Abstract
The present quasi-experiment examined the direct and indirect effects of recovery support telephone calls following adolescent substance use disorder treatment. Six-month outcome data from 202 adolescents who had received recovery support calls from primarily pre-professional (i.e., college-level social service students) volunteers was compared to 6-month outcome data from a matched comparison sample of adolescents (n = 404). Results suggested adolescents in the recovery support sample had significantly greater reductions in their recovery environment risk relative to the comparison sample (β = -.17). Path analysis also suggested that the reduction in recovery environment risk produced by recovery support calls had indirect impacts (via recovery environment risk) on reductions in social risk (β = .22), substance use (β = .23), and substance-related problems (β = .16). Finally, moderation analyses suggested the effects of recovery support calls did not differ by gender, but were significantly greater for adolescents with lower levels of treatment readiness. In addition to providing rare empirical support for the effectiveness of recovery support services, an important contribution of this study is that it provides evidence that recovery support services do not necessarily have to be “peer-based,” at least in terms of the recovery support service provider having the experiential credentials of being “in recovery.” If replicated, this latter finding may have particularly important implications for helping increase the recovery support workforce.
Keywords: Adolescent, Recovery support, Substance use, Volunteers
Introduction
Although research has identified effective interventions for the treatment of adolescent substance use disorders and related problems [1-4], research also has shown relapse and continued substance use are common following discharge from treatment [5-7]. These findings combined with longer-term findings with adults [8-10] have prompted increasing recognition that substance use disorders can be a chronic condition requiring long-term treatment and support similar to other chronic conditions such as mental illness, hypertension, diabetes, and congestive heart failure [11-15]. One approach to the long-term care of substance use problems that has received considerable research attention is known as continuing care (historically referred to as “aftercare”). Although reviews of the continuing care research have revealed mixed support for the effectiveness of continuing care [16-18], a recent meta-analytic review of continuing care for substance use disorders found that continuing care had a significant positive effect at both the end of the continuing care interventions (g = .19) and at follow-up (g = .27) [18].
Despite demonstrated support for the effectiveness of continuing care approaches, broader dissemination and implementation of evidence-based continuing care services within practice settings remains limited [19,20]. While additional research to more fully understand the barriers to greater implementation of evidence-based continuing care services within real-world settings is clearly needed, cost and accessibility have been two common concerns. To decrease associated costs (e.g., travel to client homes) and increase accessibility of continuing care services, research has increasingly focused on the potential effectiveness of providing continuing care services via the telephone [21-31]. Similar to the general continuing care literature, research support for the effectiveness of telephone-based continuing care appears to be equivocal [21-23,25-28,30,31]. Thus, further research is needed to better understand factors associated with effective telephone-based continuing care.
Another approach to the long-term care of substance use disorders is “recovery support.” In contrast to professionally delivered continuing care approaches, recovery support has been defined as “the process of giving and receiving non-professional, non-clinical assistance to achieve long-term recovery from severe alcohol and/or other drug-related problems” [32]. Recovery support via participation in secular, spiritual, or religious recovery mutual-aid societies (e.g, SMART Recovery, Alcoholics Anonymous (AA), Narcotics Anonymous (NA), Celebrate Recovery) or other recovery community institutions (e.g., recovery community centers, recovery social clubs, recovery homes, recovery schools) has a long and rich history [32]. Of particular import for those serving substance-involved adolescents is the growth of support structures specifically for youth (e.g., young people's AA and NA meetings, Teen Addiction Anonymous) and youth-led or youth-focused recovery advocacy organizations (e.g., Young People in Recovery, Transforming Youth Recovery).
Consistent with the increasing frequency of continuing care delivered via the telephone, there also has been increasing use of the telephone to deliver recovery support services. For example, as described by Valentine [33], in 2009, the Connecticut Community for Addiction Recovery (CCAR) made 36,865 outbound support calls to 1,420 recovering individuals. Particularly noteworthy is that although the equivalent of approximately $380,000 in services were provided, the actual cost to CCAR was limited primarily to costs associated with paid staff time spent recruiting, training, coordinating, and supervising volunteers. Given the minimal costs associated with providing recovery support by volunteers, this appears to be a promising approach. To date, however, examinations of the effectiveness of recovery support services via experimental tests have been limited and focused on recovery support services for adults [32,34-36].
Recovery support delivered by the groups and organizations noted above (e.g., recovery mutual aid groups, recovery social clubs, recovery homes, recovery schools) are commonly provided by other individuals who are “in recovery.” As such, these types of recovery support services are often more specifically referred to as “peer-based recovery support” [32]. Although research has found service provider recovery status to have a significant positive relationship with client perceptions of credibility [37], therapeutic relationship [38], and treatment satisfaction [39], research has not generally supported service provider recovery status as being significantly associated with client substance use outcomes [40-43]. These latter findings, combined with other research supporting the use of non-professionals to address substance use disorders [44-46], has raised questions about the extent to which recovery support services could be provided effectively by non-professional individuals who do not identify as being “in recovery.”
In order to help address this important question, the current paper conducted a quasi-experimental examination of the direct and indirect effects of recovery support telephone calls following adolescent substance use disorder treatment, as delivered by mostly pre-professional (i.e., college-level social service students) volunteers, the majority [75%] of whom did not identify themselves as being in recovery. We hypothesized that relative to a matched comparison sample, adolescents receiving the recovery support telephone calls would report greater post-treatment reductions in recovery environment risk, social risk, substance use, and substance-related problems. Additionally, based on prior research [47,48], we hypothesized that the impact of the recovery support telephone calls on substance use and substance-related problems would be mediated by reductions in recovery environment risk and social risk (see Figure 1). Finally, based on research that has found gender [27,49-51] and readiness to change [27,51] to be important moderators of continuing care interventions, we hypothesized that the effects of the recovery support telephone calls would be significantly greater for females and for individuals reporting lower levels of treatment readiness.
Figure 1.

Hypothesixed Model.
Methods
Study context
In 2009, the Substance Abuse and Mental Health Services Administration's Center for Substance Abuse Treatment (SAMHSA/CSAT) funded an innovative project called Recovery Support for Adolescents and Families (RSAF). The primary goal of this project was to provide recovery support services to adolescents and their families following episodes of outpatient or residential substance use disorder treatment. The project included four adolescent substance use disorder treatment providers located in Bloomington, IL, Fitchburg, MA, Seattle, WA, and Tucson, AZ.
