Abstract
Background
Failure to detect metastasis to para-aortic nodes in patients with locally advanced cervical cancer leads to suboptimal treatment. No previous studies have prospectively compared PET/CT with laparoscopic extraperitoneal staging in the evaluation of para-aortic lymph nodes.
Methods
Sixty-five patients were enrolled; 60 were available for analysis. Patients with stage IB2-IVA cervical cancer without evidence of para-aortic lymphadenopathy on preoperative CT or MRI were prospectively enrolled. All patients underwent preoperative PET/CT. Laparoscopic extraperitoneal lymphadenectomy was performed from the common iliac vessels to the left renal vein.
Results
The median age at diagnosis was 48 years (range, 23-84). The median operative time was 140 minutes (range, 89-252). The median blood loss was 22.5 ml (range, 5-150). The median length of hospital stay was 1 day (range, 0-4). The median number of lymph nodes retrieved was 11 (range, 1-39). Fourteen patients (23%) had histopathologically positive para-aortic nodes. Of the 26 patients with negative pelvic and para-aortic nodes on PET/CT, 3 (12%) had histopathologically positive para-aortic nodes. Of the 27 patients with positive pelvic but negative para-aortic nodes on PET/CT, 6 (22%) had 4 histopathologically positive para-aortic nodes. The sensitivity and specificity of PET/CT in detecting positive para-aortic nodes when nodes were negative on CT or MRI were 36% and 96%, respectively. Eleven patients (18.3%) had a treatment modification based on surgical findings.
Conclusion
Laparoscopic extraperitoneal para-aortic lymphadenectomy is safe and feasible. Surgical staging of patients with locally advanced cervical cancer should be considered prior to planned radiation and chemotherapy.
Keywords: cervical cancer, PET/CT scan, surgery, laparoscopy
INTRODUCTION
The staging for cervical cancer remains one based on clinical features. While this strategy is generally reproducible in assessing local extent of disease, it poorly represents regional spread of disease. 1 In a collective series from the Gynecologic Oncology Group protocols, the most important predictor of disease recurrence in patients with cervical cancer was para-aortic nodal status. 2 Failure to detect metastasis to these lymph nodes may lead to suboptimal treatment.
Surgical staging of patients with locally-advanced cervical cancer remains controversial. While a gain in sensitivity for nodal metastatic para-aortic disease is achieved over radiographic surveillance alone, historically, only modest gains in survival have been achieved with routine practice. Further, an open transperitoneal approach is associated with high morbidity and mortality secondary to bowel complications, particularly when surgery is followed by radiotherapy. An extraperitoneal approach by laparotomy has been shown to decrease the complication rate from 30% to 2% compared with the transperitoneal approach. 3 More recently, minimally invasive surgery has offered the option of performing extraperitoneal surgical staging by laparoscopy 4 or robotic surgery. 5
As an alternative to surgery, imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) have been used to detect metastasis to the para-aortic nodes. Unfortunately, these modalities are limited by low sensitivity and specificity compared with surgical staging. 6,7 However, a number of studies have shown that positron emission tomography (PET) is more effective at detecting abnormal lymph nodes than either CT or MRI. 7,8 PET/CT combines the anatomic detail provided by CT with the metabolic information provided by PET. This fusion modality is increasingly being used to identify distant spread of disease more accurately.
To our knowledge, no studies have prospectively compared PET/CT with laparoscopic extraperitoneal surgical staging in the evaluation of para-aortic lymph nodes. The goals of this study were to determine the safety and feasibility of performing laparoscopic extraperitoneal para-aortic lymphadenectomy in patients with stage IB2- IVA cervical carcinoma scheduled to undergo radiotherapy and concurrent chemotherapy and to determine the utility of preoperative PET/CT in detecting metastasis to the para-aortic lymph nodes.
