Abstract
Indian data on epidemiology of HCC is not available. Cancer is not a reportable disease in India and the cancer registries in India are mostly urban. National cancer registry program of the Indian Council of Medical Research (ICMR) has been recently expanded to include 21 population based and 6 hospital based cancer registries. The last published registry data by ICMR available in the cancer registry website (www.ncrpindia.org) was in 2008 which provides information on various cancers from 2006 to 2008. The other source of information was the report published by International Agency for Research on Cancer (WHO). According to these available data the age adjusted incidence rate of hepatocellular carcinoma (HCC) in India for men ranges from 0.7 to 7.5 and for women 0.2 to 2.2 per 100,000 population per year. The male:female ratio for HCC in India is 4:1. The age of presentation varies from 40 to 70 years. According to a study conducted by verbal autopsy in 1.1 million homes representing the whole country, the age standardized mortality rate for HCC in India for men is 6.8/100,000 and for women is 5.1/100,000. According to another study the incidence of HCC in cirrhotics in India is 1.6% per year. The unpublished data from various tertiary care centers suggest that the incidence of HCC is increasing in India. There is a need for a multi-centric HCC registry under the aegis of INASL.
Keywords: epidemiology, HCC, India
Abbreviations: AAIR, age adjusted incidence rate; ASMR, age standardized mortality rate; HBCR, hospital based cancer registry; HCC, hepatocellular carcinoma; IARC, international agency for cancer research; ICMR, Indian Council of Medical Research; PBCR, population based cancer registry
Hepatocellular carcinoma (HCC) is the most frequent cause of all liver cancers and constitutes 90% of cancers of liver globally.1 Even though cancers of lungs, breast and large intestine have been identified as three most common cancers, the three leading causes of annual death due to cancers include lungs, stomach and liver.1 Approximately 7.5 Lakhs of new cases of HCC per year occurs globally which makes HCC as the 5th common cause of cancers effecting human.1 The mortality in HCC is very high; about 7 Lakhs death due to HCC occur annually and has been estimated to be 3rd common cause of death due to cancers effecting human.1
In India, information on HCC is inadequate. From 1988 till December 2012, over two and half decades only 68 publications have been listed in the PUBMED, all from tertiary care center, on select areas and most studies included small samples. The cancer registries in India probably do not provide accurate estimates of HCC prevalence due to its predominant urban locations and the source of information on cancers are from cytology, oncology sites, and municipal registers of death. HCC predominantly is diagnosed and treated by Gastroenterologists/Hepatologist/Transplant Surgeons/G.I. Surgeons. These patients treated by the later doctors are presumably are not being listed in the registries. Further, the diagnosis of hepatocellular cancer is achieved frequently by non-invasive imaging technique rather than by histology/cytological techniques as used in almost all other cancers. Therefore the collated informations from oncology/cytology/pathology departments may not be having the records of a considerable proportion of HCC cases. Lastly cancers are not reportable disease in India.
With these limitations, the specific issues which this review intend to do includes the following:
-
1.
How common is HCC in India?
-
2.
Status of reporting of HCC to cancer registries in India?
-
3.
HCC burden in tertiary care centers?
-
4.
Causes of mismatch of documented and likely actual burden.
-
5.
Regional differences in HCC burden in India.
How common is hepatocellular carcinoma in India?
The source of information to assess the frequency of occurrence of HCC in India includes autopsy data, cancer registries and population based surveillance data.
Autopsy Data
The prevalences of HCC described in autopsy series from India are very old and were published between 1966 to 1982.2,3 The autopsy data has been published earlier by Dhir and Mohandas in 1998,3 which is depicted in Table 1.
Table 1.