Participants
Two hundred and two adolescents (94% of the 215 eligible adolescents) were recruited to participate in the project. In order to be eligible for the project, adolescents must have: a) been 13-18 years of age at the time of recruitment, b) met DSM-IV-TR diagnostic criteria for substance abuse or dependence, c) been enrolled and remained in either outpatient treatment for at least 4 sessions within 44 days from the intake session or in residential treatment for at least 2 weeks, d) resided in one of the four respective RSAF project catchment areas, and e) had telephone access either at their home or another location. Additionally, adolescents were excluded from the project if they met any of the following exclusion criteria: a) showed evidence of a psychotic or organic state of sufficient severity to interfere with understanding of project instruments, project procedures, or the informed consent process, b) were deemed an imminent danger to self or others, c) were a ward of child protective services, or d) were scheduled to enter a state juvenile justice or correctional system institution within 3 months of recruitment. All project procedures were conducted under the auspices of Chestnut Health Systems' Institutional Review Board.
Recovery support volunteers
Sixty project volunteers, who were primarily recruited from local university undergraduate and graduate social work and nursing programs, were included as part of the current study. The average volunteer age was 29 years, with approximately half (n=29) between the ages of 17 and 22. Seventy-two percent were female. Allowing for self-report of more than one race/ethnicity, the volunteers described themselves as follows: 82% Caucasian; 17% Asian; 15% Hispanic; 3% Alaska Native/American Indian; and 2% Native Hawaiian/Pacific Islander. Forty-eight percent completed some college education; 32% had a bachelor's degree; 8% had a master's degree; 5% had an associate's degree; 5% completed high school; and 2% had not finished a high school or equivalent education. Finally, the majority (77%) did not report being in recovery. All volunteers agreed to participate in background checks and in a training session on support call procedures, ethics, and confidentiality that incorporated didactic learning, role-plays using support call procedures, and listening to examples of actual telephone support sessions. In addition to documenting call information (e.g., call date, call minutes, notes), volunteers also recorded recovery support calls using a digital recorder. Both call documentation and session audio files were uploaded to a secure server via a web-based program created specifically for this project. Volunteers received weekly supervision and feedback from project coordinators based on reviews of randomly selected cases.
Procedures
Participant recruitment
Adolescents were approached about project participation during outpatient or residential substance use treatment by project staff not associated with treatment at each performance site. Parent/guardian consent was required and obtained for all assenting adolescents. All adolescents who passed inclusion and exclusion criteria and signed the informed assent with guardian consent were provided project services and retained for follow-up interviews.
Recovery support service calls
Within the first week after discharge from treatment, trained volunteers (described above) initiated recovery support service telephone calls, which incorporated concepts from two evidence-based treatments for adolescent substance use disorders: the Adolescent Community Reinforcement Approach (A-CRA) [6,52] and Assertive Continuing Care (ACC) [7,48,53]. More specifically, volunteers were trained to deliver eleven procedures (two optional). During each session, volunteers were instructed to ask about: a) significant events since the last call (i.e., completed a “check-in”); b) substance use, if any, since the last contact; c) steps adolescents recently took to stay clean and sober; d) additional ways adolescents could think of to stay clean and sober; e) the occurrence of any using thoughts and strategies for dealing with them; f) pro-recovery goals and homework to set for the next week; g) progress on goals set during the previous call; h) recovery-related events in adolescents' home communities; and i) the use of additional support services (e.g., recovery-oriented websites). The two optional procedures were referrals for further substance abuse treatment services if relapse occurred and referrals for mental health services if emotional and/or behavioral difficulties were reported. Consistent with the goals of ACC, volunteers reached out to adolescents to schedule and hold the first telephone session within two weeks of discharge from their index treatment episode. Once telephone sessions began, volunteers guided adolescents to create goals that were positive, specific, brief, and under their control to complete. Volunteers also explored potential barriers to completing homework goals to overcome practical issues, such as problems with transportation or negative mood states. Telephone calls were typically 15 minutes or less in length. Text messaging was used to remind adolescents of upcoming calls and to encourage them to answer their phones. On rare occasions, texting sessions were completed at an adolescent's request. The goal during the recovery support call phase was to complete sessions with adolescents once per week during the first 90 days after discharge. The frequency of contacts after that time varied depending on adolescents' functioning and preference. For example, a decrease in calls may have been triggered when adolescents reported an extended period of abstinence or when adolescents asked volunteers to do so, and an increase in call frequency may have been triggered by a relapse, worsening of existing problems, or the emergence of new problems.
Protocol adherence
All telephone recovery support sessions were recorded with the participant's permission. Coordinators at each site reviewed a random sample of calls for each volunteer and provided positive and corrective feedback on protocol adherence during weekly supervision meetings with volunteers. Over the course of the study, 1,742 telephone sessions were completed out of a possible 3,786, for a telephone session completion rate of 46%. For telephone protocols, this rate compares favorably to the average of 37.5% found by Godley et al. [25] and the mean of 11.5 sessions completed out of 32 planned calls completed by McKay et al [26]. An average of nine specific recovery support procedures were completed per call. In addition, homework assignments were agreed to in 94% of sessions, and 69% of homework was reported by adolescents in subsequent sessions to be completed.
Participant assessments
Baseline assessments using the Global Appraisal of Individual Needs (GAIN), [54] which is a widely used comprehensive biopsychosocial assessment that integrates research and clinical assessment into one structured interview, were conducted by trained staff with adolescents at intake to outpatient or residential treatment. The GAIN's main scales have been shown to demonstrate good internal consistency (with alphas greater than .90 on main scales, .70 on subscales) and test–retest reliability (Rhos greater than .70 on days/problem counts, kapp as greater than .60 on categorical measures) and to be highly correlated with measures of use based on timeline follow-back methods, urine tests, collateral reports, treatment records, and blind psychiatric diagnosis (Rho of .70 or more, kappa of .60 or more) [6,54-63]. Copies of the instruments, manual, publications, and documentation on the 100 plus scales in the GAIN are available at www.chestnut.org/li/gain. In addition to the baseline assessment, a follow-up version of the GAIN was completed at 3 and 6 months post-intake. Participants were compensated $30 in gift cards for the time and effort required to complete follow-up measurement interviews, as well as an additional $10 in gift cards for completing interviews within 1 week of its due date.
