at the posterior spinal joints. In a cadaver experiment, Sran et al36 found that PAS was related to ROM. ROM in the cadaver might be more related to passive ROM in the living human, which we did not measure.
The lack of correlation between indicators of back pain severity (RMQ and VAS) is not surprising in light of the results seen in previous studies. Other authors have found small changes (1.2 N/mm) in patients with LBP on repeat testing when their pain was resolved,33 but they could not detect any difference in spinal stiffness between patients with LBP and pain-free control subjects.9 If, as Lee et al18 suggested and as we have seen in our data, PAS measures depend on patient factors that might not be directly related to spinal stiffness, we could expect significant variance between individuals that might mask differences due to the presence of LBP.
We saw very little difference on the average between PAS measures at different segments of the lumbar spine. This result is different from that of Viner et al10 who found greater stiffness in the lower lumbar spine. That study was done with healthy pain-free participants rather than patients with LBP as in our study. On the other hand, we saw larger intersegmental differences within patients, in contrast to Viner et al.10 In our study, the average range between patients’ least and most stiff segments was 5.00 N/mm. Viner et al suggest that any difference between adjacent segments needs to exceed 3.6 N/mm to be greater than that seen in 90% of normal cases. If our system is able to detect intersegmental stiffness differences in patients, this may be a useful tool to determine which segment might be most appropriate for the application of manipulative thrusts. Much more work needs to be done; perhaps looking at the changes that occur with spinal manipulation in a symptomatic patient population will be enlightening.
In our data, we saw very little correspondence between palpation and PAS as indications of segmental stiffness. The palpatory indicator of the stiffest segment and the PAS indicator agreed less than 40% of the time. No attempt was made to calculate a κ value because our experiment was not designed to test intermeasure agreement. The main problem with this design as a reliability study is that the clinical palpation tests were not intended to identify a single segment as most stiff or most tender in all patients. If we had seen good agreement, it would suggest the need, perhaps, for a more detailed comparison of palpatory and objective measures of spinal stiffness. From our results, and that of others, there does not seem to be any indication that these measures would agree. A recent study used MRI to measure joint movement during PA spinal loading and compared this measure of spinal stiffness to a clinical test of the patient’s most painful segment.41 The authors found no association between the degree of intersegmental motion and the level of pain experienced by patients. As Maher and Adams42 pointed out, spinal stiffness testing as performed by an experienced palpator is multidimensional, with intersegmental stiffness being perhaps only one dimension evaluated by palpators. Other cues about spinal function are available to the observant human palpator, such as soft tissue consistency, muscular contractions, or viscous properties that our instrument is not intended to detect.
Limitations
Manual palpation was used to locate and mark the spinous processes before PAS testing. The patients were marked in the same prone position that was used for testing so we can be reasonably sure that a spinous process was contacted for the test, but there may be some uncertainty as to the precise segment being tested. None of our palpation methods, whether for landmark location or stiffness or tenderness rating, were tested for reliability before the study. Hence, the lack of agreement between clinical measures and PAS might have been due to inaccuracies in the clinical measures. This is very much the state of the art of palpatory methods for spinal joint function1,2 and underscores the importance of developing more objective methods of spinal assessment.
Conclusion
The PAS system of computer-monitored equipment with human operation performed well in this clinical study of LBP. Spinal stiffness was found to be different between males and females, and age and BMI were related to PAS. We found no significant relationship between the severity or chronicity of the LBP complaint and spinal stiffness. There was little agreement between the stiff or tender segments identified by the clinicians using palpation and the segment that measured most stiff using the PAS device. Future work could be done to measure the sensitivity of PAS measurements in a clinical population of patients with LBP and test whether interventions aimed particularly at changing spine biomechanics affect PAS measurements.
Practical Applications
A system for measuring posterior-to-anterior spinal stiffness performed well in a large clinical study.
Spinal stiffness was found to depend on patients’ sex, age, and BMI.
