Abstract
Objective
To determine the proportion of young patients with early-stage invasive cervical cancer treated with radical hysterectomy who may have been eligible for fertility-sparing surgery consisting of cervical conization with pelvic lymph node dissection.
Methods
We retrospectively identified all patients with early-stage cervical cancer (stage IA2-IB1) who underwent a radical hysterectomy at The University of Texas M. D. Anderson Cancer Center between 1990 and 2009. We reviewed these patients’ records to identify patients who were < 40 years who had not previously undergone tubal ligation and who would have been considered candidates for cold-knife conization with pelvic lymph node dissection—i.e., women with tumors smaller than 2 cm, low-risk histology (squamous, adenocarcinoma, or adenosquamous), and no lymphovascular space invasion (LVSI).
Results
A total of 507 patients with early-stage cervical cancer were identified who underwent radical hysterectomy during the review period. Of these women, 277 (55%) were 40 years or younger. Of these 277 patients, 75 (27%) had had a previous tubal ligation and 202 (73%) had not. Of these 202 patients potentially interested in fertility preserving surgery, 53 (26%) had favorable pathologic characteristics including low-risk histology, tumors ≤2cms in size and no LVSI present. Of these 53 patients, none had parametrial involvement or positive lymph nodes.
Conclusion
Among 202 women with age younger than 40 years and no previous tubal ligation who underwent radical hysterectomy, 53 (26%) may have been eligible for fertility-sparing surgery such as cold-knife conization with pelvic lymph node dissection.
Introduction
It is estimated that women under the age of 45 years old account for 22% of the new cases diagnosed each year [1]. Statistics from the U.S. Census Bureau indicate that 28 in 1000 U.S. women will give birth to their first child between the ages of 30 and 34 years and 10 in 1000 will give birth to their first child between the ages of 35 and 39 years [2]. The relatively young age at which cervical cancer is often diagnosed, coupled with the postponement of childbearing, poses new challenges in the management of this disease.
The standard surgical management for early-stage cervical carcinoma, stage IA2 and IB1, is radical hysterectomy and bilateral pelvic lymph node dissection. In 1994, Dargent reported a fertility-sparing surgical approach for young patients with cervical cancer known as a radical trachelectomy [3]. Since that initial report, a number of other institutions have published their experiences with the vaginal, the abdominal, and more recently, the robotic approach to radical trachelectomy [4–8].
Radical trachelectomy performed through any of the techniques described is a complex procedure with varying impact on future fertility. A review of the literature revealed a 41–79% success pregnancy rate in patients who attempted conception after radical trachelectomy [9]. Among the pregnancies that occurred, 18% ended in a miscarriage, and 38% resulted in preterm delivery (< 37 weeks). Another study noted a 20% risk of preterm labor, with approximately 21% of pregnancies ending in miscarriage in the first trimester and 8% ending in miscarriage in the second trimester [10].
The morbidity associated with abdominal or vaginal radical trachelectomy is not insignificant. Complications are seen in about 10–15% of cases of abdominal or vaginal radical trachelectomy with laparoscopic lymphadenectomy. These complications have included bladder or bowel trauma, pelvic hematoma, pelvic abscess, and transient neuropathy requiring long-term catheterization [11]. Postoperative complications may also occur and have included dysmenorrhea, dysplastic Pap smears, irregular or intermenstrual bleeding, excessive vaginal discharge, isthmic stenosis, and amenorrhea [12].
Based on these observations, a number of investigators have studied the potential to preserve fertility with less radical surgery in highly selected low-risk patients. An early study by Kinney et al. evaluated 83 patients with stage IB1 squamous cell carcinoma of the cervix, with tumor size <2 cm and no lymphovascular space involvement (LVSI). None of the patients in that study were found to have parametrial involvement. A subsequent report by Covens and colleagues evaluated 842 patients with stage IA1 to IB1 cervical cancer who underwent radical hysterectomy. They noted that 33 patients (4%) had parametrial involvement. Parametrial involvement was associated with larger tumor size, LVSI, greater depth of invasion and positive pelvic lymph nodes. They performed a subset analysis of 536 patients with tumor size ≤2 cm, negative lymph nodes and <10 mm of cervical stromal invasion. In this subgroup of patients, the incidence of parametrial involvement was only 0.6%.
