Abstract
Objectives
A significant proportion of women who self-quit smoking during pregnancy subsequently relapse to smoking post-partum. This study examined free-text responses describing attributions of smoking relapse or maintained abstinence at 1, 8, and 12 months post-partum.
Method
This study reports secondary analyses from a randomized clinical trial (N = 504) for preventing post-partum smoking relapse. At each follow-up, one survey item asked the participant to describe why she resumed smoking or what helped her maintain abstinence. A thematic content analysis was conducted on responses from the 472 participants (94.0 % of the original sample) who returned at least 1 survey.
Results
Content analyses revealed several themes for participants’ reasons for relapse and abstinence. Stress was the most frequently cited reason for smoking relapse across all follow-ups. Health concerns for children and family was the most common reason provided for remaining abstinent. Chi-square analyses revealed differences in written responses related to income, age, and depressive symptoms.
Conclusions
Overall, these findings suggest that during the post-partum period, stress and familial health concerns are perceived contributors to smoking relapse and abstinence, respectively. These results confirmed key risk and protective factors that have been identified through other assessment modalities (e.g., quantitative surveys and focus groups). They also provide support for targeting these variables in the development, content, and delivery of future post-partum smoking relapse-prevention interventions. The high response rate to these open-ended attribution questions suggests that future studies would benefit from including these and similar items, to allow for additional insight into participant perspectives.
Keywords: post-partum, smoking, relapse prevention, content analysis
Despite a recent decline in the prevalence of smoking during pregnancy, 12% of pregnant women continue to smoke while they are pregnant (1), It is estimated that between 35 and 56% of pregnant smokers make an attempt to quit smoking during their pregnancy (2–4); however, quitting during pregnancy does not assure long-term cessation in the post-partum period (5). In fact, studies have estimated that nearly half of those who quit smoking during pregnancy resume smoking within 6 months of giving birth (6), and up to 80% relapse by 1 year post-partum (7). Post-partum relapse is a significant public health concern due to the adverse health effects of smoking for both the woman and her infant. Exposure to secondhand smoke during childhood is associated with several negative health outcomes such as increased incidence of sudden infant death syndrome, respiratory infections, and reduced lung functioning (8).
As noted by Coleman-Cowger (9), development and evaluation of novel post-partum relapse-prevention interventions constitutes an important research area. The identification of risk and protective factors for this population are necessary for effective intervention development. Prior quantitative and qualitative research has identified several risk factors for smoking relapse among post-partum women. For example, using longitudinal methodological approaches, risk factors have included several psychosocial and demographic characteristics such as low socioeconomic status (10), lack of social support (11), lower education (12), and post-partum depressive symptoms (13). Results from focus groups and interviews are consistent with longitudinal studies and have revealed additional protective factors such as strong social networks (14) and partner support (15), maintaining smoke-free environments for the child’s health (16), and implementing effective coping strategies when craving a cigarette (17, 18).
Several strategies have been evaluated for their ability to prevent post-partum smoking relapse, but as a whole, these interventions have been largely ineffective (19, 20). Given the lack of efficacious interventions for this population, our research team developed a series of self-help booklets designed to prevent post-partum smoking relapse (21–23). The booklet series, entitled Forever Free for Baby & Me (FFBM), was created based on prior research and formative evaluation and was recently tested in a randomized clinical trial. Women who self-quit due to pregnancy were provided with either the FFBM booklets (distributed from study enrollment through 8 months post-partum) or smoking cessation material from the National Cancer Institute and the American Cancer Society (distributed at study enrollment). Smoking behavior was assessed at 1, 8, and 12 months postpartum. Briefly, the FFBM booklets produced lower rates of smoking relapse, particularly among lower income women, at 8 and 12 months post-partum (24).
At each time point when smoking behavior was assessed, participants also responded to open-ended questions asking for their attributions for their continued abstinence or their smoking relapse. The current study describes a content analysis of these open-ended free responses, thereby summarizing participants’ attributions for abstinence and relapse. In contrast to forced-choice self-report measures, analysis of free responses allows for additional understanding of participant perspectives, and it reflects perceived relevancy and importance of various contributors to maintained abstinence or smoking relapse. A secondary aim of the current study was to identify differences in reasons for smoking or abstinence in terms of income (25), age (12), and depression (26), which constitute key demographic and psychosocial risk factors for post-partum relapse to smoking. Results from these analyses provide additional qualitative evidence concerning relapse risk factors, complement the parent trial’s quantitative results, and inform continued development and refinement of post-partum smoking relapse prevention interventions.
Method
Participants
Potential participants were 504 pregnant women who had recently self-quit smoking because of their pregnancy, recruited via a range of methods (24). Participants had to be at least 18 years of age and between 4 and 8 months pregnant to be eligible for enrollment in the parent study (24). The parent study was approved by the Institutional Review Board at the University of South Florida, and all participants provided verbal informed consent before being enrolled in the trial. Additional inclusion criteria were as follows: able to speak and read English; smoked 10 or more cigarettes per day for at least 1 year before their pregnancy; had quit smoking either in anticipation of or during pregnancy; and had abstained from smoking for the week prior to enrollment. Analyses reported here are based on the 472 women who returned at least 1 of the 3 follow-up surveys. A full description of recruitment procedures can be found in a prior publication (24).
Clinical Trial Materials and Procedures
Intervention Booklets
After providing informed consent, the original 504 participants were randomized into one of 2 conditions: usual care (n=259) or FFBM (n=245). The usual care group received Clearing the Air, a self-help booklet for quitting smoking that was created by the National Cancer Institute, and Living Smoke-Free for You and Your Baby, a pamphlet designed by the American Cancer Society to motivate women to quit smoking during and after their pregnancy. The FFBM group received the Forever Free for Baby & Me series, which was adapted from empirically supported self-help materials (27, 28) and included 10 booklets that were mailed to participants at standardized intervals from study enrollment through 8 months post-partum. Detailed descriptions of the content of the usual care and the FFBM intervention materials can be found in the primary outcomes paper (24).
