Abstract
STUDY DESIGN
Cohort study, cross-sectional.
OBJECTIVES
To determine if self-reported knee function assessed with the International Knee Documentation Committee 2000 Subjective Knee Form (IKDC2000) could discriminate between successful and non-successful performance on return to activity criteria (RTAC) tests after anterior cruciate ligament (ACL) reconstruction.
BACKGROUND
Rehabilitation specialists are challenged in selecting appropriate performance-based and patient-reported tests that can detect side-to-side asymmetries, assess global knee function, and determine a participant's readiness to return to activity after ACL reconstruction. A simple tool or questionnaire that could identify athletes with neuromuscular impairments or activity limitations could provide rehabilitation specialists crucial data pertinent to their current knee function and their readiness to return to higher level activities.
METHODS
One hundred fifty-eight Level I/II athletes 6 months after ACL reconstruction and 141 athletes 12 months after ACL reconstruction completed a functional test battery to determine readiness to return to activity and the IKDC2000 to determine self-reported knee function. For each athlete, status on return to activity tests criteria was dichotomized as “Passed” or ”Failed” and status on the IKDC2000 scores was dichotomized as being “within” or “below age- and sex-matched normal ranges”. Comparisons were made between status on RTAC and IKDC2000 using Chi-square tests. Accuracy statistics were also calculated.
RESULTS
Six months after ACL reconstruction, 112 athletes (70.9%) failed RTAC and 76 (48.1%) were classified as having self-reported knee function below normal ranges. Among the 76 participants with IKDC2000 scores below normal ranges, 69 (90.8%) failed RTAC test battery (P<.001). However, among the 82 participants whose IKDC2000 scores were within normal limits at 6 months, only 39 (47.6%) passed RTAC test battery (P=.74). Twelve months after ACL reconstruction, 67 athletes (47.5%) failed RTAC and 31 (78.0%) had knee function below normal ranges. Among the 31 participants with IKDC2000 scores below normal ranges, 25 (80.6%) failed RTAC test battery (P<.001). However, among the 110 participants whose IKDC2000 scores were within normal limits at 12 months, only 68 (61.8%) passed RTAC test battery (P=.017).
CONCLUSION
The IKDC2000 may be a clinically relevant tool to determine the timeliness or necessity of RTAC testing. For scores obtained 6 and 12 months after ACL reconstruction, low IKDC2000 scores were reasonably indicative of failure on RTAC test battery, whereas normal IKDC2000 scores were not predictive of passing scores on the RTAC test battery.
Keywords: ACL, IKDC2000, patient-reported measure, return to sport
Injuries to the anterior cruciate ligament (ACL) are frequent during sporting activities,39 resulting in more than 125 000 reconstruction surgeries annually in the United States.33 Despite mechanical stabilization, surgical reconstruction of the ACL does not guarantee a return to previous levels of activity, good knee function, or the preservation of future joint health.1, 14, 25, 35, 40, 42, 46 Because not all individuals regain optimal knee function after ACL reconstruction,3, 8 it is critical to understand if knee function is associated with other clinical factors that may provide insight into the patient's current functional status. The International Knee Documentation Committee 2000 Subjective Knee Form (IKDC2000) has been used frequently after ACL reconstruction to measure knee function.24 The IKDC2000 can differentiate between individuals with low versus high knee function, as well as those with more versus less knee symptoms.2 The published IKDC2000 normative dataset2 provides a reference standard for normal knee function.22, 37 However, it is unknown if scores on the IKDC2000 are associated with performance-based measures used to assess readiness to return to activity.
One of the challenges of post-operative management after ACL reconstruction has been to develop accurate tests that can assess global knee function, detect side-to-side asymmetries, and determine a patient's readiness to return to activity. After ACL reconstruction, many individuals continue to exhibit impaired function characterized by dynamic knee instability and pain, limited range of motion, quadriceps strength deficits, reduced functional performance, neuromuscular dysfunction, and biomechanical mal-adaptations that may account for inferior outcomes and increased risk for second injury. 12, 13, 25, 30, 43, 48, 58 Assessment of modifiable factors may enhance a clinician's ability to determine a participant's potential for success after ACL reconstruction. Batteries of tests have been developed to predict the risk for musculoskeletal injuries,32 classify individuals early after ACL injury,17 and identify important limb asymmetries after ACL injury and reconstruction.23, 44 A test battery of performance-based measures and patient-reported outcomes demonstrated that participants who successfully returned to high-level activity after non-operative management of an ACL injury had less than a 10% deficit on their baseline scores on average.17 A functional test instrument using a battery of performance-based tests was moderately correlated with the IKDC2000 and discriminated between the operated and nonoperated limbs of participants after ACL reconstruction.9 While a battery of tests is typically easy to administer, the combination of tests may be inappropriate for some athletes, such as those with residual impairments, pain, or fear of reinjury. They also can be time-consuming for both athlete and clinician. Furthermore, equipment limitations, such as the lack of electromechanical dynamometry, may be reality in many clinics. Thus, the use of a simple tool or questionnaire that can identify those athletes with neuromuscular impairments and activity limitations can provide rehabilitation specialists crucial data pertinent to participants’ current knee function and their readiness to return to higher level activities, as well as, their progress during rehabilitation and the necessity for additional rehabilitation.
It is unclear whether knee function measured with the IKDC2000 can serve as an accurate surrogate to a more time-intensive battery of tests used to determine readiness to return to activities. Therefore, the aim of this study was to determine if self-reported knee function assessed with the IKDC2000 could discriminate between successful and non-successful performance on return to activity tests criteria after ACL reconstruction. We hypothesized that 1) athletes with self-reported knee function below normal ranges would be more likely to fail return to activity criteria (RTAC) tests 6 and 12 months after ACL reconstruction compared to those with self-reported knee function within normal ranges and 2) athletes with patient-reported knee function within normal ranges would be more likely to pass RTAC tests 6 and 12 months after ACL reconstruction compared with those with knee function below normal ranges. A secondary aim was to examine the differences and magnitudes of differences between performance on return to activity tests and knee function as measured by IKDC2000 scores.