We found no significant relationship between the severity or chronicity of the LBP complaint and spinal stiffness.
Acknowledgments
The project described was supported by the grant number U19 AT002006 from the National Center for Complementary and Alternative Medicine (NCCAM). The investigation was conducted in a facility constructed with support from the Research Facilities Improvement Program grant number C06 RR15433-01 from the National Center for Research Resources, National Institute of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCCAM or the National Institutes of Health, Bethesda, MD.
References
- 1.Stochkendahl MJ, Christensen HW, Hartvigsen J, et al. Manual examination of the spine: a systematic critical literature review of reproducibility. J Manipulative Physiol Ther. 2006;29:475–85. 485. doi: 10.1016/j.jmpt.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 2.Seffinger MA, Najm WI, Mishra SI, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29:E413–25. doi: 10.1097/01.brs.0000141178.98157.8e. [DOI] [PubMed] [Google Scholar]
- 3.Brodeur RR, DelRe L. Stiffness of the thoracolumbar spine for subjects with and without low back pain. J Neuromusculoskel Syst. 1999;7:127–33. [Google Scholar]
- 4.Kawchuk G, Herzog W. A new technique of tissue stiffness (compliance) assessment: its reliability, accuracy and comparison with an existing method. J Manipulative Physiol Ther. 1996;19:13–8. [PubMed] [Google Scholar]
- 5.Kawchuk GN, Fauvel OR, Dmowski J. Ultrasonic indentation: a procedure for the noninvasive quantification of force-displacement properties of the lumbar spine. J Manipulative Physiol Ther. 2001;24:149–56. [PubMed] [Google Scholar]
- 6.Latimer J, Goodsell MM, Lee M, Maher CG, Wilkinson BN, Moran CC. Evaluation of a new device for measuring responses to posteroanterior forces in a patient population, Part 1: Reliability testing. Phys Ther. 1996;76:158–65. doi: 10.1093/ptj/76.2.158. [DOI] [PubMed] [Google Scholar]
- 7.Latimer J, Lee M, Goodsell M, Maher C, Wilkinson B, Adams R. Instrumented measurement of spinal stiffness. Man Ther. 1996;1:204–9. doi: 10.1054/math.1996.0270. [DOI] [PubMed] [Google Scholar]
- 8.Lee M, Liversidge K. Posteroanterior stiffness at three locations in the lumbar spine. J Manipulative Physiol Ther. 1994;17:511–6. [PubMed] [Google Scholar]
- 9.Shirley D, Lee M. A preliminary investigation of the relationship between lumbar postero-anterior mobility and low back pain. J Man Manip Ther. 1993;1:22–5. [Google Scholar]
- 10.Viner A, Lee M, Adams R. Posteroanterior stiffness in the lumbosacral spine. The correlation between adjacent vertebral levels. Spine. 1997;22:2724–9. doi: 10.1097/00007632-199712010-00004. [DOI] [PubMed] [Google Scholar]
- 11.Owens EF. An objective measurement of muscle tone. Chiropr Res J. 1988;1:34–46. [Google Scholar]
- 12.Edmondston SJ, Allison GT, Gregg CD, Purden SM, Svansson GR, Watson AE. Effect of position on the posteroanterior stiffness of the lumbar spine. Man Ther. 1998;3:21–6. doi: 10.1054/math.1998.0312. [DOI] [PubMed] [Google Scholar]
- 13.Latimer J, Holland M, Lee M, Adams R. Plinth padding and measures of posteroanterior lumbar stiffness. J Manipulative Physiol Ther. 1997;20:315–9. [PubMed] [Google Scholar]