Assessments
Assessment packets were mailed to participants at baseline and 1, 8, and 12 months post-partum. Participants provided demographic information and reported their smoking history at baseline. Self-report surveys at all four time points included measures related to smoking status and other psychosocial variables. The primary psychosocial variable for the current analyses was depression, which was measured by the Center for Epidemiologic Studies Depression Scale (CES-D, 29).
The surveys administered at 1, 8, and 12 months post-partum included 2 open-ended items: “If you have returned to smoking, please tell us why you think it happened.” and “If you have not returned to smoking, please tell us what has helped you stay smoke free.” Participants received $20 for completing the baseline survey, and $25, $30, and $35 for completing follow-up surveys at 1, 8, and 12 months post-partum, respectively.
Data Analysis
A qualitative content analysis was conducted on the 2 free response items for each of the 3 follow-ups. Verbatim handwritten responses were transcribed into electronic format by trained research assistants. Following transcription, each response was independently coded by two members of the research team (JC and LM). A coding manual was developed using an “intuitive” or “crystallizing” process whereby each response was carefully read and examined to identify themes (30). Written comments that were illegible were excluded, and comments that did not appropriately fit into any of the pre-determined themes were categorized as miscellaneous. Categories and themes were continually refined until an initial inter-rater agreement of 89.9% was reached across all open-ended responses at all time points (90.6% for abstinent responses, 88.8% for abstinent responses). Discrepancies were resolved by developing consensus among the two raters along with a third rater (VS).
Frequencies were calculated for attribution themes for both relapse and abstinence at 1, 8, and 12 months post-partum. Chi-square analyses were used to assess differences in response patterns based on three variables of interest: annual household income (less than $30,000 vs. greater than $30,000, which represented a median split), age (18–24 years old vs. 25 years old and above, which represented a median split), and depressive symptoms (assessment-specific median split on 10-item version of CES-D, median of 11 at 1 month and 10 at 8 and 12 months).
Results
Response Rates and Themes
Characteristics of the 472 participants are presented in Table 1. The number of participants returning surveys at 1, 8, and 12 months was 442 (94%), 415 (88%), and 400 (85%), respectively. Of those returning a survey, the number of participants smoking/abstinent at 1, 8, and 12 months was 116/326, 154/261, and 156/244, respectively.
Table 1.
Demographic, Pregnancy, and Smoking Variables as Reported at Baseline.
| Total Sample (n = 472) | |
|---|---|
| Demographic Variables | |
| Race (%) | |
| White/Caucasian | 92.4 |
| Black/African American | 4.0 |
| Other | 3.6 |
| Hispanic ethnicity (%) | 5.9 |
| Age (18–50 years): M (SD) | 25.7 (5.6) |
| Education (%) | |
| Less than HS diploma | 8.7 |
| HS Diploma or GED | 36.0 |
| Some College or Tech. School | 44.7 |
| Bachelor’s Degree | 8.3 |
| Graduate School/Degree | 2.3 |
| Married or living together (%) | 69.7 |
| Household Income <= $30,000 (%) | 41.6 |
| Pregnancy Variables | |
| Number of pregnancies: M (SD) | 2.2 (1.5) |
| Plan to Breastfeed (%) | 78.0 |
| Had prior miscarriage(s) (%) | 27.3 |
| Mood Variable | |
| CES-D at baseline: M (SD) | 16.6 (10.4) |
| Smoking Variables | |
| Pre-cessation FTND score: M (SD) | 3.7 (2.6) |
| Number of cigarettes per day: M (SD) | 15.2 (6.6) |
Notes. (1) FTND: Fagerström Test for Nicotine Dependence
The themes extracted from the content analysis of the 1,136 open-ended responses are presented in Tables 2 and 3. The percentage of surveys with a written response was greater than 90% of all surveys returned and ranged from 92.3% for women smoking at 12 months to 87.6% for women abstinent at 12 months. A large proportion of participants provided written comments that included more than one theme. For those abstinent at 1, 8, and 12 months, the percent of respondents with more than one theme identified was 51.5, 47.1, and 48.8. For those smoking at 1, 8, and 12 months, the percent of respondents with more than one theme coded was 14.7, 26.6, and 21.2, respectively.
Table 2.
Coding categories and descriptions of attributions for continued smoking abstinence.
| Category | Key Participant Phrases | Example |
|---|---|---|
| Self-Efficacy | Having the will power to stay quit; using self-control; making a commitment to remain abstinent; having the resolve to not relapse. | “Self control and will power have been my 2 main steadfasts to remaining smoke free. It’s all about mind over matter.” |
| Personal/general health | Feeling healthy/feeling better; having the desire to be healthy; wanting to watch children grow up; wanting to live longer; breathing more clearly. | “Thinking that I had to stay healthy for my daughter, so I could be around when she has a child.” |
| Child/family health | Quitting for the health of the baby, children, or family; breastfeeding; planning another pregnancy; providing a clean environment for the newborn child. | “My devotion to my baby. I want to do the best possible things for her.” |
| Coping | Using gum/candy; keeping busy; giving up triggers for smoking; giving rewards for not smoking; finding new hobbies. | “Finding new hobbies that involve my hands, eating carrot or celery sticks, staying in a non smoking environment.” |
| Treatment/External Resources | Reading the Forever Free booklets; relying on prayer, church, and a relationship with God, talking to doctors, enrolling in the Stop Smoking for Diapers program, using nicotine replacement. | “The books you sent were very very helpful to me, and I use them often!” |
| Social | Having support from family, friends, and husband/romantic partner; serving as a role model; setting an example for the new baby. | “My kids! I do not want them seeing me smoke and think that it is ok. It is hard telling them it is wrong and when doing it, how do you explain that?” |
| Financial | Not having enough money to buy cigarettes; wanting to save money; enjoying having more money; wanting to spend money on things for the baby. | “I also feel that the 4 dollars a day could be spent on more important things like my children.” |
| Motivation | Not having a desire to smoke; disliking the smell of cigarettes; not having a desire to quit again; not having enough time to smoke; no longer enjoying smoking; feeling ready to stay quit. | “The thought of having to quit again is stronger then wanting to start again.” |
| Cravings | Not having an urge to smoke, not craving cigarettes, not feeling the want/need to smoke. | “Just do not have the urge anymore. Tried one cigarette, it hurt to smoke and turned off my urge to smoke.” |
| Miscellaneous | “Freezing local climate.” |
Table 3.