METHODS
Between October 2006 and September 2010, 279 participants with a unilateral ACL rupture were recruited as part of a larger prospective international cohort study between The University of Delaware (Delaware) and Norwegian Research Center for Active Rehabilitation (Oslo). ACL rupture was confirmed by magnetic resonance imaging (MRI) and a 3 mm or greater side-to-side difference in anterior tibial translation12 with a maximal pull on a KT-1000 arthrometer (MedMetrics, San Diego, CA). Athletes were eligible to participate in the study if they were between the ages of 13 and 60 years and were regular participants in level I or II activities (at least 50 hours/year) prior to ACL rupture.12, 26 Level I activities are sports that involve jumping, pivoting, and hard cutting (eg, basketball, soccer) and occupations comparable to Level I sports.12 Level II activities are sports that involve less jumping and hard cutting than Level I but still include lateral motion (eg, baseball, racquet sports) and occupations that involve heavy manual labor, climbing, or working on uneven surfaces.12 Potential participants were excluded if they had concomitant grade III ligament injury, bilateral lower limb involvement, symptomatic meniscal injury (pain associated with activities of daily living or repairable meniscus identified by MRI), fracture, or full-thickness articular cartilage damage. All participants gave informed consent at the time of inclusion. The study was approved by the Ethical/Human Subjects committees of the University of Delaware and South-Eastern Norway and conducted within the guidelines given by the Helsinki declaration.
Testing and Rehabilitation
All participants went through initial rehabilitation after the ACL injury to address acute impairments. Once participants had resolution of initial impairments, they were enrolled in a 10-session pre-operative rehabilitation program.16, 18 This program consisted of progressive exercises emphasizing aggressive strength and specialized perturbation training to help restore muscle strength and appropriate neuromuscular responses. Muscle strength training involved the use of high intensity, low repetition non-weight bearing and weight bearing quadriceps strengthening exercises augmented with neuromuscular electrical stimulation if participants demonstrated a quadriceps strength index of less than 80%.15, 56 Perturbation training was administered according to the protocol outlined by Fitzgerald et al.19
Participants underwent reconstructive surgery with either a semitendinosus-gracilis autograft (n=81), bone-patellar tendon-bone autograft (n=30), or soft tissue allograft (n=63). Graft type was not reported for 20 of the participants. After surgery, the same ACL reconstruction rehabilitation guidelines5, 50 were followed for all participants, and participants were systematically progressed through rehabilitation based on the clinical milestones outlined in the guidelines.5, 50
Six and 12 months after ACL reconstruction, participants completed a battery of functional tests and measures to assess their current knee function and determine their readiness for returning to activity that consisted of quadriceps strength testing, single-legged hop testing,45 and 2 patient-reported outcome measures.27, 29 Quadriceps strength testing consisted of either maximal voluntary isometric contraction (MVIC) (Delaware) or peak torque with isokinetic strength testing of the quadriceps (Oslo). For quadriceps strength testing, the uninvolved side was tested first, followed by the involved side. For MVIC testing, the participant was seated on the seat of the dynamometer and the hips and knees were placed in 90° of flexion. Participants performed up to a maximum of 3 MVICs on an electromechanical dynamometer (Kin-Com, Chattanooga Corp., Chattanooga, TN). Verbal encouragement from the therapist and visual feedback from the dynamometer's real-time visual display were used to help facilitate maximal effort. Customized written code in LabVIEW software (National Instruments, Austin, TX) was used to determine the maximal volitional force in Newtons (N). For isokinetic peak torque, the participant was seated on the seat of the dynamometer and the range of motion was set from 90° knee flexion to full extension (0°). Participants performed 5 repetitions at 60° per second on an electromechanical dynamometer (Biodex 6000, Biodex Medical Systems Inc, Shirley, NY). Peak torque values were measured in newton-meters as per the Biodex software (Nm). The level of association between isometric and isokinetic quadriceps strength testing as performed in this study has been reported to be r=0.93.38 Peak force or torque values achieved during quadriceps strength testing were recorded. Quadriceps index (QI) was expressed as a percentage of the peak value on the involved side divided by the peak value on the uninvolved side for each participant.
Following quadriceps strength testing, participants performed 4 single-legged hop tests in the following order: single hop for distance (single hop), cross-over hop for distance (crossover hop), triple hop for distance (triple hop), and 6-meter timed hop.45 These hop tests are valid and have demonstrated good test-retest reliability in normal, young adults10, 53 and in individuals after ACL reconstruction.49 For each test, the uninvolved leg was tested before the involved side. The participants performed 1-2 practice trial followed by 2 recorded trials for each leg. The hop score for each test was then calculated as the average of the 2 recorded trials. The single hop, the crossover hop, and the triple hop for distance were considered successful if the landing was stable. If not successful, the hop test was repeated. For these 3 hop tests, participants were instructed to place their lead toe behind a marked starting line. The hop distance was measured to the nearest centimeter from the starting line to the participant's heel with a standard tape measure. For the 6-meter timed hop, participants stood on 1 leg, then hopped as fast as possible over a marked distance of 6 meters. The time was measured to the nearest 100th of a second with a standard stopwatch. The stopwatch was started when the participant's heel left the floor and stopped when the participant crossed the finish line. All single–legged hop tests were conducted by physical therapists trained in the test procedures. For the single hop, cross-over hop, and triple hop, limb symmetry index (LSI) was expressed as the percentage performance on the involved side compared to the uninvolved side. For the 6-meter timed hop, LSI was expressed as the percentage performance of the uninvolved side compared to the involved side.
