Abstract
Background
Lipid accumulation product (LAP) is a novel biomarker of central lipid accumulation related to risk of diabetes and cardiovascular disease. In this study, we assessed the association of LAP with glucose homeostasis, lipid and lipid peroxidation, and subclinical systemic inflammation in diabetic patients.
Methods
Thirty-nine male and 47 female type 2 diabetic patients were assessed for anthropometrics and biochemical measurements. LAP was calculated as [waist circumference (cm)-65]×[triglycerides (mmol/L)] in men, and [waist circumference (cm)-58]×[triglycerides (mmol/L)] in women. Associations of LAP with fasting glucose, insulin, insulin resistance index, lipid and lipoprotein levels, malondialdehyde, and high-sensitive C-reactive protein (hs-CRP) were assessed.
Results
Mean age and LAP index were 53.6±9.6 and 51.9±31.2 years, respectively. After adjustments for age, sex and body mass index status, a significant positive correlation was observed between LAP index and fasting glucose (r=0.39, P<0.001), and homeostasis model assessment of insulin resistance (r=0.31, P<0.05). After additional adjustment for fasting glucose levels, antidiabetic and antilipidemic drugs, the LAP index was also correlated to total cholesterol (r=0.45, P<0.001), high density lipoprotein cholesterol (HDL-C) levels (r=-0.29, P<0.05), triglycerides to HDL-C ratio (r=0.89, P<0.001), malondialdehyde (r=0.65, P<0.001), and hs-CRP levels (r=0.27, P<0.05).
Conclusion
Higher central lipid accumulation in diabetic patients was related to higher insulin resistance, oxidative stress and systemic inflammation.
Keywords: Diabetes mellitus, type 2; Lipid accumulation product; Subclinical inflammation; Oxidative stress
INTRODUCTION
Lipid accumulation product (LAP) index, a newly developed biomarker of central lipid accumulation, has been proposed as an accurate and independent indicator of the risk of insulin resistance, metabolic syndrome, type 2 diabetes and cardiovascular disease [1,2,3]. LAP, which is estimated based on the combination of waist circumference (WC) and triglyceride levels, and is compared to anthropometric measures, including body mass index (BMI), WC, and waist to hip ratio, has recently been considered a better predictor of all-cause and cardiovascular mortality as well as diabetes development in different ages and ethnic populations [4,5,6]. Since LAP was developed taking into account both triglyceride levels and WC, it is suggested that this index has a stronger correlation with visceral adiposity, higher levels of lypolysis and adipocytokines including interleukin-6, and plasminogen activator inhibitor-1 [7]. Recent studies report that higher LAP is related to abnormal glucose homeostasis and insulin resistance, as well as elevated alanine aminotransferase, an indicator of the hepatic feature of metabolic syndrome, in apparently healthy individuals [8,9]. Higher LAP was also found to be related to lower levels of sex-hormone-binding globulin and higher free androgen index as potential mediators of cardiovascular disease [10].
Despite data available regarding the association of LAP and cardiometabolic risk factors in healthy populations, little is known concerning LAP and the metabolic status of diabetic patients. Our primary focus in this study was to assess whether LAP index could be related to glucose homeostasis parameters, lipid and lipoprotein levels, lipid peroxidation, and subclinical systemic inflammation in type 2 diabetic patients.
METHODS
Study population
This study was conducted from April 2012 to January 2013. Men and women, aged 25 to 60 years, with a clinical diagnosis of type 2 diabetes for at least 1 year, were recruited from the Iran Diabetes Society and the endocrine clinic of Taleghani Medical Center. Patients were excluded from the study if they had severe impairment of cardiac, hepatic or renal function, gestation or lactation and if they used insulin injection or consumed dietary supplements. Finally, 86 of the initially eligible patients, were included in the study. Written informed consent was obtained from all participants. Ethics approval for the trial was obtained from the Ethical Committee of the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences.