Autopsy Data on HCC in India.
| Place | Autopsies (No.) | HCC (%) |
|---|---|---|
| India | ||
| • Mumbai | 6000 | 0.2 |
| • Mumbai | 4000 | 0.2 |
| • Agra | 1234 | 0.7 |
| • Guntur | 629 | 1.1 |
| • Andhra Pradesh | 2789 | 1.6 |
| • Chennai | 1218 | 1.9 |
| Bangladesh | 5450 | 0.2 |
| Denmark | 14881 | 0.3 |
| USA (Boston) | 14000 | 0.6 |
| Japan | 401,381 | 3.1 |
| Hong Kong | 1480 | 6.8 |
The autopsy data reveals that 0.2–1.9% of autopsy cases had HCC with a higher prevalence of HCC in South-eastern states of India. However, these information have been replaced by cancer registry data in India.
Cancer Registry Data
National cancer registry program was established by Indian Council of Medical Research (ICMR) in 1981.4 Initially, three hospital-based cancer registries (HBCRs) and three population-based cancer registries (PBCRs) were established. By now, 21 PBCRs and 6 HBCRs have been established. The last published registry data by ICMR available in the cancer registry website (ncrpindia.org) was in 2008 which provides information on various cancers from 2006 to 2008. The present write-up includes the information retrieved from this later report to provide the recent trends of HCC in India, which has been depicted in Table 2.
Table 2.
Population Based Cancer Registry (PBCR), ICMR (ncrpindia.org). (Report on First 20 PBCR in India (2006–2008)—25 Geographical Area Population 3.81 Lakhs–156 Lakhs: Mizoram/Delhi, [1st Jan 2006–31st December 2008].
| PBCRs | Population | Total cancer | Liver cancer | CR | AAIR | Comment |
|---|---|---|---|---|---|---|
| Bangalore | 6,892,642 | 12624 | Not in 10 leading causes | 2.2 | 4.5 | |
| Barshi | 4,855,549 | 4308 | 7.5%* (1st common) | 3.5* | 4.7* | Males F X |
| Bhopal | 1,812,045 | 39757 | X (not in 10) | – | – | |
| Chennai | 4,695,780 | 15258 | X | 1.2 | 2.1 | |
| Delhi | 16,501,678 | 26333 | 1.07–2% | 1.5 | 2.6 | |
| Mumbai | 13,494,514 | 33230 | 4.9% (6th common) | 3.4 | 5.2 | F X |
| Cachar | 1,626,339 | 2539 | 2.1% (10th common) | 2.0 | 2.8 | |
| Dibrugarh | 1,285,538 | 2521 | X | – | – | |
| Kamrup | 1,117,804 | 3256 | X | – | – | |
| Manipur | 2,436,500 | 3969 | 4.4% (6th common) | 2.3 | 3.1 | F X |
| Mizoram | 1,043,775 | 3380 | 3.8% (5th common) | 4.3 | 6.4 | |
| Sikkim | 648,806 | 1155 | 8% (4th common) | 4.7 | 7.5 | |
| Ahmedabad | 6,313,384 | 11844 | X | 1 | 1.7 | |
| Aurangabad | 1,119,142 | 1888 | X | – | – | |
| Kolkata | 4,677,682 | 9038 | X | – | – | |
| Kollam | 2,704,837 | 9030 | 3.7% (8th common) | 4.5 | 4.1 | F X |
| Nagpur | 2,322,117 | 5422 | X | 1.4 | 2.2 | |
| Pune | 4,676,184 | 8594 | 4.5% (10th common) | 2.5 | 3.8 | F X |
| Trivandrum | 1,160,104 | 5755 | 3.6% (9th common) | 4.6 | 4.5 | F X |
| Basis of diagnosis | 61–94% | At various center by tissue diagnose | ||||
| 0.2–20% | Radiology | |||||
| <10% | Other method | |||||
NB: 4.8% of all cancers are liver cancer.
Male preponderance in all center.
8/20 PBCR–do not list liver cancer in the first 10 causes of cancer.
Median age—40 year to 70 years.
With increasing age—Numbers of liver cancer higher.
The summary interpretations of data depicted in ICMR cancer registry are as follows:
-
a)
In 8 of the 23 PBCRs HCC was not included in the first 10 common cancers and in all these centers the age adjusted incidence rate (AAIR) of HCC/100,000 population was between 1 and 1.5. In the remaining PBCRs the AAIR ranged from 2.1 to 7.5 per 100,000 population.
