Abstract
Background
The objectives of this study are to examine the prevalence of disorder-specific mental health service use for mood and anxiety disorders, and relationships between helpseeking and age, sex, and psychiatric comorbidity.
Methods
The authors used Wave 2 data from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC), which included 34,653 adults. Cross tabulations provided helpseeking prevalence rates for five anxiety disorders and three mood disorders by age and sex, as well as for individuals with and without comorbid anxiety and mood disorders. Logistic regression analyses explored the likelihood of helpseeking among younger and middle-aged adults in comparison to older adults.
Results
The prevalence of helpseeking was highest for panic disorder (45.3%) and dysthymia (44.5%) and lowest for specific phobias (7.8%). For each condition except panic disorder service use was most likely among middle-aged adults and especially unlikely among older individuals. Sex differences in treatment seeking favoring women showed only modest variability with age. Finally, the prevalence of helpseeking was generally lower among individuals without comorbid anxiety or mood disorders, and the hill-shaped influence of age on service use was attenuated in this pure group.
Conclusions
The results of this study highlight the highest prevalence of disorder-specific service use among middle-aged adults and women, and among individuals with panic disorder and dysthymia. For purposes of identifying groups who are in need of targeted efforts to increase service use, helpseeking was especially unlikely among people suffering from specific phobia, as well as among men and older adults.
Keywords: mental health services, prevalence, mental disorders, aged, epidemiology
Despite increasing rates of mental health service use in recent decades, the majority of individuals with clinically significant mental health problems still do not seek professional help (1–3). Furthermore, certain demographic groups, such as older adults and men, are especially unlikely to seek mental health services. With respect to age, a wealth of data suggests a hill-shaped distribution, with middle-aged adults being more likely to seek help than younger and especially older adults (4–7). Furthermore, the low likelihood of older adults seeking mental health services is evident even after controlling for other sociodemographic variables, health insurance coverage, psychiatric disorders, number of chronic medical conditions, poor physical health, and perceived need for care (8).
With respect to sex, men consistently use fewer mental health services than women. Although sex differences are reliably found in the general population (4, 6, 9), the effects of sex on service use in later life is more equivocal. Various studies have found that older women are approximately 1.5 times more likely to seek professional help than older men (8, 10), that there are no significant sex differences in service use in late life (11, 12), or that women’s greater likelihood of helpseeking decreases with age, such that men over the age of 80 are more likely to seek mental health services than women over the age of 80 (13).
In addition to confusion about sex differences in mental health service use later in life, existing mental health service use research is limited in two other important ways. First, relatively few studies have examined disorder-specific mental health service use. National surveys typically ask whether respondents have used a variety of services over the past 12 months for general problems with emotions or use of substances. Researchers then explore the prevalence of helpseeking for these general problems among those with disorders rather than examining disorder-specific treatment. This distinction is important given that treatment within the past year specifically for panic attacks (14) and social anxiety disorder (15) is roughly two thirds less likely than general mental health treatment among individuals with those mental health problems. Given the high degree of overlap between mood and anxiety disorders (16) a second related limitation is that researchers have not examined associations between psychiatric comorbidity and helpseeking for specific disorders. So although we know that comorbid mood and anxiety disorders are especially likely to result in helpseeking (4, 17), we do not yet understand the associations between psychiatric comorbidity and disorder-specific treatment seeking.
The first objective of the current study is to explore the prevalence of disorder-specific mental health service use for mood and anxiety disorders using a nationally representative sample of community dwelling adults. Our second objective is to investigate differences in this service use across the adult lifespan. Our third objective is to examine whether there are sex differences in helpseeking by age, and our final objective is to investigate the prevalence of disorder-specific helpseeking for individuals who do not have comorbid mood or anxiety disorders. Based on previous research we expect to find especially low estimates of service use among individuals with anxiety disorders, older adults, men, and individuals who do not have psychiatric comorbidity.
Methods
Sample
We used data from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (18), conducted by the U.S. National Institute on Alcohol Abuse and Alcoholism. Wave 1 of the NESARC is described in detail elsewhere (19, 20). The first wave was collected in 2001–2002, had a 81.0% response rate, and included 43,093 respondents from a representative sample of community-dwelling adults aged 18 years and older residing in the United States. The Wave 2 NESARC is a longitudinal follow-up to Wave 1 and was collected between August 2004 and September 2005. We chose to analyze data from Wave 2 because the first wave did not assess post-traumatic stress disorder. The NESARC oversampled adults aged 18–24, Non-Hispanic Black, and Hispanic respondents. The data are weighted to account for this oversampling, to reflect the survey’s complex sampling design, and to accurately reflect the U.S. population in terms of age, sex, race/ethnicity, and region of the country. A total of 34,653 adults aged 20 years and older completed the second wave interviews, with a response rate of 86.7%. The overall response rate from both waves was 70.2%.
Measures
Sociodemographic Variables
Our analyses included age, sex, marital status, household income and race/ethnicity. We classified age into seven categories (20–24, 25–34, 45–44, 45–54, 55–64, 65–74, 75+) for cross-tabulations and into three categories (20–34, 35–64, 65+) for logistic regression analyses. We classified marital status into three categories (married/common law, widowed/separated/divorced, and never married), household income into four categories ($0–$19,999; $20,000–$34,999; $35,000–$59,999; and $60,000+), and race/ethnicity into four categories (non-Hispanic White; Black; Hispanic; and Asian and Native American).
