Abstract
Background and objectives
Fluid overload is a common characteristic associated with renal progression in CKD. Additionally, fluid overload is an independent predictor of all-cause or cardiovascular mortality in patients on dialysis, but its influence on patients not on dialysis is uncertain. The aim of the study was to assess the relationship between the severity of fluid status and clinical outcomes in an advanced CKD cohort.
Design, setting, participants, & measurements
In total, 478 predialysis patients with stages 4 and 5 CKD in the integrated CKD care program were enrolled from January of 2011 to December of 2011 and followed-up until August of 2013. The clinical outcomes included cardiovascular morbidity and all-cause mortality. The relative hydration status (overhydration/extracellular water) was used as the presentation of the severity of fluid status and measured using a body composition monitor. Overhydration/extracellular water >7% was defined as fluid overload.
Results
Over a median follow-up period of 23.2 (12.6–26.4) months, 66 (13.8%) patients reached all-cause mortality or cardiovascular morbidity. The adjusted hazard ratio of the combined outcome of all-cause mortality or cardiovascular morbidity for every 1% higher overhydration/extracellular water was 1.08 (95% confidence interval, 1.04 to 1.12; P<0.001). The adjusted overhydration/extracellular water for the combined outcome of all-cause mortality or cardiovascular morbidity in participants with overhydration/extracellular water ≥7% compared with those with overhydration/extracellular water <7% was 1.93 (95% confidence interval, 1.01 to 3.69; P=0.04). In subgroup analysis, higher overhydration/extracellular water was consistently associated with increased risk for the combined outcome independent of diabetes, cardiovascular disease, and serum albumin. There was no significant interaction between all subgroups.
Conclusions
These findings suggest that fluid overload is an independent risk factor of the combined outcome of all-cause mortality or cardiovascular morbidity in patients with advanced CKD.
Keywords: cardiovascular disease, CKD, mortality
Introduction
CKD is characterized as an independent risk factor for cardiovascular morbidity and mortality (1,2). Fluid overload is a common phenomenon in patients with CKD. The abnormal fluid status increases cardiac load, contributing to increased BP, left ventricular hypertrophy, and congestive heart failure (3,4). Fluid overload has been an independent predictor of all-cause or cardiovascular mortality in patients on dialysis (5,6). Strict volume control strategies might diminish BP and progression of left ventricular hypertrophy (7) and improve the general wellbeing of patients on dialysis (8). Hence, fluid overload is an important element of progression to adverse clinical outcome in patients on dialysis.
For patients with CKD not on dialysis, only a few studies have analyzed the influence of actual fluid status on clinical performance. Some substitutes for fluid status, such as left atrial diameter and N-terminal probrain natriuretic peptide, have been positively associated with cardiovascular morbidity or all-cause mortality (9,10). However, these substitutes for fluid status are affected by intravascular hydration, cardiac dysfunction, and renal progression. Recently, bioelectric impedance spectroscopy has been used to measure fluid status in different populations and provide more precise information of body composition (11–14). Our previous report showed a significant correlation between fluid overload and renal progression (15). Hung et al. (16) suggested that fluid overload is strongly associated with traditional and nontraditional risk factors for cardiovascular disease in CKD. However, the relationship between fluid overload, cardiovascular morbidity, and all-cause mortality has not been well explored in CKD. This observational study was designed to evaluate the association of fluid overload, cardiovascular morbidity, and all-cause mortality in late-stage CKD.
Materials and Methods
Study Participants
This observational study was conducted at a hospital in southern Taiwan. This study was approved by the Institutional Review Board at Kaohsiung Medical University Hospital. All study participants with CKD stages 4 or 5 who were in our integrated CKD program for >3 months were invited to participate in the study from January of 2011 to December of 2011. CKD was staged according to Kidney Disease Outcomes Quality Initiative definitions, and the eGFR was calculated using the equation of the four-variable Modification of Diet in Renal Disease Study (17). Participants with disabilities, pacemaker implantation, and impaired skin integrity were excluded. Finally, 478 participants were enrolled and scheduled for a study interview after informed consent. No participant was excluded because of personal reasons.
Measurement of Fluid Status
To measure the severity of fluid status in study participants, the bioelectric impedance spectroscopy method (body composition monitor [BCM]; Fresenius Medical Care) was used at enrollment, which has been validated intensively against all available gold standard methods in the general population and patients on dialysis (11–14). Electrodes were attached to one hand and one foot on the ipsilateral side after the patient had been in the recumbent position for at least 5 minutes. The BCM measures impedance spectroscopy at 50 different frequencies between 5 kHz and 1 MHz. At low frequency, the current cannot penetrate cell membranes and then passes through the extracellular water (ECW) space, whereas high-frequency current flows through both ECW and intracellular water. These impedance data were used to estimate the amounts of total body water, intracellular water, and ECW using the model by Moissl et al. (12) and then to obtain the value of overhydration (OH) as absolute change in tissue hydration through a new three-component tissue-based model that includes normally hydrated lean tissue, normally hydrated adipose tissue, and excess fluid mass (18). OH is regarded as excess fluid mass. Accumulating evidence shows that the relative hydration status (ΔHS; ΔHS=OH/ECW) has been used as an indicator of fluid status (6,19); 15% ΔHS could be used as a cutoff for severe fluid overload and 6.8% could be used as a cutoff for mild fluid overload in patients on hemodialysis (6). The 90th percentile of ΔHS was 7% in the normal reference population (16). Accordingly, when ΔHS was >7%, it was classified as fluid overload (16,19). The same cutoff threshold for the definition of fluid overload has also been validated in 350 Taiwanese healthy controls (16). Thus, this study used ΔHS as the presentation of the severity of fluid status, and ΔHS>7% was defined as fluid overload.