Materials and Methods
This study was approved by our Institutional Review Board, and informed consent was obtained from all patients. All patients were enrolled at The University of Texas M. D. Anderson Cancer Center or Lyndon Baines Johnson General Hospital between April 2004 and May 2009. All PET/CT scans were performed at M. D. Anderson Cancer Center, and laparoscopic procedures were performed at both institutions.
Patient Eligibility
Patients were eligible for this study if they met the following criteria: stage IB2-IVA cervical cancer and a candidate for treatment with radiotherapy and concurrent chemotherapy; biopsy-proven cervical carcinoma, any histology; no evidence of para-aortic lymphadenopathy (all nodes < 2 cm in diameter) on a preoperative CT or MRI scan of the abdomen and pelvis; adequate bone marrow, renal, and hepatic function; Zubrod Performance Status of 0, 1, or 2, and a suitable candidate for surgery. Patients who had a PET/CT scan performed prior to study entry could participate in the study and were not required to repeat the scan unless the scan was done more than 6 weeks from the date of surgery or if, in the opinion of the diagnostic radiologist, interpretation of the scan was limited due to poor quality. All patients required a PET/CT prior to surgery and the results of the PET/CT did not affect eligibility.
Patients were excluded from the study if they had undergone prior retroperitoneal surgery or had received prior pelvic or abdominal radiotherapy; were known to have upper abdominal intraperitoneal disease or evidence of ovarian metastases; were pregnant; had evidence of distant metastases on imaging studies or physical examination; or had contraindications to laparoscopy
PET/CT Imaging
Fluorodeoxyglucose PET/CT scans were performed on a dedicated PET/CT system (Discovery ST, STe, or RX, General Electric Medical Systems, Milwaukee, Wis). Scan coverage was generally from the orbits to the proximal thighs. Scans were acquired 60 to 90 minutes after intravenous administration of [[18]F]fluorodeoxyglucose with a dose range of 15 to 20 mCi (555-740 MBq). PET studies were acquired in either two-dimensional or three-dimensional acquisition mode at 3-5 minutes per bed position depending on the patient's body mass index. Images were reconstructed using ordered-subset expectation maximum with a 128 × 128 matrix size and a field of view of 70 cm (5.47-mm pixels). CT scans were acquired without administration of oral or intravenous contrast material, and CT was used for attenuation correction of the PET scan. The CT acquisition parameters were 120-kV peaks, 300 mA, 0.5-second rotation, with a pitch of 1.375. The CT images were reconstructed using a 3.75-mm slice thickness with a slice interval of 3.27 mm to match the PET data. PET/CT images were reviewed on an Advantage Workstation (General Electric Medical Systems). PET, CT, and PET/CT fusion datasets were reviewed in multiple imaging planes. All PET/CT scans were reviewed by the nuclear radiologists at our institution.
Surgical Technique
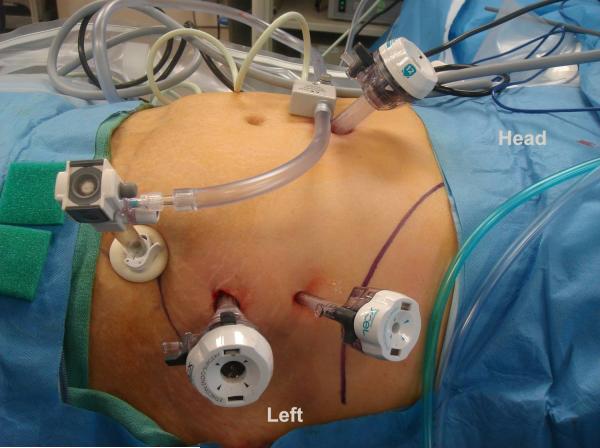
All patients had pneumatic compression stockings placed prior to the induction of anesthesia. Prophylactic antibiotics were given at the surgeon's discretion. The patient was placed in a supine position under general anesthesia with the right arm adducted and secured and the left arm placed at a right angle to the patient. A 5-mm endoscope was placed at the inferior margin of the umbilicus. Pneumoperitoneum was obtained, and the abdominal and pelvic cavity was inspected for any evidence of intraperitoneal metastatic disease. If none was found, a 15-mm incision was made 3-4 cm medial and superior to the left anterior iliac spine. The skin, fascia, transverse muscles, and deep fascia were incised, with care taken not to open the peritoneum. The surgeon's left forefinger was introduced in the incision to free the peritoneal sac from the deep surface of the muscles of the abdominal wall under laparoscopic monitoring. A 10-mm balloon-tip trocar was then placed in the extraperitoneal space of the flank. The retroperitoneum was insufflated to a pressure not exceeding 15 mm of mercury. At the same time the peritoneal cavity was deflated. The laparoscope was then introduced through the balloon-tip trocar. A second 10-mm trocar was then introduced into the extraperitoneal space. The penetration point was located in the midaxillary line under the subcostal margin approximately 5 cm cephalad to and 3-4 cm lateral to the initial point. A 5-mm trocar was then placed 3-4 cm cephalad to this second 10-mm trocar. The final trocar set up is demonstrated in Figure 1.