Creation of Quasi-Experimental comparison sample
In addition to using data collected as part of the RSAF project, data for the current study came from the GAIN 2009 Summary Analytic dataset, which is one of the largest substance use disorder treatment datasets (N = 22,548). As described in more detail below, this data set was used to create a matched comparison sample that would allow us to quasi-experimentally examine the impact of the recovery support calls. Over two-thirds of the assessments were conducted by independent investigators, funded by a wide range of organizations (e.g., SAMHSA/CSAT; National Institute on Alcohol Abuse and Alcoholism, National Institute on Drug Abuse, Robert Wood Johnson Foundation), and conducted in a variety of settings and levels of care. All data were collected as part of general clinical practice or specific research studies under their respective voluntary consent procedures, and all data were subsequently de-identified and made available for secondary analysis under the supervision of Chestnut Health Systems' Institutional Review Board.
After sub setting the GAIN Summary Analytic dataset to 6,696 adolescents similar to those in the RSAF project in terms of age, level of care, and engagement in treatment, we then created a propensity score [64,65] using the variables listed in Table 1 to predict the probability (i.e., propensity) of being in the RSAF sample. Propensity scores were created separately for adolescents treated in outpatient and residential in order maximize the ability of the propensity procedure to create a matched comparison sample. In order to emphasize the contribution of those cases more similar to the RSAF sample and de-emphasize the contributions of those cases less similar to the RSAF sample, weights were created. More specifically, the propensity score for each case was divided by the respective group mean to create an initial Weight variable (W1). Next, a second weight variable was created by dividing the N of the RSAF sample (n = 202) by the N of the GAIN Summary Analytic dataset subset (n = 5,865). The final weighting variable (W3) was then created by multiplying W1 by W2. Finally, to reduce achieving statistical significance for all analyses due to our relatively large comparison sample, we reduced the size of our matched comparison sample to 404, which provided 80% power to detect at least small effect sizes (d = .20).
Table 1. Baseline Characteristics.
| Baseline Characteristics | Recovery Support Sample (N = 202) | Matched Comparison Sample (N = 404) | Effect Size |
|---|---|---|---|
| Female (%) | 26% | 31% | -0.13 |
| Race | |||
| African American | 6% | 12% | -0.21 |
| Caucasian | 56% | 45% | 0.22 |
| Hispanic | 23% | 22% | 0.04 |
| Mixed/Other | 14% | 21% | -0.18 |
| Age (Mean [SD]) | 16.0 [1.2] | 15.9 [1.3] | -0.11 |
| Single Parent | 55% | 51% | 0.07 |
| School | |||
| In School | 70% | 81% | -0.24 |
| Behind < 1 year | 58% | 57% | 0.01 |
| Expelled or Dropped out | 42% | 43% | -0.03 |
| Employeda | 19% | 18% | 0.01 |
| Illegal Activity | |||
| Any Illegal activityb | 80% | 79% | 0.02 |
| Any property crimeb | 69% | 64% | 0.11 |
| Any interpersonal crimeb | 54% | 52% | 0.04 |
| Any drug crimeb | 58% | 57% | 0.01 |
| Delinquency Level | |||
| None | 4% | 3% | 0.04 |
| Unofficial delinquency | 15% | 11% | 0.11 |
| Arrest/Police contact | 8% | 13% | -0.19 |
| Court/Probation/Parole | 34% | 37% | -0.05 |
| Correctional Institution | 39% | 36% | 0.08 |
| Justice Involvement | |||
| Lifetime Justice System Involvement | 80% | 85% | -0.13 |
| Current Justice System Involvement | 70% | 68% | 0.04 |
| In a controlled environmenta | 60% | 57% | 0.05 |
| 13+ days In Controlled Environmenta | 45% | 40% | 0.11 |
| Intensity of Juvenile Justice System Involvement | |||
| In detention/jail 30+ days | 15% | 13% | 0.05 |
| In detention/jail 14-29 days | 14% | 13% | 0.05 |
| On probation/parole 14+ days with 1+ drug screens | 23% | 27% | -0.09 |
| Other probation/parole/detention | 13% | 11% | 0.06 |
| Other Juvenile Justice status | 9% | 12% | -0.10 |
| Arrest/Juvenile Justice statusb | 4% | 6% | -0.07 |
| Illegal activityb | 22% | 19% | 0.07 |
| Environment | |||
| Any physical violenceb | 78% | 73% | 0.10 |
| Weekly Alcohol Use in homea | 28% | 31% | -0.07 |
| Weekly Drug Use in homea | 16% | 17% | -0.03 |
| Work/School Peers Weekly Intoxication | 55% | 52% | 0.05 |
| Social Peers Weekly Intoxication | 61% | 66% | -0.10 |
| Work/School Peers Regular Drug use | 71% | 70% | 0.03 |
| Social Peers Weekly Regular Drug use | 80% | 80% | 0.00 |
| Ever Homeless or Runaway | 46% | 45% | 0.02 |
| Lifetime Victimization | 64% | 69% | -0.10 |
| High Severity Victimization Lifetime | 48% | 55% | -0.13 |
| Victimizationa | 23% | 24% | -0.02 |
| Substance Use | |||
| First Use under Age of 15 | 86% | 85% | 0.03 |
| Weekly Tobacco Usea | 71% | 68% | 0.06 |
| Weekly Alcohol Usea | 31% | 27% | 0.09 |
| Weekly Marijuana Usea | 63% | 61% | 0.03 |
| Weekly Other Drug Use (not Tobacco, Alcohol or Marijuana)a | 28% | 22% | 0.12 |
| Any Lifetime Dependence | 82% | 79% | 0.08 |
| Any Lifetime Abuse | 14% | 18% | -0.11 |
| Any Past Year Dependence | 77% | 75% | 0.06 |
| Any Past Year Abuse | 18% | 21% | -0.07 |
| Any lifetime withdrawal symptoms | 47% | 49% | -0.03 |
| Any past week withdrawal symptoms | 11% | 17% | -0.17 |
| Any Prior Substance Abuse Treatment | 57% | 54% | 0.05 |
| Self-Perceived Substance Problem | 51% | 52% | -0.01 |
| Self-Perceived Need for Treatment | 90% | 88% | 0.06 |
| Physical and Mental Health | |||
| High Health Problemsa | 20% | 20% | 0.01 |
| Pregnant or got someone pregnantb | 16% | 16% | 0.00 |
| Major Depressive Disorderb | 47% | 51% | -0.08 |
| Generalized Anxiety Disorderb | 18% | 20% | -0.04 |
| Any homicidal/suicidal thoughtsb | 33% | 31% | 0.04 |
| Any Traumatic Stress Disorderb | 36% | 38% | -0.05 |
| Conduct Disorderb | 65% | 61% | 0.08 |
| AD/HDb | 50% | 51% | -0.02 |
| Any prior mental health treatment | 60% | 63% | -0.06 |
| Sexual Activity | |||
| Any sexual activitya | 68% | 68% | 0.00 |
| Multiple sexual partnersa | 42% | 40% | 0.04 |
| Any unprotected sexual activitya | 34% | 36% | -0.03 |
| Needle Usea | 5% | 5% | 0.02 |
| Index Substance Use Treatment episode | |||
| Outpatient | 19% | 21% | -0.06 |
| Intensive Outpatient | 14% | 11% | 0.08 |
| Residential | 67% | 67% | 0.00 |
| Length of stay in index treatment in months (Mean [SD]) | 2.0 [1.2] | 2.4 [1.2] | 0.34 |
| Planned discharge from index treatment | 82% | 60% | 0.49 |
| Problem Summaryb | |||
| No major problems | 0% | 1% | -0.02 |
| 1 problem | 2% | 2% | 0.01 |
| 2 problems | 7% | 10% | -0.07 |
| 3 to 12 problems | 90% | 88% | 0.07 |
In Past 90 days
In Past 12 months
Measures
Recovery environment risk