Coding categories and descriptions of attributions for smoking relapse.
| Category | Key Participant Phrases | Example |
|---|---|---|
| Stress | Feeling stresses, emotional, or tense; adjusting to life as a mother; using smoking to calm down or relax, using smoking to cope, feeling pressured/anxious | “Being a little more stressed being a new mother. Knowing that cigarettes relaxed me. It was a stress reliever.” |
| Social | Living with others who smoked; constantly being around other who smoked; planning to smoke during social occasions or when drinking. | “My husband smokes and he provides little motivation for me. He’s never really tried to help.” |
| Motivational Decline | Enjoying cigarettes; no longer feeling bad about smoking; not feeling ready to quit long-term; not having enough will power to stay abstinent; falling back into the habit of smoking. | “I do smoke on a daily basis, but not as much as I used to. I guess I see it as ‘breaktime’ away from two small children. It’s enjoyable.” |
| Cravings | Craving cigarettes, never losing the urge, not being able to resist cravings. | “It’s easier to smoke than fight the craving.” |
| Miscellaneous | “I do not know.” |
Attributions for Abstinence
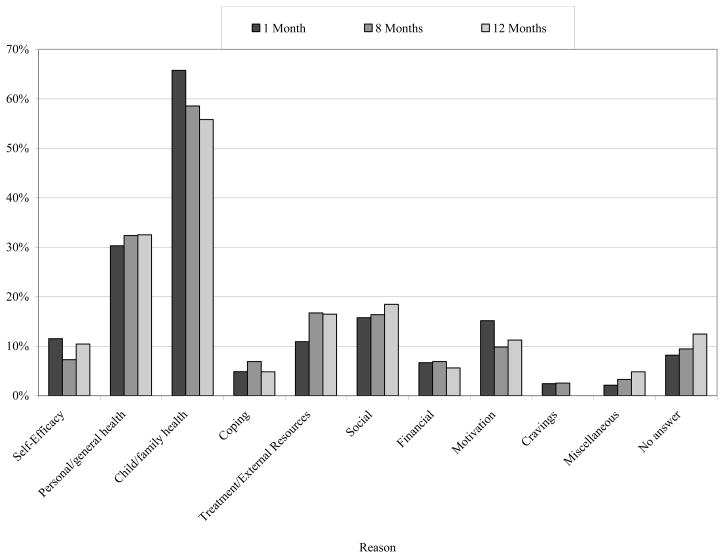
As shown in Figure 1, Child/family health was the most highly cited response among abstainers at all three time points. Responses reflected participants’ intentions to remain smoke-free for the good of their family, and often more specifically, for the good of their newborn child. Participants’ written comments reflected concern that smoking may negatively affect their child’s health, and their desire to establish a healthy environment during this critical developmental stage. Another frequent response within this theme was related to breastfeeding, as many participants reported that they did not want smoking to interfere with breastfeeding. Below are illustrative responses that were coded under the category of Child/family health:
“Knowing what could happen to the baby if I smoked kept me from smoking. It doesn’t matter what happens to me but I would feel bad if anything happened to her.”
“Being pregnant and breastfeeding have helped me to remain smoke free. I want my daughter to be as healthy as possible. I do not want to endanger her health by smoking.”
Figure 1.
Frequencies of responses in abstainers at 1 month, 8 months, and 12 months post-partum.
Personal/general health was the second most frequently cited response at all three time points. Written comments reflected participants’ desires to be healthy for themselves and their resolution to maintain the lifestyle changes they began while pregnant. Illustrative written responses are below:
“Thinking about my children and me dying of cancer. When they’re 30 and them having to bury me. It makes me sad to think about it.”
“Being able to be there for my son all of his life that I possibly can be without coughing, being out of breath, or dying of lung cancer or emphysema.”
Both Treatment/External Resources and Social themes were cited more frequently as the 12 month post-partum period progressed. Many of the responses within the Treatment/External Resources theme specifically mentioned that the Forever Free for Baby & Me booklets were supportive resources that helped them maintain abstinence. However, some participants also mentioned other quit aids (e.g., nicotine replacement therapy) and community resources (e.g., religion) as tools they used to stay smoke free. Sample responses for this theme follow:
“Reading your helpful books again has helped me like a good friend is talking to me. Sometimes you need that extra encouragement.”
“I give God all of the credit. This was my third time I quit smoking, after my first 2 pregnancies I started smoking again. After I got saved and started going to church he gave me the strength to stay smoke free.”
Responses in the Social theme reflected comments about living in a smoke-free household and having the support of romantic partners and family members to stay smoke free and serve as a positive role model for the newborn child.. Below are sample responses included under the Social theme:
“My kids! I do not want them seeing me smoke and think that it is ok. It is hard telling them it is wrong and when doing it, how do you explain that?”
