ABSTRACT
Background
Perception of body size is a key factor driving health behavior. Mothers directly influence children’s nutritional and exercise behaviors. Mothers of ethnic minority groups and lower socioeconomic status are less likely to correctly identify young children as overweight or obese. Little evaluation has been done of the inverse—the child’s perception of the mother’s weight.
Objective
To determine awareness of weight status among mother-child dyads (n = 506).
Design
Cross-sectional study conducted in an outpatient pediatric dental clinic of Columbia University Medical Center, New York, NY.
Participants
Primarily Hispanic (82.2 %) mothers (n = 253), 38.8 ± 7.5 years of age, and children (n = 253), 10.5 ± 1.4 years of age, responding to a questionnaire adapted from the validated Behavioral Risk Factor Surveillance System.
Main Measures
Anthropometric measures—including height, weight, and waist circumference—and awareness of self-size and size of other generation were obtained.
Key Results
71.4 % of obese adults and 35.1 % of overweight adults underestimated size, vs. 8.6 % of normal-weight (NW) adults (both p < 0.001). Among overweight and obese children, 86.3 % and 62.3 % underestimated their size, vs. 14.9 % NW children (both p < 0.001). Among mothers with overweight children, 80.0 % underestimated their child’s weight, vs. 7.1 % of mothers with NW children (p < 0.001); 23.1 % of mothers with obese children also underestimated their child’s weight (p < 0.01). Among children with obese mothers, only 13.0 % correctly classified the adult’s size, vs. 76.5 % with NW mothers (p < 0.001). Among obese mothers, 20.8 % classified overweight body size as ideal, vs. 1.2 % among NW mothers (p < 0.001).
Conclusion
Overweight/obese adults and children frequently underestimate their size. Adults misjudge overweight/obese children as being of normal weight, and children of obese mothers often underestimate the adult’s size. Failure to recognize overweight/obesity status among adults and children can lead to prolonged exposure to obesity-related comorbidities.
KEY WORDS: Size misperception, Intergenerational, Families, Underestimation
INTRODUCTION
Over the past 30 years, the prevalence of obesity in the United States has doubled among adults over the age of 20 years1 and nearly 70 % of American adults are either overweight or obese.2 Since 1980, obesity among American youth has almost tripled, and over 30 % of children are now classified as overweight or obese (BMI > 85th percentile).3 Compared to their white peers, amongst low-income preadolescent black girls and Hispanic boys, there is 10 % higher prevalence of obesity.1,4 Cultural standards have been postulated to contribute to increased prevalence of obesity among minority children.5 In a report of minority families, two-thirds of mothers with overweight preschool children were either satisfied with the child’s current size or wished them to be heavier.5 Mothers are influential in the nutritional behavior of children,6 and children tend to mimic parental attitudes towards physical activity, food preferences, and other behaviors affecting weight.7
Children of overweight parents are likely to be reared in environments promoting accelerated weight gain, the so-called obesogenic household.7 Moreover, obesity in one or both parents influences the risk of obesity in offspring as a consequence of shared genetics and environmental factors.8 Children from households with overweight/obese parents are likely to become overweight/obese adults,7,9 with the prospective risk of development of obesity-related cardiovascular risk factors and subsequent cardiovascular disease (CVD).10,11 The significance of excessive weight during childhood is a challenge for the biomedical community at large, particularly pediatricians, primary care physicians, nutritionists, cardiologists, and public health advocates. Understanding weight perception is critical in addressing the national increase in obesity and consequent cardiovascular disease morbidity and mortality attributed to it.11 To investigate intergenerational views concerning weight status and size, we examined 1) mother and child’s awareness of self-weight, 2) mother’s perception of child’s weight, and 3) mother's and child’s attitudes concerning ideal size and size dissatisfaction. Moreover, a key goal was to explore child’s perception of mother’s weight, an approach that has not been reported previously.
METHODS
Subjects
A convenience sample of 253 mother–child dyads was recruited from the ambulatory Pediatric Dentistry Clinic of the Columbia University Medical Center. The study was approved by Columbia University’s Institutional Review Board; participants provided written informed consent/assent prior to participating. Children (7–13 years), accompanied by mothers (or other primary female caregiver), were enrolled from July 2009 to April 2014. Exclusion criteria for adults included history of coronary artery disease, CVD procedure (angioplasty, bypass surgery, stent placement), myocardial infarction, stroke or transient ischemic attack, pregnancy, and age ≤ 21 years. Adults completed a five-page standardized face-to-face questionnaire in English or Spanish, adapted from the validated Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System.12 Demographic data (age, race/ethnicity, education, health insurance, and income) was collected. Adults were queried on perception of current, healthy, and ideal body size and dissatisfaction with size using figural stimuli scales matched to BMI; the scale has validity and test–retest reliability for a wide range of subjects.13,14 Children completed a 19-page standardized face-to-face questionnaire in English, either independently or with aid from research staff, consisting of questions assessing the child’s perception of his/her weight status, perception of current, healthy and ideal body size, dissatisfaction with size, perception of mother’s size, and what constitutes an underweight, normal-weight, and overweight/obese BMI.
