Abstract
To better understand the financial viability of hospital emergency departments (EDs), we created national estimates of the cost to hospitals of providing ED care and the associated hospital revenue using hospital financial reports and patient claims data from 2009. We then estimated the effect the Affordable Care Act (ACA) will have on the future profitability of providing ED care. We estimated that hospital revenue from ED care exceeded costs for that care by $6.1 billion in 2009, representing a profit margin of 7.8 percent (net revenue expressed as a percentage of total revenue). However, this is primarily because hospitals make enough profit on the privately insured ($17 billion) to cover underpayment from all other payer groups, such as Medicare, Medicaid, and unreimbursed care. Assuming current payer reimbursement rates, ACA reforms could result in an additional 4.4-percentage-point increase in profit margins for hospital-based EDs compared to what could be the case without the reforms.
There is increasing financial pressure being placed on hospitals. Payment cuts in Medicare and Medicaid, coupled with tighter restrictions from private insurance, have reduced the rate of hospital revenue growth to its lowest level in decades.1 Although all parts of hospitals are under financial pressures, the emergency department (ED) may be particularly vulnerable. Emergency care has high fixed costs in terms of standby capacity, or the additional resources needed to accommodate large increases in patients that could result, for example, from natural disasters, accidents, or pandemics. EDs also provide care for low-acuity visits at a substantially higher cost to insurers than similar outpatient care, and they treat many patients who do not have insurance or have insurance that pays poorly.
To date, however, little is known about ED finances. Are EDs significant money losers, as a cursory look at their payer mix would suggest? Or are they gateways to admission for complex, well-insured patients and other downstream outpatient services, and thus profitable aspects of the health care system for hospitals? The literature is mixed on this topic. There are some indications that EDs are profitable for hospitals. From 2000 to 2006, despite an 11.6 percent decrease in inpatient bed capacity, the average ED bed capacity increased by 15 percent.2 Indeed, the majority of ED closures are associated with the closing of the entire hospital, not a selective closing of that department.3,4 Furthermore, the emergence of freestanding EDs in some markets suggests that emergency care is profitable—at least for some visits.5
There are also indications to the contrary. ED payment for the most vulnerable patients, who frequently depend on ED availability, has declined in real terms. Between 2003 and 2008 Medicaid physician payments for care other than primary care grew at 1.5 percent annually, compared to growth in the Consumer Price Index of 3.4 percent per year.6 In addition, there were 27 percent fewer EDs in nonrural areas in 2009 than there were ten years earlier, and hospitals that disproportionately care for the poor are more likely to close than others.7 Finally, the persistent and pervasive nature of ED overcrowding suggests that hospitals do not have sufficient financial incentives to expand capacity to meet demand.8 Future profitability is at risk, given the perception among many policy makers that emergency care represents a significant potential source of savings for payers, from reductions in “unnecessary” ED visits and resulting hospital admissions.
As more Americans obtain health insurance coverage as a result of the Affordable Care Act (ACA), understanding the effect of this coverage on ED use and ED admissions will become increasingly important. If the Massachusetts experience with universal coverage represents the experience for the United States as a whole, there may be no significant increase in ED usage.9 There is, however, evidence from the Oregon Health Insurance Experiment that providing the uninsured with Medicaid increases ED use.10 Furthermore, allowing young adults to stay on their parents’ health insurance until age twenty-six results in increased ED visit and hospital admission rates.11
In this study we addressed two related questions. First, we explored whether patient care provided in EDs is profitable for hospitals, and if so, for which kinds of patients. Second, we estimated the impact of the ACA on future profitability of EDs and their likely financial viability.
In this article we start by providing a brief overview of several unique aspects of ED services that are relevant to this study. We then discuss the specific methods used and their limitations. Finally, we present our results, followed by a discussion of their implications for ED health policy.
