Abstract
Rhinoviruses are the most common virus to infect man causing a range of serious respiratory diseases including exacerbations of asthma and COPD. Type I IFN and IL-15 are thought to be required for antiviral immunity however their function during rhinovirus infection in vivo is undefined. In RV infected human volunteers, IL-15 protein expression in fluid from the nasal mucosa and in bronchial biopsies was increased. In mice, RV induced type I IFN-dependent expression of IL-15 and IL-15Rα which in turn were required for NK- and CD8+ T-cell responses. Treatment with IL-15-IL-15Rα complexes (IL-15c) boosted RV-induced expression of IL-15, IL-15Rα, IFN-γ, CXCL9 and CXCL10 followed by recruitment of activated, IFN-γ expressing NK, CD8+ and CD4+ T cells. Treating infected IFNAR1−/− mice with IL-15c similarly increased IL-15, IL-15Rα, IFN-γ and CXCL9 (but not CXCL10) expression also followed by NK-, CD8+- and CD4+-T cell recruitment and activation. We have demonstrated that type I IFN induced IFN-γ and cellular immunity to RV was mediated by IL-15 and IL-15Rα. Importantly we also show that IL-15 could be induced via a type I IFN-independent mechanism by IL-15 complex treatment which in turn was sufficient to drive IFN-γ expression and lymphocyte responses.
Introduction
Human rhinoviruses (RV) are the most common viral infection afflicting mankind. Whilst the nasal epithelium is the primary site of replication manifesting as the common cold, RV can also be detected in the lower airways 1,2 where it can cause severe and life threatening exacerbations in patients with asthma, chronic obstructive pulmonary disease (COPD) and pneumonia 3,4. Collectively these diseases are responsible for significant morbidity and mortality and enormous health care costs5.
Despite their significant involvement in respiratory diseases, surprisingly little is known about the role of cellular immune responses in RV pathogenesis. The involvement of natural killer (NK) cells and T cells during RV infection has been inferred from numerous studies demonstrating robust induction of lymphocyte recruiting chemokines such as CXCL10 during infection 6. Experimental infection studies in man have demonstrated infiltrating lymphocytes in nasal mucosa and bronchial biopsies associated with blood lymphopenia 7. Characterisation of blood leukocyte responses identified a significant reduction of CD4+ T cells suggesting that these are preferentially recruited to the site of RV infection 8. More recently mouse infection models have been developed allowing more detailed analyses of immune responses to RV. These have begun to confirm that RV can induce a range of lymphocyte recruiting mediators associated with infiltration of NK cells and T cells to the lung9,10.
Interleukin-15 (IL-15) is a type I interferon (IFN)-induced cytokine that exerts anti-viral effects by activation of NK cells and CD8+ T cells 11, 12. IL-15 shares the IL-2Rβ and common-γ chains of the IL-2 receptor13,14, but also binds its specific IL-15Rα chain with much greater affinity 15. Signalling occurs via a unique trans-presentation mechanism involving IL-15 expression by macrophages, dendritic cells (DCs) and epithelial cells where it is bound and stabilised by IL-15Rα and transported to the cell surface membrane for presentation to adjacent neighbouring cells in trans 16,17. During infection IL-15 is critical for the activation, recruitment and expansion of NK cells and CD8+ T cells. NK cells are innate effector lymphocytes that can act to directly eliminate virally infected cells via production of cytolytic enzymes such as granzymes and produce cytokines such as IFN-γ that regulate adaptive immune responses 18,19. Direct type I IFN signalling is reported important for regulating NK cell functions during viral infections 20-22. NK cell development and homeostasis is also dependent on IL-15 signalling as illustrated by the severe deficiency of NK cells in IL-15−/− and IL-15Rα−/− mice 23,24. IL-15 and NK cells are also important for regulating adaptive T cell responses during respiratory infections, with depletion of NK cells causing impaired CD8+ T cell responses against influenza and M. tuberculosis 25,26.
We have previously used in vitro RV infection models involving bronchial epithelial cells and bronchoalveolar lavage (BAL) macrophages to identify deficient expression of type I IFN in asthma and COPD 27,28 and IL-15 in asthma 29, identifying a potentially important link between IFN and IL-15 in the pathogenesis of RV induced disease. To investigate the effect of loss of type I IFN-mediated responses in vivo, we used a mouse RV infection model observing severely impaired NK cell and T cell responses in type I IFN receptor knockout (IFNAR1−/−) mice. Clearly type I IFN was critical for NK cell responses to RV however, the role of IL-15 was not studied 10.
In the present study, we investigated the interaction between type I IFN-mediated responses, IL-15 and cellular immunity following RV infection in vivo in man and mouse. We found that RV infection induced IL-15 protein production in nasal and bronchial mucosa of healthy human subjects. We have provided novel in vivo data showing that RV-induced IL-15/IL-15Rα expression was mediated by type I IFN, which in turn was required for early expression of IFN-γ and recruitment of activated, IFN-γ-expressing NK cells and T cells. We have further demonstrated that exogenous delivery to the airways of biologically active IL-15 complexed with IL-15Rα (IL-15c) during RV infection in both wild-type (wt) and IFNAR1−/− mice boosted early lung expression of IFN-γ and the lymphocyte recruiting chemokine CXCL9/MIG (monokine induced by gamma interferon) followed by lymphocyte recruitment.
Results
RV infection induced IL-15 in nasal and bronchial mucosa was associated with Th1 immunity
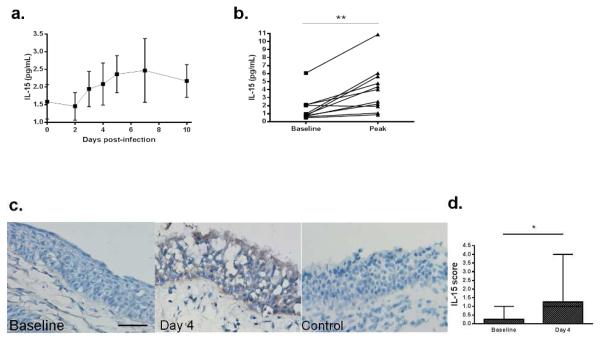
We employed a human experimental RV infection model recruiting healthy volunteers to determine if RV infection induced IL-15 expression in vivo. In a group of 11 human subjects we repeatedly sampled the nasal mucosal fluid prior to infection and up to ten days after infection (Fig. 1a). When baseline levels were compared with the peak infection levels for each subject we observed a significant increase in IL-15 protein (Fig. 1b). Viral load in nasal lavage was determined by PCR analysis of viral RNA levels. Although viral RNA- and IL-15 protein-levels typically peaked between day 2 and day 6 post-infection no statistically significant correlation for peak viral load with IL-15 was observed (data not shown).The lack of a clear relationship between peak IL-15 expression and viral load was likely due to the small number of subjects (11) which meant the study was not powered to quantify the dynamic interaction between IL-15 and viral load.
Figure 1. Experimental human RV infection induced IL-15 and associated Th1 and inflammatory mediators.
Healthy volunteers were infected with RV-16 and levels of soluble mediators in the nasal mucosal fluid were measured by MSD platform and IL-15 in the epithelium of bronchial biopsies measured by IHC. (a) Levels of IL-15 protein in the nasal mucosa during infection. (b) Baseline and peak infection levels of IL-15. (c) Images of representative IHC staining for IL-15 protein in human bronchial biopsies at 14 days before infection (baseline), 4 days post-infection with RV and normal mouse serum staining control. (d) IHC staining score for IL-15 in bronchial biopsies. Scale bar 50μm. IL-15 data are presented as mean ±SEM, baseline compared to infection peak data were analysed by Mann-Whitney test. ***p<0.001, **p<0.01 and *p<0.05 as indicated, NS not significant. Differences were considered significant for all statistical tests at p<0.05. All reported p values are two-sided.
