Abstract
Background
Prior to INASL guidelines, there were no Indian guidelines for management of hepatocellular carcinoma (HCC) in India. The guidelines given by other societies like AASLD, EASL etc are not uniform and not tailored for Indian patients. Hence management practices for HCC in India largely depended on physicians' individual preferences. This survey aimed to study current practices in management of HCC in India.
Methods
An online survey was conducted from the platform of a survey portal (www.surveymonkey.com), from December 2012 to April 2013. Invitation to participate in the survey was sent to 1383 doctors of India who were expected to be involved in management of patients of HCC. The survey was of 10 min duration and consisted of questions on how the respondents diagnosed and managed patients of HCC.
Results
Three hundred and seventy-seven doctors answered the survey questions (72% gastroenterologists, 95% working in India). The important points which emerged from the survey are following: (i) The incidence of HCC is increasing in India; (ii) The most common etiologic agent is Hepatitis B responsible for 43% cases; (iii) Only 14% patients present in early stage when curative treatment is possible (BCLC-A); (iv) 90% of these respondents screen for HCC when they first evaluate a cirrhotic patient; (v) While following a patient of cirrhosis most respondents screen for HCC by ultrasound and AFP at every 6 months to 1 year; and (vi) Most (82%) respondents follow some international guideline for staging and treatment of HCC. The respondents also suggested that there is a need for spreading awareness about HCC in public as well as in medical fraternity, and there is a need for a national registry of HCC.
Conclusions
This is the first survey on management practices on HCC. With the publication of the INASL guidelines on HCC, the diagnosis and treatment of HCC will be more uniform and protocol based. Further such surveys should be carried out at periodic interval to track increasing awareness and better management practices for HCC in India.
Keywords: liver cancer, survey, guidelines, hepatocellular carcinoma, management practices
Abbreviations: AASLD, American Association for the Study of Liver Diseases; AFP, alpha–fetoprotein; BCLC, Barcelona clinic liver cancer; CECT, contrast enhanced computerized tomography; CTP, Child Turcotte Pugh; EASL, European Association for the Study of the Liver; ESDO, European Society of Digestive Oncology; FNAC, fine needle aspiration cytology; GI, gastro-intestinal; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; INASL, Indian National Association for the Study of Liver; MBBS, Bachelor of Medicine, Bachelor of Surgery; SOL, space occupying lesion; TACE, transcatheter arterial chemoembolization
Hepatocellular carcinoma (HCC) is one of the major causes of mortality among patients with chronic liver disease. The incidence of HCC is rising in India and is poised to become the leading GI cancer.1 Prior to INASL guidelines,2 published in the present issue, there were no Indian guidelines for management of hepatocellular carcinoma (HCC) in India. The guidelines given by other societies like AASLD, EASL etc are not uniform and not tailored for Indian patients. Hence management practices for HCC in India largely depended on physicians' individual preferences. This survey aimed to study current practices in management of HCC in India. This survey is the first of its kind done in India, and the results of this survey were presented and discussed during the round table discussion that was held on 9th and 10th February, 2013 at Puri, Odisha, to discuss, debate, and finalize the consensus statements.
Methods
Survey Platform
An online survey was conducted from the platform of a survey portal (www.surveymonkey.com), from December 2012 to April 2013. The survey was of 10 min duration and consisted of questions related to the topics how the respondents diagnosed and managed patients of HCC. The questions and their response options are given in Table 1. The survey consisted of 24 questions, mostly in objective response format, and each question appeared as separate screen on clicking ‘next’.
Table 1.
The Survey Questionnaire.