Additionally, because BCM cannot differentiate fluid overload that is a result of increased intravascular volume or increased interstitial volume, this study also tried to define interstitial fluid volume by subtracting plasma volume from extracellular fluid volume on the basis of the report by Ebah et al. (20). The plasma volume was calculated from the hematocrit and the weight using the formulas described by Kaplan (21).
Data Collection
Demographic and clinical characteristics were obtained from interviews and medical records of study participants at enrollment. Cardiovascular disease was defined as a history of heart failure, acute or chronic ischemic heart disease, or myocardial infarction. Cerebrovascular disease was defined as a history of cerebral infarction or hemorrhage. Diabetes mellitus and hypertension were defined as those with a medical history through chart review. Information regarding patient medications, including diuretics, β-blockers, calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers, within 3 months before and after enrollment was obtained from medical records. BP was recorded as the mean of two consecutive measurements with a 5-minute interval using one single-calibrated device. Participants were asked to fast for at least 12 hours before blood sample collection for the biochemistry study, and the severity of proteinuria was measured using the urine protein-to-creatinine ratio.
Clinical Outcome
Study participants were contacted at outpatient clinics at 3-month intervals to ascertain vital status. If the contact was unsuccessful, at least three telephone calls were made to participants at his/her last-known telephone number. The clinical outcomes included all-cause mortality and cardiovascular morbidity. Cardiovascular morbidity was defined as new onset of acute myocardial infarction, acute hemorrhagic or ischemic stroke, peripheral artery disease, or hospitalization related to congestive heart failure or arrhythmia but did not include death. The information obtained by direct contact with participants and families was further supplemented by reviewing medical records and screening the data bank of the National Mortality File. Participants were censored at last contact, when initially commencing dialysis, or at the end of observation in August of 2013. Events happening after initial dialysis were excluded.
Statistical Analyses
Statistical results of baseline characteristics of all participants were stratified by 7% of △HS. Continuous variables were expressed as means±SDs or medians (25th, 75th percentiles) as appropriate, and categorical variables were expressed as percentages. Skewed distribution continuous variables were log-transformed to approximate normal distribution. The significance of differences in continuous variables between groups was tested using the independent t test or the Mann–Whitney U test as appropriate. The difference in the distribution of categorical variables was tested using the chi-squared test or the Fisher’s exact test. The difference of events between groups was analyzed using Poisson distribution. Time-to-event survival analysis by Kaplan–Meier survival curve was used to test the severity of fluid status as a predictor of the risk of the combined outcome of all-cause mortality or cardiovascular morbidity. The association between the severity of fluid status and the combined outcome of all-cause mortality or cardiovascular morbidity was assessed by a modified stepwise procedure in four modeling steps. The first model consisted of age and sex. The second model consisted of adding diabetes mellitus, cardiovascular disease, and medication, including diuretics, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers , and β-blockers or CCBs. The third model was adding renal function status, including eGFR and urine protein-to-creatinine ratio. The fourth model was entering clinical and biochemical factors, including body mass index, hemoglobin, serum albumin, log cholesterol level, and systolic BP. We also performed subgroup analysis of study participants stratified by sex, cardiovascular disease, diabetes mellitus, serum albumin, and high-sensitivity C-reactive protein (hsCRP) for the investigation of the effect of these comorbidities. Interactions between subgroups were tested. Statistical analyses were conducted using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL). Statistical significance was set at a two-sided P value <0.05.
Results
Characteristics of the Entire Cohort
Of all study participants, the median level of △HS was 7%. Table 1 shows the baseline clinical characteristics organized by the median level of △HS. Participants with △HS of 7% or more were more likely to have preexisting cerebral vascular disease, hypertension, and diabetes mellitus and received more diuretics, CCBs, and β-blockers. The significant dissimilarities in clinical characteristics between groups included serum BUN and uric acid levels and urine protein-to-creatinine ratios, which were higher in participants with △HS of 7% or more. There were lower eGFR, serum albumin, cholesterol, triglyceride, and hemoglobin levels in participants with △HS of 7% or more.
Table 1.
