Abstract
Since Baskin et al. reported the first documented case of failure of a laparoscopically-induced ventriculoperitoneal shunt (VP) in 1998, the cerebrospinal fluid shunt has been generally considered a relative contraindication to laparoscopy. Although the literature is limited there is a small body of evidence indicating that it is safe to perform laparoscopic surgery on these patients with routine anaesthetic monitoring.
In this study we report the case of a laparoscopic cholecystectomy in the presence of a ventriculoperitoneal shunt. A review of the literature suggests that laparoscopic cholecystectomy can be safely performed in patients with a ventriculoperitoneal shunt. The only related contraindication should be if a catheter has recently been placed.
Keywords: Miniinvasive surgery, Entriculoperitoneal shunt
1. Introduction
Hydrocephalus is an abnormal build-up of the cerebrospinal fluid (CBF) in the ventricles of the brain [1]. The incidence of hydrocephalus is around 0.9–1.5 cases per 1000 births. The aetiology is variable and includes acqueductal stenosis, myelomeningocele, intraventricular bleeding, meningitis, tumour, and head injury. The treatment of hydrocephalus involves the shunting of cerebrospinal fluid to another area of the body, which is commonly the abdominal cavity. Ventriculoperitoneal shunting is the most common approach because the placement of the distal catheter is simple from a technical standpoint and surgical revision is rare [2], [3], [4], [5].
Since Baskin et al. reported the first documented case of failure of a laparoscopically-induced ventriculoperitoneal shunt (VP) in 1998, the cerebrospinal fluid shunt has been generally regarded as a relative contraindication to laparoscopy [1]. Intra-abdominal insufflation may cause an increase in intracranial pressure that can result in hindbrain herniation.
Here, we report on a clinical case of a laparoscopic cholecyctectomy performed in the presence of a VP shunt without any complication. Even if only a few cases are reported in the literature on laparoscopy in patients with ventriculoperitoneal shunts, improvements in ventricular shunting techniques have improved the survival rate of patients with hydrocephalus. Thus they are more likely to require abdominal surgery. To support our point we report on a review of the medical literature, and we believe that VP should not be a total contraindication to laparoscopy (Table 1).
Table 1.
Cholecystectomy upon patients with a ventriculoperitoneal shunt has seldom been described. The table details the current reports from literature and the outcome observed.
| Relevant literature and clinical outcomes | |||
|---|---|---|---|
| Year | Author | N | Outcome |
| 1992 | Schwed et al. | 1 case | Massive subcutaneous emphysema |
| 1995 | Collure et al. | 4 cases | No complications |
| 1998 | Baskin et al. | 1 case | Ventriculoperitoneal shunt failure |
| 2001 | Kerwat et al. | 1 case | No complications |
| 2006 | Martinez Ramos et al. | 1 case | No complications |
| 2011 | Allam et al. | 14 cases | 8 converted to open procedures |
| 2012 | Magnani et al. | 1 case | No complications |
2. Case presentation
A 41-year-old Caucasian male presented to the outpatient ward of our surgery department for an occasional diagnosis of gallbladder polyps.
The patient's medical past history had a particular focus upon the onset of meningitis, which occurred the year before the diagnosis of gallbladder polyps. This condition led to a Magendie foramina occlusion with hydrocephalus. The treatment was a ventriculoperitoneal shunt that was placed without any neurological complication (Depuy Codman Hakim programmable valve + Bactiseal catheter. Codman & Shutleff Inc. Raynham, MA. USA).
Later on the patient had a routine medical consultation. He did not report any abdominal pain or febrile episodes, and the physical examination was unremarkable. An abdominal US showed the presence of multiple gallbladder polyps and a common bile duct of normal diameter without stones. No abnormal values were found by routine blood tests, including full blood count, CRP, amylase, electrolytes, kidney and liver function test. Chest X-ray confirmed the presence of a ventriculoperitoneal shunt catheter passing through the right side of the chest; EKG showed sinus rhythm with 1st degree atrio-ventricular block. A neurosurgical consultation was performed to verify the correct function of the shunt valve.
The patient gave informed consent for laparoscopic cholecystectomy, after a formal discussion about the possible evolution of polyps and the risk of surgery. The eventual conversion to open surgery was explained as well (Fig. 1). Prophylactic antibiotic (cefazolin 2 g) was given intravenously 30 min before starting the surgical incision. Pneumoperitoneum was achieved by an open access technique with an incision near the right side of the umbilicus and the insertion of a Hasson trocar. The maximum insufflation pressure was maintained at 12 mm Hg for the duration of the procedure (55 min). The shunt catheter was found in the right-upper side of the abdomen during the intra-abdominal exploration with a 30° laparoscopic optic. A routine laparoscopic cholecystectomy was performed without complications using the French technique. No drainage was placed.
