Abstract
Anterior hip pain is common in young, active adults. Clinically, we have noted that patients with anterior hip pain often walk in a swayback posture, and that their pain is reduced when the posture is corrected. The purpose of this study was to investigate a potential mechanism for the reduction in pain by testing the effect of posture on movement patterns and internal moments during gait in healthy subjects. Fifteen subjects were instructed to walk while maintaining three postures: 1) natural, 2) swayback, and 3) forward flexed. Kinematic and force data were collected using a motion capture system and a force plate. Walking in the swayback posture resulted in a higher peak hip extension angle, hip flexor moment and hip flexion angular impulse compared to natural posture. In contrast, walking in a forward flexed posture resulted in a decreased hip extension angle and decreased hip flexion angular impulse. Based on these results, walking in a swayback posture may result in increased forces required of the anterior hip structures, potentially contributing to anterior hip pain. This study provides a potential biomechanical mechanism for clinical observations that posture correction in patients with hip pain is beneficial.
Keywords: gait, posture, hip, kinematics, kinetics
1. Introduction
Anterior hip or groin pain is an increasingly common complaint in young active adults (Meyers et al., 2008). Potential causes of this pain include a tear of the acetabular labrum (Fitzgerald, 1995; Byrd, 1996; Lewis and Sahrmann, 2006) or structural abnormalities of the hip including dysplasia (Dorrell and Catterall, 1986; Klaue et al., 1991; McCarthy and Lee, 2002) and femoroacetabular impingement (FAI) as initially proposed by Ganz and colleagues (Ito et al., 2001; Ganz et al., 2003; Beck et al., 2005) and more recently reported by others (Philippon et al., 2007; Clohisy et al., 2009; Nepple et al., 2013; Sankar et al., 2013; Byrd, 2014). Overuse of anterior hip structures, such as the hip flexor muscles, particularly the iliopsoas may also result in anterior hip pain (Johnston et al., 1998; Anderson et al., 2001).
Clinically, we have noted that a number of patients with anterior hip pain stand and walk in a swayback posture, and that their pain is immediately reduced when positioned in a more neutral posture. A swayback posture has been described as an atypical posture “in which there is a posterior displacement (swaying back) of the upper trunk and an anterior displacement (swaying forward) of the pelvis [which] is in posterior tilt” (Kendall et al., 1993) (p 419). In the swayback standing posture, the body's line of gravity passes posterior to the hip (Somers, 2001). During gait, therefore, the swayback posture may require the generation of a hip flexor moment of higher magnitude or longer duration, than a posture in which the line of gravity passes through or anterior to the hip. The increased magnitude and longer duration moment may result in repetitive microtrauma and pain. Reducing the required moment would theoretically reduce the force required from the muscular tissue and thereby reduce the pain.
As part of a treatment program, we instruct patients with anterior hip pain who stand and walk in a swayback posture to change their posture and movement patterns (Sahrmann, 2002; Lewis and Sahrmann, 2006). The patients are instructed to maintain the trunk in line with the pelvis. The patients are also instructed to avoid hip and knee extension beyond neutral during gait (Hunt et al., 2012). Specifically, patients are instructed to ‘flex the knee’ and ‘roll over’ the foot more in the late stance phase of gait than they do naturally. Often, these modifications of posture and gait result in an immediate reduction in the patient's anterior hip pain.
The purpose of this study was to investigate a potential mechanism for the clinically observed reduction in anterior hip pain by investigating the effect of posture on the movement patterns and the required moments during gait in healthy subjects. We hypothesized that walking in a swayback posture would require greater hip extension motion and greater hip flexor moments than walking in a natural posture. We also hypothesized that walking in a forward flexed posture with the hips and knees maintained in slight flexion, an exaggeration of the correction given to patients with anterior hip pain (Sahrmann, 2002), would reduce hip extension and reduce the moment requirements of the anterior hip muscles when compared to the natural posture. Modifications at one joint can have clinically important consequences at other joints (Zajac, 1993; Sueki et al., 2013), therefore, we also investigated changes in kinematics and kinetics at the knee and ankle.
2. Methods
2.1 Subjects
A convenience sample of fifteen healthy and asymptomatic subjects (3 males, 12 females) participated in this study (Table 1). All subjects agreed to participate voluntarily and signed informed consent forms approved by the Washington University Medical School Institutional Review Board prior to participation. Inclusion criteria were: age between 18 and 50 years old, and self-reported good health. Exclusion criteria were: (i) history of hip or back pain lasting greater than 1 week within the past 5 years, (ii) current lower extremity injury, and (iii) hip pain with active straight leg raising or passive hip flexion with adduction and medial rotation (anterior impingement test), two tests which are sensitive for labral tears (Narvani et al., 2003; Troelsen et al., 2009) and FAI (Clohisy et al., 2009). Each subject's posture was visually screened by an experienced physical therapist for obvious or significant postural deviations, and none were noted. We selected only healthy, asymptomatic subjects for this study in order to eliminate the effect of pain on movement pattern (Hodges and Tucker, 2011).
