Abstract
Objective
To describe a process for developing low-literacy health education materials that increase knowledge and activate patients toward healthier behaviors.
Methods
We developed a theoretically informed process for developing educational materials. This process included convening a multidisciplinary creative team, soliciting stakeholder input, identifying key concepts to be communicated, mapping concepts to a behavioral theory, creating a supporting behavioral intervention, designing and refining materials, and assessing efficacy.
Results
We describe the use of this process to develop a diabetes self-management guide.
Conclusions
Developing low-literacy health education materials that will activate patients toward healthier behaviors requires attention to factors beyond reading level.
Keywords: patient education, educational status, self care, health promotion
One half of American adults lack the literacy and numeracy skills necessary to effectively obtain, process, and act on the information in most patient education materials.1 Recognizing this, the Institute of Medicine's 2004 report on health literacy recommended making the creation of understandable health materials a national priority.1 An increasing number of patient education materials are written at lower reading levels,2 and these materials have been shown to improve knowledge among readers of all literacy levels.3,4 However many patients with chronic illness must go beyond knowledge and enact long-term behavior change. Designing educational materials effective at activating patients toward healthier behaviors is becoming increasingly urgent as chronic diseases such as obesity and diabetes become more prevalent, particularly among those with lower levels of educational attainment, and as patients are asked to assume greater responsibility for managing their health care.
All health behavior theories consider adequate knowledge of the benefits of healthy behaviors a prerequisite for behavior change.5 Within social cognitive theory, the success of behavior change is also strongly affected by self-efficacy, outcome expectations, perceived facilitators and impediments, and goal setting.6 Self-efficacy in the health care context refers to one's confidence in successfully organizing and executing the courses of action necessary to manage one's health care needs, for example, adhering to a diabetic diet.7 Self-efficacy influences patients' choices about their health behavior, the effort they put forth toward achieving behavior change, how long they persist in the face of obstacles, and their feelings accompanying the process of behavior change.
Social cognitive theory suggests that patient education materials designed to activate patients toward healthier behaviors ought to (1) improve knowledge of the health effects of behavior change, (2) positively influence outcome expectations, (3) emphasize facilitators to behavior change, (4) address impediments to behavior change, and (5) enable the creation and achievement of short-term goals.6 Success at communicating these elements can be assessed by measuring changes in self-efficacy and behaviors.8
This paper outlines a theoretically informed process for developing low-literacy health education materials that activate patients toward behavior change. We illustrate important principles by describing the development of a diabetes self-management guide and accompanying brief behavior-change intervention. This review is limited to written patient educational materials; however, many of the principles are also applicable to web-based, telephone, and other interactive health education innovations.
Methods
Described below are 6 steps for developing low-literacy education materials to activate patients toward healthier behaviors. These 6 steps were subsequently used in the development of a diabetes self-management guide.
1. Convene a working team and solicit stakeholder input early
Critical stakeholders include health care providers patients, families, and caregivers. To guarantee the experiences and needs of a diverse audience are considered, these stakeholders should each be represented either on the development team or in focus groups during the design process. Provider input ensures clinical accuracy and provides real-world patient education strategies. Patient, family, and caregiver input ensure the message is clear, manageable, practical, relevant, and culturally appropriate.9 Soliciting feedback early in the design process facilitates incorporation of varied perspectives and enhances the materials' effectiveness and dissemination potential. Focus groups providing examples of existing patient education materials can be used to elicit concrete opinions about content, layout, and artwork.
2. Identify key concepts to be communicated
A key objective of stakeholder focus groups is to identify critical content and determine how it can be clearly communicated. Patient educational materials commonly attempt to communicate many concepts, rather than focusing on the 2 to 3 concepts recommended for audiences with low literacy skills.10 Focus group feedback is essential to reducing this scope. Identifying content which, if absent, would render the materials useless for providers or unhelpful for patients helps create low-literacy materials that are effective and more likely to be disseminated. Eliminating content which, if present, might confuse or overwhelm the reader is also critical.
