Abstract
Objective
It is possible that disturbances of systems modulating reward may contribute to a vulnerability to develop an eating disorder.
Method
This hypothesis was tested by assessing functional magnetic resonance brain imaging response to a monetary reward task known to activate the anterior ventral striatum (AVS), a region implicated in motivational aspects toward stimuli. To avoid the confounding effects of malnutrition, 10 women who had recovered from bulimia nervosa (BN) were compared with 10 healthy comparison women (CW).
Results
For the AVS, CW distinguished positive and negative feedback, whereas recovered BN women had similar responses to both conditions. In addition, these groups had similar patterns of findings for the dorsal caudate.
Discussion
We have previously shown that individuals recovered from anorexia nervosa (AN) also had altered striatal responses and difficulties in differentiating positive and negative feedback. Thus BN and AN individuals may share a difficulty in discriminating the emotional significance of a stimulus.
Keywords: bulimia nervosa, magnetic resonance imaging, reward, recovery, striatum
Introduction
Bulimia nervosa (BN), a disorder of unknown etiology, most commonly has its onset in adolescent females and is characterized by body image distortions and mood and impulse control dysregulation.1 Typically episodes of overeating are followed by compensatory behaviors such as vomiting, fasting, misuse of laxatives, or overexercising. In addition, individuals with BN tend to be impulsive and sensation seeking and often abuse alcohol and drugs.2,3 Considerable data in the past decade has raised the possibility that disturbed appetitive behaviors for food and drugs may reflect a dysregulation of reward mechanisms.4
Few studies have investigated the neurobiology of reward in BN. In contrast, it has been found that anorexia nervosa (AN), a related disorder characterized by restrictive eating and an ascetic temperament, have altered striatal dopamine (DA) function.5,6 The DA system is thought to contribute to an optimal response to reward stimuli.7 Altered DA function has been reported in individuals with binge-eating behavior, for example, altered allele frequencies for the DA transporter gene (DAT1)8 and DA receptor genes.9,10
To assess striatal response to reward in AN, our group11 used a monetary reward task with event-related functional magnetic resonance imaging (fMRI). To avoid the confounding effects of malnutrition, we focused upon individuals recovered from restricting-type AN (REC AN). REC AN showed increased hemodynamic activation in the caudate nucleus (CN). Although control women (CW) distinguished positive and negative feedback within the anterior ventral striatum (AVS), REC AN women had similar responses to both conditions. Based on the functional gradient of inputs to the striatum, this pattern of activation may imply that REC AN are impaired in identifying the emotional significance of a stimulus (lack of differential signal to win/loss in the AVS), but increased traffic in neurocircuits concerned with planning and consequences (enhanced activation in dorsostriatal circuits through the CN). Because there is little data on DA function or other aspects of reward in BN, we performed this pilot study in order to explore striatal response to this task in women recovered from BN (REC BN). We hypothesized that BN women would have an opposite CN response. That is, they would have reduced CN activation consistent with a reduced ability to plan or foresee consequences.
Method
Sample
Ten REC BN women were recruited who had previously met DSM-IV criteria for BN. They were previously treated in the eating disorder treatment program at Western Psychiatric Institute and Clinic (University of Pittsburgh Medical Center), Pittsburgh, PA or were recruited nationally through advertisements. All individuals underwent four levels of screening: (1) a brief phone screening; (2) an intensive screening assessing psychiatric history, lifetime weight, binge eating and methods of weight loss/control, and menstrual cycle history as well as eating pattern for the past 12 months; (3) a comprehensive assessment using structured and semi-structured psychiatric interviews conducted by phone or in person; and (4) a face-to-face interview and physical examination with a psychiatrist. To be considered ‘‘recovered,’’ for the previous year individuals had to1 maintain a weight above 90% of average body weight2; have regular menstrual cycles3; have not binged, purged, restricted food intake, or exercised excessively4; not used psychoactive medications such as antidepressants. Also, they must have not used psychoactive medications nor met criteria for alcohol or drug abuse or dependence, major depressive disorder, or severe anxiety disorder within 3 months of the study. Forty-seven CW were recruited through local advertisements. The CW had no history of an eating disorder or any psychiatric disorder, medical, or neurological illness. They had normal menstrual cycles and had been within normal weight range since menarche (above 90% of average body weight).
