Abstract
Objectives
The objective was to measure the variation in missed diagnosis and costs of care for older acute myocardial infarction (AMI) patients presenting to emergency departments (EDs), and to identify the hospital and ED characteristics associated with this variation.
Methods
Using 2004–2005 Medicare inpatient and outpatient records, the authors identified a cohort of AMI patients age 65 years and older who presented to the ED for initial care. The primary outcome was missed diagnosis of AMI, i.e. AMI hospital admission within 7 days of an ED discharge for a condition suggestive of cardiac ischemia. Costs were defined as Medicare hospital payments for all services associated with and immediately resulting from the ED evaluation. The effect of ED and hospital characteristics on quality and costs were estimated using multilevel models with hospital random effects.
Results
There were 371,638 AMI patients age 65 and older included in the study, of whom 4,707 were discharged home from their initial ED visits and subsequently admitted to the hospital. The median unadjusted hospital-level missed diagnosis percentage was 0.52% (interquartile range [IQR] 0 to 3.45%). ED characteristics protective of adverse outcomes include higher ED chest pain acuity (adjusted odds ratio [aOR] 0.23, 99% confidence interval [CI] = 0.19 to 0.27), and American Board of Emergency Medicine certification (aOR 0.60, 99% CI = 0.50 to 0.73). Protective hospital characteristics include larger hospital size (aOR 0.46, 99% CI = 0.37 to 0.57), and academic status (aOR 0.74, 99% CI = 0.58 to 0.94). All of these characteristics were associated with higher costs as well.
Conclusions
The proportion of missed AMI diagnoses and cost of care for patients age 65 years and older presenting to EDs with AMI varies across hospitals. Hospitals with more board-certified emergency physicians and higher average acuity are associated with significantly higher quality. All hospital characteristics associated with better ED outcomes are associated with higher costs.
INTRODUCTION
Identifying the best providers of acute myocardial infarction (AMI) care is vital as we endeavor to improve the quality and lower the costs of medical care. AMI is associated with high mortality and costs, and provider-level payment reform is seen by many as the best hope for “bending the cost curve” while maintaining or improving quality.1,2 Correctly identifying AMI patients who present to the ED is essential to providing high quality care – over 60% of AMI admissions originate in the ED,3 and delays in therapy and missed diagnoses increase mortality.4–8 Despite improvements in some aspects of AMI care, like decreased door-to-balloon times, the percentage of AMI patients inappropriately discharged from the ED (2% to 4%) has remained relatively stable over the last decade.4,5,7 Patients age 65 years and older represent 82% of in-hospital deaths following ED admission for AMI.9 While variations in spending and quality for patients age 65 years and older have been extensively documented, little is known about the ED and hospital factors associated with either the quality of this initial evaluation or resulting costs.10
We sought to measure the cross-sectional variation in missed diagnosis and resulting costs for Medicare patients age 65 years and older who presented to EDs nationwide with AMI, and to identify the hospital and ED characteristics associated with this variation.
We considered several ED factors (board certification, years of clinical experience, chest pain patient volume) and hospital factors (cardiac specialization, academic status, hospital size, amount of technology available) as predictors of quality and cost.
METHODS
Study Design
This was an observational study using Medicare fee-for-service records from the 100% sample Inpatient and Outpatient Standard Analytic files (SAF) from January 1, 2004 to December 31, 2005. Institutional review board approval was obtained for this study.
Study Setting and Population
We used Medicare claims data to identify a cohort of patients age 65 years and older with AMI who presented to EDs for initial care, regardless of whether or not they were identified as having AMI while in the ED. We included patients who were admitted to the hospital, discharged to home or a skilled nursing facility, or transferred to another facility for further care.
Acute myocardial infarction patients who were directly admitted to the hospital from the ED were identified using Inpatient SAF records where AMI was the primary hospital discharge diagnosis (International Classification of Diseases, 9th revision, clinical modification [ICD-9-CM] 410.xx) and the Emergency Room Charge Amount field was greater than $0. This method of identifying AMI patients using Medicare data has been shown to be accurate when compared to medical chart review.11,12
Study Protocol
To capture AMI patients who were discharged home from the ED, we first developed a list of diagnoses suggestive of cardiac ischemia (see Data Supplement 1) by reviewing the relevant literature5, 7 and coming to a consensus among three emergency physicians (EPs) (MW, JW, JS). These patients had diagnoses such as chest pain, shortness of breath, and gastritis and we collectively term them patients with chest pain. We then included only ED patients with ‘chest pain’ who were discharged to home or to a skilled nursing facility, and within 7 days were admitted to a hospital with AMI listed as the primary hospital discharge diagnosis. ED visits were identified in the outpatient SAF using revenue center codes 0450–0459.
Patients with AMI who were transferred after their initial visits were identified using records from the transferring and receiving facilities. Patients were considered to have been transferred if either record indicated a transfer had occurred, the receiving facility was a short-stay hospital, and the dates of service for the two visits were within 1 day of each other. AMI patients were identified among the ED transfers using the methods described above. Patients who were transferred to federal hospitals could not be captured using Medicare claims data.
