Abstract
A young women developed unilateral facial neuropathy 2 weeks after a motor vehicle collision involving fractures of the skull and mandible. MRI showed contrast enhancement of the facial nerve. We review the literature describing facial neuropathy after trauma and facial nerve enhancement patterns with different causes of facial neuropathy.
Keywords: Bell's palsy, enhancement, facial nerve, idiopathic, MRI, paralysis, trauma
Idiopathic facial neuropathy, eponymously named Bell's palsy, was first described by Charles Bell in 1821, and is the most common syndrome of acute onset isolated unilateral facial weakness [1]. Bell's palsy accounts for 60–75% of cases of this syndrome [2], with an annual incidence of 20–25 cases per 100,000 [3]. The eponym Bell's palsy is specific to idiopathic cases, although the eponym is frequently erroneously used for facial neuropathy from known causes as well [3].
The highest incidence of Bell's palsy is seen in individuals between 15 and 45 years old [4], followed by persons above 70 years of age and then individuals below 10 years of age [5]. Although Bell's palsy affects men and women equally, there is a higher incidence seen in pregnant women [4]. Bell's palsy in pregnancy usually occurs in the third trimester and puerperium, possibly from the relatively immunosuppressed state causing susceptibility to viral infections during this period, or from changes to interstitial fluid or connective tissue [6]. There may be an increased risk of Bell's palsy for patients with diabetes or hypertension [7]. A higher incidence of Bell's palsy among diabetics may indicate that microangiopathic dysfunction predisposes to its development [8]. A study in Egypt concluded that Bell's palsy has higher incidence rates among females and people residing in rural areas [6].
Viral infections, autoimmune reaction and ischemia are all proposed causes of Bell's palsy with viral infection being the most likely cause [9]. Infection with Borrelia burgdorferi in Lyme disease and zoster virus in Ramsay Hunt syndrome can cause facial neuropathy [10,11]. Bell's palsy is believed to be linked to herpes simplex virus type-1 infection reactivation in the geniculate ganglion. Once reactivated the virus may infect ganglion and Schwann cells causing demyelinization and inflammation of the facial nerve [9]. Triggers associated with Bell's palsy are known to be associated with herpes simplex virus reactivation, including recent upper respiratory tract infection, fever, dental extraction, menstruation or exposure to cold [9].
The history and physical examination is generally sufficient to diagnose Bell's palsy, and imaging is usually unnecessary. However, it can be helpful in ruling out other pathological causes of facial neuropathy presenting with atypical symptoms including slow recovery and recurrence [12]. Enhancement of the facial nerve on MRI may be seen in normal subjects, commonly involving the tympanic or vertical segments. This is likely due to the extensive venous plexus surrounding the nerve as it passes through the facial canal [12]. With Bell's palsy a common MRI finding is enhancement of the labyrinthine portion of the facial nerve, where the facial canal is narrowest. The poor vascularity of this segment may pre-dispose it to ischemia and venous congestion, which may cause the high intensity enhancement pattern seen on MRI in Bell's palsy [13]. This finding can allow it to be distinguished from pathologies such as middle or external ear infections, which usually show no characteristic facial nerve enhancement on MRI because there is no breakdown of the blood–nerve barrier hence not allowing contrast material to diffuse into the endoneural space [12,13].
The majority of the patients with Bell's palsy (70%) have a complete spontaneous recovery within 6 months [14]. The remaining cases have either mild impairments, or around 4% have severe sequelae with facial distortion and/or synkinesis [14,15]. It is recommended that patients with Bell's palsy should receive corticosteroid treatment as part of their medical treatment [16,17]. A recent study in Egypt showed that Bell's palsy patients who received prednisolone had a better outcome than those who were not treated with prednisolone, regardless of severity of palsy at presentation [16]. Berg et al. studied 829 patients with Bell's palsy and concluded that prednisolone reduces mild and moderate sequelae significantly in Bell's palsy [15].
One study divided the many etiologies of facial paralysis into five groups: idiopathic, traumatic, infectious, neoplastic and neurologic [18]. Traumatic causes include temporal fractures, which are seen most commonly with motor vehicle collisions (MVCs), assault and falls leading to cerebral injuries. Traffic accidents causing facial palsy usually manifests immediately after occurrence of the injury [19]. Concussion and other life threatening injuries may cause delayed recognition of facial weakness, however, so that the time course of the facial nerve weakness or paralysis manifestation is also difficult to predict [20].
