Abstract
Objectives To investigate trends in the incidence of acute pancreatitis resulting in admission to hospital, and mortality after admission, from 1963 to 1998.
Design Analysis of hospital inpatient statistics for acute pancreatitis, linked to data from death certificates.
Setting Southern England.
Subjects 5312 people admitted to hospital with acute pancreatitis.
Main outcome measures Incidence rates for admission to hospital, case fatality rates at 0-29 and 30-364 days after admission, and standardised mortality ratios at monthly intervals up to one year after admission.
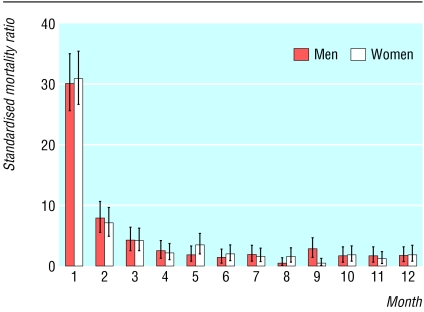
Results The incidence of acute pancreatitis with admission to hospital increased from 1963-98: age standardised incidence rates were 4.9 per 100 000 population in 1963-74, 7.7 in 1975-86, and 9.8 in 1987-98. Age standardised case fatality rates within 30 days of admission were 14.2% in 1963-74, 7.6% in 1975-86, and 6.7% in 1987-98. From 1975-98, standardised mortality ratios at 30 days were 30 in men and 31 in women (compared with the general population of equivalent age in the same period = 1), and they remained significantly increased until month 5 for men and month 6 for women.
Conclusions Incidence rates for acute pancreatitis with admission to hospital rose in both men and women from 1963 to 1998, particularly among younger age groups. This probably reflects, at least in part, an increase in alcoholic pancreatitis. Mortality after admission has not declined since the 1970s. This presumably reflects the fact that no major innovations in the treatment of acute pancreatitis have been introduced. Pancreatitis remains a disease with a poor prognosis during the acute phase.
Introduction
Acute pancreatitis has become increasingly common in Western countries in recent decades.1-8 When severe it has a high risk of mortality, but few studies have quantified mortality after hospital admission in defined populations and time periods.4-10 We investigated long term trends in the incidence of acute pancreatitis with admission to hospital and in mortality after admission.
Methods
Study population
We used the Oxford record linkage study, which comprises anonymised hospital statistical records linked to death certificate data (population of 0.35 million from 1963, 0.9 million from 1968, 1.8 million from 1975, and 2.5 million from 1987). We selected all admissions for acute pancreatitis as the principal diagnosis recorded in the database. We identified each patient's first admission and any death that followed it within 365 days. At the end of each 365 day period we included any subsequent admission for a “new” period of one year follow up. The database covered admissions from 1963 to 31 March 1998 with linkage to death certificates to 31 March 1999.
Statistical methods
We used admissions for acute pancreatitis as the numerator and the total resident population in the area covered by the data as the denominator to calculate incidence rates for admission to hospital. We used the direct method and the standard European population to standardise trends in incidence rates. We used admissions for acute pancreatitis as the denominator and deaths from any cause after admission as the numerator to calculate case fatality rates. Our standard population to standardise trends in case fatality rates directly was the total population of patients admitted for acute pancreatitis from 1963 to 1998. We used the indirect method, applying the age and sex specific death rates in the whole population of the region (the “standard” population) to the number of people admitted for acute pancreatitis in the equivalent age and sex strata to calculate standardised mortality ratios.
Results
Altogether 5312 people were admitted with acute pancreatitis; 2776 (52.3%) were men. The mean age of the patients was 56.3 (SD 19.2) years overall (men 53.2 (SD 18.0) years, women 59.7 (SD 19.8) years). The age of the patients admitted increased significantly over the study period (χ21 test for trend 8.1, P = 0.004 for men; and χ21 test for trend 15.1, P < 0.001 for women). Excluding all readmissions within one year of a previous admission for acute pancreatitis, 4778 people (89.9%) were admitted on only one occasion, 406 (7.6%) were admitted twice, and 128 (2.4%) were admitted on three or more occasions at least one year apart.
Incidence rates for both men and women increased substantially and significantly during the study period (table 1; figure A on bmj.com). Percentage increases in incidence rates were larger in younger than older age groups. Incidence rates also increased sharply with age (table 1).
Table 1.