3. Map concepts to a behavioral theory, such as social cognitive theory, and construct a brief intervention to support the use of written materials
Educational materials designed to activate patients toward healthy behaviors should be mapped to a health behavior model to give a theoretically informed framework for development and assessment. As described above, social cognitive theory suggests that materials should improve knowledge, positively influence outcome expectations, emphasize facilitators of behavior change, address impediments to behavior change, and facilitate the creation of goals. Long-term goals offer general direction to guide health behavior change, but are too remote to offer everyday incentive. Short-term goals, developed to work toward achieving long-term goals, offer daily incentive to change. Interventions designed on the basis of social cognitive theory have resulted in sustained behavior change.11
With additional guidance, patients with low literacy skills may be able to achieve the full benefit of written health materials. This guidance, provided by medical or nonmedical personnel, can orient readers to content and contextualize the materials as a tool for behavior change. A brief intervention to teach patients how to develop their own action plans can help them learn to create the short-term goals that are the springboard for sustained behavior change.12 Action plans are short-term, easily achievable, and highly specific goals for immediate behavior change. For example, the patient who is interested in losing weight as a long-term goal may create as an action plan “I will walk around the block before I sit down to watch television 3 times during the next week.” Action plans are designed by the patient with support from the health care pro-vider.12
The use of action plans is consistent with the framework offered by social cognitive theory. Action plans operationalize the process of goal setting and can lead to early successes, which build self-efficacy. Improved self-efficacy facilitates the identification and completion of new action plans, thus creating a trajectory of increasing self-efficacy and continued behavior change. Permitting patients to control the process of creating an action plan preselects the behavior changes that the patient is motivated to undertake, allowing health care providers to offer targeted counseling assistance in those domains for which the patient is likely to be receptive.
4. Carefully design materials using low-literacy principles
Designing patient education materials that patients with low literacy can understand and act on is challenging. Text, artwork, and layout design must each be developed to emphasize the 2 to 3 key concepts chosen for communication. Effective materials pay particular attention to writing style.10,13-15 Shortening words, substituting general terms for jargon, simplifying sentence structure, using the active voice, eliminating extraneous words, and replacing abstract principles with concrete suggestions will make the material more easily understood.
Illustrations are engaging for all audiences, particularly those with low literacy, but careful attention to content is important.16 Drawings and photographs should emphasize key concepts, rather than be purely decorative. Well-designed pictures can effectively illustrate complex concepts that are difficult to communicate with simple words.17 However, readers with low literacy skills are often unable to interpret complex figures, such as those illustrating the secretion of insulin from the pancreas into the bloodstream. Artwork must also be culturally appropriate and represent the diversity of the target population.
Using a large (12-point or higher), clear font, a logical flow of information, flags to draw attention to important text, headers to orient the reader to new topics, and adequate white space facilitate ease of reading.10,13-15 Readers with low-literacy skills may have particular difficulty with cross-referencing text, such as using a glossary or referring readers to other pages for additional information. They may also have difficulty with unusual layouts, such as not starting text in the upper left-hand corner of the page.10,13
5. Refine materials using input from the target population
In-depth, semistructured interviews with patients critiquing preliminary materials should proceed 1 page at a time, with the facilitator stopping at each passage and illustration (particularly those flagged during the design process as difficult to communicate) to probe understanding and areas of potential confusion. To elicit honest feedback it is imperative that the facilitator be curious about learning which passages and pictures are appealing, relevant, and clearly understood and which need to be revised or eliminated. During these sessions interviewers can also probe the patient's emotions accompanying use of the materials. Educational materials engendering patient confidence and enthusiasm may be more likely to facilitate behavior change than those that engender fear or pessimism.18
6. Assess success of efforts in target audience and learn from failures
The final stage of material development is to assess its use in the target population. Such an assessment should proceed with 2 distinct goals in mind: creating a product with high potential for dissemination and communicating intended information in a way that supports and facilitates behavior change. Patients, health care providers, and health system administrators can each help gauge success with creating a product that is likely to be disseminated. Replacing existing materials requires effort, and often expense, for each group of stakeholders. Besides being easily implemented and cost-effective, materials with high dissemination potential need to meet stakeholder needs and address problems in existing materials.