The 12-item Recovery Environment Risk Index (RERI) was used to assess the adolescent's recovery environment. RERI items focus on content breadth rather than homogeneity, and the items represent causal indicators of the construct (i.e., one's recovery environment risk is determined by the number of risk factors present). As such, strong correlations among items would not be expected, and internal consistency would not be an appropriate method of estimating reliability [66]. The summative RERI measure includes days or recency (divided by range) of support group attendance (reversed); homelessness; living with alcohol or drug use in the home; violent arguments; and physical, emotional, or sexual abuse. Higher scores indicate less involvement in support groups (e.g., Alcoholics Anonymous, Cocaine Anonymous, Narcotics Anonymous) and more environmental risk from alcohol/drug use in the home, fighting, and/or victimization.
Social risk
The six-item Social Risk Index (SRI) was used to assess the adolescent's social networks. Similar to RERI, because items on the SRI are causal indicators, we did not compute coefficient alpha for this heterogeneous measure. The summative SRI measure represents a sum of items indicating how many individuals the respondent “hangs out” with socially who are involved in school, training, illegal activities, substance use, or treatment or in recovery. Higher scores indicate more time with individuals in their social environment who are using alcohol/drugs, are involved in illegal activity, argue, are not in school or work, and have never been in treatment.
Substance use
The Substance Frequency Scale (SFS; alpha = .83) was used to measure frequency of adolescents' substance use. The SFS is an average percentage of days during a 90-day period that an adolescent reports each of the following: days of “any” substance use, days of heavy substance use, days of alcohol use, cannabis use, crack/cocaine use, and heroin/opioid use. The scale ranges from 0 to 1, with a higher number indicating more overall reported use. The SFS has been demonstrated to be a better overall predictor of substance-related problems (e.g., withdrawal, abuse/dependence symptoms, illegal activity, and emotional problems) than individual self-report items (e.g., past-month abstinence, days of use, peak use, and recency of use), biometric measures (e.g., urine and saliva), or various combinations of these measures in both adults and adolescents [62,63]. Prior to administration of 6-month interview questions regarding adolescents' substance use, adolescents were asked if they had used any drug other than alcohol in the past week. If past week use was denied, project staff asked adolescents for a urine sample that was screened immediately on-site using the Quik Screen 5 Plus immunochromatographic assay with a one-step drug cup (www.cliawaived.com). Specimens were monitored for temperature and color and checked for adulterants using a built-in strip that tested pH, specific gravity, and level of creatinine, nitrites, bleach, and pyridiumchlorochromate. Standard cutoffs for drug metabolites were: amphetamine (1000 ng/ml), cocaine/benzoylecgonine (300 ng/ml), methamphetamine (1000 ng/ml), opiates/morphine (2000 ng/ml), and cannabis (50 ng/ml). Adolescents were told test results and then administered interview questions. If they tested positive for a drug but did not report using it in the past week, they were asked about reasons for this difference in an attempt to reconcile the conflicting information. This on-site testing procedure resulted in a relatively low false negative rate (positive on urine test; but no past month use self-reported) of 8%.
Substance-related problems
The Substance Problem Scale (SPS; alpha = .91) was used to assess problems related to substance use or substance using behavior. It is based on recency ratings (e.g., past month, 2–12 months ago, more than 12 months ago, or never) on 16 symptoms: 7 corresponding to DSM–IV criteria for dependence, 4 for abuse, 2 for substance-induced health and psychological problems, and 3 on lower severity symptoms of use (hiding use, people complaining about use, weekly use). Although associated with substance use, scores on this scale are conceptually and statistically distinct [67,68].
Treatment readiness
The Treatment Readiness Index (TRI) was used to measure adolescents' readiness for treatment. Similar to RERI and SRI, because items represent causal indicators, coefficient alpha for this heterogeneous measure was not computed. It represents a count of 9 items. Five are related to treatment motivation and include responding “yes” to the following: a) pressure to be in treatment, b) belief that treatment can help, c) belief that 1+ months of treatment are needed, d) recognition of the potential need to come back to treatment, and e) recognition of the need for support from family and friends. Four items are related to treatment resistance and include participants responding “no” to the following: a) treatment being too demanding; b) having too many responsibilities to be in treatment; c) hard to resist alcohol or other drug use where the participant lives, works, or goes to school; d) old friends may try to get the participant to use.
Analytic plan
All analyses were conducted using version 17.2 of Amos structural equation modeling software [69]. In order to control for baseline differences and address the slight skewness of the data identified as part of preliminary data examination, we used change scores (follow-up score minus intake score) for all analyses. Initial analyses, which focused on examination of the direct effects of recovery support calls on the four outcomes of primary interest, were conducted via four models that regressed each respective outcome measure on a recovery support call indicator measure (1 = recovery support sample; 0 = comparison sample). Next, we tested the hypothesized direct and indirect effects model, which was based on prior research (see Figure 1) [47,48]. Missing data were handled using the full information maximum likelihood estimation method, which has been shown to closely estimate population parameters and standard errors [70]. Several standard fit indices were used, including the Root Mean Square Error of Approximation (RMSEA), the Comparative Fit Index (CFI), and the Tucker–Lewis Index (TLI). As noted by Browne and Cudeck [71], RMSEA values of less than .05 indicate a close fit in relation to the degrees of freedom, values of .08 or less indicate a fit with reasonable errors of approximation in the population, and values greater than .10 are a poor fit. Both the CFI and TLI range from 0 to 1, with values greater than .95, indicating very good fit [72-74]. Finally, we tested the extent to which the hypothesized model was invariant (i.e., not significantly different) by gender (1 = Male; 0 = Female) and treatment readiness (1 = High Treatment Readiness; 0 = Low Treatment Readiness). High vs. low treatment readiness was based on a median split.