Age specific and age standardised hospital admission rates for acute pancreatitis per 100 000 population, 1963-74, 1975-86 and 1987-98
|
1963-74
|
1975-86
|
1987-98
|
||||
|---|---|---|---|---|---|---|
| Age group | No of admissions | Rate per 100 000 population (95% CI) | No of admissions | Rate per 100 000 population (95% CI) | No of admissions | Rate per 100 000 population (95% CI) |
| Men | ||||||
| <35 | 18 | 0.7 (0.4 to 1.1) | 174 | 2.5 (2.1 to 2.9) | 299 | 3.6 (3.2 to 4.0) |
| 35-44 | 27 | 5.0 (3.1 to 6.8) | 126 | 7.6 (6.3 to 9.0) | 295 | 13.8 (12.2 to 15.3) |
| 45-54 | 41 | 8.4 (5.8 to 11.0) | 177 | 12.6 (10.8 to 14.5) | 284 | 15.7 (13.9 to 17.5) |
| 55-64 | 43 | 10.5 (7.4 to 13.7) | 176 | 14.4 (12.2 to 16.5) | 251 | 18.6 (16.3 to 20.9) |
| 65-74 | 34 | 13.5 (9.0 to 18.1) | 199 | 23.1 (19.9 to 26.3) | 253 | 25.4 (22.2 to 28.5) |
| 75+ | 28 | 21.7 (13.6 to 29.9) | 131 | 33.5 (27.4 to 39.6) | 214 | 35.5 (30.6 to 40.4) |
| All ages | 191 | 5.2 (4.5 to 5.9) | 983 | 8.6 (8.1 to 9.2) | 1596 | 11.2 (10.6 to 11.7) |
| Women | ||||||
| <35 | 18 | 0.8 (0.4 to 1.2) | 128 | 1.9 (1.6 to 2.2) | 219 | 2.8 (2.4 to 3.1) |
| 35-44 | 18 | 3.6 (1.9 to 5.3) | 81 | 5.1 (4.0 to 6.2) | 162 | 7.7 (6.5 to 8.9) |
| 45-54 | 20 | 4.1 (2.3 to 5.9) | 89 | 6.5 (5.1 to 7.8) | 185 | 10.6 (9.0 to 12.1) |
| 55-64 | 49 | 11.1 (8.0 to 14.2) | 157 | 12.3 (10.3 to 14.2) | 194 | 14.4 (12.4 to 16.4) |
| 65-74 | 50 | 14.9 (10.8 to 19.0) | 208 | 19.8 (17.1 to 22.5) | 250 | 21.3 (18.7 to 24.0) |
| 75+ | 46 | 19.5 (13.8 to 25.2) | 285 | 35.2 (31.0 to 39.3) | 373 | 34.2 (30.7 to 37.7) |
| All ages | 201 | 4.5 (3.9 to 5.2) | 948 | 6.7 (6.3 to 7.2) | 1383 | 8.4 (7.9 to 8.8) |
| Total* | 392 | 4.9 (4.4 to 5.4) | 1931 | 7.7 (7.3 to 8.0) | 2979 | 9.8 (9.4 to 10.1) |
The International Classification of Diseases (ICD) code used for acute pancreatitis was 587.0 in the 7th revision, 577.0 in ICD-8 and ICD-9, and K85 in ICD-10.
The ages of 10 people were not known.
Standardised case fatality rates at 0-29 and 30-364 days are summarised for the three periods 1963-74, 1975-86, and 1987-98 in table 2 and table A on bmj.com, and at 0-29 days for individual calendar years in figure B on bmj.com. Case fatality in men declined through the late 1960s but not thereafter, and we found no evidence of a decline in women (figure B on bmj.com). From 1975 to 1998, within a month of admission, the case fatality rate was 7.1%; at 30-364 days it was 5.1% (table 3). Case fatality rates increased substantially with age (table 3). We found no significant difference between men and women in age adjusted case fatality rates (table 3).
Table 2.
Case fatality rates per 100 patients, adjusted for age groups and sex, with odds ratios for the case fatality rates derived through logistic regression analysis, at 0-29 days and 30-364 days after hospital admission for acute pancreatitis, 1963-74, 1975-86, and 1987-98
|
0-29 days
|
30-364 days
|
||||||
|---|---|---|---|---|---|---|---|
| Time period | No of admissions | No of deaths | Case fatality rate (95% CI) | Odds ratio (95% CI) | No of deaths | Case fatality rate (95% CI) | Odds ratio (95% CI) |
| 1963-74 | 396 | 55 | 14.2 (9.9 to 18.4) | 1.00 | 25 | 5.6 (3.3 to 8.0) | 1.00 |
| 1975-86 | 1934 | 156 | 7.6 (6.4 to 8.8) | 0.48 (0.34 to 0.68) | 105 | 5.1 (4.2 to 6.1) | 0.88 (0.56 to 1.41) |
| 1987-98 | 2982 | 193 | 6.7 (5.7 to 7.7) | 0.41 (0.29 to 0.58) | 146 | 5.1 (4.3 to 5.9) | 0.87 (0.55 to 1.37) |
| 1963-98 (total) | 5312 | 404 | 7.6 (6.9 to 8.4) | 276 | 5.2 (4.6 to 5.8) | ||
Table 3.