Hospice patients (defined as having received hospice care within the previous 6 months) and patients who left the ED against medical advice were excluded, as were patients who died in the ED during the initial visit prior to being admitted to the hospital.
Our indicator of missed AMI diagnosis is ED discharge home with a condition suggestive of cardiac ischemia with subsequent hospital admission within 7 days with AMI. Patients with AMI who were directly admitted to the hospital from the presenting ED or transferred to another hospital for further care were considered to have been accurately diagnosed with AMI.
Costs were defined as Medicare payments for hospital services associated with and resulting from the ED evaluation. For patients who were discharged home after the initial ED visit, this included only ED costs. For patients who were admitted to the hospital after the initial ED visit, this included ED and inpatient costs. Thus, our cost variable captures all resources used in the treatment of the acute presentation. Costs, which are skewed, were log transformed prior to inclusion in the regression models, as is standard practice.13
Variation in hospital labor costs comprises a significant portion of variation in Medicare payments not associated with variations in resource use for patient care. To control for this, we performed separate regressions with total hospital costs deflated by the hospital’s local labor market costs using wage index data from the Centers for Medicare and Medicaid Services.
Hospital and ED-Level Predictors
We created several ED-focused and hospital-level variables from the American Medical Association Physician Masterfile, 2005 American Hospital Association Annual Survey, and American College of Emergency Physicians web site to determine their importance as predictors of high-value care. One category of variables measures the staffing and operation of the ED, including categorical variables reflecting the ED’s average chest pain acuity (percentage of all chest pain patients diagnosed with AMI within 1 week of ED visit, divided into high [>1.5%] and low [<1.5%] groups), volume of chest pain patients seen, and being an emergency medicine (EM) residency core site. In addition, from the AMA we obtained information on 42,000 physicians who provided care for ‘chest pain’ patients in the ED on a regular basis during the study period (using Medicare outpatient data). We then created variables reflecting the percentage of EPs who were American Board of Emergency Medicine (ABEM) certified, U.S. trained, or male, as well as the average years in practice for each EP group.
In addition, we created several variables characterizing the hospital as a whole. These include presence of an interventional cardiac catheterization lab, dedicated cardiac intensive care unit (ICU), academic status (non-academic, academic with medical school affiliation, or academic with medical school affiliation and residency programs), size (small, medium, or large; based on the Healthcare Cost and Utilization Project definitions that consider number of beds, location, and teaching status), urbanization14 (metropolitan, micropolitan, small town, and rural, defined using hospital zip codes), ownership type (non-profit, private, or public), and region of country. We also assessed the hospitals’ overall technology level using a Saidin index (a summary index weighted by the percent of hospitals without that technology) focusing on a broad array of technologies that are present in less than 50% of hospitals nationally.15,16
Patient Level Predictors
We categorized patients’ comorbid medical conditions (derived from the index visit and prior 12 months of inpatient and outpatient records) into 29 categories using Elixhauser et al.’s risk adjustment method.17 Other patient variables included age and sex (5-year age groups, sex-specific), race, and socioeconomic status (median family income based on race-specific averages in patients’ residential zip codes using 2000 U.S. Census data). We also controlled for day of week and season (four 3-month periods).
Creation of Analysis File
Our initial analytic file contained 432,771 observations. Patients admitted to the hospital and discharged home alive in less than 2 days (1.44%) were not likely to have sustained AMI and were excluded.11,12,18 Patients with a prior AMI diagnosis within 6 months (3.99%), or inpatient discharge within 7 days preceding the index ED visit (0.85%), were excluded so as to identify a homogeneous group of patients with similar expected hospital costs. Observations indicating that a patient was discharged home from the initial ED visit with a diagnosis of AMI (0.32%), admitted to a hospital with an unusually large (greater than three standard deviations [SD] from the mean) number of ‘chest pain’ patients (0.38%), or charged an amount that was negative, zero, missing (1.55%), or too large to be consistent with ED care (0.07%), were not considered reliable and were also excluded.
Data Analysis
We initially report unadjusted median AMI missed diagnosis percentages with interquartile ranges (IQR) and median costs at the hospital level. To account for the nested structure of the data (patients within hospitals) while simultaneously examining the effect of both patient- and hospital-level predictors on the outcome variable distribution, we report results of our random intercept log-linear and logistic models.19 Continuous variables were rescaled to z-statistics. We used single imputation with dummy variables for missing predictor values. In our sensitivity analyses, missingness was modeled using multiple imputation and complete case analysis, and same-day readmissions were excluded. The exclusion of same-day readmissions was designed to evaluate for possible misclassification bias. All statistical analyses used STATA 11. For our large analytic dataset, results were considered statistically significant at the p < 0.01 level to minimize the detection of statistically significant but clinically irrelevant findings.20 This Type I error rate was not adjusted for multiple comparisons.