| Q. No. | Question | Options |
|---|---|---|
| 1 | Tell us about yourself |
|
| 2 | In your practice do you come across patients of HCC? |
|
| 3 | On an average, how many NEW patients of HCC do you see every month? |
|
| 4 | Is the number of new HCC patients increasing in your practice? |
|
| 5 | Do you feel that there is a need for a Registry for HCC? |
|
| 6 | If a National Registry for primary liver cancers were to be set up by INASL, are you willing to contribute your patients' details to this registry? |
|
| 7 | In your experience of all patients of HCC you see in your practice what is the approximate etiological break-up percentage? |
|
| 8 | When you are evaluating a patient of cirrhosis for the first time, do you ROUTINELY screen for HCC? |
|
| 9 | What is the value of AFP in your opinion for screening for HCC? |
|
| 10 | When you are following a patient of cirrhosis, how frequently do you screen for HCC? |
|
| 11 | What will make you suspect HCC in a known patient of cirrhosis and will lead you to investigate for HCC? |
|
| 12 | When you detect a SOL in liver on USG/CT abdomen how do you proceed further? |
|
| 13 | Once HCC is diagnosed, what do you do? |
|
| 14 | Do you use the BCLC classification to treat HCC? |
|
| 15 | BCLC classification refers to the stage of HCC, where BCLC-A is early HCC while BCLC-D is terminal HCC. In your practice what is the approximate break-up (%) of new cases you see according to stage? Note: the total must add up to hundred. |
|
| 16 | Do you strictly follow clinical practice guidelines (e.g. AASLD, EASL) for staging and treating HCC in your practice? |
|
| 17 | Does the hospital where you work has any of these facilities for treating HCC? (Tick all those which apply) |
|
| 18 | Which patients of HCC do you refer for TACE? |
|
| 19 | Do you feel that targeted therapy for liver cancer will be better managed by |
|
| 20 | Are you comfortable in prescribing Sorafenib? |
|
| 21 | Do you put patients on HBV related HCC on anti-virals before starting their HCC treatment to prevent flares? |
|
| 22 | Do you use opioid medication for pain control in HCC patients who are terminally ill? |
|
| 23 | In your practice do you come across patients with intrahepatic cholangiocarcinoma? |
|
| 24 | In your opinion, how can INASL help in prevention or better management of HCC in India? |
|
Sample Size Calculation
There are approximately 2000 qualified gastroenterologists in India and almost all of them are life members of The Indian Society of Gastroenterology.3 This comprised of the target population for the survey. For the survey to adequately represent the target population (n = 2000), with a confidence level of 95% and a confidence interval of 5, a sample of 322 responders are needed. Expecting a 25% response from invitees, invitation to participate in the survey was sent to 1383 doctors of India who were expected to be involved in management of patients of HCC.
Results
Participants
Invitation to participate in the survey was sent to 1383 doctors of India. Of them, 377 (27%) responded to the questionnaire; in 11 (0.8%) the email bounced; 5 (0.4%) opted out: and 990 (72%) did not respond. Among the 377 who responded to the survey questionnaire, 313 (83%) answered all the 24 questions, while rest 64 (17%) answered some of the questions, but not all.
Most respondents (273/377, 72%) were gastroenterologists; followed by gastro-surgeons (47/377, 12%); and general physicians (18/377, 5%). Ninety-five percent (359/377) respondents were working as consultants or faculty. Eighty-five percent (322/377) respondents had completed their medical school (MBBS) between 1977 and 2003. Ninety-five percent respondents (360/377) were working in India.
The survey was designed in such a way that it proceeded further only if the respondent answered “Yes” to the question “In your practice do you come across patients of HCC?”. Ninety-seven percent (367/377) respondents answered “yes” to this question.
Epidemiology of Hepatocellular Carcinoma
For the question “On an average, how many NEW patients of HCC do you see every month?” 40% of respondents answered as 0–1 patients per month; 30% respondents answered as 2–3 patients per month; and 20% respondents answered as 4–6 patients per month. Less than 10% respondents see 7 or more patients per month.
For the question “Is the number of new HCC patients increasing in your practice?” most (64%) respondents answered “Yes”; while 18% responded as “No” and another 18% were unable to comment.
Respondents were asked about the approximate etiological break-up percentage of HCC patients they see. The result is shown in Figure 1. According to the respondents the most common etiologic agent for HCC in India is Hepatitis B (43%), followed by Hepatitis C (22%), unknown or cryptogenic (17%), and alcohol (15%).
Figure 1.
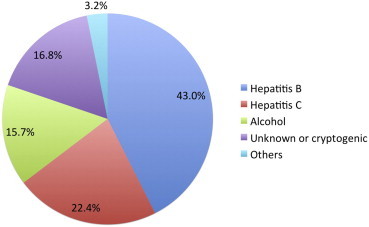
Etiological break-up of HCC in India according to 334 respondents of the survey.
Apart from HCC, 78% of the respondents also come across intrahepatic cholangiocarcinoma in their practice, which resembles HCC.
Screening for Hepatocellular Carcinoma and Diagnosis
When asked how many of the respondents ROUTINELY screen for HCC when evaluating a patient of cirrhosis for the first time, more than 90% respondents answered that they do screen for HCC. The modalities of screening for HCC on their first evaluation of cirrhotic patients is shown in Figure 2. The most frequently used modality for screening for HCC is a combination of AFP and ultrasound abdomen.
Figure 2.