“I have been able to stay mostly smoke free because my husband quit as well and I developed a strong support system.”
Motivation, however, was cited less frequently throughout the course of the first year post-partum. Responses within this theme reflected concepts such as less enjoyment from smoking, less time that could be spent smoking, and less desire go through the quit process again. Sample responses from this theme are below:
“The thought of having to quit again is stronger then wanting to start again.”
“Motivation mostly. After quitting was so hard, I don’t want to go through it again. It’s been since Jan and I could care less about smoking. I am happy to be free for my baby and me!!”
Attributions for Relapse
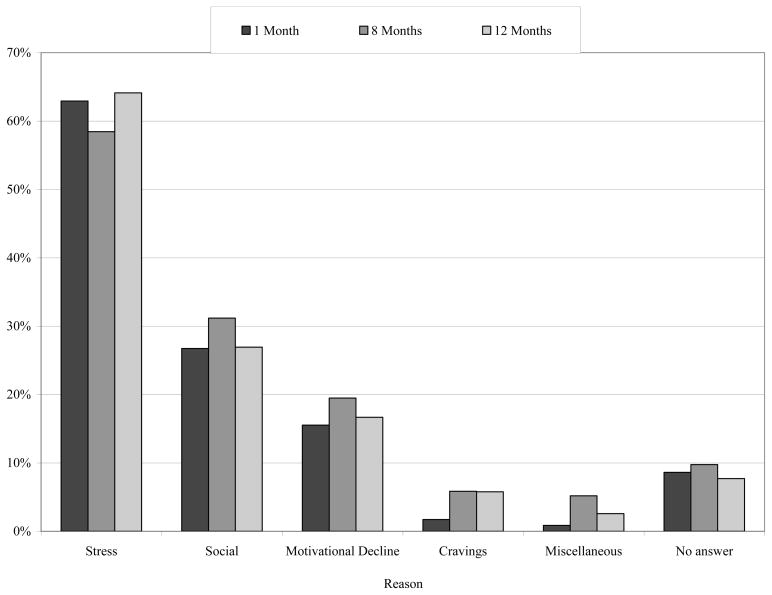
As seen in Figure 2, Stress/Coping was the most commonly cited reason for smoking at each time point, and participants cited several causes of their stress in their written responses. Participants reported using smoking as a coping strategy to help them manage problems related to post-partum depression, stress of new motherhood, and financial stress, among other difficulties. Illustrative comments categorized as Stress/Coping are below:
“Because it helps me feel better when I get depressed or worried. Since I’ve had my baby, his father hasn’t visited, supported, or helped with his son. It hurts me very bad and what I think or talk about it, I get to wanting a cigarette. I don’t want to smoke and hope that things in my life will change for the best very soon.”
“I have been going through a lot. My husband left me two months pregnant for a 16 year old girl. He smears it in my face. I stay stressed. My son asks about my husband all the time and that doesn’t help. So I would say I started smoking again because I stay depressed and stressed.”
Figure 2.
Frequencies of responses in smokers at 1 month, 8 months, and 12 months post-partum.
The second most frequently cited theme at all three time points was the Social theme. It was also noted that the frequency of participant’s responses related to this theme increased throughout the first year post-partum. Participants attributed their return to smoking as being caused by their partners, family, and friends smoking around them in the home or in social settings (e.g., in bars or restaurants). Below are sample responses that were coded under the Social theme:
“I feel I started smoking again because my spouse never quit. It is hard to be around it and not want to do it. I feel that if he had quit I never would have started back.”
“I was tempted while spending time with my girlfriends while the baby was at home (not with me). Nearly all of my friends smoke and its hard not to around them.”
At each time point, Motivational Decline was the third most cited reason for resuming smoking. This category reflected temptations that were causing participants to decline in their motivation to remain smoke free. Some examples from participant responses included missing the enjoyment of smoking, falling back into the habit of smoking, and not feeling prepared to maintain long-term abstinence. Sample responses coded under this theme follow:
“I thought I could have one after going months without and remain a quitter. But one made it ok for more.”
“I’m not sure why. I have always enjoyed smoking and I didn’t want to when I was pregnant. I didn’t really want to quit for life.”
Sub-Group Analyses
We were interested in exploring whether the frequency of attributions differed across different levels of household income (split at $30,000/year), age (median split at 24 years), and depressive symptoms (median split at each follow-up, ~13), as all three represent demographic and psychosocial variables that were associated with post-partum smoking relapse. Further descriptions of the coding categories which served as dependent variables can be found in Tables 2 and 3.
Individuals were dichotomized at $30,000/year. Lower income participants (41.6% of the sample) more frequently cited Treatment/External Resources as a reason for abstinence at month 1, χ2 (1) = 6.22, p = .013, and month 12, χ2 (1) = 8.79, p = .003, with the difference trending toward significance at month 8 (p = .073). When analyzing responses written by those who were smoking, income-related differences were seen for the Stress and Social categories, namely at 1 month post-partum. Lower income participants more frequently cited Stress as a reason for smoking, χ2 (1) = 14.33, p < .001, while there was a trend suggesting that higher income participants more frequently cited Social as a reason for smoking, χ2 (1) = 3.68, p = .055.
Age was dichotomized using a median split at 24 years. This created younger/older subgroups that positively covaried with income level (φ = .314). For abstinent participants, the only significant differences across these groups were seen at month 12. Younger participants more frequently cited Self-Efficacy, χ2 (1) = 6.16, p = .013, and Treatment/External Resources, χ2 (1) = 6.79, p = .009, as reasons for maintaining abstinence, whereas older participants more frequently cited Personal/general health, χ2 (1) = 5.49, p = .019, as a reason for abstinence. Responses cited by smokers differed at 1 month post-partum. Younger women mentioned Stress more often, χ2 (1) = 10.05, p = .002, whereas, older women expressed Social reasons more often, χ2 (1) = 4.47, p = .035.