In a separate study also involving 11 healthy volunteers experimentally infected with the same RV-16 inoculum 30, we used immunohistochemistry (IHC) to detect IL-15 protein expression in the lower airways (bronchial biopsies) at baseline (2 weeks before infection) and 4 days after infection. IL-15 positivity was apparent on the apical surface of the epithelium and in cells directly below the epithelium (Fig. 1d) and was significantly increased compared to uninfected subjects (Fig. 1e).
IL-15 and IL-15 receptor α (IL-15Rα) expression during RV infection
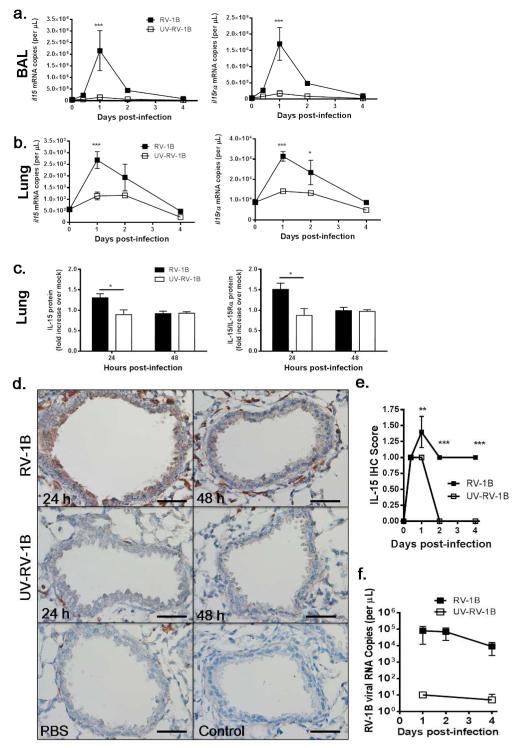
We used a mouse RV infection model to analyse Il15 and Il15rα mRNA expression by BAL cells (Fig. 2a) and lung tissue (Fig. 2b) observing significantly increased levels compared to baseline and UV-inactivated RV-1B (UV-RV-1B)-dosed mice. Expression of mRNA for both molecules peaked at 1 day post-infection (p.i.) returning to baseline levels by 4 days p.i. (Fig. 2a,b). Up-regulated expression of IL-15 and IL-15Rα proteins (measured as soluble IL-15-IL-15Rα complexes) in lung tissue similarly peaked at 1 day p.i. (Fig. 2c). Further analysis of lung IL-15 protein by IHC revealed increased expression by bronchial epithelial cells and sub-epithelial DC-like cells in RV infected mouse lungs (Fig. 2d), which when scored was significantly higher than IL-15 expression in uninfected mice and mice dosed with UV-RV-1B (Fig. 2e). A small increase in IL-15 protein following UV-inactivated virus was detected by IHC but was not apparent in lung homogenate using ELISA. This was likely due to differences in sensitivity of the two assays. The peak of IL-15 and IL-15Rα expression coincided with peak viral loads in the lung at 1 day p.i., which remained elevated at 2 days p.i. and declined thereafter (Fig. 2e).
Figure 2. Rhinovirus-induced IL-15 and IL-15Rα gene and protein expression.
BALB/c mice were either infected i.n. with 5×106 TCID50 of RV-1B or dosed with inactivated UV-RV-1B or PBS (mock infected/0 days post-infection). (a and b) Levels of Il15 and Il15rα mRNA were measured by qPCR in BAL cells (a) and lung tissue (b). (c) IL-15 and soluble IL-15-IL-15Rα complex (IL-15c) protein levels in lung homogenate expressed as fold increase over mock infected. (d) Images of representative IHC staining for IL-15 protein in lung sections at 24 h and 48 h post-infection (RV-1B) or treatment with UV-inactivated virus (UV-RV-1B), mock infection (PBS) and normal goat serum staining control. Total magnification of ×400. Scale bar 50 μm. (e) Time course of IL-15 staining based on IHC score. (f) Time course of RV-1B viral load measured by qPCR in lung tissue. All data are representative of two to three independent experiments, n = 4-6 mice per group. Data was analysed by two-way ANOVA, ***p<0.001, **p<0.01 and *p<0.05 as indicated, all data are expressed as mean ± SEM.
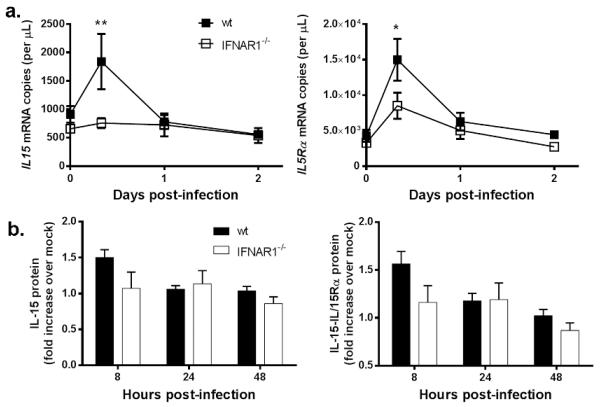
Type I IFN receptor is required for IL-15 and IL-15Rα expression
Type I IFNs are reported to induce expression of IL-15 by macrophages, DCs and epithelial cells11, and RV-induced expression of IFN-α and IFN-β in BALB/c mice (Fig. S1) was associated with expression of IL-15 and IL-15Rα at 24 h p.i. We have previously shown that type I IFN receptor knockout (IFNAR1−/−) mice have deficient type I and type III IFN production and NK cell responses during RV infection however, IL-15 expression was not assessed 10. Therefore we used these mice to determine if type I IFN signalling was required for IL-15 expression during RV infection. Significantly attenuated Il15 and Il15rα mRNA expression was observed in IFNAR1−/− mice compared to strain-matched wt mice (Fig. 3a) with trends for reduction in IL-15 and IL-15-IL-15Rα protein complexes in lung tissue (Fig. 3b).
Figure 3. Type I IFN receptor is necessary for RV-induced IL-15 and IL-15Rα.
IFNAR1−/− and wt strain matched controls were either infected i.n. with 5×106 TCID50 of RV-1B or dosed with PBS (mock/0 h post-infection). (a) Levels of Il15 and Il15rα mRNA were measured by qPCR in lung tissue. (b) IL-15 and soluble IL-15-IL-15Rα complex (IL-15c) protein levels in lung homogenate expressed as fold increase over mock infected. All data are representative of three independent experiments, n = 4-6 mice per group. Data was analysed by two-way ANOVA, **p<0.01 and *p<0.05 as indicated, all data are expressed as mean ± SEM.
IL-15 is critical for the NK cell and CD8+ T cell responses during RV infection
Next we performed a time course analysis of NK cell responses in the BAL and lung observing peak NK cell accumulation at 2 days p.i., and peak numbers of NK cells expressing CD69, IFN-γ and granzyme B was also detected at this time point (Fig. S2). NK cell numbers declined to baseline by day 4 and day 7 in the BAL and lung respectively, with levels of IFN-γ+ NK cells remaining significantly elevated over controls at day 4 p.i. in the lung. UV-inactivated RV failed to induce NK cell responses.