Figure 1.
Port placement for laparoscopic extraperitoneal para-aortic lymphadenectomy
The dissection was performed bilaterally from the level of the common iliac vessels to the level of the left renal veins. When there was evidence of grossly positive lymph nodes, these were sent to pathology for frozen section evaluation. If metastatic disease was confirmed, the laparoscopic procedure was aborted. At the completion of the procedure all patients had an incision performed in the peritoneum overlying the left para-colic gutter in order to minimize the likelihood of development of postoperative lymphocysts. No drains were placed at the completion of surgery.
Pathologic Evaluation
The lymph nodes were submitted for routine sectioning and pathologic evaluation. If all lymph nodes sampled were negative, the case was submitted for further processing. On each block, five hematoxylineosin- stained slides were cut at 40 μm intervals, and three unstained slides were cut at each level. If any of the blocks were found to be histologically positive with this additional evaluation, the results were reported in an addendum. If all five levels were negative by hematoxylineosin staining, the case was submitted for immunohistochemical analysis, which was performed as follows. Tissue sections were deparaffinized in xylene and rehydrated. The tissue sections were soaked in 0.3% hydrogen peroxide to block endogenous peroxidase activity. Microwave antigen retrieval in pH 6.0 citrate buffer was performed for a total of 30 minutes. Specimens were then incubated overnight for pankeratin antibody evaluation.
Statistical Design
The study employed a Bayesian rule to monitor the surgical complication rate, such that the study would be stopped if there was at least a 97% probability that the complication rate would exceed 30%. Potential complications included bleeding requiring conversion to laparotomy; injury to abdominal or pelvic viscera secondary to endoscopic instrument placement or manipulation (including injury to bowel, bladder, vessels, ureter, or kidney); development of symptomatic lymphocysts requiring percutaneous drainage or hospitalization; nerve injury requiring physical therapy or restricting function; intensive care unit admission; and death. The utility of pre-operative PET/CT in detecting metastasis to the para-aortic lymph nodes was assessed by estimating the sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) of the PET/CT to identify para-aortic lymph node metastasis that were identified by laparoscopic extraperitoneal para-aortic lymphadenectomy. The study was planned to include a total of 60 patients.
Results
A total of 65 patients were enrolled in this study. Five patients were excluded from the final analysis because blood glucose levels too high to permit safe PET/CT (n=2); supraclavicular nodal metastases were detected on PET/CT and surgery was cancelled (n=2); or the patient agreed to participate in the trial but never returned after giving informed consent (n=1). Patient characteristics for the remaining 60 patients are shown in Table 1. The median age at diagnosis was 48 years (range, 23-84). A total of 35 patients (58%) had prior abdominal surgery. The median time from PET/CT to surgery was 3 days (range, 0-44).
Table 1.