Table 1.
Characteristics of subjects who participated in this study, mean (range).
| Subjects (N=15) | |
|---|---|
| Sex | 12 females, 3 males |
| Age (years) | 29.5 (22-38) |
| Height (cm) | 170.6 (161-190) |
| Mass (kg) | 68.0 (54.0-93.0) |
| BMI (kg/m2) | 23.2 (19.7-26.0) |
2.2 Instrumentation
Kinematic and kinetic data were collected using a 6 camera, motion capture system (Motion Analysis Corp., Santa Rosa, CA, USA) sampling at 60Hz. Ground reaction forces during walking were measured at 1200Hz using a Bertec force plate (Columbus, OH, USA) imbedded in the middle of the 20-foot (6.1 meter) walkway. A standard Helen Hayes marker set (Kadaba et al., 1990) was used for kinematic data collection. Retroreflective markers were placed bilaterally between the heads of the second and third metatarsals, on the posterior aspect of the calcaneus, and on the medial and lateral malleoli, medial and lateral knee joint lines, and anterior superior iliac spine. A 3.75-inch (9.5 cm) stick with a retroreflective marker attached to the end of it was placed on the sacrum equidistant between the posterior superior iliac spines, as well as laterally on bilateral shank and thigh.
2.3 Experimental procedures
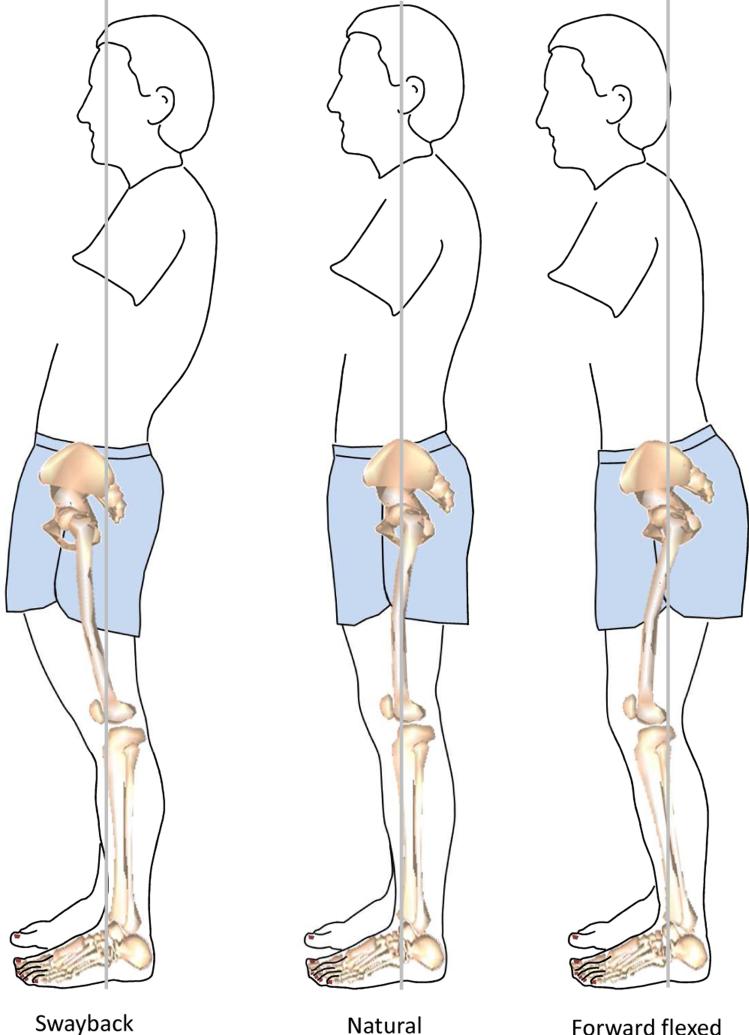
After markers were placed on the subject, the subject was asked to stand naturally while a static neutral standing trial was obtained to create a model. The medial markers, which were used to establish knee and ankle joint centers, were then removed to allow normal gait. Each subject was instructed to walk barefoot along the walkway at a self-selected speed. Practice trials were permitted until the subject was comfortable walking and was able to contact the force plate with only one foot without altering his or her gait. Typically, three or less practice trials were performed. Each subject was asked to walk while maintaining three different postures (Figure 1). First, each subject walked while maintaining the self-selected natural posture. The natural posture was collected first in order to capture each subject's typical posture prior to any modification. Second, each subject walked while maintaining a swayback posture. To facilitate the swayback posture, the subject was positioned in posterior pelvic tilt with the trunk posterior to the hips, and in hip and knee hyperextension. The subject was instructed to maintain the swayback posture while walking even though it would feel like “leading with the hips”. Third, each subject walked while maintaining a forward flexed posture. In order to facilitate the flexed posture, the subject was positioned in slight hip and knee flexion with the trunk leaned forward so that the trunk was in front of the hips. The subject was instructed to maintain this posture while walking and that it would feel like “leading with the head”. For the swayback and flexed postures, each subject was instructed to walk at the same speed as during the natural trials. To monitor walking speed, the subject was timed using a stop watch while walking 3.045 m. Based on pilot testing, a criterion of ± 0.4 seconds of the subject's average time for the natural trials was used and feedback was given if necessary after each trial to speed up or slow down. In order to be accepted, the subject had to walk within the expected time, contact the force plate with a single foot, and maintain the posture as determined visually. Three acceptable trials were obtained for each limb while maintaining each posture. For this study, only data from the right lower extremity were analyzed.