Results
Baseline sample differences
Table 1 presents a comparison of baseline characteristics for adolescents who received recovery support telephone calls as part of the RSAF project (n = 202) and the matched comparison sample (n = 404), adjusted for the propensity score. Overall, the two samples were well balanced, with only a few differences. Characteristics with effect sizes greater than .20 included the percentage of African American adolescents (RSAF = 6%; Comparison = 12%), percentage of Caucasian adolescents (RSAF = 56%; Comparison = 45%), percentage of adolescents in school (RSAF = 70%; Comparison = 81%), mean months of index treatment episode (RSAF = 2; Comparison = 2.4), and percentage of planned discharges from index treatment episode (RSAF = 82%; Comparison = 60%).
Direct effects of recovery support on 6-month post-discharge client change
Table 2 presents results of analyses of examining the impact of recovery support calls on adolescents' reduction in their recovery environment risk, social risk, substance use, and substance-related problems as assessed six months post-discharge from their index treatment episode. The only direct effect of the recovery support calls was on reductions in adolescents' recovery environment risk, with the adolescents in the recovery support sample having significantly greater reductions (β = -.17, p< .001) compared to the comparison sample. An inspection of individual items contributing to the significant improvement in RERI were items associated with increasing pro-social activities, attendance at mutual aid meetings, and decreasing days alcohol was used at home by significant others.
Table 2.
Direct effects of recovery support on 6-month post-discharge client change.
| Recovery Environment | Social Risk | Substance Use | Substance-related Problems | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | P= | β | SE | P= | β | SE | P= | β | SE | P= | |
| Recovery Support Sample | -0.17 | 0.011 | <.001 | -0.05 | 0.585 | 0.301 | -0.01 | 0.021 | 0.776 | 0.02 | 0.522 | 0.652 |
Indirect effects of recovery support calls on 6-month post-discharge client change
Overall, the data fit the hypothesized model very well (see Figure 2; RMSEA = .057; CFI = .995; TLI = .953). Additionally, analyses supported all but two hypothesized relationships. That is, in addition to having a direct impact on reducing adolescents' recovery environment risk (β = -.16), the recovery support calls had significant indirect impacts (via recovery environment risk) on adolescents' social risk, substance use, and substance-related problems. Again, recovery support calls did not have significant direct impacts on social risk or substance use.
Figure 2.

Results for Hypothesized Model. Solid lines are statistically significant (p< .05); Dotted lines are not statistically significant: Root Mean square Error of Approximation= .057, Comparative Fit Index= 0995; Tucker- Lewis Index= .953
Moderation analyses
Invariance analyses examining the extent to which the hypothesized relationships varied by gender did not reveal gender to significantly moderate any of the hypothesized relationships; however, analyses examining the extent to which the hypothesized relationships varied by treatment readiness did support treatment readiness as a significant moderator (see Figure 3). More specifically, the inverse relationship between recovery support and change in recovery environment risk was significantly greater for adolescents with low treatment readiness (Low Treatment Readiness = β = -.25; High Treatment Readiness = β = -.08). Additionally, the positive relationship between recovery environment risk and substance-related problems was significantly greater for adolescents with high treatment readiness than those with low treatment readiness (High Treatment Readiness = β = .25; Low Treatment Readiness = β = .02). Although not statistically significant, results also indicated a differential relationship between recovery support and substance use by level of treatment readiness (Low Treatment Readiness = β = -.04; High Treatment Readiness = β =.09).
Figure 3.
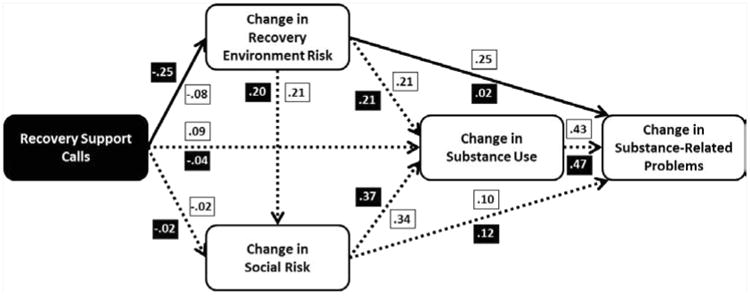
Treatment readliness as a moderator. Black boxes with white font indicate coefficient for adolescent with low treatment readiness; white boxes with black font indicate coefficient for adolescents with high treatment readiness. Solid lines indicate paths that differ significantly (p< .05) by level of treatment readiness.
Discussion
Study reprise
The present quasi-experimental study sought to advance the limited current understanding about the effectiveness of recovery support services following adolescent substance use disorder treatment, as well as to examine the extent to which the effect of such services may differ by factors known to moderate the impact of continuing care interventions (i.e., gender, treatment readiness). As hypothesized, adolescents who received recovery support calls had significantly greater reductions in their recovery environment risk, relative to a matched comparison sample. Results from the current study did not support the recovery support calls having direct effects on post-treatment measures of improvement in social risk, substance use, or substance-related problems; however, consistent with prior research suggesting recovery environment risk as a key mechanism of change, [47,48] findings supported the hypothesis that recovery support calls would have indirect effects on adolescents' post-treatment social risk, substance use, and substance-related problems via reductions in recovery environment risk.
In contrast to similar research that has suggested stronger effects of continuing care interventions for females, our study suggested the recovery support calls worked similarly well for both male and female adolescents. Additional research will be needed to further explore the extent to which recovery support services have differential effects for males and females, as well as the extent to which these effects may differ between adolescents and adults. Nonetheless, we are encouraged that these preliminary findings do not suggest the need for adapting services based on gender differences. As hypothesized, and similar to research suggesting continuing care interventions have stronger effects for individuals with lower levels of treatment readiness, [27,51] the recovery support calls used as part of the RSAF project did appear to have significantly greater effects for adolescents with lower treatment readiness at intake to treatment, at least with regard to its impact on reducing recovery environment risk. Again, additional research, preferably some of which include randomized designs, will be needed to examine the differential impact of recovery support services by level of treatment readiness.