Background
ED visits are classified as outpatient or inpatient visits, depending upon the patient’s disposition at the end of the ED visit. When patients are discharged home from the ED, are transferred to another facility, die in the ED prior to hospital admission, are admitted to an ED-run short-stay observation unit, or are admitted to the hospital under observation status, their ED visit is classified as an outpatient hospital visit. When patients are directly admitted to the hospital affiliated with that ED, which occurred 15.3 percent of the time in 2010, these ED visits are classified as inpatient visits.12
The level of billing detail for ED visits varies by ED disposition and payer type. Medicare and most Medicaid programs pay for both inpatient hospitalizations and outpatient ED visits using a fixed fee–based system. Their corresponding inpatient data sets do not have detailed ED payment or charge data. Payments are aggregated at the visit level and, for admitted patients, include payment for inpatient and ED services. For ED visits resulting in hospital admission, charges are aggregated at the hospital revenue center level, and the ED charge component does not contain charges for some ancillary services (labs and radiology studies) provided in the ED. Charges for these services are reflected in the aggregate radiology and laboratory revenue center charge components and reflect both ED and inpatient services. Commercial payers reimburse hospitals for admissions in a variety of ways, including a fee-for-service or per diem basis.13 For patients whose care is reimbursed in this way, their more detailed payer billing records allow for revenue from individual ED services to be separated from inpatient service revenue. For outpatient ED visits across all payers, hospital charges and revenue data reflect all facility services, including ancillary services, billed for during the ED visits.
Finally, there are a variety of arrangements between hospitals and emergency physicians that affect hospital revenue and costs. Twenty-one percent of ED physicians are hospital employees, so the hospitals that employ them incur salary costs and collect revenue for physician services.14 Fifty-seven percent of ED physicians are in single-specialty groups. Hospitals partially or wholly own a minority (22 percent) of all such groups. Single-specialty physician groups typically collect revenue for ED physician services, are responsible for salary costs, and sometimes receive hospital subsidies in exchange for providing ED services.
Study Data And Methods
We created national estimates of the cost to hospitals of providing ED care and the associated hospital revenue using hospital financial reports and patient claims data from 2009.We then estimated the effect the ACA will have on the distribution of ED visits by payer type and associated changes in ED revenue. For this analysis we defined the scope of emergency care to include ED facility services, ancillary services such as labs and radiology services, and physician services for which the hospital collects revenue or incurs direct costs.
REVENUE ESTIMATES
To obtain ED-associated hospital revenue, we created national estimates of use and reimbursement by insurance type. Our ED revenue estimates reflect payments to hospitals from patients’ primary and coinsurance carriers, out-of-pocket payments, and physician payments for services provided by hospital employees or members of hospital-owned physician groups.
For Medicare patients, we used the 5 percent sample Medicare Provider Analysis and Review (MEDPAR) File and Medicare Outpatient File to capture data on fee-for-service Medicare beneficiaries who received ED care in 2009. Hospital revenue for outpatient visits was obtained directly from the claims files and reflects hospital payments for all facility services provided in the ED, including ancillary services.
For Medicare patients admitted to the hospital from the ED, we attributed a portion of hospital downstream revenue for the admission to the ED, to reflect hospital payment for services provided in the ED. To accomplish this, we applied a ratio of total ED facility charges (including charges for ancillary services) to total hospital charges to the hospital payment amount. As mentioned in the background section, in Medicare inpatient claims files, the ED revenue center charges component does not include charges for ancillary services provided in the ED. To create a measure of total ED facility charges, we needed to attribute a portion of total lab and radiology charges for the admission to the ED. We assumed that lab and radiology resource use is skewed toward the early part of an admission, as is true for resource use overall. We therefore added one full day’s worth of lab and radiology charges for that admission to the ED charges component contained in the inpatient claims file. For one-day inpatient admissions, this method would attribute all radiology and lab charges for the admission to the ED. For these admissions we added half a day’s worth of charges.
We were not able to determine the relative impact of care received in the ED versus care received during the remainder of an admitted patient’s hospital stay on total hospital revenue generated. However, care in both settings is likely necessary, and attributing either all or none of the revenue to the ED seems less reasonable.
To account for hospital revenue from services provided by physicians employed by hospitals or physicians in hospital-owned practices, we first measured aggregate Medicare physician payments for care provided in the ED using Medicare’s Physician/Supplier Part B claims file. We then inflated our hospital revenue estimates by 34 percent of this total, given that 21 percent of ED physicians are hospital employees and, we estimate, that an additional 13 percent belong to single-specialty practices partially or completely owned by a hospital.
Demonstrating that EDs are profitable has important implications for health care’s transition to accountable care organizations.