This study was conducted according to the institutional review board regulations of the University of Pittsburgh, and all participants gave written informed consent. The MR imaging was performed during the first 10 days of the follicular phase for all subjects to standardize phase of cycle.
Assessments
Axis I diagnoses were made using the Structured Clinical Interview for DSM-IV Axis I Disorders.12 Current symptoms were assessed using the State-Trait Anxiety Inventory Form Y13 and personality was assessed by the Temperament and Character Inventory (TCI).14 A modified form of the South Oaks Gambling survey15,16 identified participants with excessive gambling behaviors.
Guessing-Game Paradigm
The task used was developed by Delgado and described previously.11,17,18 In brief, participants guessed whether a hidden number behind a virtual playing card was greater or less than 5. The participant won $2.00 for a correct guess, lost $1.00 for every incorrect guess, and lost $0.50 if she failed to make a guess in the required time. At the beginning of each trial a question mark “?” appeared inside the virtual playing card as a cue for the participant to guess. Feedback for wins was indicated by a green up arrow, for losses by a red down arrow, and a failure to respond by a yellow down arrow. Responses were acquired via an ergonomically designed button response unit attached to the right hand. The participants were told that the computer picked numbers randomly, so that there was no way to know what number was going to be revealed. In actuality, the stimulus control program randomly preselected each trial to be a win or loss trial and presented to the participants a number that was congruent with the outcome. A total of four blocks were run, with each consisting of 26 trials (13 wins, 13 losses).
Scanning Procedures
Imaging data were collected with a 3T Signa scanner (GE Medical Systems). High-resolution anatomical images (1.5 mm3) were acquired for each subject. Additionally, T1 structural images were acquired (3.2 mm thickness, in-plane with the functional images, 36 oblique axial slices, AC-PC aligned, in-plane resolution of 0.78 mm2, and with a field of view of 200 mm2). Functional images were acquired using a one-shot reverse spiral pulse sequence19 with TE = 26 ms and TR = 2000 ms; 30 oblique axial slices were acquired with an in-plane resolution of 64 × 64 with 3.125 mm2 pixels and a slice thickness of 3.2 mm, with a field of view of 200 mm2. Seven functional volumes were acquired per trial.
Data Processing and Analysis
The data preprocessing for the Regions of Interest (ROI)-based analyses were performed by NeuroImaging Software (NIS; http://kraepelin.wpic.pitt.edu/nis/), Automated Image Registration (AIR20) and Analysis of Functional NeuroImages (AFNI21), and Statistical Parametric Mapping (SPM222). Functional MRI data were preprocessed with slice-time correction (AFNI-3dtshift), motion correction using 6-parameter algorithm (AIR), high-pass filtering (AFNI-3dfourier, 0.024 Hz), a between-block baseline correction, and a within-block linear detrend (NIS, four standard deviation correction for outliers). Each subject’s brain was registered to the Montreal Neurologic Institute (MNI) reference brain (ftp://ftp.mrc-cbu.cam.ac.uk/pub/imaging/Colin/) and smoothed (6.25 × 6.25 × 6.4 mm full with half maximum (FWHM)) using SPM2.