The AAIR for HCC for men ranged from 0.9 to 7.5 and for women it ranged from 0.2 to 2.2 per 100,000 population. The highest AAIR was reported from Sikkim and Mizoram (Table 2). However at Barshi, HCC constituted 7.5% of all cancer and was the most common cause of all cancers recorded in the cancer registry. Table 3 provides the AAIR of HCC in various cancer registries in India as depicted by WHO,5 which was updated in 2011 and provides similar data on frequency of HCC in India.
Table 3.
AAIR of HCC in India (IARC–WHO).5
| Male |
Female |
|||||
|---|---|---|---|---|---|---|
| Cases | ASR | Cum | Cases | ASR | Cum | |
| Chennai | 269 | 3.0 | 0.37 | 83 | 0.9 | 0.10 |
| New Delhi | 491 | 2.4 | 0.28 | 232 | 1.3 | 0.16 |
| Karunagappally | 34 | 3.9 | 0.43 | 8 | 0.8 | 0.10 |
| Mumbai | 895 | 4.5 | 0.56 | 433 | 2.2 | 0.25 |
| Nagpur | 65 | 1.6 | 0.19 | 35 | 0.9 | 0.10 |
| Poona | 209 | 3.4 | 0.41 | 88 | 1.4 | 0.15 |
| Trivandrum | 78 | 2.8 | 0.32 | 30 | 1.0 | 0.12 |
International Agency for Research on Cancer (IARC–WHO).
Age–standardized (per 100,000) and cumulative 0–74 incidence (%) rates http://Ci5.iarc.fr.
IARC–WHO data indicate that Africa and East Asia has the highest frequency of HCC globally with an AAIR of 14–36 per 100,000 people and account for approximately 80% of HCC globally.5,6
-
b)
As per cancer registry data,4 4–8% of the cancers were due to HCC in at least 13 of 21 PBCRs. At these centers males predominantly had been documented to have HCC with a M:F at 4:1 and the median age ranged from 40 to 70 and the frequency of liver cancers seems to be higher with increasing age.
-
c)
To assess trend of frequency of digestive tract cancer Yeole et al analyzed PBCRs in five sites (Mumbai, Bangalore, Chennai, Delhi and Bhopal) over almost two decades (1980–2003).7
The annual percentage change in AAIR for Gut and liver cancer is depicted in Table 4.
Table 4.
Annual Percentage Change in Age Adjusted Incidence Rates for Gut and Liver Cancer.
| Registry | Esophagus | Stomach | Colon | Rectum | Liver |
|---|---|---|---|---|---|
| Mumbai | −2.91** | −2.45** | 0.64NS | 0.17NS | 1.74** |
| Chennai | 1.12* | −0.98* | 2.07** | 2.39** | 0.25* |
| Bangalore | 0.13NS | −0.74NS | 2.08* | 1.69* | 1.54* |
| Delhi | −1.36* | −1.57* | 1.71* | −0.36NS | 1.32NS |
| Bhopal | 1.24NS | −6.13* | 2.79NS | 2.75NS | 2.10NS |
NS—Not significant, *p < 0.05, **p < 0.01.
The Table 4 indicates that there is a significant increase in liver cancer frequency in Mumbai, Chennai and Bangalore cancer registry over two decades.
Without visible control strategy for HCC, this trend of increase in frequency of occurrence of HCC is likely to continue. Indeed, in 1998 ICMR cancer registry from all sites documented 10,000 HCC cases.4 In 2002, IARC collated data and reported 13,630 HCC cases from India.5 In 2009, ICMR cancer registries have documented 25,000 cases of HCC. This would indicates that either HCC frequency is increasing or are being diagnosed more often.
IF approximately we presume that AAIR for HCC in India is about 3–5/100,000 population annually, than in a year, approximately 30,000 to 50,000 HCC would be occurring in India.