Successful dissemination potential may be gauged by offering materials to health care providers and patients to pilot test for a short period of time. Providers can be asked whether they agreed with the information communicated, if they would use the materials in the future, if materials were appropriately targeted to their patients, and whether materials lengthened their patient visits or distracted them from taking care of other important patient care issues. Patients can be asked how they used the material, whether they would recommend it to family members or friends, whether they preferred it to alternatives (such as meeting a health educator or receiving standard educational materials), and whether they felt it was important they receive such materials from their health care provider or hospital.
After distributing patient education materials, formal assessment of patients to assess knowledge improvement is an important way of gauging success with communicating intended information. It is important to also assess changes in self-efficacy, outcome expectations, and actual behaviors, as knowledge improvement is not closely associated with health outcomes.
Results
The American College of Physicians Foundation commissioned a guide, entitled Living with Diabetes: An Everyday Guide for You and Your Family, to teach diabetes self-management skills to patients with low literacy skills.19 We used the described 6-step process as a framework for guide development.
We convened a multidisciplinary development team which included 3 primary care physicians, 2 behavioral scientists with expertise in developing low-literacy health education materials, 1 diabetes educator, a nurse, a pharmacist, 3 health educators (including 1 with diabetes), and an advertising agent. Because we simultaneously developed the self-management guide in Spanish, the team also included 2 native Spanish-speakers with expertise in providing diabetes education to the Latino community. The multidisciplinary team identified varied stakeholders, including patients with diabetes and their families, physicians, diabetes educators, nurses, dietitians, and pharmacists in both public and private sectors.
The authors (TD, CA, DD, AW, and LK) conducted semistructured focus groups with a convenience sample of health care providers and patients to solicit opinions about designing effective health education materials to activate patients toward behavior change. Eighty-five physicians and physician's assistants, 13 registered nurses or diabetes nurse educators, and 3 dietitians working in the public and private sectors participated in the provider focus groups. We recruited these participants from rural and urban areas near the institutions of the development team members. Focus groups were held during the weekly staff meeting at the clinics where the providers worked. Additional participants were recruited from a national medical meeting hosted by the funding agency. Most of the physicians were general internists. All of the providers regularly took care of patients with type 2 diabetes. Participants were offered food and reimbursement of $50 to $100.
During the focus groups we asked providers their opinions on which topics they felt were critical to address in a diabetes self-management guide, the ways in which patient education materials were used in their practices, and barriers they encountered to effective self-management counseling. In general, health care providers were pessimistic about their ability to help their patients achieve sustained behavior change. However, they were enthusiastic about trying new strategies to become more effective counselors.
We recruited patients from the same private and public clinics and held interviews in Texas, Louisiana, North Carolina, and California. Fifty-two patients participated in these interviews. Participants were paid $20 for their time. Facilitators queried patients about diabetes self-management barriers and facilitators, critical topic areas to include in a diabetes self-management guide, criticisms of existing patient education materials, and suggestions for more effectively engaging patients with written materials.
Focus groups revealed a number of conflicts about essential content. Health care providers emphasized the content that patients needed to be taught—the “need to know,” such as diabetes' severity, associated health risks, and the meaning of the hemoglobin A1c test. Patients emphasized the need for practical advice on how to achieve behavior recommendations in their daily life—the “need to do.” For example, patients requested realistic strategies for combating hunger, preparing quick and healthy breakfasts, budgeting exercise into their daily activity, and sustaining healthy behaviors. To create a patient-centered self-management guide, we chose to include only the most critical “need to know” content favored by health care providers and to focus the majority of our content on practically conveying the “need to do” favored by patients. This decision was based on our appreciation that future dissemination required acceptance of the materials from community providers, but that our primary goal was to design a guide that was effective for patients.
Focus groups also identified key content areas to be addressed by revealing communication gaps between patients and health care providers. For example, health care providers voiced frustration that patients failed to log their blood sugar values. Many patients felt they checked their blood sugar in order to assist their health care provider in managing their diabetes. When health care providers neglected to examine the logs, as frequently occurred, patients felt frustrated and concluded that checking their blood sugar was not important. Few patients recognized that the purpose of checking their blood sugar was to guide their own self-management decisions. Making this concept explicit became the key piece of information we aimed to communicate in the “checking your blood sugar” chapter.