- 14.Kawchuk GN, Fauvel OR. Sources of variation in spinal indentation testing: indentation site relocation, intraabdominal pressure, subject movement, muscular response, and stiffness estimation. J Manipulative Physiol Ther. 2001;24:84–91. doi: 10.1067/mmt.2001.112566. [DOI] [PubMed] [Google Scholar]
- 15.Shirley D, Hodges PW, Eriksson AE, Gandevia SC. Spinal stiffness changes throughout the respiratory cycle. J Appl Physiol. 2003;95:1467–75. doi: 10.1152/japplphysiol.00939.2002. [DOI] [PubMed] [Google Scholar]
- 16.Lee M, Esler M-A, Mildren J. Effect of extensor muscle activation on the response to lumbar posteroanterior forces. Clin Biomech (Bristol, Avon) 1993;8:115–9. doi: 10.1016/0268-0033(93)90051-I. [DOI] [PubMed] [Google Scholar]
- 17.Shirley D, Lee M, Ellis E. The relationship between submaximal activity of the lumbar extensor muscles and lumbar posteroanterior stiffness. Phys Ther. 1999;79:278–85. [PubMed] [Google Scholar]
- 18.Lee M, Steven GP, Crosbie J, Higgs RJ. Variations in posteroanterior stiffness in the thoracolumbar spine: preliminary observations and proposed mechanisms. Phys Ther. 1998;78:1277–87. doi: 10.1093/ptj/78.12.1277. [DOI] [PubMed] [Google Scholar]
- 19.Allison G. Effect of direction of applied mobilization force on the posteroanterior response in the lumbar spine. J Manipulative Physiol Ther. 2001;24:487–8. [PubMed] [Google Scholar]
- 20.Allison GT, Edmondston SJ, Roe CP, Reid SE, Toy DA, Lundgren HE. Influence of load orientation on the posteroanterior stiffness of the lumbar spine. J Manipulative Physiol Ther. 1998;21:534–8. [PubMed] [Google Scholar]
- 21.Caling B, Lee M. Effect of direction of applied mobilization force on the posteroanterior response in the lumbar spine. J Manipulative Physiol Ther. 2001;24:71–8. doi: 10.1067/mmt.2001.112568. [DOI] [PubMed] [Google Scholar]
- 22.Viner A, Lee M. Direction of manual force applied during assessment of stiffness in the lumbosacral spine. J Manipulative Physiol Ther. 1995;18:441–7. [PubMed] [Google Scholar]
- 23.Lee M, Svensson NL. Effect of loading frequency on response of the spine to lumbar posteroanterior forces. J Manipulative Physiol Ther. 1993;16:439–46. [PubMed] [Google Scholar]
- 24.Squires MC, Latimer J, Adams RD, Maher CG. Indenter head area and testing frequency effects on posteroanterior lumbar stiffness and subject’s rated comfort. Man Ther. 2001;6:40–7. doi: 10.1054/math.2000.0379. [DOI] [PubMed] [Google Scholar]
- 25.Latimer J, Lee M, Adams RD. The effects of high and low loading forces on measured values of lumbar stiffness. J Manipulative Physiol Ther. 1998;21:157–63. [PubMed] [Google Scholar]
- 26.Lee M, Kelly DW, Steven GP. A model of spine, ribcage and pelvic responses to a specific lumbar manipulative force in relaxed subjects. J Biomech. 1995;28:1403–8. doi: 10.1016/0021-9290(95)00001-x. [DOI] [PubMed] [Google Scholar]
- 27.Chansirinukor W, Lee M, Latimer J. Contribution of ribcage movement to thoracolumbar posteroanterior stiffness. J Manipulative Physiol Ther. 2003;26:176–83. doi: 10.1016/S0161-4754(02)54131-2. [DOI] [PubMed] [Google Scholar]
- 28.Chansirinukor W, Lee M, Latimer J. Contribution of pelvic rotation to lumbar posteroanterior movement. Man Ther. 2001;6:242–9. doi: 10.1054/math.2001.0420. [DOI] [PubMed] [Google Scholar]
- 29.Lee M, Lau H, Lau T. Sagittal plane rotation of the pelvis during lumbar posteroanterior loading. J Manipulative Physiol Ther. 1994;17:149–55. [PubMed] [Google Scholar]