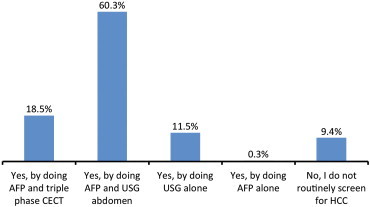
Answer of 340 respondents for the question “When you are evaluating a patient of cirrhosis for the first time, do you ROUTINELY screen for HCC?”.
While following a patient of cirrhosis 55% respondents screen for HCC once in every six months and 30% screen once a year (Figure 3).
Figure 3.
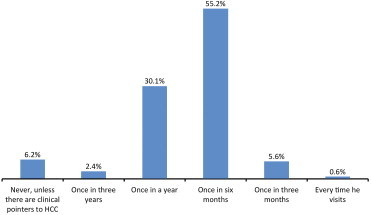
Screening interval for HCC for a patient of cirrhosis on follow up, according to 339 respondents of the survey.
When asked “What is the value of AFP in your opinion for screening for HCC?”, 79% responded that they USUALLY order it recognizing its limitations because it is cheap and readily available.
Figure 4 shows the answers to the question “What will make you suspect HCC in a known patient of cirrhosis and will lead you to investigate for HCC?”. Development of new portal vein thrombosis, worsening of ascites, worsening of CTP score, and pain abdomen were the most commonly encountered clinical pointers to HCC.
Figure 4.
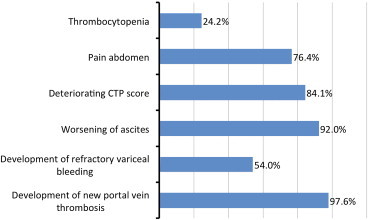
Clinical pointers to HCC in a patient of cirrhosis which lead to investigation for HCC, according to 339 respondents.
On detection of SOL in the liver in a cirrhotic patient, 90% of the respondents order triple phase CECT abdomen and AFP for diagnosis of HCC. Only 7% resort to FNAC for diagnosis of HCC.
Staging
Once HCC is diagnosed 76% (257/337) respondents will do staging and follow established guidelines for treatment as per the stage; while 16% (53/337) respondents will refer the patient to higher center for further management.
When asked, “Do you use the BCLC classification to treat HCC?” only 43% (143/336) respondents answered that they classify all their patients; while 30% (100/336) respondents classify some of their patients (Figure 5).
Figure 5.
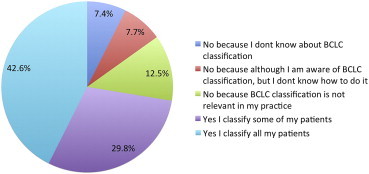
Responses of 336 survey participants to the question “Do you use the BCLC classification to treat HCC?”
It was asked what is the approximate break-up of BCLC stages of new HCC cases they encounter. Three hundred and seventeen respondents answered and results are shown in Figure 6. About 40% of patients of HCC they see for the first time are already in the BCLC stage D when curative or palliative treatment is not possible. Only 14% patients present in BCLC stage A when curative treatment is possible.
Figure 6.
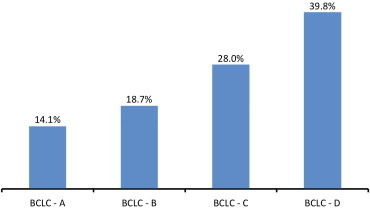
BCLC stage of HCC patients on their first presentation, according to 317 respondents.
Treatment of Hepatocellular Carcinoma
Various international societies like EASL, AASLD, ESDO etc. have given their guidelines for treatment of HCC depending on the stage of HCC. Most (82%, 271/329) respondents agreed that they do follow these guidelines.
Availability of various treatment options was asked from the respondents at their hospital. Their responses are shown in Figure 7. Sorafenib was the most commonly available treatment and 88% respondents said that it was available at their hospital. The second most commonly available treatment modality was resection, which 72% respondents said it was available in their hospital.
Figure 7.
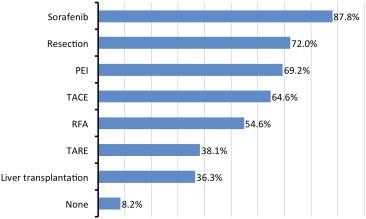
Availability of various treatment modalities for HCC at the hospital of 328 survey respondents.
According to 320 respondents, the most common indication for TACE was when the tumors were of large size, up to two in number, and located in the single lobe (Table 2).
Table 2.