Following hop testing, participants completed 3 self-report questionnaires: the Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADLS), the Global Rating Scale of Perceived Function (GRS), and the IKDC2000. The KOS-ADLS is a 14 item patient-reported outcome of symptoms and functional limitations of the knee during activities of daily living.29 The GRS asks participants to rate their current knee function on a scale from 0 to 100, with 0 being the inability to perform any activity and 100 being the level of knee function prior to the injury, including sports.27, 29 The IKDC2000 was used as the primary self-report outcome variable for this study. It is a knee-specific outcome measure pertinent to a variety of knee conditions for assessing symptoms, function, and sports activity.28 The form contains 18 questions, in which the total scores are expressed as a percentage with higher scores representing better knee function and less symptoms.
Pass/Fail criteria
To pass readiness for return to activity, participants were required to achieve 90% or greater on each of the functional tests and measures from the battery of tests (QI, 4 hop LSIs, KOS-ADLS, and GRS).17, 25 Participants were dichotomized into 2 groups: “Pass” (greater than 90% on all 7 measures) or “Fail” (less than 90% on 1 or more measures) (TABLE 1). Athletes who presented to the clinic for testing but were not able to complete 1 or more aspects of testing due to clinical reasons (pain, effusion, fear of hopping, etc) were classified as having “Failed” return to activity tests.
TABLE 1.
| Measure | Pass | Fail |
|---|---|---|
| Quadriceps Index | ≥ 90% on all criteria | < 90% on 1 or more criteria |
| 4 single-legged hop indexes | ||
| KOS-ADLS | ||
| GRS | ||
Abbreviations: KOS-ADLS, Knee Outcome Survey-Activities of Daily Living Scale; GRS, Global Rating Scale of Perceived Function
Normative data for the IKDC2000 for men and women with no current or history of knee problems has been previously established.2 In this study, athletes under the age of 18, were classified using the age 18 to 24 year normative data. We operationally defined normal ranges on the IKDC2000 as scores greater than or equal to the 15th percentile of the participant-specific age- and sex-matched population.22, 37 The 15th percentile from the normative data from uninjured individuals was chosen as the cut-off score to ensure that individuals who scored below the cutoff were different from what could be considered a normal variation in IKDC scores (TABLE 2).
TABLE 2.
Cutoffs for IKDC2000 scores to be within normal ranges for age- and sex-specific groups
| Age Group, Men | Age Group, Women | ||||||
|---|---|---|---|---|---|---|---|
| 18-24 | 25-34 | 35-50 | 51-65 | 18-24 | 25-34 | 35-50 | 51-65 |
| 89.7 | 86.2 | 85.1 | 74.7 | 83.9 | 82.8 | 78.5 | 69.0 |
Abbreviation: IKDC2000, International Knee Documentation Committee 2000 subjective knee form
Statistical analysis
All statistical analyses were conducted in SPSS v.21 (Chicago, IL). No interaction of site and IKDC2000 at 6 months (P=.97) and 12 months (P=.34) after ACL reconstruction was found in identifying RTAC at 6 months and 12 months, respectively, and therefore data from both sites were merged for further analysis. For the primary aim of this study, sensitivity, specificity, positive likelihood ratio (PLR), and negative likelihood ratio (NLR) and their 95% confidence intervals (CIs) were calculated for RTAC and self-reported knee function assessed with the IKDC2000. Sensitivity was reported as the percentage of participants not passing RTAC correctly identified by having knee function below normal ranges. Specificity was defined as the percentage of participants passing RTAC correctly identified by having knee function within normal ranges. PLR was calculated as sensitivity divided by 1 minus specificity and NLR was calculated as 1 minus sensitivity divided by specificity. Comparisons were made between participants who reported knee function within and below normal ranges based on IKDC2000 scores and between participants who passed or failed RTAC using Chi-square tests for nominal data and Mann-Whitney U analysis for continuous data. The magnitude of the differences between the groups with knee function within and groups with knee function below normal ranges were calculated using effect size for nonparametric data (the quotient of the z-score divided by the square root of the total number of observations). Interaction was assessed in a logistic regression model that included dichotomized IKDC2000, site, and a multiplicative interaction term.
RESULTS
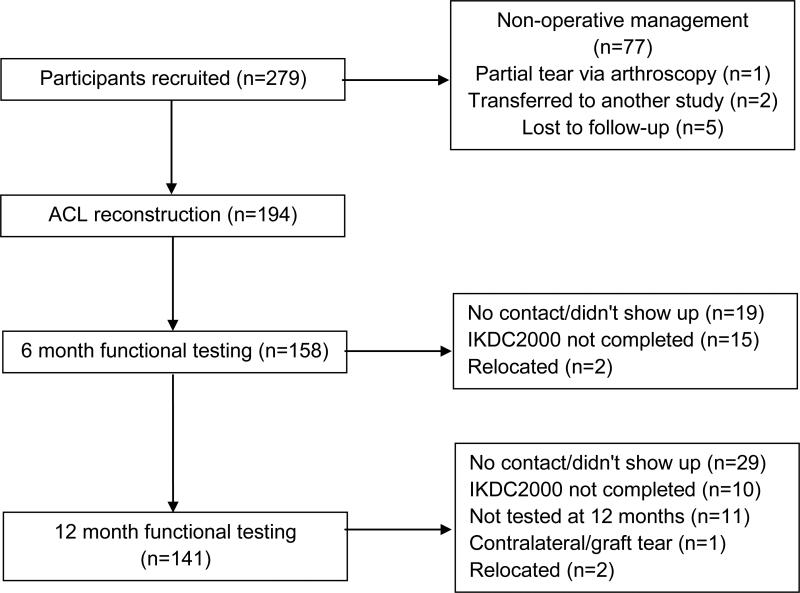
Of the 279 potential participants included in this study, 77 chose not to undergo reconstructive surgery (FIGURE). In addition, 5 participants were lost to follow-up and we were unable to determine if they had undergone ACL reconstruction; 1 participant did not have ACL surgery due to a partial tear of the ACL identified during arthroscopy, and; 2 participants transferred to another study. Therefore, 194 participants underwent reconstructive surgery, and comprise the target population in this study.