Measures
Self-reported medical history and cardiovascular risk factors—diabetes mellitus, hypertension, hyperlipidemia, smoking, overweight, and obesity—were queried. Physical measures among adults included height, weight, waist circumference, and blood pressure; among children, height and weight were measured. Both groups were measured without shoes by a trained research assistant using a tape measure (Tech-Med, 72”), manual blood pressure cuff (Omron Intellisense [portable], model HEM-711DLX), and calibrated portable electronic scale (TANITA digital weight scale). Body mass index (BMI) [weight (kg)/height (m2)] was calculated from the measured weight and height and classified as underweight (≤18.4 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), or obese (≥30 kg/m2). Children were classified as underweight (<5 % on standardized growth curve [SGC]) normal weight (≥5 % and <85 % on SGC), overweight (≥85 % and <95 % on SGC), or obese (≥95 % on SGC).
Race and ethnicity were self-identified, modeled after the U.S. Census Office of Management and Budget15 and defined by six categories: Hispanic/Latino, non-Hispanic Caucasian, Native American, non-Hispanic Black/African-American, Asian/Pacific Islander, and Other.
Years of education were categorized as: never or attended < 8 years (elementary); attended 9–12 years (high school); attended > 12 years (college).
Perception
Adult perception of body size was assessed in two ways: 1) the nine-figure sex-specific Stunkard silhouette scale13; and 2) the response to the query, “Are you normal, underweight, or overweight?” Participants selected from among silhouettes identified as current, ideal, and healthy, represented by underweight (silhouettes # 1–2), normal weight (# 3–4), overweight (# 5–6), and obese (# 7–9). Current size was the silhouette selected in response to the question, “Which figure do you think you look like?” Ideal size was assessed in response to “Which figure do you think is ideal?” Healthy size was the silhouette in response to“Which figure do you think is healthiest?” The silhouette selected was matched to the BMI category depicted by the silhouette.16,17 National guidelines and normative data link the Stunkard figural stimuli with BMI; the scale has validity and test–retest reliability for a wide range of subjects.13,14 Adults were asked to specify the child’s body size by selecting if the child was “underweight,” “normal,” or “overweight.”
For children, size perception was assessed using a seven-figure sex- and age-specific pictorial set of silhouettes for preadolescent children.11,18 Participants chose silhouettes ranging from overweight (silhouettes # 1–2), normal weight (# 3–5), and underweight (# 6–7), identified as current, ideal, and healthy.11Current size was the silhouette selected in response to “Which figure do you look like?” Ideal was assessed in response to “Is there another figure you want to look like?” Healthy was the silhouette in response to “Circle all figures that look healthy for a girl (boy) your age.” Validated figural stimuli for children are consistent with accurate identification of body size at varied age levels.19
Children were asked which Stunkard silhouette described adult current size, i.e., “Which figure does your mother look like now?” The question, “Which figure do you think your mother wants to look like?” assessed child’s perception of ideal adult size. The question, “Which figure looks healthy for a woman?” assessed child’s perception of healthy adult size. The Stunkard scale has been utilized to assess adult children’s perception of parents’ weight; we extrapolated the use to preadolescent children.20
To assess body size dissatisfaction, the difference between current and ideal size was calculated by subtracting the ideal silhouette from the current size silhouette.
Statistical Analysis
All analyses were performed with SAS for 9.3 (SAS Institute, Cary, NC). The significance of differences in perceptions among normal-weight, overweight, and obese adults was determined using logistic regression. Specifically, normal-weight adults were compared to overweight and obese adults with respect to their own body size, their ideal size, and their children’s weight. Similar analyses were performed comparing normal-weight, overweight, and obese children. The effect of the child’s gender on their perceptions and those of their mothers was assessed by adding interaction terms to the logistic regression models reflecting differences between boys and girls. The association between the mother’s degree of dissatisfaction with her figure and the child’s degree of dissatisfaction with his/her figure was assessed using Spearman’s rank correlation. A p value of < 0.05 was considered significant for all analyses.
RESULTS
Demographics and Risk Factors
Of the 253 mother-child dyads, 208 self-classified as Hispanic (82.2 %, primarily of Caribbean origin), 28 as non-Hispanic black (11.1 %), 10 as non-Hispanic white (4.0 %); and 7 as Asian or other (2.8 %). The mean adult age was 38.8 ± 7.5 years and mean child age was 10.5 ± 1.4 years. Most adults had completed at least some high school (211/251, 84.1 %), and average years of education was11.8 ± 3.3 years. Children were in grades 2–8. Mean family income was $37,700 ± $18,100; 71.0 % were Medicaid recipients (179/252). CVD risk factors were common among adults, including hypertension (38), hyperlipidemia (26), and diabetes mellitus (12); waist size ≥ 35 in. was measured in 49.0 % (Table 1). Among those with hypertension (84.2 %), hyperlipidemia (69.2 %), and diabetes mellitus (75 %), the majority were overweight/obese.
Table 1.