- 30.Lee R, Evans J. An in vivo study of the intervertebral movements produced by posteroanterior mobilization. Clin Biomech (Bristol, Avon) 1997;12:400–8. doi: 10.1016/s0268-0033(97)00019-3. [DOI] [PubMed] [Google Scholar]
- 31.Kulig K, Landel R, Powers CM. Assessment of lumbar spine kinematics using dynamic MRI: a proposed mechanism of sagittal plane motion induced by manual posterior-to-anterior mobilization. J Orthop Sports Phys Ther. 2004;34:57–64. doi: 10.2519/jospt.2004.34.2.57. [DOI] [PubMed] [Google Scholar]
- 32.Powers CM, Kulig K, Harrison J, Bergman G. Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clin Biomech (Bristol, Avon) 2003;18:80–3. doi: 10.1016/s0268-0033(02)00174-2. [DOI] [PubMed] [Google Scholar]
- 33.Latimer J, Lee M, Adams R, Moran CM. An investigation of the relationship between low back pain and lumbar posteroanterior stiffness. J Manipulative Physiol Ther. 1996;19:587–91. [PubMed] [Google Scholar]
- 34.Kawchuk GN, Kaigle AM, Holm SH, Rod FO, Ekstrom L, Hansson T. The diagnostic performance of vertebral displacement measurements derived from ultrasonic indentation in an in vivo model of degenerative disc disease. Spine. 2001;26:1348–55. doi: 10.1097/00007632-200106150-00018. [DOI] [PubMed] [Google Scholar]
- 35.Kawchuk GN, Fauvel OR, Dmowski J. Ultrasonic quantification of osseous displacements resulting from skin surface indentation loading of bovine para-spinal tissue. Clin Biomech (Bristol, Avon) 2000;15:228–33. doi: 10.1016/s0268-0033(99)00066-2. [DOI] [PubMed] [Google Scholar]
- 36.Sran MM, Khan KM, Zhu Q, Oxland TR. Posteroanterior stiffness predicts sagittal plane midthoracic range of motion and three-dimensional flexibility in cadaveric spine segments. Clin Biomech (Bristol, Avon) 2005;20:806–12. doi: 10.1016/j.clinbiomech.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 37.Allison G, Edmonston S, Kiviniemi K, Lanigan H, Simonsen AV, Walcher S. Influence of standardized mobilization on the posteroanterior stiffness of the lumbar spine in asymptomatic subjects. Physiother Res Int. 2001;6:145–56. doi: 10.1002/pri.223. [DOI] [PubMed] [Google Scholar]
- 38.Lee M, Latimer J, Maher C. Manipulation: investigation of a proposed mechanism. Clin Biomech (Bristol, Avon) 1993;8:302–6. doi: 10.1016/0268-0033(93)90004-2. [DOI] [PubMed] [Google Scholar]
- 39.Goodsell M, Lee M, Latimer J. Short-term effects of lumbar posteroanterior mobilization in individuals with low-back pain. J Manipulative Physiol Ther. 2000;23:332–42. [PubMed] [Google Scholar]
- 40.Owens EF, DeVocht J, Gudavalli MR, Wilder DG, Meeker WC. The reliability of a posterior-to-anterior spinal stiffness measure in a population of patients with low back pain. J Manipulative Physiol Ther. 2007;30:116–23. doi: 10.1016/j.jmpt.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 41.Beneck GJ, Kulig K, Landel RF, Powers CM. The relationship between lumbar segmental motion and pain response produced by a posterior-to-anterior force in persons with nonspecific low back pain. J Orthop Sports Phys Ther. 2005;35:203–9. doi: 10.2519/jospt.2005.35.4.203. [DOI] [PubMed] [Google Scholar]
- 42.Maher C, Adams R. Is the clinical concept of spinal stiffness multidimensional? Phys Ther. 1995;75:854–60. doi: 10.1093/ptj/75.10.854. [DOI] [PubMed] [Google Scholar]