Mental Disorders
Trained U.S. Census Bureau Field Representatives conducted face-to-face computer-assisted personal interviews in respondents’ homes. The NESARC employs an interleafed survey format (21) where respondents who answered affirmatively to disorder screening questions throughout the survey then answered detailed questions about both psychiatric disorders and use of professional services for those disorders. Disorders were diagnosed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS-IV) (22) according to Diagnostic and Statistical Manual of Mental Disorders 4th edition criteria (23). Consistent with the DSM-IV, disorder diagnoses are primary and exclude those due to general medical conditions or substances. The AUDADIS-IV exhibits fair to good test-retest reliability (kappa = 0.40–0.77) for mood and anxiety disorders in community-dwelling populations (22, 24). We examined past-year diagnosis of specific mood and anxiety disorders because of methodological limitations associated with lifetime diagnoses (25) and to maintain consistency with past-year helpseeking variables. In addition to past year variables for each mood (major depression, dysthymia and mania) and anxiety (generalized anxiety disorder, panic disorder with and without agoraphobia, social phobia, specific phobia and post-traumatic stress disorder) disorder assessed in the NESARC we created composite “any mood” and “any anxiety” disorder variables. We also created “pure” individual and composite past-year mood and anxiety variables by removing individuals who had another mood or anxiety disorder in addition to the disorder of interest.
Helpseeking
We examined the prevalence of past-year disorder-specific helpseeking for mood and anxiety disorders. For each disorder module respondents screened into, they indicated if, with respect to each mental disorder, they: (1) saw “any kind of counselor, therapist, doctor, psychologist, or any person like that”, (2) “were a patient in a hospital for at least one night”, (3) went to “an emergency room for help”, or (4) had “a doctor prescribe any medicines or drugs”. Respondents who answered affirmatively to one or more of these questions within each disorder module then answered the following questions, which we used to identify past-year helpseeking: Major Depression – “During the last 12 months, did you go anywhere or see anyone to get help for feeling sad, blue, depressed or down/not caring about things or enjoying things?”; Dysthymia – “Did you go anywhere or see anyone to get help to improve your mood or to feel better in the last 12 months?”; Mania – “During the last 12 months, did you go anywhere or see anyone to get help for feeling extremely excited, elated or hyper/irritable or easily annoyed?”; Generalized Anxiety Disorder (GAD) – “During the last 12 months, did you go anywhere or see anyone to get help for feeling tense, nervous or worried?”; Panic Disorder – “During the last 12 months, did you go anywhere or see anyone to get help for your panic attacks?”; Social Phobia – “During the last 12 months, did you go anywhere or see anyone to get help for your fear or avoidance of social situations?”; Specific Phobia – “During the last 12 months, did you go anywhere or see anyone to get help for your fear or avoidance of any of these objects or situations?”; and Post Traumatic Stress Disorder (PTSD) – “Did you go anywhere or see anyone to get help for your reactions in the past 12 months?” We examined helpseeking for respondents with each mood and anxiety disorder, and we ran separate models for those with each “pure” disorder. We also created composite variables for past year helpseeking for any anxiety and any mood disorder including and excluding comorbid disorder diagnoses. Positive helpseeking status was limited to respondents with a past year diagnosis of the specific mood or anxiety disorder being examined.
Analytic strategy
We used the Taylor Series Linearization method (26) in SUDAAN 10.0.1 (27) for variance estimation to account for the complex sampling design of the NESARC. We applied statistical weights and stratification information from the NESARC in all analyses to ensure that data are representative of the U.S. adult population. Cross-tabulations provided prevalence estimates of helpseeking across the adult lifespan for each disorder, and for the “any mood” and “any anxiety” groups. Pearson Chi-squared analyses examined the influence of age on the likelihood of seeking help for the individual and composite diagnoses. Cross-tabulations also provided helpseeking prevalences across the adult lifespan for men versus women, and for those with “pure” disorders. In both of these cases we provide Chi-squared analyses only for the composite “any mood” and “any anxiety” variables due to small cell sizes across age for the individual disorders. Finally, we explored the relationship between age and helpseeking for specific mood and anxiety disorders, and the composite mood and anxiety variables, using logistic regression analyses. In these analyses we compared the likelihood of seeking help in younger (20–34) and middle-aged (35–64) adults to the older (65+) reference group with an unadjusted model as well a model adjusted for sex, marital status, household income, and race/ethnicity.
Results
The disorder-specific helpseeking prevalence data can be found in Table 1. Overall, 19.3% of individuals with an anxiety disorder sought help for their disorder, as did 36.8% of those with a mood disorder. There was also tremendous variability in rates of helpseeking for specific disorders, ranging from only 7.8% of those with specific phobias to 45.3% of those with panic disorder.
Table 1.