The development team performed a search to identify previously developed materials for patients to critique. Often these materials were not designed for an audience with low literacy skills, but they were commonly used in clinics or disseminated by key organizations. Most patients could recall having received other patient education materials from their health care providers and were asked to comment on their experiences with those materials as well. Patients generally felt that the clip art format (stylized black and white line drawings) of most low-literacy materials was unappealing, that the text was difficult to read, and that the layout was cluttered. They also described many existing materials as either condescending or overwhelming. Patients suggested these education materials could be improved by using photographs of real people, letting the patient's voice be heard rather than the health care provider's, and removing complex diagrams. They also offered numerous suggestions for making materials more engaging and more focused on their educational needs (Table 1).
Table 1. Feedback From Patients During Initial Focus Groups Can Guide the Development of Health Education Materials.
| Guiding Themes Identified by Patient Feedback | Sample Quotes From Patients |
|---|---|
| Health care providers give general advice (for example, “You need to lose weight”), but patients want practical advice. | “I've got a box full of literature on the disease. It would be helpful to show me what to do on a daily basis.” |
| “Tell me what I need to do now to take care of myself.” | |
| Health care providers do not assist patients with overcoming barriers to good diabetes self-management, for example, affording testing strips for their glucose monitor or healthy foods. | “I can buy a whole carton of sugar for what I would spend on one pack of Equal©.” |
| Patients indicated substantially greater interest in diet and exercise than in all other domains of diabetes care. | “Eating is extremely hard.” |
| Patients have a difficult time staying motivated to change their behaviors when they are stressed, frustrated, helpless, or feel alone with their disease. | “When my doctor told me I had to go on insulin I wanted to die. I felt like I failed.” “Don't scold me, support me.” |
| Patients felt fear worked as a good motivator, but wanted empowering stories as well. | “You want to show people living successfully with diabetes, so I know that I can do it too.” |
| Real people with diabetes are more credible than actors. | “It helps to see that other people have the same problems that I have.” |
Patients and health care providers offered numerous suggestions of tools to include in the self-management guide, such as a pedometer, an easily-accessible blood sugar log, and a full-scale example of a healthy diabetic plate. These options were carefully considered within the constraints of the product's ultimate dissemination. Because of concerns about incurring production costs, shipping costs, and storage difficulties, these options had to offer clear additional value. Neither health care providers nor patients felt they would use content available on a website. Based on these opinions we limited the initial version of the guide to paper-based content and used available budget to produce high-quality photographs.
To facilitate the design process, our national development team met weekly by phone to discuss progress and establish consensus on difficult issues. Between meetings, individual group members took responsibility for specific tasks, such as writing text, revising drafts, or developing artwork. We kept detailed notes of difficulties we encountered with simplifying concepts and choosing wording. For example, in the insulin chapter we struggled with how to appropriately use the words syringe, shot, and needle in order to be accurate while also avoiding the use of jargon. Our notes were used to identify segments of the guide which needed additional patient feedback.
The scope of information we wished to cover in our diabetes self-management guide was broad. Given the available budget, we had to limit the domains covered to those in which patients were most interested or physicians felt were most critical—diet, exercise, glucose monitoring, use of insulin, and taking of oral medicines. The decision to neglect other important domains, such as smoking cessation and depression management, was difficult. We hope to add additional domains to the guide in the future.
With the expectation that patients would read a single chapter at a sitting, we decided on 2 to 3 important concepts to clearly communicate in each chapter. The diet chapter, for example, conveys 2 general concepts: eat smaller portions, and eat fewer carbohydrates. All text and photography supports these 2 messages. We did not introduce diet-control strategies such as carbohydrate counting or exchanges, or use measurement terms such as “1/3 cup” for 2 reasons: (1) the numeracy skills required to understand these concepts and make them useful on a daily basis are higher than the numeracy skills of the average patient, and (2) health care providers did not identify these skills as critical for the majority of patients with diabetes.
Each of the 5 factors identified by social cognitive theory as positively influencing behavior change was specifically addressed in the context of reinforcing the 2 to 3 key concepts of each chapter. For example, text in the diet chapter explicitly links behavior change to health outcomes: “Eating the right portion sizes may help you lose weight.” Positive outcomes from behavior change are highlighted: “Most people with diabetes will feel better if they lose even a few pounds,“ or “Eating breakfast will help fill you up and give you energy.”