The clinical characteristics of study participants stratified by fluid overload
| Parameters | Entire Cohort (n=478) | △HS<7% (n=239) | △HS≥7% (n=239) | P Value |
|---|---|---|---|---|
| Demographics | ||||
| Age (yr) | 65.4±12.7 | 64.2±13.0 | 66.5±12.2 | 0.04 |
| Sex (men), % | 54.6 | 51.5 | 57.7 | 0.16 |
| Smoke, % | 20.5 | 20.9 | 20.1 | 0.82 |
| Alcohol, % | 9.8 | 10.5 | 9.2 | 0.64 |
| Cardiovascular disease, % | 18.6 | 15.9 | 21.3 | 0.12 |
| Cerebral vascular disease, % | 9.6 | 5.9 | 13.4 | <0.01 |
| Hypertension, % | 84.9 | 80.3 | 89.5 | <0.01 |
| Diabetes mellitus, % | 44.1 | 34.3 | 54.0 | <0.001 |
| Hyperlipidemia, % | 52.5 | 51.5 | 53.6 | 0.64 |
| CKD stage 4, % | 49.2 | 52.3 | 46.0 | 0.17 |
| CKD stage 5, % | 50.8 | 47.7 | 54.0 | |
| Body mass index (kg/m2) | 24.4±3.8 | 24.6±3.7 | 24.1±3.8 | 0.13 |
| Systolic BP (mmHg) | 139.6±20.3 | 133.7±17.2 | 145.4±21.6 | <0.001 |
| Diastolic BP (mmHg) | 75.5±11.6 | 76.2±11.0 | 74.9±12.3 | 0.22 |
| Body composition | ||||
| Lean tissue index (kg/m2) | 13.8±2.6 | 14.1±2.6 | 13.4±2.6 | 0.003 |
| Fat tissue index (kg/m2) | 9.8±4.2 | 10.3±4.4 | 9.4±3.9 | 0.01 |
| Total body water (L) | 32.7±6.7 | 32.3±6.0 | 33.2±7.3 | 0.12 |
| Intracellular water (L) | 17.1±3.6 | 17.5±3.4 | 16.7±3.8 | 0.02 |
| Extracellular water (L) | 15.6±3.6 | 14.8±3.1 | 16.4±3.8 | <0.001 |
| Extracellular water/total body water, % | 47.7±3.5 | 45.8±3.1 | 49.6±2.8 | <0.001 |
| Overhydration (L) | 1.0 (0.4, 2.2) | 0.4 (−0.1, 0.7) | 2.1 (1.5, 3.6) | <0.001 |
| Medications | ||||
| Diuretics, % | 29.4 | 20.5 | 38.5 | <0.001 |
| Calcium channel blocker, % | 60.0 | 49.4 | 70.7 | <0.001 |
| β-Blocker, % | 27.8 | 22.2 | 33.5 | <0.01 |
| ACEI/ARB, % | 53.1 | 53.1 | 53.2 | 0.99 |
| Laboratory parameters | ||||
| BUN (mg/dl) | 47.3 (34.3, 64.9) | 42.2 (32.5, 61.8) | 50.6 (37.5, 68.4) | <0.001 |
| eGFR (ml/min per 1.73 m2) | 15.3±7.5 | 16.1±7.9 | 14.5±7.0 | 0.02 |
| Glycated hemoglobin, % | 5.9 (5.6, 6.8) | 5.8 (5.6, 6.4) | 6.0 (5.6, 7.0) | 0.06 |
| Hemoglobin (g/dl) | 10.4±1.7 | 10.8±1.7 | 10.1±1.7 | <0.001 |
| Albumin (g/dl) | 4.0±0.4 | 4.2±0.3 | 3.9±0.5 | <0.001 |
| Calcium-phosphate product (mg2/dl2) | 38.5 (34.2, 44.0) | 38.5 (33.3, 44.1) | 38.3 (34.8, 44.1) | 0.47 |
| Uric acid (mg/dl) | 7.7±1.7 | 7.5±1.6 | 7.9±1.8 | 0.01 |
| Cholesterol (mg/dl) | 180 (153, 210) | 185 (161, 211) | 174 (146, 206) | 0.01 |
| Triglyceride (mg/dl) | 116 (80, 166) | 123 (86, 173) | 107 (74, 158) | <0.01 |
| High-sensitivity C-reactive protein (mg/L) | 1.3 (0.6, 3.6) | 1.4 (0.7, 3.0) | 1.3 (0.6, 4.0) | 0.88 |
| Parathyroid hormone (pg/ml) | 95 (50, 238) | 83 (44, 205) | 117 (58, 270) | 0.07 |
| Urine protein-to-creatinine ratio (g/g) | 1.3 (0.6, 2.8) | 1.0 (0.5, 1.7) | 2.1 (0.9, 4.4) | <0.001 |
Data are expressed as numbers (percentages) for categorical variables and means±SDs or medians (25th, 75th percentiles) for continuous variables as appropriate. Conversion factors for units: eGFR in milliliters per minute per 1.73 m2 to milliliters per second 1.73 m2, ×0.01667; hemoglobin in grams per deciliter to grams per liter, ×10; albumin in grams per deciliter to grams per liter, ×10; calcium-phosphate product in milligrams2 per deciliter2 to millimoles2 per liter2, ×0.0806; cholesterol in milligrams per deciliter to millimoles per liter, ×0.02586; triglyceride in milligrams per deciliter to millimoles per liter, ×0.01129; and uric acid in milligrams per deciliter to micromoles per liter, ×59.48. P value was measured by comparisons between participants with △HS≥7% and those with △HS<7%. ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker; △HS, relative hydration status.
Fluid Overload, All-Cause Mortality, and Cardiovascular Morbidity
Over a median follow-up period of 23.2 (12.6, 26.4) months, 66 (16.1%) participants reached the combined outcome of all-cause mortality or cardiovascular morbidity; 25 participants died, 51 participants had cardiovascular morbidity, and 10 participants had both mortality and cardiovascular morbidity during the follow-up period. The combined outcome rates were 4.4 and 14.3 combined outcome/100 patient-yr in the △HS<7% and △HS≥7% groups, respectively (Table 2). The causes of death included sepsis (10 patients), acute myocardial infarction (three patients), acute stroke (two patients), malignancy (four patients), refusal of dialysis (one patient), gastrointestinal bleeding (one patient), liver cirrhosis (one patient), trauma accident (one patient), and natural at home (two patients). No significant differences in the causes of death were found between the two groups. More participants with △HS of 7% or more had cardiovascular morbidity than those with △HS<7%. The causes of cardiovascular morbidity included acute myocardial infarction (10 patients), acute hemorrhagic or ischemic stroke (11 patients), congestive heart failure (28 patients), and peripheral artery disease (two patients). No hospitalization on the basis of arrhythmia occurred during the follow-up period. Significant differences in the causes of cardiovascular morbidity were found between the two groups. Thirteen (2.7%) participants were lost to follow-up, including five (2.1%) participants with △HS<7% and eight (3.3%) participants with △HS of 7% or more (the median follow-up period=9.9 months). There were no significant differences in proportions of loss to follow-up and clinical characteristics between the two groups.