In 2004, Sonoda et al. [15] evaluated the percentage of patients with early-stage cervical cancer who underwent radical hysterectomy and who may have been eligible for laparoscopic radical vaginal trachelectomy. The authors found that approximately 48% of patients younger than 40 years of age with operable stage I cervical cancer would have been eligible for fertility-sparing surgery. Our goal was to define a subset of highly select patients who could undergo an even less radical surgery than a radical trachelectomy in the management of their early-stage cervical cancer. The objective of this study was to determine the percentage of young patients with early-stage invasive cervical cancer who were treated with radical hysterectomy who may have been eligible for a more conservative procedure such as cold-knife conization with pelvic lymph node dissection to maintain their fertility while avoiding the potential complications associated with a radical trachelectomy.
Methods
This study was approved by the Institutional Review Board of The University of Texas M.D. Anderson Cancer Center. A retrospective review was performed of all patients with early-stage cervical cancer (stage IA1 with lymphvascular space invasion (LVSI), stage IA2, and stage IB1) who underwent a radical hysterectomy at M. D. Anderson Cancer Center between 1990 and 2009. All medical records were reviewed for patient’s age, International Federation of Gynecology and Obstetrics stage, surgical history, tumor histology, tumor size, and evidence of LVSI. We identified patients younger than 40 years who did not have a history of tubal ligation who would have been considered candidates for conservative surgery consisting of cold-knife conization with pelvic lymph node dissection—i.e., women with a confirmed diagnosis of primary cervical cancer, a cervical tumor smaller than 2 cm, low-risk histology (squamous, adenocarcinoma, or adenosquamous), and no LVSI present on preoperative histology. All pathology specimens were reviewed and diagnoses were confirmed at M. D. Anderson Cancer Center by a gynecologic pathologist. Patients were excluded if information needed for data analysis was missing.
Because this was a retrospective study, information on desire to preserve fertility was not accessible from the patients’ medical records. Therefore, an age of 40 years or younger and no previous tubal ligation was used as surrogates for potential desire for future fertility. Also, since routine fertility evaluation is not performed in patients who are scheduled to undergo a radical hysterectomy, it was not possible to objectively evaluate fertility potential in this retrospective study.
Results
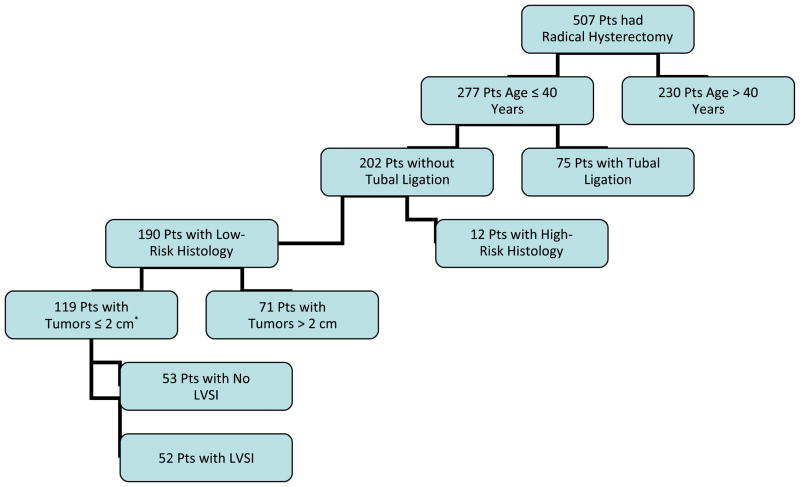
We identified 507 patients who underwent a radical hysterectomy at M. D. Anderson Cancer Center during the study period. Of these women, 277 (55%) were 40 years or younger. Of these 277 patients, 75 (27%) had a previous tubal ligation, while 202 (73%) did not. Of these 202 patients, 12 had high-risk histology (6 neuroendocrine, 3 clear cell, 1 small cell, 1 lymphoepithelioid carcinoma, 1 sarcoma), and 190 (94%) had low-risk histology (113 squamous carcinoma, 57 adenocarcinoma, and 20 adenosquamous carcinoma). Of these 190 women, 71 had tumors larger than 2 cm (stage IB1 in 65, IB2 in 3, IIA in 2, and IIB in 1), and 119 had tumors 2 cm or smaller. Interestingly, of these 119 patients, 57 (48%) were either nulliparous or had had just one child prior to radical hysterectomy. Of these 119 patients, 53 did not have LVSI. Therefore, among 202 women with age younger than 40 years and no previous tubal ligation who underwent a radical hysterectomy, 53 (26%) may have been eligible for a cervical conization with pelvic lymphadenectomy. The median depth of invasion in the tumors from the 53 patients deemed eligible for cervical conization was 4 mm. In addition, we found that 51 (96%) of these 53 patients had a depth of invasion less than 10 mm. Identification of patients eligible for fertility-sparing surgery is outlined in Figure 1.