Demographics, anthropometrics, and clinical measurement
Trained interviewers collected information using the pretested questionnaires. Information on age, educational levels, medical history and medications, duration of diabetes and oral antidiabetic drugs, was collected. Anthropometric measurements were assessed by trained staff. Weight was measured to the nearest 100 g using digital scales, while the subjects were minimally clothed, without shoes. Height was measured to the nearest 0.5 cm, in a standing position without shoes, using a tape measure. BMI was calculated as weight (kg), divided by the square of the height (m2). WC was measured to the nearest 0.1 cm, midway between the lower border of the ribs and the iliac crest at the widest portion, over light clothing, using a soft measuring tape, without any pressure to the body.
Biochemical measurement
For all biochemical measurements, 12-hour fasting blood samples were collected into tubes containing 0.1% Ethylenediaminetetraacetic acid disodium salt dihydrate and were centrifuged at 4℃ and 500 g for 10 minutes to separate plasma. Fasting serum glucose was measured by the enzymatic colorimetric method using a glucose oxidation kit (Pars Azmun Co., Tehran, Iran). Serum insulin concentrations were measured using an enzyme-linked immunosorbent assay (ELISAs) kit (Mercodia, Uppsala, Sweden). Insulin resistance was estimated using the homeostasis model assessment of insulin resistance (HOMA-IR) index, which is defined as fasting plasma insulin (mU/L) multiplied by the fasting plasma glucose (mmol/L) divided by 22.5.
Serum total cholesterol and triglyceride levels were measured by enzymatic colorimetric analysis with cholesterol esterase/cholesterol oxidase and glycerol phosphate oxidase, respectively (Pars Azmun Co.). High density lipoprotein cholesterol (HDL-C) was measured by the immunoturbidimetry method after precipitation of apo B-containing lipoproteins with phosphotungstic acid (Pars Azmun Co.). Low density lipoprotein-cholesterol was calculated from serum total cholesterol, triglycerides and HDL-C, according to the Friedewald equation.
Serum high-sensitive C-reactive protein (hs-CRP; pg/mL) concentration was measured using the ELISA kit (Diagnostics Biochem Canada Inc., Thames Centre, Ontario, Canada). Serum malondialdehyde (MDA) was measured spectrophotometrically by the thiobarbituric acid reactive substances (TBARs) assay kit (Cayman Chemical Inc., Ann Arbor, MI, USA). Inter- and intra-assay coefficients of variations of all assays were <5%.
LPA index, a novel measure of central lipid accumulation and predictor of metabolic syndrome and cardiovascular disease, was calculated as [WC (cm)-65]×[triglycerides (mmol/L)] in men, and [WC (cm)-58]×[triglycerides (mmol/L)] in women [11,12].
Statistical methods
The Kolmogorov-Smirnov test was used to test for normal distributions. If the variable was not normally distributed, logarithm of the skewed variable was entered in the models. The LAP index was categorized into quartiles (<24.5, 24.5 to 43.9, 44 to 65.5, and >65.5) metabolic parameters of the patients were compared across the quartile categories using the general linear models with adjustments for age and gender. A partial correlation test with adjustments for age, sex, antidiabetic and antilipidemic drugs, BMI status (≤24.9, 25 to 29.9, ≥30) and fasting glucose levels was used to clarify the association of LAP index and BMI with glucose homeostasis parameters, lipid and lipoprotein levels, MDA, and hs-CRP. To better estimate the association of LAP and the mentioned parameters, linear regression curve estimation analysis was also conducted and significant associations were presented as plots. Statistical analysis was performed with SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). A P<0.05 was considered significant.