Finally, a median split for CES-D scores at each time point created low depression and high depression subgroups. Differences in Coping as a reason for abstinence fluctuated over time. Women with higher CES-D scores more frequently endorsed Coping at month 1, χ2 (1) = 8.37, p = .004, and month 8, χ2 (1) = 4.05, p = .044. However, this relationship reversed at 12 months such that women with lower CES-D scores more frequently described Coping as a reason for abstinence, χ2 (1) = 4.78, p = .029. Among smokers, women with higher CES-D scores at 12 months more frequently described Stress as a reason for smoking, χ2 (1) = 8.38, p = .004.
Discussion
The goal of the current study was to examine participants’ attributions for maintaining abstinence or resuming smoking during the first 12 months post-partum. Our main findings indicate that personal, child, and family health were the most prevalent protective factors cited for abstinence maintenance, as they were the most frequently cited reasons for remaining abstinent at 1, 8, and 12 months post-partum. Meanwhile, stress was the most frequently cited reason for smoking relapse at all three time points. Our content analysis produced several other important reasons for abstinence and relapse, although their frequencies changed over time. More specifically, smoking cessation treatments, community resources, and social support became important contributors to abstinence as the post-partum period progressed, while a decline in motivation to remain smoke free and a lack of social support were consistent secondary contributors to relapse throughout the study period.
Employing a mixed-methods analysis strategy, we also explored whether responses differed by demographic and psychosocial risk factors for relapse, and we found evidence for the presence of differing themes based on household income, age, and level of depressive symptoms. For low income participants, treatments and external resources were important aids to assist abstinence at 1 and 12 months post-partum, and stress was a particularly powerful attribution for relapse at 1 month post-partum. Not surprisingly, given the covariance between income and age, similar patterns were seen for younger participants. They mentioned treatments and external resources, as well as increased self-efficacy, as reasons for abstinence at 12 months post-partum, whereas stress was mentioned as a reason for relapse at 1 month post-partum. Finally, women exhibiting higher levels of depression post-partum, tended to attribute their successful early abstinence (1 and 8 months postpartum) to using effective coping strategies. However, by 12 months this relationship reversed, with less depressed women more likely to attribute their success to coping, perhaps reflecting the difficulty of maintaining effective coping in the face of extended depression.
Implications for Intervention Development
Qualitative data can help researchers understand motivations and reasons for smoking (or in this case, resuming smoking) to assist in the development and tailoring of interventions (31). Our results suggest that open-ended written response data represents an easily-collected, yet underutilized, qualitative methodology that can enhance client-centered formative evaluation of an intervention. Formative research is an empirically supported approach for developing smoking cessation and relapse prevention interventions for this population (21, 32, 33), and the booklets that comprised the intervention described here were generated through a formative process involving in-person interviews (23).
In the vein of formative evaluation, our results identified several contributors to smoking relapse, including elevated stress, social pressures to return to smoking, and a lack of motivation to remain abstinent. Elevated stress during the post-partum period (26), living with a smoker (25), and intention to resume smoking (34) have all been identified as predictors of post-partum smoking relapse. Our results also support previous findings regarding key factors that contribute to postpartum smoking abstinence, including breastfeeding (35), social support (36), confidence in staying quit (37), and using effective coping strategies (17).
Taken together, these findings build on previous research by examining perceptions related to post-partum smoking relapse and determining which attributions appear most problematic to vulnerable sub-samples of post-partum women. Our results suggest that stress is consistently the most frequently cited contributor to post-partum smoking relapse, and this was a particularly relevant relapse factor for women who were younger, of lower income, and had more depressive symptoms. To that end, these results support the need to tailor intervention development for vulnerable sub-populations of pregnant women (38) and to incorporate stressors unique to the post-partum period, as well as social support networks, into the context of relapse prevention interventions (39)
Methodological Triangulation
This study also represents an extension of the primary outcomes of the parent trial (24) and reflects an initial attempt at implementing methodological triangulation within a smoking cessation intervention. Methodological triangulation involves utilizing multiple data collection strategies (e.g., surveys and open-ended responses) to explore a research question (40). Combining qualitative and quantitative methods allows researchers to increase confidence in findings from a single methodology (41) and glean meaningful information from their data that may have remained unknown if only one methodology were employed (42).
The parent trial (24) reports age and income as moderators of the intervention’s effectiveness; the results reported here share similar interaction effects for open-ended responses, as younger and lower income participants were more likely to cite treatment as a reason for abstinence. Thus, using a methodological triangulation approach and combining the open-ended results reported here with the quantitative results from the parent trial (24) allows for greater confidence in interpreting the effectiveness of the intervention, especially among lower-income and younger pregnant women. Similarly, our results support previous findings regarding key factors that contribute to postpartum smoking abstinence, including health concerns (for mother and baby), social support (36), confidence in staying quit (37), and coping with stress (43). These relationships would not have been discovered within our sample without an exploration of the qualitative data collected during the study, and they offer potential mediators of success for the FFBM intervention. To that end, given the breadth of responses for certain categories (e.g., stress), our results also support the idea of using a mixed-methods approach for generating new quantitative measures (e.g., measures that capture various stressors to explore which are most closely related to relapse).
Strengths and Limitations
The results of this study should be considered in light of its strengths and limitations. Strengths of the study include a longitudinal design, inclusive coding categories determined via content and thematic saturation, a large and diverse sample, and an extremely high response rate. Previous studies that have used a qualitative content analysis of open-ended free-text items have received significantly lower response rates than those seen among this sample (44, 45). This suggests that women find post-partum smoking relapse to be a salient, important issue, and they may feel more compelled to provide their perspectives on this topic than others. It also speaks to the value of including open-ended response questions in survey-based research, and these results support the assertion that this is an effective way to obtain individual perspectives on important issues among a large, diverse sample. Utilizing open-ended items, individuals are able to respond using their own words, which provides richer data as compared to closed-ended items and reinforces the notion that open-ended questions are viable research tools (46).