Figure 1.
Schema of eligible patients for simple conization and pelvic lymphadenectomy
On final pathology, none of these 53 patients were found to have parametrial involvement or lymph node involvement. Data on adjuvant therapy were available for 51 of these 53 patients, and none of these patients received adjuvant therapy.
Discussion
In our study, we found that 53 (26%) of the 202 patients younger than 40 years who had not previously had tubal ligation and who underwent a radical hysterectomy may have been eligible for fertility-sparing surgery such as cold-knife conization with pelvic lymph node dissection. On the basis of the documented histology, tumor size, and absence of LVSI, a less radical surgical procedure would have been feasible and fertility could have been preserved. This was confirmed by the fact that final review of the pathology in these 53 patients revealed no evidence of parametrial or lymph node involvement. Due to the retrospective nature of our study, we were not able to collect information on fertility plans and acceptance of fertility sparing surgery at a time of diagnosis.
The surgical and reproductive outcomes, cure rates, and survival associated with radical trachelectomy have been previously evaluated. In a recent review of the literature by Gien and Covens [16], the authors reported that the intraoperative complication rate is 4% and postoperative complication rate is 12%. The most common intraoperative complications were bladder related, with vascular injuries being the second most common type of injury. The majority of postoperative complications were mainly related to bladder hypotonia. The authors also highlighted the fact that despite careful patient selection, 10–12% of patients who undergo a radical trachelectomy receive adjuvant treatment for positive pelvic lymph nodes, or for close or positive margins of the removed cervix. In addition, the authors reported that the tumor recurrence rates range from 4.2–5.3% and the death rate ranged from 2.5–3.2%.
Cibula et al. [17] recently reviewed abdominal radical trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer. The patients enrolled in that study were diagnosed with either stage IA2 or stage IB1 cervical cancer. The results of that study demonstrated that 29% of women who underwent abdominal radical trachelectomy were not able to preserve their fertility due to positive cranial margins or involved lymph nodes. In a recent study by Carter et al. [18], the authors evaluated the emotional, sexual, and physical impact of cancer-related infertility on gynecologic oncology survivors. In that study, 77% of patients reported clinically significant levels of distress in relation to loss of fertility or impaired fertility.
Although radical trachelectomy has been a very viable alternative to radical hysterectomy for fertility preservation in young women with early-stage cervical cancer, it is associated with considerable morbidity and obstetrical outcomes following this procedure are not ideal. In an effort to decrease the complication rate and improve obstetrical outcomes, further efforts have been made to identify a subgroup of patients with favorable characteristics who might be candidates for even less radical surgery than a radical trachelectomy.
The utility of parametrial resection in women with early stage cervical cancer is controversial. A recent study by Stegeman et al. evaluated 103 premenopausal patients with stage IA1 to IB1 cervical cancer. All patients had tumors measuring <2 cm in diameter, <10 mm of invasion and negative pelvic lymph nodes. Only two of the103 patients (1.9%) had parametrial involvement. Of note, both of these patients had LVSI present. Wright and colleagues subsequently reported on 594 patients who underwent radical hysterectomy. Parametrial involvement was noted in 64 patients (10.8%) and was associated with advanced grade, deep stromal invasion, LVSI, large tumor size and lymph node metastases. In a subgroup of 270 patients with negative lymph nodes, no LVSI and tumors <2 cm, the incidence of parametrial involvement was only 0.4%. Among these 270 patients, two recurrences (0.7%) were noted after a median follow-up of 59 months.
These data were consistent with those from a study by Frumovitz et al. [21], who evaluated the incidence of parametrial involvement in women with early-stage cervical cancer. One hundred twenty-five women (36%) had squamous, adenocarcinoma, or adenosquamous lesions, all grades, with primary tumor size 2 cm or smaller and no lymphvascular space invasion. In this group of patients, there was no pathologic evidence of parametrial involvement in any of the patients.