Figure 1.
The three postures maintained during gait. For the swayback posture, the subject was positioned in posterior pelvic tilt with the trunk posterior to the hips and in knee and hip hyperextension. For the self-selected natural posture, the subject was instructed to assume his or her normal posture. For the forward flexed posture, the subject was positioned in slight hip and knee flexion with the trunk leaned slightly forward of the hips.
2.4 Dependent Variables
2.4.1 Kinematic Variables
The primary kinematic variable of interest was the maximum hip extension angle during the stance phase of gait. We expected that in the swayback posture, maximum hip extension angle would increase compared to the natural posture. In the forward flexed posture, we expected hip extension would decrease compared to the natural posture. Changes in pelvic, knee and ankle angles in the sagittal plane were also investigated. We expected that the pelvic tilt angle would reflect the posture instructions. That is, in the swayback trial, the pelvis would be in decreased anterior pelvic tilt, while in the forward flexed trials, the pelvis would be in increased anterior pelvic tilt compared to the natural posture. We also expected greater knee extension and ankle dorsiflexion in the swayback posture, and greater knee flexion and ankle plantar flexion in the forward flexed posture.
2.4.2 Kinetic Variables
As the primary focus of this study was on the magnitude of the moment required of the hip musculature during walking, the kinetic variables included the peak hip flexor and extensor moments and the hip flexion and extension angular impulses. Angular impulse is the area under the hip moment curve. Therefore, angular impulse encompasses both the magnitude and the duration of the moment. Flexion angular impulse was calculated separate from extension angular impulse. The changes in sagittal knee and ankle peak moments and angular impulse between postures were also analyzed.
For each variable, the mean value of the data from the right lower extremity from the three walking trials for each posture was calculated and used in statistical analyses.
2.5 Data processing
To obtain the variables of interest, three-dimensional marker trajectories were recorded using a real-time tracking system (EvaRT v4.0, Motion Analysis Corp.). The kinematic data were smoothed using a 6Hz Butterworth filter. Visual3D (C-Motion, Inc, Rockville, MD, USA) was used to locate the joint centers and record the pelvis, hip, knee and ankle angles based on a three-dimensional model. The standing trial was used to create the model and three dimensional joint angles were determined using a Cardan x-y-z (flexion/extension, abduction/adduction, longitudinal rotation) rotation sequence. The hip, knee and ankle angles were defined relative to the proximal segment. Orientation of the pelvis segment was defined relative to the global (laboratory) coordinate system with pelvic tilt being about the global Y axis which was horizontal and perpendicular to the direction of gait. Inertial properties were estimated based on anthropometric measurements of the subjects (Zatsiorsky, 2002). Hip, knee and ankle moments were calculated using inverse dynamics and the kinematic and force data.
2.6 Data analysis
To examine the effects of posture on lower extremity angles and moments, a repeated measures analysis of variance (ANOVA) was used for each variable. As the ANOVA assumes homogeneity of variance, the Mauchly test of sphericity was used, and the Greenhouse-Geisser epsilon correction was applied to the degrees of freedom when the Mauchly test was significant (p < 0.05). The within subjects factor, posture, had three levels (Natural, Swayback, and Forward flexed). To evaluate if subjects walked in the altered posture, the pelvic tilt angle averaged over the gait cycle was analyzed. The average pelvic angle is thought to better represent the pelvic tilt over the gait cycle than using discrete points. The 18 dependent variables were maximum angles, peak moments, and angular impulse for the hip, knee and ankle in the sagittal plane. All statistical analyses were performed in PASW Statistics 18 (SPSS Inc, Chicago, IL) with an alpha level of 0.05. All significant main effects of the ANOVA were further investigated using bonferonni adjusted contrasts. Effect size (Cohen d) was calculated as the absolute difference in means divided by the pooled variance (Cohen, 1988). Pooled variance was calculated as the root mean square of the two standard deviations (Rosenthal and Rosnow, 1991). Small, moderate, and large effects are indicated by values of 0.2, 0.5, and 0.8 respectively (Cohen, 1988).