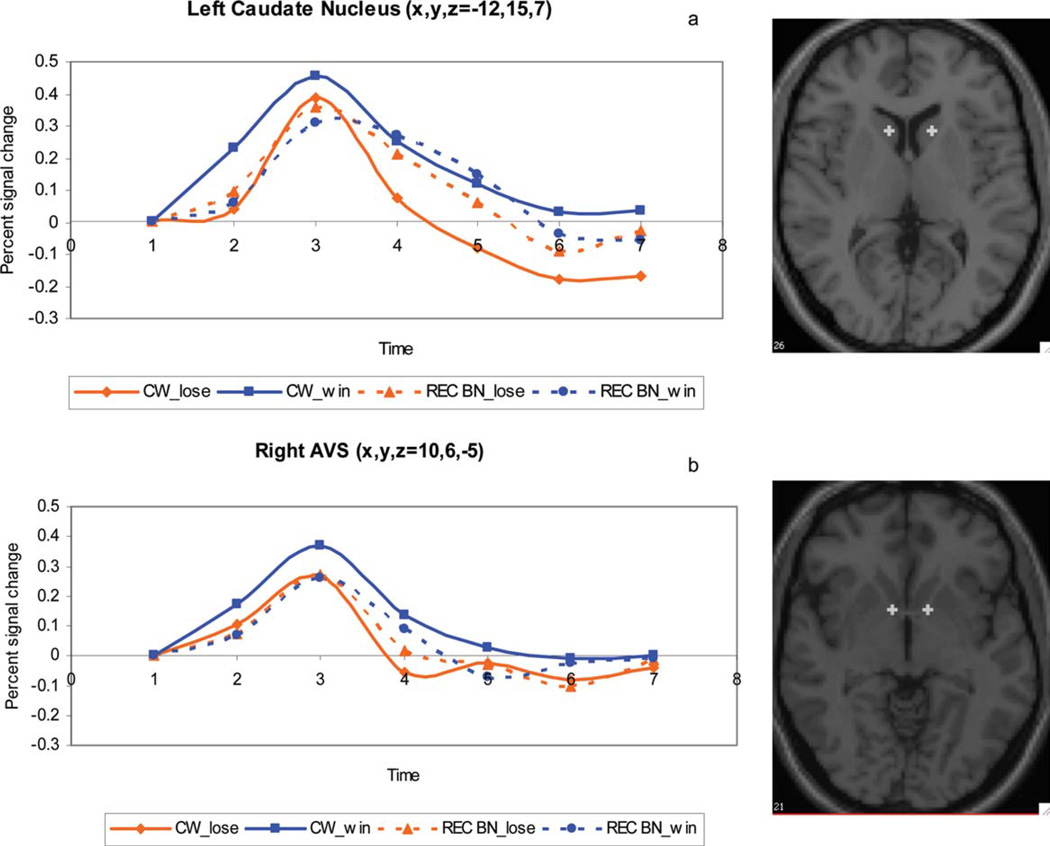
The ROI-Based Analysis (Table 2, Fig. 1) focused on the caudate and ventral striatal regions previously identified in healthy controls by Delgado15,18 for this task. The talairach coordinates for three striatal regions were: left caudate nucleus (−12, 15, 7), right caudate nucleus (11, 16, 7), and left ventral striatum (−10, 6, 25). We also included the right ventral striatum (10, 6, −5). We extracted the mean signal in a 3.2 mm radius (1 voxel radius) sphere centered at these talairach coordinates. The time-course of the BOLD response within each ROI was transformed to a percent change from baseline (T01) for visual inspection and interpretation. The time-series were subjected to a 3-way ANOVA with group as a between-subjects factor (2 levels), outcome (win or loss) as a within-subjects factor (2 levels), and time (time-points T01-T07) as a repeated measures factor (7 levels). The ANOVAR was a fully saturated model with subject interactions combined with error.
TABLE 2.
ANOVA statistics for comparisons between the groups (women recovered from bulimia nervosa versus controls), and the interactions between group and condition (loss versus win), group and time (time course of trial), and group, condition, and time
| Group*Condition |
Group*Time |
Condition*Time |
Group*Condition *Time |
|||||
|---|---|---|---|---|---|---|---|---|
| F Ratio | p | F Ratio | p | F Ratio | p | F Ratio | p | |
| Left caudate nucleus | 12.92 | 0.0021 | 1.59 | 0.1572 | 1.32 | 0.2535 | 0.60 | 0.7285 |
| Right caudate nucleus | 2.96 | 0.1026 | 1.72 | 0.1227 | 1.30 | 0.2622 | 0.57 | 0.7526 |
| Left ventral striatum | 5.30 | 0.0334 | 0.40 | 0.8771 | 0.36 | 0.9049 | 0.33 | 0.9211 |
| Right ventral striatum | 1.26 | 0.2764 | 0.21 | 0.9727 | 0.41 | 0.8726 | 0.13 | 0.9923 |
FIGURE 1.