Population Based Surveys
Hepatocellular Carcinoma Related Mortality in General Population
Dixit et al8 published an important population based survey to identify the cancer related mortality in India.8 The study was conducted by verbal autopsy study in 1.1 million homes representing the whole country. People who died between 2001 and 2003 were included in the study and the deaths were projected for year 2010. For both sexes and all ages 122,429 deaths occurred in 2001–2003 and 7137 of these were attributable to cancers. In 2010, more than 556,000 cancer deaths were estimated in people of all ages and 72% of these deaths were between 30 and 69 years. In 2010 at all ages, rates of cancer deaths about 59/100,000 for men and about 52/100,000 for women. Among men, the first four causes of mortality included oral, stomach, lung and liver cancer. In 2010 approximately 14,000 deaths would have occurred due to liver cancer with an age standardized mortality rate (ASMR) of 6.8/100,000 population. In women liver cancer was the 8th common cause of cancer related mortality accounting for 12,000 death in 2010 with an ASMR of 5.1/100,000 population.
Incidence of Hepatocellular Carcinoma in High Risk Individuals
The well known high risk patient to develop HCC includes cirrhosis of liver of any cause.1 About 80% of HCC has been reported globally in cirrhotic livers.1 The frequency of HCC in a cirrhotic may vary depending upon underlying etiology of cirrhosis, such as HBV, HCV, alcohol and nonalcoholic fatty liver disease.9
Reports from tertiary care centers in India on HCC indicate that 70–97% of patients with HCC at the time of diagnosis had underlying cirrhosis of liver.10,11 Long term cohort follow-up studies from Europe and USA indicate that annual frequency of HCC in HBV-cirrhosis, HCV-cirrhosis and alcohol induced cirrhosis have been 2.2%, 3.8% and 1.7% respectively.12,13 The frequency of HCC occurrence is East Asian countries is further higher.14,15 These annual frequencies at HCC in HBV-cirrhosis may further vary as per their HBeAg status, HBV DNA load, age, sex and status of liver function.1,9,12–15
The ICMR cancer registries in India have documented low incidence of HCC on comparison to South East Asia, Japan and European countries, despite the fact that there are about 40–45 million HBV carrier, 10 million HCV infected individuals in India.
The discrepancy between higher prevalence of HCC risk factor and objective cancer registry data have been attributed to lower reporting by many. Further, prospective longitudinal study among cirrhotic cohorts, to document HCC incidence in India is scarce.
The only Indian study by Paul et al conducted a prospective observational study to assess the HCC incidence among patients with child's A and B cirrhotic without having any HCC at enrollment (n = 194) who were followed up for a median duration of 44 months.16 Each patient had ultrasonography and AFP at 6 month interval and TPCT annually. During a cumulative 563 person years follow-up nine cases of HCC (all males) were detected with an annual incidence rate of 1.6% (95% CI—0.07–3).16 The authors concluded that incidence rate of HCC among Indian patient with cirrhosis is intermediate between high rates in Japan for East and European countries.16
In absence of estimates of accurate burden of cirrhosis in India, the absolute number of HCC occurring in India in a year is difficult to assess. Mohandas et al discussed this issue in an editorial published in the Indian Journal of Gastroenterology in 2007.9 This editorial reported that even if HCC in HCV and alcohol associated HCC are ignored, and assuming that 45 million HBV infected individuals with a 15% presumable HBeAg+ve frequency and 0.01% annual HCC frequency, an over whelming 68,000 new HCC cases are likely to occur in India among HBV associated patients with chronic liver disease. However, the international agency for cancer research (IARC) had estimated 13,630 primary liver cancer in India (9153 males, 4477 females) in India in 2002. In contrast, the number of primary liver cancers from seven population based cancer registries included in the ‘Cancer incidence in five continents’ (Vol 9, 1998–2002) was 3023 during 179 million person years.9 Therefore at least there exists a fivefold difference between documented an estimated annual frequency of occurrence of HCC in India. The possible reasons of such discrepancy have been discussed later in the review.
Status of reporting hepatocellular carcinoma to cancer registries in India and causes of mismatch of documented and likely actual burden of hepatocellular carcinoma in India
As per the cancer registry website (ncrpindia.org) by now there are 23 population based cancer registries and 6 hospital cancer registries in India.