Medicare claims data sets contain billing records only for Medicare fee-for-service visits. To account for missing ED visits from Medicare-managed care patients, we weighted Medicare fee-for-service visit rates using national estimates for all Medicare visits from the 2009 Nationwide Emergency Department Sample (NEDS),12,15 adjusted for age, sex, region, clinical condition, and ED disposition (admission to same hospital, low-acuity ED discharge [discharge to home, nursing home, or a rehabilitation facility], or high-acuity ED discharge [transfers to another inpatient facility or death in the ED]). These weights were applied to our hospital revenue estimates for the ED visit to obtain national revenue estimates.16
For patients with private insurance, we used a 5 percent sample of the 2009 MarketScan Research Databases from Truven Health Analytics claims data for people with employer-sponsored health insurance. With this data set, we directly measured hospital payments for all ED services for discharged patients and ED facility payments for patients admitted to the hospital. Payments for ancillary services provided in the ED for admitted patients could not be identified. We therefore attributed to the ED one day of total inpatient ancillary service payments for admissions originating from the ED. For one-day inpatient admissions, we added a half day’s worth of charges, for reasons previously explained.
To obtain national estimates from this large convenience sample, we weighted the observed visit rates using national estimates of visit totals for patients with private insurance from the 2009 NEDS, adjusting for age, sex, clinical condition, and ED disposition.17 These weights were then applied to the hospital revenue associated with the ED visit to obtain national estimates.
For Medicaid patients, we started with the 2009 NEDS database, which has patient-level ED charges but not hospital payments. We then imputed hospital payments in two steps. First, using our Medicare claim database, we found the nearest Medicare match for each Medicaid patient, matching on clinical condition, hospital region, location (urban, micropolitan, or rural), academic status, and ED charges (−$50). This method of matching resulted in a 22 percent loss in sample size (16.5 percent from missing charges in NEDS, 5.5 percent from unmatching). We inflated our matched sample to the original NEDS sample total charges for this group to account for this. With these matched data, we used 2008 state-based Medicaid-to-Medicare fee ratios for outpatient care (excluding obstetrics and primary care) aggregated to the region level18 to impute Medicaid payments for the visit.19
For the uninsured, we started with the 2009 NEDS database for self-pay patients. We then estimated revenue from the uninsured assuming that the ratio of payment to costs for the uninsured was the same as for Medicaid, using the methods outlined above.20
To account for hospital revenue from physician services provided to patients with Medicaid, private insurance, and the uninsured, we began by using Medicare data to estimate missing physician revenue as a percentage of total hospital revenue (excluding physician fees) for ED visits. We then applied this percentage to our Medicaid, private insurance, and uninsured revenue estimates.
COST ESTIMATES
We created our cost estimates by applying ED-specific cost-to-charge ratios from the 2009 Medicare Cost Reports to charges for each visit. The ED-specific ratios are calculated from information hospitals report on Worksheet C for the ED cost center. “Costs” are total reasonable hospital costs for ED services, including salary costs for ED physicians if they are hospital employees, minus certain capital reductions. The charges include gross inpatient and outpatient charges, including charges for charity care. We used three-year average cost-to-charge ratios (2008–10) and excluded hospitals for which the ratios were unreasonably large (>10).
For Medicare patients, we created a measure of total ED charges that reflected patient-level use of ED resources, including ancillary services as well as a portion of physician charges. For Medicaid, self-pay, and patients with private insurance, we used the ED charges measure available in the NEDS data sets. This measure does not include charges for ancillary services for patients admitted from the ED or any physician charges. We therefore adjusted the NEDS charges using Medicare data to estimate missing charges for ancillary services as a percentage of ED facility charges (adjusted for clinical condition, academic status, urban or rural location, and region) and missing physician charges as a percentage of aggregate charges by payer group.
For Medicare patients, we applied the ED-specific cost-to-charge ratio from the individual hospital where the patient was seen to the charges attributed to each ED patient. For Medicaid and self-pay patients, we used average ratios for hospitals from the same region; urban, micropolitan, or rural location; and academic status. For patients with private insurance, we used a national average hospital cost-to-charge ratio. These average ratios were weighted averages using Medicare ED visit volumes as a proxy for the ED’s overall visit volume.