Prevalence of Seeking Disorder-Specific Treatment for Anxiety and Mood Disorders Across the Adult Lifespan
| Total n (%) |
20–24 n (%) |
25–34 n (%) |
35–44 n (%) |
45–54 n (%) |
55–64 n (%) |
65–74 n (%) |
75+ n (%) |
X2 | df | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety Disorders | |||||||||||
| Generalized Anxiety Disorder | 432 (31.6) | 15 (23.2) | 67 (26.1) | 137 (39.1) | 113 (34.4) | 71 (33.2) | 17 (18.9) | 12 (25.1) | 3.1 | 6 | 0.011 |
| Posttraumatic Stress Disorder | 366 (21.6) | 14 (16.2) | 61 (22.6) | 98 (23.4) | 112 (25.7) | 63 (22.8) | 13 (10.2) | 5 (8.6) | 4.1 | 6 | 0.002 |
| Panic Disorder | 422 (45.3) | 22 (38.5) | 90 (41.3) | 115 (46.7) | 116 (51.1) | 53 (46.9) | 16 (46.9) | 10 (29.0) | 1.0 | 6 | 0.418 |
| Social Phobia | 239 (26.9) | 14 (20.4) | 51 (28.9) | 63 (27.1) | 67 (33.4) | 34 (24.6) | 8 (20.4) | 2 (4.1) | 2.9 | 6 | 0.014 |
| Specific Phobia | 213 (7.8) | 11 (6.5) | 42 (7.5) | 55 (9.0) | 56 (8.9) | 40 (9.4) | 3 (2.1) | 6 (4.7) | 3.7 | 6 | 0.003 |
| Any Anxiety Disorder | 1145 (19.3) | 59 (16.2) | 219 (19.5) | 311 (22.4) | 309 (21.5) | 175 (19.3) | 42 (10.3) | 30 (11.0) | 7.4 | 6 | < 0.001 |
| Mood Disorders | |||||||||||
| Major Depression | 1158 (37.8) | 68 (29.5) | 228 (37.4) | 318 (44.1) | 295 (43.2) | 155 (31.9) | 57 (28.5) | 37 (28.8) | 4.9 | 6 | < 0.001 |
| Dysthymia | 225 (44.5) | 10 (36.6) | 31 (34.1) | 54 (51.9) | 71 (52.9) | 47 (51.0) | 8 (33.1) | 4 (12.7) | 2.3 | 6 | 0.046 |
| Mania | 202 (27.8) | 12 (21.7) | 45 (25.2) | 67 (33.0) | 49 (29.8) | 25 (34.6) | 2 (7.3) | 2 (4.1) | 3.0 | 6 | 0.011 |
| Any Mood Disorder | 1293 (36.8) | 76 (27.6) | 257 (36.3) | 352 (42.5) | 327 (41.8) | 180 (33.8) | 61 (27.0) | 40 (28.0) | 5.4 | 6 | < 0.001 |
Note: Reported Ns are for the sample, whereas percentages are weighted to be representative of the U.S. population
Our second objective was to examine mental health service use prevalence estimates across seven age cohorts. As shown in Table 1, each disorder except panic disorder showed a significant hill-shaped distribution with the highest prevalence of use among adults 35 to 54 years of age. The logistic regression analyses presented in Table 2 provide further support for this hill-shaped distribution. After adjusting for sex, age, marital status, household income and race/ethnicity, older adults were significantly less likely than younger adults to seek help for four of the eight disorders (OR range from 1.76 to 4.26) and significantly less likely than middle-aged adults to seek help for seven of eight disorders (OR range from 1.91 to 6.92).
Table 2.
Odds Ratios (with 95% CIs) of Seeking Disorder-Specific Treatment for Anxiety and Mood Disorders Among Younger and Middle-Aged Adults in Comparison to the Older (65+) Adult Reference Group
| Unadjusted Model |
Adjusted Model |
|||
|---|---|---|---|---|
| Young (20–34) Adults |
Middle-Aged (35–64) Adults |
Young (20–34) Adults |
Middle-Aged (35–64) Adults |
|
| Anxiety Disorders | ||||
| Generalized Anxiety Disorder | 1.24 (.70–2.17) | 2.03 (1.20–3.44)** | 1.46 (0.79–2.70) | 2.09 (1.20–3.64)* |
| Posttraumatic Stress Disorder | 2.46 (1.30–4.66)** | 3.03 (1.71–5.37)*** | 2.94 (1.51–5.73)** | 3.26 (1.84–5.81)*** |
| Panic Disorder | 1.06 (.54–2.10) | 1.47 (0.75–2.86) | 1.24 (0.61–2.55) | 1.66 (0.83–3.34) |
| Social Phobia | 2.15 (0.94–4.92) | 2.50 (1.14–5.49)* | 2.29 (0.97–5.41) | 2.73 (1.24–6.01)* |
| Specific Phobia | 2.38 (1.06–5.34)* | 3.07 (1.40–6.72)** | 3.61 (1.49–8.71)** | 3.97 (1.70–9.28)** |
| Any Anxiety Disorder | 1.91 (1.37–2.67)*** | 2.28 (1.66–3.14)*** | 2.74 (1.88–3.97)*** | 2.88 (2.05–4.05)*** |
| Mood Disorders | ||||
| Major Depression | 1.33 (0.98–1.82) | 1.73 (1.30–2.30)*** | 1.76 (1.25–2.48)** | 1.91 (1.41–2.57)*** |
| Dysthymia | 1.69 (0.72–3.95) | 3.43 (1.57–7.47)** | 1.95 (0.73–5.19) | 4.07 (1.82–9.12)** |
| Mania | 4.64 (1.20–17.95)* | 7.00 (1.90–25.71)** | 4.26 (1.08–16.73)* | 6.92 (1.88–25.45)** |
| Any Mood Disorder | 1.33 (0.99–1.78) | 1.78 (1.35–2.35)*** | 1.68 (1.21–2.33)** | 1.96 (1.47–2.62)*** |
Note: Adjusted model includes sex, age, marital status, household income and race.
p < .05,
p < .01,
p < .001
Table 3 presents the prevalence of treatment seeking by sex across the seven age groups. A significant age by sex by helpseeking Chi-squared analysis for the "any anxiety disorder" group is due to especially large sex differences (favoring women) for younger (20–44) and older (65+) adults. Sex differences did not vary by age for the "any mood disorder" group.
Table 3.