Responses to the Question “Which Patients of HCC Do You Refer for TACE?”.
| Parameter | Tumor characteristics | Response count (n = 320) |
|---|---|---|
| Size | Small size | 82 (26%) |
| Large size | 141 (44%) | |
| Any size | 97 (30%) | |
| Location | Located in single lobe | 206 (64%) |
| Located in both the lobes | 36 (11%) | |
| Any | 78 (24%) | |
| Number | Single | 54 (17%) |
| Up to two | 172 (54%) | |
| Multicentric | 51 (16%) | |
| Any | 43 (13%) |
Most survey participants were in the favor that targeted therapy for liver cancer will be better managed by either Gastroenterologists (48%, 154/320) or by a team of Gastroenterologist and Oncologist (47%, 149/320); while only 5% (17/320) favored that it should be managed by oncologists alone. Most (62%) respondents were comfortable in prescribing sorafenib if required. Seventy-nine percent of respondents (251/319) agreed that they put patients of HBV related HCC on anti-virals before starting their HCC treatment to prevent flares. Eighty percent (253/318) of respondents agreed that they used opioid medication in titrated dose, for pain control in HCC patients, who are terminally ill.
Future Directions for Indian National Association for the Study of Liver
When it was asked whether they felt that there was need for a registry for HCC, 88% (316/360) responded in ‘yes’; and most (87%, 312/358) said that they will contribute their HCC patients details to the registry if such a registry is set up by the INASL.
The last question of the survey was “In your opinion, how can INASL help in prevention or better management of HCC in India?” and the response was in text format. Three hundred and thirteen respondents answered this question, and the most frequent responses are shown in Table 3.
Table 3.
Most Common Text Responses to the Question “In Your Opinion, How Can INASL Help in Prevention or Better Management of HCC in India”. Total Response Count 313.
| Increase public awareness about HCC |
| Education of medical fraternity involved in management of HCC by regular CMEs |
| Develop Indian guidelines on HCC based on Indian healthcare realities |
| Promote screening for HCC and early referral of HCC patients |
| Make HCC database/registry |
| Universal immunization for hepatitis B |
Discussion
This is the first survey on management practices on HCC in India. The important points which emerged from the survey are that the incidence of HCC is increasing in India; the most common etiologic agent is Hepatitis B responsible for 43% cases; only 14% patients present in early stage when curative treatment is possible (BCLC-A); 90% of these respondents screen for HCC when they first evaluate a cirrhotic patient; while following a patient of cirrhosis most respondents screen for HCC by ultrasound and AFP at every 6 months to 1 year; and most (82%) respondents follow some international guideline for staging and treatment of HCC.
One of the important and pleasantly surprising finding was that, most physicians managing HCC in India, were following some International guidelines like EASL, AASLD, ESDO etc for staging and treatment of HCC. Since there were no Indian guidelines that could cater to Indian needs, it was physicians' personal choice which international guideline he or she followed. However, with the publication of the INASL guidelines on HCC in the present issue of the journal,2 the diagnosis and treatment of HCC is expected to be more uniform and protocol based.
The one disturbing finding of the survey was that most patients of HCC present very late especially in the BCLC stage C or D. Only 14% patients present early (BCLC-A) when curative treatment is possible. The main reason for this could be poor awareness about risk of HCC among general physicians who were primarily managing cirrhotic patients. Although most gastroenterologists of India, who answered the survey, were regularly screening their patients of cirrhosis for early detection of HCC, the same may not be true for the general physicians, who may not be using regular and adequate screening practices as is necessary for early detection of HCC. Hence there is an urgent need, especially for INASL, to spread the awareness among the primary care physicians of India about regular and effective screening practices for HCC in the patients of cirrhosis they are managing.
According to this survey, the most important etiological agent for HCC in India is hepatitis B, which accounts for 43% of cases. Fortunately, the spread of hepatitis B can be effectively prevented by vaccination. Many survey respondents suggested that INASL should take lead in spreading the awareness of universal hepatitis B immunization.
In conclusion, this survey has highlighted the need for increasing the awareness about HCC in India, especially in the medical fraternity, so that HCC can be prevented or detected early at a curable stage. Further such surveys should be carried out at periodic interval to track increasing awareness and better management practices for HCC in India.
Conflicts of interest
The author has none to declare.
References
- 1.Acharya S.K. Epidemiology of hepatocellular carcinoma in India. J Clin Exp Hepatol. 2014;4(S3):S27–S33. doi: 10.1016/j.jceh.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar A., Acharya S.K., Singh S.P. The Indian National Association for Study of the Liver (INASL) consensus on prevention, diagnosis and management of hepatocellular carcinoma in India: the Puri recommendations. J Clin Exp Hepatol. 2014;4(S3):S3–S26. doi: 10.1016/j.jceh.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Indian Society of Gastroenterology [Internet] [cited 2014 Jun 26]. Available from: http://www.isg.org.in/.