Characteristics of Participants
| (N[%] or mean ± SD) | Overall | Male Children | Female Children |
|---|---|---|---|
| Number of Subjects (Mother-Child Dyad) | 253 | 123 | 130 |
| Race/Ethnicity | |||
| Hispanic | 208 (82.2) | 104 (84.6) | 104 (80.0) |
| Non-Hispanic Black | 28 (11.1) | 11 (8.9) | 17 (13.1) |
| Non-Hispanic White | 10 (4.0) | 5 (4.1) | 5 (3.9) |
| Asian | 3 (1.2) | 2 (1.6) | 1 (0.8) |
| Other | 4 (1.6) | 1 (0.8) | 3 (2.3) |
| Age (years) mean ± SD of Mother | 38.8 ± 7.5 | 39.1 ± 7.9 | 38.6 ± 7.2 |
| Age Range (years) of Mother | 24–64 | 24–62 | 25–64 |
| Years of Education mean ± SD of Mother | 11.8 ± 3.3 | 11.5 ± 3.4 | 12.0 ± 3.3 |
| Elementary (≤8 years) | 40 (15.9) | 21 (17.4) | 19 (14.6) |
| High School (9–12 years) | 122 (48.6) | 57 (47.1) | 65 (50.0) |
| College (≥12 years) | 89 (35.5) | 43 (35.5) | 46 (35.4) |
| Body Mass Index mean(kg/m2) of Mother | 28.3 ± 6.7 | 27.8 ± 5.1 | 28.8 ± 8.0 |
| Family Income ($ US dollar) | 37,700 ± 18,100 | 37,000 ± 18,500 | 38,400 ± 17,800 |
| Age (years) mean ± SD of Child | 10.5 ± 1.4 | 10.4 ± 1.4 | 10.6 ± 1.4 |
| Age Range (years) of Child | 7–13 | 7–13 | 7–13 |
| School Grade of Child | 5.3 ± 1.5 | 5.1 ± 1.5 | 5.6 ± 1.4* |
| Body Mass Index mean (percentile) of Child | 70.6 ± 26.8 % | 72.2 ± 26.8 % | 69.1 ± 26.9 % |
| Insurance | |||
| Medicaid | 179 (71.0) | 89 (73.0) | 90 (69.2) |
| Medicare | 6 (2.4) | 3 (2.5) | 3 (2.3) |
| Private-Pay | 18 (7.1) | 9 (7.4) | 9 (6.9) |
| Self-Pay | 49 (19.4) | 21 (17.2) | 28 (21.5) |
| Self-Reported Traditional Cardiovascular Risk Factors of Mother | |||
| Diabetes Mellitus | 12 (4.7) | 8 (6.5) | 4 (3.1) |
| Hypertension | 38 (15.0) | 21 (17.1) | 17 (13.1) |
| Hyperlipidemia | 26 (10.3) | 12 (9.8) | 14 (10.8) |
| Measured Waist Size of Mother ≥ 35 in. | 121 (48.0) | 61 (49.6) | 60 (46.5) |
| Body Mass Index (kg/m2) of Mother | |||
| Underweight (≤18.4) | 1 (0.4) | 1 (0.8) | 0 (0.0) |
| Normal Weight (18.5–24.9) | 81 (32.0) | 40 (32.5) | 41 (31.5) |
| Overweight (25.0–29.9) | 94 (37.2) | 45 (36.6) | 49 (37.7) |
| Obese (≥30.0) | 77 (30.4) | 34 (30.1) | 40 (30.8) |
| Body Mass Index (percentile) of Child | |||
| Underweight (<5th percentile) | 5 (2.0) | 3 (2.5) | 2 (1.6) |
| Normal Weight (≥5th and <85th percentile) | 141 (56.4) | 61 (50.4) | 80 (62.0) |
| Overweight (≥85th and <95th percentile) | 51 (20.4) | 28 (23.1) | 23 (17.8) |
| Obese (≥95th percentile) | 53 (21.2) | 29 (24.0) | 24 (18.6) |
*p < 0.05 versus male children
BMI by Mother-Child Dyad
Adults were classified by BMI as underweight (1), normal-weight (81), overweight (94), and obese (77). Children were classified by BMI as underweight (5), normal-weight (141), overweight (51), and obese (53). Mean adult BMI was 28.3 ± 6.7 kg/m,2 and mean child BMI percentile was 70.6 %. Male children (n = 123) were more likely than female children (n = 130) to be overweight (23.1 % vs. 17.8 %) or obese (24.0 % vs. 18.6 %), but differences were not statistically significant (Table 1). Nearly 70 % of normal-weight mothers (69.6 %) had a child of normal weight, compared to 50.0 % of overweight mothers (p < 0.01) and 53.5 % of obese mothers (p < 0.05).