3. Results
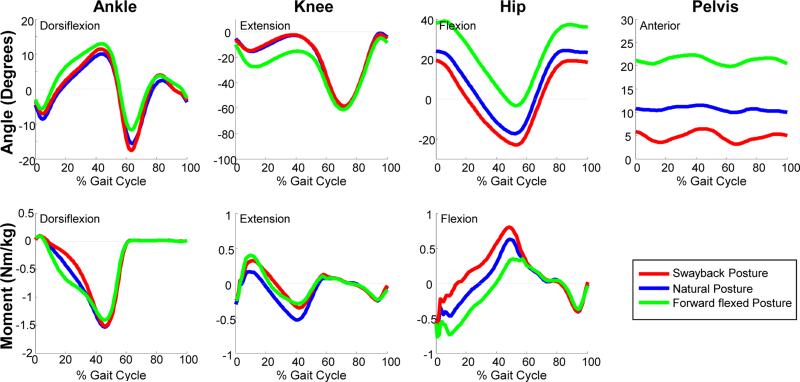
The instructions to walk in an altered posture resulted in significant changes in both the kinematics and the kinetics of gait (Figure 2). Repeated measures ANOVA revealed significant differences (p < 0.05) in all dependent variables except peak ankle dorsiflexor moment and maximum knee flexion angle. Maximum knee flexion, maximum hip extension, peak ankle dorsiflexor moment and hip extensor angular impulse did not have homogenous variance, and therefore were evaluated using the Greenhouse-Geisser epsilon correction. The average (± standard deviation) walking speeds for swayback, natural and forward flexed were 1.18 ± 0.16, 1.22 ± 0.16 and 1.23 ± 0.19 m/s, respectively.
Figure 2.
Ankle, knee and hip joint and pelvis kinematic and kinetic data. Data are the mean of all subjects walking in each of the three postures. Data are normalized from right heel strike to right heel strike. Ankle dorsiflexion, knee extension, hip flexion and anterior pelvic tilt are positive.
3.1 Swayback
Subjects walked in the swayback posture as indicated by the large decrease in mean anterior pelvic tilt compared to the natural and forward flexed trials. Maintaining the swayback posture during gait also resulted in a large increase in the maximum hip extension angle and a moderate decrease in the maximum hip flexion angle compared to the natural posture (Table 2). Compared to the forward flexed posture, the swayback posture resulted in a large increase in the maximum hip extension angle and decrease in the maximum hip flexion angle. There was also a large increase in the maximum knee extension angle in the swayback posture compared to the forward flexed posture. The maximum ankle dorsiflexion angle increased slightly in the swayback posture compared to natural. The maximum ankle plantar flexion angle was moderately increased in the swayback posture compared to the forward flexed posture.
Table 2.
Mean and standard deviations of the kinematic and kinetic data from all subjects (N=15). Statistical analysis includes results of paired t-tests between the Natural, Swayback and Forward flexed postures.
| Condition | Statistical analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Swayback | Natural | Forward flexed | Natural vs. Swayback | Natural vs. Forward flexed | Swayback vs. Forward flexed | ||||
| Kinematics (degrees) | p | ES (d) | p | ES (d) | p | ES (d) | |||
| Maximum ankle DF | 11.9±5.8 | 10.3±5.5 | 13.6±7.6 | 0.038 | 0.28 | 0.006 | 0.50 | 0.267 | 0.25 |
| Maximum ankle PF | −19.7±8.7 | −17.7±8.3 | −14.0±8.7 | 0.105 | 0.23 | 0.001 | 0.44 | <0.001 | 0.66 |
| Maximum knee extension | 0.9±4.7 | 0.6±4.1 | −4.3±6.4 | 1.000 | 0.07 | <0.001 | 0.91 | <0.001 | 0.92 |
| Maximum knee flexion | −59.4±7.3 | −60.5±5.8 | −61.8±5.9 | NS | |||||
| Maximum hip flexion | 20.7±8.6 | 25.4±7.2 | 40.2±8.2 | 0.002 | 0.60 | <0.001 | 1.92 | <0.001 | 2.33 |
| Maximum hip extension | −23.4±6.6 | −17.8±7.2 | -3.8±6.4 | <0.001 | 0.81 | <0.001 | 2.06 | <0.001 | 3.01 |
| Mean pelvic tilt | 4.8±3.4 | 10.7±3.6 | 21.1±4.3 | <0.001 | 3.55 | <0.001 | 1.68 | <0.001 | 1.53 |
| Kinetics (Nm/kg or Nms/kg) | |||||||||
| Peak ankle DF moment | 0.10±0.03 | 0.10±0.04 | 0.11±0.05 | NS | |||||
| Peak ankle PF moment | −1.54±0.12 | −1.55±0.11 | −1.44±0.09 | 1.000 | 0.13 | <0.001 | 1.21 | 0.006 | 0.96 |
| Ankle DF angular impulse | 0.009±0.004 | 0.008±0.003 | 0.008±0.004 | 0.051 | 0.40 | 0.595 | 0.16 | 0.262 | 0.20 |
| Ankle PF angular impulse | −0.40±0.07 | −0.44±0.07 | −0.46±0.08 | <0.001 | 0.65 | 0.132 | 0.26 | <0.001 | 0.83 |
| Peak knee extension moment | 0.37±0.18 | 0.22±0.12 | 0.44±0.19 | 0.001 | 0.94 | 0.001 | 1.31 | 0.386 | 0.37 |
| Peak knee flexion moment | −0.44±0.18 | −0.56±0.13 | −0.38±0.12 | 0.004 | 0.78 | <0.001 | 1.44 | 0.472 | 0.38 |
| Knee extension angular impulse | 0.083±0.053 | 0.037±0.026 | 0.077±0.042 | 0.001 | 1.10 | 0.004 | 1.15 | 1.000 | 0.13 |
| Knee flexion angular impulse | −0.083±0.054 | −0.138±0.048 | −0.079±0.045 | 0.001 | 1.08 | <0.001 | 1.27 | 1.000 | 0.07 |