RESULTS
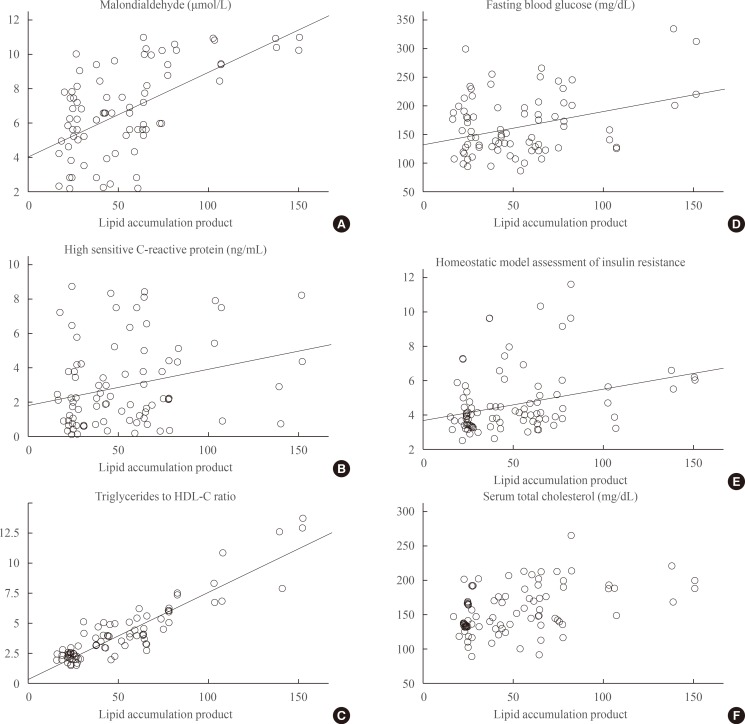
The mean age of participants was 53.6±9.6 years, and 45% were men. The mean of LAP index was 22±3.8, 35±3.7, 56±4.1, and 93±3.7 in the 1st, 2nd, 3rd, and 4th quartile categories of LAP, respectively. Table 1 presents the characteristics, biochemical and anthropometric values of the participants across quartile categories of LAP index. Participants in the highest quartile of LAP also had higher BMI. A significant increasing trend of serum fasting glucose, insulin, insulin resistance index, and total cholesterol levels was observed across increasing LAP. Mean levels of HDL-C significantly decreased across increasing LAP quartiles. Compared to the lowest quartile category of LAP index, participants in the highest had higher triglyceride/HDL-C ratios, MDA and hs-CRP levels. Partial correlation coefficients of LAP index and BMI with metabolic parameters are presented in Table 2. After adjustments for age, sex and BMI status, significant positive correlations were observed between LAP index and fasting glucose (r=0.39, P<0.001), and LAP index and HOMA-IR (r=0.31, P<0.05). After additional adjustment for fasting glucose levels, antidiabetic and antilipidemic drugs, it was found that total cholesterol (r=0.45, P<0.001), HDL-C levels (r=-0.29, P<0.05), triglyceride/HDL-C ratio (r=0.89, P<0.001), MDA (r=0.65, P<0.001), and hs-CRP levels (r=0.27, P<0.05) were also correlated to the LAP index. There were significant correlations between BMI and serum insulin (r=0.44, P<0.01), HOMA-IR (r=0.29, P<0.05), triglyceride/HDL-C ratio (r=0.28, P<0.05), and hs-CRP levels (r=0.40, P<0.01). Curve estimation plots are presented in Fig. 1. Significant linear associations between LAP index with fasting glucose, HOMA-IR, and total cholesterol levels were observed. Triglyceride/HDL-C ratio (β=0.91, P<0.001), MDA (β=0.58, P<0.001), and hs-CRP levels (β=0.27, P<0.05) also had linear associations with the LAP index.
Table 1.