Compared to the physician's voice, focus group participants felt that the patient's voice was more engaging for modeling health behaviors. We therefore used patients' faces and voices to emphasize facilitators and address impediments to behavior change. For example, many focus group participants were interested in hearing diet-control strategies used by other patients when dining out, especially because super-size portions were prevalent and all-you-can-eat options seemed cost-effective. A patient quoted in the guide stated, “When I eat out, I box up half my meal. Now it's like I get 2 meals for the price of 1. I save money, and I do not overeat.” The quotation is accompanied by a photograph illustrating this behavior. This suggestion is consistent with the portion-control concept emphasized in the chapter, offers a concrete suggestion to facilitate behavior change, and addresses financial barriers to healthier eating.
In our previous experience assisting patients to create action plans in the clinical setting, we noted that patients encounter difficulty both because of poor motivation and because of a lack of independent problem-solving and creative skills necessary to identify small steps toward a larger goal. The emphasis on providing concrete suggestions for behavior change addresses this lack of creativity by providing patients with dozens of suggestions for easily achievable action plans. For example, the page about a healthy breakfast includes a practical behavior suggestion— “if you are in a hurry, eat a piece of toast with some peanut butter on it”—using a patient's words and a picture of the patient eating breakfast. This suggestion can be easily turned into a personal action plan: “For 3 days during the next week, I will eat a piece of toast with peanut butter on it before work.” The last page of each chapter offers a list of potential action plans under the heading “You Can Do It!” For readers with low literacy skills, brief instruction can emphasize how these suggestions can be used to create personal action plans, allowing these patients to gain the full benefit of the material.
After an initial draft of the guide was written, we identified messages that would be enhanced by supplemental illustration. To increase patient engagement with and comprehension of the materials, we used photographs rather than drawings. We hired a professional photographer to take appealing photographs of healthy foods we had prepared in recommended portion sizes. We also recruited real people with diabetes of various ages, weights, and cultural backgrounds to serve as models demonstrating healthy diabetes self-management behaviors. Photographs were taken in homes, offices, clinics, and restaurants to illustrate the range of locations in which self-management behaviors occur. We hoped to foster familiarity, and thus increase patient engagement, by using the same models throughout the self-management guide. Subsequent input from cognitive interview participants revealed that the photographs were instructive, warm, and appealing. They commented that the models looked like real people with diabetes, were “about my size,” and “look[ed] like they [were] doing well with their diabetes.”
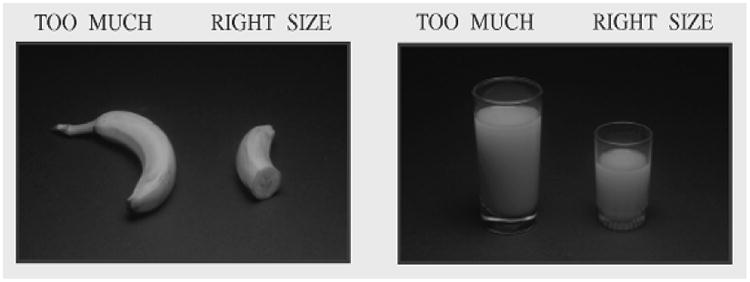
Using clear labels on the photographs often allowed the images to represent important concepts without having to read any additional text. For example, sample plates with different amounts of food were labeled either “too much” or “right size” (Figure 1). Photographs which were particularly effective at illustrating important concepts allowed us to eliminate text. For the Spanish version of the diabetes guide, we took additional photographs of culturally appropriate foods and models. For example, we replaced images of broccoli and spinach with the more frequently eaten cauliflower and nopales (prickly pear cactus).
Figure 1. Clear Labels May Allow Images to Communicate Important Concepts Without Having to Read Additional Text.
Because the guide we created was lengthy and included multiple chapters, we printed each chapter on a different background color to help orient the reader. Examples of patients offering concrete suggestions for behavior change were isolated in color boxes to maintain consistency between the chapters and separate them visually from the main text (Figure 2).