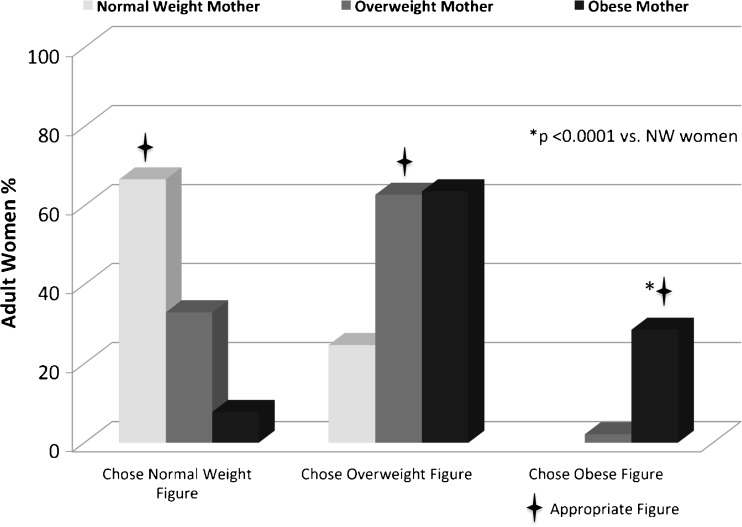
Adult’s Perception of Their Own Size and of Child’s Size
Most normal-weight and overweight adults (66.7 and 62.8 %, respectively) chose appropriate silhouettes as representative of current size. Among obese adults, 71.4 % chose inappropriate—that is, merely overweight or normal-weight—silhouettes as representative of current size (p < 0.001). Similarly, 35.1 % of overweight adults underestimated size, vs. 8.6 % of normal-weight adults (p < 0.001). No obese adult chose the largest silhouette, including those with a BMI as high as 43.9 kg/m2 (Fig. 1).
Fig. 1.
Mother’s perception of self-size—Mothers classified by BMI and perception of current figure. Symbol indicates that participant chose the appropriate figure to represent self.
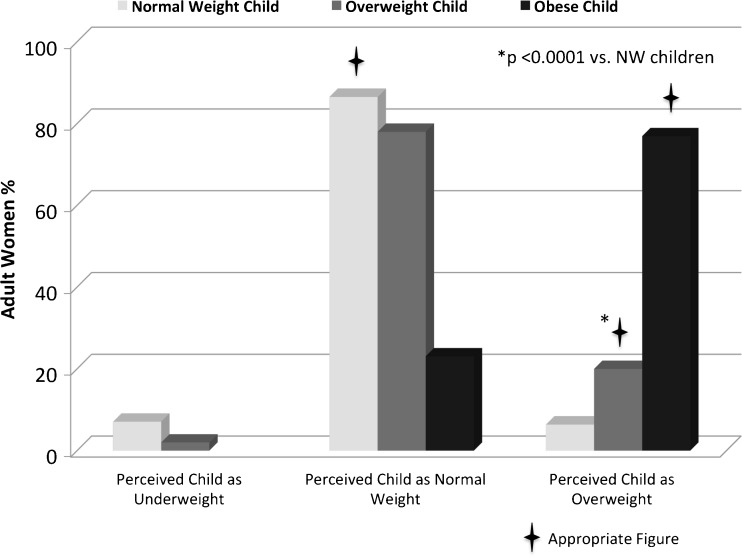
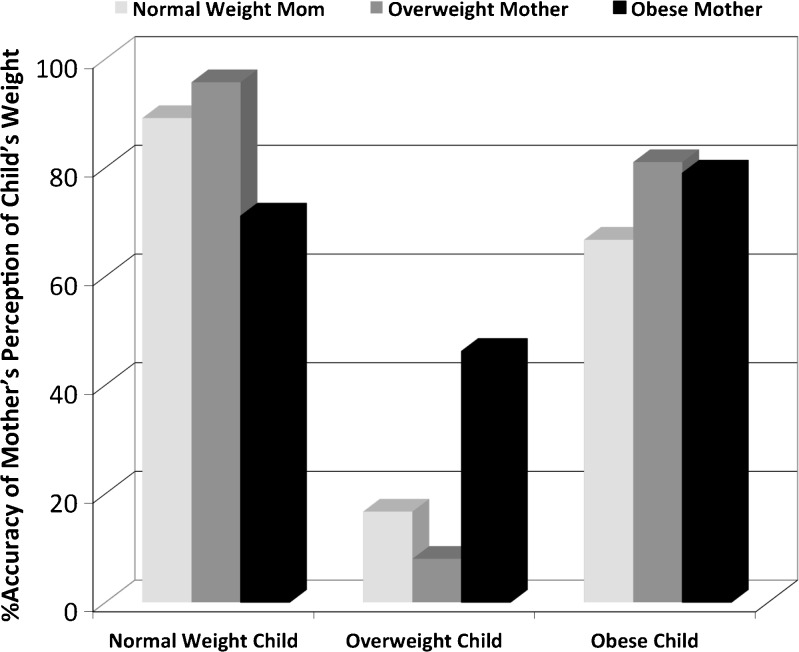
Among adults, 86.5 % with a normal-weight child correctly perceived the child's weight to be normal. Those with an overweight/obese child, however, did not classify their child’s weight as reliably; 80.0 % of adults with an overweight child (p < 0.001) and 23.1 % with an obese child (p < 0.01) underestimated their child’s weight as normal (Fig. 2). Obese mothers of overweight/obese children were less likely than normal-weight mothers of overweight/obese children to underestimate child’s weight, but differences were not statistically significant (Fig. 3). Child’s gender did not influence mother’s perception of child’s weight.