Limitations
Despite being one of the more rigorous evaluations of recovery support services to date, findings of the current study must be viewed in light of at least two important limitations. First, although the use of a matched comparison sample provided a strong quasi-experimental design, such a design does not allow for as strong of inferences as randomized controlled trials. Second, while the results at the six-month follow-up suggest positive implications for recovery support calls, a six-month follow-up is inadequate to predict longer term recovery outcomes. Thus, future research should extend the length of follow-up for at least one year or longer.
Clinical and workforce implications
At least three key clinical implications may be drawn from the current study. First, the current study provides rare empirical evidence supporting the widely held, but little empirically supported assumption that recovery support services following episodes of formal outpatient and/or residential treatment are indeed effective in improving client outcomes. Thus, we hope that one important clinical implication of this study is that it serves as a springboard for both the provision of recovery support services in community-settings, as well as additional research to identify the most effective and cost-effective recovery support services. Second, this study supports other research with adolescents that suggest encouragement from treatment or continuing care staff to attend mutual aid meetings is predictive of greater attendance. Third, this study provided evidence that recovery support services do not necessarily have to be “peer-based,” at least in terms of the recovery support service provider having the experiential credentials of being “in recovery.”
Although acknowledged as a preliminary quasi-experimental finding, if these results can be replicated, an important workforce implication would be to broaden the base of the recovery support workforce. The development of effective recovery support models that utilize pre-professionals (e.g., college-level human service students) could have a significant impact on the extent to which recovery support services are delivered. Moreover, given the broad availability of college-level human service students that would potentially be both interested and available to volunteer (and earn course credit) to provide this service in exchange for the opportunity to gain valuable applied experience, such recovery support models may have very good potential for successful implementation and sustainment, both of which are known issues within the substance use treatment field [19].
Conclusions and additional directions for future research
In conclusion, there is evidence that the provision of recovery support calls to adolescents following formal outpatient or residential substance use disorder treatment can be beneficial in terms of helping improve post-treatment outcomes, and such services may have greater impact for adolescents with lower levels of treatment readiness. Additionally, there is evidence for both the feasibility and effectiveness of using pre-professional volunteers to provide recovery support calls. Since the present positive outcomes were achieved with the majority of volunteers not having addiction recovery experience, the question of whether there are differences in outcomes based on the recovery status of those providing post-treatment recovery support services remains to be tested. Also left unanswered is the question of how the organizational setting through which recovery support services are provided to adolescents might affect key outcomes. It is unknown whether such services are best provided by an addiction treatment organization, research institute, recovery community organization, school, youth center, or other organization. Although the present results are promising, considerable research remains needed. There is clearly a need for randomized controlled trials, at least one of which is currently underway [77]. In addition to the need for research to provide support for the efficacy and effectiveness of recovery support services, however, is the need for research to better understand the cost-effectiveness and/or cost-benefits of providing evidence-based recovery support. Indeed, similar research has been suggested for continuing care research [78]. Finally, consistent with recommendations for research to identify methods to increase implementation of evidence-based continuing care interventions [20], we suggest the need to identify strategies to increase implementation of evidence-based recovery support services. Ideally, the current study will help serve as a springboard for greater empirical research related to post-treatment recovery support services to address these and other important questions that will ultimately lead to better outcomes for individuals impacted by substance use.
Acknowledgments
Preparation of this manuscript was supported by funding from the Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration, Department of Health and Human Services (We stat Subcontract No. s8440 of SAMHSA Contract No. HHSS28320070006I) and the National Institute on Alcohol Abuse and Alcoholism, (grant no. R01 AA-021118). This publication reflects the views of the authors and do not reflect official positions of the government. The authors wish to acknowledge Randy Muck for his leadership in the field adolescent treatment and recovery, as well as project staff at each performance site for overseeing participant recruitment and follow-up and volunteer recruitment and supervision: Gina Grappone, Dave Hamolsky, Lisa Pineo, Bridget Ruiz, Stephanie Schade, Stephanie Springer, and Jamie Weber. This project would also not have been possible without the many volunteers who contributed their time and dedication providing support to youth. Finally, the authors want to acknowledge the work of Stephanie Kerns with manuscript preparation.
References
- 1.Deas D, Thomas SE. An overview of controlled studies of adolescent substance abuse treatment. Am J Addict. 2001;10:178–189. doi: 10.1080/105504901750227822. [DOI] [PubMed] [Google Scholar]
- 2.Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. J Clin Child Adolesc Psychol. 2008;37:238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- 3.Bender K, Tripodi SJ, Sarteschi C, Vaughn MG. A meta-analysis of interventions to reduce adolescent cannabis use. Res Soc Work Pract. 2011;21:153–164. [Google Scholar]
- 4.Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: a meta-analysis. J Subst Abuse Treat. 2013;44:145–158. doi: 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. J Consult Clin Psychol. 2001;69:802–813. [PubMed] [Google Scholar]