CATEGORIZING ED VISITS
In addition to overall totals, we report hospital revenue and costs for similar ED visits using several different classification schemes. We started with ED visits by insurance type. We then estimated revenue and costs for patients based on visit acuity, using Dustin Ballard and colleagues’ modification of the New York University ED Algorithm using a 75/25 threshold for high- and low-acuity categories.21 This method categorizes visits into “emergent,” “nonemergent,” and “indeterminate” categories using the highest-acuity ED International Classification of Diseases, Ninth Revision (ICD-9), diagnosis associated with the visit. If the highest-acuity ICD-9 diagnosis was associated with a greater than 0.75 probability of being emergent, then that visit was classified as emergent. If the highest-acuity diagnosis was associated with a less than 0.25 probability of being emergent, then that visit was classified as nonemergent. Those in between were classified as indeterminate. Using the 75/25 thresholds yielded similar proportions of emergent, nonemergent, and indeterminate visits as found in the 2009 National Hospital Ambulatory Medical Care Survey.22
Finally, we report revenue and costs based on clinical condition. For this, we started with the multilevel Clinical Classifications Software (CCS) from the Agency for Healthcare Research and Quality (AHRQ).23 These “body system” classifications were then reclassified to reflect conditions typically seen by distinct medical specialists. We believe that this reclassification of ED visits groups them by similar expected resource use, because of both similar health care needs and similar practice patterns of consultants who may be involved in the ED care for the most critically ill cases.
LIMITATIONS
The methods we used for this study have several important limitations. We used imputed hospital payments for both Medicaid and self-pay visits. While this is unavoidable for self-pay visits, a study using nationally representative Medicaid claims would provide more accurate estimates. We also used national data on ED physician practice type to estimate hospital revenue and costs from physician services. Furthermore, our claims database for Medicare and private insurance was not completely nationally representative on its own and required weighting using another nationally representative database, NEDS. Finally, our hospital cost estimates were based on average cost-to-charge ratios for Medicaid, self-pay, and private insurance groups, not the ratio from the specific hospital where care was received. Ultimately, studies based upon microcosting methods,which collect detailed information on the specific resources used and their value, are needed to measure patient-level costs, although revenue center cost-to-charge ratios can produce reliable measures of average costs for large groups of patients.24
Study Results
Our final analytic data set includes more than eleven million ED visits with patient-level revenue information in 2009 and twenty million observations with charge data. When weighted, this represents 120 million ED visits. Put another way, there is approximately one ED visit per three Americans annually. The largest payer group of visits was the private insurance group, representing 35 percent of ED visits; 26 percent were Medicaid, 21 percent were Medicare, and 18 percent were uninsured. Fifteen percent of these visits resulted in hospital admission, 3 percent were transfers or ED deaths, and the remaining were discharged home.
We estimate that hospitals generated approximately $78.7 billion in revenue for care delivered in the emergency department in 2009, at a cost of about $72.5 billion (Exhibit 1). This represents a profit margin (net revenue expressed as a percentage of total revenue) of 7.8 percent. When the data were examined by payer group, patients with private insurance were the only group producing a positive profit margin, at 39.6 percent (Exhibit 2). People covered by all other payer groups are cared for in the ED at a substantial financial loss, with profit margins between −15.6 percent (Medicare) and −54.4 percent (uninsured).
EXHIBIT 1. Emergency Department (ED) Revenue And Cost, By Visit Category, 2009.
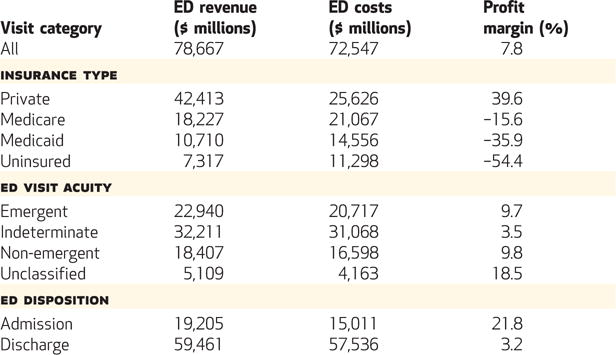
SOURCE Authors’ analysis conducted in January 2013 using the 2009 5 percent sample Medicare Provider and Analysis Review File; a 5 percent sample of the 2009 Truven Health MarketScan Commercial Claims and Encounters Database; 2009 Nationwide Emergency Department Sample (NEDS) database; 2009 Medicare Cost Reports; 2009 Medicaid enrollment by state from the Kaiser Family Foundation; and 2008 state-based Medicaid-to-Medicare fee ratios for outpatient care from Zuckerman et al., 2009 (Note 19 in text). NOTE Profit margin is defined as net revenue (revenue minus costs) divided by total revenue.