RESULTS
The final dataset included 371,638 Medicare patients with AMI who presented to EDs for initial care; demographics are available in Table 1. These patients were seen at 4,576 hospital-based EDs across the United States, the largest share being community (56%), not-for-profit (48%), and urban (42%); few had interventional cardiac catheterization capability (22%) (see Table 2).
Table 1.
Characteristics of Patients in the Analytic Dataset (n=371,638)
| Characteristic | n (%) |
|---|---|
| Demographics (# missing values) | |
| Age – median years (0) | 80 (73–86) |
| Sex (878) | |
| Female | 193,988 (52) |
| Race‡(0) | |
| White | 326,129 (88) |
| African American | 29,292 (8) |
| Hispanic | 7,685 (2) |
| Others | 8,533 (2) |
| Median income – yearly (0) | $39,831 ($33,325–$51,918) |
| Comorbid conditions* (0) | |
| Hypertension | 240,729 (65) |
| Congestive heart failure | 187,109 (50) |
| Diabetes, uncomplicated | 112,862 (30) |
| Chronic pulmonary disease | 109,121 (29) |
| Valvular disease | 86,037 (23) |
| Peripheral vascular disease | 54,289 (15) |
| Renal failure | 51,554 (14) |
| Solid cancer, no metastases | 45,067 (12) |
| Diabetes, complicated | 31,949 (9) |
| Obesity | 18,209 (5) |
| Pulmonary hypertension | 13,959 (4) |
| Peptic ulcer disease | 9,492 (3) |
| Metastatic cancer | 1,898 (1) |
Medians are reported with interquartile ranges
Federal race/ethnicity categories (social-political constructs)
Comorbid condition categories defined using Elixhauser et al.'s risk adjustment method using prior 12 months inpatient and outpatient records. No missing values by construction.
Table 2.
Pooled Estimates by Hospital Characteristics (n=4,576)
| Characteristic | Median AMI Revisit Rate (IQR) |
Median Cost (IQR) |
|---|---|---|
| EM boarded bottom quartile (n=1,134) | 1.99 (0–33.33) | $2,907 ($841–$6,179) |
| EM boarded 3rd quartile (n=1,494) | 0.81 (0–4.76) | $6,086 ($2,948–$7,754) |
| EM boarded 2nd quartile (n=774) | 0.44 (0–1.54) | $7,388 ($4,650–$10,473) |
| EM boarded top quartile (n=1,134) | 0.30 (0–1.15) | $8,247 ($6,209–$13,498) |
| Missing EM board certification (n=40) | 0 (0–100) | $4,222 ($1,418–$8,154) |
| Low chest pain acuity (n=1,794) | 3.39 (0–31.25) | $3,225 ($891–$6,685) |
| High chest pain acuity (n=2,742) | 0.39 (0–1.37) | $7,417 ($4,779–$11,069) |
| Missing chest pain acuity (n=40) | 0 (0–100) | $4,222 ($1,418–$8,154) |
| No cath lab (n=1,962) | 1.32 (0–11.11) | $4,242 ($1,497–$7,047) |
| Cath lab hospitals (n=1,019) | 0.46 (0–1.08) | $8,782 ($6,881–$14,817) |
| Missing cath lab status (n=1,595) | 0 (0–3.13) | $6,515 ($3,287–$8,843) |
| Technology score 1 (n=1,916) | 0.0 (0–11.11) | $4,642 ($1,735–$7,407) |
| Technology score 2 (n=387) | 1.37 (0–16.67) | $3,992 ($1,276–$6,864) |
| Technology score 3 (n=900) | 0.68 (0–2.76) | $6,708 ($3,405–$8,599) |
| Technology score 4 (n=669) | 0.55 (0–1.63) | $7,127 ($4,466–$8,727) |
| Technology score 5 (n=704) | 0.45 (0–1.08) | $9,181 ($6,966–$15,110) |
| Missing technology score (n=0) | - | - |