Demographics, Anthropometric Measurements, and Cardiometabolic Risk Factors of the Patients by Categories of LAP Index
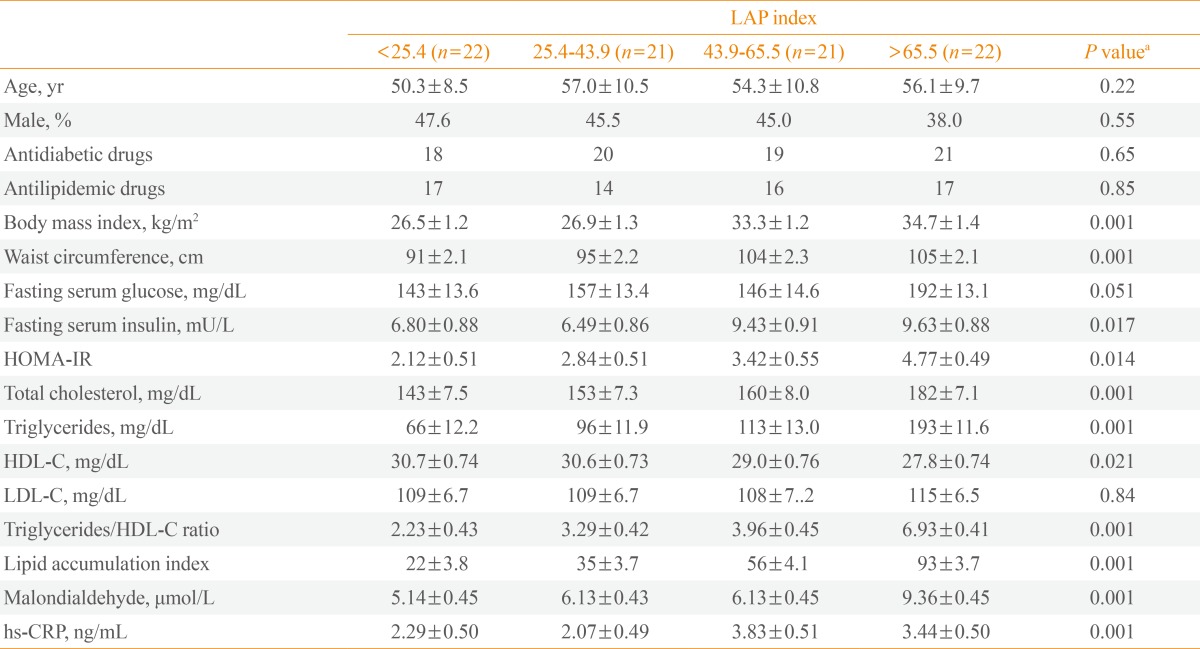
Values are expressed as mean±SEM.
LAP, lipid accumulation product; HOMA-IR, homeostatic model assessment of insulin resistance; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; hs-CRP, high-sensitive C-reactive protein.
aP values compared the mean values across quartile categories of LAP using age- and sex-adjusted analysis of covariance.
Table 2.
The Correlation of LAP Index and BMI with Glucose Homeostasis Parameters, Lipid and lipoprotein Levels, Lipid Peroxidation and Systemic Inflammation
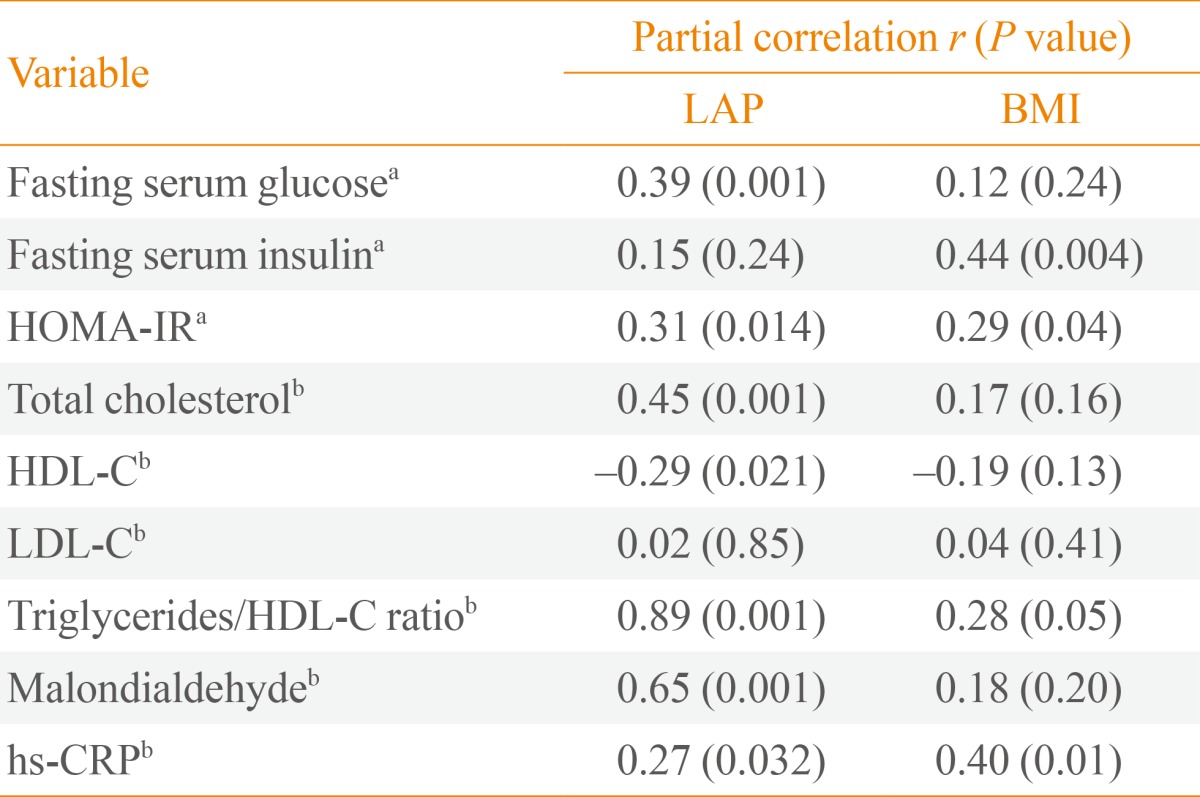
LAP, lipid accumulation product; BMI, body mass index; HOMA-IR, homeostatic model assessment of insulin resistance; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; hs-CRP, high-sensitive C-reactive protein.
aAdjusted for age, sex, and BMI status (for LAP only); bAdditionally adjusted for fasting glucose levels, antidiabetic and antilipidemic drugs.
Fig. 1.
Linear association of lipid accumulation product (LAP) and metabolic parameters in type 2 diabetic patients (regression curve estimation models were used). (A) Linear association of LAP and malondialdehyde (β=0.58, P<0.01). (B) Linear association of LAP with C-reactive protein (β=0.27, P<0.05). (C) Linear association of LAP with the triglycerides to high density lipoprotein cholesterol (HDL-C) ratio (β=0.91, P<0.01). (D) Linear association of LAP with fasting serum glucose (β=0.39, P<0.05). (E) Linear association of LAP with homeostasis model assessment of insulin resistance (β=0.31, P<0.05). (F) Linear association of LAP with serum total cholesterol (β=0.42, P<0.01).
DISCUSSION