FIGURE.
Flow diagram for participants in the study. Abbreviations: ACL, anterior cruciate ligament; IKDC2000, International Knee Documentation Committee 2000 subjective knee form
Of the 194 participants who underwent ACL reconstruction, 158 (81.4%; 92 men and 66 women ranging from 13 to 56 [mean ±SD, 26.9 ±9.7] years of age) performed 6 month and 141 (72.7%) performed 12 month functional testing (FIGURE). Pregnancy, rupture of ACL graft or contralateral ACL, or missed appointments accounted for the majority of missing data. Six months after ACL reconstruction, the mean ± SD IKDC2000 score for the 158 participants was 82.4 −12.8. Twelve months after ACL reconstruction, the mean IKDC2000 score for the 141 participants was 90.4 ± 10.7.
Six months after ACL reconstruction, 82 (51.9%) participants were classified as having self-reported knee function within normal ranges. The remaining 76 (48.1%) participants were classified as having self-reported knee function below normal ranges. Among the 76 participants with IKDC2000 scores below normal ranges, 69 (90.8%) failed the RTAC test battery (P<.001). However, of the 82 participants whose IKDC2000 scores were within normal limits at 6 months, only 39 (47.6%) passed the RTAC test battery (P=.74). Self-reported knee function had a sensitivity of 61.6%, specificity of 84.8%, PLR of 4.1, and NLR of 0.5 (TABLE 3). Participants who were classified as having self-reported knee function within normal ranges based on their IKDC2000 score at the 6-month testing had significantly higher QI, LSI for all 4 single-legged hop tests, and self-reported outcome scores on the KOS-ADLS and GRS than those with self-reported knee function below normal ranges (P<.001) (TABLE 4). Of the 158 participants who completed 6 month functional testing, men more frequently reported knee function within normal ranges based on their IKDC2000 score than women (P<.001), but no significant differences were seen in mean age or time from surgery to testing (TABLE 5).
TABLE 3.
Discriminatory profile between IKDC2000 score cutoffs and success cutoffs on RTAC 6 months after ACL reconstruction
| Measures | Accuracy | 95% Confidence Interval |
|---|---|---|
| Sensitivity | 61.6% | 50.7, 72.5% |
| Specificity | 84.8% | 77.0, 92.6% |
| Positive predictive value | 90.8% | 85.4, 96.2% |
| Negative predictive value | 47.6% | 33.1, 62.0% |
| Positive likelihood ratio | 4.1 | 2.0, 8.1 |
| Negative likelihood ratio | 0.5 | 0.4, 0.6 |
Abbreviation: IKDC2000, International Knee Documentation Committee 2000 subjective knee form; RTAC: Return to Activity Criteria; ACL: anterior cruciate ligament
TABLE 4.
Performance-based and patient-reported outcome measures after ACL reconstruction.*
| RTAC | IKDC2000 scores | |||
|---|---|---|---|---|
| Knee function below normal ranges | Knee function within normal ranges | P-value | Effect size | |
| 6 months postoperative | ||||
| Quadriceps index (%) | 80.4 (67.3, 88.9) | 94.3 (85.6, 102.1) | <.001 | 0.46 |
| Single hop for distance LSI (%) | 89.9 (79.5, 96.6) | 95.1 (90.2, 99.6) | <.001 | 0.31 |
| Cross-over hop for distance LSI (%) | 90.7 (81.5, 95.4) | 97.1 (92.2, 101.4) | <.001 | 0.43 |
| Triple hop for distance LSI (%) | 91.3 (83.0, 96.5) | 97.0 (92.4, 100.1) | <.001 | 0.39 |
| 6-m timed hop LSI (%) | 92.3 (87.3, 98.3) | 97.3 (93.7, 102.1) | <.001 | 0.35 |
| KOS-ADLS (%) | 89.6 (81.4, 94.3) | 97.1 (94.3, 99.0) | <.001 | 0.59 |
| GRS (%) | 80.0 (70.5, 90.0) | 95.0 (90.0, 99.0) | <.001 | 0.61 |
| IKDC2000 | 74.7 (65.8, 80.5) | 92.0 (86.2, 96.5) | <.001 | 0.78 |
| 12 months postoperative | ||||
| Quadriceps index (%) | 92.3 (82.3, 100.2) | 94.1 (89.1, 101.9) | .054 | 0.16 |
| Single hop for distance LSI (%) | 92.3 (85.4, 100.0) | 98.0 (93.0, 102.0) | .026 | 0.20 |
| Cross-over hop for distance LSI (%) | 92.7 (84.8, 99.5) | 97.9 (93.1, 102.0) | .005 | 0.25 |
| Triple hop for distance LSI (%) | 96.0 (88.3, 99.7) | 98.0 (95.0, 101.1) | .049 | 0.18 |
| 6-m timed hop LSI (%) | 94.7 (90.5, 98.2) | 98.0 (95.0, 102.6) | .003 | 0.26 |
| KOS-ADLS (%) | 90.0 (81.0, 94.3) | 97.1 (94.3, 100.0) | <.001 | 0.52 |
| GRS (%) | 90.0 (79.0, 95.0) | 98.0 (95.0, 100.0) | <.001 | 0.48 |
| IKDC2000 | 79.0 (72.4, 83.9) | 95.4 (91.0, 98.8) | <.001 | 0.69 |
Abbreviations: ACL, anterior cruciate ligament; RTAC: Return to Activity Criteria; LSI: Limb Symmetry Index; KOS-ADLS, Knee Outcome Survey-Activities of Daily Living Scale; GRS, Global Rating Scale of Perceived Function; IKDC2000, International Knee Documentation Committee 2000 subjective knee form
Data are Medians (25%, 75% quartiles)
TABLE 5.