Patient characteristics
| Median | Total N=60 |
|---|---|
| Age, years, median (range) | 48 (23-84) |
| Body mass index, kg/m2, median (range) | 26.7 (15.2-41.3) |
| Histology, no. of patients (%) | |
| Squamous cell carcinoma | 48 (80) |
| Adenocarcinoma | 9 (15) |
| Neuroendocrine carcinoma | 2 (3) |
| Transitional cell carcinoma | 1 (2) |
| Stage, no. of patients (%) | |
| IB2 | 16 (27) |
| IIA | 12 (20) |
| IIB | 16 (27) |
| IIIA | 4 (6) |
| IIIB | 12 (20) |
The median operative time was 140 minutes (range, 89-252). The median blood loss was 22.5 ml (range, 5-150). There was one intraoperative complication: bleeding from an ascending lumbar vein at the level of the left renal vein. Attempts to control bleeding by laparoscopy were unsuccessful and a Jincision was made to permit access to the retroperitoneum and control of the bleeding. The median length of hospital stay was 1 day (range, 0-4). Five procedures were performed as an outpatient procedure. The median number of lymph nodes retrieved was 11 (range, 1-39). Seven patients (12%) developed a lymphocyst postoperatively requiring drain placement. Six of these seven patients were part of the first 30 patients entered in the study. There were no other postoperative complications. The median time from surgery to initiation of radiotherapy was 10 days (range, 2-167). One patient was delayed 167 days to start radiation therapy for financial and social reasons. The median time from surgery to initiation of radiotherapy in patients who developed a lymphocyst was 12 days (range, 5-20).
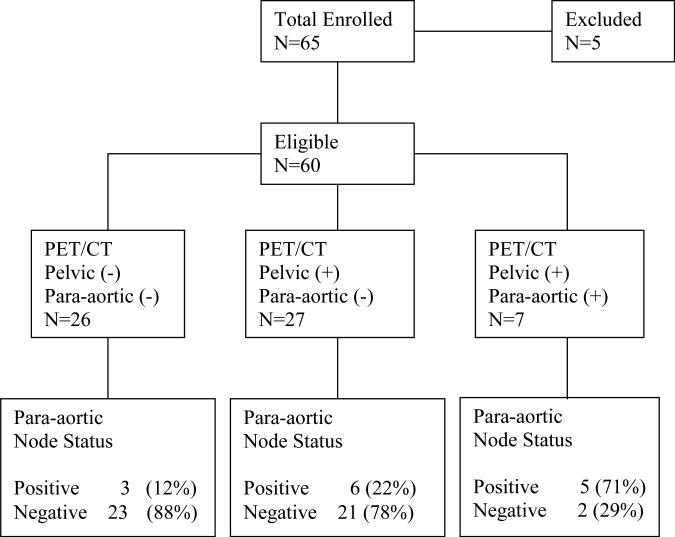
Fourteen patients (23%) were found to have histopathologically positive para-aortic nodes. Of these, seven (50%) had evidence of grossly positive paraaortic nodes at surgery. Of the remaining seven patients, six were found to have metastases in the para-aortic nodes through routine H&E staining and one patient was found to have evidence of micrometastases by ultrastaging. Twenty-six patients had preoperative PET/CT scans that were negative for pelvic and para-aortic lymphadenopathy (Figure 2). Of these, three patients (12%) were found to have histopathologically positive para-aortic nodes. Twenty-seven patients had preoperative PET/CT scans that showed evidence of positive pelvic nodes but were negative for para-aortic lymphadenopathy. Of these, six patients (22%) had para-aortic disease on final pathology. Seven patients had preoperative PET/CT scans that showed evidence of positive pelvic and paraaortic nodes. Of these, five patients (71.4%) had metastases in the para-aortic nodes on final pathology.
Figure 2.