In the current cross-sectional study, a higher LAP index was related to higher fasting glucose and insulin resistance in type 2 diabetic patients. Central lipid accumulation was also correlated with total cholesterol, HDL-C and triglyceride/HDL-C ratio, independent of fasting serum glucose. Moreover, a strong correlation between LAP, MDA and hs-CRP levels was observed.
LAP has previously been reported as a predictor of diabetes, metabolic syndrome, and cardiovascular disease [2,3,4,5,6]. The odds ratio of diabetes in subjects with high LAP was 7.40 (95% confidence interval [CI], 5.10 to 10.75) and 19.09 (95% CI, 6.57 to 55.50) in Japanese men and women, respectively [1]. Some previous studies indicated that, compared to other anthropometric measures such as WC and BMI, LAP could be considered a better predictor of diabetes development and cardiovascular disease risk [4,5,6]. A recent cross-sectional study on 2,524 nondiabetic Chinese subjects showed that, compared to BMI and WC, LAP had a greater impact on the insulin resistance index [13]. In an analysis conducted in the third National Health and Nutrition Examination Survey, LAP had better correlation with cardiovascular risk factors, including lipid risk variables, uric acid concentration, and heart rate, among US adults compared to BMI [3]. A possible explanation for these observations may be that the two components of LAP, abdominal fat and triglyceride concentrations, have greater physiological correlations with lipid and lipoprotein metabolism, as well as lipoprotein particle size, compared to BMI (describing lipid over-accumulation) [3]. In our study, compared to BMI, LAP had greater correlation with fasting serum glucose, lipid and lipoprotein parameters, and lipid peroxidation index. BMI rather than LAP was correlated with serum insulin and hs-CRP; the association of both BMI and LAP with HOMA-IR were similar.