The study limitations also deserve mention. First, different individuals completed the free-response item at each time point, making it difficult to establish trends in themes across time. Therefore, conclusions about changes over time should be considered tentative. Second, although Treatment/External Resources was commonly cited as a reason for maintaining abstinence, this theme could be considered a somewhat coarse categorization, as it included a variety of different treatments and resources from the community. Third, based solely on the free-text responses, we were unable to determine if the intervention itself was a sufficient contributor to the reported abstinence among participants. However, the primary study outcome results indicated treatment efficacy, particularly among lower income women (24). Fourth, as in the parent study (24), there is significant overlap between income and age in the sample used for this analysis, with a significant proportion of the lower income sub-group being comprised of younger participants. Therefore, given the univariate nature of our analyses, it is possible that the consistencies seen in attributions for abstinence and relapse might be explained by this covariation. However, it is also important to note that differences across these risk factors did emerge despite this relationship, particularly in attributions for abstinence. Fifth, smoking status at each time point was obtained through self-report, but could not be validated via bio-chemical verification due to the challenges associated with validating abstinence via mail (47). However, a sub-sample of the participants in the parent study did have smoking status verified via breath carbon monoxide and saliva cotinine samples. Among this sub-sample, self-reported smoking status was highly consistent with biochemical verification (24). Finally, we must guard against reifying self-attributions, which are subject to a range of biases and do not necessarily reflect empirical facts (48).
Conclusions
In summary, this study describes the process and highlights the value of analyzing commonly collected, yet frequently unreported, data for examining participant perspectives in smoking cessation trials. Open-ended response data from a smoking relapse prevention-intervention indicate that stress is the most frequent attribution for smoking relapse in the short-term and long-term post-partum period. Child/family health was the most frequently cited attribution for abstinence in both the short-term and long-term post-partum period, and differences in themes across time were seen for several predictors of smoking relapse.
These findings reinforce the idea that there are multiple contributors to post-partum smoking relapse. Future relapse-prevention interventions should address issues such as stress management and motivational enhancement within their therapeutic approaches, as well as differentiate whether interventions focusing on personal vs. family health are more effective at promoting abstinence post-partum. Future directions could also consider exploring reasons for relapse in both longitudinal and cross-sectional study designs. More specifically, it would be important to understand how these attributions for smoking and abstinence change from pregnancy to the post-partum period. It would be important to extend this methodology to other vulnerable populations, such as women who live with partners who smoke or do not plan to breastfeed (37). Outside of smoking cessation, our results encourage the use of open-ended response data within formative research, as this approach is easily utilized, cost-efficient, and highly acceptable for collecting client-centered data among large, diverse samples.
Acknowledgments
This study was funded by National Cancer Institute grant R01 CA94256. The authors wish to thank Monica Carrington and Krissie Sismilich for their assistance in data transcription and management. We also would like to acknowledge the Survey Methods Core and Biostatistics Core at H. Lee Moffitt Cancer Center for their assistance in data collection and analysis.
References
- 1.Tong VT, Dietz PM, Morrow B, D’Angelo DV, Farr SL, Rockhill KM, et al. Trends in smoking before, during, and after pregnancy--Pregnancy Risk Assessment Monitoring System, United States, 40 sites, 2000–2010. MMWR Surveill Summ. 2013 Nov;62(6):1–19. [PubMed] [Google Scholar]
- 2.Colman GJ, Joyce T. Trends in smoking before, during, and after pregnancy in ten states. Am J Prev Med. 2003 Jan;24(1):29–35. doi: 10.1016/s0749-3797(02)00574-3. [DOI] [PubMed] [Google Scholar]
- 3.Tong VT, Dietz PM, Farr SL, D’Angelo DV, England LJ. Estimates of smoking before and during pregnancy, and smoking cessation during pregnancy: comparing two population-based data sources. Public Health Rep. 2013 May;128(3):179–88. doi: 10.1177/003335491312800308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahn RS, Certain L, Whitaker RC. A reexamination of smoking before, during, and after pregnancy. Am J Public Health. 2002 Nov;92(11):1801–8. doi: 10.2105/ajph.92.11.1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grover KW, Zvolensky MJ, Lemeshow AR, Galea S, Goodwin RD. Does quitting smoking during pregnancy have a long-term impact on smoking status? Drug Alcohol Depend. 2012 Jun 1;123(1–3):110–4. doi: 10.1016/j.drugalcdep.2011.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carmichael SL, Ahluwalia IB. Correlates of postpartum smoking relapse. Results from the Pregnancy Risk Assessment Monitoring System (PRAMS) Am J Prev Med. 2000 Oct;19(3):193–6. doi: 10.1016/s0749-3797(00)00198-7. [DOI] [PubMed] [Google Scholar]