Figure 2.
Mother’s perception of child’s body size—Children classified by BMI and their mother’s perception of their current figure. Symbol indicates that participant classified child’s weight correctly.
Figure 3.
Accuracy of normal-weight, overweight, and obese mother’s perception of child’s body weight—Children classified by BMI and the accuracy of their mother’s perception of their weight. Findings are not statistically significant.
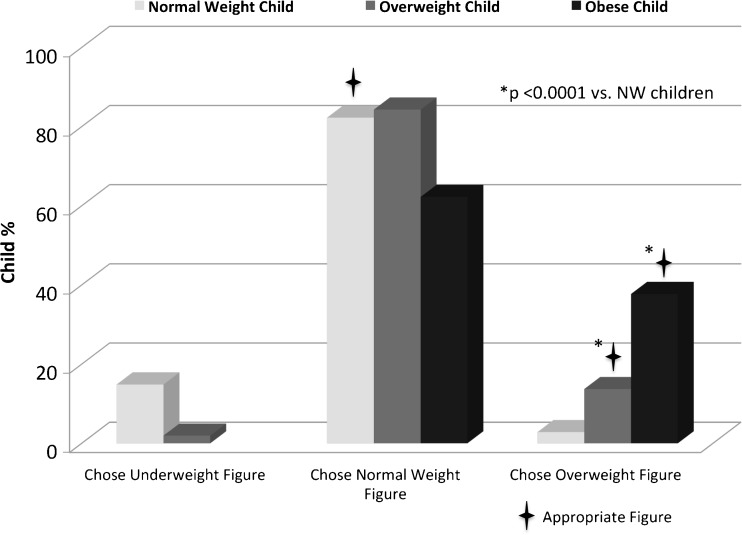
Child’s Perception of Their Own Size and of Mother’s Size
Normal-weight children were more likely to self-identify with appropriate silhouettes compared to overweight/obese children. Among normal-weight children, 82.3 % identified current size correctly. In comparison, 86.3 % of overweight children (p < 0.001) and 62.3 % of obese children (p < 0.001) underestimated size (Fig. 4). Gender did not affect perception.
Figure 4.
Child’s perception of self-size—Children classified by BMI and perception of current figure. Symbol indicates that participant chose the appropriate figure to represent self.
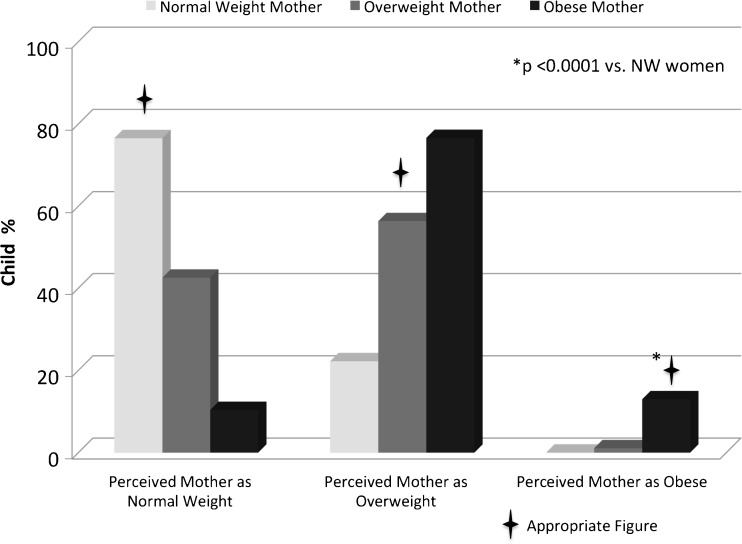
Normal weight children were more likely than overweight/obese children to choose appropriate silhouettes to describe mother’s current size. Most children with normal weight mothers (76.5 %) correctly categorized them, but only 56.4 % of children with overweight mothers classified them correctly (p < 0.01). Among children with obese mothers, 13.0 % appropriately chose representative adult silhouettes; 76.6 % misclassified obese adults as overweight and 10.4 % as normal weight (p < 0.001) (Fig. 5).
Figure 5.
Child’s perception of mother’s body size.—Mothers classified by BMI and their children’s perception of their current figure. Symbol indicates that participant classified mother’s weight correctly.
Perception of “Ideal” Size
The majority of normal-weight (82.7 %), overweight (75.5 %), and obese (70.1 %) adults chose normal-weight silhouettes as ideal; 1.2 % of normal-weight and 4.3 % of overweight women chose overweight silhouettes as ideal. In contrast, 20.8 % of obese women chose an overweight silhouette as ideal (p < 0.001). Child’s perception of the ideal figure for an adult woman did not differ by BMI.
Dissatisfaction With Current Size
Among the normal-weight adults, 45.7 % were dissatisfied and considered an ideal silhouette to be ≥ 1 silhouette smaller. Moreover, among overweight adults, 85.1 % were dissatisfied, preferring ideal figures that were ≥ 1 silhouette smaller (p < 0.001). Among obese adults, almost all were dissatisfied—97.4 % considered an ideal figure to be ≥ 1 silhouette smaller (p < 0.001). Additionally, most obese women (71.4 %) aspired to be ≥ 2 silhouettes smaller.