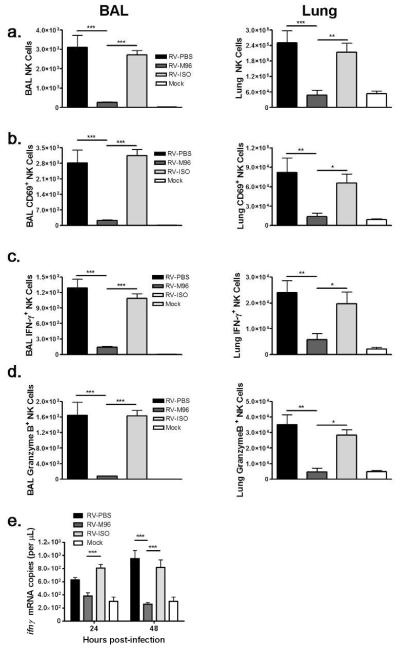
IL-15−/− and IL-15Rα−/− mice have a severe deficiency of NK cells. One option available to study IL-15 mediated NK cell responses during RV infection was to transiently block IL-15 in the lung. We investigated the dependence of RV-induced NK cell responses on IL-15 by i.n. administration of an IL-15 neutralising antibody (M96) at the time of infection, to transiently block virus-induced lung IL-15 activity. To ensure the antibody did not greatly affect basal lymphocyte levels systemically, we assessed lung and spleen in uninfected mice observing no significant change in total leukocyte cell numbers or percentage of CD4+ and CD8+ T cells indicating that cells other than NK cells were not affected by antibody treatment in the absence of infection. In the spleen, the percentage of NK cells declined approximately 30% at 48 h, and in the lungs approximately 50% at 48 h after antibody treatment (Fig. S3).
Although antibody treatment modestly affected NK cell baseline levels by 48 h post-treatment, the administration of antibody at the time of infection, when NK cell numbers were normal, permitted investigation into the role of RV-induced IL-15 on the accumulation and activation of NK cells. The presence of IL-15 neutralising antibody at the time of infection resulted in a >90% and approximately 75% reduction in total NK cell numbers in BAL and lung tissue respectively by 48 h after infection (Fig. 4a). Similarly CD69+ , IFN-γ+ or granzyme B+ NK cells failed to accumulate with IL-15 neutralisation, further evidence of a critical role in pulmonary NK cell responses during RV infection (Fig. 4b-d). In association with these deficient NK cell responses, Ifnγ gene expression in the lung was also significantly suppressed (Fig. 4e).
Figure 4. Rhinovirus induced NK cell responses were dependent on IL-15 signalling.
BALB/c mice were either infected i.n. with 5×106 TCID50 of RV-1B or dosed with PBS in addition to an IL-15 neutralising antibody (M96), isotype control antibody or PBS at the time of infection. (a-d) Flow cytometry was used to determine the total number of NK cells (CD3− NKp46+) (a), CD69+ NK cells (b), IFN-γ+ NK cells (c) and granzyme B+ NK cells (d) in the BAL and lung tissue, at 48 h post-infection. (e) Levels of Ifnγ mRNA were measured by qPCR in lung tissue. All data are representative of two independent experiments, n = 4-7 mice per group. Data were analysed by two-way ANOVA, ***p<0.001, **p<0.01 and *p<0.05 as indicated, all data are expressed as mean ± SEM.
Since CD8+ T cell responses during RV infection have not been studied in vivo we analysed these cells and assessed the role of IL-15 using M96. We found that CD8+ T cell responses were also impaired in RV-M96 treated mice compared to controls (Fig. 5a), analysed at 48 h p.i. which was previously observed to be the peak of the CD8+ T cell response to RV infection in mice (data not shown). RV-M96 treated mice demonstrated significantly reduced numbers of total CD8+ T cells, CD69+ CD8+ T cells and IFN-γ+ CD8+ T cells compared to control infected mice in the BAL. The same trend was observed in lung tissue but statistical significance was only reached for reduced numbers of total CD8+ T cells between RV-M96 and RV-PBS treated mice (Fig. 5a).
Figure 5. IL-15 signalling was important for CD8+ T cell responses during rhinovirus infection.
BALB/c mice were either i.n. infected with 5×106 TCID50 of RV-1B or dosed with PBS in addition to an IL-15 neutralising antibody (M96), isotype control antibody or PBS at the time of infection. Alternatively, IL-15Rα−/− and strain matched control wt mice were either i.n. infected with 5×106 TCID50 of RV-1B or dosed with PBS (mock/0 h post-infection). Flow cytometry was used to determine the total number of CD8+ T cells (CD3+ CD8+), CD69+ CD8+ T cells and IFN-γ+ CD8+ T cells in the BAL and lung of (a) M96 treated BALB/c mice at 48 h post-infection and (b) IL-15Rα−/− or wt mice at the indicated time points after treatment. (c) Levels of Ifnγ mRNA were measured by qPCR in lung tissue. Levels of RV-1B viral RNA in lung tissue were measured by qPCR to determine the viral load in (d). M96 treated BALB/c mice and (e) IL-15Rα−/− and wt mice. All data are representative of two to three independent experiments, n = 4-7 mice per group. Data was analysed by two-way ANOVA, ***p<0.001, **p<0.01 and *p<0.05 as indicated, all data are expressed as mean ± SEM.
To further investigate the role of IL-15 during RV infection we studied IL-15Rα knockout (IL-15Rα−/−) mice which have a severe deficiency of NK cells. We confirmed this and that RV infection could not induce NK cell responses in these mice (Fig. S4). We next assessed total, CD69+ and IFN-γ+ CD8+ T numbers in the airways and lung tissue during RV infection, observing that CD8+ T cell responses were also severely impaired in IL-15Rα−/− mice (Fig. 5b) as was IFN-γ expression (Fig. 5c). Transiently blocking IL-15 using M96 did not significantly impact on the level of RV RNA in the lungs (Fig. 5d). In contrast, by 24 h p.i. we did observe significantly increased RV RNA in the lungs of IL-15Rα−/− mice when compared with infected wt controls (Fig. 5e). We noted that viral load was higher in B6.129 mice (control for IL-15Rα−/− mice) compared to BALB/c mice used in the anti-IL-15 antibody blocking studies. Therefore differences in mouse strain susceptibility to viral infection may have also contributed to the greater apparent effect of IL-15 receptor deficiency on lung viral load.
Exogenous IL-15-IL-15 receptor complexes do not require type I IFN to induce IFN-γ and lymphocyte recruitment
RV infection studies with models of IL-15 deficiency revealed that IL-15 was required for IFN-γ expression and lymphocyte activation and recruitment (Fig. 4 and 5). We hypothesised that supplementing bioactive IL-15 complexed to IL-15Rα (IL-15c) should boost these responses. The role of type I IFN in this process was also investigated using IFNAR1−/− mice. We have previously reported that IFNAR1−/− mice fail to recruit and activate NK cells in response to RV infection10 which was confirmed for this study (Fig. S5). IL-15c treatment alone (in the absence of infection) did not affect baseline lung NK cell or CD4+ and CD8+ T cell numbers or activation status in either wt or IFNAR1−/− mice. In RV infected wt mice, IL-15c treatment significantly boosted NK cell responses over that induced by infection alone in the BAL (Fig. 6a) and lung (Fig. 6b) as indicated by increased total, CD69+ , IFN-γ+ and granzyme B+ NK cell numbers. Furthermore, administering IL-15c to IFNAR1−/− mice completely restored NK cell responses to RV infection to levels similar to those observed in IL-15c-treated wt mice. Similarly, IL-15c treatment also significantly boosted RV-induced BAL (Fig. 6c) and lung (Fig. 6d) activated CD8+ T cell responses in wt mice. In IFNAR1−/− mice IL-15c-stimulated CD8+ T cell responses were comparable to those observed in IL-15c-treated wt mice. CD4+ T cell responses were also boosted with IL-15c treatment to similar levels in both wt and IFNAR1−/− RV infected mice compared to infection alone in BAL (Fig. 6e) and lung (Fig. 6f). These results demonstrate that IL-15 can augment RV-induced lymphocyte responses independently of type I IFN signalling.