Prevalence of Disorder-Specific Professional Helpseeking Across the Adult Lifespan for Men and Women
| Total n (%) |
20–24 n (%) |
25–34 n (%) |
35–44 n (%) |
45–54 n (%) |
55–64 n (%) |
65–74 n (%) |
75+ n(%) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| Anxiety Disorders | ||||||||||||||||
| Generalized Anxiety Disorder | 107 (25.1) | 325 (74.9) | 3 (11.3) | 12 (88.7) | 13 (19.2) | 54 (80.8) | 29 (24.6) | 108 (75.4) | 32 (27.9) | 81 (72.1) | 23 (35.1) | 48 (64.9) | 4 (18.8) | 13 (81.2) | 3 (19.4) | 9 (80.6) |
| Posttraumatic Stress Disorder | 84 (26.2) | 282 (73.8) | 5 (31.8) | 9 (68.2) | 8 (13.9) | 53 (86.1) | 18 (22.7) | 80 (77.3) | 25 (24.7) | 87 (75.3) | 23 (47.3) | 40 (52.7) | 3 (8.6) | 10 (91.4) | 2 (46.1) | 3 (53.9) |
| Panic Disorder | 111 (31.7) | 311 (68.3) | 4 (16.8) | 18 (83.2) | 20 (26.2) | 70 (73.8) | 29 (33.0) | 86 (67.0) | 40 (39.0) | 76 (61.0) | 17 (43.0) | 36 (57.0) | 0 (0.0) | 16 (100) | 1 (18.5) | 9 (81.5) |
| Social Phobia | 71 (31.9) | 168 (68.1) | 3 (9.4) | 11 (90.6) | 15 (34.2) | 36 (65.8) | 18 (34.8) | 45 (65.2) | 21 (28.3) | 46 (71.7) | 11 (47.4) | 23 (52.6) | 3 (32.7) | 5 (67.3) | 0 (0.0) | 2 (100) |
| Specific Phobia | 55 (29.6) | 158 (70.4) | 3 (28.2) | 8 (71.8) | 9 (24.5) | 33 (75.5) | 11 (29.8) | 44 (70.2) | 17 (25.5) | 39 (74.5) | 13 (42.5) | 27 (57.5) | 1 (40.4) | 2 (59.6) | 1 (12.4) | 5 (87.6) |
| Any Anxiety Disorder | 287 (28.6) | 858 (71.4) | 13 (18.6) | 46 (81.4) | 47 (23.9) | 172 (76.1) | 66 (27.0) | 245 (73.0) | 88 (31.9) | 221 (68.1) | 58 (40.9) | 117 (59.1) | 9 (17.7) | 33 (82.3) | 6 (23.3) | 24 (76.7) |
| Mood Disorders | ||||||||||||||||
| Major Depression | 270 (25.6) | 888 (74.4) | 17 (21.0) | 51 (79.0) | 50 (25.2) | 178 (74.8) | 66 (23.5) | 252 (76.5) | 71 (27.2) | 224 (72.8) | 37 (26.8) | 118 (73.2) | 16 (25.4) | 41 (74.6) | 13 (38.9) | 24 (61.1) |
| Dysthymia | 51 (25.1) | 174 (74.9) | 3 (11.8) | 7 (88.2) | 5 (33.6) | 26 (66.4) | 11 (23.5) | 43 (76.5) | 17 (23.8) | 54 (76.2) | 11 (24.9) | 36 (75.1) | 2 (25.6) | 6 (74.4) | 2 (57.6) | 2 (42.4) |
| Mania | 57 (33.5) | 145 (66.5) | 4 (37.1) | 8 (62.9) | 16 (35.9) | 29 (64.1) | 17 (32.1) | 50 (67.9) | 12 (23.9) | 37 (76.1) | 8 (47.3) | 17 (52.7) | 0 (0.0) | 3 (100) | 0 (0.0) | 2 (100) |
| Any Mood Disorder | 305 (26.5) | 988 (73.5) | 21 (25.8) | 55 (74.2) | 58 (26.3) | 199 (73.7) | 73 (24.1) | 279 (75.9) | 79 (27.4) | 248 (72.6) | 43 (27.5) | 137 (72.5) | 16 (23.5) | 45 (76.5) | 15 (40.9) | 25 (59.1) |
Note: Reported Ns are for the sample, whereas percentages are weighted to be representative of the U.S. population
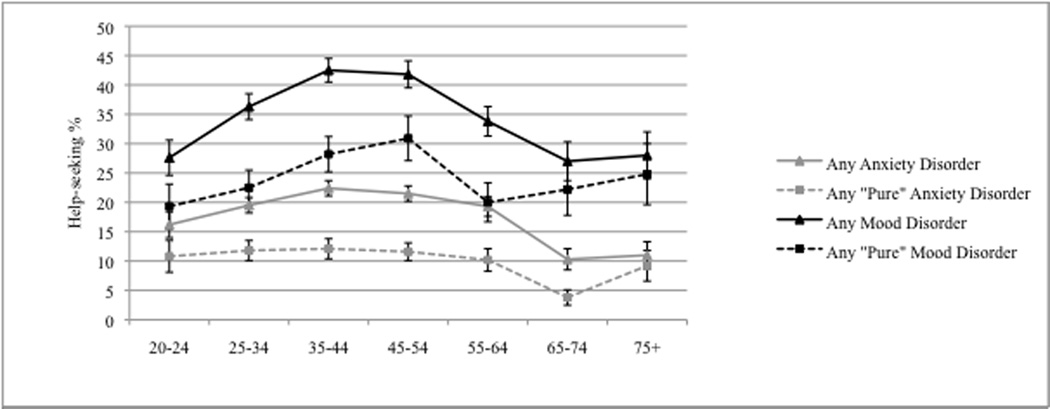
Finally, Table 4 provides data to examine our fourth objective of exploring disorder-specific helpseeking among individuals who do not have another comorbid anxiety or mood disorder. The pattern of findings for the any anxiety and any mood groups are shown in Figure 1clearly indicating: (a) a much lower likelihood of seeking help among the “pure” disorder groups, as well as (b) an attenuation or flattening of the hill-shaped age distribution. Age differences are no longer significant for the any “pure” mood disorder group, due in part to the larger band of error at each age point in comparison to the any “pure” anxiety disorder group.