| Small hospitals (n=1,115) | 1.61 (0–33.33) | $3,469 ($944–$7,162) |
| Medium hospitals (n=867) | 0.43 (0–2.37) | $6,816 ($3,858–$8,715) |
| Large hospitals (n=1,431) | 0.59 (0–1.83) | $7,003 ($4,327–$9,693) |
| Missing hospital size (n=1,163) | 0 (0–2.87) | $6,515 ($3,591–$9,135) |
| Community hospitals (n=2,584) | 0.85 (0–6.67) | $4,886 ($2,116–$7,469) |
| Academic hospitals (n=880) | 0.49 (0–1.32) | $8,470 ($6,029–$14,067) |
| Missing academic status (n=1,112) | 0 (0–2.80) | $6,658 ($3,671–$9,306) |
| Rural area (n=269) | 5.55 (0–50.00) | $1,794 ($725–$4,915) |
| Small town (n=667) | 4.00 (0–29.17) | $2,920 ($828–$6,346) |
| Micropolitan (n=699) | 1.10 (0–3.57) | $6,413 ($3,365–$7,501) |
| Urban (n=1,936) | 0.39 (0–1.24) | $8,053 ($5,927–$12,779) |
| Missing urban status (n=1,005) | 0 (0–10) | $4,584 ($2,062–$7,056) |
| Public (n=764) | 1.69 (0–25.00) | $3,773 ($1,028–$7,095) |
| Private, for profit (n=519) | 0.47 (0–2.77) | $6,704 ($3,781–$8,401) |
| Private, nonprofit (n=2,181) | 0.62 (0–2.33) | $6,725 ($3,365–$8,782) |
| Missing ownership status (n=1,112) | 0 (0–2.80) | $6,658 ($3,671–$9,306) |
| All hospitals (n=1,112) | 0.52 (0–3.45) | $6,474 ($3,040–$8,532) |
AMI death after ED discharge rate = frequency (expressed as a percentage) of deaths after ED discharge for chest pain
AMI revisit rate = frequency (expressed as a percentage) of AMI patient admissions within 7 days of ED discharge for chest pain
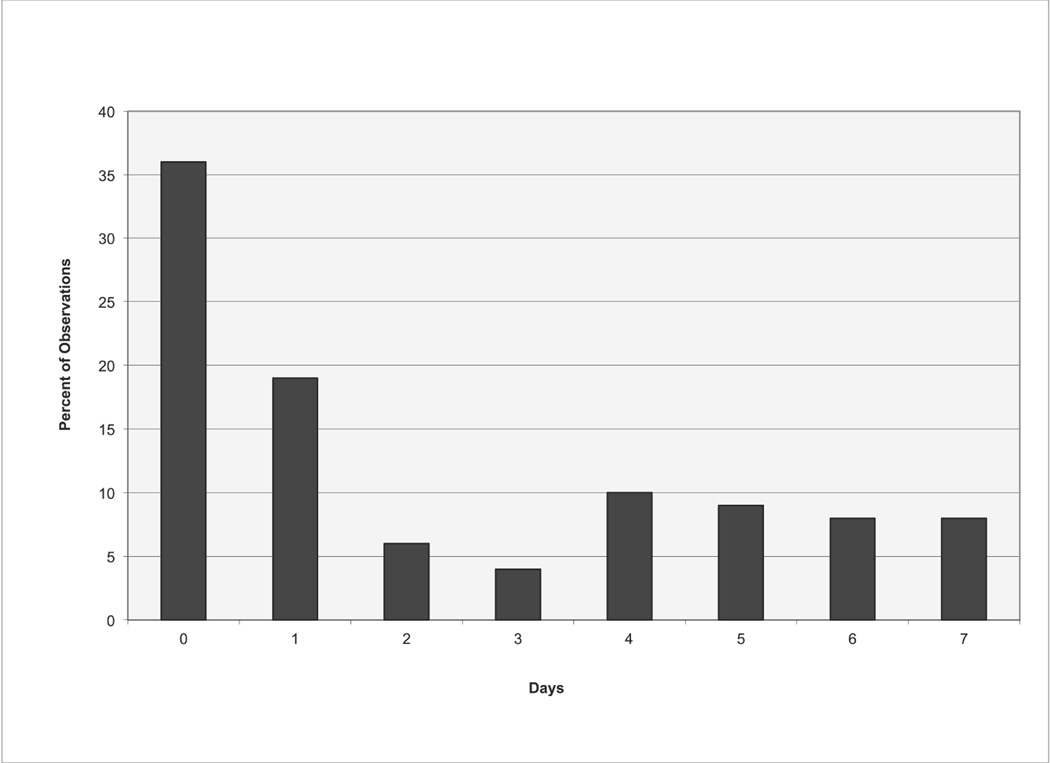
There were 4,774 AMI hospital admissions within 7 days of ED discharge, for a missed diagnosis percentage of 1.2%. Similar to the ‘death after ED discharge’ group, the majority (65%) of these admissions occurred within 3 days of the initial ED visits (see Figure 1). The median unadjusted hospital-level missed diagnosis percentage was 0.52% (IQR 0 to 3.45%).
Figure 1.
The unadjusted missed diagnosis percentage was less than 1% for most hospital subgroups, but the upper range varied significantly. For example, the missed diagnosis percentage IQR for hospitals in the top quartile for EM board certification was 0 to 1.15, compared to 0 to 33.33 for hospitals in the bottom quartile. This pattern was still evident when restricting the analysis to hospitals with at least 30 AMI patients during the study period. The variability around the median was similarly wide for hospitals without catheterization capabilities, lowest technology scores, small hospitals, rural, and public hospitals. The median missed diagnosis percentage was 2% or higher for hospitals with low chest pain acuity, in non-urban locations, and in the bottom quartile for ABEM physician certification.
The median cost of treatment of the acute presentation for all hospitals was $6,474 (IQR $3,040 to $8,532). Costs were at least twice as high for hospitals in the in urban areas, the top quartile for ABEM certification, with high average acuity, and with interventional cardiac catheterization capabilities. when compared to their counterparts. The largest absolute cost difference was seen between urban and rural hospitals.