Figure 6. IL-15 complex restored NK cell, CD8+ and CD4+ T cell responses in the absence of type I IFN receptor signalling.
IFNAR1−/− and strain matched wt control mice were either infected with 5×106 TCID50 of RV-1B i.n. or dosed with PBS (mock/0 h post-infection) in the absence or presence of IL-15-IL-15Rα complex (IL-15c). (a-f) Flow cytometry was used to determine the time course of total numbers of NK cells (CD3− NKp46+), CD69+ NK cells, IFN-γ+ NK cells and Granzyme B+ NK cells in the BAL (a) and lung (b); CD8+ T cells (CD3+ CD8+), CD69+ CD8+ T cells and, IFN-γ+ CD8+ T cells in the BAL (c) and lung (d); and CD4+ T cells (CD3+ CD4+), CD69+ CD4+ T cells and IFN-γ+ CD4+ T cells in the BAL (e) and lung (f) at the indicated time points post infection. All data are representative of three independent experiments, n = 4-6 mice per group. Data were analysed by two-way ANOVA, ###/***p<0.001, ##/**p<0.01 and #/*p<0.05 as indicated, all data are expressed as mean ± SEM. * refers to wt vs. wt IL-15c groups and # refers to IFNAR1−/− vs. IFNAR1−/− IL-15c groups.
IL-15c increased IL-15 and type I and type II IFN responses
To determine which IL-15 stimulated responses do not require type I IFN signalling during RV infection, we assessed expression of anti-viral/Th1-associated molecules in wt and IFNAR1−/− mice following IL-15c treatment with RV infection. IL-15c enhanced both Il15 and Il15rα lung gene expression in wt and IFNAR1−/− mice (Fig. 7a). There was a trend for increased Ifnβ gene expression in wt and IFNAR1−/− mice with IL-15c treatment (Fig. 7b) and this corresponded with significantly increased BAL IFN-β protein levels in IFNAR1−/− mice but no increase was detected in wt mice (Fig. 7b). IFN-α was poorly induced during RV infection in IFNAR1−/− mice in contrast to wt mice. Even so, IL-15c treatment was able to significantly increase the detectable level of BAL IFN-α protein in IFNAR1−/− mice. For wt, mice despite robust induction IL-15c actually reduced the level of IFN-α. IL-15c treatment significantly increased IFN-λ mRNA expression in both RV infected wt and IFNAR1−/− mice however, corresponding increases in BAL IFN-λ protein was only significant in IFNAR1−/− mice (Fig. 7b). Furthermore, despite similar levels of IFN-λ mRNA detected in corresponding treatment groups of wt and IFNAR1−/− mice, greater levels of protein was observed in wt mice.
Figure 7. IL-15c administration during rhinovirus infection boosts expression of IL-15, IL-15Rα, type I, II and III IFNs and ISGs.
IFNAR1−/− and strain matched control wt mice were either infected i.n. with 5×106 TCID50 of RV-1B or dosed with PBS (mock/0 h post-infection) in the presence or absence of IL-15c. (a) Levels of Il15 and Il15rα mRNA were measured by qPCR in lung tissue at 24 and 48 h post-infection. (b) Levels of IFN-α, IFN-β and IFN-λ2/3 protein in BAL fluid were measured by ELISA and Ifnβ and Ifnλ mRNA in lung tissue by qPCR at 24 h post-infection. (c) Expression of ISGs Pkr and Oasl mRNA in lung tissue and CXCL10 protein in BAL 24 h post infection. (d) Lung Ifnγ mRNA and CXCL9 protein in BAL fluid 24 h post infection; * refers to wt vs. wt IL-15c groups and # refers to IFNAR1−/− vs. IFNAR1−/− IL-15c groups. All data are representative of two to three independent experiments, n = 4-6 mice per group. Data were analysed by two-way ANOVA, ###/***p<0.001, ##/**p<0.01 and #/*p<0.05 as indicated, all data are expressed as mean ± SEM.
We have previously shown full induction of the ISGs 2′-5′-oligoadenylate synthetase 1 (Oas1), protein kinase R (Pkr) and CXCL10 during RV infection required expression of type I IFN receptor10. IL-15c treatment augmented RV induced expression of (Oas1) mRNA, (Pkr) mRNA and CXCL10 protein in wt mice however, statistical significance was only reached for increased CXCL10 expression (Fig. 7c). IL-15c treatment also significantly increased lung Ifnγ gene expression at 8 h p.i., which was followed by significantly increased production of CXCL9 at 24 h p.i. in wt and IFNAR1−/− mice to equal levels (Fig. 7d). These data show that IL-15c treatment greatly boosted expression of IFN-γ and IFN-γ stimulated chemokines during RV infection via a type I IFN-independent mechanism.
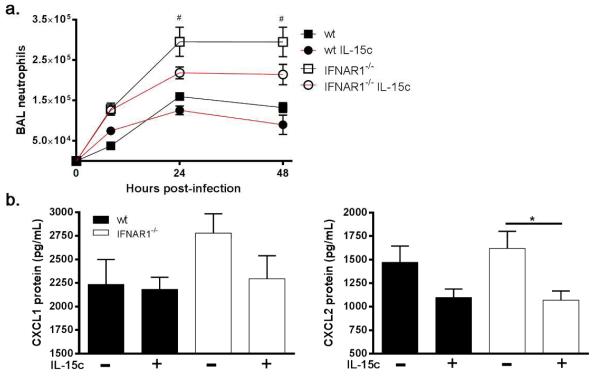
IL-15c treatment reduced airway neutrophilic inflammation
A feature of the response to RV infection in human and mouse models is neutrophilic inflammation and this is exacerbated by IFN deficiency 10. We compared airway neutrophilia following RV infection observing a significant increase in IFNAR1−/− mice compared to wt as previously reported. IL-15c treatment reduced the numbers of neutrophils in the airways of IFNAR1−/− mice (Fig. 8a). This was associated with reduced expression of the neutrophil recruiting chemokines CXCL1 and CXCL2 at 8 h p.i. (Fig. 8b), and by 24 h p.i. levels had declined to baseline in all groups (data not shown).
Figure 8. IL-15c suppressed exacerbated neutrophilic inflammation and associated chemokine expression in RV-infected type I IFN receptor deficient mice.
IFNAR1−/− and wt mice were either infected i.n. with 5×106 TCID50 of RV-1B or dosed with PBS (mock/0 h post-infection) in the absence or presence of IL-15c. (a) Timecourse of neutrophils in the BAL was assessed by differential cell counts, at the indicated time points after treatment; # refers to IFNAR1−/− vs. IFNAR1−/− IL-15c groups. (b) Neutrophil chemokines CXCL1 and CXCL2 were analysed in BAL fluid 8 h post-infection by ELISA. All data are representative of two to three independent experiments, n = 4-6 mice per group. Data were analysed by two-way ANOVA, ***p<0.001 and #/*p<0.05 as indicated, all data are expressed as mean ± SEM.