| Peak hip flexion moment | 0.82±0.14 | 0.65±0.15 | 0.44±0.14 | <0.001 | 1.16 | <0.001 | 1.48 | <0.001 | 2.73 |
| Peak hip extension moment | −0.68±0.23 | −0.76±0.24 | −0.94±0.25 | 0.513 | 0.32 | 0.018 | 0.76 | 0.002 | 1.09 |
| Hip flexion angular impulse | 0.24±0.06 | 0.14±0.02 | 0.08±0.03 | <0.001 | 2.43 | <0.001 | 2.42 | <0.001 | 3.75 |
| Hip extension angular impulse | −0.04±0.02 | −0.10±0.04 | −0.20±0.09 | <0.001 | 1.80 | 0.001 | 1.41 | <0.001 | 2.36 |
Note: NS indicated that the repeated measures ANOVA for effect of posture was not significant (p ≥ 0.05); therefore, pair-wise comparisons were not conducted. Bold text indicated significant differences (p < 0.05)
Walking in the swayback posture also resulted in a large increase in the hip flexor peak moment and angular impulse and decrease in the hip extensor angular impulse when compared to walking in the natural posture or forward flexed posture. The hip extensor peak moment had a large decrease in the swayback posture compared to the forward flexed posture. At the knee, there was a large increase in the knee extensor peak moment and angular impulse and a moderate and large decrease in the knee flexor peak moment and angular impulse, respectively, compared to natural posture. At the ankle, there was a large increase in the ankle plantar flexion peak moment and decrease in the plantar flexion angular impulse compared to the forward flexed posture. There was also a moderate decrease in the plantar flexor angular impulse compared to the natural posture.
3.2 Forward flexed
Subjects walked in the forward flexed posture as indicated by the large increase in average anterior pelvic tilt compared to the natural trials. Maintaining the flexed posture during gait also resulted in a large reduction of the maximum hip extension angle and increase of the maximum hip flexion angle when compared to the natural posture. The maximum knee extension angle had a large decrease and the maximum ankle plantar flexion angle had a small decrease in the forward flexed posture, while the maximum ankle dorsiflexion angle had a small increase compared to natural.
Walking in the forward flexed posture resulted in a large decrease in the hip flexor peak moment and angular impulse, and a large increase in the hip extensor peak moment and angular impulse when compared to the natural posture. There was also a large increase in the knee flexor peak moment and angular impulse and decrease in the knee extensor peak moment and angular impulse. At the ankle, there was a large decrease in the ankle plantar flexor peak moment despite a small increase in the angular impulse.
4. Discussion
The main finding of this study is that posture has a notable effect on movement patterns and moments during gait. Walking in the swayback posture resulted in an average increase of 5.6° in the maximum hip extension angle over the natural posture, and an increase of nearly 20° over the forward flexed posture. These kinematic differences, along with the differences in pelvic tilt, indicate that subjects were able to modify their gait. The increase in hip extension could significantly increase the force on the anterior hip. Through a series of simulation studies using musculoskeletal modeling to estimate hip joint forces, we have previously demonstrated that the hip joint force in the anterior direction increases with increased hip extension angle during exercises (Lewis et al., 2007; Lewis et al., 2009), despite generating the same joint moment. Specific to gait, we have demonstrated that a 2° increase in hip extension increased the maximum anterior hip joint force by 156 N (24%) (Lewis et al., 2010); however, this was in a small number of males and trunk position was not monitored. It has been suggested that the increased force could contribute to acetabular labral tears and hip pain (Mason, 2001; McCarthy et al., 2001). Furthermore, in a cadaveric study, Safran et al. (2011) demonstrated that hip extension increases the strain in the anterolateral labrum, a common location for labral tears (Lewis and Sahrmann, 2006).