- 6.Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of assertive continuing care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- 8.Hser YI, Anglin MD, Grella C, Longshore D, Prendergast ML. Drug treatment careers. A conceptual framework and existing research findings. J Subst Abuse Treat. 1997;14:543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- 9.Dennis ML, Scott CK, Funk R, Foss MA. The duration and correlates of addiction and treatment careers. J Subst Abuse Treat. 2005;28(Suppl 1):S51–62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 10.Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 12.McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- 13.Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007;4:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White WL, McLellan AT. Addiction as a chronic disease: key messages for clients, families and referral sources. Counselor. 2008;9:24–33. [Google Scholar]
- 15.McKay JR, Carise D, Dennis ML, Dupont R, Humphreys K, Kemp J, et al. Extending the benefits of addiction treatment: practical strategies for continuing care and recovery. J Subst Abuse Treat. 2009;36:127–130. doi: 10.1016/j.jsat.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKay JR. Effectiveness of continuing care interventions for substance abusers. Implications for the study of long-term treatment effects. Eval Rev. 2001;25:211–232. doi: 10.1177/0193841X0102500205. [DOI] [PubMed] [Google Scholar]
- 17.McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blodgett JC, Maisel NC, Fuh IL, Wilbourne PL, Finney JW. How effective is continuing care for substance use disorders? A meta-analytic review. J Subst Abuse Treat. 2014;46:87–97. doi: 10.1016/j.jsat.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garner BR. Research on the diffusion of evidence-based treatments within substance abuse treatment: a systematic review. J Subst Abuse Treat. 2009;36:376–399. doi: 10.1016/j.jsat.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lash SJ, Timko C, Curran GM, McKay JR, Burden JL. Implementation of evidence-based substance use disorder continuing care interventions. Psychol Addict Behav. 2011;25:238–251. doi: 10.1037/a0022608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, et al. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. J Consult Clin Psychol. 2004;72:967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- 22.McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Arch Gen Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- 23.Hubbard RL, Leimberger JD, Haynes L, Patkar AA, Holter J, Liepman MR, et al. Telephone enhancement of long-term engagement (TELE) in continuing care for substance abuse treatment: a NIDA clinical trials network (CTN) study. Am J Addict. 2007;16:495–502. doi: 10.1080/10550490701641678. [DOI] [PubMed] [Google Scholar]
- 24.Cacciola JS, Camilleri AC, Carise D, Rikoon SH, McKay JR, McLellan AT, et al. Extending residential care through telephone counseling: initial results from the Betty Ford Center Focused Continuing Care protocol. Addict Behav. 2008;33:1208–1216. doi: 10.1016/j.addbeh.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Godley MD, Coleman-Cowger VH, Titus JC, Funk RR, Orndorff MG. A randomized controlled trial of telephone continuing care. J Subst Abuse Treat. 2010;38:74–82. doi: 10.1016/j.jsat.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKay JR, Van Horn DH, Oslin DW, Lynch KG, Ivey M, Ward K, et al. A randomized trial of extended telephone-based continuing care for alcohol dependence: within-treatment substance use outcomes. J Consult Clin Psychol. 2010;78:912–923. doi: 10.1037/a0020700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKay JR, Van Horn D, Oslin DW, Ivey M, Drapkin ML, Coviello DM, et al. Extended telephone-based continuing care for alcohol dependence: 24-month outcomes and subgroup analyses. Addiction. 2011;106:1760–1769. doi: 10.1111/j.1360-0443.2011.03483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burleson JA, Kaminer Y, Burke RH. Twelve-month follow-up of aftercare for adolescents with alcohol use disorders. J Subst Abuse Treat. 2012;42:78–86. doi: 10.1016/j.jsat.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKellar J, Wagner T, Harris A, Oehlert M, Buckley S, Moos R. One-year outcomes of telephone case monitoring for patients with substance use disorder. Addict Behav. 2012;37:1069–1074. doi: 10.1016/j.addbeh.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 30.Farabee D, Cousins SJ, Brecht ML, Antonini VP, Lee AB, Brummer J, et al. A comparison of four telephone-based counseling styles for recovering stimulant users. Psychol Addict Behav. 2013;27:223–229. doi: 10.1037/a0029572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKay JR, van Horn D, Ivey M, Drapkin ML, Rennert L, Lynch KG. Enhanced continuing care provided in parallel to intensive outpatient treatment does not improve outcomes for patients with cocaine dependence. J Stud Alcohol Drugs. 2013;74:642–651. doi: 10.15288/jsad.2013.74.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White WL. Peer-based addiction recovery support: history, theory, practice, and scientific evaluation. Chicago, IL: Great Lakes Addiction Technology Transfer Center; 2009. [Google Scholar]
- 33.Valentine P. Peer-based recovery support services within a recovery community organization: the CCAR experience. In: Kelly JF, White WL, editors. Addiction recovery management: theory, science and practice. New York: Springer; 2011. pp. 259–279. [Google Scholar]
- 34.Kaplan L. The role of recovery support services in recovery-oriented systems of care DHHS Publication No (SMA)08 4315. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2008. [Google Scholar]
- 35.Ryan JP, Choi S, Hong JS, Hernandez P, Larrison CR. Recovery coaches and substance exposed births: an experiment in child welfare. Child Abuse Negl. 2008;32:1072–1079. doi: 10.1016/j.chiabu.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 36.Davidson L, White W, Sells D, Schmutte T, O'Connell M, Bellamy C, et al. Enabling or engaging? The role of recovery support services in addiction recovery. Alcohol Treat Q. 2010;28:391–416. doi: 10.1080/07347324.2010.511057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sinnett ER, Hagen K, Harvey WM. Credibility of sources of information about drugs to heroin addicts. Psychol Rep. 1975;37:1239–1242. doi: 10.2466/pr0.1975.37.3f.1239. [DOI] [PubMed] [Google Scholar]
- 38.Lawson G. Relation of counselor traits to evaluation of the counseling relationship by alcoholics. J Stud Alcohol. 1982;43:834–839. doi: 10.15288/jsa.1982.43.834. [DOI] [PubMed] [Google Scholar]
- 39.Mavis BE, Stöffelmayr BE. Program factors influencing client satisfaction in alcohol treatment. J Subst Abuse. 1994;6:345–354. doi: 10.1016/s0899-3289(94)90546-0. [DOI] [PubMed] [Google Scholar]
- 40.Brown BS, Thompson RF. The effectiveness of formerly addicted and nonaddicted counselors on client functioning. Drug Forum. 1975;5:123–129. [Google Scholar]
- 41.Connett GE. Comparison of progress of patients with professional and paraprofessional counselors in a methadone maintenance program. Int J Addict. 1980;15:585–589. doi: 10.3109/10826088009040039. [DOI] [PubMed] [Google Scholar]
- 42.Moos RH, Finney JW, Chan DA. The process of recovery from alcoholism. I. Comparing alcoholic patients and matched community controls. J Stud Alcohol. 1981;42:383–402. doi: 10.15288/jsa.1981.42.383. [DOI] [PubMed] [Google Scholar]