Table 4.
Prevalence of Disorder-Specific Helpseeking for "Pure" Anxiety and Mood Disorders Across the Adult Lifespan
| Total n (%) |
20–24 n (%) |
25–34 n (%) |
35–44 n (%) |
45–54 n (%) |
55–64 n (%) |
65–74 n (%) |
75+ n (%) |
X2 | df | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety Disorders | |||||||||||
| GAD | 46 (20.6) | 1 (18.6) | 8 (18.2) | 15 (26.5) | 7 (20.3) | 8 (17.6) | 2 (9.3) | 5 (26.7) | -- | -- | -- |
| PTSD | 94 (15.1) | 5 (18.0) | 19 (19.7) | 15 (11.0) | 34 (20.7) | 16 (16.0) | 2 (0.9) | 3 (7.0) | -- | -- | -- |
| Panic Disorder | 76 (42.5) | 6 (58.6) | 19 (33.9) | 21 (51.2) | 15 (42.1) | 9 (50.8) | 3 (21.8) | 3 (17.3) | -- | -- | -- |
| Social Phobia | 19 (9.2) | 1 (8.1) | 5 (15.7) | 5 (6.8) | 4 (10.3) | 1 (0.4) | 2 (16.2) | 1 (9.6) | -- | -- | -- |
| Specific Phobia | 40 (2.6) | 3 (2.9) | 8 (2.9) | 11 (2.7) | 9 (1.9) | 6 (3.5) | 0 (0.0) | 3 (3.7) | -- | -- | -- |
| Any Anxiety Disorder | 275 (10.7) | 16 (10.8) | 59 (11.8) | 67 (12.1) | 69 (11.6) | 40 (10.2) | 9 (3.8) | 15 (9.2) | 3.83 | 6 | 0.003 |
| Mood Disorders | |||||||||||
| Major Depression | 311 (26.1) | 23 (20.3) | 58 (24.8) | 80 (30.7) | 71 (32.5) | 34 (18.0) | 25 (22.4) | 20 (25.7) | -- | -- | -- |
| Dysthymia | 24 (30.0) | 2 (100.0) | 2 (6.1) | 4 (17.5) | 9 (41.3) | 5 (36.5) | 2 (46.7) | 0 (0.0) | -- | -- | -- |
| Mania | 20 (14.9) | 1 (10.2) | 6 (14.1) | 7 (18.6) | 3 (11.0) | 3 (36.2) | 0 (0.0) | 0 (0.0) | -- | -- | -- |
| Any Mood Disorder | 355 (24.9) | 26 (19.3) | 66 (22.5) | 91 (28.2) | 83 (30.9) | 42 (20.0) | 27 (22.2) | 20 (24.8) | 1.40 | 6 | 0.230 |
Note: Reported Ns are for the sample, whereas percentages are weighted to be representative of the U.S. population. We report X2 analyses for the summary anxiety and mood disorder categories only because of small cell sizes for the individual disorders. The term “pure” refers to no comorbid anxiety or mood disorder.
Figure 1.
Prevalence of disorder-specific professional helpseeking across the adult lifespan for those with any anxiety and any mood disorder (including comorbidity) and for those with any “pure” anxiety and any “pure” mood disorders (excluding comorbidity).
Discussion
With respect our first objective, exploring the prevalence of disorder-specific mental health service use, there is a dearth of directly comparable prior research. Our finding that 45% of respondents with panic disorder sought help for panic is very similar to Kessler and colleagues’ (14) finding of 12-month panic-specific treatment among 44% and 53% of National Comorbidity Survey (NCS) respondents with panic disorder without and panic disorder with agoraphobia, respectively. In contrast, our finding that 27% of respondents with social phobia sought treatment is higher than the 17% of respondents who sought social phobia-specific treatment in the NCS replication (NCS-R) (15). This difference may be due to either variability in the NCS-R and NESARC samples (e.g., the NESARC has a much larger sample size and oversampled younger adults and ethnic minorities), or to methodological differences in the way that disorders and/or helpseeking were assessed both between and within the two surveys. With respect to disorder diagnoses, the NESARC uses the AUDADIS whereas the NCS-R uses the World Health Organization Composite International Diagnostic Interview. With respect to helpseeking, as outlined in the methods section, the NESARC uses four specific questions and a summary question to assess service use for each mood and anxiety disorder. The NCS-R provides a much richer source of questions pertaining to service use, including several questions at the end of each disorder module as well as an entire module devoted to comprehensive assessment of general help with emotions, nerves, mental health, or use of alcohol or drugs.
Importantly, the studies by Kessler (14) and Ruscio (15) examined both disorder-specific treatment prevalence and any 12-month treatment seeking and found much higher rates of general treatment seeking. While it is true that disorder-specific treatment prevalence estimates may underestimate actual helpseeking because mental disorders are often comorbid and most treatments for them target a broad range of anxiety and mood symptoms, findings from these studies highlight the importance of understanding both general helpseeking for mental health problems, as well as mental health service use tied directly to specific disorders.