Recent studies by Rob et al. reported on the feasibility and safety of performing less radical, fertility-sparing surgery in women with stage IA1 to IB1 cervical carcinoma. Of the 40 patients enrolled, 6 (15%) had positive sentinel lymph nodes on frozen section, and radical hysterectomy with pelvic lymphadenectomy was immediately performed. In the remaining patients, only a pelvic lymphadenectomy was performed. Following a 7-day interval to allow pathologic confirmation of negative lymph nodes, a large cone or simple vaginal trachelectomy was performed. With a follow-up of 47 months, one recurrence has been reported in a patient with a stage IB1 tumor with 8 mm invasion and LVSI present. Of the 24 women who tried to conceive, 17 (71%) became pregnant and 11 delivered infants. The authors concluded that large cone or simple trachelectomy with laparoscopic pelvic lymph node dissection is safe and feasible with a high pregnancy rate in women with early stage cervical cancer.
At M. D. Anderson Cancer Center and other sites, a prospective, international, multi-institutional cohort study evaluating the safety and feasibility of performing conservative surgery in women with stage IA2-IB1 cervical cancer with favorable histologic characteristics (histologically confirmed squamous cell or adenocarcinoma of the cervix; tumor diameter 2 cm or less on examination or imaging studies; no LVSI) is in process. Patients desiring future fertility undergo a cone biopsy and laparoscopic, robotic, or open pelvic lymph node dissection only. Patients not desiring future fertility undergo laparoscopic, robotic, or open simple hysterectomy and pelvic lymph node dissection with lymphatic mapping. The primary end point of the study is recurrence rate at 2 years.
All patients diagnosed with early-stage cervical cancer who are interested in future fertility should be encouraged to discuss less radical options for treatment, including cold-knife conization. If fertility-preserving surgery is desired, the patient should be referred to centers with a gynecologic oncologist specializing in fertility-sparing treatment who may counsel the patient of all her options.
Footnotes
Conflict of Interest Statement
The authors have no conflict of interest to declare
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.SEER Cancer Statistics Review 1975–2005. ( http://seer.cancer.gov/csr/1975-2005/results_single/sect_01_table.10_2pgs.pdf)
- 2.Bachu A, O’Connell M. Current Population Reports. Washington (DC): U.S. Census Bureau; 2001. Fertility of American Women: June 2000; pp. 20RV–543RV. [Google Scholar]
- 3.Dargent D, Brun JL, Roy M, Mathevet P, Remy I. La trachelectomie elargie (te), une alternative a l’hysterectomie radicale dans le traitement des cancers infiltrants developpes sur la face externe du col uterin. J Obstet Gynecol. 1994;2:285–292. [Google Scholar]
- 4.Ramirez PT, Schmeler KM, Malpica A, Soliman PT. Safety and feasibility of robotic radical trachelectomy in patients with early-stage cervical cancer. Gynecol Oncol. 2010;116:512–5. doi: 10.1016/j.ygyno.2009.10.063. [DOI] [PubMed] [Google Scholar]
- 5.Geisler JP, Orr CJ, Manahan KJ. Robotically assisted total laparoscopic radical trachelectomy for fertility sparing in stage IB1 adenosarcoma of the cervix. J Laparoendosc Adv Surg Tech A. 2008;18:727–9. doi: 10.1089/lap.2007.0236. [DOI] [PubMed] [Google Scholar]
- 6.Persson J, Kannisto P, Bossmar T. Robot-assisted abdominal laparoscopic radical trachelectomy. Gynecol Oncol. 2008;111:564–7. doi: 10.1016/j.ygyno.2008.05.034. [DOI] [PubMed] [Google Scholar]
- 7.Chuang LT, Lerner DL, Liu CS, Nezhat FR. Fertility-sparing robotic-assisted radical trachelectomy and bilateral pelvic lymphadenectomy in early-stage cervical cancer. J Minim Invasive Gynecol. 2008;15:767–70. doi: 10.1016/j.jmig.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Ungar L, Palfalvi L, Hogg R, Siklos P, Boyle DC, Del Priore G, et al. Abdominal radical trachelectomy: a fertility-preserving option for women with early cervical cancer. BJOG. 2005;112:366–9. doi: 10.1111/j.1471-0528.2004.00421.x. [DOI] [PubMed] [Google Scholar]