We report our experience in managing a patient presenting with delayed facial neuropathy after trauma and imaging enhancement of the facial nerve on MRI.
Case presentation
A 25-year-old woman presented with progressively worsening left facial weakness over 2 days. Two weeks prior, she was in a MVC and suffered fractures of the left temporal bone and left mandibular condyle. She had noted prominent swelling of the left preauricular area since the accident, but no facial weakness. Two days prior to presentation she noted inability to fully close her left eye when she was squinting against the sun, and asymmetry of her smile in the mirror. Over the day she developed dizziness and nausea as well; she could not further characterize the dizziness, but denied lightheadedness, vertigo or disequilibrium. She had a persistent left-sided headache since the MVC which was worse when she sat up. This headache had been improving gradually until the last few days. She also endorsed intermittent confusion and slow speech. She also complained of a persistent ‘smudge’ in her left eye that floated around but never went away. She denied other symptoms.
Her past medical history was significant only for the MVC. Pertinent medications included oxycodone. She had no known allergies. She had no mental or physical limitations prior to the accident, but had not yet returned to farm work because of her injuries. She has moved frequently and worked many types of jobs. She had smoked a few cigarettes in the past but never regularly. She consumed two to three beers a few times a week. She initially denied recreational drug use but when asked about the positive drug screen she endorsed using marijuana, amphetamines and alprazolam on occasion. She had a positive family history for diabetes and late onset strokes. Review of systems also included diarrhea on presentation which then resolved.
The vital signs and nonneurological examination were normal except for a small, firm, tender mass over the left mandibular condyle. Pain limited jaw opening. The neurological examination was normal except for weakness of left: eyebrow elevation, eye closure and lower facial muscles with smile. There was mild weakness of all movements of the left arm that was inconsistent, and improved to full strength with coaching.
Routine serum and urine studies were normal except for a urine toxicology screen positive for amphetamines, benzodiazepines, opiates and tetrahydrocannabinoids. Her computed tomography head showed the healing left temporal bone fracture.
Radiology reading
MRI was significant for diffuse abnormal, asymmetric enhancement of the left intracanalicular (Figures 1 & 2), labyrinthine (Figure 3), geniculate (Figure 1), tympanic (Figure 1) and mastoid (Figure 4) segments of the left facial nerve. There is a moderate left mastoid effusion. Edema is noted involving the left mandibular condyle. There is also edema and enhancement in the soft tissues overlying the left mandibular condyle and preauricular region, compatible with recent trauma (Figures 1–4). The brain and cerebrovasculature was normal on all MRI sequences.
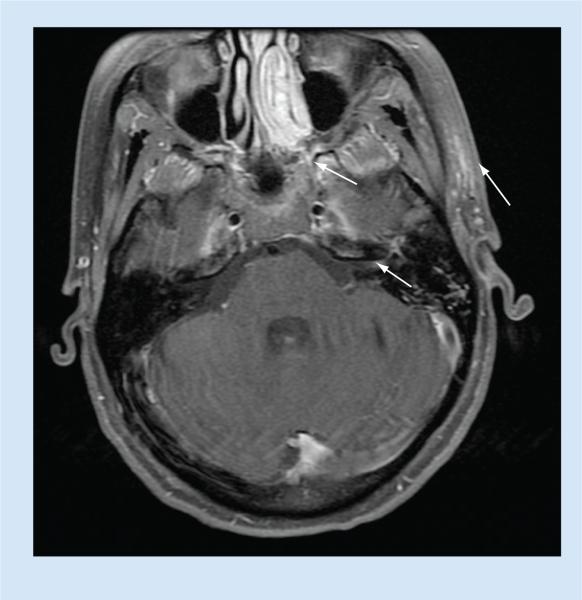
Figure 1. MRI brain T1-weighted image with contrast (section 1).
Arrows show enhancement of intracanalicular and geniculate segments of facial nerve. Note the soft tissue enhancement over the left preauricular region (arrow far right).