Table 2.
Events of all participants
| Events | Entire Cohort (n=478) | △HS<7% (n=239) | △HS≥7% (n=239) | P Value |
|---|---|---|---|---|
| Patient-yr of follow-up | 763.5 | 434.4 | 329.1 | <0.001 |
| Combined outcomes per 100 patient-yr (95% CI) | 8.6 (6.7 to 11.0) | 4.4 (26.4 to 68.4) | 14.3 (10.5 to 19.0) | <0.001 |
| Cardiovascular morbidity per 100 patient-yr (95% CI) | 6.7 (5.0 to 8.8) | 3.0 (1.6 to 5.1) | 11.5 (8.2 to 15.9) | <0.001 |
| Death per 100 patient-yr (95% CI) | 3.3 (2.1 to 4.8) | 1.4 (0.5 to 3.0) | 5.8 (3.5 to 9.0) | <0.01 |
Data are expressed as numbers (percentages) for categorical variables and medians (25th, 75th percentiles) for continuous variables as appropriate. P value was measured by comparisons between participants with △HS≥7% and those with △HS<7%. 95% CI, 95% confidence interval.
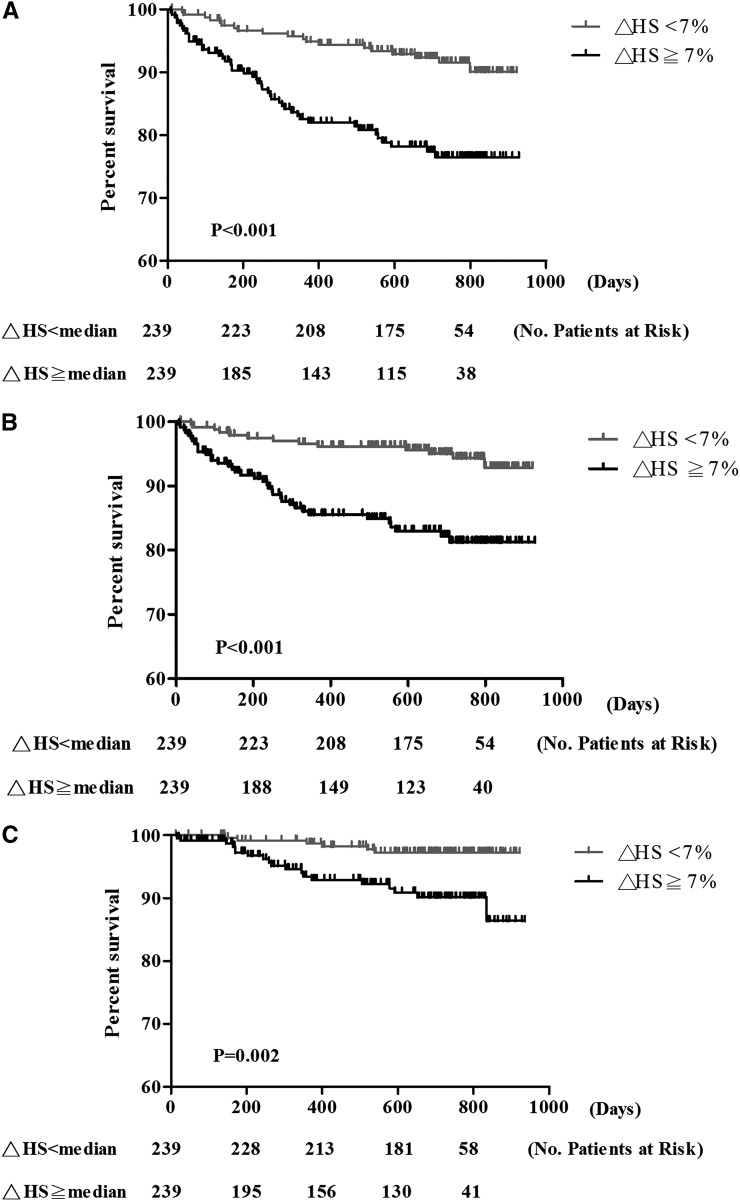
Participants with △HS of 7% or more had higher risk for the combined outcome of all-cause mortality or cardiovascular morbidity (Figure 1). The unadjusted and adjusted hazard ratios (HRs) of the combined outcome of all-cause mortality or cardiovascular morbidity for every 1% higher △HS were 1.09 (95% confidence index [95% CI], 1.07 to 1.11; P<0.001) and 1.08 (95% CI, 1.04 to 1.12; P<0.001), respectively (Table 3). The unadjusted and adjusted HRs for the combined outcome in participants with △HS of 7% or more compared with those with △HS<7% were 3.04 (95% CI, 1.78 to 5.19; P<0.001) and 1.93 (95% CI, 1.01 to 3.69; P=0.04), respectively. The adjusted HRs of the combined outcome for every 1 L higher interstitial fluid volume and plasma volume were 1.16 (95% CI, 1.06 to 1.25; P=0.001) and 2.17 (95% CI, 0.58 to 8.11; P=0.2), respectively.