In young healthy Korean women, higher LAP was also related to higher postprandial glucose levels, insulin response and homeostatic assessment model of insulin resistance [8]. Polycystic ovary syndrome patients in the higher quartile of LAP, had a risk of impaired glucose tolerance of 41.81 (95% CI, 5.52 to 316.54) [14]. An 11-year follow-up of nondiabetic patients showed that visceral adiposity, but not abdominal subcutaneous fat, directly measured by computed tomography (CT) scan as the volume of intra-abdominal fat at the umbilicus level, was an independent predictor of insulin resistance [15]. In the current study, the insulin resistance index in patients with higher visceral lipid accumulation was twice as high (4.77±0.49 vs. 2.12±0.51, in the first and fourth quartiles, respectively). Some possible mechanisms have been proposed regarding the association of visceral fat and insulin resistance; first, visceral fat, compared to subcutaneous fat, has a higher rate of lypolysis and subsequently, could produce a higher free fatty acid load, which leads to fat accumulation in the liver and induces insulin resistance; second, adipocytokines derived from the visceral fat may be responsible for induction of insulin resistance [16].
Another finding of this study was the strong association of LAP with total cholesterol, HDL-C levels and triglyceride/HDL-C ratio, independent risk factors of cardiovascular disease. LAP has been correlated with total cholesterol (r=0.498, P<0.001), and HDL-C (r=-0.319, P=0.026) [10]. In a previous study, visceral adipose tissue assessed by CT scan was significantly related to apolipoprotein B (β=1.33, P=0.001) and HDL-C (β=-1.89, P=0.004) [11]. Another study also showed that visceral fat accumulation was correlated with apolipoprotein B (r=0.26, P<0.05), and HDL-C (r=-0.26, P<0.05) [12]. Abnormal levels of adipocytokines caused by higher levels of visceral adiposity, including decreased levels of adiponectin and increased levels of visfatin, have been suggested as mediators of dyslipidemia [17]. Triglyceride/HDL-C ratio in patients with higher LAP was more than 3-fold (6.93±0.41 vs. 2.23±0.43, in the first and fourth quartiles, respectively); this ratio is directly related to lipoprotein particle size and the risk of atherosclerosis [18,19].
In the current study, LAP was strongly correlated with MDA, an important biomarker of lipid peroxidation and oxidative stress, independent of age, gender, and fasting glucose levels. Although the association between LAP and oxidative stress parameters has not yet been determined, previous studies have reported that higher visceral adiposity induced oxidative stress and lipid peroxidation. In healthy men and women, TBARs as biomarkers of systemic oxidative stress were positively related to visceral adipose tissue and development of subclinical atherosclerosis [20]. Visceral fat was also correlated with serum TBARs/cholesterol ratio (r=0.541, P<0.001) in patients with metabolic syndrome [21]. Moreover, visceral fat was reported as a significant determinant of expression of genes related to oxidative stress [22].
A moderately significant correlation between LAP and hs-CRP (r=0.25, P=0.007), an indicator of subclinical systemic inflammation, was also observed in this study. A similar association was recently reported in postmenopausal women (r=0.315, P=0.042) [10]. It is well known that obesity and increased visceral adipocytes contribute to increased levels of several inflammatory proteins such as CRP, interleukine-6, plasminogen activator inhibitor-1, P-selectin, vascular cell adhesion molecule 1, fibrinogen, and α1-acid glycoprotein [23,24]. In a prospective cohort, a 6-year follow-up of middle-aged individuals showed that increases in visceral adiposity, measured by CT scan, were associated with increased levels of CRP (r2=17.9%) [25].
Although, previous studies have indicated that LAP index is correlated to some cardiometabolic risk factors, to our knowledge these associations in diabetic patients are reported for the first time in this study. Moreover the correlation between LAP and oxidative stress in diabetic patients has not been previously reported. There were some limitations which might be considered important in the current study: cross-sectional setting and small sample size. Also, some potentially confounding variables including duration of diabetes, levels of glycosylated hemoglobin, and chronic vascular complications in diabetic patients have been not considered in the analysis. In addition, the validity of HOMA-IR as an insulin resistance parameter has not validated in the patients.