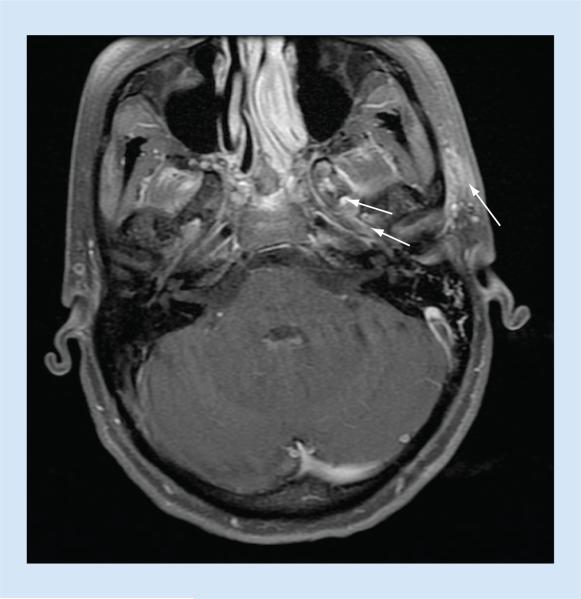
Figure 2. MRI brain T1-weighted image with contrast (section 2).
Arrows indicate enhancement of the intracanalicular segment of facial nerve. Note the soft tissue enhancement over the left preauricular region (arrow far right).
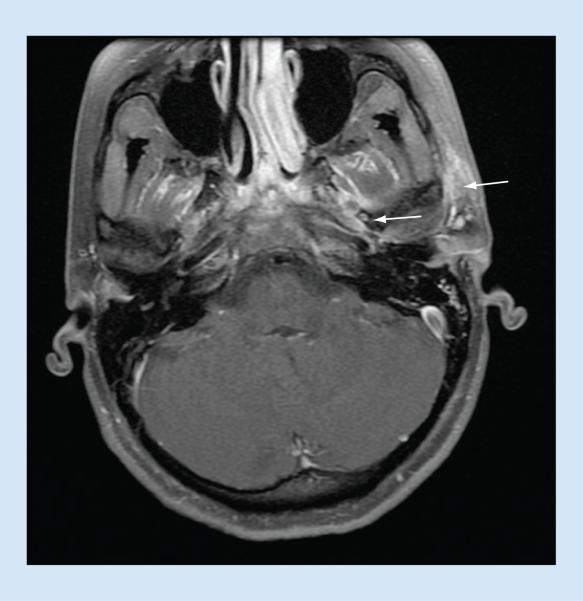
Figure 3. MRI brain T1-weighted image with contrast (section 3).
Arrows indicate enhancement of labyrinthine segment of facial nerve. Note the soft tissue enhancement over the left preauricular region (arrow far right).
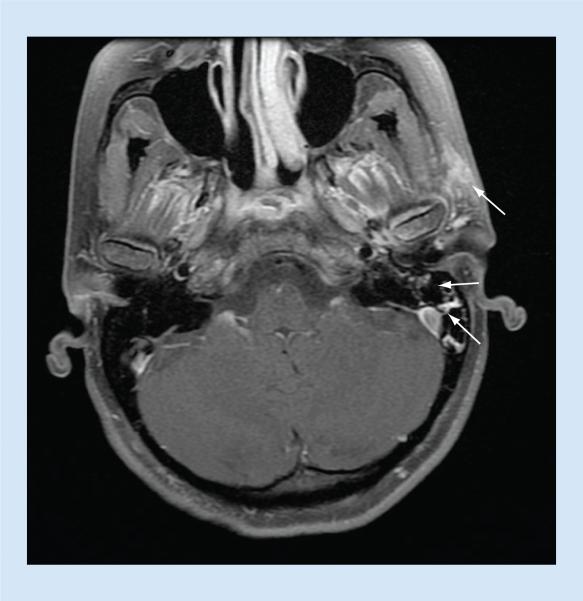
Figure 4. MRI brain T1-weighted image with contrast (section 4).
Arrows indicate enhancement of mastoid segment of facial nerve. Note the soft tissue enhancement over the left preauricular region (arrow far right).
The patient was diagnosed with Bell's palsy unrelated to the trauma, and treated with a short course of corticosteroids. She was seen in clinic 1 week later with subjective and objective improvement of both the facial weakness and the preauricular swelling.