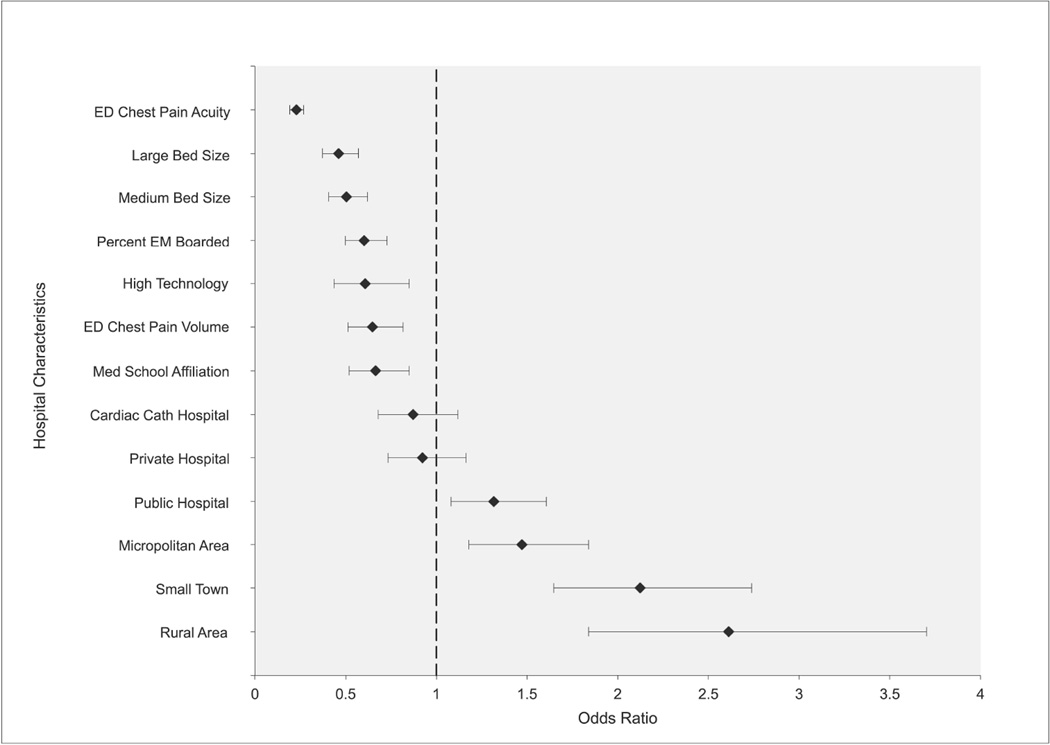
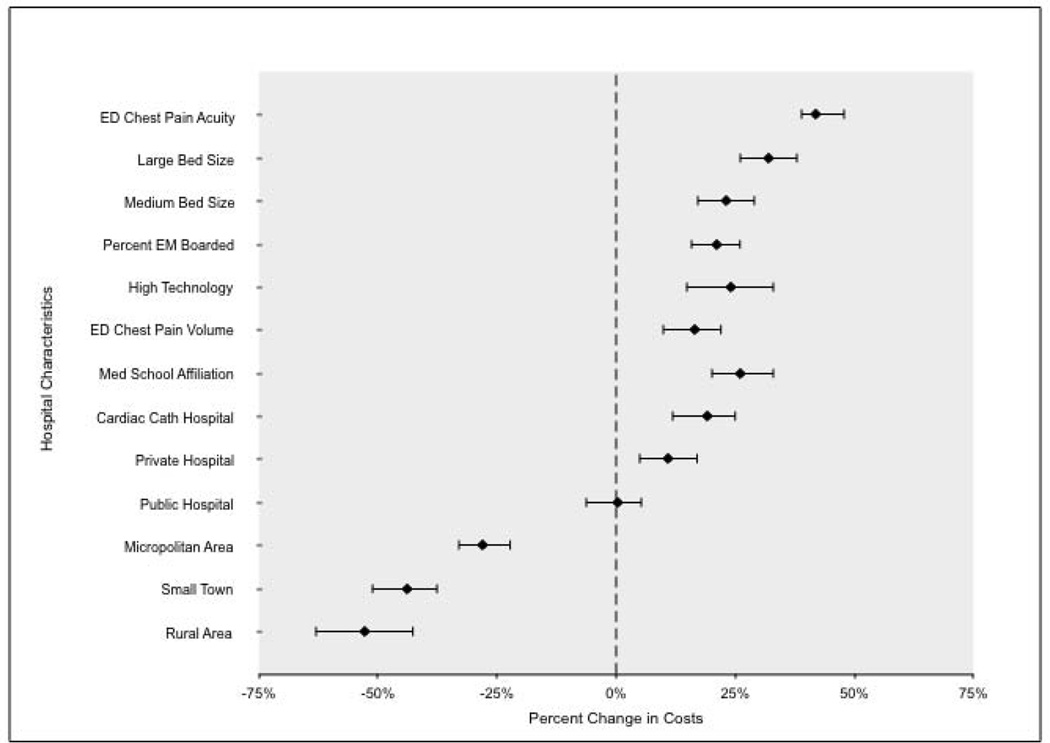
Figure 2 shows the adjusted odds ratios (aOR) for each of our explanatory factors in predicting poor quality AMI care, as defined in our study, as well as spending; the full set of coefficients is reported in Data Supplement 2. Among the ED-specific variables, we found significant effects for ABEM certification and average chest pain acuity.