Figure 1.
Kaplan–Meier survival curves for cardiovascular morbidity or all-cause mortality. (A) The combined outcome of all-cause mortality or cardiovascular morbidity. (B) Cardiovascular morbidity. (C) All-cause mortality. △HS, relative hydration status.
Table 3.
The adjusted risks for cardiovascular morbidity or all-cause mortality according to every 1% higher relative hydration status
| Relative Hydration Status | Cardiovascular Morbidity or All-Cause Mortality | Cardiovascular Morbidity | All-Cause Mortality | |||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | |
| Unadjusted model | 1.09 (1.07 to 1.11) | <0.001 | 1.10 (1.07 to 1.12) | <0.001 | 1.08 (1.04 to 1.11) | <0.001 |
| Age and sex adjusted | 1.11 (1.08 to 1.13) | <0.001 | 1.11 (1.08 to 1.14) | <0.001 | 1.10 (1.05 to 1.15) | <0.001 |
| Multivariate adjusted model 1 | 1.09 (1.06 to 1.12) | <0.001 | 1.09 (1.06 to 1.12) | <0.001 | 1.09 (1.04 to 1.14) | <0.001 |
| Multivariate adjusted model 2 | 1.07 (1.03 to 1.10) | <0.001 | 1.07 (1.03 to 1.11) | 0.001 | 1.05 (0.98 to 1.11) | 0.15 |
| Multivariate adjusted model 3 | 1.08 (1.04 to 1.12) | <0.001 | 1.11 (1.06 to 1.16) | <0.001 | 1.03 (0.96 to 1.10) | 0.38 |
Multivariate model 1 is adjusted for age, sex, diabetes mellitus, cardiovascular disease, diuretics use, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers use, β-blocker, and calcium channel blocker use. Multivariate model 2 comprises model 1 as well as eGFR and log urine protein-to-creatinine ratio. Multivariate model 3 comprises model 2 as well as body mass index, serum albumin, log cholesterol, hemoglobin levels, and systolic BP.
The unadjusted and adjusted HRs of cardiovascular morbidity for every 1% higher △HS were 1.10 (95% CI, 1.07 to 1.12; P<0.001) and 1.11 (95% CI, 1.06 to 1.16; P<0.001), respectively. The unadjusted and adjusted HRs for cardiovascular morbidity in participants with △HS of 7% or more compared with those with △HS<7% were 3.47 (95% CI, 1.84 to 6.52; P<0.001) and 2.70 (95% CI, 1.19 to 6.10; P=0.01), respectively. The adjusted HRs of cardiovascular morbidity for every 1 L higher interstitial fluid volume and plasma volume were 1.18 (95% CI, 1.08 to 1.28; P<0.001) and 3.39 (95% CI, 0.76 to 15.02; P=0.10), respectively.
The univariate regression analysis showed that the increase in △HS was associated with a significant increase in reaching all-cause mortality (HR, 1.08; 95% CI, 1.04 to 1.11; P<0.001). Participants with △HS of 7% or more had higher risk for all-cause mortality than those with △HS<7% (P=0.002) (Figure 1). However, there was no significant association between increased △HS and all-cause mortality in multivariate analysis.
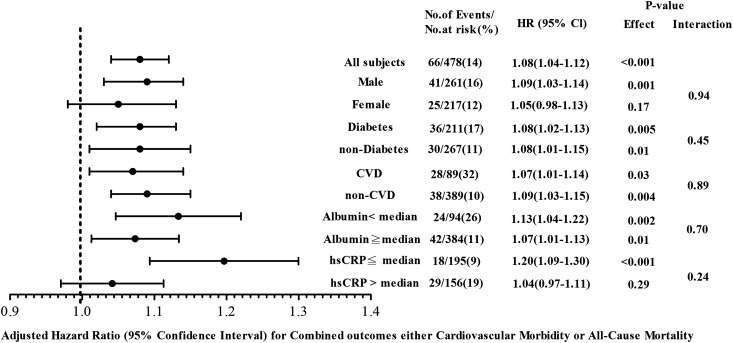
In subgroup analysis, higher △HS was consistently associated with increased risk for all-cause mortality or cardiovascular morbidity independent of cardiovascular disease, diabetes, and serum albumin. The association was not significant in women and the hsCRP more than the median group (Figure 2). No significant interaction was found between all subgroups.
Figure 2.
Adjusted hazard ratios (HRs) for combined outcome, cardiovascular morbidity, and all-cause mortality per 1% greater relative hydration status in all participants stratified by sex, diabetes mellitus, cardiovascular disease (CVD), and serum albumin. Ratios were adjusted for age, sex, diabetes mellitus, CVD, diuretics use, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers use, β-blocker, calcium channel blocker use, eGFR, log urine protein-to-creatinine ratio, body mass index, serum albumin, log cholesterol, hemoglobin levels, and systolic BP. The median values of serum albumin and high-sensitivity C-reactive protein (hsCRP) are 3.8 g/dl and 1.3 mg/L, respectively. 95% CI, 95% confidence interval.