Almost half of the children (47.9 %) were dissatisfied with current size. Among normal-weight children, 31.6 % were dissatisfied, whereas 59.6 % of overweight and 85.4 % of obese children were dissatisfied (both p < 0.001). Adult dissatisfaction with current size and child’s perception of difference of mother’s current size from ideal adult size were correlated (r = 0.22, p < 0.001). Adult and child dissatisfaction with respect to their own figures was also correlated (r = 0.19, p < 0.01).
DISCUSSION
Important factors acknowledged to influence weight perception include the triad of minority race/ethnicity, low income, and limited education, which are shared features of the current cohort.21,22 We investigated views concerning weight and perception of size among two generations—women and their children. Attention to Hispanic women and children, particularly the overweight and obese, provides an opportunity to understand a relatively understudied population. Moreover, as minority children constitute a disproportionate percentage of overweight/obese children in the U.S., it is important to analyze this high-risk population in order to appropriately tailor prevention efforts. Others who report data about families and weight status, including Hispanics, primarily concentrate on maternal attitudes.9 However, we evaluated the views of children towards their mothers—an approach that had not previously been undertaken. The key findings were as follows: 1) Overweight/obese adults often underestimate self-size; 2) adults underestimate overweight/obese children to be normal weight; 3) overweight and obese children are likely to underestimate self-weight and to regard themselves as normal-weight; and importantly, 4) children of obese mothers often underestimate adult size, selecting normal or merely overweight silhouettes to represent mothers. These observations are troubling, and suggest that perception of normal body size is shifting to larger sizes, possibly beginning in childhood.
Intergenerational attitudes have consequences for personal and public health.5,9 Cultural norms among Hispanic families favor larger-sized children, and among Hispanic families with fewer years of residence in the United States, mothers frequently identify overweight children as normal weight.23,24 This has been ascribed to community contextual factors and socioeconomic status.25 Children with overweight/obese parents and schoolmates are more likely to underestimate self-size, possibly secondary to desensitization of normal weight. Additionally, children considering weight status from figural stimuli may be less likely to self-identify with larger sizes due to the stigma of being “fat”.26 Failure to recognize abnormal weight status and tolerance of overweight or obese status makes it less likely that calls for weight control are seen as personally relevant, and might be ignored by those who neither perceive their weight as abnormal nor recognize associated risks.27,28
Many individuals who underestimate self-size recognize the variance between current size and ideal size. Overweight/obese adults and children are more likely to be dissatisfied than their normal-weight counterparts.29,30 In this report, there was a correlation with respect to maternal and child dissatisfaction, and the degree of adult dissatisfaction and the child’s perception of variance of mother’s figure from the ideal. These findings suggest that adult dissatisfaction with body size may transfer to the child. While size dissatisfaction serves as an impetus for attaining healthy weight,4 it also diminishes feelings of self-worth, and can be detrimental to healthy emotional development and peer relationships.31–33
The consequences of childhood obesity are considerable, given that 50 % of young obese children become obese adults8, 30–50 % of obese adolescents meet the criteria for metabolic syndrome34, and childhood and adolescent obesity are associated with diabetes mellitus, dyslipidemia, hypertension, sleep apnea. and atherosclerosis.35 Flawed weight classification in childhood can set in motion lifelong distorted perceptions of what is acceptable, contributing to adolescent and adult obesity.36,37 Rising rates of youth obesity theoretically account for a reduction of between two and five years in average lifespan,38,39 and are expected to shorten overall life expectancy in the U.S. for the first time in two centuries.38
Timely diagnosis of abnormal weight status for children is critical, and prevention efforts are challenging, given that many parents of obese children are unlikely to initiate action to prevent obesity 1) if weight is not perceived as a problem, or 2) if the link between current and future adverse health outcomes is not appreciated.40 Failure to properly assess a child’s weight constrains interventions26 such as encouraging diet and physical activity,23 utilizing growth charts and other standardized instruments,41 encouraging shared family meals, and reducing television time.42 Here, we found that over 60 % of obese children misidentified body size. Assurance that children appropriately perceive normal body weight requires parental, health care provider, school, and community-based efforts. Currently, only 7 % of pediatricians follow recommended evaluations for comorbid conditions associated with abnormal weight status.43 It has been suggested that primary care practitioners assume a stronger role in identifying and managing overweight/obesity status, including intervention with automatic school notification.40 School initiatives and community-based programs hold promise for improving early interventions including diet and physical activity, marketing, and physical environments.44
LIMITATIONS
The current report is a cross-sectional design, and causal relationships cannot be determined. The data based upon ethnic designation focused upon Hispanics, and findings may not be generalizable to other ethnic groups. Since data was self-reported and recruited from one site, it is subject to recall and selection bias. Figural stimuli, although used extensively among varied racial/ethnic groups, may not detect subtle differences in size perception; moreover, validity has not been established for children’s use of scale to characterize adults.13 For some, the full range of the scale is not appreciated, and those with high BMI may not choose larger figures. Confounding by variables, both measured and unmeasured, was not controlled for and may be present.