Figure 2.
The most protective hospital characteristic was having an above-minimum level of ‘chest pain’ patient acuity, measured as hospitals where greater than 1.5% of all chest pain patients had an AMI. Patients seen at hospitals above this threshold were significantly less likely (aOR 0.23, 99% CI = 0.19 to 0.27) to have been misdiagnosed and discharged home after their initial ED visits. No additional benefit accrued for hospitals above this minimal acuity threshold. ABEM certification (aOR 0.60, 99% CI = 0.50 to 0.73), ED chest pain patient volume (aOR 0.65, 99% CI = 0.51 to 0.82), large hospital bed size (aOR 0.46, 99% CI = 0.37 to 0.57), and academic status (aOR 0.74, 99% CI = 0.58 to 0.94), were similarly protective. Several hospital characteristics (i.e., interventional cardiac catheterization capability, cardiac ICU, and EM residency training programs) were not independently protective. Patients at rural (AOR 2.61, 99% CI = 1.84 to 3.70) or public (AOR 1.33, 99% CI = 1.08 to 1.61) hospitals received lower quality of care using this indicator.
When we excluded same-day readmissions from our analysis, high ED chest pain acuity (aOR 0.35, 99% CI = 0.30 to 0.42), ABEM physician certification (aOR 0.74, 99% CI = 0.62 to 0.88), large hospital bed size (aOR 0.59, 99% CI = 0.48 to 0.73), and academic status (aOR 0.77, 99% CI = 0.61 to 0.96) were still protective. ED chest pain volume was no longer protective (aOR 0.84, 99% CI = 0.66 to 1.05). Patients at rural (aOR 1.49, 99% CI = 1.02 to 2.18) or public (aOR 1.25, 99% CI = 1.03 to 1.52) hospitals still received lower quality of care (see Data Supplement 3).
Hospitals with lower missed AMI diagnosis percentages were more costly. Patients seen at hospitals with high average ED chest pain acuity received 43% (99% CI = 36% to 48%) more costly care. Similar patterns appeared for large (32%, 99% CI = 26% to 38%) and academic (26%, 99% CI = 20% to 33%) hospitals, as well as hospital with the most technology (24%, 99% CI = 15% to 33%), and ABEM certified physicians (21%, 99% CI = 16% to 26%). Private for-profit hospitals and those with interventional cardiac catheterization capabilities were more expensive but were not associated with better quality care. Rural hospitals had lower costs but lower quality of care as well. This same cost pattern was evident when same-day readmissions and same-day deaths after ED discharge were excluded from the analysis (see Data Supplement 3).
Local labor market costs explained most of the higher costs associated with more ABEM certified physicians (62%) and high-volume EDs (58%), and some of the higher costs associated with the largest hospitals (49%), hospitals with high average chest pain acuity (37%), high technology index scores (3% to 19%), and private hospitals (23%) (see Data Supplement 2). They also explained most of the lower costs associated with small town (56%) and rural hospitals (70%). Still, these factors predicted spending even adjusted for input costs. All of our regression results were robust to the sensitivity analyses (see Data Supplements 4 and 5).
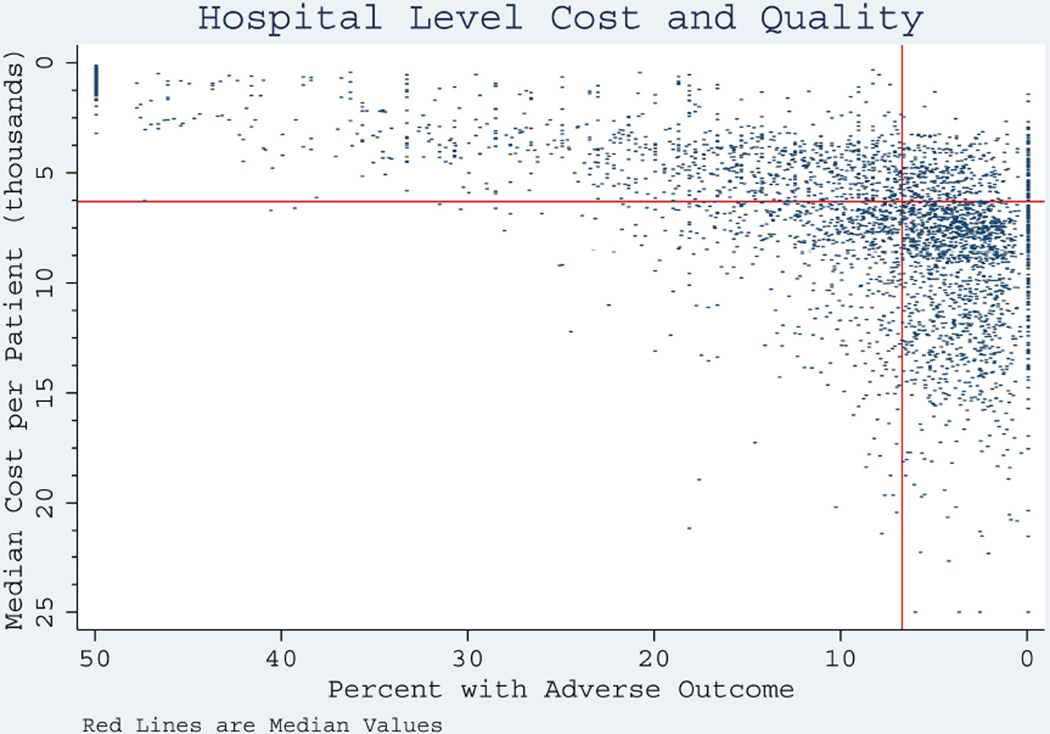
Finally, we placed hospitals in quadrants based upon cost and missed AMI diagnosis percentage, and 78% fell into either the high-quality/high-cost quadrant or the low-quality/low-cost quadrant (Figure 3). Eleven percent of hospitals had above median outcomes and below median costs.