Demographics of participants with self-reported knee function within and below normal ranges based on the IKDC2000 scores.*
| Knee function below normal ranges | Knee function within normal ranges | P-value | |
|---|---|---|---|
| 6 month postoperative | |||
| Women/Men (N) | 47/29 | 19/63 | <.001 |
| Age (years) | 23.0 (18.0, 28.1) | 24.6 (18.6, 36.0) | .09 |
| Time from surgery (weeks) | 26.0 (25.2, 27.0) | 26.3 (25.6, 27.8) | .17 |
| 12 month postoperative | |||
| Women/Men (N) | 13/18 | 49/61 | .84 |
| Age (years) | 23.0 (18.0, 27.9) | 24.0 (17.9, 33.0) | .71 |
| Time from surgery (weeks) | 52.0 (52.0, 54.0) | 53.0 (52.0, 54.6) | .20 |
Abbreviation: IKDC2000, International Knee Documentation Committee 2000 subjective knee form
Data are Medians (25%, 75% quartiles) except for women/men
Twelve months after ACL reconstruction, 110 (78.0%) participants were classified as having patient-reported knee function within normal ranges. The remaining 31 (22.0%) participants were classified as having knee function below normal ranges. Among the 31 participants with IKDC2000 scores below normal ranges, 25 (80.6%) failed the RTAC test battery (P<.001). However, among the 110 participants whose IKDC2000 scores were within normal limits at 12 months, only 68 (61.8%) passed the RTAC test battery (P=.017). Self-reported knee function had a sensitivity of 37.3%, specificity of 91.9%, PLR of 4.6, and NLR of 0.7 (TABLE 6). Participants who were classified as having self-reported knee function within normal ranges at the 12-month testing had significantly higher single-legged hop indexes, and patient-reported outcome scores on the KOS-ADLS and GRS than those with patient-reported knee function below normal ranges based on the IKDC2000 scores (TABLE 4). Of the 141 participants who completed 12 month functional testing, no significant differences were seen in the number of men and women reporting normal knee function based on the IKDC2000, mean age or time from surgery to testing (TABLE 5).
TABLE 6.
Discriminatory profile between IKDC2000 score cutoffs and success cutoffs on RTAC 12 months after ACL reconstruction
| Measures | Accuracy | 95% Confidence Interval |
|---|---|---|
| Sensitivity | 37.3% | 20.3, 54.3% |
| Specificity | 91.9% | 86.8, 97.0% |
| Positive predictive value | 80.7% | 71.2, 90.1% |
| Negative predictive value | 61.8% | 50.8, 72.9% |
| Positive likelihood ratio | 4.6 | 2.0, 10.5 |
| Negative likelihood ratio | 0.7 | 0.6, 0.8 |
Abbreviation: IKDC2000, International Knee Documentation Committee 2000 subjective knee form; RTAC: Return to Activity Criteria; ACL: anterior cruciate ligament
DISCUSSION
The primary findings in the current study partially support the hypothesis that self-reported knee function assessed with the IKDC2000 can discriminate between successful and non-successful performance on a battery of tests used for RTAC after ACL reconstruction. We have demonstrated that for IKDC2000 scores reported 6 and 12 months after ACL reconstruction, low IKDC2000 scores is a reasonable indicator of failure on RTAC. Patients with low IKDC scores were more likely to fail RTAC than patients with normal IKDC scores. However, normal IKDC2000 scores is not predictive of successfully passing RTAC. Patients with normal knee function were no more likely to pass RTAC than patients with poor knee function. The data also indicate that overall, participants with self-reported knee function within normal ranges using the IKDC200 had significant higher limb symmetry indexes and patient-reported outcome scores than participants with self-reported knee function below normal ranges. But this is not an indicator of successfully passing RTAC. In fact, many of those patient who had normal IKDC2000 scores were not able to pass RTAC at 6 or 12 months after ACL reconstruction. Therefore the decision making for return to activities cannot be solely predicated on normal IKDC2000 scores. If an athlete self-reports a low IKDC2000 score, she is likely to perform poorly on the RTAC test battery and not pass the RTAC. Using the information from the results of the RTAC test battery can then determine what areas are deficient. Subsequently, if an athlete self-reports a normal IKDC2000 score, she is likely to perform better on the RTAC test battery but it cannot predict if she will pass the RTAC.
The IKDC2000 may be a clinically relevant questionnaire to determine the timeliness or necessity of RTAC testing. Six months after ACL reconstruction, participants with self-reported knee function below normal ranges were more than 4 times more likely to have failed RTAC than those participants with self-reported knee function within normal ranges. By 12 months, participants with self-reported knee function below normal ranges were more than 4.5 times more likely to have failed RTAC than those participants with self-reported knee function within normal ranges. The IKDC2000 is highly specific, and thus if the athlete reports self-reported knee function below normal ranges, the athlete will likely fail RTAC. Furthermore, the limitations of using the below normal IKDC2000 values as a surrogate measure for RTAC failure is that the specific impairments or activity limitations which lead to failure cannot be gleaned from the IKDC2000 alone. The administration of RTAC test battery can be used to determine which factors need to be addressed and further interventions to be implemented.
The reporting of normal knee function may not be a good indicator of the ability to pass RTAC. At 6 months after ACL reconstruction, participants with self-reported knee function within normal ranges were only twice more likely to have passed RTAC than those participants with self-reported knee function below normal ranges. At 12 months after ACL reconstruction, participants with self-reported knee function within normal ranges were less than 1.5 times more likely to have passed RTAC than those participants with self-reported knee function below normal ranges. Due to its low negative likelihood ratio, the independent use of IKDC2000 as a screening tool is not justified. Furthermore, the self-reporting of normal IKDC2000 scores does not reflect successful performance on the RTAC test battery. Many patients (38%) may overestimate their functional ability despite self-reporting normal knee function. The relatively low relationship between normal IKDC2000 scores and passing RTAC may indicate that each method captures different domains of physical performance and knee function, especially when patient are self-reporting normal knee function. Fitzgerald et al20 summarized the low correlations between hop tests scores and self-reported knee questionnaires. In contrast, in a previous study with the patients from the same cohort, the crossover hop test could predict patients with future normal knee function.37 We are currently exploring the relationships with the performance-based measures with the activity-specific questions on the IKDC2000. This may elucidate the relationship between performance-based measures and specific domains of activities with the IKDC2000. Therefore, if an athlete reports self-reported knee function within normal ranges, the clinician cannot assume that the athlete will pass RTAC.