Walking in the swayback posture also resulted in a higher peak hip flexor moment and higher hip flexion angular impulse when compared to walking in the natural or the forward flexed posture. The higher hip flexor moment and angular impulse could require the hip flexor muscles to produce a higher magnitude force and for a longer period of time to generate the required moment. It is also possible that the moment arm of the iliopsoas for hip flexion significantly increases with increased hip extension; however, modeling and imaging studies suggest little to no increase in hip flexor moment arm with hip extension (Delp et al., 1990; Arnold et al., 2000; Blemker and Delp, 2005). The hip flexor muscle force controls the hip extension from midstance to terminal stance and initiates hip flexion. As some of the force requirement is occurring near maximum hip extension, it could be produced by both muscle and passive structures (Winter, 1990) including the acetabular labrum. The higher magnitude and longer duration of force required of the anterior hip structures could over time result in repetitive microtrauma and injury of these structures. Thus, walking in a swayback posture may predispose one to injury of the anterior hip structures and contribute to anterior hip pain.
Conversely, the results of this study indicate that walking in a forward flexed posture would reduce the moment required of the anterior hip musculature, and therefore may reduce the force required of anterior structures. Walking in the forward flexed posture resulted in less hip extension, which implies that it results in a lower maximum anterior hip force (Lewis et al., 2010). While walking in the flexed posture, the average maximum hip extension angle was only 4°. This finding provides a plausible mechanistic explanation for the effect of correcting the swayback posture in patients with anterior hip pain.
Walking in the flexed posture also reduces the moment required of the hip flexor muscles. Both the peak hip flexor moment and the angular impulse were less in the flexed posture compared to the natural posture. Thus, walking in a forward flexed posture with the hips and knees maintained in slight flexion may reduce forces required of the anterior hip structures and musculature. This reduction may be particularly important as hip flexor strength is decreased in individuals with labral pathology (Mendis et al., 2014) and in individuals with FAI both before (Casartelli et al., 2011) and after hip arthroscopy (Casartelli et al., 2014). This finding provides a plausible mechanistic explanation for the immediate reduction in pain that we clinically observed following correction of posture. These findings may also inform therapists who are instructing patients in appropriate gait patterns, such as after hip arthroplasty.
While this study's primary focus is the anterior hip structures, there are important concomitant changes at other lower extremity joints. These changes appear to be necessary to maintain gait at the same speed. In the swayback posture, the increase in ankle dorsiflexion and ankle plantar flexion during the terminal stance and initial swing, respectively, is interesting given that there were not significant changes at the knee. In the forward flexed posture, the increase in ankle dorsiflexion and accompanying increase in knee flexion during stance phase was expected because the subjects were instructed to maintain slight knee flexion during gait.
The pattern of ankle plantar flexor moment in the forward flexed posture is very similar to the plantar flexor moment when subjects were instructed to pushoff more when they walked than their normal pushoff (Lewis and Ferris, 2008). Similar to the forward flexed posture, the simple instruction to “push more with your foot” resulted in a decrease in the peak hip flexor moment (Lewis and Ferris, 2008). Therefore, changing posture and simultaneously increasing pushoff may further decrease hip moments and forces.
The results of this study are similar to the results reported by Leteneur and colleagues (Leteneur et al., 2009). In their study, which was limited to males, subjects were grouped based on natural trunk inclination. Leteneur found that, in subjects who habitually maintained a more forward trunk posture, the hip extensor moment had a longer duration and the hip flexor moment had a lower magnitude (Leteneur et al., 2009). In our study, the use of simulated exaggerated postures most likely contributed to the greater differences than those reported by Leteneur.
There are limitations due to the design of this study. Although hip moment and angular impulse data would suggest that walking in a swayback posture could lead to increased forces on anterior tissues and subsequent injury, the study design does not allow us to draw conclusions regarding causation. A longitudinal study of the development of anterior hip pain would clarify the issue of causation. The gait modification evaluated was specifically designed to reduce forces on anterior hip structures. As such, it may increase forces on other areas of the hip, such as lateral structures. This aspect of the gait modification has yet to be tested. The use of simulated forced postures (swayback and forward flexed) in healthy subjects may have resulted in different lower extremity kinematic and kinetics from individuals who habitually maintain these postures because the subject was unfamiliar with walking in the posture. We selected healthy, asymptomatic subjects to allow us to investigate within subject changes without pain affecting the movement pattern (Hodges and Tucker, 2011). Practice trials allowed subjects to become more familiar with the gait posture. Subjects did walk slightly slower in the swayback trials. While speed does affect joint moments, the large differences noted with posture are unlikely the result of the small speed differences. Furthermore, as posture and gait modification are commonly used physical therapy interventions, assessing the resulting effects on gait patterns and joint kinematics and kinetics, particularly the hip, is important. We used visual appraisal to ensure that the subjects walked in the appropriate trunk position during the trials. A multi-segmented trunk model would provide more information on the kinematics of the trunk.