In conclusion, LAP showed strong associations with glucose hemostasis parameters, lipid and lipoprotein levels, atherosclerotic lipid parameters, lipid peroxidation, and a subclinical inflammatory marker in type 2 diabetic patients. It is plausible to suggest that LAP may be a useful and simple clinical marker for assessment of cardiometabolic risk factors in type 2 diabetic patients. Further studies of longer durations are recommended to better estimate the power of LAP in the prediction of diabetes complications.
ACKNOWLEDGMENTS
This study was funded by the Research Institute of Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran. The authors express appreciation to the participants of this study. The authors wish to thank Ms. N. Shiva for critical editing of English grammar and syntax of the manuscript.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Wakabayashi I, Daimon T. A strong association between lipid accumulation product and diabetes mellitus in japanese women and men. J Atheroscler Thromb. 2014;21:282–288. doi: 10.5551/jat.20628. [DOI] [PubMed] [Google Scholar]
- 2.Xiang S, Hua F, Chen L, Tang Y, Jiang X, Liu Z. Lipid accumulation product is related to metabolic syndrome in women with polycystic ovary syndrome. Exp Clin Endocrinol Diabetes. 2013;121:115–118. doi: 10.1055/s-0032-1333261. [DOI] [PubMed] [Google Scholar]
- 3.Kahn HS. The "lipid accumulation product" performs better than the body mass index for recognizing cardiovascular risk: a population-based comparison. BMC Cardiovasc Disord. 2005;5:26. doi: 10.1186/1471-2261-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ioachimescu AG, Brennan DM, Hoar BM, Hoogwerf BJ. The lipid accumulation product and all-cause mortality in patients at high cardiovascular risk: a PreCIS database study. Obesity (Silver Spring) 2010;18:1836–1844. doi: 10.1038/oby.2009.453. [DOI] [PubMed] [Google Scholar]
- 5.Wehr E, Pilz S, Boehm BO, Marz W, Obermayer-Pietsch B. The lipid accumulation product is associated with increased mortality in normal weight postmenopausal women. Obesity (Silver Spring) 2011;19:1873–1880. doi: 10.1038/oby.2011.42. [DOI] [PubMed] [Google Scholar]
- 6.Yang C, Guo ZR, Hu XS, Zhou ZY, Wu M. A prospective study on the association between lipid accumulation product or body mass index and diabetes. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31:5–8. [PubMed] [Google Scholar]
- 7.Chiang JK, Koo M. Lipid accumulation product: a simple and accurate index for predicting metabolic syndrome in Taiwanese people aged 50 and over. BMC Cardiovasc Disord. 2012;12:78. doi: 10.1186/1471-2261-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oh JY, Sung YA, Lee HJ. The lipid accumulation product as a useful index for identifying abnormal glucose regulation in young Korean women. Diabet Med. 2013;30:436–442. doi: 10.1111/dme.12052. [DOI] [PubMed] [Google Scholar]
- 9.Ji BL, Li R, Zhang SH, Gong LL, Wang ZH, Ren W, Li QF. The lipid accumulation product is highly related to serum alanine aminotransferase level in male adults. Nutr Res. 2012;32:581–587. doi: 10.1016/j.nutres.2012.06.019. [DOI] [PubMed] [Google Scholar]
- 10.Maturana MA, Moreira RM, Spritzer PM. Lipid accumulation product (LAP) is related to androgenicity and cardiovascular risk factors in postmenopausal women. Maturitas. 2011;70:395–399. doi: 10.1016/j.maturitas.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 11.Onat A, Avci GS, Barlan MM, Uyarel H, Uzunlar B, Sansoy V. Measures of abdominal obesity assessed for visceral adiposity and relation to coronary risk. Int J Obes Relat Metab Disord. 2004;28:1018–1025. doi: 10.1038/sj.ijo.0802695. [DOI] [PubMed] [Google Scholar]