The RTAC employs a group of tests that assess multiple domains of side-to-side comparisons and global knee function: impairments, performance-based measures, patient-reported outcomes.6, 20, 23, 31, 57 To pass the RTAC, athletes must score greater than or equal to 90% on all 7 tests (TABLE 1). These cut-off scores assure that an acceptable level of limb-to-limb symmetry is present before returning to activities or sport so participants must be confident in the function of their involved limb and favor it less during functional activities.25 It is noteworthy that a substantial percentage of athletes 6 and 12 months post ACL reconstruction still demonstrate self-reported knee function below normal values and asymmetrical performance on functional testing. These limb asymmetries and lower patient-reported outcomes may be indicative of inadequate or incomplete rehabilitation. Using the RTAC test battery, clinicians can identify the modifiable factors that can be readily addressed to develop targeted interventions to potentially improve knee function and performance.
The criteria used in this study incorporate both performance-based and patient-reported outcomes, capturing clinically important aspects of overall knee performance and function.6, 20, 21, 31 In a previous report, on a similar cohort, athletes who failed our RTAC 6 months after ACL reconstruction exhibited greater limb-to-limb biomechanical movement asymmetries than those who passed our RTAC.21 Specifically, athletes who failed RTAC demonstrated smaller peak knee flexion angles and lower extensor moments on the involved knee.21 After ACL reconstruction, athletes with side-to-side biomechanical movement asymmetries are more likely to sustain a second ACL injury than those with more symmetrical movements.48 The restoration of symmetrical function between limbs remains an important goal of post-operative ACL rehabilitation. Sports-specific activities are more challenging than clinic-based testing in a controlled environment; therefore the deficits seen in a clinical test battery may be magnified in sports-specific activities, potentially predisposing the ipsilateral or contralateral knee to injury.
The IKDC2000 is frequently used as an outcome measure for knee function.11, 22, 34 After ACL reconstruction, slightly more than half of the athletes in the current study self-reported knee function within normal ranges 6 months after ACL reconstruction, and 78% self-reported knee function within normal ranges 12 months after surgery, similar to findings reported by Hartigan et al.25. Beynnon et al7 reported that more than 77% of participants had normal or nearly normal knee function based on the IKDC2000 6 months after surgery. Others have found similar outcomes at 12 months with 79 to 93% of participants exhibiting normal or nearly normal knee function.4, 8, 34
The current findings show that 6 months after ACL reconstruction participants with IKDC2000 scores below normal ranges had significantly lower QI than those with IKDC2000 scores within normal ranges. By 12 months after ACL reconstruction, patients with lower IKDC2000 scores had similar QI values compared to those with normal IKDC2000 scores, demonstrating improvement in the strength of the quadriceps muscle in the poorer functioning group. However, in those patients with normal IKDC2000 scores, at 6 months only 49.4% and at 12 months 67.4% of participants had QI values greater than 90%. Recovery of quadriceps strength is an important outcome following ACL reconstruction,13, 30, 51, 52, 54 but deficits as high as 39% are seen 6 months after ACL reconstruction.47 Quadriceps strength is significantly related to patient satisfaction and knee function during gait.36, 51, 56 Athletes cleared to return to sports after ACL reconstruction with a QI less than 85% had lower IKDC2000 scores than athletes with QI greater than 90% and controls.55 The identification and treatment of quadriceps weakness after ACL reconstruction may contribute to the resolution of knee function and the ability to successfully pass RTAC.
Our results 6 and 12 months after ACL reconstruction showed that all 4 hop indexes were lower in participants with self-reported knee function below normal ranges compared to those with self-reported knee function within normal ranges. In their study, Myer et al41 reported a mean LSI scores in athletes within 1 year of reconstruction in the 4 hop tests that exceeded 90% but were still lower compared to healthy controls. In our study, the group median values in both groups at both testing sessions for the four hop limb symmetry indexes were at or exceeded the 90% cut-off values needed to pass the RTAC test battery (TABLE 4). However, in those patients with normal IKDC2000 scores, at 6 months only 53.2% and at 12 months, 78.7% of participants exceeded 90% on all 4 hop tests. The findings in this study reinforce the point that despite self-reporting IKDC2000 scores within normal ranges, it is highly recommended that a test battery that identifies limb-to-limb asymmetries is needed.
Scores on the patient-reported measures included in the test battery for RTAC (KOSADLS and GRS) at both testing sessions were significantly lower in the participants with self-reported knee function below normal ranges assessed with the IKDC 2000 compared to the athletes with self-reported knee function within normal ranges. Previous work from our laboratory indicated that noncopers who failed RTAC did so because of lower GRS scores.25 The KOS-ADLS and GRS self-report measures complement the impairment (quadriceps strength) and performance-based measures (hop tests) by providing valuable information on how a participant perceives his or her function. Participants must be able to perform their activities of daily living at a normal level prior to attempting returning to sports. If participants report difficulty with daily activities, they are likely to report having difficulty with sporting activities, placing themselves at risk for subpar performance and re-injury.