PET/CT findings and correlation with final pathology
The sensitivity and specificity of PET/CT in detecting positive para-aortic nodes in the study patients, who had no evidence of para-aortic metastasis on CT or MRI, were 36% and 96%, respectively. The positive- and negative predictive values of PET/CT for para-aortic metastasis were 71% and 83%, respectively. For the subset of patients with positive pelvic lymph nodes on preoperative PET/CT the sensitivity of PET/CT for identifying para-aortic lymph node metastases was 45%, the specificity was 91%, the PPV was 71% and the NPV was 78%.
Eleven patients (18.3%) had a treatment modification based on surgical or final pathologic findings. Thirteen (93%) of 14 patients with documented disease in the para-aortic nodes went on to receive extended field radiation therapy. Of the seven patients with a preoperative PET/CT demonstrating evidence of paraaortic nodal involvement, five patients with confirmed metastatic disease by final pathology were treated with extended field. Survival events are still maturing and will be the subject of a later report.
Discussion
The key finding from our study is that laparoscopic extraperitoneal paraaortic lymphadenectomy is safe and feasible in patients with locally advanced cervical cancer. In addition, we found that in patients with positive pelvic lymph nodes and negative para-aortic nodes on preoperative PET/CT, the rate of histopathologically positive para-aortic nodes was 22%. In our cohort, nearly 20% of patients had a modification in their treatment plan based on the pathologic findings from para-aortic lymphadenectomy.
Recent studies have shown that surgical staging of patients with locally advanced cervical cancer may lead to a treatment modification in 18-44% of patients. 9-13 A study by the Gynecologic Oncology Group of 320 patients with cancer of the cervix who were surgically staged showed para-aortic node metastases in 21% of stage IIB, 31% of stage III, and 13% of stage IVA patients.6 In addition to the prognostic and therapy-directing value of surgical staging, there is recent evidence that patients may gain a therapeutic benefit from removal of para-aortic lymph nodes affected with metastatic disease. A recent review of three phase III trials by the Gynecologic Oncology Group compared patients with cervical cancer who had negative para-aortic lymph nodes established by pretreatment surgical staging with patients who had only radiographic exclusion of para-aortic node metastases before they received treatment with radiation plus cisplatin-based chemotherapy. The authors showed that there was a survival advantage for women who underwent surgical staging compared to those who were treated based on radiologic findings alone 14 .
The ideal surgical approach remains elusive. Marnitz et al. 10 reported their experience with laparoscopic transperitoneal surgical staging in 84 patients with locally advanced cervical cancer. The authors showed that removal of metastatic lymph nodes was associated with significant improvement in overall survival. Interestingly, it was shown that there was a significant survival benefit for patients if more than five para-aortic nodes were removed, compared to patients in whom fewer than five para-aortic nodes were removed. In another study, by LeBlanc et al., 9 the investigators performed surgical staging by a laparoscopic extraperitoneal approach in 156 patients with locally advanced cervical cancer. The authors noted that para-aortic node dissection may have a therapeutic benefit as survival for patients with microscopic nodal disease treated with extended-field radiotherapy concurrently with chemotherapy was similar to patients with node-negative disease who received pelvic radiotherapy alone. To date, only one trial has prospectively evaluated the role of pretreatment surgical staging for locally advanced cervical carcinoma in a randomized fashion. 15 The authors of that study reported that patients who underwent surgical staging had worse survival. However, in that study, the number of patients in the surgical staging group was low, standard treatment was not performed in 13% of patients, the proportion of patients with unfavorable histologies and who did not receive concurrent chemotherapy with radiotherapy was higher in the surgical staging group, and the time to start of radiotherapy was significantly longer in the surgical staging group.