Case fatality rates per 100 patients, with odds ratios for the case fatality rates derived through logistic regression analysis, for the effects of age group and sex at 0-29 days and 30-364 days after hospital admission for acute pancreatitis, 1975-98
|
0-29 day follow-up
|
30-364 day follow up
|
||||||
|---|---|---|---|---|---|---|---|
| No of admissions | No of deaths | Case fatality rate (95% CI) | Odds ratio (95% CI) | No of deaths | Case fatality rate (95% CI) | Odds ratio (95% CI) | |
| Age group*: | |||||||
| <35 | 820 | 15 | 1.8 (0.9 to 2.7) | 1.00 | 8 | 1.0 (0.3 to 1.6) | 1.00 |
| 35-44 | 664 | 10 | 1.5 (0.6 to 2.4) | 0.82 (0.37 to 1.83) | 11 | 1.7 (0.7 to 2.6) | 1.69 (0.68 to 4.24) |
| 45-54 | 735 | 20 | 2.7 (1.5 to 3.9) | 1.49 (0.76 to 2.93) | 20 | 2.7 (1.5 to 3.9) | 2.82 (1.23 to 6.43) |
| 55-64 | 778 | 41 | 5.3 (3.7 to 6.9) | 2.99 (1.64 to 5.45) | 39 | 5.0 (3.4 to 6.6) | 5.38 (2.50 to 11.6) |
| 65-74 | 910 | 73 | 8.0 (6.2 to 9.8) | 4.72 (2.69 to 8.30) | 68 | 7.4 (5.7 to 9.2) | 8.30 (3.96 to 17.4) |
| 75+ | 1003 | 190 | 18.9 (16.2 to 21.6) | 12.91 (7.55 to 22.1) | 105 | 10.5 (8.5 to 12.5) | 12.31 (5.95 to 25.5) |
| Sex*: | |||||||
| Male | 2583 | 161 | 7.5 (6.3 to 8.7) | 1.00 | 124 | 5.3 (4.4 to 6.3) | 1.00 |
| Female | 2333 | 188 | 6.5 (5.6 to 7.5) | 0.88 (0.70 to 1.11) | 127 | 4.7 (3.8 to 5.5) | 0.86 (0.66 to 1.11) |
| All patients | 4910 | 349 | 7.1 (6.4 to 7.8) | 251 | 5.1 (4.5 to 5.8) | ||
Age specific mortality is adjusted for sex, and sex specific mortality is adjusted for age group. The ages of 6 patients admitted from 1975-98 were not known.
At one month after hospital admission, mortality was 30 times higher in men and 31 times higher in women than that in the general populations of men and women of equivalent age from 1975 to 1998 (figure). At month 2, mortality was, respectively, eight and seven times higher. Mortality remained significantly elevated until month 5 for men and month 6 for women.
Figure 1.
Standardised mortality ratios with 95% confidence intervals at monthly intervals after hospital admission for acute pancreatitis in men and women, 1975-98. (Standardised mortality ratio in the general population = 1)
The underlying cause of death was acute pancreatitis in 314 (46.2%) of 680 deaths within one year of admission, chronic pancreatitis in 11, other or unspecified diseases of the pancreas (6), other diseases of the gastrointestinal system (76), malignant neoplasms of the pancreas (33), other neoplasms (48), diseases of the circulatory system (108), and various other causes (84).
Discussion
Acute pancreatitis remains a disease with high mortality: death rates in the first month after admission are 30 times higher than in the general population of the same age. Case fatality rates have not improved since the 1970s.
Limitations of the study
Our study's main limitations are that little clinical information and no pathology data were available about individuals. It was therefore not possible to report on the evidence on which the diagnoses were based, to study treatment, or to distinguish between the two main aetiologies, biliary tract disease and alcoholic pancreatitis. The relative contribution of these two aetiologies varies between different places, over time, between men and women, and at different ages. For example, alcohol consumption is higher in young people than in elderly women, but pancreatitis is more common in elderly women. Acute pancreatitis among young people is more commonly alcohol related, whereas in elderly women it is mainly caused by biliary tract disease.