Limitations
The inability to pass RTAC may be the result of several factors not captured by IKDC2000 scores. The participants in this study were young and active and the results may therefore not apply to other populations. This study had some incomplete data due to unforeseeable circumstances. A portion of participants did not complete either 6-month or 12-month testing, reducing the participants available for analysis. One potential bias is that those that did not complete the study may be inherently different from those that did. Some patients may have not shown up due to either the patient's knee function was not improving or that the patient was doing so well and decided not to return. The results can only be generalized to those with isolated ACL injuries or asymptomatic concomitant injuries and may not reflect the functional status of individuals with symptomatic concomitant injuries. The hop test battery was administered in the same fashion each session and may not be generalized to different hop test paradigms.
CONCLUSION
Six and 12 months after surgery, low IKDC2000 function scores were reasonably indicative of RTAC test battery failure, whereas normal IKDC2000 scores were not predictive of passing scores on the RTAC test battery. In general, patients with lower IKDC2000 scores had lower scores on the RTAC test battery. The decision making for return to activities cannot be solely predicated on normal IKDC2000 scores. The administration of RTAC test battery can be used to determine which factors need to be addressed and further interventions to be implemented.
KEY POINTS.
FINDINGS: For scores obtained at 6 and 12 months after surgery, low IKDC2000 function scores were reasonably indicative of RTAC test battery failure, whereas normal IKDC2000 scores were not predictive of passing scores on the RTAC test battery.
IMPLICATIONS: The IKDC2000 is not sufficient to make a decision on return to activity and that a RTAC test battery should be implemented.
CAUTION: The results can only be generalized to young and active Level I/II athletes with isolated ACL injuries or asymptomatic concomitant injuries.
Acknowledgments
We acknowledge the Norwegian Sport Medicine Clinic, Nimi (www.nimi.no), for supporting the Norwegian Research Center for Active Rehabilitation (NAR) (www.active-rehab.no) with rehabilitation facilities and research staff. We thank physical therapists Håvard Moksnes, Annika Storevold, Ida Svege, Espen Selboskar, Karin Rydevik, and Marte Lund for their assistance with data collection. We thank Airelle Hunter-Giordano, Angela Smith, the University of Delaware Physical Therapy Clinic (http://www.udptclinic.com) and physical therapists with their assistance in the data collection of this study. We acknowledge Martha Callahan and DRI Clinical Research Core (http://www.udel.edu/dri/ResCore.html) for their assistance with participant scheduling and data organization.
This work was supported in full/part by National Institutes of Health (NIH R37 HD37985; P30 GM103333) and Promotional of Doctoral Studies scholarships from the Foundation for Physical Therapy.
The study protocol was approved by the Ethical/Human Subjects committees at the University of Delaware and Regional Ethics Committee for South-Eastern Norway and conducted within the guidelines given by the Helsinki declaration.
Footnotes
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in this article.
References
- 1.Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. The American journal of sports medicine. 2010;38:1334–1342. doi: 10.1177/0363546510361218. [DOI] [PubMed] [Google Scholar]
- 2.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. The American journal of sports medicine. 2006;34:128–135. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. British journal of sports medicine. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 4.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. The American journal of sports medicine. 2011;39:538–543. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 5.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. The American journal of sports medicine. 1995;23:694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 6.Bent NP, Wright CC, Rushton AB, Batt ME. Selecting outcome measures in sports medicine: a guide for practitioners using the example of anterior cruciate ligament rehabilitation. British journal of sports medicine. 2009;43:1006–1012. doi: 10.1136/bjsm.2009.057356. [DOI] [PubMed] [Google Scholar]
- 7.Beynnon BD, Uh BS, Johnson RJ, et al. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. The American journal of sports medicine. 2005;33:347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 8.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta- analysis of functional scores. Clinical orthopaedics and related research. 2007;458:180–187. doi: 10.1097/BLO.0b013e31803dcd6b. [DOI] [PubMed] [Google Scholar]
- 9.Bjorklund K, Andersson L, Dalen N. Validity and responsiveness of the test of athletes with knee injuries: the new criterion based functional performance test instrument. Knee Surg Sports Traumatol Arthrosc. 2009;17:435–445. doi: 10.1007/s00167-008-0674-z. [DOI] [PubMed] [Google Scholar]
- 10.Bolgla LA, Keskula DR. Reliability of lower extremity functional performance tests. The Journal of orthopaedic and sports physical therapy. 1997;26:138–142. doi: 10.2519/jospt.1997.26.3.138. [DOI] [PubMed] [Google Scholar]
- 11.Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. The Journal of orthopaedic and sports physical therapy. 2008;38:746–753. doi: 10.2519/jospt.2008.2887. [DOI] [PubMed] [Google Scholar]
- 12.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. The American journal of sports medicine. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 13.de Jong SN, van Caspel DR, van Haeff MJ, Saris DB. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21–28. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 14.Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. The American journal of knee surgery. 2001;14:85–91. [PubMed] [Google Scholar]
- 15.Delitto A, Rose SJ, McKowen JM, Lehman RC, Thomas JA, Shively RA. Electrical stimulation versus voluntary exercise in strengthening thigh musculature after anterior cruciate ligament surgery. Physical therapy. 1988;68:660–663. doi: 10.1093/ptj/68.5.660. [DOI] [PubMed] [Google Scholar]
- 16.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A Progressive 5-Week Exercise Therapy Program Leads to Significant Improvement in Knee Function Early After Anterior Cruciate Ligament Injury. The Journal of orthopaedic and sports physical therapy. 2010;40:705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8:76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 18.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Physical therapy. 2000;80:128–140. [PubMed] [Google Scholar]
- 19.Fitzgerald GK, Axe MJ, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. The Journal of orthopaedic and sports physical therapy. 2000;30:194–203. doi: 10.2519/jospt.2000.30.4.194. [DOI] [PubMed] [Google Scholar]
- 20.Fitzgerald GK, Lephart SM, Hwang JH, Wainner RS. Hop tests as predictors of dynamic knee stability. The Journal of orthopaedic and sports physical therapy. 2001;31:588–597. doi: 10.2519/jospt.2001.31.10.588. [DOI] [PubMed] [Google Scholar]