Acknowledgments
We thank Shannon Hoffman for assistance with data collection and processing. Research reported in this publication was supported by Boston University's Peter Paul Career Development Professorship, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number K23 AR063235. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Mechanistic terms
- Kinematics
Kinematics is the study of joint motion, and is expressed in terms of joint angles and excursions.
- Kinetics
Kinetics is the study of the forces which produce motion, and is expressed in terms of joint moments, angular impulse and power.
- Joint moment
A joint moment is the rotational potential of a force; that is, it is the ability of a force to rotate a segment. The force can be from active tissue (muscle) as well as passive tissue (ligaments, capsule, and at the hip, acetabular labrum).
- Angular impulse
Angular impulse is the area under the joint moment curve. It takes into account both the magnitude and the duration of a joint moment.
- Joint (contact) force
Joint force is the force between the two segments (bones, in this case). Both active and passive tissues contribute to joint force.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am.J.Sport.Med. 2001;29(4):521–533. doi: 10.1177/03635465010290042501. [DOI] [PubMed] [Google Scholar]
- Arnold AS, Salinas S, Asakawa DJ, Delp SL. Accuracy of muscle moment arms estimated from MRI-based musculoskeletal models of the lower extremity. Comp.Aided.Surg. 2000;5(2):108–119. doi: 10.1002/1097-0150(2000)5:2<108::AID-IGS5>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J.Bone.Joint.Surg.Br. 2005;87(7):1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- Blemker SS, Delp SL. Three-dimensional representation of complex muscle architectures and geometries. Ann.Biomed.Eng. 2005;33(5):661–673. doi: 10.1007/s10439-005-1433-7. [DOI] [PubMed] [Google Scholar]
- Byrd JW. Femoroacetabular impingement in athletes: current concepts. Am.J.Sport.Med. 2014;42(3):737–751. doi: 10.1177/0363546513499136. [DOI] [PubMed] [Google Scholar]
- Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy. 1996;12(5):603–612. doi: 10.1016/s0749-8063(96)90201-7. [DOI] [PubMed] [Google Scholar]
- Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, Impellizzeri FM, Leunig M. Hip muscle strength recovery after hip arthroscopy in a series of patients with symptomatic femoroacetabular impingement. Hip.Int. 2014 doi: 10.5301/hipint.5000131. In press. [DOI] [PubMed] [Google Scholar]
- Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, Staehli S, Bizzini M, Impellizzeri FM, Leunig M. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthr.Cartil. 2011;19(7):816–821. doi: 10.1016/j.joca.2011.04.001. [DOI] [PubMed] [Google Scholar]
- Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin.Orthop.Relat.Res. 2009;476(3):638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates, Inc.; Hillsdale, NJ: 1988. [Google Scholar]
- Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE.Trans.Biomed.Eng. 1990;8(37):757–767. doi: 10.1109/10.102791. [DOI] [PubMed] [Google Scholar]
- Dorrell JH, Catterall A. The torn acetabular labrum. J.Bone.Joint.Surg.Br. 1986;3:400–403. doi: 10.1302/0301-620X.68B3.3733805. [DOI] [PubMed] [Google Scholar]
- Fitzgerald RH., Jr. Acetabular labrum tears. diagnosis and treatment. Clin.Orthrop.Relat.Res. 1995;311:60–68. [PubMed] [Google Scholar]
- Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin.Orthrop.Relat.Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain. 2011;152(3 Suppl):S90–8. doi: 10.1016/j.pain.2010.10.020. [DOI] [PubMed] [Google Scholar]
- Hunt D, Prather H, Harris Hayes M, Clohisy JC. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM.R. 2012;7:479–487. doi: 10.1016/j.pmrj.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito K, Minka MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J.Bone.Joint.Surg.Br. 2001;2:171–176. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- Johnston CA, Wiley JP, Lindsay DM, Wiseman DA. Iliopsoas bursitis and tendinitis. A review. Sports.Med. 1998;4:271–283. doi: 10.2165/00007256-199825040-00005. 0112-1642. [DOI] [PubMed] [Google Scholar]
- Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J.Orthop.Res. 1990;3:383–392. doi: 10.1002/jor.1100080310. 0736-0266. [DOI] [PubMed] [Google Scholar]
- Kendall FP, McCreary EK, Provance PG. Muscles Testing and Function. Williams & Wilkins; Baltimore, MD: 1993. [Google Scholar]
- Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J.Bone.Joint.Surg.Br. 1991;3:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- Leteneur S, Gillet C, Sadeghi H, Allard P, Barbier F. Effect of trunk inclination on lower limb joint and lumbar moments in able men during the stance phase of gait. Clin.Biomech. (Bristol, Avon) 2009;2:190–195. doi: 10.1016/j.clinbiomech.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Lewis CL, Ferris DP. Walking with increased ankle pushoff decreases hip muscle moments. J.Biomech. 2008;10:2082–2089. doi: 10.1016/j.jbiomech.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CL, Sahrmann SA. Acetabular labral tears. Phys.Ther. 2006;1:110–121. doi: 10.1093/ptj/86.1.110. [DOI] [PubMed] [Google Scholar]
- Lewis CL, Sahrmann SA, Moran DW. Effect of hip angle on anterior hip joint force during gait. Gait.Posture. 2010;4:603–607. doi: 10.1016/j.gaitpost.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CL, Sahrmann SA, Moran DW. Effect of position and alteration in synergist muscle force contribution on hip forces when performing hip strengthening exercises. Clin.Biomech. (Bristol, Avon) 2009;1:35–42. doi: 10.1016/j.clinbiomech.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CL, Sahrmann SA, Moran DW. Anterior hip joint force increases with hip extension, decreased gluteal force, or decreased iliopsoas force. J.Biomech. 2007;16:3725–3731. doi: 10.1016/j.jbiomech.2007.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason JB. Acetabular labral tears in the athlete. Clin.Sports.Med. 2001;4:779–790. doi: 10.1016/s0278-5919(05)70284-2. [DOI] [PubMed] [Google Scholar]
- McCarthy JC, Lee JA. Acetabular dysplasia: a paradigm of arthroscopic examination of chondral injuries. Clin.Orthop.Relat.Res. 2002;405:122–128. doi: 10.1097/00003086-200212000-00014. [DOI] [PubMed] [Google Scholar]
- McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin.Orthop.Relat.Res. 2001;393:25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- Mendis MD, Wilson SJ, Hayes DA, Watts MC, Hides JA. Hip flexor muscle size, strength and recruitment pattern in patients with acetabular labral tears compared to healthy controls. Man.Ther. 2014 doi: 10.1016/j.math.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann.Surg. 2008;4:656–665. doi: 10.1097/SLA.0b013e318187a770. [DOI] [PubMed] [Google Scholar]
- Narvani AA, Tsiridis E, Kendall S, Chaudhuri R, Thomas P. A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee.Surg.Sports.Traumatol.Arthrosc. 2003;6:403–408. doi: 10.1007/s00167-003-0390-7. [DOI] [PubMed] [Google Scholar]
- Nepple JJ, Prather H, Trousdale RT, Clohisy JC, Beaule PE, Glyn-Jones S, Kim YJ. Clinical diagnosis of femoroacetabular impingement. J.Am.Acad.Orthrop.Surg. 2013:S16–9. doi: 10.5435/JAAOS-21-07-S16. [DOI] [PubMed] [Google Scholar]
- Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee.Surg.Sports.Traumatol.Arthrosc. 2007;8:1041–1047. doi: 10.1007/s00167-007-0348-2. [DOI] [PubMed] [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of behavioral research: Methods and data analysis. 2nd ed. McGraw Hill; New York: 1991. [Google Scholar]
- Safran MR, Giordano G, Lindsey DP, Gold GE, Rosenberg J, Zaffagnini S, Giori NJ. Strains across the acetabular labrum during hip motion: a cadaveric model. Am.J.Sport.Med. 2011:92S–102S. doi: 10.1177/0363546511414017. [DOI] [PubMed] [Google Scholar]
- Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. Mosby, Inc; St. Louis, MO: 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar WN, Nevitt M, Parvizi J, Felson DT, Agricola R, Leunig M. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J.Am.Acad.Orthrop.Surg. 2013:S7–S15. doi: 10.5435/JAAOS-21-07-S7. [DOI] [PubMed] [Google Scholar]
- Somers MF. Spinal Cord Injury: Functional Rehabilitation. Prentice Hall; NJ: 2001. [Google Scholar]
- Sueki DG, Cleland JA, Wainner RS. A regional interdependence model of musculoskeletal dysfunction: research, mechanisms, and clinical implications. J.Man.Manip.Ther. 2013;2:90–102. doi: 10.1179/2042618612Y.0000000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Soballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta.Orthop. 2009;3:314–318. doi: 10.3109/17453670902988402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter DA. Biomechanics and Motor Control of Human Movement. John Wiley & Sons, Inc.; New York, NY: 1990. [Google Scholar]
- Zajac FE. Muscle coordination of movement: a perspective. J.Biomech. 1993;26(Suppl 1):109–124. doi: 10.1016/0021-9290(93)90083-q. [DOI] [PubMed] [Google Scholar]
- Zatsiorsky VM. Kinetics of human motion. Human Kinetics; Champaign, IL: 2002. [Google Scholar]