- 7.Mullen PD. How can more smoking suspension during pregnancy become lifelong abstinence? Lessons learned about predictors, interventions, and gaps in our accumulated knowledge. Nicotine Tob Res. 2004 Apr;6(Suppl 2):S217–38. doi: 10.1080/14622200410001669150. [DOI] [PubMed] [Google Scholar]
- 8.Hofhuis W, de Jongste JC, Merkus PJFM. Adverse health effects of prenatal and postnatal tobacco smoke exposure on children. Arch Dis Child. 2003 Dec 1;88(12):1086–90. doi: 10.1136/adc.88.12.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coleman-Cowger VH. Smoking cessation intervention for pregnant women: a call for extension to the postpartum period. Matern Child Health J. 2012 Jul;16(5):937–40. doi: 10.1007/s10995-011-0837-2. [DOI] [PubMed] [Google Scholar]
- 10.Businelle MS, Kendzor DE, Reitzel LR, Vidrine JI, Castro Y, Mullen PD, et al. Pathways linking socioeconomic status and postpartum smoking relapse. Ann Behav Med. 2013 Apr;45(2):180–91. doi: 10.1007/s12160-012-9434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park ER, Chang Y, Quinn VP, Ross K, Rigotti NA. Perceived support to stay quit: what happens after delivery? Addict Behav. 2009 Dec;34(12):1000–4. doi: 10.1016/j.addbeh.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins ST, Heil SH, Badger GJ, Skelly JM, Solomon LJ, Bernstein IM. Educational disadvantage and cigarette smoking during pregnancy. Drug Alcohol Depend. 2009 Oct 1;104(Suppl 1):S100–5. doi: 10.1016/j.drugalcdep.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allen AM, Prince CB, Dietz PM. Postpartum depressive symptoms and smoking relapse. Am J Prev Med. 2009 Jan;36(1):9–12. doi: 10.1016/j.amepre.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen SN, Von Kohorn I, Schulman-Green D, Colson ER. The importance of social networks on smoking: perspectives of women who quit smoking during pregnancy. Matern Child Health J. 2012 Aug;16(6):1312–8. doi: 10.1007/s10995-011-0896-4. [DOI] [PubMed] [Google Scholar]
- 15.Bottorff JL, Kalaw C, Johnson JL, Stewart M, Greaves L, Carey J. Couple dynamics during women’s tobacco reduction in pregnancy and postpartum. Nicotine Tob Res. 2006 Aug;8(4):499–509. doi: 10.1080/14622200600789551. [DOI] [PubMed] [Google Scholar]
- 16.Ashford K, Hahn E, Hall L, Peden AR, Rayens MK. Postpartum smoking abstinence and smoke-free environments. Health Promot Pract. 2011 Jan;12(1):126–34. doi: 10.1177/1524839909353727. [DOI] [PubMed] [Google Scholar]
- 17.Psaros C, Pajolek H, Park ER. The role of negative affect management in postpartum relapse to smoking. Arch Womens Ment Health. 2012 Feb;15(1):15–20. doi: 10.1007/s00737-011-0250-2. [DOI] [PubMed] [Google Scholar]
- 18.Ripley-Moffitt CE, Goldstein AO, Fang WL, Butzen AY, Walker S, Lohr JA. Safe babies: a qualitative analysis of the determinants of postpartum smoke-free and relapse states. Nicotine Tob Res. 2008 Aug;10(8):1355–64. doi: 10.1080/14622200802238936. [DOI] [PubMed] [Google Scholar]
- 19.Levitt C, Shaw E, Wong S, Kaczorowski J. Systematic review of the literature on postpartum care: effectiveness of interventions for smoking relapse prevention, cessation, and reduction in postpartum women. Birth. 2007 Dec;34(4):341–7. doi: 10.1111/j.1523-536X.2007.00194.x. [DOI] [PubMed] [Google Scholar]
- 20.Hajek P, Stead LF, West R, Jarvis M, Hartmann-Boyce J, Lancaster T. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev. 2013;8:CD003999. doi: 10.1002/14651858.CD003999.pub4. [DOI] [PubMed] [Google Scholar]
- 21.Simmons VN, Cruz LM, Brandon TH, Quinn GP. Translation and adaptation of smoking relapse-prevention materials for pregnant and postpartum Hispanic women. J Health Commun. 2011 Jan;16(1):90–107. doi: 10.1080/10810730.2010.529492. [DOI] [PubMed] [Google Scholar]
- 22.Litvin EB, Rojas A, Brandon TH, Quinn G, Meade CD, Simmons VN, et al. Cultural Acceptability of a Smoking Relapse Prevention Intervention for Pregnant Women in Puerto Rico: Providers’ Feedback. Hispanic Health Care International. 2011;9(3):117–26. doi: 10.1891/1540-4153.9.3.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quinn G, Ellison BB, Meade C, Roach CN, Lopez E, Albrecht T, et al. Adapting smoking relapse-prevention materials for pregnant and postpartum women: formative research. Matern Child Health J. 2006 May;10(3):235–45. doi: 10.1007/s10995-005-0046-y. [DOI] [PubMed] [Google Scholar]
- 24.Brandon TH, Simmons VN, Meade CD, Quinn GP, Lopez Khoury EN, Sutton SK, et al. Self-help booklets for preventing postpartum smoking relapse: a randomized trial. Am J Public Health. 2012 Nov;102(11):2109–15. doi: 10.2105/AJPH.2012.300653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin LT, McNamara M, Milot A, Bloch M, Hair EC, Halle T. Correlates of smoking before, during, and after pregnancy. Am J Health Behav. 2008 May-Jun;32(3):272–82. doi: 10.5555/ajhb.2008.32.3.272. [DOI] [PubMed] [Google Scholar]