The disorder-specific treatment seeking prevalence findings in this study replicate two important findings from prior research focusing on general helpseeking. First, consistent with past research (4, 7, 8, 10, 28) NESARC respondents were much more likely to seek help for mood than anxiety disorders – nearly twice as likely when comparing the overall rate of 19% for any anxiety disorder to 37% for any mood disorder. Second, the rank order of disorder-specific mental health use in this study is exactly the same as the rank order of general treatment seeking among individuals with disorders from Part II of the NCS (7). Specifically, panic disorder was the most likely anxiety disorder to result in treatment seeking in both studies, followed by generalized anxiety disorder, social phobia, and finally specific phobia. For the mood disorders, dysthymia was most likely to result in helpseeking in both surveys, followed by major depression and mania/bipolar disorder.
It is noteworthy that panic disorder and dysthymia are the psychiatric diagnoses that were most likely to lead individuals to seek professional help in both this study and the NCS. The relatively high likelihood of helpseeking for panic disorder makes sense when considering that its course is typically chronic and relapsing (29) and its severe symptom profile is especially likely to bring sufferers in contact with the healthcare system, even if there are often significant delays in accurately diagnosing the problem as psychological (30, 31). What is particularly interesting is that panic disorder is the only diagnosis that did not result in different rates of helpseeking across the adult lifespan, and its influence on helpseeking was largely unaffected by psychiatric comorbidity. Individuals with this disorder may be relatively likely to seek mental health services, regardless of age or psychiatric comorbidity, as a result of openness to both attributing a psychological cause to panic symptoms and to seeking mental health treatment (32). In contrast to the intuitive nature of helpseeking for panic, a similarly high likelihood of seeking professional help for dysthymia is somewhat less intuitive considering that it is, by definition, less severe than major depression. One potential explanation, that many individuals with this disorder seek help because of comorbid anxiety or mood problems (33), is not supported by our data. Dysthymia remained the second most likely disorder to result in service use when limiting our sample to those without comorbid diagnoses. The most probable explanation for prevalent helpseeking among those with dysthymia is that chronic depression is more likely than acute depression to impair quality of life (34) and result in suicide attempts and hospitalizations (35). Our data suggest a need to explore these possibilities and to address the current dearth of research focusing on dysthymia and helpseeking.
In contrast to the high prevalence of mental health service use for panic disorder and dysthymia, treatment seeking was least likely for specific phobia. This finding deserves special attention considering that although it may be less disabling than other disorders, exposure-based treatments for it are exceptionally effective (36). The fact that only 8% of individuals with specific phobias sought help suggests the need for public education about these phobias and the availability of relatively quick and highly effective psychological treatments for it.
With respect to our second objective concerning the relationship between age cohorts and service use specifically tied to disorders, this study replicated the hill-shaped distribution of helpseeking across the adult lifespan reported in previous research (7). Novel findings from this study include the lack of age effects on helpseeking specifically for panic disorder, some evidence of leveling off of treatment seeking rates after age 65, and less dramatic age effects when examining mental health service use for “pure” disorders. In fact, the hill-shaped distribution for pure mood disorders was not significant in this study. Finally, we found that after adjusting for sociodemographic variables, older adults were nearly two times less likely than middle-aged adults to seek help for any mood disorder and nearly three times less likely than middle-aged adults to seek help for any anxiety disorder. The especially low prevalence of mental health service by older adults therefore remains a significant and growing public health concern as older individuals continue to make up an increasingly large portion of the population in the coming decades (37).
Our third objective was to explore sex differences in service use across the lifespan, with particular attention to sex differences in helpseeking among older adults. Consistent with previous studies (8, 10) older women in this study were more likely than older men to seek help. Women’s greater likelihood of treatment seeking remained similar across the adult lifespan for mood disorders but not for anxiety disorders, where they were more likely than men to seek help if they were younger (20–44) or older (65+).
Finally, this study explored associations between helpseeking and comorbid mood and anxiety disorders. As expected, individuals who did not have comorbid mood or anxiety disorders were less likely to seek help overall, likely because their symptom presentations were less complex and severe than those with comorbid psychiatric problems. After removing the effect of comorbidity, helpseeking for the any mood category dropped from 37% to 25%, and helpseeking for the any anxiety category dropped from 19% to 11%. Perhaps most striking was the drop in treatment seeking for those with phobias. More than one quarter of individuals with social phobia sought professional help, whereas only 9% of individuals with social phobia and no other mood or anxiety disorder sought help. Similarly, rates of treatment seeking among those with specific phobias dropped from 8% to 3%. This finding further suggests the need for mental health literacy surrounding these highly treatable conditions.
The results of this study should be considered in light of a number of limitations. First, the prevalence data presented in this study does not include people with subthreshold disorders; it only represents individuals with diagnosed disorders who sought help for those disorders. Second, although the NESARC is a nationally representative sample, it does not include institutionalized individuals and therefore does not generalize to those populations. Third, the NESARC does not provide information about what kinds of services people received (e.g., pharmacotherapy versus psychotherapy) or whether the services received are evidence based or meet minimum standards for adequacy (38). Fourth, in our analyses exploring the role of psychiatric comorbidity we focused on mood and anxiety disorders. It is quite possible that individuals in our “pure” disorder analyses may have had other psychiatric comorbidities, including substance problems, psychosis, and personality disorders. Fifth, in addition to the reasons outlined earlier for why estimates of disorder-specific treatment may underestimate the true prevalence of helpseeking, survey conditioning also likely resulted in underestimates of treatment seeking. Specifically, Duan and colleagues (21) have demonstrated that when mental health service use screening questions are placed at the beginning of long surveys, as opposed to being “interleafed” throughout along with follow-up branch questions (as they are in the NESARC), substantially greater and arguably more accurate service rates are reported. Finally, given that the prevalence of both psychiatric disorders and helpseeking for those disorders decreases with age, small cell sizes for estimates of helpseeking for specific disorders later in life prevented us from analyzing age and sex effects for some of our specific disorder variables.