Time course of BOLD signal as a mean percent signal change (from first scan per trial) over all 10 recovered bulimia nervosa subjects (REC BN) and 10 control women (CW) for reward-related response corresponding to (1a) Left Caudate Nucleus < –12, 15, 7> (1b) Right Ventral Striatum <10, 6, −5>. [Color figure can be viewed in the online issue, which is available at www.interscience.wiley.com.]
All clinical behavioral data analyses were performed using SPSS (14.0). To compare BN and CW groups, a nonparametric Mann Whitney-U Test was performed.
Results
Demographic Variables and Clinical Behavioral Assessments
REC BN and CW were of similar age and BMI (Table 1). REC BN had the onset of illness at 17.2 ± 3.4 years old and had been recovered for 20.6 ± 13.6 months. When compared with CW, the REC BN individuals had significantly higher values for trait anxiety and harm avoidance. Lifetime (but not current) history for the REC BN included six with major depressive disorder (MDD), eight with obsessive-compulsive disorder (OCD), two with social phobia, two with panic disorder, five with alcohol abuse/dependence, and two with drug abuse/dependence. Groups did not differ in reaction time or on choice (high or low guess) (p > 0.05, data not shown).
TABLE 1.
Demographic and eating related variables
| CW (n = 10) |
REC BN (n = 10) |
|||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | U | p-value | |
| Study age (years) | 26.3 | 4.7 | 26.6 | 5.0 | 48 | 0.9111 |
| Current BMI (kg/m2) | 22.1 | 2.2 | 22.3 | 1.5 | 45 | 0.7254 |
| High past BMI (kg/m2) | 23.2 | 2.0 | 24.5 | 2.1 | 34 | 0.2395 |
| Low past BMI (kg/m2) | 20.1 | 1.6 | 18.6 | 1.2 | 21.5 | 0.0303 |
| Age of onset (years) | 17.2 | 3.4 | ||||
| Length of recovery (months) | 20.6 | 13.6 | ||||
| BDI | 1.3 | 1.4 | 7.5 | 8.2 | 14.5 | 0.0054 |
| TCI novelty seeking | 20.9 | 5.2 | 23.1 | 8.0 | 37.5 | 0.3615 |
| TCI harm avoidance | 11.2 | 8.2 | 17.7 | 8.4 | 27.5 | 0.0910 |
| Trait anxiety | 27.1 | 4.3 | 45.2 | 12.3 | 5 | 0.0004 |
CW, healthy control women; REC BN, recovered bulimic women, BDI, beck depression inventory; TCI, temperament and character inventory; Trait anxiety, Spielberger state-trait anxiety inventory. U: Mann Whitney U Test.
ROI-Based Image Analysis
Overall, the pattern of the left CN activation was significantly different between REC BN participants when compared with CW measured by a group × condition analysis [(F = 12.92, df = 1,18, p = 0.0021) (Fig. 1a) (Table 2)]. Importantly, CW response showed a significant difference between wins and losses (left CN, p = 0.0006), whereas REC BN showed a similar response pattern.
The left AVS showed a significant group × condition (F = 5.30, df = 1,18, p = 0.0334) interaction. The time series revealed a higher peak and more sustained activation for win trials in CW when compared with REC BN individuals. Using a within group analysis, CW showed a significant difference between wins and losses (p = 0.0468) in the right AVS, whereas REC BN individuals had a similar response (p = ns; Fig. 1b).