In our study, we showed that surgical staging by a laparoscopic extraperitoneal approach is safe and feasible. Our median blood loss, operative time, and intraoperative- and postoperative complication rates were similar to those previously reported for studies using a similar laparoscopic approach. 4,9,16-19 The fact that our complication rates were low is particularly important in light of the fact that the complication rate of extended-field radiotherapy is estimated to be 10-14%. 20 Our laparoscopic extraperitoneal approach also offers patients the benefit of a faster recovery. In our cohort, the median length of hospitalization was 1 day, and in five patients, the procedure was performed as an outpatient procedure. Others have also shown that laparoscopic extraperitoneal lymphadenectomy can be performed safely as an outpatient procedure. 21
In our study, the median time to initiation of radiotherapy was only 10 days. In comparison, Sonoda et al. 18 reported a median interval from surgery to radiotherapy of 3.2 weeks in patients undergoing laparoscopic extraperitoneal para-aortic lymphadenectomy. Time to radiotherapy initiation in both our study and the series by Sonoda et al. compares favorably to that in a study of open extraperitoneal lymph node dissection, where the time to initiation of radiotherapy following the procedure was 32 days. 12 In addition, because of the findings at the time of surgery, a significant number of patients will have their treatments modified. Others have shown that surgical staging of patients with cervical cancer can lead to modifications of radiation field in up to 43% of patients. 13
Radiographic imaging is often used as an alternative to surgical staging to determine the status of the para-aortic lymph nodes. Unfortunately, routine CT or MRI is hindered by limited sensitivity and high false-negative rates. Hertel et al. 22 concluded that there was a poor correlation between the histopathologic status of the resected para-aortic nodes and the results of CT and MRI. Tsai et al. 23 evaluated the utility of PET in determining the appropriate treatment field for cervical cancer patients with enlarged pelvic nodes on CT or MRI. They found that PET findings modified treatment in 28% of patients.
Rose et al. 24 evaluated the utility of PET in detecting para-aortic nodal metastasis in patients with locally advanced cervical cancer and no evidence of extrapelvic disease before planned surgical staging lymphadenectomy. In that study, patients were operated on via a laparotomy extraperitoneal approach, and dissection was limited to the inferior mesenteric artery. The authors found that PET had a sensitivity of 75% and a specificity of 92%. Mortier et al. 16 evaluated the role of laparoscopic para-aortic lymphadenectomy (extraperitoneal in 47 patients and transperitoneal in 22 patients) and PET in staging of cervical carcinoma and found that in the subgroup of patients with negative findings on PET scan, 11% had metastases on histopathologic evaluation of the surgical specimen.
Combined PET/CT offers the anatomic details of CT scan together with the metabolic information provided by PET scan. 25 The largest study to date comparing PET/CT findings with histopathologic findings after laparotomy for extraperitoneal para-aortic lymphadenectomy was recently reported by Yildirim et al. 26 In that study, 16 patients with stage IIB-IVA cervical cancer who had no evidence of nodal metastases on CT underwent PET/CT followed by surgery. The authors reported that the sensitivity and specificity of PET/CT in detecting metastasis to the para-aortic nodes were 75% and 50%, respectively. Treatment was modified based on PET/CT findings in 25% of patients.
In summary, we found that laparoscopic extraperitoneal para-aortic lymphadenectomy is safe and feasible. Our results suggest that this procedure should be discussed with patients with locally advanced cervical cancer scheduled to undergo chemoradiation, particularly if preoperative PET/CT shows positive pelvic nodes and negative para-aortic nodes. A prospective randomized trial evaluating the impact of surgical staging on disease-free interval and overall survival is currently being developed in our institution to address this important question.
Condensed Abstract.
Laparoscopic extraperitoneal para-aortic staging is safe and feasible and should be considered prior to radiation therapy in patients with locally-advanced cervical cancer. The correlation of PET/CT findings with histopathologic results is limited.
Acknowledgment
We wish to thank Drs. Denis Querleu and Eric LeBlanc for their mentorship. We wish to thank Jacalyn B. Gano and Jody Folloder for their valuable input in this study. This work was supported in part by the Cancer Center Support Grant (NCI Grant P30 CA016672).