CONCLUSIONS
We found that failure to recognize abnormal weight occurred more often among overweight or obese mothers and children. Flawed weight perception impedes recognition of obesity and its risks as a personal health issue. The finding that children of obese mothers often underestimate adult size suggests that tolerance of overweight status is common among children of obese parents. For the first time in two centuries, the United States may see shortened life expectancy, as prolonged exposure to obesity beginning in childhood results in a dramatic rise in rates of coronary artery disease.45 Recognition of misperception of size among families is critical to the future design and implementation of programs to reverse trends contributing to the current prevalence of obesity. Our findings underscore the significance of evaluating high-risk and understudied subgroups and examining age, ethnicity, and socioeconomic status in efforts to understand ways to avoid the consequences of childhood obesity.
ACKNOWLEDGMENTS
This work is supported in part by the Department of Health and Human Services (1HHCWHO5003-01-11), Arlene and Joseph Taub Foundation, Paterson NJ, Edwina and Charles Adler Foundation, and by Columbia University’s CTSA grant UL1-RR024156 from the NCRR/NIH. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; or preparation, review, and approval of the manuscript. The content is the responsibility of the authors. The authors have no competing interests. This data was presented in part in poster format at the American Heart Association’s Epidemiology and Prevention/Nutrition, Physical Activity and Metabolism Meeting on March 21, 2013 in New Orleans, LA.
Elsa-Grace V. Giardina and Tracy K. Paul had full access to all data in the study, and take responsibility for the integrity of the data and accuracy of the data analysis.
Conflict of Interest
The authors declare that they have no conflicts of interest.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Liang H, Chen X. Measured body mass index, body weight perception, dissatisfaction and control practices in urban, low-income African American adolescents. BMC Public Health. 2009;9:183. doi: 10.1186/1471-2458-9-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Killion L, Hughes SO, Wendt JC, Pease D, Nicklas TA. Minority mothers’ perceptions of children’s body size. Int J Pediatr Obes. 2006;1(2):96–102. doi: 10.1080/17477160600684286. [DOI] [PubMed] [Google Scholar]
- 6.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr. 2005;24(2):83–92. doi: 10.1080/07315724.2005.10719448. [DOI] [PubMed] [Google Scholar]
- 7.Davison KK, Birch LL. Obesigenic families: parents’ physical activity and dietary intake patterns predict girls’ risk of overweight. Int J Obes Relat Metab Disord. 2002;26(9):1186–1193. doi: 10.1038/sj.ijo.0802071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 9.Olvera N, Suminski R, Power TG. Intergenerational perceptions of body image in hispanics: role of BMI, gender, and acculturation. Obes Res. 2005;13(11):1970–1979. doi: 10.1038/oby.2005.242. [DOI] [PubMed] [Google Scholar]
- 10.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 11.Maximova K, McGrath JJ, Barnett T, O’Loughlin J, Paradis G, Lambert M. Do you see what I see? Weight status misperception and exposure to obesity among children and adolescents. Int J Obes (Lond) 2008;32(6):1008–1015. doi: 10.1038/ijo.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Department of Health & Human Services CfDCP. Centers for Disease Control & Prevention Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia.
- 13.Stunkard AJ, Sørensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis. 1983;60:115–120. [PubMed] [Google Scholar]
- 14.Kronenfeld LW, Reba-Harrelson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body Image. 2010;7(2):131–136. doi: 10.1016/j.bodyim.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office of Management and Budget Race and ethnic standards for federal statistics and administrative reporting. (Directive no, 15) Fed Regist. 1978;43(87):19269. [Google Scholar]
- 16.Bulik CM, Wade TD, Heath AC, Martin NG, Stunkard AJ, Eaves LJ. Relating body mass index to figural stimuli: population-based normative data for Caucasians. Int J Obes Relat Metab Disord. 2001;25(10):1517–1524. doi: 10.1038/sj.ijo.0801742. [DOI] [PubMed] [Google Scholar]
- 17.Bhuiyan AR, Gustat J, Srinivasan SR, Berenson GS. Differences in body shape representations among young adults from a biracial (Black-White), semirural community: the Bogalusa Heart Study. Am J Epidemiol. 2003;158(8):792–797. doi: 10.1093/aje/kwg218. [DOI] [PubMed] [Google Scholar]
- 18.Collins ME. Body figure perceptions and preferences among preadolescent children. Int J Eat Disord. 1991;10(2):199–208. doi: 10.1002/1098-108X(199103)10:2<199::AID-EAT2260100209>3.0.CO;2-D. [DOI] [Google Scholar]
- 19.Williamson S, Delin C. Young children’s figural selections: accuracy of reporting and body size dissatisfaction. Int J Eat Disord. 2001;29(1):80–84. doi: 10.1002/1098-108X(200101)29:1<80::AID-EAT13>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 20.Sørensen TI, Stunkard AJ, Teasdale TW, Higgins MW. The accuracy of reports of weight: children’s recall of their parents’ weights 15 years earlier. Int J Obes. 1983;7(2):115–122. [PubMed] [Google Scholar]