Figure 2. Using the Patient's Voice to Offer Concrete Behavior Change Suggestions.

After preliminary design of the guide was completed, the authors (TD, CA, AW, AD, and JP) conducted 1-hour cognitive interviews with a convenience sample of 51 English-speaking and 19 Spanish-speaking patients. Participants were offered a $20 reimbursement. Each interview addressed a small portion of the guide. The interview moderator used a general script to guide feedback about words and pictures. Questions included “What did this picture say to you?”, “Is this tip something you would do?”, “What do you think the message is here?”, and “What should the message be here?” At the end of each chapter, we asked participants, “How does this chapter make you feel—anxious, confident, happy, afraid, intimidated?” We incorporated patient feedback in an iterative revision process. Based on patient feedback for the diet chapter, for example, we added photographs of additional vegetables, removed unappealing photographs, added labels to clarify pictures, and revised sentences for clarity.
Careful notes during the cognitive interviews allowed us to capture patient quotes which offered more concrete suggestions for behavior change and more precise emotions related to having diabetes than those we had obtained during the original focus groups. For example, one patient stated after reading the insulin chapter: “At first, I didn't really want to take shots, but I didn't realize how much better I could feel. It made a big difference to me.” This empowering quote, which positively influences outcome expectations, was added to the insulin chapter. Our final cognitive interviews drew positive patient comments which included “I feel like I can do this,” and “It lets me know I'm not alone.”
Written health education materials used in isolation are unlikely to be adequate for activating patients, particularly those with low literacy skills, to achieve difficult behavior change. However, well-designed written materials may be synergistic with brief behavioral counseling and offer a valuable resource for patients and families when they are outside the health care system. We therefore elected to evaluate how our materials influenced behavior change when implemented in the context of brief instruction on how to create successful action plans. Although implemented in the clinical setting, nonmedical personnel provided 5-10 minutes of orientation to the guide and instruction in the generation of action plans. We also elected to call patients on the phone 2, 4, and 12 weeks after receiving the guide to assess success with their action plans and facilitate the creation of new action plans.
We measured dissemination potential by asking patients satisfaction questions which included “How likely are you to keep using this guide?” and “How likely is it that you will recommend the guide to others with diabetes?” In pre- and postexposure testing, we assessed our success with each of the 5 factors influencing behavior change according to social cognitive theory. Finally, we measured how many action plans were remembered at the next visit and how successful participants were in completing their action plans in order to obtain a preliminary estimate of behavior change. This evaluation is ongoing, and a report of our results will be forthcoming.
Discussion
Most low-literacy educational materials are written at a lower reading level than average health education materials. However, designing materials which are effective at activating patients toward healthier behaviors requires attention to factors beyond reading level. Materials should be focused on offering practical strategies for behavior change, the “need to do”, rather than focused on teaching facts, the “need to know”. Determining essential content and how to effectively communicate that content requires input from patients and providers during all phases of design.
Mapping content to be communicated to a behavioral model, such as social cognitive theory, offers a framework for designing and evaluating patient education materials.
Teaching patients to create their own action plans may be a particularly effective way for health care providers to assist patients with setting goals.12,20,21 Further research is necessary to evaluate the success of using written health materials in conjunction with brief provider interventions to assist patients in making sustained behavior change.
Acknowledgments
The authors would like to thank Lewis Kalmbach, Jorge Palacios, Kathryn Davis, Mary Bocchini, Jimmy Joyner, and Neil Johnson for their dedication to the project. We would also like to express our deepest appreciation to the patients and healthcare providers whose feedback helped make Living with Diabetes so successful. This work was supported by the American College of Physicians Foundation.
Contributor Information
Hilary K. Seligman, Division of General Internal Medicine.
Andrea S. Wallace, University of North Carolina School of Nursing.
Darren A. DeWalt, Division of General Internal Medicine, University of North Carolina School of Medicine.
Dean Schillinger, UCSF Center for Vulnerable Populations.
Connie L. Arnold, Feist-Weiller Cancer Center Section of Cancer Prevention and Control.
Betsy Bryant Shilliday, Division of General Internal Medicine, University of North Carolina School of Medicine, Chapel Hill, NC.