- 26.Park ER, Chang Y, Quinn V, Regan S, Cohen L, Viguera A, et al. The association of depressive, anxiety, and stress symptoms and postpartum relapse to smoking: A longitudinal study. Nicotine Tob Res. 2009 Jun 1;11(6):707–14. doi: 10.1093/ntr/ntp053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brandon TH, Collins BN, Juliano LM, Lazev AB. Preventing relapse among former smokers: a comparison of minimal interventions through telephone and mail. J Consult Clin Psych. 2000 Feb;68(1):103–13. doi: 10.1037//0022-006x.68.1.103. [DOI] [PubMed] [Google Scholar]
- 28.Brandon TH, Meade CD, Herzog TA, Chirikos TN, Webb MS, Cantor AB. Efficacy and cost-effectiveness of a minimal intervention to prevent smoking relapse: dismantling the effects of amount of content versus contact. J Consult Clin Psych. 2004 Oct;72(5):797–808. doi: 10.1037/0022-006X.72.5.797. [DOI] [PubMed] [Google Scholar]
- 29.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 30.Aita V, McIlvain H, Susman J, Crabtree B. Using Metaphor as a Qualitative Analytic Approach to Understand Complexity in Primary Care Research. Qual Health Res. 2003;13(10):1419–31. doi: 10.1177/1049732303255999. [DOI] [PubMed] [Google Scholar]
- 31.Nichter M, Quintero G, Nichter M, Mock J, Shakib S. Qualitative research: contributions to the study of drug use, drug abuse, and drug use(r)-related interventions. Subst Use Misuse. 2004;39(10–12):1907–69. doi: 10.1081/ja-200033233. [DOI] [PubMed] [Google Scholar]
- 32.Lowe JB, Windsor R, Balanda KP, Woodby L. Smoking relapse prevention methods for pregnant women: a formative evaluation. Am J Health Promot. 1997 Mar-Apr;11(4):244–6. doi: 10.4278/0890-1171-11.4.244. [DOI] [PubMed] [Google Scholar]
- 33.Crawford MA, Woodby LL, Russell TV, Windsor RA. Using formative evaluation to improve a smoking cessation intervention for pregnant women. Health Commun. 2005;17(3):265–81. doi: 10.1207/s15327027hc1703_4. [DOI] [PubMed] [Google Scholar]
- 34.Roske K, Hannover W, Grempler J, Thyrian JR, Rumpf HJ, John U, et al. Post-partum intention to resume smoking. Health Educ Res. 2006 Jun;21(3):386–92. doi: 10.1093/her/cyh069. [DOI] [PubMed] [Google Scholar]
- 35.Ratner PA, Johnson JL, Bottorff JL, Dahinten S, Hall W. Twelve-month follow-up of a smoking relapse prevention intervention for postpartum women. Addict Behav. 2000 Jan-Feb;25(1):81–92. doi: 10.1016/s0306-4603(99)00033-7. [DOI] [PubMed] [Google Scholar]
- 36.Pollak KI, Baucom DH, Peterson BL, Stanton S, McBride CM. Rated helpfulness and partner-reported smoking cessation support across the pregnancy-postpartum continuum. Health Psychol. 2006 Nov;25(6):762–70. doi: 10.1037/0278-6133.25.6.762. [DOI] [PubMed] [Google Scholar]
- 37.Simmons VN, Sutton SK, Quinn GP, Meade CD, Brandon TH. Prepartum and Postpartum Predictors of Smoking. Nicotine Tob Res. 2013 Nov 7; doi: 10.1093/ntr/ntt177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simonelli MC, Velicer WF. Cluster subtypes appropriate for preventing postpartum smoking relapse. Addict Behav. 2012 Mar;37(3):280–6. doi: 10.1016/j.addbeh.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fang WL, Goldstein AO, Butzen AY, Hartsock SA, Hartmann KE, Helton M, et al. Smoking Cessation in Pregnancy: A Review of Postpartum Relapse Prevention Strategies. J Am Board Fam Pract. 2004 Jul;17(4):264–75. doi: 10.3122/jabfm.17.4.264. [DOI] [PubMed] [Google Scholar]
- 40.Duffy ME. Methodological triangulation: a vehicle for merging quantitative and qualitative research methods. Image J Nurs Sch. 1987 Fall;19(3):130–3. doi: 10.1111/j.1547-5069.1987.tb00609.x. [DOI] [PubMed] [Google Scholar]
- 41.Östlund U, Kidd L, Wengström Y, Rowa-Dewar N. Combining qualitative and quantitative research within mixed method research designs: A methodological review. Int J Nurs Stud. 2010 Mar;48(3):369–83. doi: 10.1016/j.ijnurstu.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thurmond VA. The Point of Triangulation. J Nurs Scholarsh. 2001;33(3):253–8. doi: 10.1111/j.1547-5069.2001.00253.x. [DOI] [PubMed] [Google Scholar]
- 43.Polanska K, Hanke W, Sobala W, Lowe JB, Jaakkola JJ. Predictors of smoking relapse after delivery: prospective study in central Poland. Matern Child Health J. 2011 Jul;15(5):579–86. doi: 10.1007/s10995-010-0639-y. [DOI] [PubMed] [Google Scholar]
- 44.Corner J, Wagland R, Glaser A, Richards SM. Qualitative analysis of patients’ feedback from a PROMs survey of cancer patients in England. BMJ Open. 2013;3(4) doi: 10.1136/bmjopen-2012-002316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Denscombe M. Item non-response rates: a comparison of online and paper questionnaires. International Journal of Social Research Methodology. 2009 Oct 01;12(4):281–91. [Google Scholar]
- 46.Krosnick JA. Survey Research. Annu Rev Psychol. 1999;50:537–567. doi: 10.1146/annurev.psych.50.1.537. [DOI] [PubMed] [Google Scholar]
- 47.Etter JF, Perneger TV, Ronchi A. Collecting saliva samples by mail. Am J Epidemio. 1998 Jan 15;147(2):141–6. doi: 10.1093/oxfordjournals.aje.a009426. [DOI] [PubMed] [Google Scholar]
- 48.Mezulis AH, Abramson LY, Hyde JS, Hankin BL. Is there a universal positivity bias in attributions? A meta-analytic review of individual, developmental, and cultural differences in the self-serving attributional bias. Psychol Bull. 2004 Sep;130(5):711–47. doi: 10.1037/0033-2909.130.5.711. [DOI] [PubMed] [Google Scholar]