EXHIBIT 2. Hospitals’ Profit Margins For Emergency Department Care, By Insurance Type, 2009.
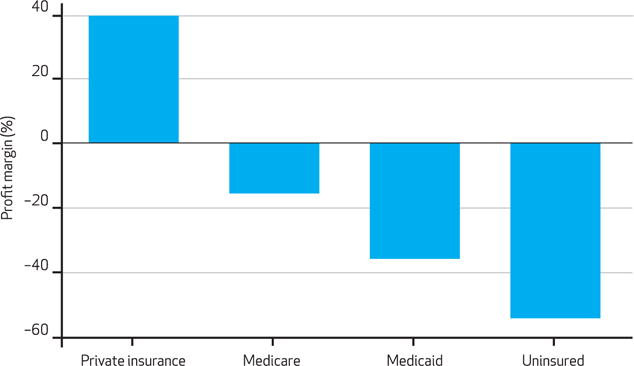
SOURCE Authors’ analysis conducted in January 2013 using the 2009 5 percent sample Medicare Provider and Analysis Review File; a 5 percent sample of the 2009 Truven Health MarketScan Commercial Claims and Encounters Database; 2009 Nationwide Emergency Department Sample (NEDS) database; 2009 Medicare Cost Reports; 2009 Medicaid enrollment by state from the Kaiser Family Foundation; and 2008 state-based Medicaid-to-Medicare fee ratios for outpatient care from Zuckerman et al., 2009 (Note 19 in text).
We also analyzed revenue and costs by ED visit acuity. Care for visits categorized as emergent and nonemergent was equally profitable for hospitals, with profit margins of 9.7 percent and 9.8 percent, respectively. Visits of indeterminate acuity represent the largest share of cost and revenue and were less profitable, with a profit margin of 3.5 percent (Exhibit 1).
Patients who were admitted to the hospital from the ED represented 24.4 percent of ED revenue and 20.7 percent of ED costs, and they were profitable overall, with a profit margin of 21.8 percent, because of the profitability of the private insurance and Medicare groups (Exhibit 1). Patients discharged from the ED represent the vast majority of ED costs and were profitable for hospitals as well, with a profit margin of 3.2 percent. ED discharges were markedly less profitable than admissions for patients with Medicaid and private insurance. For Medicare visits, the profit margin for ED discharges was −53.6 percent, compared to an admission profit margin of 18.4 percent. For patients with private insurance, ED discharges were profitable, but less so than hospital admissions. For patients with Medicaid and the uninsured, both ED discharges and admissions were associated with negative profits (see the online Appendix for details).27
When profitability was examined with respect to patient condition, patients with infectious diseases, traumatic conditions, and other surgical conditions (such as urology; ear, nose, and throat; or ophthalmology) were associated with the highest net profits of $1.29 billion, $1.15 billion, and $846 million, respectively (Exhibit 3). Patients with psychiatric conditions and those in the “signs/symptoms” category (patients with abdominal pain, transient loss of consciousness, weakness, or other ill-defined conditions) were the least profitable for hospitals ($45 million and −$245 million, respectively). This pattern was driven largely by the profitability of privately insure patients with indeterminate-acuity ED visits.
EXHIBIT 3. Hospitals’ Net Revenue (In Millions Of Dollars) For Emergency Department Care, By Condition, 2009.