- 9.Beiner ME, Covens A. Surgery insight: radical vaginal trachelectomy as a method of fertility preservation for cervical cancer. Nat Clin Pract Oncol. 2007;4:353–61. doi: 10.1038/ncponc0822. [DOI] [PubMed] [Google Scholar]
- 10.Mandic A, Novakovic P, Nincic D, Zivaljevic M, Rajovic J. Radical abdominal trachelectomy in the 19th gestation week in patients with early invasive cervical carcinoma: case study and overview of literature. Am J Obstet Gynecol. 2009;201:e6–8. doi: 10.1016/j.ajog.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Koliopoulos G, Sotiriadis A, Kyrgiou M, Martin-Hirsch P, Makrydimas G, Paraskevaidis E. Conservative surgical methods for FIGO stage IA2 squamous cervical carcinoma and their role in preserving women’s fertility. Gynecol Oncol. 2004;93:469–73. doi: 10.1016/j.ygyno.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Alexander-Sefre F, Chee N, Spencer C, Menon U, Shepherd JH. Surgical morbidity associated with radical trachelectomy and radical hysterectomy. Gynecol Oncol. 2006;101:450–4. doi: 10.1016/j.ygyno.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 13.Kinney WK, Hodge DO, Egorshin EV, Ballard DJ, Podratz KC. Identification of a low-risk subset of patients with stage IB invasive squamous cancer of the cervix possibly suited to less radical surgical treatment. Gynecol Oncol. 1995;57:3–6. doi: 10.1006/gyno.1995.1091. [DOI] [PubMed] [Google Scholar]
- 14.Covens A, Rosen B, Murphy J, Laframboise S, DePetrillo AD, Lickrish G, Colgan T, Chapman W, Shaw P. How important is removal of the parametrium at surgery for carcinoma of the cervix? Gynecol Oncol. 2002;84:145–9. doi: 10.1006/gyno.2001.6493. [DOI] [PubMed] [Google Scholar]
- 15.Sonoda Y, Abu-Rustum NR, Gemignani ML, Chi DS, Brown CL, Poynor EA, et al. A fertility-sparing alternative to radical hysterectomy: how many patients may be eligible? Gynecol Oncol. 2004;95:534–8. doi: 10.1016/j.ygyno.2004.07.060. [DOI] [PubMed] [Google Scholar]
- 16.Gien LT, Covens A. Fertility-sparing options for early stage cervical cancer. Gynecol Oncol. 2010;117:350–7. doi: 10.1016/j.ygyno.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 17.Cibula D, Slama J, Svarovsky J, Fischerova D, et al. Abdominal radical trachelectomy in fertility-sparing treatment of early-stage cervical cancer. Int J Gynecol Cancer. 2009;19:1407–11. doi: 10.1111/IGC.0b013e3181b9549a. [DOI] [PubMed] [Google Scholar]
- 18.Carter J, Chi DS, Brown CL, Abu-Rustum NR, Sonoda Y, Aghajanian C, Levine DA, Baser RE, Raviv L, Barakat RR. Cancer-related infertility in survivorship. Int J Gynecol Cancer. 2010;20:2–8. doi: 10.1111/IGC.0b013e3181bf7d3f. [DOI] [PubMed] [Google Scholar]
- 19.Stegeman M, Louwen M, van der Velden J, ten Kate FJ, den Bakker MA, Burger CW, Ansink AC. The incidence of parametrial tumor involvement in select patients with early cervix cancer is too low to justify parametrectomy. Gynecol Oncol. 2007;105:475–80. doi: 10.1016/j.ygyno.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 20.Wright JD, Grigsby PW, Brooks R, Powell MA, Gibb RK, Gao F, Rader JS, Mutch DG. Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy. Cancer. 2007;110:1281–6. doi: 10.1002/cncr.22899. [DOI] [PubMed] [Google Scholar]
- 21.Frumovitz M, Sun CC, Schmeler KM, Deavers MT, Dos Reis R, Levenback CF, et al. Parametrial involvement in radical hysterectomy specimens for women with early-stage cervical cancer. Obstet Gynecol. 2009;114:93–9. doi: 10.1097/AOG.0b013e3181ab474d. [DOI] [PubMed] [Google Scholar]
- 22.Rob L, Pluta M, Strnad P, Hrehorcak M, Chmel R, Skapa P, et al. A less radical treatment option to the fertility-sparing radical trachelectomy in patients with stage I cervical cancer. Gynecol Oncol. 2008;111:S116–20. doi: 10.1016/j.ygyno.2008.07.021. [DOI] [PubMed] [Google Scholar]