Footnotes
Manuscript was presented at the Society of Gynecologic Oncology 41st Annual Meeting, San Francisco, CA March, 2010
REFERENCES
- 1.Lagasse LD, Creasman WT, Shingleton HM, et al. Results and complications of operative staging in cervical cancer: Experience of the Gynecologic Oncology Group. Gynecol Oncol. 1980;9:90–98. doi: 10.1016/0090-8258(80)90013-x. [DOI] [PubMed] [Google Scholar]
- 2.Stehman FB, Bundy BN, DiSaia PJ, et al. Carcinoma of the cervix treated with radiation therapy: A multi-variate analysis of prognostic variables in the Gynecologic Oncology Group. Cancer. 1991;67:2776–2785. doi: 10.1002/1097-0142(19910601)67:11<2776::aid-cncr2820671111>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 3.Berman ML, Lagasse LD, Watring WG, et al. The operative evaluation of patients with cervical carcinoma by an extraperitoneal approach. Obstet Gynecol. 1977;50:658–664. [PubMed] [Google Scholar]
- 4.Querleu D, Dargent D, Ansquer Y, et al. Extraperitoneal endosurgical aortic and common iliac dissection in the staging of bulky or advanced cervical carcinomas. Cancer. 2000;88:1883–1891. [PubMed] [Google Scholar]
- 5.Vergote I, Pouseele B, van Gorp T, et al. Robotic retroperitoneal lower para-aortic lymphadenectomy in cervical carcinoma: first report on the technique used in 5 patients. Acta Ostet Gynecol Scand. 2008;87:783–787. doi: 10.1080/00016340802146946. [DOI] [PubMed] [Google Scholar]
- 6.Heller PB, Malfetano JH, Bundy BN, et al. Clinical-pathologic study of stage IIB, III, and IVA carcinoma of the cervix: Extended diagnostic evaluation for para-aortic node metastasis—A Gynecologic Oncology Group study. Gynecol Oncol. 1990;38:425–430. doi: 10.1016/0090-8258(90)90085-y. [DOI] [PubMed] [Google Scholar]
- 7.Choi HJ, Roh JW, Seo SS, et al. Comparison of the accuracy of magnetic resonance imaging and positron emission tomography/computed tomography in the presurgical detection of lymph node metastases in patients with uterine cervical carcinoma. Cancer. 2006;106:914–922. doi: 10.1002/cncr.21641. [DOI] [PubMed] [Google Scholar]
- 8.Grigsby PW, Siegel BA, Dehdashti F. Lymph node staging by positron emission tomography in patients with carcinoma of the cervix. J Clin Oncol. 2001;19:3745–3749. doi: 10.1200/JCO.2001.19.17.3745. [DOI] [PubMed] [Google Scholar]
- 9.Leblanc E, Narducci F, Frumovitz M, et al. Therapeutic value of pretherapeutic extraperitoneal laparoscopic staging of locally advanced cervical carcinoma. Gynecol Oncol. 2007;105:304–311. doi: 10.1016/j.ygyno.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 10.Marnitz S, Kohler C, Roth C, et al. Is there a benefit of pretreatment laparoscopic transperitoneal surgical staging in patients with advanced cervical cancer? Gynecol Oncol. 2005;99:536–544. doi: 10.1016/j.ygyno.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Denschlag D, Gabriel B, Mueller-Lantzsch C, et al. Evaluation of patients after extraperitoneal lymph node dissection for cervical cancer. Gynecol Oncol. 2005;96:658–664. doi: 10.1016/j.ygyno.2004.08.053. [DOI] [PubMed] [Google Scholar]
- 12.Hasenburg A, Salama JK, Van TJ, et al. Evaluation of patients after extraperitoneal lymph node dissection and subsequent radiotherapy for cervical cancer. Gynecol Oncol. 2002;84:321–326. doi: 10.1006/gyno.2001.6528. [DOI] [PubMed] [Google Scholar]