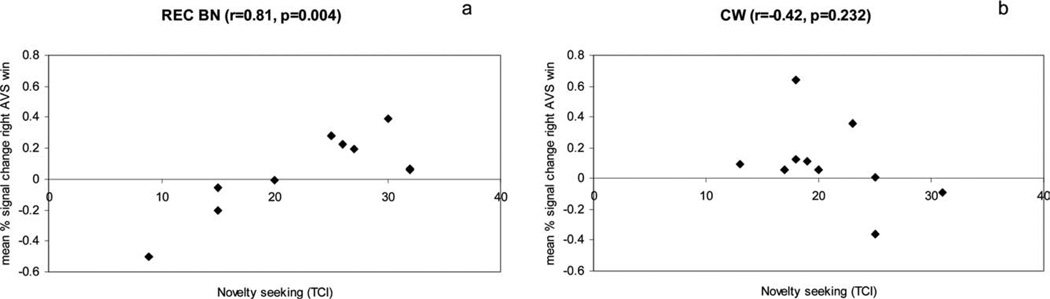
Relationship to Symptoms
The findings were unchanged in relation to age, BMI and novelty seeking scores. REC BN individuals showed a positive relationship between novelty seeking (TCI) and percent signal change in both the right (r = 0.81, p = 0.005) (Fig. 2a) and left AVS (r = 0.61, p = 0.062) for wins. Such a relationship was not detected for CW (Fig. 2b). Mean percent signal changes were not related to age of onset, length of recovery, harm avoidance or anxiety scores, depression or Axis I diagnoses.
FIGURE 2.
Correlation between novelty seeking and mean percentage signal change in the right AVS for win in REC BN (2a) and CW (2b) CW; control women, REC BN; women recovered from bulimia nervosa.
Discussion
This is the first study using fMRI to investigate reward processing in REC BN women. The CW showed a response in the AVS and dorsal striatum that distinguished positive and negative feedback. In comparison, the REC BN individuals had a similar response to positive and negative feedback.
In terms of the AVS response, the REC BN appears to be similar to the REC AN. That is, both groups revealed difficulty in discriminating between positive and negative feedback relative to healthy CW. Animal studies show that the AVS processes motivational aspects toward stimuli by modulating the influence of limbic inputs on striatal activity.23–25 Even abstract rewards (money) activate the AVS in proportion to the reward amount or the deviation from an expected payoff.26 These AVS responses to cues may reflect a failure to appropriately bind, scale, or discriminate responses to salient stimuli, supporting the possibility that REC BN and REC AN may have impaired ability to identify the emotional significance of stimuli.27
Similar to the AVS, the controls were able to distinguish between negative and positive feedback in the dorsal CN. In contrast, the REC BN individuals showed a similar response to both stimuli. The dorsal striatum includes the rostral, dorsal CN, which is involved in linking action to outcome.28,29 It is well known that many BN individuals have altered impulsivity.30 A recent study reported that behavioral/motoric impulsivity is linked to binge-eating type eating disorders in general, but that the non-planning dimension of impulsivity was only characteristic of BN individuals.31 Whether the different activity pattern finding in REC BN reflect some difficulty in foreseeing or integrating consequences is conjectural, but may offer important clues for understanding the biology this behavior. It is worth noting that our group previously found that REC AN participants had elevated CN activation in response to negative and positive feedback,11 perhaps reflecting symptoms of worrying about feedback and excessive need to control/plan consequences of their actions.
Both REC BN and REC AN individuals had elevated anxiety and harm avoidance scores, and neither group had altered novelty seeking or sensation seeking scores. In this respect, REC AN and REC BN appear to be similar. Still, novelty seeking scores were positively associated with AVS activation for the win condition within the BN group. Literature on personality in BN consistently reports high impulsivity, lack of goal direction, and sensation seeking.2,3,32 Thus, the more pronounced the personality trait of novelty seeking, the greater capacity to display a neuronal response to reward.
In terms of limitations, these data need to be interpreted cautiously due to the relatively small sample size. However, this was a relatively homogeneous BN group, because we excluded individuals with an antecedent of AN. We did not compare REC BN, REC AN, and CW due to lack of power. The time series (Fig. 1a) displayed a non significant diminished amplitude for REC BN for wins in comparison to CW (mean % signal change REC BN = 0.09 ± 0.16, mean % signal change CW = 0.16 ± 0.12). Whether REC BN have an opposite response when compared with REC AN is of interest and should be followed up in a larger sample. We chose a hypothesis driven, ROI based analysis, so there was a risk of not identifying other interesting findings.