Figure 3.
DISCUSSION
While many studies focus on the quality of inpatient care for AMI patients,4–8 this is the first national study to examine the reasons for hospital variation in missed AMI diagnosis in the ED. Pope et al. reported 19 missed AMI diagnoses resulting in hospital discharge out of a total of 889 patients for a missed diagnosis percentage of 2.1%. Previous studies have reported missed AMI diagnosis percentages of between 2% and 6%. None of the prior studies were large enough to study variation in missed AMI diagnosis by hospital.
We found two characteristics of the ED that are associated with better outcomes. EDs where more than 1.5% of all chest pain patients have AMI were associated with the largest odds reductions for missed AMI. Before policy makers consider triaging patients away from low-acuity centers when possible, which would be difficult for the 41% of low-acuity centers in our study that are in rural areas or small towns, we need more research to establish a causal link between ED average acuity and outcomes.
The second characteristic is ABEM certification. This is the first study to examine its effect on quality and found that ABEM certification is associated with significantly lower odds of a patient being discharged home when they present to an ED with AMI. However, from 2004–2005, only 54% of ED patients age 65 years and older with chest pain were seen by ABEM-certified physicians. Policies to increase the number of ABEM-certified physicians could increase quality of care for patients aged 65 years and older with AMI.
In contrast, hospitals with interventional cardiac catheterization capabilities and coronary care units had higher costs per AMI presentation, but no improvement in the odds of missed AMI diagnosis. Thus, quality in the ED is not synonymous with high technological capacity overall.
Finally, studies exploring the link between hospital costs and quality care have found conflicting results.21,22 We find that all characteristics associated with lower odds of missed AMI diagnosis – ABEM certification, chest pain acuity, hospital bed size, and academic status – were associated with higher costs as well. For example, the odds of admission within 1 week of ED discharge are 0.23 for hospitals with high average acuity. These hospitals also have 43% higher costs.
LIMITATIONS
This study relies on an administrative dataset that has limited clinical information. These studies are generally hypothesis-generating as opposed to hypothesis-testing. Using this dataset, we identified a complete cohort of patients who presented to EDs with AMI, including those who were not initially diagnosed with an AMI. We included only patients with a primary discharge diagnosis of AMI because this method has a 95% positive predictive value in identifying AMI patients when compared to clinical records.8 Nevertheless, a study using both clinical records and death records, particularly for those who were discharged home, could validate our overall results and establish the most appropriate way of identifying the entire cohort of patients presenting to an ED with AMI using administrative records. Furthermore, we used a narrow list of ICD-9 ED discharge diagnoses for conditions suggestive of cardiac ischemia, so that any hospital-level variation observed in the study would reflect true differences between hospitals as opposed to statistical noise resulting from the limited precision with which we measured this outcome. The cost of this choice is that we underestimate the true incidence of missed AMI. Our unadjusted missed AMI estimate, using the hospital readmission definition, was 1.2%, as compared to 2% to 6% reported in the literature.4–6
Our analysis focused on costs from a payer perspective, i.e. Medicare. While this perspective has obvious policy relevance, the conclusions of this study might have been different if we had examined costs from a hospital or patient perspective. Further study, using a micro-costing method, would provide a more complete picture of the effect of patient and provider characteristics on costs.
This analysis relies on Medicare data from 2004–2005, prior to enactment of Affordable Care Act and associated Medicare payment reform. These results can serve as a baseline for future studies that evaluate the effect of health reform on quality and costs in EM.
We focus on the effect of ABEM certification in this analysis. The effect of American Osteopathic Board of Emergency Medicine certification was not examined and represents a further limitation of this study.