Strengths of the study
The main strengths of this study are that it is a large, population based analysis of more than 5000 cases. It shows long term trends in hospital admission rates and mortality after admission over a 36 year period, and it is based on systematic follow up through linkage to death certificate data.
Comparison with other studies
Almost all people who receive a diagnosis of acute pancreatitis will have been admitted to hospital. Our figures on admission rates are therefore a good approximation of true, diagnosed incidence. A recent national study, covering a much shorter period of time than ours, reported an age standardised admission rate for acute pancreatitis in the whole of England that increased from 14.5 per 100 000 in 1989-90 to 20.7/100 000 in 1999-2000.7 This is higher than in our study of the Oxford region. However, the national study used hospital episode statistics: these are based on finished consultant episodes of care, which are invariably higher than the actual numbers of people treated.
What is already known on this topic
The incidence of acute pancreatitis has increased in Britain in recent decades
Acute pancreatitis has a poor prognosis, although data on its incidence and prognosis in defined populations are sparse
What this study adds
Hospital admission rates in the population studied have doubled over the past 30 years
Increases in admission rates over time were greater in the younger age groups and, at least in part, probably represent an increase in alcoholic pancreatitis
Death rates in the first month after an attack are about 30 times higher than mortality in the general population of equivalent age
Case fatality rates have shown little or no improvement since the 1970s
The authors of the English national study,7 and others,11,12 have suggested that the rise in pancreatitis is probably, in particular, a rise in alcoholic pancreatitis related to increasing use of alcohol in the community. The similarities between the trend profiles for incidence of acute pancreatitis in our study, and those of increasing alcohol consumption7,13,14 and alcohol related deaths,15 indicate an increase in alcoholic pancreatitis. However, the possibility exists that other factors, too, may have contributed to the rise. One possibility is an increase in the prevalence of gall stones; another is improvements in case ascertainment.
Acute pancreatitis is fairly uncommon. Our unstandardised incidence rates of 4.6 per 100 000 in 1963-74, 7.7/100 000 in 1975-86, and 10.2/100 000 in 1987-98 are comparable to those reported in earlier English studies.2,10,16,17 Reported rates have tended to be higher in Scotland,5,18 the United States,1,19 Germany,20 and the Scandinavian countries8,21,22 than in England, although rates in the Netherlands6,23 have been more comparable.
Although some studies have reported reductions over time in case fatality rates,4-8 a large Finnish study found no decrease from the 1980s onwards.24 The fact that case fatality in our study has not fallen since the 1970s is no doubt because no major innovations in treatment have been introduced in recent times.
Supplementary Material
 Additional figures A and B and table A are on bmj.com
Additional figures A and B and table A are on bmj.com
The database was built over many years by Leicester Gill, Glenys Bettley, and Myfanwy Griffith. We thank David Yeates for extraction of data for analysis.
Contributors: MJG and SER designed the study and wrote the manuscript. SER reviewed the literature and undertook the analyses. MJG and SER are guarantors.
Funding: The Research and Development Directorate of the Department of Health funds the Unit of Health Care Epidemiology to undertake research using the database. The database was funded by the former Oxford Regional Health Authority.
Competing interests: None declared.
Ethical approval: Oxford Region Data Protection Steering Group and the health authorities' Caldicott Guardians for building the original database. Ethical approval was not needed for analysis of a fully anonymised statistical dataset.