Discussion
This study is the first to show that fluid overload measured by BCM is associated with cardiovascular morbidity or all-cause mortality in patients with stages 4 and 5 CKD after adjustment of associated risk factors. The risk for cardiovascular morbidity or all-cause mortality increases by 8% for every 1% higher △HS. Fluid overload is a significant risk factor for adverse clinical outcome in late CKD.
Fluid overload is one of the major complications in late CKD. Fluid overload has independent influences on the vascular and endothelial levels, contributing to arterial stiffness, atherosclerosis, and left ventricular hypertrophy (22). Cardiomyocyte elongation, hypertrophy, and dysfunction occur during left ventricle remodeling and decompensation response to fluid overload (23,24). Accumulating evidence shows a strong association between fluid overload and impaired cardiac function, and removal of excess volume induces the reduction of left ventricular mass index (25,26). CKD and heart disease frequently coexist, and the interaction between kidney and heart disease is complex and indefinable (27). It is difficult to distinguish the influence of CKD or heart disease on the association of fluid overload with adverse clinical outcome. We adjusted heart disease history and baseline renal function in multivariate analysis, and the association between fluid overload and cardiovascular morbidity or all-cause mortality is also consistent in the presence or absence of heart disease. Fluid overload is probably a significant predictor of adverse clinical outcome independent of heart disease.
Aside from cardiovascular effect, fluid overload has been associated with activation of malnutrition and inflammation (16,28). Inflammation has played a key role in the pathophysiologic pathway, progression to atherosclerosis, and cardiac dysfunction. It is difficult to evaluate whether malnutrition or inflammation is a cause or consequence of fluid overload. Our subgroup analysis revealed a significant association between fluid overload and adverse outcome independent of serum albumin and in participants with the median of hsCRP or less. Although the result is not consistent in those of hsCRP more than the median, it seems to be a trend in the association between fluid overload and adverse outcome. Additional study is needed to evaluate the interaction between inflammation, fluid overload, and clinical outcome in late-stage CKD.
In our study, infection is the leading cause of mortality rather than cardiovascular disease. Compared with populations in Western countries (29,30), cardiovascular morbidity and mortality occur less frequently in Asians, probably resulting in a higher likelihood of Asian patients with CKD progressing to commencing dialysis rather than dying of cardiovascular disease (31). Bowel wall edema and ischemia have been reported as sequelae of fluid overload (32), thereby resulting in the increase in gut permeability, destroying protective barriers, and admitting overgrowth of pathogenic species (33). Additionally, brain natriuretic peptide as a surrogate of fluid status has a physiologic role in modulating components of the innate immune system, including diminishing the total numbers of monocytes, B cells, and natural killer cells and impairing natural killer cell cytotoxicity (34). According to the above mechanism, fluid overload might be associated with immunologic deficiency and increased risk for infection. Additional study is needed to evaluate the cross-link between fluid status and infection. Although the cause of death seems to be different in our cohort compared with other populations, our results show a significant association of fluid overload with cardiovascular events. Fluid overload could be regarded as a risk factor of adverse outcome in different populations.
Fluid status evaluated by BCM is a result of intra- or extracellular volume. The device cannot differentiate increased extracellular fluid volume that is a result of increased intravascular volume from increased interstitial volume. Our results show a significant association of cardiovascular morbidity or all-cause mortality with interstitial fluid volume instead of plasma volume. It is probable that the correlation between abnormal fluid distribution and clinical outcome is more important than that between fluid amount and clinical outcome in CKD. Fluid overload caused by interstitial fluid may result from endothelial leak or expanded plasma volume. Under some conditions, such as diabetic vasculopathy and ischemia-reperfusion injury, the integrity of the endothelium is disturbed, leading to leakage of fluid into the extravascular space (35,36). Pro-permeability factors, such as thrombin, hydrogen peroxide, or inflammatory stimuli (e.g., TNF-α), induce paracellular vascular leak by perturbation of the cell-cell junctions between endothelial cells and cytoskeletal contraction, leading to widening intracellular space (37,38). Additional study is necessary to evaluate the influence of endothelial leakage on interstitial fluid overload and the mechanism between interstitial fluid overload and adverse outcome.
Because there is a significant relationship between fluid overload and adverse outcome as well as the improvement of BP and cardiac function after removal of excess volume (7,26,39), physicians need to pay more attention to monitoring of fluid status and controlling of fluid volume. Physical examination is not efficient for detection of small increases in volume status (40). The low cost and availability of bioimpedance measurement might make it an adequate tool for fluid evaluation in a large CKD population.
This study has several limitations that must be considered. First, this was a single-center study. Second, fluid status, clinical parameters, and use of drugs were measured only one time (at enrollment). The association of time-variable fluid status, clinical parameters, and use of drugs with clinical outcome could not be estimated. Third, this study did not measure urine sodium and sodium intake, and positive sodium balance may increase arterial pressure and contribute edema formation (41,42). The effect of sodium retention on fluid status and clinical outcome may be underestimated. Fourth, the follow-up period was relatively short. The median follow-up time was around 23.2 months. This limitation may confound the interpretation of the association between fluid overload and mortality.
In conclusion, our study shows that fluid overload is associated with increased risks for all-cause mortality or cardiovascular morbidity in patients with stages 4 and 5 CKD. Prospective randomized control trials, ideally double-blind, are needed to evaluate whether strict volume control may improve clinical outcome in CKD.
Disclosures
None.
Acknowledgments
The authors thank the Statistical Analysis Laboratory, Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung Medical University for help.