Fig. 1.
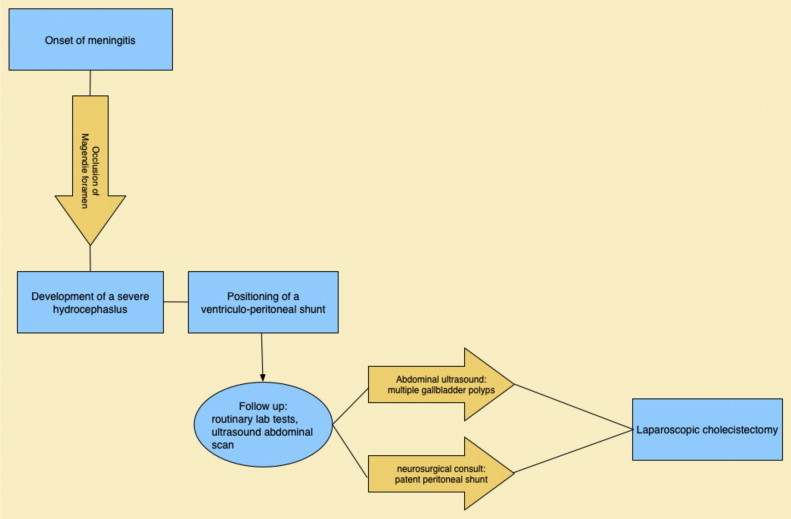
Diagnostic cascade – clinical history at a glance.
The postoperative course was uneventful and the patient remained neurologically stable. He was discharged on the third postoperative day. The postoperative follow-up, two weeks later, demonstrated a satisfactory and stable outcome.
The histology reported the specimen to be a chronically inflamed gallbladder containing several polyps (maximum diameter 1 cm).
3. Discussion
In 1998, Gaskill et al. published a new technique for laparoscopic surgery in patients with a ventriculoperitoneal shunt (VPS). In that report they clamped the shunt tubing with a rubber-shod haemostat through a skin incision in the ninth rib and then they insufflated the peritoneum using a Verres needle. Before Gaskill's report and since laparoscopic surgery has became the standard approach in a growing number of surgical operations, several case reports have highlighted the hazard of laparoscopic technique in patients with VPS. In particular the development of severe thoracic subcutaneous emphysema with compromised ventilation and increase in intracranial pressure has been reported. A clinical experience published by Uzzo et al. in the 1997 described the potential adverse effects of the laparoscopic surgery, monitoring the intracranial pressure in two children with an Arnold-Chiari malformation [5], [6], [7], [8]. They underlined that the potential mechanism of increase in the intracranial pressure during laparoscopy is due to an increased outflow resistance (the cerebrospinal fluid is secreted at 1–2 ml per kg-1 per min) or (though less likely) a retrograde flow. Theoretically, high intra-abdominal pressure may directly obstruct the antegrade cerebrospinal fluid flow and the retrograde passage of carbon dioxide gas may result in a sudden increase in intracranial pressure. The combined effect of hypercapnia-induced cerebral arterial dilatation, and venous pressure elevation generated by abdominal pressure may cause increased intracranial blood volume and increased intra-pressure in the fixed volume of the cranium.
While the very original shunting equipment was quite similar to a simple catheter, quite soon a no-reflow valve was added. This design was effective and did not change significantly thereafter. Thus the risk of a sharp rise of the intracranial pressure has possibly been over-evaluated.
The patient in our study had a remarkably routine laparoscopic procedure and we did not place any clamp since the shunting device did not allow a reflow. We believe that such an approach should be standard.
Yet we do suggest paying careful attention to possible effects of the abdominal pressure, for it could not invert the flow while still inducing an obstacle to the correct drainage.
The elevated intracranial pressure in pneumoperitoneum seems to be a risk only during a long procedure (more than three hours). In 1995, Collure et al. reported four cases of laparoscopic cholecystectomy without any complication and they determined that it was unlikely that a pneumocephalus would be produced by CO2 insufflation at a pressure of 10–15 mmHg [2], [9], [10]. But in the late nineties, Baskin et al. reported a case history of a ventriculoperitoneal shunt failure as a complication of laparoscopic cholecystectomy. After Baskin, few reports of laparoscopic surgery performed on adults and children have been reported. In particular, a series of 10 laparoscopic procedures in children with ventriculoperitoneal shunts appeared in 2000 by Walker et al. In this report the researchers conclude that the laparoscopic abdominal surgery can be safely performed on children without an increase in technical or shunt-related complications [11], [12]. In the same year, Jackman et al. reviewed the existing data and concluded that specific recommendations on the intra-operative condition of patients with a ventriculoperitoneal shunt are premature. An in vitro study found that none of the last generation valves tested showed any signs of leakage associated with increased gaseous back pressure below a value of 80 mm Hg.