References
- 1.O'Sullivan JN, Nobrega FT, Morlock CG, Brown AL Jr, Bartholomew LG. Acute and chronic pancreatitis in Rochester, Minnesota, 1940 to 1969. Gastroenterology 1972;62: 373-9. [PubMed] [Google Scholar]
- 2.Corfield AP, Cooper MJ, Williamson RC. Acute pancreatitis: a lethal disease of increasing incidence. Gut 1985;26: 724-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lankisch PG, Schirren CA, Schmidt H, Schonfelder G, Creutzfeldt W. Etiology and incidence of acute pancreatitis: a 20-year study in a single institution. Digestion 1989;44: 20-5. [DOI] [PubMed] [Google Scholar]
- 4.Wilson C, Imrie CW. Changing patterns of incidence and mortality from acute pancreatitis in Scotland, 1961-1985. Br J Surg 1990;77: 731-4. [DOI] [PubMed] [Google Scholar]
- 5.McKay CJ, Evans S, Sinclair M, Carter CR, Imrie CW. High early mortality rate from acute pancreatitis in Scotland, 1984-1995. Br J Surg 1999;86: 1302-5. [DOI] [PubMed] [Google Scholar]
- 6.Eland IA, Sturkenboom MJ, Wilson JH, Stricker BH. Incidence and mortality of acute pancreatitis between 1985 and 1995. Scand J Gastroenterol 2000;35: 1110-6. [DOI] [PubMed] [Google Scholar]
- 7.Tinto A, Lloyd DA, Kang JY, Majeed A, Ellis C, Williamson RC, Maxwell JD. Acute and chronic pancreatitis—diseases on the rise: a study of hospital admissions in England 1989/90-1999/2000. Aliment Pharmacol Ther 2002;16: 2097-105. [DOI] [PubMed] [Google Scholar]
- 8.Floyd A, Pedersen L, Nielsen GL, Thorladcius-Ussing O, Sorensen HT. Secular trends in incidence and 30-day case fatality of acute pancreatitis in North Jutland County, Denmark: a register-based study from 1981-2000. Scand J Gastroenterol 2002;37: 1461-5. [DOI] [PubMed] [Google Scholar]
- 9.Mann DV, Hershman MJ, Hittinger R, Glazer G. Multicentre audit of death from acute pancreatitis. Br J Surg 1994;81: 890-3. [DOI] [PubMed] [Google Scholar]
- 10.Toh SK, Phillips S, Johnson CD. A prospective audit against national standards of the presentation and management of acute pancreatitis in the south of England. Gut 2000;46: 239-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mero M. Changing aetiology of acute pancreatitis. Ann Chir Gynaecol 1982;71: 126-9. [PubMed] [Google Scholar]
- 12.Secknus R, Mössner J. Inzidenzund Prävalenzveränderungen der akuten und chronischen Pankreatitis in Deutschland [Changes in incidence and prevalence of acute and chronic pancreatitis in Germany]. Chirurg 2000;71: 249-52. [PubMed] [Google Scholar]
- 13.Johnson CD, Hosking S. National statistics for diet, alcohol consumption, and chronic pancreatitis in England and Wales, 1960-88. Gut 1991;32: 1401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Statistics. Living in Britain: results from the 2000 general household survey. London: Stationery Office, 2001: 159.
- 15.Baker A, Rooney C. Recent trends in alcohol-related mortality, and the impact of ICD-10 on the monitoring of these deaths in England and Wales. Health Stat Q 2003;17: 5-14. [Google Scholar]
- 16.Trapnell JE, Duncan EH. Patterns of incidence in acute pancreatitis. BMJ 1975;2: 179-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourke JB. Variation in annual incidence of primary acute pancreatitis in Nottingham, 1969-74. Lancet 1975;2: 967-9. [DOI] [PubMed] [Google Scholar]
- 18.Thomson SR, Hendry WS, McFarlane GA, Davidson AI. Epidemiology and outcome of acute pancreatitis. Br J Surg 1987;74: 398-401. [DOI] [PubMed] [Google Scholar]
- 19.Go VLW. Etiology and epidemiology of pancreatitis in the United States. In: Bradley EL III, ed. Acute pancreatitis: diagnosis and therapy. New York: Raven Press, 1994: 235-9.
- 20.Lankisch PG, Assmus C, Maisonneuve P, Lowenfels AB. Epidemiology of pancreatic diseases in Luneburg county. A study in a defined German population. Pancreatology 2002;2: 469-77. [DOI] [PubMed] [Google Scholar]
- 21.Halvorsen FA, Ritland S. Acute pancreatitis in Buskerud county, Norway. Incidence and etiology. Scand J Gastroenterol 1996;31: 411-4. [DOI] [PubMed] [Google Scholar]
- 22.Appelros S, Borgstrom A. Incidence, aetiology and mortality rate of acute pancreatitis over 10 years in a defined urban population in Sweden. Br J Surg 1999;86: 465-70. [DOI] [PubMed] [Google Scholar]
- 23.Tran DD, Van Schilfgaarde R. Prevalence and mortality from acute pancreatitis in the Netherlands during 1971-1990 [abstract]. Digestion 1994;55: 342-3. [Google Scholar]
- 24.Gronroos JM, Nylamo EI. Mortality in acute pancreatitis in Turku University Central Hospital 1971-1995. Hepatogastroenterology 1999;46: 2572-4. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.