This is the first study showing evidence of altered reward processing in REC BN. Considered together with the REC AN data, these findings may reflect factors that are shared by these subgroups. That is, REC AN and REC BN may share an inability to precisely modulate emotionality and reward in response to salient stimuli. Whether there are possible differences in dorsostriatal activity related to consequences of choice is less certain, but is a question that should be asked of future studies with adequate power.
Acknowledgments
Supported by MH46001, MH42984, K05-MD01894, National Institute of Mental Health (NIMH), and by T32-MH18399 from NIMH Training Grant, and by the Price Foundation.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Cassin S, von Ranson K. Personality and eating disorders: A decade in review. Clin Psychol Rev. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Wagner A, Barbarich N, Frank G, Bailer UF, Weissfeld L, Henry S, et al. Personality traits after recovery from eating disorders: Do subtypes differ? Int J Eat Disord. 2006;39:276–284. doi: 10.1002/eat.20251. [DOI] [PubMed] [Google Scholar]
- 4.Volkow ND, Wang G, Fowler JS, Telang F. Overlapping neuronal circuits in addiction and obesity: Evidence of systems pathology. Philos Trans R Soc Lond B Biol Sci. 2008;363:3191–3200. doi: 10.1098/rstb.2008.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergen A, Yeager M, Welch R, Haque K, Ganjei JK, Mazzanti C, et al. Association of multiple DRD2 polymorphisms with anorexia nervosa. Neuropsychopharmacology. 2005;30:1703–1710. doi: 10.1038/sj.npp.1300719. [DOI] [PubMed] [Google Scholar]
- 6.Frank G, Bailer UF, Henry S, Drevets W, Meltzer CC, Price JC, et al. Increased dopamine D2/D3 receptor binding after recovery from anorexia nervosa measured by positron emission tomography and [11C]raclopride. Biol Psychiatry. 2005;58:908–912. doi: 10.1016/j.biopsych.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Schultz W. Getting formal with dopamine and reward. Neuron. 2002;36:241–263. doi: 10.1016/s0896-6273(02)00967-4. [DOI] [PubMed] [Google Scholar]
- 8.Davis C, Levitan RK, Kaplan AS, Carter JC, Reid C, Curtis C, et al. Dopamine transporter gene (DAT1) associated with appetite suppression to methylphenidate in a case-control study of binge eating disorder. Neuropsychopharmacology. 2007;32:2199–2206. doi: 10.1038/sj.npp.1301348. [DOI] [PubMed] [Google Scholar]
- 9.Nisoli E, Brunani A, Borgomainerio E, Tonello C, Dioni L, Briscini L, et al. D2 dopamine receptor (DRD2) gene Taq1A polymorphism and the eating-realted psychological traits in eating disorders (anorexia nervosa and bulimia) and obesity. Eat Weight Disord. 2007;12:91–96. doi: 10.1007/BF03327583. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan A, Levitan R, Yilmaz Z, Davis C, Tharmalingam S, Kennedy J. A DRD4/BDNF gene-gene interaction associated with maximum BMI in women with bulimia nervosa. Int J Eat Disord. 2008;41:22–28. doi: 10.1002/eat.20474. [DOI] [PubMed] [Google Scholar]
- 11.Wagner A, Aizenstein H, Venkatraman M, Fudge J, May J, Mazurkewicz L, et al. Altered reward processing in women recovered from anorexia nervosa. Am J Psych. 2007;164:1842–1849. doi: 10.1176/appi.ajp.2007.07040575. [DOI] [PubMed] [Google Scholar]
- 12.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User’s Guide for the Structured Clinical Interview for DSM-IV Axis II Personal Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 13.Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 14.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI): A Guide to Its Development and Use. St. Louis, MO: Center for Psychobiology of Personality, Washington University; 1994. [Google Scholar]