Each cancer registry has dedicated staff and electronic data collation capabilities. The information on site of cancers, death due to cancer and other etiological and demographic profile of each cancer are collated by visit of cancer registry staff to cytology, oncology, pathology department of the hospitals of the area designated for each cancer registries. The municipal death registers are also included as the source of information. These data are further supervised, cleaned and analyzed by supervisors and experts of each cancer registry site.
As mentioned earlier there exists a discrepancy between documented frequency of HCC in cancer registry and estimated likely frequency of HCC. The reason for such discrepancy may be due to many reasons. It is possible that actual burden of HCC in India may be lower. Mohandas et al9 had provided elegant explanation for documented lower incidence of HCC which are as follows.
Over Estimation of Hepatitis B Virus Infection in Indians
A systematic review of 54 Indian studies reported true prevalence of HBV infection in non-tribal and tribal populations to be 2.4% (95% CI—2.2–2.7) and 15.9% (95% CI—11.4–20.4) respectively.17 Therefore the estimated HCC due HBV annually may be between 25 and 35000 HCC cases per year. Further, a large proportion of HCC cases may be HBeAg–ve with low HBV DNA load which is associated with lower frequency of HCC.1
Average Life Span of Indians is Still 64 Years
The population based incidence of HCC peaks at 75 years. The incidence rate of HCC in 100,000 males by age groups 40–44, 50–54, 60–64 and 70–74 years are 1.6, 5.7, 12.9 and 22.6 respectively.5
In India Horizontal Transmission of Hepatitis B Virus is More Common
Vertical transmission more frequently documented in genotype B and C HBV, particularly in South East Asian countries which have been associated with high HCC incidence. In India, horizontal transmission of HBV infection with prevalence of HBV genotype A and D may be associated with lower incidence of HCC.
On the other hand it may be true that there is under reporting of HCC in the cancer registries. All the cancer registries in India indicate that most of the HCCs (61–95%) documented had histological/cytological basis for the diagnosis of HCC. However, HCC during last decade is diagnosed mostly by imaging technique and FNAC is only performed in select number of cases in whom imaging characteristics of HCC are not evident. Further, most HCCs are managed by Gastroenterologists/Hepatologists and there is doubtful evidence that these patients are reported to the cancer registries.
Burden of hepatocellular carcinoma in tertiary care center
There are four large case series reports from India emanating from various tertiary care centers in India which included total 952 cases.9,15,18,19 However, none of these case series have provided HCC burden data in details, nor has provided the year wise breakup to assess whether HCC burden is increasing in the tertiary care centers. In absence of collated data from multiple tertiary care center, we evaluated our own center data (unpublished). From 1990 to 2012, 1062 consecutive patients with confirmed diagnosis were registered at the liver clinic at the All India Institute of Medical Sciences, New Delhi. Figure 1 provides the number of HCC presented every year which indicate that, there is progressive risk of number of HCC cases at our center. From 2006 we have been registering about 100 HCC patients per year (see Figure 2–4). HCC cases at our center. Figure 2–4 depicts the age distribution, BCLC staging and etiology of the HCC respectively in these cases at our center. These data indicates that 55% of the patients with HCC presented at late age (>62 years). About half of the patients had BCLC stage A and B in whom definitive therapy could be offered and 65% (688/1062) of HCC were due to HBV and HCV.
Figure 1.
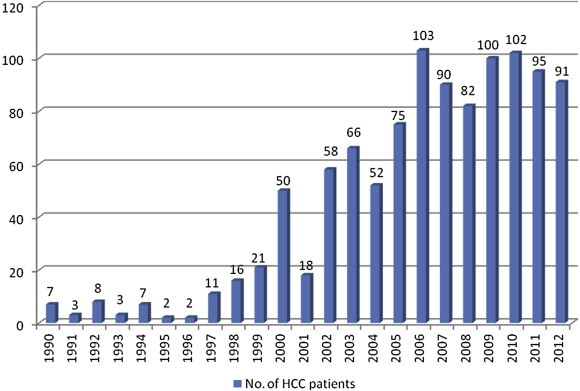
Year wise distribution of patients with HCC (AIIMS 1990–2012).