Despite these limitations, this is the first study to examine and present in a single, unified paper the prevalence of disorder-specific mental health services for mood and anxiety disorders, and associations between helpseeking and age, sex, and psychiatric comorbidity using a large nationally representative sample. Other research using the NESARC has explored mood and anxiety disorder-specific mental health treatment as a secondary aim of research focusing on chronic and nonchronic major depressive disorder (34), PTSD (39), panic disorder and agoraphobia (40), bipolar disorder with or without alcohol use (41), GAD (42, 43), hypomania (44), and co-occurring substance use disorders (45). Our study clearly highlights disorders that are more likely to result in professional treatment (panic disorder and dysthymia) as well as those that especially unlikely to result in helpseeking (specific phobias). It also emphasizes that men, older adults, and individuals with a single mood or anxiety disorder are especially unlikely to seek mental health services. Identifying groups of individuals who need treatment but are unlikely to receive it is an effective method of targeting prevention and treatment efforts to reduce the burden of mental disorders.
Acknowledgments
This study was supported by a Manitoba Health Research Council Establishment Grant to Corey Mackenzie, a Canadian Institutes for Health Research Master’s Award to Kristin Reynolds, and a Canadian Institutes of Health Research New Investigator Award (#152348) and a Manitoba Health Research Council Research Chair to Jitender Sareen. The NESARC was conducted and funded by the National Institute on Alcohol Abuse and Alcoholism, with supplemental support from the National Institute on Drug Abuse. We thank the NIAAA and the US Census Bureau field representatives who administrated the NESARC interviews and made it available for researchers.
References
- 1.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olfson M, Marcus SC, Druss B, Elinson L, Tanielian T, Pincus HA. National trends in the outpatient treatment of depression. JAMA. 2002;287:203–209. doi: 10.1001/jama.287.2.203. [DOI] [PubMed] [Google Scholar]
- 3.Wang PS, Demler O, Olfson M, Pincus HA, Wells KB, Kessler RC. Changing Profiles of Service Sectors Used for Mental Health Care in the United States. Am J Psychiatry. 2006;163(7):1187–1198. doi: 10.1176/appi.ajp.163.7.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alonso J, Angermeyer MC, Bernert S, et al. Use of mental health services in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand. 2004;420:47–54. doi: 10.1111/j.1600-0047.2004.00330.x. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Ustun TB. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. Cambridge, UK: Cambridge University Press; 2008. [Google Scholar]
- 6.Sareen J, Cox BJ, Afifi TO, Yu BN, Stein MB. Mental health service use in a nationally representative Canadian survey. Can J Psychiatry. 2005;50(12):753–761. doi: 10.1177/070674370505001204. [DOI] [PubMed] [Google Scholar]
- 7.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 8.Klap R, Unroe KT, Unutzer J. Caring for mental illness in the United States: A focus on older adults. Am J Geriatr Psychiatry. 2003;11:517–524. [PubMed] [Google Scholar]
- 9.Andrews G, Henderson S, Hall W. Prevalence, comorbidity, disability and service utilisation: Overview of the Australian National Mental Health Survey. Br J Psychiatry. 2001;178:145–153. doi: 10.1192/bjp.178.2.145. [DOI] [PubMed] [Google Scholar]
- 10.Mackenzie CS, Pagura J, Sareen J. Correlates of help-seeking and perceived need for mental health services among older adults in the Collaborative Psychiatric Epidemiology Surveys. Am J Geriatr Psychiatry. 2010;18:1103–1115. doi: 10.1097/JGP.0b013e3181dd1c06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cairney J, Corna LM, Streiner DL. Mental Health Care Use in Later Life: Results From a National Survey of Canadians. Can J Psychiatry. 2010;55(3):157–164. doi: 10.1177/070674371005500307. [DOI] [PubMed] [Google Scholar]
- 12.Cole MG, McCusker J, Sewitch M, Ciampi A, Dyachenko A. Health services use for mental health problems by community-living seniors with depression. Int Psychogeriatr. 2007;20(3):554–570. doi: 10.1017/S1041610207005935. [DOI] [PubMed] [Google Scholar]
- 13.Mosier KE, Vasiliadis HM, Lepnurm M, Puchala C, Pekrul C, Tempier R. Prevalence of mental disorders and service utilization in seniors: results from the Canadian community health survey cycle 1.2. Int J Geriatr Psychiatry. 2010;25(10):960–967. doi: 10.1002/gps.2434. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The Epidemiology of Panic Attacks, Panic Disorder, and Agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63(4):415–424. doi: 10.1001/archpsyc.63.4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: results from the National Comorbidity Survey Replication. Psychol Med. 2008;38(01):15–28. doi: 10.1017/S0033291707001699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaufman J, Charney D. Comorbidity of mood and anxiety disorders. Depress Anxiety. 2000;12 Suppl 1:69–76. doi: 10.1002/1520-6394(2000)12:1+<69::AID-DA9>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 17.Scott T, Mackenzie CS, Chipperfield J, Sareen J. Mental health service use among Canadian older adults with anxiety disorders and high levels of anxiety symptoms. Aging Ment Health. 2010;14(7):790–800. doi: 10.1080/13607861003713273. [DOI] [PubMed] [Google Scholar]