- 21.Flanigan DC, Everhart JS, Pedroza A, Smith T, Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1322–1329. doi: 10.1016/j.arthro.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 22.Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self- reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. The American journal of sports medicine. 2011;39:2347–2354. doi: 10.1177/0363546511417085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gustavsson A, Neeter C, Thomee P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:778–788. doi: 10.1007/s00167-006-0045-6. [DOI] [PubMed] [Google Scholar]
- 24.Hambly K, Griva K. IKDC or KOOS: which one captures symptoms and disabilities most important to patients who have undergone initial anterior cruciate ligament reconstruction? The American journal of sports medicine. 2010;38:1395–1404. doi: 10.1177/0363546509359678. [DOI] [PubMed] [Google Scholar]
- 25.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to- sports criteria after anterior cruciate ligament reconstruction. The Journal of orthopaedic and sports physical therapy. 2010;40:141–154. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 27.Hopper DM, Goh SC, Wentworth LA, et al. Test-retest reliability of knee rating scales and functional hop tests one year following anterior cruciate ligament reconstruction. Phys Ther in Sport. 2002;3:10–18. [Google Scholar]
- 28.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. The American journal of sports medicine. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 29.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. The Journal of bone and joint surgery. 1998;80:1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. The Knee. 2001;8:229–234. doi: 10.1016/s0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 31.Keskula DR, Duncan JB, Davis VL, Finley PW. Functional outcome measures for knee dysfunction assessment. Journal of athletic training. 1996;31:105–110. [PMC free article] [PubMed] [Google Scholar]
- 32.Kiesel K, Plisky PJ, Voight ML. Can Serious Injury in Professional Football be Predicted by a Preseason Functional Movement Screen? N Am J Sports Phys Ther. 2007;2:147–158. [PMC free article] [PubMed] [Google Scholar]
- 33.Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. The Journal of bone and joint surgery. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 34.Kowalchuk DA, Harner CD, Fu FH, Irrgang JJ. Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:457–463. doi: 10.1016/j.arthro.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports medicine (Auckland, N.Z. 2004;34:269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 36.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clinical biomechanics (Bristol, Avon) 2002;17:56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 37.Logerstedt D, Grindem H, Lynch A, et al. Single-legged Hop Tests as Predictors of Self- reported Knee Function After Anterior Cruciate Ligament Reconstruction: The Delaware-Oslo ACL Cohort Study. The American journal of sports medicine. 2012;40:2348–2356. doi: 10.1177/0363546512457551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lord JP, Aitkens SG, McCrory MA, Bernauer EM. Isometric and isokinetic measurement of hamstring and quadriceps strength. Archives of physical medicine and rehabilitation. 1992;73:324–330. doi: 10.1016/0003-9993(92)90004-g. [DOI] [PubMed] [Google Scholar]
- 39.Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: A 10-year study. The Knee. 2006;13:184–188. doi: 10.1016/j.knee.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 40.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 41.Myer GD, Schmitt LC, Brent JL, et al. Utilization of Modified NFL Combine Testing to Identify Functional Deficits in Athletes Following ACL Reconstruction. The Journal of orthopaedic and sports physical therapy. 2011;41:377–387. doi: 10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. British journal of sports medicine. 2005;39:127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Myklebust G, Holm I, Maehlum S, Engebretsen L, Bahr R. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. The American journal of sports medicine. 2003;31:981–989. doi: 10.1177/03635465030310063901. [DOI] [PubMed] [Google Scholar]
- 44.Neeter C, Gustavsson A, Thomee P, Augustsson J, Thomee R, Karlsson J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:571–580. doi: 10.1007/s00167-006-0040-y. [DOI] [PubMed] [Google Scholar]
- 45.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. The American journal of sports medicine. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 46.Ott SM, Ireland ML, Ballantyne BT, Willson JD, McClay Davis IS. Comparison of outcomes between males and females after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2003;11:75–80. doi: 10.1007/s00167-003-0348-9. [DOI] [PubMed] [Google Scholar]
- 47.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clinics in sports medicine. 2008;27:405–424, vii-ix. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 48.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. The American journal of sports medicine. 2010;38:1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Physical therapy. 2007;87:337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 50.Risberg MA, Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. The American journal of sports medicine. 2009;37:1958–1966. doi: 10.1177/0363546509335196. [DOI] [PubMed] [Google Scholar]
- 51.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. The Journal of orthopaedic and sports physical therapy. 1999;29:400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 52.Ross MD, Irrgang JJ, Denegar CR, McCloy CM, Unangst ET. The relationship between participation restrictions and selected clinical measures following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2002;10:10–19. doi: 10.1007/s001670100238. [DOI] [PubMed] [Google Scholar]
- 53.Ross MD, Langford B, Whelan PJ. Test-retest reliability of 4 single-leg horizontal hop tests. Journal of strength and conditioning research / National Strength & Conditioning Association. 2002;16:617–622. [PubMed] [Google Scholar]
- 54.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. The Journal of orthopaedic and sports physical therapy. 2013;42:750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schmitt LC, Quatman CE, Paterno MV, Best TM, Flanigan DC. Functional Outcomes After Surgical Management of Articular Cartilage Lesions in the Knee: A Systematic Literature Review to Guide Post-Operative Rehabilitation. The Journal of orthopaedic and sports physical therapy. 2014:1–53. doi: 10.2519/jospt.2014.4844. [DOI] [PubMed] [Google Scholar]
- 56.Snyder-Mackler L, Delitto A, Bailey SL, Stralka SW. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. The Journal of bone and joint surgery. 1995;77:1166–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 57.Thomee R, Neeter C, Gustavsson A, et al. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012 doi: 10.1007/s00167-012-1912-y. [DOI] [PubMed] [Google Scholar]
- 58.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Annals of the rheumatic diseases. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]