Figure 2.
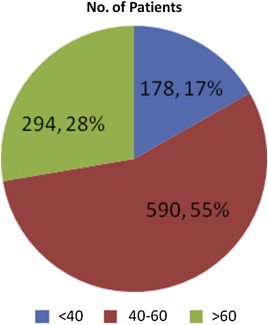
Age distribution of patients with HCC (AIIMS 1990–2012). The figure indicates that the age distribution and 55% of these 1062 patients were above the age 62 years at the time of diagnosis.
Figure 3.
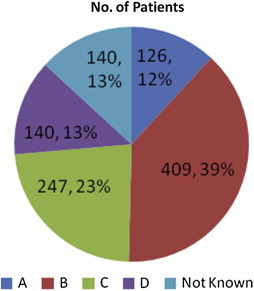
BCLC staging of HCC (AIIMS 1990–2012). The figure depicts the BCLC staging and indicates that more than 50% of HCC patients of presentation has BCLC-A and B staging which were offered treatment where as a equal proportion of patient had advanced stage (BCLC-C and D).
Figure 4.
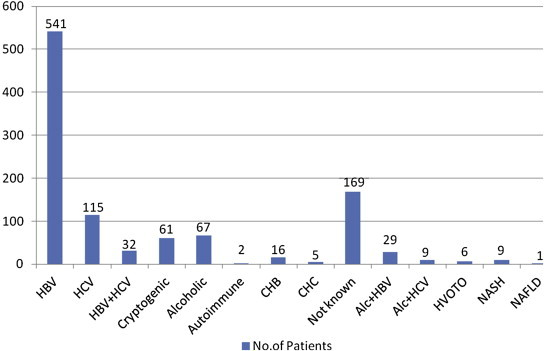
Etiology of HCC (AIIMS 1990–2012). The figure indicates the etiology of HCC in these 1062 patients which confirmed that HBV is the major cause of HCC in India as reported by other tertiary care centers from India.9,15,18,19
We had access to some information from Christian Medical College (CMC) Vellore, Tamil Nadu and Sir Ganga Ram Hospital (SRGH) Delhi. At CMC, Vellore, between December 2003 and 2010, 331 cases of HCC were registered, indicating that approximately 60 patients with HCC are registered annually at this center. Forty of these patients were offered therapy.
At SRGH, Delhi between January 2000 and December 2012,142 patients with HCC were registered. The BCLC staging in these patients indicate that 13% of the patients had BCLC-A, 23% had BCLC-B, 35% had BCLC-C and about 29% had BCLC-D. Eighty of these 142 patients were offered treatment.
Even though the information from tertiary center on HCC is limited, it seems that every tertiary care center registers about 50–60 HCC patients in a year. Approximately 320 tertiary care centers in India than would be registering approximately 16000 to 20,000 HCC cases in a year.
Regional differences on hepatocellular carcinoma burden in India
Clinicians practicing in country feels that the HCC burden in South India may be higher than remaining part of the country. The cancer registries indicate that the incidence of HCC in population at large is highest in north-eastern states. However, in absence of properly designed prospective study, comparing the burden of HCC in different region of the country, it may be difficult to assess the differences of regional burden in India.
Conclusions
Thus to conclude, the available data indicates that the age adjusted incidence rate of HCC in India for men ranges from 0.7 to 7.5 and for women 0.2 to 2.2 per 100,000 population per year. The incidence of HCC in cirrhotics in India is 1.6% per year. The male:female ratio for HCC in India is 4:1. The age of presentation varies from 40 to 70 years. The age standardized mortality rate for HCC in India for men is 6.8/100,000 and for women is 5.1/100,000. The unpublished data from various tertiary care centers suggest that the incidence of HCC is increasing in India. There is a need for a multi-centric HCC registry under the aegis of INASL.
Conflicts of interest
The author has none to declare.