The research presented in this article was supported by the grant from Kaohsiung Medical University Research Foundation (KMU-Q103011).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Is Fluid Overload as Measured by Bioimpedance Spectroscopy Harmful in CKD—If So, Why?,” on pages 1–3.
References
- 1.Meguid El Nahas A, Bello AK: Chronic kidney disease: The global challenge. Lancet 365: 331–340, 2005 [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351: 1296–1305, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Wizemann V, Leibinger A, Mueller K, Nilson A: Influence of hydration state on plasma volume changes during ultrafiltration. Artif Organs 19: 416–419, 1995 [DOI] [PubMed] [Google Scholar]
- 4.Wizemann V, Schilling M: Dilemma of assessing volume state—the use and the limitations of a clinical score. Nephrol Dial Transplant 10: 2114–2117, 1995 [PubMed] [Google Scholar]
- 5.Paniagua R, Ventura MD, Avila-Díaz M, Hinojosa-Heredia H, Méndez-Durán A, Cueto-Manzano A, Cisneros A, Ramos A, Madonia-Juseino C, Belio-Caro F, García-Contreras F, Trinidad-Ramos P, Vázquez R, Ilabaca B, Alcántara G, Amato D: NT-proBNP, fluid volume overload and dialysis modality are independent predictors of mortality in ESRD patients. Nephrol Dial Transplant 25: 551–557, 2010 [DOI] [PubMed] [Google Scholar]
- 6.Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C, Malecka-Masalska T, Marcelli D: The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant 24: 1574–1579, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hur E, Usta M, Toz H, Asci G, Wabel P, Kahvecioglu S, Kayikcioglu M, Demirci MS, Ozkahya M, Duman S, Ok E: Effect of fluid management guided by bioimpedance spectroscopy on cardiovascular parameters in hemodialysis patients: A randomized controlled trial. Am J Kidney Dis 61: 957–965, 2013 [DOI] [PubMed] [Google Scholar]
- 8.Ozkahya M, Ok E, Toz H, Asci G, Duman S, Basci A, Kose T, Dorhout Mees EJ: Long-term survival rates in haemodialysis patients treated with strict volume control. Nephrol Dial Transplant 21: 3506–3513, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Chen SC, Chang JM, Liu WC, Huang JC, Tsai JC, Lin MY, Su HM, Hwang SJ, Chen HC: Echocardiographic parameters are independently associated with increased cardiovascular events in patients with chronic kidney disease. Nephrol Dial Transplant 27: 1064–1070, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Desai AS, Toto R, Jarolim P, Uno H, Eckardt KU, Kewalramani R, Levey AS, Lewis EF, McMurray JJ, Parving HH, Solomon SD, Pfeffer MA: Association between cardiac biomarkers and the development of ESRD in patients with type 2 diabetes mellitus, anemia, and CKD. Am J Kidney Dis 58: 717–728, 2011 [DOI] [PubMed] [Google Scholar]
- 11.Wabel P, Chamney P, Moissl U, Jirka T: Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif 27: 75–80, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, Korth O, Müller MJ, Ellegård L, Malmros V, Kaitwatcharachai C, Kuhlmann MK, Zhu F, Fuller NJ: Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27: 921–933, 2006 [DOI] [PubMed] [Google Scholar]
- 13.Crepaldi C, Soni S, Chionh CY, Wabel P, Cruz DN, Ronco C: Application of body composition monitoring to peritoneal dialysis patients. Contrib Nephrol 163: 1–6, 2009 [DOI] [PubMed] [Google Scholar]
- 14.Wizemann V, Rode C, Wabel P: Whole-body spectroscopy (BCM) in the assessment of normovolemia in hemodialysis patients. Contrib Nephrol 161: 115–118, 2008 [DOI] [PubMed] [Google Scholar]
- 15.Tsai YC, Tsai JC, Chen SC, Chiu YW, Hwang SJ, Hung CC, Chen TH, Kuo MC, Chen HC: Association of fluid overload with kidney disease progression in advanced CKD: A prospective cohort study. Am J Kidney Dis 63: 68–75, 2014 [DOI] [PubMed] [Google Scholar]
- 16.Hung SC, Kuo KL, Peng CH, Wu CH, Lien YC, Wang YC, Tarng DC: Volume overload correlates with cardiovascular risk factors in patients with chronic kidney disease. Kidney Int 85: 703–709, 2014 [DOI] [PubMed] [Google Scholar]
- 17.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D, Modification of Diet in Renal Disease Study Group : A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Chamney PW, Wabel P, Moissl UM, Müller MJ, Bosy-Westphal A, Korth O, Fuller NJ: A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr 85: 80–89, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Van Biesen W, Williams JD, Covic AC, Fan S, Claes K, Lichodziejewska-Niemierko M, Verger C, Steiger J, Schoder V, Wabel P, Gauly A, Himmele R, EuroBCM Study Group : Fluid status in peritoneal dialysis patients: The European Body Composition Monitoring (EuroBCM) study cohort. PLoS ONE 6: e17148, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ebah LM, Wiig H, Dawidowska I, O’Toole C, Summers A, Nikam M, Jayanti A, Coupes B, Brenchley P, Mitra S: Subcutaneous interstitial pressure and volume characteristics in renal impairment associated with edema. Kidney Int 84: 980–988, 2013 [DOI] [PubMed] [Google Scholar]