- 43.McLellan AT, Woody GE, Luborsky L, Goehl L. Is the counselor an “active ingredient” in substance abuse rehabilitation? An examination of treatment success among four counselors. J Nerv Ment Dis. 1988;176:423–430. doi: 10.1097/00005053-198807000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Durlak JA. Comparative effectiveness of paraprofessional and professional helpers. Psychol Bull. 1979;86:80–92. [PubMed] [Google Scholar]
- 45.Pearl A. The paraprofessional in human service. In: Robbin S, Wagonfeld W, editors. Paraprofessionals in the human services. New York: Human Science Press; 1981. [Google Scholar]
- 46.Hattie JA, Sharpley CF, Rogers HJ. Comparative effectiveness of professional and paraprofessional helpers. Psychol Bull. 1984;95:534–541. [PubMed] [Google Scholar]
- 47.Godley MD, Kahn JH, Dennis ML, Godley SH, Funk RR. The stability and impact of environmental factors on substance use and problems after adolescent outpatient treatment for cannabis abuse or dependence. Psychol Addict Behav. 2005;19:62–70. doi: 10.1037/0893-164X.19.1.62. [DOI] [PubMed] [Google Scholar]
- 48.Garner BR, Godley MD, Funk RR, Dennis ML, Godley SH. The impact of continuing care adherence on environmental risks, substance use and substance-related problems following adolescent residential treatment. Psychol Addict Behav. 2007;21:488–497. doi: 10.1037/0893-164X.21.4.488. [DOI] [PubMed] [Google Scholar]
- 49.Carter RE, Haynes LF, Back SE, Herrin AE, Brady KT, Leimberger JD, et al. Improving the transition from residential to outpatient addiction treatment: gender differences in response to supportive telephone calls. Am J Drug Alcohol Abuse. 2008;34:47–59. doi: 10.1080/00952990701764599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: a randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2008;47:1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lynch KG, Van Horn D, Drapkin M, Ivey M, Coviello D, McKay JR. Moderators of response to telephone continuing care for alcoholism. Am J Health Behav. 2010;34:788–800. doi: 10.5993/ajhb.34.6.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Godley SH, Meyers RJ, Smith JE, Godley MD, Titus JC, Karvinen T, et al. Adolescent Community Reinforcement Approach (A-CRA) for adolescent cannabis users Cannabis Youth Treatment (CYT) Manual Series, Volume 4, DHHS Publication No (SMA) 01-3489. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. [Google Scholar]
- 53.Godley SH, Godley MD, Karvinen T, Slown LL, Wright KL. The Assertive Continuing Care protocol: a clinician's manual for working with adolescents after residential treatment of alcohol and other substance use disorders. Bloomington IL: Lighthouse Institute; 2006. [Google Scholar]
- 54.Dennis ML, Titus JC, White M, Unsicker J, Hodgkins D. Global Appraisal of Individual Needs (GAIN): administration guide for the GAIN and related measures Version 5. Bloomington, IL: Chestnut Health Systems; 2003. [Google Scholar]
- 55.Dennis M, Titus JC, Diamond G, Donaldson J, Godley SH, Tims FM, et al. The Cannabis Youth Treatment (CYT) experiment: rationale, study design and analysis plans. Addiction. 2002;97(Suppl 1):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- 56.Godley MD, Godley SH, Dennis ML, Funk R, Passetti LL. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat. 2002;23:21–32. doi: 10.1016/s0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- 57.Dennis ML, Dawud-Noursi S, Muck RD, McDermeit M. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent substance abuse treatment in the United States: exemplary models from a national evaluation study. Binghamton, NY: Haworth Press; 2003. pp. 3–34. [Google Scholar]
- 58.Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Program Plann. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shane P, Jasiukaitis P, Green RS. Treatment outcomes among adolescents with substance abuse problems: the relationship between comorbidities and post-treatment substance involvement. Eval Program Plann. 2003;26:393–402. [Google Scholar]
- 60.Godley SH, Jones N, Funk R, Ives M, Passetti LL. Comparing outcomes of best-practice and research-based outpatient treatment protocols for adolescents. J Psychoactive Drugs. 2004;36:35–48. doi: 10.1080/02791072.2004.10399722. [DOI] [PubMed] [Google Scholar]
- 61.Dennis ML, Chan YF, Funk RR. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15(Suppl 1):80–91. doi: 10.1080/10550490601006055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lennox R, Dennis ML, Ives M, White MK. The construct and predictive validity of different approaches to combining urine and self-reported drug use measures among older adolescents after substance abuse treatment. Am J Addict. 2006;15(Suppl 1):92–101. doi: 10.1080/10550490601006089. [DOI] [PubMed] [Google Scholar]
- 63.Lennox R, Dennis ML, Scott CK, Funk R. Combining psychometric and biometric measures of substance use. Drug Alcohol Depend. 2006;83:95–103. doi: 10.1016/j.drugalcdep.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 65.Dehejia RH, Wahba S. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84:151–161. [Google Scholar]
- 66.Bollen KA. Multiple indicators: internal consistency or no necessary relationship? Qual Quant. 1984;18:377–385. [Google Scholar]
- 67.Titus JC, Dennis ML, White WL, Scott CK, Funk RR. Gender differences in victimization severity and outcomes among adolescents treated for substance abuse. Child Maltreat. 2003;8:19–35. doi: 10.1177/1077559502239612. [DOI] [PubMed] [Google Scholar]
- 68.Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(Suppl 2):120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- 69.Arbuckle JL. AMOS 16 users guide. Chicago; IBM SPSS; 2007. [Google Scholar]
- 70.Mehrotra DV, Li X, Liu J, Lu K. Analysis of longitudinal clinical trials with missing data using multiple imputation in conjunction with robust regression. Biometrics. 2012;68:1250–1259. doi: 10.1111/j.1541-0420.2012.01780.x. [DOI] [PubMed] [Google Scholar]
- 71.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res. 1993;21:230–258. [Google Scholar]
- 72.Tucker LR, Lewis C. The reliability of coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- 73.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 74.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 75.Kelly JF, Dow SJ, Yeterian JD, Kahler CW. Can 12-step group participation strengthen and extend the benefits of adolescent addiction treatment? A prospective analysis. Drug Alcohol Depend. 2010;110:117–125. doi: 10.1016/j.drugalcdep.2010.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Passetti LL, Godley SH, Godley MD. Youth participation in mutual support groups: history, current knowledge and areas for future research. J Groups Addict Recover. 2012;7:253–278. [Google Scholar]
- 77.Godley MD. Effectiveness of Volunteer Telephone Continuing Care (VTCC) for adolescents with alcohol and other drug use disorders R01 AA021118. National Institute on Alcohol Abuse and Alcoholism (NIAAA); 2012. [Google Scholar]
- 78.Popovici I, French MT, McKay JR. Economic evaluation of continuing care interventions in the treatment of substance abuse: recommendations for future research. Eval Rev. 2008;32:547–568. doi: 10.1177/0193841X08316311. [DOI] [PubMed] [Google Scholar]