Discussion
Despite their dominant role in respiratory diseases globally, much is still unknown about the immunopathogenesis of RV infections. In this study, we first used a human experimental RV infection model observing increased IL-15 protein expression in the upper and lower respiratory tract. The nasosorption™ method of repeated sampling of the upper respiratory tract provided undiluted samples of nasal mucosal lining fluid that allowed detection of numerous immune mediators. This enabled us to detect IL-15 protein (as well as many other immune mediators) directly in the mucosa of both the upper and lower airways during RV infection, a first for RV and indeed any respiratory virus.
RVs primarily replicate in nasal epithelial cells of the upper respiratory tract and cause the common cold. RVs can also infect the lungs but usually only cause disease when infection exacerbates a pre-existing respiratory condition such as asthma30 or COPD28. To study ‘normal’ host immunity to RV infection in the absence of pre-existing respiratory disease we employed a mouse RV infection model. This involved delivery of a high dose of RV-1B that, whilst not designed to model human disease per se, is widely used to study immunity to RV as it generates robust and reproducible inflammatory-and anti-viral immune responses in commonly used mouse strains including Balb/c9, C57BL/631 and B6.12910 which were the strains used in this study. For all of these mouse strains it was reported that RV infection induced an acute neutrophilc response accompanied by expression of neutrophil recruiting chemokines, proinflammatory cytokines and interferons. This was followed by expression of lymphocyte recruiting chemokines, resolution of neutrophilc inflammation and recruitment of lymphocytes to the lungs.
Investigation of the role of IL-15 is complicated by constitutive expression and requirement for NK cell homeostasis. This potentially contributed to the modest induction levels of IL-15 protein expression observed during RV infection in human and mouse models. We employed two strategies to block IL-15 activity during RV infection. The first involved lung delivery of an IL-15 neutralising antibody to transiently block IL-15 during infection. In uninfected mice this eventually caused a 50% reduction in lung NK cells after two days. During infection IL-15 neutralisation (at the time of infection so NK cell numbers intact) almost completely ablated lung tissue and airway NK cell responses providing direct evidence that IL-15 is required for acute NK cell responses during RV infection. We also studied IL-15Rα−/− mice which have a constitutive severe deficiency of NK cells and lower numbers of CD8+ T cells in the lungs at baseline. IL-15Rα−/− mice had severely deficient CD8+ T cell responses, demonstrating that IL-15 is necessary for recruitment of activated IFN-γ expressing CD8+ T cells. Reduced CD8+ T cell responses were also observed with IL-15 neutralisation by antibody during infection however, the reduction was modest.
Despite having profound effects on host immune responses, IL-15 activity only modestly influenced viral replication. IL-15Rα−/− mice had a transient increase in viral load. Anti-IL-15 antibody treatment had no effect on levels of lung viral RNA. This difference is associated with the different degrees of CD8+ T cell deficiency discussed above. Little is known about the kinetics of RV replication in the human lung as it is technically difficult to repeatedly sample individual subjects during infection32. In the absence of this information it is difficult to interpret lung replication data in the mouse. Also the dose of virus required to induce robust pulmonary immune responses in mice is high and did not reflect a natural infection in humans which usually does not induce substantial lower respiratory tract inflammation. Thus RV replication data in the mouse should be interpreted with caution particularly in the absence of good human in vivo lung infection data to support such analyses. This is the first in vivo demonstration of type I IFN-dependant IL-15 and IL-15Rα up-regulation in response to RV infection. IHC staining indicated that IL-15 was predominantly expressed on the apical surface of epithelial cells lining the airway as well as infiltrating leukocytes in the sub-epithelium. The location and morphology of these cells was consistent with them being activated DCs which are part of the complex network that lie directly beneath the airway epithelial layer33. McGill et al demonstrated higher levels of surface IL-15 on pulmonary plasmacytoid (pDCs) and CD8α+ DCs compared to alveolar macrophages after influenza infection, and IL-15 trans-presentation by these DC subsets promoted CD8+ T cell survival and accumulation in the lungs 17.
We demonstrate that even in the absence of type I IFN signalling, previously reported to be critical for activation of anti-viral NK cell and CD8+ T cell responses, IL-15c was able to rescue these responses and even boost them above levels observed in wt mice. Thus, we have identified IL-15 (and IL-15Rα) as the only ISGs necessary for these key anti-viral lymphocyte responses. One other study has demonstrated the ability of exogenous IL-15 to mediate the accumulation of proliferating NK cells independently of type I IFNs 22 however, the effect on activation of anti-viral lymphocyte subsets and IFN-γ expression during virus infection was not investigated. We observed rapid and enhanced induction of lung Ifnγ mRNA followed by CXCL9 protein expression, which preceded the increased recruitment of IFN-γ expressing NK and T cells with IL-15c treatment. These data identify the capacity of IL-15 to mediate Ifnγ expression and lymphocyte responses independently of type I IFN signalling in vivo.
A key question is how does IL-15c restore NK and Th1 cell responses during RV infection in the absence of ISG expression? Especially since many lymphocyte recruiting chemokines such as CXCL10 are induced by type I IFN signalling, which are deficient in RV infected IFNAR1−/− mice 10. This raises the possibility that the IL-15c-augmented early IFN-γ expression induced production of non-type I IFN-dependant chemokines which could recruit NK and T cells to the lung. CXCL9, CXCL10 and CXCL11 all bind CXCR3 on NK cells and CD4+ and CD8+ T cells to mediate chemotaxis to sites of inflammation. Although originally described as interferon gamma-inducible protein 10 (IP-10), IL-15c treatment failed to induce CXCL10 production in IFNAR1−/− mice (despite robust Ifnγ expression) whilst RV-induced expression was further boosted in wt mice suggesting that CXCL10 is dependent on type I rather than type II IFNs. In contrast, we observed robust expression of CXCL9 (originally identified as monokine induced by gamma interferon) in both wt and IFNAR1−/− mice peaking at 24 h. The requirement of IFN-γ for CXCL9 expression has been observed during Klebsiella infection using IFN-γ knockout mice 34. Pertaining to lung responses, treatment of cultured human bronchial epithelial cells with IFN-γ induced CXCL9 expression 35. We suggest that the early induction of Ifnγ gene expression in the lung, potentially stimulated by the combination of RV infection/TLR activation signals in conjunction with enhanced IL-15c stimulation of resident DCs and macrophages, was critical to recruitment of IFN-γ expressing NK cells and T cells via enhanced expression of CXCL9. We have previously demonstrated that human macrophages infected with RV in vitro produce IFN-γ 30. This is the first report to our knowledge demonstrating RV infection in vivo induces expression of CXCL9 in the airways, which is potentially the critical CXCR3 binding chemokine necessary for recruitment of NK cells and CD8+ T cells to lungs/airway. IL-15 is also reported to have direct chemotactic effects on NK cells and CD8+ T cells as demonstrated by migration through transwell systems to IL-15 supplemented media 36,37. The increased numbers of NK cells observed following exogenously administered IL-15 may have also been a result of proliferation within the lung as IL-15 has been reported to stimulate NK cell proliferation during cytomegalovirus and influenza infection22,37.