- 18.Grant BF, Kaplan KK, Stinson FS. Source and accuracy statement: The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. In: http://www.niaaa.hin.gov NIAAA. 2007
- 19.Grant BF, Moore TC, Shepard J, Kaplan K. Source and accuracy statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). In: http://www.niaaa.nih.gov NIAAA. 2007
- 20.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 21.Duan N, Alegria M, Canino G, McGuire TG, Takeuchi D. Survey conditioning in self-reported mental health service use: Randomized comparison of alternative instrument formats. Health Research and Educational Trust. 2007;42(2):890–907. doi: 10.1111/j.1475-6773.2006.00618.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 23.Association AP, et al. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 24.Ruan WJ, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92(1–3):27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Streiner DL, Patten SB, Anthony JC, Cairney J. Has ‘lifetime prevalence’ reached the end of its life? An examination of the concept. International J Methods Psychiatric Res. 2009;18(4):221–228. doi: 10.1002/mpr.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy PS, Lemeshow S. Sampling of populations. New York: John Wiley & Sons; 1999. [Google Scholar]
- 27.Shah BV, Barnswell BG, Bieler GS. SUDAAN User's Manual: Release 10.0. Research Triangle Park, NC: Research Triangle Institute; 2009. [Google Scholar]
- 28.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Arch Gen Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 29.Francis JL, Weisberg RB, Dyck IR, et al. Characteristics and Course of Panic Disorder and Panic Disorder With Agoraphobia in Primary Care Patients. Prim Care Companion J Clin Psychiatry. 2007;9(3):173–179. doi: 10.4088/pcc.v09n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roy-Byrne PP, Stein MB, Russo J, et al. Panic disorder in the primary care setting: comorbidity, disability, service utilization, and treatment. J Clin Psychiatry. 1999;60(7):492–499. doi: 10.4088/jcp.v60n0713. quiz 500. [DOI] [PubMed] [Google Scholar]
- 31.Teng EJ, Chaison AD, Bailey SD, Hamilton JD, Dunn NJ. When anxiety symptoms masquerade as medical symptoms: what medical specialists know about panic disorder and available psychological treatments. J Clin Psychol Med Settings. 2008;15(4):314–321. doi: 10.1007/s10880-008-9129-4. [DOI] [PubMed] [Google Scholar]
- 32.Johnson MR, Gold PB, Siemion L, Magruder KM, Frueh BC, Santos AB. Panic disorder in primary care: patients' attributions of illness causes and willingness to accept psychiatric treatment. Int J Psychiatry Med. 2000;30(4):367–384. doi: 10.2190/TXNB-V7VU-7H32-C7YT. [DOI] [PubMed] [Google Scholar]
- 33.Goldney RD, Fisher LJ. Double depression in an Australian population. Soc Psychiatry Psychiatr Epidemiol. 2004;39(11):921–926. doi: 10.1007/s00127-004-0832-7. [DOI] [PubMed] [Google Scholar]
- 34.Rubio JM, Markowitz JC, Alegria A, et al. Epidemiology of chronic and nonchronic major depressive disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Depress Anxiety. 2011;28:622–631. doi: 10.1002/da.20864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cuijpers P, van Straten A, Schuurmans J, van Oppen P, Hollon SD, Andersson G. Psychotherapy for chronic major depression and dysthymia: A meta-analysis. Clin Psychol Rev. 2010;30(1):51–62. doi: 10.1016/j.cpr.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Hamm AO. Specific Phobias. Psychiatr Clin North Am. 2009;32(3):577–591. doi: 10.1016/j.psc.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 37.Bartels SJ. Improving the system of care for older adults with mental illness in the United States: Findings and recommendations from the President's New Freedom Commission on Mental Health. Am J Geriatr Psychiatry. 2003;11(5):486–497. [PubMed] [Google Scholar]
- 38.Wang PS, Aguilar-Gaxiola S, Alonso J, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to trauatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grant BF, Hasin DS, Stinson FS, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(3):363–374. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- 41.Oquendo MA, Currier D, Liu SM, Hasin DS, Grant BF, Blanco C. Increased risk for suicidal behavior in comorbid bipolar disorder and alcohol use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J Clin Psychiatry. 2010;71(7):902–909. doi: 10.4088/JCP.09m05198gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mackenzie CS, Reynolds K, Chou K, Pagura J, Sareen J. Correlates of generalized anxiety disorder in a national sample of older adults. Am J Geriatr Psychiatry. 2011;19(4):305–315. doi: 10.1097/JGP.0b013e318202bc62. [DOI] [PubMed] [Google Scholar]
- 43.Vesga-Lopez O, Schneier FR, Wang S, et al. Gender differences in generalized anxiety disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J Clin Psychiatry. 2008;69(10):1606–1616. [PMC free article] [PubMed] [Google Scholar]
- 44.Agosti V, Stewart JW. Hypomania with and without dysphoria: Comparison of comorbidity and clinical characteristics of respondents from a national community sample. J Affect Disord. 2008;108:177–182. doi: 10.1016/j.jad.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Hatzenbuehler ML, Keyes KM, Narrow WE, Grant BF, Hasin DS. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69:1112–1121. doi: 10.4088/jcp.v69n0711. [DOI] [PMC free article] [PubMed] [Google Scholar]