- 15.Delgado M, Nystrom L, Fissel C, Noll D, Fiez J. Tracking the hemodynamic responses to reward and punishment in the striatum. J Neurophysiology. 2000;84:3072–3077. doi: 10.1152/jn.2000.84.6.3072. [DOI] [PubMed] [Google Scholar]
- 16.Lesieur H, Blume S. The south oaks gambling screen (SOGS): A new instrument for the identification of pathological gamblers. Am J Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- 17.Delgado MR, Locke HM, Stenger VA, Fiez JA. Dorsal striatum responses to reward and punishment: Effects of valence and magnitude manipulations. Cogn Affect Behav Neurosci. 2003;3:27–38. doi: 10.3758/cabn.3.1.27. [DOI] [PubMed] [Google Scholar]
- 18.May JC, Delgado MR, Dahl RE, Stenger VA, Ryan ND, Fiez JA, et al. Event-related functional magnetic resonance imaging of reward-related brain circuity in children and adolescents. Biol Psychiatry. 2004;55:359–366. doi: 10.1016/j.biopsych.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Bornert P, Aldefeld B, Eggers H. Reversed spiral MR imaging. Magn Reson Med. 2000;44:479–484. doi: 10.1002/1522-2594(200009)44:3<479::aid-mrm20>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 20.Woods RP, Cherry SR, Mazziotta JC. Rapid automated algorithm for aligning and reslicing PET images. J Comput Assist Tomogr. 1992;16:620–633. doi: 10.1097/00004728-199207000-00024. [DOI] [PubMed] [Google Scholar]
- 21.Cox R. AFNI: Software for analysis and visualization of functinoal magnetic resonance neuroimages. Comput Biomed Res. 1996;119(Part 4):1239–1247. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- 22.Friston K, Holmes A, Worsley K, Poline J, Frith C, Frackowiak R. Statistical parametric maps in functional imaging: A general linear approach. Hum Brain Mapp. 1995;2:189–210. [Google Scholar]
- 23.Goto Y, Grace A. Dopaminergic modulation of limbic and cortical drive of nucleus accumbens in goal-directed behavior. Nat Neurosci. 2005;386:14–17. doi: 10.1038/nn1471. [DOI] [PubMed] [Google Scholar]
- 24.Schultz W. Neural coding of basic reward terms of animal learning theory, game theory, microeconomics and behavioural ecology. Science. 2004;14:139–147. doi: 10.1016/j.conb.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 25.Yin H, Knowlton B. The role of the basal ganglia in habit formation. Nat Neurosci Rev. 2006;7:464–476. doi: 10.1038/nrn1919. [DOI] [PubMed] [Google Scholar]
- 26.Montague R, Hyman S, Cohen J. Computational roles for dopamine in behavioural control. Nature. 2004;431:760–767. doi: 10.1038/nature03015. [DOI] [PubMed] [Google Scholar]
- 27.Phillips ML, Drevets WC, Rauch SL, Lane R. Neurobiology of emotion perception I: The neural basis of normal emotion perception. Biol Psychiatry. 2003;54:504–514. doi: 10.1016/s0006-3223(03)00168-9. [DOI] [PubMed] [Google Scholar]
- 28.Tricomi EM, Delgado MR, Fiez JA. Modulation of caudate activity by action contingency. Neuron. 2004;41:281–292. doi: 10.1016/s0896-6273(03)00848-1. [DOI] [PubMed] [Google Scholar]
- 29.O’Doherty J. Reward representations and reward related learning in the human brain: Insights from neuroimaging. Science. 2004;14:769–776. doi: 10.1016/j.conb.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Engel S, Corneliussen S, Wonderlich S, Crosby R, le Grange D, Crow S, et al. Impulsivity and compulsivity in bulimia nervosa. Int J Eat Disord. 2005;38:244–251. doi: 10.1002/eat.20169. [DOI] [PubMed] [Google Scholar]
- 31.Rosval L, Steiger H, Bruce K, Israel M, Richardson J, Aubut M. Impulsivity in women with eating disorders: Problem of response inhibition, planning, or attention? Int J Eat Disord. 2006;39:590–593. doi: 10.1002/eat.20296. [DOI] [PubMed] [Google Scholar]
- 32.Bulik CM, Sullivan PF, Joyce PR, Carter FA. Temperament, character, and personality disorder in bulimia nervosa. J Nerv Ment Dis. 1995;183:593–598. doi: 10.1097/00005053-199509000-00006. [DOI] [PubMed] [Google Scholar]