Discussion
Charles Bell described the facial nerve as “the respiratory nerve of the face. It ministered to the motions of the face which are connected with respiration.” [1]. The facial nerve is vulnerable to injury due to its long course through the skull. There are many causes of facial neuropathy, the most common being trauma and idiopathic (Bell's palsy) [21].
We diagnosed the patient in this report as most likely having Bell's palsy, unrelated to the recent trauma, based on the 2-week delay, and treated her accordingly. We also wondered, however, if contraction of the preauricular hematoma could have compressed the nerve in a delayed fashion after the trauma, and/or if inflammation or other secondary processes from the trauma could have contributed to the facial neuropathy.
Motor vehicle accidents commonly cause facial neuropathy, which usually manifests immediately after occurrence of the injury [19]. With temporal bone fracture, 7–10% of patients have some kind of facial nerve impairment [22,23]. Anecdotally, delayed facial neuropathy may occur after lateral skull base surgery, and our case may share a similar unclear mechanism.
It is pertinent to note the swelling on her left jaw, which was the same side as the facial weakness. A case of a patient with a ganglion cyst of the temporomandibular joint presenting with facial nerve palsy has been reported [24]. Mumert et al. speculated the cyst exerted a mass effect on the geniculate ganglion, the intratemporal segment or the extratemporal segment of the facial nerve [24]. Synovial cysts and ganglion cysts both can appear after trauma [24], although we did not see that in this case.
Injury to the facial nerve may lead to edema and increased permeability of the surrounding vascular structures with increased extra-cellular fluid [25]. The blood–nerve barrier of cranial nerves consists of tight junctions in the endothelium and perineurium that form the sheath surrounding the nerves. Damage to this blood–nerve barrier secondary to insults such as ischemia, trauma, demyelination, neoplasms or autoimmune diseases may cause abnormal cranial nerve enhancement on MRI, but the specificity of this finding for diagnosing Bell's palsy has to be explored further [25].
Since the facial canal is long and narrow, swelling can put pressure on the nerve, resulting in damage either by direct mechanical injury or by reducing blood flow [25]. This may explain how soft tissue facial swellings could potentially cause facial nerve enhancement on MRI.
Cranial nerves may sometimes enhance to a degree in normal people, as well. Relative enhancement of the geniculate, tympanic and mastoid segments of the facial nerve is seen most likely due to accumulation of contrast material in the presence of venous plexuses [26,27]. The intracanalicular labyrinthine segment usually does not enhance. In Bell's palsy, along with the possibility of increased enhancement of these segments, the characteristic pattern includes enhancement of the intracanalicular labyrinthine segment [27].
Daniel et al. reviewed MRI findings in four patients with Bell's palsy between 4 and 8 weeks after acute onset of unilateral facial paralysis. The facial nerve on the symptomatic side enhanced at the apex of the internal auditory canal and within the facial nerve canal including the labyrinthine, geniculate ganglion, tym-panic and vertical portions. Three out of the four patients showed enhancement along the entire intratemporal facial nerve [25]. In our case all segments of the facial nerve enhanced on MRI, possibly due to inflammation or secondary to compression by swelling on the left jaw or due to Bell's palsy unrelated to the trauma.
Conclusion & future perspective
The cause of some of the symptoms she experienced including one-sided headache, nausea, dizziness and the smudge in her eye may have been attributed to a migraine episode or substance abuse. Her limited eye closure was consistent with facial neuropathy; this made it difficult to localize her left face and arm weakness together. Considering her left face weakness alone, it was consistent with facial nerve palsy, and the left arm weakness appeared to be psychogenic on examination. The radiological features of the lesion made for a perplexing diagnosis, especially since no cases of Bell's palsy presenting with soft tissue swelling in the face with MRI facial nerve enhancement have been described. This calls for the need of more investigation into facial nerve enhancement patterns on MRI in different etiologies of facial nerve paralysis especially with regards to Bell's palsy.
EXECUTIVE SUMMARY.
Background
Bell's palsy is idiopathic facial neuropathy. Increased risk for Bell's palsy is seen in pregnancy, diabetes, hypertension, viral infections and stress. A clinical diagnosis is usually sufficient. Enhancement pattern of facial nerve on MRI can give an insight into Bell's palsy diagnosis, characteristically involving enhancement of the labyrinthine segment of the facial nerve. It resolves spontaneously in most cases and in rare cases the patient experiences severe sequelae such as facial paralysis and synkinesis.