IL-15c augmented expression of ISGs (OAS1, PKR and CXCL10) in wt mice during RV infection which we suspect was via increased signalling from the type I IFN receptor. However whilst Ifnβ mRNA was increased BAL IFN-β protein levels were not, and BAL IFN-α protein was actually lower in the IL-15c treated group. This was potentially due to increased type I IFN receptor expression with IL-15c treatment resulting in increased ligand binding and less free detectable IFN in the BAL. This hypothesis is supported by the increased BAL type I IFN proteins observed in IL-15c/RV treated IFNAR1−/− mice. One study has reported the capacity of IL-15 to induce IFN-β expression in macrophages in vitro 38, whilst another report described IL-15 induced type I IFN by cultured human DCs 39. IL-15c treatment also augmented type III IFN production independently of type I IFN signalling. This study is the first to demonstrate that IL-15 treatment can augment IFN and ISG expression during a viral infection in vivo. Although IL-15c treatment could boost ISG expression via increased type I IFN signalling, the increased endogenous Il15 and Il15rα expression detected also occurred in the absence of type I IFN signalling, suggesting that IL-15 was capable of increasing its own expression and signalling independently of type I IFN. Boosted expression of IL-15 and its receptor, in conjunction with endosomal recycling of membrane bound IL-15-IL-15Rα complexes which allows longer and persistent IL-15 signalling 40,41 could contribute to the enhanced lymphocyte responses and cytokine and chemokine expression detected in IL-15c treated mice.
Our data provides novel insight into the immune response to RV infection providing first in vivo evidence of the importance of IL-15 for NK cell, CD8+ T cell and CD4+ T cell responses to RV infection. In addition we have identified a novel function for IL-15 in augmenting anti-viral IFN-γ expression and lymphocyte responses independently of type I IFNs. Our data suggests that boosting NK and CD8+ T cell responses during RV infection in healthy subjects is unlikely to provide substantial benefit as the virus is efficiently cleared without causing disease. In the case of asthma exacerbations, RV infection can augment lung inflammation driven by type-2 immunity. In this case we would predict that increasing IFN-γ production by recruitment of IL-15-activated NK and CD8+ T cells may inhibit production of type-2 cytokines and associated immunopathological responses such as airway hyper-reactivity and mucus secretion. Asthmatic bronchial epithelial cells also exhibit deficient anti-viral responses and are more permissive for viral replication27. Boosting anti-viral cellular responses may also compensate for this asthma-associated immune defect. Our data supports the view that therapeutic administration of IL-15c during asthma exacerbations would be the most beneficial approach with the important caveat that therapeutic administration of IL-15c has the potential to induce exaggerated type-1 immune responses with excessive IFN-γ production and associated airways inflammation 42. Thus IL-15c must be developed and used with caution. This could be achieved by detailed titration studies to identify a dose range that stimulates type-1 immunity that is sufficient for better control of viral infections and suppression of type-2-driven inflammation and results in a net reduction in airways inflammation and disease.
Materials and Methods
Human experimental rhinovirus infection and measurement of nasal cytokines
Two cohorts of eleven healthy, non-smoking volunteers with no history of asthma or respiratory disease, negative skin prick tests, no evidence of bronchial hyper-reactivity (PC20 >8 mg/mL) and no cold in the last 6 weeks were entered in this study. Infection was induced with rhinovirus serotype 16 via nasal spray into both nostrils 30. For one cohort, nasal responses were measured. Prior to RV infection (baseline) and at days 2, 3, 4, 5, 7 and 10 post inoculation the Nasosorption™ technique 43-45 was used to sample soluble mediators in the nasal mucosa. IL-15 was measured using the Meso-Scale Discovery (MSD) platform (sensitivity of <0.6 pg/ml). The second cohort has been described previously 30. Bronchial biopsies were obtained at baseline (two week prior to infection) and at day 4 after infection.
Mouse rhinovirus infection
IL-15Rα−/− mice on a B6.129 background, B6.129 control mice (both purchased from the Jackson Laboratory, USA) and IFNAR1−/− mice on a C57BL/6 background were bred in house under specific pathogen-free conditions. Balb/c and C57BL/6 control mice were purchased from Harlan (Harlan-Sprague-Dawley, UK). Rhinovirus sertotype 1B (RV-1B) obtained from the American Type Culture Collection was grown in HeLa cells (European Collection of Cell Cultures) and purified for in vivo use as previously described 9. The virus was inactivated by exposure to UV light at 1,200mJ/cm2 for 30 min. Mice were lightly anaesthetised with isofluorane and infected intra-nasally (i.n.) with 50 μL of RV-1B (5×106 TCID50) or PBS (mock-infected represented as 0 h in time course studies. All mouse experiments were performed using 6-8 week old mice, and only female mice were used in studies involving wt Balb/c, wt B6.129 and IL-15Rα−/− mice, and males and females were used in studies involving wt C57BL/6 and IFNAR1−/− mice.
Anti-IL-15 antibody and IL-15 complex treatment
Balb/c mice were treated i.n. with 20 μg of an IL-15 neutralising antibody (M96, Amgen Inc.), or mouse IgG2a isotype control (R&D Systems) at the time of infection (0 h) and 24 h after infection. In other studies IFNAR1−/− and C56BL/6 control mice were treated i.n. with 1.5 μg IL-15 complexed to IL-15Rα (IL-15c) (eBiosciences) at the time of infection.
Cytokine ELISA
For BAL fluid, ELISAs for mouse IFN-α, IFN-β, IFN-λ2/3 (IL-28A/B), CXCL9 and CXCL10 (R&D Systems, Abingdon, UK). The right azygous, cardiac and diaphramic lung lobes were excised post-BAL and homogenised in PBS with EDTA-free protease cocktail inhibitor (Roche); the clarified supernatant after centrifugation was used for IL-15 (R&D Systems, Abingdon, UK) and IL-15c (eBiosciences) ELISAs according to the manufacturers recommended protocol.
TaqMan quantitative real-time PCR (qPCR)
The mouse apical lung lobe was excised and stored in RNA later (Qiagen) prior to total RNA extraction (RNeasy miniprep kit, Qiagen), and 5 μg of RNA was reverse-transcribed for cDNA synthesis using random hexamers as primers (Omniscript RT kit, Qiagen). RNA from BAL cells was also extracted and converted to cDNA by the same process. Quantitative PCR was conducted using primers and probes specific to each gene analysed, using an ABI 7500 TaqMan (ABI Foster City, CA, USA). Each gene was normalised to 18s rRNA and expressed as mRNA copies per μL of cDNA reaction, quantified by a standard curve from amplified plasmid DNA standards.
Immunohistochemistry
Human bronchial biopsies were embedded in Tissue Tek II OCT, frozen within 15 min in isopentane pre-cooled in liquid nitrogen, and stored at −80°C. The best frozen sample was then oriented and 6μm thick cryostat sections were cut for immunohistochemical light microscopy analysis. After blocking non-specific binding, 1.3 μg/mL mouse anti-human IL-15 (Santa Cruz Biotechnology sc-73311) were applied for 1 h at room temperature in a humidified chamber. As positive control we have used human nasal polyps and these were used for negative control slides which were treated with normal mouse non-specific immunoglobulins (Santa Cruz Biotechnology). After repeated washing steps with TBS, the sections were subsequently incubated with horse anti-mouse biotinylated antibody (Vectastain Elite ABC Kit, Vector Laboratories) for 30 min at room temperature. After further washing the sections were subsequently incubated with ABC reagent (Vectastain Elite ABC Kit, Vector Laboratories) for 30 min at room temperature. Slides were then incubated with chromogen-fast diaminobenzidine (DAB) as a chromogenic substance, after which they were counterstained in haematoxylin and mounted on aqueous mounting medium.