We used a conventional imputation method, single imputation with dummy variables for missing predictor variables, which can lead to biased results. However, our results were robust to sensitivity analyses that included multiple imputation and complete case analysis.
Finally, our assumption is that hospitals with lower odds of missed AMI diagnosis were providing higher quality of care and not simply practicing more conservative care by admitting a higher proportion of chest pain patients seen. This assumption could not be tested with our analytic dataset and warrants further investigation.
CONCLUSIONS
The odds of missed acute myocardial infarction diagnosis and resulting cost of care for patients age 65 years and older presenting to EDs with acute myocardial infarction varies across hospitals and is related to the capabilities and staffing of the ED, including American Board of Emergency Medicine certification. As more attention is placed on health care value, policy makers should recognize that increasing the quality of ED care might be associated with increased costs as well.
Supplementary Material
Acknowledgments
This project was supported by grants from the National Institute on Aging (P01AG031098), and Brigham and Women’s Hospital.
Footnotes
Disclosures: The authors have no relevant financial information or potential conflicts of interest to disclose.
References
- 1.Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Aff (Millwood) 2007;26:38–48. doi: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- 2.McClellan M. Reforming payments to healthcare providers: the key to slowing healthcare cost growth while improving quality? J Economic Perspectives. 2011;25:69–92. doi: 10.1257/jep.25.2.69. [DOI] [PubMed] [Google Scholar]
- 3.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;367:391–393. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 4.Lee TH, Rouan GW, Weisberg MC, et al. Clinical characteristics and natural history of patients with acute myocardial infarction sent home from the emergency room. Am J Cardiol. 1987;60:219–224. doi: 10.1016/0002-9149(87)90217-7. [DOI] [PubMed] [Google Scholar]
- 5.Pope JH, Aufderheide TP, Ruthazer R, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med. 2000;342:1163–1170. doi: 10.1056/NEJM200004203421603. [DOI] [PubMed] [Google Scholar]
- 6.Schor S, Behar S, Modan B, Barell V, Drory J, Kariv I. Disposition of presumed coronary patients from an emergency room. A follow-up study. JAMA. 1976;236:941–943. [PubMed] [Google Scholar]
- 7.McCarthy BD, Beshansky JR, D'Agostino RB, Selker HP. Missed diagnoses of acute myocardial infarction in the emergency department: results from a multicenter study. Ann Emerg Med. 1993;22:579–582. doi: 10.1016/s0196-0644(05)81945-6. [DOI] [PubMed] [Google Scholar]
- 8.Masoudi FA, Magid DJ, Vinson DR, et al. Implications of the failure to identify high-risk electrocardiogram findings for the quality of care of patients with acute myocardial infarction: results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study. Circulation. 2006;114:1565–1571. doi: 10.1161/CIRCULATIONAHA.106.623652. [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) Nationwide Emergency Department Sample (NEDS) [Accessed Jul 25, 2014]; Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=A013AF252A0D96E5&Form=MAINSEL&JS=Y&Action=%3E%3ENext%3E%3E&_MAINSEL=NEDS%20Statistics.
- 10.MaCurdy T, Bhattacharya J, Perlroth D, et al. Geographic Variation in Spending, Utilization and Quality: Medicare and Medicaid Beneficiaries. [Accessed Jul 24, 2014]; Available at: http://iomedu/Reports/2013/Variation-in-Health-Care-Spending-Target-Decision-Making-Not-Geography/~/media/Files/Report%20Files/2013/Geographic-Variation2/Subcontractor-Reports/Updated%20Acumen%20Reportpdf. [Google Scholar]
- 11.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148:99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Petersen LA, Wright S, Normand SL, Daley J. Positive predictive value of the diagnosis of acute myocardial infarction in an administrative database. J Gen Intern Med. 1999;14:555–558. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weintraub WS. Cardiovascular health care economics. Totowa, NJ: Humana Press; 2003. [Google Scholar]
- 14.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006;83:162–175. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spetz J, Maiuro LS. Measuring levels of technology in hospitals. Quart Rev Economics Finance. 2004;44:430–447. [Google Scholar]
- 16.Silvio D, Laurence CB. Did the Butler Really Do It? [Accessed Jul 18, 2014];Examining the Impact of Technology on Hospital Cost Growth. Available at: http://dx.doi.org/10.2139/ssrn.1905429. [Google Scholar]
- 17.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 19.Rabe-Hesketh S, Skrondal A. Linear Random-Intercept Models. In: Rabe-Hesketh S, Skrondal A, editors. Multilevel and longitudinal modeling using stata. College Station, TX: Stata Press Publication; 2008. pp. 91–97. [Google Scholar]
- 20.Noymer A. Alpha, significance level of test. In: Lavrakas PJ, editor. Encyclopedia of survey research methods. Thousand Oaks, CA: Sage Publications; 2008. [Google Scholar]
- 21.Schreyogg J, Stargardt T. The trade-off between costs and outcomes: the case of acute myocardial infarction. Health Serv Res. 2010;45:1585–1601. doi: 10.1111/j.1475-6773.2010.01161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med. 2010;170:340–346. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.