Case presentation
A 25-year-old female presented with progressively worsening left facial weakness over past 2 days. She noted an asymmetric smile and an inability to close her left eye. She had a history of a motor vehicle collision 2 weeks ago. On examination, firm, tender swelling was noted over the left mandibular condyle. Left-sided facial weakness was elicited with an otherwise normal neurological examination. Routine laboratory investigations were sent including urine toxicology screen, CT scan and MRI. MRI showed diffuse, abnormal enhancement of all segments of the facial nerve.
Discussion
The facial nerve is vulnerable to injury due to its long course and narrow route. We wanted to determine the cause of facial neuropathy in our patient considering her history of trauma and preauricular swelling and MRI finding. Injury to the facial nerve leads to edema, which may lead to abnormal enhancement on MRI. The preauricular mass could have compressed a segment of the facial nerve, leading to facial nerve damage and hence facial weakness. The facial nerve may enhance on MRI in normal cases, however, usually excluding the enhancement of the intracanalicular labyrinthine segment as seen in Bell's palsy.
Conclusion
The patient was diagnosed with Bell's palsy unrelated to trauma and improved with a short course of corticosteroids. The radiological findings along with the preauricular swelling on examination made for a perplexing diagnosis. More research into MRI enhancement patterns of facial nerve in facial neuropathy and Bell's palsy is called for.
Acknowledgments
MB Jensen received an NIH grant (1K08NS079622–01A1).
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Informed consent disclosure
The authors state that they have obtained verbal and written informed consent from the patient/patients for the inclusion of their medical and treatment history within this case report.
References
- 1.Pearce JMS. Historical note: Bell's or Friedreich's palsy. J. Neurol. Neurosurg. Psychiatry. 1999;67:732. doi: 10.1136/jnnp.67.6.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marques LM, Pimentel JC, Escada PA, et al. Late surgical decompression of facial nerve in Bell's palsy: a case report. J. Neurol. Surg. B. 2012;73:A516. [Google Scholar]
- 3.Karadima G, Kokotis P, Kalfakis N, et al. Bell's palsy and hereditary neuropathy with liability to pressure palsy (HNPP): is there a common genetic background. J. Clin. Neurosci. 2013;20(7):1042. doi: 10.1016/j.jocn.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Holland NJ, Weiner GM. Recent developments in Bell's palsy. BMJ. 2004;329(7465):553–537. doi: 10.1136/bmj.329.7465.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katusic SK, Beard CM, Wiederholt WC, et al. Incidence, clinical features, and prognosis in Bell's palsy, Rochester, Minnesota, 1968–1982. Ann. Neurol. 1986;20(5):622–627. doi: 10.1002/ana.410200511. [DOI] [PubMed] [Google Scholar]
- 6.Cohen Y, Lavie O, Granovsky-Grisaru S, et al. Bell palsy complicating pregnancy: a review. Obstet. Gynecol. Surv. 2000;55:184–188. doi: 10.1097/00006254-200003000-00027. [DOI] [PubMed] [Google Scholar]
- 7.El Tallawy HN, Farghaly WM, Abo-Elfetoh N, et al. Epidemiology of Bell's palsy in Al-Kharga district, New Valley, Egypt. Neurol. Res. 2013;35(7):663–670. [Google Scholar]
- 8.Savadi-Oskouei D, Abedi A, Sadeghi-Bazargani H. Independent role of hypertension in Bell's palsy: a case–control study. Eur. Neurol. 2008;60(5):253–257. doi: 10.1159/000151701. [DOI] [PubMed] [Google Scholar]
- 9.Akkuzu G, Ozgirgin ON, Akkuzu B, et al. Diabetes mellitus affect the prognosis of idiopathic peripheral facial paralysis? Mediterr. J. Otol. 2006;2:78–82. [Google Scholar]