References
- 1.EASL–EORTC Clinical Practice Guideline Management of hepatocellular carcinoma. J Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Prabhakar V., Rao K.S., Reddy D.J. Primary cancer of liver in Vishakhapatnam. Indian J Pathol Microbiol. 1966;9:54–60. [PubMed] [Google Scholar]
- 3.Dhir V., Mohandas K.M. Epidemiology of digestive tract cancers in India III liver. Indian J Gastroenterol. 1998;17:100–103. [PubMed] [Google Scholar]
- 4.National Cancer Registry Program, ICMR http://ncrpindia.org/.
- 5.International Agency for Research on Cancer (IARC–WHO) http://Ci5.iarc.fr (Access number 9).
- 6.Yuen F., Hou J.C., Chuttapati A. Hepatocellular cancer in Asia Pacific region. J Gastroenterol Hepatol. 2009;24:346–353. doi: 10.1111/j.1440-1746.2009.05784.x. [DOI] [PubMed] [Google Scholar]
- 7.Yeole B. Trends in cancer incidences in esophagus, stomach, colon, rectum and liver in males in India. Asian Pac J Cancer Prev. 2008;9:97–100. [PubMed] [Google Scholar]
- 8.Dikshit R., Gupta P.C., Ramasundarahelige C., Million Death Study Collaborators Lancet. 2012;79:1807–1816. [Google Scholar]
- 9.Mohandas K.M. Surveillance of Indian with liver cirrhosis for treatable hepatocellular carcinoma: another enigma. J Gastroenterol. 2007;26:261–264. [PubMed] [Google Scholar]
- 10.Sarin S.K., Thakur V., Guptan R.C. Hepatocellular cancer in India. J Gastroenterol Hepatol. 2001;16:666–673. doi: 10.1046/j.1440-1746.2001.02476.x. [DOI] [PubMed] [Google Scholar]
- 11.Paul S.B., Chalamalasetty B., Vishnubatla S. Clinical profile, etiology and therapeutic outcome in 324 hepatocellular cancer in India. Oncology. 2009;77:162–171. doi: 10.1159/000231886. [DOI] [PubMed] [Google Scholar]
- 12.Coon J.T., Rogers G., Hewson P. Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis. Health Technol Assess. 2007;11:1–206. doi: 10.3310/hta11340. [DOI] [PubMed] [Google Scholar]
- 13.Fattovitch G., Stroffolini T., Zagni I., Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factor (review) Gastroenterology. 2004;127(suppl I):S35–S50. doi: 10.1053/j.gastro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 14.Chu C.M. Natural history of chronic hepatitis B virus infection in adults with emphasis on the occurrence of cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol. 2000;15(Sujppl-1):E25–E30. doi: 10.1046/j.1440-1746.2000.02097.x. [DOI] [PubMed] [Google Scholar]
- 15.Tanaka K., Sakai H., Hashizume M., Hirohata T. A long term follow up study on risk factors for hepatocellular carcinoma among Japanese patients with liver cirrhosis. Jpn J Cancer Res. 1998;89:1241–1250. doi: 10.1111/j.1349-7006.1998.tb00520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paul S.B., Sreenivas V., Gulati M.S. Incidence of hepatocellular carcinoma among Indian patients with cirrhosis of liver: an experience from tertiary care center in northern India. Indian J Gastroenterol. 2007;26:274–278. [PubMed] [Google Scholar]
- 17.Battam A., Narula D., Tofeja T., Sreenivas V., Puliyel J.M. Systematic review and meta analysis of prevalence of hepatitis B in India. Indian Paediatr. 2007;44:663–674. [PubMed] [Google Scholar]
- 18.Ashim M., Sarma M.P., Kar P. Etiological and molecular profile of hepatocellular cancer in India. Int J Cancer. 2013;133:437–445. doi: 10.1002/ijc.27993. [DOI] [PubMed] [Google Scholar]
- 19.Sharma S., Sharma B., Chawla Y.K. Comparison of 7 staging system in north Indian cohort of hepatocellular carcinoma. Trop Gastroenterol. 2010;35:271–278. [PubMed] [Google Scholar]