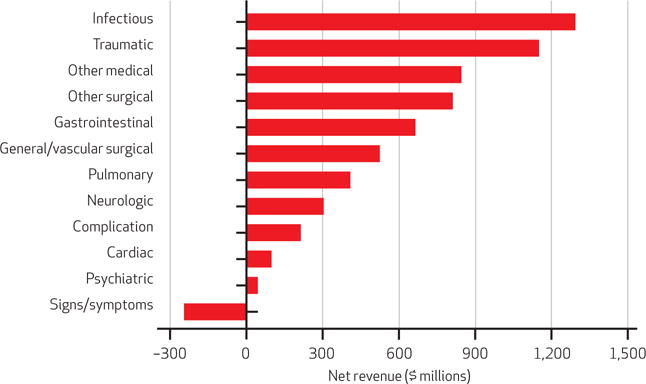
SOURCE Authors’ analysis conducted in January 2013 using the 2009 5 percent sample Medicare Provider and Analysis Review File; a 5 percent sample of the 2009 Truven Health MarketScan Commercial Claims and Encounters Database; 2009 Nationwide Emergency Department Sample (NEDS) database; 2009 Medicare Cost Reports; 2009 Medicaid enrollment by state from the Kaiser Family Foundation; and 2008 state-based Medicaid-to-Medicare fee ratios for outpatient care from Zuckerman et al., 2009 (Note 19 in text).
We estimated the future profitability of emergency care with and without the ACA. First we used projected population growth through 2023 to examine how ED profitability would change simply as a result of changing demographics, assuming continued growth in ED visit rates per person.25 Under this scenario, ED profit margins would be 7.3 percent in 2023. We then examined the likely impact of the ACA on ED profitability using a scenario in which 50 percent of the expected uninsured remain uninsured, 25 percent obtain private insurance, and 25 percent enroll in Medicaid. We assumed that hospital reimbursement for patients who obtain private insurance through the insurance exchanges, or Marketplaces, is at the midpoint between employer-sponsored private insurance and Medicaid reimbursement. We also assumed that the ACA will not have a significant impact on the number of people who obtain employer-sponsored insurance.26 Under this coverage scenario, ED revenues increase to $98.1 billion, with costs at $86.7 billion (Exhibit 4). This results in a projected profit margin of 11.7 percent.
EXHIBIT 4. Simulations Of Future Emergency Department (ED) Revenue And Cost.
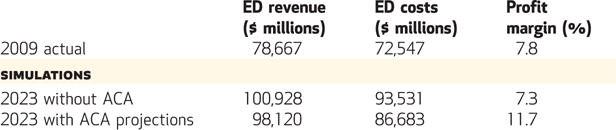
SOURCE Authors’ analysis conducted in January 2013 using the 2009 5 percent sample Medicare Provider and Analysis Review File; a 5 percent sample of the 2009 Truven Health MarketScan Commercial Claims and Encounters Database; 2009 Nationwide Emergency Department Sample (NEDS) database; 2009 Medicare Cost Reports; 2009 Medicaid enrollment by state from the Kaiser Family Foundation; and 2008 state-based Medicaid-to-Medicare fee ratios for outpatient care from Zuckerman et al., 2009 (Note 19 in text). Both 2023 projections were based upon the following sources: 2013 Congressional Budget Office projections of the effect of the Affordable Care Act (ACA); 2013 Kaiser Family Foundation estimates of the projected growth of the Medicare population; and the authors’ projections of growth in emergency department volume using National Hospital Ambulatory Medicare Care Survey data from 2000–10. NOTE Profit margin is defined as net revenue (revenue minus costs) divided by total revenue.
As mentioned, one of the limitations of our methods was our dependence upon regional average cost-to-charge ratios for our cost analysis of private, Medicaid, and uninsured ED visits. A supplemental analysis using Medicare claims demonstrates that our method of using weighted regional average cost-to-charge ratios overestimates ED costs by only 1.4 percent when compared to using hospital-specific ratios (see the online Appendix for details).27 Furthermore, we did not specifically account for possible reductions in reimbursement from private insurance companies in our ACA modeling.
Discussion
We estimate that hospital revenue from ED care exceeds costs for that care by $6.1 billion. However, this is primarily because hospitals make enough profit on the privately insured ($17 billion) to cover the losses from the other payer groups. Underpayment, defined as the amount of revenue below costs, is $2.8 billion for Medicare28 and $3.8 billion for Medicaid. If we assume that hospital reimbursement for the uninsured is similar to that for Medicaid patients, underpayment for this group of patients is $4 billion.