- 21.Kaplan AA: A simple and accurate method for prescribing plasma exchange. ASAIO Trans 36: M597–M599, 1990 [PubMed] [Google Scholar]
- 22.Bock JS, Gottlieb SS: Cardiorenal syndrome: New perspectives. Circulation 121: 2592–2600, 2010 [DOI] [PubMed] [Google Scholar]
- 23.Ryan TD, Rothstein EC, Aban I, Tallaj JA, Husain A, Lucchesi PA, Dell’Italia LJ: Left ventricular eccentric remodeling and matrix loss are mediated by bradykinin and precede cardiomyocyte elongation in rats with volume overload. J Am Coll Cardiol 49: 811–821, 2007 [DOI] [PubMed] [Google Scholar]
- 24.Grossman W, Jones D, McLaurin LP: Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Invest 56: 56–64, 1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fagugli RM, Reboldi G, Quintaliani G, Pasini P, Ciao G, Cicconi B, Pasticci F, Kaufman JM, Buoncristiani U: Short daily hemodialysis: Blood pressure control and left ventricular mass reduction in hypertensive hemodialysis patients. Am J Kidney Dis 38: 371–376, 2001 [DOI] [PubMed] [Google Scholar]
- 26.Zamboli P, De Nicola L, Minutolo R, Chiodini P, Crivaro M, Tassinario S, Bellizzi V, Conte G: Effect of furosemide on left ventricular mass in non-dialysis chronic kidney disease patients: A randomized controlled trial. Nephrol Dial Transplant 26: 1575–1583, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R: Cardiorenal syndrome. J Am Coll Cardiol 52: 1527–1539, 2008 [DOI] [PubMed] [Google Scholar]
- 28.Menon V, Gul A, Sarnak MJ: Cardiovascular risk factors in chronic kidney disease. Kidney Int 68: 1413–1418, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Weiner DE, Tabatabai S, Tighiouart H, Elsayed E, Bansal N, Griffith J, Salem DN, Levey AS, Sarnak MJ: Cardiovascular outcomes and all-cause mortality: Exploring the interaction between CKD and cardiovascular disease. Am J Kidney Dis 48: 392–401, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Manjunath G, Tighiouart H, Coresh J, Macleod B, Salem DN, Griffith JL, Levey AS, Sarnak MJ: Level of kidney function as a risk factor for cardiovascular outcomes in the elderly. Kidney Int 63: 1121–1129, 2003 [DOI] [PubMed] [Google Scholar]
- 31.Hwang SJ, Lin MY, Chen HC, Hwang SC, Yang WC, Hsu CC, Chiu HC, Mau LW: Increased risk of mortality in the elderly population with late-stage chronic kidney disease: A cohort study in Taiwan. Nephrol Dial Transplant 23: 3192–3198, 2008 [DOI] [PubMed] [Google Scholar]
- 32.Lundsgaard-Hansen P, Blauhut B: Relation of hypoxia and edema of the intestinal wall and skin to colloid osmotic pressure. Anaesthesist 37: 112–119, 1988 [PubMed] [Google Scholar]
- 33.McIntyre CW, Harrison LE, Eldehni MT, Jefferies HJ, Szeto CC, John SG, Sigrist MK, Burton JO, Hothi D, Korsheed S, Owen PJ, Lai KB, Li PK: Circulating endotoxemia: A novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol 6: 133–141, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shaw SM, Fildes JE, Puchałka CM, Basith M, Yonan N, Williams SG: BNP directly immunoregulates the innate immune system of cardiac transplant recipients in vitro. Transpl Immunol 20: 199–202, 2009 [DOI] [PubMed] [Google Scholar]
- 35.Mehta D, Malik AB: Signaling mechanisms regulating endothelial permeability. Physiol Rev 86: 279–367, 2006 [DOI] [PubMed] [Google Scholar]
- 36.Kumar P, Shen Q, Pivetti CD, Lee ES, Wu MH, Yuan SY: Molecular mechanisms of endothelial hyperpermeability: Implications in inflammation. Expert Rev Mol Med 11: e19, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McKenzie JA, Ridley AJ: Roles of Rho/ROCK and MLCK in TNF-alpha-induced changes in endothelial morphology and permeability. J Cell Physiol 213: 221–228, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Moy AB, Blackwell K, Kamath A: Differential effects of histamine and thrombin on endothelial barrier function through actin-myosin tension. Am J Physiol Heart Circ Physiol 282: H21–H29, 2002 [DOI] [PubMed] [Google Scholar]
- 39.Moissl U, Arias-Guillén M, Wabel P, Fontseré N, Carrera M, Campistol JM, Maduell F: Bioimpedance-guided fluid management in hemodialysis patients. Clin J Am Soc Nephrol 8: 1575–1582, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Essig M, Escoubet B, de Zuttere D, Blanchet F, Arnoult F, Dupuis E, Michel C, Mignon F, Mentre F, Clerici C, Vrtovsnik F: Cardiovascular remodelling and extracellular fluid excess in early stages of chronic kidney disease. Nephrol Dial Transplant 23: 239–248, 2008 [DOI] [PubMed] [Google Scholar]
- 41.Guyton AC: Roles of the kidneys and fluid volumes in arterial pressure regulation and hypertension. Chin J Physiol 32: 49–57, 1989 [PubMed] [Google Scholar]
- 42.Safar ME, London GM, Plante GE: Arterial stiffness and kidney function. Hypertension 43: 163–168, 2004 [DOI] [PubMed] [Google Scholar]