- 12.Ribeiro-Filho FF, Faria AN, Kohlmann O, Jr, Ajzen S, Ribeiro AB, Zanella MT, Ferreira SR. Ultrasonography for the evaluation of visceral fat and cardiovascular risk. Hypertension. 2001;38(3 Pt 2):713–717. doi: 10.1161/01.hyp.38.3.713. [DOI] [PubMed] [Google Scholar]
- 13.Xia C, Li R, Zhang S, Gong L, Ren W, Wang Z, Li Q. Lipid accumulation product is a powerful index for recognizing insulin resistance in non-diabetic individuals. Eur J Clin Nutr. 2012;66:1035–1038. doi: 10.1038/ejcn.2012.83. [DOI] [PubMed] [Google Scholar]
- 14.Wehr E, Gruber HJ, Giuliani A, Moller R, Pieber TR, Obermayer-Pietsch B. The lipid accumulation product is associated with impaired glucose tolerance in PCOS women. J Clin Endocrinol Metab. 2011;96:E986–E990. doi: 10.1210/jc.2011-0031. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi T, Boyko EJ, McNeely MJ, Leonetti DL, Kahn SE, Fujimoto WY. Visceral adiposity, not abdominal subcutaneous fat area, is associated with an increase in future insulin resistance in Japanese Americans. Diabetes. 2008;57:1269–1275. doi: 10.2337/db07-1378. [DOI] [PubMed] [Google Scholar]
- 16.Jensen MD. Adipose tissue as an endocrine organ: implications of its distribution on free fatty acid metabolism. Eur Heart J Suppl. 2006;8(Suppl B):B13–B19. [Google Scholar]
- 17.Indulekha K, Anjana RM, Surendar J, Mohan V. Association of visceral and subcutaneous fat with glucose intolerance, insulin resistance, adipocytokines and inflammatory markers in Asian Indians (CURES-113) Clin Biochem. 2011;44:281–287. doi: 10.1016/j.clinbiochem.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FER(HDL)) Clin Biochem. 2001;34:583–588. doi: 10.1016/s0009-9120(01)00263-6. [DOI] [PubMed] [Google Scholar]
- 19.Frohlich J, Dobiasova M. Fractional esterification rate of cholesterol and ratio of triglycerides to HDL-cholesterol are powerful predictors of positive findings on coronary angiography. Clin Chem. 2003;49:1873–1880. doi: 10.1373/clinchem.2003.022558. [DOI] [PubMed] [Google Scholar]
- 20.Lear SA, Sarna LK, Siow TJ, Mancini GB, Siow YL, O K. Oxidative stress is associated with visceral adipose tissue and subclinical atherosclerosis in a healthy multi-ethnic population. Appl Physiol Nutr Metab. 2012;37:1164–1170. doi: 10.1139/h2012-107. [DOI] [PubMed] [Google Scholar]
- 21.Palmieri VO, Grattagliano I, Portincasa P, Palasciano G. Systemic oxidative alterations are associated with visceral adiposity and liver steatosis in patients with metabolic syndrome. J Nutr. 2006;136:3022–3026. doi: 10.1093/jn/136.12.3022. [DOI] [PubMed] [Google Scholar]
- 22.Yamaoka M, Maeda N, Nakamura S, Kashine S, Nakagawa Y, Hiuge-Shimizu A, Okita K, Imagawa A, Matsuzawa Y, Matsubara K, Funahashi T, Shimomura I. A pilot investigation of visceral fat adiposity and gene expression profile in peripheral blood cells. PLoS One. 2012;7:e47377. doi: 10.1371/journal.pone.0047377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freedland ES. Role of a critical visceral adipose tissue threshold (CVATT) in metabolic syndrome: implications for controlling dietary carbohydrates: a review. Nutr Metab (Lond) 2004;1:12. doi: 10.1186/1743-7075-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calabro P, Golia E, Maddaloni V, Malvezzi M, Casillo B, Marotta C, Calabro R, Golino P. Adipose tissue-mediated inflammation: the missing link between obesity and cardiovascular disease. Intern Emerg Med. 2009;4:25–34. doi: 10.1007/s11739-008-0207-2. [DOI] [PubMed] [Google Scholar]
- 25.Rheaume C, Arsenault BJ, Dumas MP, Perusse L, Tremblay A, Bouchard C, Poirier P, Despres JP. Contributions of cardiorespiratory fitness and visceral adiposity to six-year changes in cardiometabolic risk markers in apparently healthy men and women. J Clin Endocrinol Metab. 2011;96:1462–1468. doi: 10.1210/jc.2010-2432. [DOI] [PubMed] [Google Scholar]