If private payers choose to reduce hospital reimbursement for ED services too close to costs, this could significantly reduce access to emergency care for everyone, without hospital subsidies from other revenue centers. More than 50 percent of overall hospital costs are labor costs.29 This is likely true in emergency medicine as well. It will be difficult to substantially reduce labor costs in emergency medicine without reducing the number of health care providers available in the ED at any given point in time—equivalently, a reduction in ED standby capacity. Given the financial burden hospitals are under, some hospitals would not be able to adequately subsidize the ED for the loss in revenue. So were this to occur, Medicare and Medicaid would need to consider payment increases for emergency care. At the very least, as lawmakers and policy makers consider ways to reduce Medicare and Medicaid expenditures, they should be careful not to decrease hospital payments for emergency care, because this could lead to ED closures and decreased access.
Demonstrating that EDs are profitable has important implications for health care’s transition to accountable care organizations (ACOs). ACOs encourage groups of providers to increase quality and reduce global costs for a defined group of patients. Within a hospital-based ACO, ED care could continue to be profitable, assuming that the EDs associated with the ACO have a payer mix approaching the national average. However, for ACOs with EDs characterized by a low percentage of privately insured patients, ED care will not likely be profitable unless those EDs are significantly more efficient than average. For these ACOs, meeting global cost reduction targets may result in limiting ED capacity and therefore ED access.
Conclusion
We find that implementation of the ACA will most likely result in increased profits for hospital-based EDs. This is not surprising given that the uninsured represent a sizable portion of all ED visits (18 percent) and are associated with the highest negative profit margins for hospitals, and that 25 percent of them will likely obtain private insurance through the exchanges. However, we assumed that the impact of the insurance exchanges on hospital revenue is neutral, which has yet to be seen.
Supplementary Material
Acknowledgments
Funding was provided by the National Institute on Aging.
Contributor Information
Michael Wilson, Email: mwilson18@partners.org, Instructor of medicine at Harvard Medical School and an associate physician in emergency medicine at Brigham and Women’s Hospital, both in Boston, Massachusetts.
David Cutler, Professor of economics at Harvard University and a research associate at the National Bureau of Economic Research, both in Cambridge, Massachusetts.
NOTES
- 1.Cutler DM, Sahni NR. If slow rate of health care spending growth persists, projections may be off by $770 billion. Health Aff (Millwood) 2013;32(5):841–50. doi: 10.1377/hlthaff.2012.0289. [DOI] [PubMed] [Google Scholar]
- 2.Healthcare Financial Management Association. Trends in emergency department capacities and costs [Internet] Westchester (IL): HFMA; 2008. [cited 2014 Mar 26]. Available from: http://www.hfma.org/Content.aspx?id=2308. [PubMed] [Google Scholar]
- 3.Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA. 2011;305(19):1978–85. doi: 10.1001/jama.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melnick GA, Nawathe AC, Bamezai A, Green L. Emergency department capacity and access in California, 1990–2001: an economic analysis. Health Aff (Millwood) 2004;23:w4–136. doi: 10.1377/hlthaff.w4.136. [DOI] [PubMed] [Google Scholar]
- 5.Simon EL, Griffin PL, Jouriles NJ. The impact of two freestanding emergency departments on a tertiary care center. J Emerg Med. 2012;43(6):1127–31. doi: 10.1016/j.jemermed.2012.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Zuckerman S, Williams AF, Stockley KE. Trends in Medicaid physician fees, 2003–2008. Health Aff (Millwood) 2009;28(3):w510–9. doi: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
- 7.Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA. 2011;305(19):1978–85. doi: 10.1001/jama.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Hospital-based emergency care at the breaking point. Washington (DC): National Academies Press; 2007. [Google Scholar]
- 9.Chen C, Scheffler G, Chandra A. Massachusetts’ health care reform and emergency department utilization. N Engl J Med. 2011;365(12):e25. doi: 10.1056/NEJMp1109273. [DOI] [PubMed] [Google Scholar]
- 10.Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid increases emergency-department use: evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263–8. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson M, Dobkin C, Gross T. The effect of health insurance coverage on the use of medical services. American Economic Journal: Economic Policy. 2012;4(1):1–27. [Google Scholar]
- 12.Healthcare Cost and Utilization Project. Nationwide Emergency Department Sample (NEDS) 2009 [home page on the Internet] Rockville (MD): Agency for Healthcare Research and Quality; 2009. [cited 2013 Jun 1]. Available from: http://hcupnet.ahrq.gov/HCUPnet.jsp. [Google Scholar]
- 13.Reinhardt UE. The pricing of US hospital services: chaos behind a veil of secrecy. Health Aff (Millwood) 2006;25(1):57–69. doi: 10.1377/hlthaff.25.1.57. [DOI] [PubMed] [Google Scholar]
- 14.Kane CK, Emmons DW. Policy research perspectives: new data on physician practice arrangements: private practice remains strong despite shifts toward hospital employment [Internet] Chicago (IL): American Medical Association; 2013. [cited 2014 Mar 20]. Available from: http://www.ama-assn.org/resources/doc/health-policy/prp-physician-practice-arrangements.pdf. [Google Scholar]
- 15.The Nationwide Emergency Department Sample (NEDS) is a nationally representative database of ED visits constructed using state inpatient and emergency department databases by the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality.