Based on the available data and this case we suggest that laparoscopic cholecystectomy can be safely performed on patients with a ventriculoperitoneal shunt. We also believe that a consultation with a neurosurgeon before the operation is advisable in order to verify the correct function of the shunt valve. The only relative contraindication should if a catheter has recently been placed.
Declaration of competing interests
The authors declare that they have no competing interests.
Funding
We did not used any sources of funding for the present work.
Consent to publish
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author contributions
Lorenzo Cobianchi: wrote the paper.
Tommaso Dominioni: wrote the paper.
Claudia Filisetti: data collection and description of the clinical case.
Giovanna Riccipetitoni: review and interpretation.
Sandro Zonta: data collection and description of the clinical case.
Paolo Dionigi: review and interpretation.
Mario Alessiani: general review.
References
- 1.Baskin J.J., Vishteh A.G., Wesche D.E., Rekate H.L., Carrion C.A. Ventriculoperitoneal shunt failure as a complication of laparoscopic surgery. JSLS. 1998 Apr–Jun;2(2):177–180. [PMC free article] [PubMed] [Google Scholar]
- 2.Schwed D.A., Edoga J.K., McDonnell T.E. Ventilatory impairment during laparoscopic cholecystectomy in a patient with a ventriculoperitoneal shunt. J Laparoendosc Surg. 1992 Feb;2(1):57–59. doi: 10.1089/lps.1992.2.57. [DOI] [PubMed] [Google Scholar]
- 3.Uzzo R.G., Bilsky M., Mininberg D.T., Poppas D.P. Laparoscopic surgery in children with ventriculoperitoneal shunts: effect of pneumoperitoneum on intracranial pressure–preliminary experience. Urology. 1997 May;49(5):753–757. doi: 10.1016/S0090-4295(97)00233-1. [DOI] [PubMed] [Google Scholar]
- 4.Al-Mufarrej F., Nolan C., Sookhai S., Broe P. Laparoscopic procedures in adults with ventriculoperitoneal shunts. Surg Laparosc Endosc Percutan Tech. 2005 Feb;15(1):28–29. doi: 10.1097/01.sle.0000153733.78227.8f. [DOI] [PubMed] [Google Scholar]
- 5.Gaskill S.J., Cossman R.M., Hickman M.S., Marlin A.E. Laparoscopic surgery in a patient with a ventriculoperitoneal shunt: a new technique. Pediatr Neurosurg. 1998 Feb;28(2):106–107. doi: 10.1159/000028631. [DOI] [PubMed] [Google Scholar]
- 6.Kerwat R.M., Murali Krishnan V.P., Appadurai I.R., Rees B.I. Laparoscopic cholecystectomy in the presence of a lumboperitoneal shunt. J Laparoendosc Adv Surg Tech A. 2001 Feb;11(1):37–39. doi: 10.1089/10926420150502922. [DOI] [PubMed] [Google Scholar]
- 7.Lückers O., Born J.D., Denoel A. Pneumoperitoneum and intracranial pressure. An unrecognized relation. Rev Med Liege. 1997 Nov;52(11):712–714. French. No abstract available. [PubMed] [Google Scholar]
- 8.Collure D.W., Bumpers H.L., Luchette F.A., Weaver W.L., Hoover E.L. Laparoscopic cholecystectomy in patients with ventriculoperitoneal (VP) shunts. Surg Endosc. 1995 Apr;9(4):409–410. doi: 10.1007/BF00187161. [DOI] [PubMed] [Google Scholar]
- 9.Martínez Ramos D., Gibert Gerez J., Salvador Sanchís J.L. Laparoscopic surgery in patients with a ventriculoperitoneal shunt. Rev Esp Enferm Dig. 2006 Oct;98(10):795–796. doi: 10.4321/s1130-01082006001000015. [DOI] [PubMed] [Google Scholar]
- 10.Barina A.R., Virgo K.S., Mushi E., Bahadursingh A.M., Johnson F.E. Appendectomy for appendicitis in patients with a prior ventriculoperitoneal shunt. J Surg Res. 2007;141:40–44. doi: 10.1016/j.jss.2007.02.039. [DOI] [PubMed] [Google Scholar]
- 11.Allam E., Patel A., Lewis G., Mushi E., Audisio R.A., Virgo K.S. Cholecystectomy in patients with prior ventriculoperitoneal shunts. Am J Surg. 2011 Apr;201(4):503–507. doi: 10.1016/j.amjsurg.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Magnani C., Berti P., Lucchi A., Maffi M.F., Vandi F., Gabbianelli C. Laparoscopic cholecystectomy in adult with ventriculoperitoneal shunt: report of a case and review of the literature. Minerva Chir. 2012 Apr;67(2):205–208. [PubMed] [Google Scholar]