- 10.Murakami S, Mizobuchi M, Nakashiro Y, et al. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Ann. Intern. Med. 1996;124(1 Pt 1):27–30. doi: 10.7326/0003-4819-124-1_part_1-199601010-00005. [DOI] [PubMed] [Google Scholar]
- 11.Smouha EE, Coyle PK, Skukri S. Facial nerve palsy in Lyme disease: evaluation of clinical diagnostic criteria. Am. J. Otol. 1997;18:257–261. [PubMed] [Google Scholar]
- 12.Aitkin RS, Brain RT. Facial palsy and infectious zoster virus. Lancet. 1993;1:19–22. [Google Scholar]
- 13.Al-Noury K, Lotfy A. Normal and pathological findings for the facial nerve on magnetic resonance imaging. Clin. Radiol. 2011;66(8):701–707. doi: 10.1016/j.crad.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Hong HS, Yi BH, Cha JG. Enhancement pattern of the normal facial nerve at 3.0 T temporal MRI. Br. J. Radiol. 2010;83(986):118–121. doi: 10.1259/bjr/70067143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berg T, Bylund N, Marsk E, et al. The effect of prednisolone on sequelae in Bell's palsy. Arch. Otolaryngol. Head Neck Surg. 2012;138(5):445–449. doi: 10.1001/archoto.2012.513. [DOI] [PubMed] [Google Scholar]
- 16.Abdelghany AM, Kamel SB. The effect of prednisolone and/or acyclovir in relation to severity of Bell's palsy at presentation. Egypt. J. Ear Nose Throat Allied Sci. 2013;14(3):155–159. [Google Scholar]
- 17.Gronseth GS, Paduga R, American Academy of Neurology Evidence-based guideline update: steroids and antivirals for Bell palsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2012;79(22):2209–2213. doi: 10.1212/WNL.0b013e318275978c. [DOI] [PubMed] [Google Scholar]
- 18.Bleicher JN, Hamiel S, Gengler JS, et al. A survey of facial paralysis: etiology and incidence. Ear Nose Throat J. 1996;75(6):355–358. [PubMed] [Google Scholar]
- 19.Popović D, Stanković M, Popović Z, et al. Traumatic facial palsy. FACTA UNIVERSITATIS Series: Med. Biol. 2003;10(3):145–147. [Google Scholar]
- 20.Nash JJ, Friedland DR, Boorsma KJ, et al. Management and outcomes of facial paralysis from intratemporal blunt trauma: a systematic review. Laryngoscope. 2010;120(4):S214. doi: 10.1002/lary.21681. [DOI] [PubMed] [Google Scholar]
- 21.Cha C, Hong CK, Park MS, et al. Comparison of facial nerve paralysis in adults and children. Yonsei Med. J. 2008;49(5):725–734. doi: 10.3349/ymj.2008.49.5.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chang CY, Cass SP. Management of facial nerve injury due to temporal bone trauma. Am. J. Otol. 1999;20:96–114. [PubMed] [Google Scholar]
- 23.Darrouzet V, Duclos JY, Liguoro D, et al. Management of facial paralysis resulting from temporal bone fractures: our experience in 115 cases. Otolaryngol. Head Neck Surg. 2001;125:77–84. doi: 10.1067/mhn.2001.116182. [DOI] [PubMed] [Google Scholar]
- 24.Mumert ML, Altay T, Shelton C, et al. Ganglion cyst of the temporomandibular joint with intracranial extension in a patient presenting with seventh cranial nerve palsy. J. Neurosurg. 2012;116(2):310–312. doi: 10.3171/2011.10.JNS111247. [DOI] [PubMed] [Google Scholar]
- 25.Daniels DL, Czervionke LF, Millen SJ, et al. MR imaging of facial nerve enhancement in Bell palsy or after temporal bone surgery. Radiology. 1989;171(3):807–809. doi: 10.1148/radiology.171.3.2717756. [DOI] [PubMed] [Google Scholar]
- 26.Gebarsk SS, Telian SA, Niparko JK. Enhancement along the normal facial nerve in the facial canal: MR imaging and anatomic correlation. Radiology. 1992;183:391–394. doi: 10.1148/radiology.183.2.1561339. [DOI] [PubMed] [Google Scholar]
- 27.Saremi F, Helmy M, Farzin S, et al. MRI of cranial nerve enhancement pictorial essay. Am. J. Roentgenol. 2005;185(6):1487–1497. doi: 10.2214/AJR.04.1518. [DOI] [PubMed] [Google Scholar]