- 16.Medicare health maintenance organization (HMO) visits are reimbursed at a higher rate. However, these patients present with less severe medical conditions on average. We assume that hospital revenue from Medicare HMO patients was similar to revenue from fee-for-service Medicare visits.
- 17.We weighted to the national level because the Truven Health MarketScan Commercial Claims and Encounters Database we used does not have geographic identifiers. The database information is from 2009.
- 18.We weighted to the region level because the NEDS contains only regional identifiers. The weight is based on each state’s total number of Medicaid beneficiaries, as obtained from Kaiser Commission on Medicaid and the Uninsured.; Medicaid, a primer, 2013: key information on the nation’s health coverage program for low-income people [Internet] Washington (DC): Kaiser Family Foundation; 2013. Mar, Table 1: Medicaid enrollment by group, FY 2009 [cited 2014 Mar 28]. Available from: http://kaiserfamilyfoundation.files.wordpress.com/2010/06/7334-05.pdf. [Google Scholar]
- 19.Zuckerman S, Williams AF, Stockley KE. Trends in Medicaid physician fees, 2003–2008. Health Aff (Millwood) 2009;28(3):w510–9. doi: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
- 20.Hsia RY, MacIsaac D, Baker LC. Decreasing reimbursements for outpatient emergency department visits across payer groups from 1996 to 2004. Ann Emerg Med. 2008;51(3):265–74. doi: 10.1016/j.annemergmed.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 21.Ballard DW, Price M, Fung V, Brand R, Reed ME, Fireman B, et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010;48(1):58–63. doi: 10.1097/MLR.0b013e3181bd49ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2009 emergency department summary tables [Internet] Atlanta (GA): CDC; 2009. Table 7: triage status of emergency department visits, by selected patient characteristics: United States, 2009 [cited 2014 Mar 20]. Available from: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2009_ed_web_tables.pdf. [Google Scholar]
- 23.Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) for ICD-9-CM, 2006–2009 [Internet] Rockville (MD): Agency for Healthcare Research and Quality; 2013. Mar 8, [cited 2013 Jun 1]. Available from: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- 24.Schwartz M, Young DW, Siegrist R. The ratio of costs to charges: how good a basis for estimating costs? Inquiry. 1995–96;32(4):476–81. [PubMed] [Google Scholar]
- 25.We used 2000–10 data on visit rates per hundred people from the corresponding National Hospital Ambulatory Medical Care Surveys to estimate 2025 visit rates using simple linear regression.
- 26.Buchmueller T, Carey C, Levy HG. Will employers drop health insurance coverage because of the Affordable Care Act? Health Aff (Millwood) 2013;32(9):1522–30. doi: 10.1377/hlthaff.2013.0526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 28.Our finding of underpayment from Medicare is consistent with what is reported from the Medicare Payment Advisory Commission. Hospitals in 2010 had overall negative Medicare margins of −4.5 percent. We found ED margins to be more negative, at −13.5 percent.; Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy [Internet] Washington (DC): Med-PAC; 2013. Mar, [cited 2013 Aug 21]. Available from: http://www.medpac.gov/documents/Mar13_entirereport.pdf. [Google Scholar]
- 29.Roberts RR, Frutos PW, Ciavarella GG, Gussow LM, Mensah EK, Kampe LM, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999;281(7):644–9. doi: 10.1001/jama.281.7.644. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