- 13.Goff BA, Muntz HG, Paley PJ, et al. Impact of surgical staging in women with locally advanced cervical cancer. Gynecol Oncol. 1999;74:436–442. doi: 10.1006/gyno.1999.5472. [DOI] [PubMed] [Google Scholar]
- 14.Gold MA, Tian C, Whitney CW, et al. Surgical versus radiographic determination of para-aortic lymph node metastases before chemoradiation for locally advanced cervical carcinoma: a Gynecologic Oncology Group study. Cancer. 2008;112:1954–1963. doi: 10.1002/cncr.23400. [DOI] [PubMed] [Google Scholar]
- 15.Lai CH, Huang KG, Hong JH, et al. Randomized trial of surgical staging (extraperitoneal or laparoscopic) versus clinical staging in locally advanced cervical cancer. Gynecol Oncol. 2003;89:160–167. doi: 10.1016/s0090-8258(03)00064-7. [DOI] [PubMed] [Google Scholar]
- 16.Mortier DG, Stroobants S, Amant F, et al. Laparoscopic para-aortic lymphadenectomy and positron emission tomography scan as staging procedures in patients with cervical carcinoma stage IB2-IIIB. Int J Gynecol Cancer. 2008;18:723–729. doi: 10.1111/j.1525-1438.2007.01061.x. [DOI] [PubMed] [Google Scholar]
- 17.Burnett AF, O'Meara AT, Bahador A, et al. Extraperitoneal laparoscopic lymph node staging: the University of Southern California experience. Gynecol Oncol. 2004;95:189–192. doi: 10.1016/j.ygyno.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Sonoda Y, Leblanc E, Querleu D, et al. Prospective evaluation of surgical staging of advanced cervical cancer via a laparoscopic extraperitoneal approach. Gynecol Oncol. 2003;91:326–331. doi: 10.1016/j.ygyno.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Vasilev SA, McGonigle KF. Extraperitoneal laparoscopic para-aortic lymph node dissection. Gynecol Oncol. 1996;61:315–320. doi: 10.1006/gyno.1996.0149. [DOI] [PubMed] [Google Scholar]
- 20.Marcial VA, Marcial LV. Radiation therapy for cervical cancer. New developments. Cancer. 1993;71:1438–1445. [PubMed] [Google Scholar]
- 21.Tillmans T, Lowe MP. Safety, feasibility, and costs of outpatient laparoscopic extraperitoneal aortic nodal dissection for locally advanced cervical carcinoma. Gynecol Oncol. 2007;106:370–374. doi: 10.1016/j.ygyno.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Hertel H, Kohler C, Elhawary T, et al. Laparoscopic staging compared with imaging techniques in the staging of advanced cervical cancer. Gynecol Oncol. 2002;87:46–51. doi: 10.1006/gyno.2002.6722. [DOI] [PubMed] [Google Scholar]
- 23.Tsai CS, Chang TC, Lai CH, et al. Preliminary report of using FDG-PET to detect extrapelvic lesions in cervical cancer patients with enlarged pelvic lymph nodes on MRI/CT. Int J Radiat Oncol Biol Phys. 2004;58:1506–1512. doi: 10.1016/j.ijrobp.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 24.Rose PG, Adler LP, Rodriguez M, et al. Positron emission tomography for evaluating para-aortic nodal metastasis in locally advanced cervical cancer before surgical staging: A surgicopathologic study. J Clin Oncol. 1999;17:41–45. doi: 10.1200/JCO.1999.17.1.41. [DOI] [PubMed] [Google Scholar]
- 25.Beyer T, Townsend DW, Brun T, et al. A combined PET/CT scanner for clinical oncology. J Nucl Med. 2000;41:1369–1379. [PubMed] [Google Scholar]
- 26.Yildirim Y, Sehirali S, Avci ME, et al. Integrated PET/CT for the evaluation of para-aortic nodal metastasis in locally advanced cervical cancer patients with negative conventional CT findings. Gynecol Oncol. 2008;108:154–159. doi: 10.1016/j.ygyno.2007.09.011. [DOI] [PubMed] [Google Scholar]