Single IHC staining of mouse lung sections from formalin-fixed paraffin-embedded mouse lungs was performed as previously described 10. After blocking slides (5% rabbit serum) goat anti mouse IL-15 (RnD Systems AF447) was applied at 4 μg/mL. For the negative control slides normal goat non-specific immunoglobulins (Santa Cruz Biotechnology) were used. The intensity and distribution of positive staining in human biopsies and mouse lung sections was evaluated using a standard four point scale, with sections being scored as 0,1, 2 or 3 according to a validated method 46.
Flow cytometry
The left lung lobe was excised post BAL, crudely dissociated using the GentleMACS™ tissue dissociator (Miltenyi Biotech, Germany) and digested upon incubation at 37°C in buffer containing 1 mg/mL collagenase Type XI and 80 units/mL Bovine Pancreatic DNase Type IV (both Sigma-Aldrich, Dorset, UK). For intracellular cytokine staining (ICS) cells were stimulated with PMA (50 ng/mL) and ionomycin (500 ng/mL) with BD GolgiStop™ (BD Biosciences) for 3 h at 37°C. Lung and BAL cells were incubated with anti-mouse CD16/CD32 (FC Block, BD Biosciences) prior to staining for cell surface markers: CD3e (clone 500A2), CD4 (clone RM4-5), CD8a (clone 53-6.7), NK1.1 (clone PK136), NKp46 (clone 29A1.4) and CD69 (clone H1.2F3) (all BD Biosciences). Cells were washed and stained with Live/Dead fixable dead cell stain kit (Invitrogen), followed by incubation with BD Fix/Perm solution (BD Biosciences). For ICS, cells were stained for IFN-γ (clone XMG1.2, BD Biosciences) and granzyme B (clone GB12, Invitrogen) in BD PermWash™ (BD Biosciences). Data were acquired using a BD LSR II digital flow cytometer (BD Biosciences) and BD FACS Diva software. Analysis was performed using FlowJo 9.3.1.2 software.
Statistical Analyses
For human studies, IL-15 data are presented as mean (±SEM). Comparing baseline and infection peak data were analysed by Mann-Whitney test. Correlations between data sets were examined using Spearman’s rank correlation coefficient for nonparametric data. Differences were considered significant for all statistical tests at p< 0.05. All reported P values are two-sided. Animal experiments involved 4-7 mice per group in up to 3 independent experiments. Data were analysed using two-way ANOVA and Bonferroni’s multiple comparison test. All statistics were calculated using Prism 4 software (Graphpad, USA), with p< 0.05 taken as significant.
Study approval
The human infection studies were approved by St Mary’s National Health Service Trust Research Ethics committee. All subjects gave written informed consent. All animal work was completed in accordance with UK Home Office guidelines following approval via the ethical approval process (UK project licence PPL 70/7234).
Supplementary Material
Acknowledgements
We would like to thank Eric Butz (Amgen, Seattle, USA) for providing the IL-15 neutralising antibody and Cecilia Johansson (Imperial College London, UK) for providing IFNAR1−/− mice.
This work was supported by a Chair from Asthma UK (CH11SJ), MRC Centre Grant G1000758, ERC FP7 Advanced grant 233015, Predicta FP7 Collaborative Project grant 260895 and the Wellcome Trust sponsored Centre for Respiratory Infection (CRI).
Footnotes
Disclosure
The authors declare no competing financial interests.
Conflict of interests
The authors’ have no conflicts of interest to declare.
References
- 1.Gerna G, et al. Correlation of rhinovirus load in the respiratory tract and clinical symptoms in hospitalized immunocompetent and immunocompromised patients. J Med Virol. 2009;81:1498–1507. doi: 10.1002/jmv.21548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papadopoulos NG, et al. Rhinoviruses infect the lower airways. J Infect Dis. 2000;181:1875–1884. doi: 10.1086/315513. [DOI] [PubMed] [Google Scholar]
- 3.Johnston NW. The similarities and differences of epidemic cycles of chronic obstructive pulmonary disease and asthma exacerbations. Proc Am Thorac Soc. 2007;4:591–596. doi: 10.1513/pats.200706-064TH. [DOI] [PubMed] [Google Scholar]
- 4.Choi SH, et al. Viral infection in patients with severe pneumonia requiring intensive care unit admission. Am J Respir Crit Care Med. 2012;186:325–332. doi: 10.1164/rccm.201112-2240OC. [DOI] [PubMed] [Google Scholar]
- 5.Bertino JS. Cost burden of viral respiratory infections: issues for formulary decision makers. The American Journal of Medicine. 2002;112:42–49. doi: 10.1016/s0002-9343(01)01063-4. [DOI] [PubMed] [Google Scholar]
- 6.Spurrell JC, Wiehler S, Zaheer RS, Sanders SP, Proud D. Human Airway Epithelial Cells Produce Ip-10 (Cxcl10) in Vitro and in Vivo Upon Rhinovirus Infection. Am J Physiol Lung Cell Mol Physiol. 2005;289:85–95. doi: 10.1152/ajplung.00397.2004. [DOI] [PubMed] [Google Scholar]
- 7.Fraenkel DJ, et al. Lower airways inflammation during rhinovirus colds in normal and in asthmatic subjects. Am J Respir Crit Care Med. 1995;151:879–886. doi: 10.1164/ajrccm/151.3_Pt_1.879. [DOI] [PubMed] [Google Scholar]
- 8.Levandowski RA, Ou DW, Jackson GG. Acute-phase decrease of T lymphocyte subsets in rhinovirus infection. J Infect Dis. 1986;153:743–748. doi: 10.1093/infdis/153.4.743. [DOI] [PubMed] [Google Scholar]
- 9.Bartlett NW, et al. Mouse models of rhinovirus-induced disease and exacerbation of allergic airway inflammation. Nat Med. 2008;14:199–204. doi: 10.1038/nm1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartlett NW, et al. Defining critical roles for NF-kappaB p65 and type I interferon in innate immunity to rhinovirus. EMBO Mol Med. 2012;4:1244–1260. doi: 10.1002/emmm.201201650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mattei F, Schiavoni G, Belardelli F, Tough DF. IL-15 is expressed by dendritic cells in response to type I IFN, double-stranded RNA, or lipopolysaccharide and promotes dendritic cell activation. J Immunol. 2001;167:1179–1187. doi: 10.4049/jimmunol.167.3.1179. [DOI] [PubMed] [Google Scholar]
- 12.Hansen ML, et al. IFN-alpha primes T- and NK-cells for IL-15-mediated signaling and cytotoxicity. Mol Immunol. 2011;48:2087–2093. doi: 10.1016/j.molimm.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Rochman Y, Spolski R, Leonard WJ. New insights into the regulation of T cells by gamma(c) family cytokines. Nat Rev Immunol. 2009;9:480–490. doi: 10.1038/nri2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giri JG, et al. Utilization of the beta and gamma chains of the IL-2 receptor by the novel cytokine IL-15. EMBO J. 1994;13:2822–2830. doi: 10.1002/j.1460-2075.1994.tb06576.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giri JG, et al. Identification and cloning of a novel IL-15 binding protein that is structurally related to the alpha chain of the IL-2 receptor. EMBO J. 1995;14:3654–3663. doi: 10.1002/j.1460-2075.1995.tb00035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stonier SW, Schluns KS. Trans-presentation: a novel mechanism regulating IL-15 delivery and responses. Immunol Lett. 2010;127:85–92. doi: 10.1016/j.imlet.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGill J, Van Rooijen N, Legge KL. IL-15 trans-presentation by pulmonary dendritic cells promotes effector CD8 T cell survival during influenza virus infection. J Exp Med. 2010;207:521–534. doi: 10.1084/jem.20091711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leavy O. Maturation and function of NK cells. Nat Rev Immunol. 2012;12:150. doi: 10.1038/nri3172. [DOI] [PubMed] [Google Scholar]