- 21.Paeratakul S, White MA, Williamson DA, Ryan DH, Bray GA. Sex, race/ethnicity, socioeconomic status, and BMI in relation to self-perception of overweight. Obes Res. 2002;10(5):345–350. doi: 10.1038/oby.2002.48. [DOI] [PubMed] [Google Scholar]
- 22.Kuchler F, Variyam JN. Mistakes were made: misperception as a barrier to reducing overweight. Int J Obes Relat Metab Disord. 2003;27(7):856–861. doi: 10.1038/sj.ijo.0802293. [DOI] [PubMed] [Google Scholar]
- 23.Intagliata V, Ip EH, Gesell SB, Barkin SL. Accuracy of self- and parental perception of overweight among Latino preadolescents. N C Med J. 2008;69(2):88–91. [PMC free article] [PubMed] [Google Scholar]
- 24.Contento IR, Basch C, Zybert P. Body image, weight, and food choices of Latina women and their young children. J Nutr Educ Behav. 2003;35(5):236–248. doi: 10.1016/S1499-4046(06)60054-7. [DOI] [PubMed] [Google Scholar]
- 25.Powell LM, Wada R, Krauss RC, Wang Y. Ethnic disparities in adolescent body mass index in the United States: the role of parental socioeconomic status and economic contextual factors. Soc Sci Med. 2012;75(3):469–476. doi: 10.1016/j.socscimed.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saxton J, Hill C, Chadwick P, Wardle J. Weight status and perceived body size in children. Arch Dis Child. 2009;94(12):944–949. doi: 10.1136/adc.2009.162578. [DOI] [PubMed] [Google Scholar]
- 27.Wartak SA, Friderici J, Lotfi A, Verma A, Kleppel R, Naglieri-Prescod D, et al. Patients’ knowledge of risk and protective factors for cardiovascular disease. Am J Cardiol. 2011;107(10):1480–1488. doi: 10.1016/j.amjcard.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 28.Sivalingam SK, Ashraf J, Vallurupalli N, Friderici J, Cook J, Rothberg MB. Ethnic differences in the self-recognition of obesity and obesity-related comorbidities: a cross-sectional analysis. J Gen Intern Med. 2011;26(6):616–620. doi: 10.1007/s11606-010-1623-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xanthopoulos MS, Borradaile KE, Hayes S, Sherman S, Vander Veur S, Grundy KM, et al. The impact of weight, sex, and race/ethnicity on body dissatisfaction among urban children. Body Image. 2011;8(4):385–389. doi: 10.1016/j.bodyim.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 30.Presnell K, Bearman SK, Stice E. Risk factors for body dissatisfaction in adolescent boys and girls: a prospective study. Int J Eat Disord. 2004;36(4):389–401. doi: 10.1002/eat.20045. [DOI] [PubMed] [Google Scholar]
- 31.Wallander JL, Kerbawy S, Toomey S, Lowry R, Elliott MN, Escobar-Chaves SL, et al. Is obesity associated with reduced health-related quality of life in Latino, black and white children in the community? Int J Obes (Lond) 2013;37(7):920–925. doi: 10.1038/ijo.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mirza NM, Mackey ER, Armstrong B, Jaramillo A, Palmer MM. Correlates of self-worth and body size dissatisfaction among obese Latino youth. Body Image. 2011;8(2):173–178. doi: 10.1016/j.bodyim.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallander JL, Taylor WC, Grunbaum JA, Franklin FA, Harrison GG, Kelder SH, et al. Weight status, quality of life, and self-concept in African American, Hispanic, and white fifth-grade children. Obesity (Silver Spring) 2009;17(7):1363–1368. doi: 10.1038/oby.2008.668. [DOI] [PubMed] [Google Scholar]
- 34.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111(15):1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 35.Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1989;84(4):633–641. [PubMed] [Google Scholar]
- 36.Krauss RC, Powell LM, Wada R. Weight misperceptions and racial and ethnic disparities in adolescent female body mass index. J Obes. 2012;2012:205393. doi: 10.1155/2012/205393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, et al. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–e601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- 38.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 39.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 40.Fitzgibbon ML, Beech BM. The role of culture in the context of school-based BMI screening. Pediatrics. 2009;124(Suppl 1):S50–S62. doi: 10.1542/peds.2008-3586H. [DOI] [PubMed] [Google Scholar]
- 41.Jain A, Sherman SN, Chamberlin LA, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107(5):1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 42.Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Diet Assoc. 2007;107(1):53–61. doi: 10.1016/j.jada.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 43.Benson L, Baer HJ, Kaelber DC. Trends in the diagnosis of overweight and obesity in children and adolescents: 1999–2007. Pediatrics. 2009;123(1):e153–e158. doi: 10.1542/peds.2008-1408. [DOI] [PubMed] [Google Scholar]
- 44.Story M, Sallis JF, Orleans CT. Adolescent obesity: towards evidence-based policy and environmental solutions. J Adolesc Health. 2009;45(3 Suppl):S1–S5. doi: 10.1016/j.jadohealth.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 45.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50(22):2128–2132. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]