Adriana Delgadillo, Division of General Internal Medicine.
Nikki Bengal, Division of General Internal Medicine, San Francisco General Hospital, University of California San Francisco, San Francisco, CA.
Terry C. Davis, Department of Medicine-Pediatrics, Louisiana State University Health Sciences Center— Shreveport, Shreveport, LA.
References
- 1.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Health Literacy: A Prescription to End Confusion. Washington, D.C.: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Freda MC, Damus K, Merkatz IR. Evaluation of the readability of ACOG patient education pamphlets. The American College of Obstetricians and Gynecologists. Obstet Gynecol. 1999 May;93(5 Pt 1):771–774. doi: 10.1016/s0029-7844(98)00518-3. [DOI] [PubMed] [Google Scholar]
- 3.Eaton ML, Holloway RL. Patient comprehension of written drug information. Am J Hosp Pharm. 1980 Feb;37(2):240–243. [PubMed] [Google Scholar]
- 4.Davis TC, Bocchini JA, Jr, Fredrickson D, et al. Parent comprehension of polio vaccine information pamphlets. Pediatrics. 1996 Jun;97(6 Pt 1):804–810. [PubMed] [Google Scholar]
- 5.Bandura A. Self-efficacy: The Exercise of Control. New York: W.H. Freeman and Company; 1997. [Google Scholar]
- 6.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004 Apr;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 7.Bandura A. Self-Efficacy in Changing Societies. New York: Cambridge University Press; 1999. [Google Scholar]
- 8.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 9.Davis TC, Humiston SG, Arnold CL, et al. Recommendations for effective newborn screening communication: results of focus groups with parents, providers, and experts. Pediatrics. 2006 May;117(5 Pt 2):S326–S340. doi: 10.1542/peds.2005-2633M. [DOI] [PubMed] [Google Scholar]
- 10.Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2. Philadelphia: Lippincott Williams & Wilkins; 1996. [Google Scholar]
- 11.Whitlock EP, Orleans CT, Pender N, et al. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–284. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 12.Handley M, MacGregor K, Schillinger D, et al. Using action plans to help primary care patients adopt healthy behaviors: a descriptive study. J Am Board Fam Med. 2006;19(3):224–231. doi: 10.3122/jabfm.19.3.224. [DOI] [PubMed] [Google Scholar]
- 13.McGee J. Writing and Designing Print Materials for Beneficiaries: A Guide for State Medicaid Agencies. U.S. Department of Health and Human Services; 1999. [Google Scholar]
- 14.National Cancer Institute. Clear and Simple: Developing Effective Print-Materials for Low-Literate Readers. U.S. Department of Health and Human Services; 1994. [Google Scholar]
- 15.Scientific and Technical Information Simply Put. 2. Centers for Disease Control and Prevention (CDC); Atlanta, GA: 1999. [Google Scholar]
- 16.Michielutte R, Bahnson J, Dignan MB, et al. The use of illustrations and narrative text style to improve readability of a health education brochure. J Cancer Educ. 1992;7(3):251–260. doi: 10.1080/08858199209528176. [DOI] [PubMed] [Google Scholar]
- 17.Houts PS, Doak CC, Doak LG, et al. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns. 2006;61(2):173–190. doi: 10.1016/j.pec.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 18.Hastings G, MacFadyen L. Controversies in tobacco control: the limitations of fear messages. Tob Control. 2002;11(1):73–75. doi: 10.1136/tc.11.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Living with Diabetes: An Everyday Guide for You and Your Family. American College of Physicians Foundation; Philadelphia, PA: [Google Scholar]
- 20.MacGregor K, Handley M, Wong S, et al. Behavior-change action plans in primary care: a feasibility study of clinicians. J Am Board Fam Med. 2006;19(3):215–223. doi: 10.3122/jabfm.19.3.215. [DOI] [PubMed] [Google Scholar]
- 21.Estabrooks PA, Glasgow RE, Dzewaltowski DA. Physical activity promotion through primary care. JAMA. 2003 Jun;289(22):2913–2916. doi: 10.1001/jama.289.22.2913. [DOI] [PubMed] [Google Scholar]