- 19.Biron CA, Nguyen KB, Pien GC, Cousens LP, Salazar-Mather TP. Natural killer cells in antiviral defense: function and regulation by innate cytokines. Annu Rev Immunol. 1999;17:189–220. doi: 10.1146/annurev.immunol.17.1.189. [DOI] [PubMed] [Google Scholar]
- 20.Trinchieri G, Santoli D. Anti-viral activity induced by culturing lymphocytes with tumor-derived or virus-transformed cells. Enhancement of human natural killer cell activity by interferon and antagonistic inhibition of susceptibility of target cells to lysis. J Exp Med. 1978;147:1314–1333. doi: 10.1084/jem.147.5.1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee Ck, Fau - Rao DT, et al. Distinct requirements for IFNs and STAT1 in NK cell function. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen KB, et al. Coordinated and distinct roles for IFN-alpha beta, IL-12, and IL-15 regulation of NK cell responses to viral infection. J Immunol. 2002;169:4279–4287. doi: 10.4049/jimmunol.169.8.4279. [DOI] [PubMed] [Google Scholar]
- 23.Kennedy MK, et al. Reversible defects in natural killer and memory CD8 T cell lineages in interleukin 15-deficient mice. J Exp Med. 2000;191:771–780. doi: 10.1084/jem.191.5.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lodolce JP, et al. IL-15 receptor maintains lymphoid homeostasis by supporting lymphocyte homing and proliferation. Immunity. 1998;9:669–676. doi: 10.1016/s1074-7613(00)80664-0. [DOI] [PubMed] [Google Scholar]
- 25.Vankayalapati R, et al. NK cells regulate CD8+ T cell effector function in response to an intracellular pathogen. J Immunol. 2004;172:130–137. doi: 10.4049/jimmunol.172.1.130. [DOI] [PubMed] [Google Scholar]
- 26.Ge MQ, et al. NK cells regulate CD8+ T cell priming and dendritic cell migration during influenza A infection by IFN-gamma and perforin-dependent mechanisms. J Immunol. 2012;189:2099–2109. doi: 10.4049/jimmunol.1103474. [DOI] [PubMed] [Google Scholar]
- 27.Wark PA, et al. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med. 2005;201:937–947. doi: 10.1084/jem.20041901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mallia P, et al. Experimental rhinovirus infection as a human model of chronic obstructive pulmonary disease exacerbation. Am J Respir Crit Care Med. 2011;183:734–742. doi: 10.1164/rccm.201006-0833OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laza-Stanca V, et al. The role of IL-15 deficiency in the pathogenesis of virus-induced asthma exacerbations. PLoS Pathog. 2011;7:e1002114. doi: 10.1371/journal.ppat.1002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Message SD, et al. Rhinovirus-induced lower respiratory illness is increased in asthma and related to virus load and Th1/2 cytokine and IL-10 production. Proc Natl Acad Sci U S A. 2008;105:13562–13567. doi: 10.1073/pnas.0804181105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Newcomb DC, et al. Human rhinovirus 1B exposure induces phosphatidylinositol 3-kinase-dependent airway inflammation in mice. Am J Respir Crit Care Med. 2008;177:1111–1121. doi: 10.1164/rccm.200708-1243OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papadopoulos NG, Sanderson G, Hunter J, Johnston SL. Rhinoviruses replicate effectively at lower airway temperatures. J Med Virol. 1999;58:100–104. doi: 10.1002/(sici)1096-9071(199905)58:1<100::aid-jmv16>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 33.Lambrecht BN, Hammad H. Lung dendritic cells in respiratory viral infection and asthma: from protection to immunopathology. Annu Rev Immunol. 2012;30:243–270. doi: 10.1146/annurev-immunol-020711-075021. [DOI] [PubMed] [Google Scholar]
- 34.Zeng X, et al. Interferon-inducible protein 10, but not monokine induced by gamma interferon, promotes protective type 1 immunity in murine Klebsiella pneumoniae pneumonia. Infect Immun. 2005;73:8226–8236. doi: 10.1128/IAI.73.12.8226-8236.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sauty A, et al. The T cell-specific CXC chemokines IP-10, Mig, and I-TAC are expressed by activated human bronchial epithelial cells. J Immunol. 1999;162:3549–3558. [PubMed] [Google Scholar]
- 36.Verbist KC, Cole CJ, Field MB, Klonowski KD. A role for IL-15 in the migration of effector CD8 T cells to the lung airways following influenza infection. J Immunol. 2011;186:174–182. doi: 10.4049/jimmunol.1002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Verbist KC, Rose DL, Cole CJ, Field MB, Klonowski KD. IL-15 participates in the respiratory innate immune response to influenza virus infection. PLoS One. 2012;7:e37539. doi: 10.1371/journal.pone.0037539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu G, et al. IL-15 induces IFN-beta and iNOS gene expression, and antiviral activity of murine macrophage RAW 264.7 cells. Immunol Lett. 2004;91:171–178. doi: 10.1016/j.imlet.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 39.Jinushi M, et al. Autocrine/paracrine IL-15 that is required for type I IFN-mediated dendritic cell expression of MHC class I-related chain A and B is impaired in hepatitis C virus infection. J Immunol. 2003;171:5423–5429. doi: 10.4049/jimmunol.171.10.5423. [DOI] [PubMed] [Google Scholar]
- 40.Sato N, Patel HJ, Waldmann TA, Tagaya Y. The IL-15/IL-15Ralpha on cell surfaces enables sustained IL-15 activity and contributes to the long survival of CD8 memory T cells. Proc Natl Acad Sci U S A. 2007;104:588–593. doi: 10.1073/pnas.0610115104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dubois S, Mariner J, Waldmann TA, Tagaya Y. IL-15Ralpha recycles and presents IL-15 In trans to neighboring cells. Immunity. 2002;17:537–547. doi: 10.1016/s1074-7613(02)00429-6. [DOI] [PubMed] [Google Scholar]
- 42.Sugimoto T, et al. Interleukin 18 acts on memory T helper cells type 1 to induce airway inflammation and hyperresponsiveness in a naive host mouse. J Exp Med. 2004;199:535–545. doi: 10.1084/jem.20031368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chawes BL, et al. A novel method for assessing unchallenged levels of mediators in nasal epithelial lining fluid. J Allergy Clin Immunol. 2010;125:1387–1389. e1383. doi: 10.1016/j.jaci.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 44.Nicholson GC, et al. The effects of an anti-IL-13 mAb on cytokine levels and nasal symptoms following nasal allergen challenge. J Allergy Clin Immunol. 2011;128:800–807. e809. doi: 10.1016/j.jaci.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 45.Folsgaard NV, et al. Neonatal cytokine profile in the airway mucosal lining fluid is skewed by maternal atopy. Am J Respir Crit Care Med. 2012;185:275–280. doi: 10.1164/rccm.201108-1471OC. [DOI] [PubMed] [Google Scholar]
- 46.Varani K, et al. Alteration of adenosine receptors in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:398–406. doi: 10.1164/rccm.200506-869OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.