Abstract
The treatment of burn injuries requires high-cost services for healthcare and society. Automatic fire sprinklers are a preventive measure that can decrease fire injuries, deaths, property damage and environmental toxins. This study’s aim was to conduct a cost-analysis of patients with burn or inhalation injuries due to residential fires, and to compare this to the cost of implementing residential automatic fire sprinklers.
We conducted a cohort analysis of adult burn patients admitted to our provincial burn center (1995–2012). Patient demographics and injury characteristics were collected from medical records, and clinical and coroner databases. Resource costs included average cost per day at our intensive care and rehabilitation program, transportation, and property loss.
During the study period there were 1,557 residential fire-related deaths province-wide and 1,139 patients were admitted to our provincial burn center due to a flame injury occurring at home. At our burn center, the average cost was CAN$84,678 per patient with a total cost of CAN$96,448,194. All resources totaled CAN$3,605,775,200. This study shows the considerable healthcare costs of burn patients from homes without fire sprinklers.
Keywords: Burn injuries, automatic fire sprinklers, inhalation injuries, economic health care costs, residential fire prevention
Introduction
Burns remain the third leading cause of unintentional injury in the home with the majority of burn fatalities due to inhalation injuries.1 Approximately 45,000 burn injuries occur in Canada each year, with about 2,000 patients requiring hospitalization.2 The treatment of burn injuries comes at a high-cost for both healthcare and society, accounting for about $118 million in direct costs and $172 million in indirect costs, for a total of $290 million annually.2 The use of combustible furnishings and new home materials has accelerated the time from a fully developed fire to a flashover to about 2 – 5 minutes.3 Additionally, new homes are frequently built on small lots in close proximity, increasing the chance of spread from one home to another. Additional hazards for home fires stem from the cause of fire: in residential fires resulting in injury, the majority of fires were caused by cooking equipment followed by smoking; whereas most residential fires resulting in death were caused by smoking.4
The traditional preventative measure in residential homes is a smoke alarm, with the purpose of warning occupants of a fire. Overall, working smoke alarms reduce fatalities by about half.5 However, smoke alarms are limited by factors such as battery life, an inadequate power source, incorrect placement in the home, and can fail to alert sleeping residents.3,6 Despite this popular early smoke detection system, individuals may still not escape due to physical or mental impairments, or other frailties associated with children and the elderly.
Fire prevention using automatic fire sprinklers and smoke alarms can save lives, reduce injuries, lessen property damage, and avoid environmental toxins due to smoke. Research suggests that residential properties with automatic fire sprinklers, used in conjunction with smoke alarms, reduced death rates by 93% and reported zero deaths in single-family homes in British Columbia, Canada.6 Furthermore, fires that occur in residential buildings equipped with sprinkler protection tend to be smaller, more likely to be contained, and less likely to require intervention from a fire department.6 Modern automatic fire sprinklers are effective in saving lives and are aesthetically pleasing for home decor. A common misconception about automatic fire sprinklers is that they misfire and cause water damage. Typical automatic fire sprinklers are triggered by heat and only the sprinkler closest to the fire will open. Once activated, they usually discharge less than 20 gallons per minute, whereas a fire fighter’s hose discharges more than 200 gallons per minute.3 The reduction in water usage also means decreased water pollution. The use of automatic fire sprinklers reduce green house gas emissions by 98% and the carbon emissions accompanying reconstruction of a home and its furnishing.7
Installation of an automatic fire sprinkler system is rarely mandated despite past reports that detail the numerous lives saved and potential reduction in damage to property.8–10 One study reviewed the 15-year history of a single-family residential dwelling fire sprinkler ordinance. During the 15-year period, there were 13,494 fires, 245 of which occurred in sprinklered-protected homes and had zero deaths and six injuries, in contrast to the remaining 13,249 fires that resulted in 101 deaths and over 300 injuries in homes without such protections in Prince George’s County, US.9 Furthermore, automatic fire sprinklers reduced property loss by 50–90% in comparison to homes without fire sprinklers.9 Another 10-year report of a fire sprinkler ordinance for commercial structures, multi-family and single-family residential dwellings, also described no deaths in sprinklered homes with an average loss of US$2,166 compared to 13 deaths in unsprinklered homes with an average loss of US$45,019 in Scottsdale, Arizona, US.10–11 We hypothesize that the implementation of fire sprinklers would be beneficial for residential and business facilities. However, in order to implement such change one has to consider the economic impact of both the change and of the patient. The aim of this study was to conduct a cost-analysis of patients with burn or inhalation injuries in residential fires, and compare their estimated cost to the cost of implementing automatic fire sprinkler systems in residential homes.
Methods
We conducted a cohort analysis of adults (age ≥16 years) injured in a fire in Ontario between April 1, 1995 and March 31, 2012 admitted to our provincial burn center including those who died after injury. Subjects met inclusion criteria if they had a flame burn injury that occurred in a residential dwelling. The Research Ethics Board at our institution approved the study protocol.
Cases that investigated fire-related deaths were obtained from the Ontario Office of the Chief Coroner. All patient data were collected from medical records and clinical databases. The following patient demographics and injury characteristics were collected: percent total body surface area burned, age in years, presence of inhalation injury, length of stay in hospital in days, and mortality.
Patients were grouped based on their admission status: burn severity (percent total body surface area burned; <20%, 20–40%, >40%), medical futility (died <24 h), and reconstructive surgery. Costs for transport were calculated based on land ambulance services fees, as air ambulance costs were not available. Costing data was provided by the Decision Support department of the hospital and included clinical nutrition, burn clinic costs, nursing, pharmacist, physician support, physiotherapy, occupational therapy, operating room, respiratory therapy, skin bank, and social work costs. Burn center and rehabilitation program costs were calculated by multiplying the average cost per day by length of stay in days. Injuries and property loss data were obtained from the Office of the Fire Marshal and Emergency Management (OFMEM).
The approximate conversion rate based on currency exchange in March 2014 from Canadian to US dollars: CAN$1.00=US$0.905.12
Results
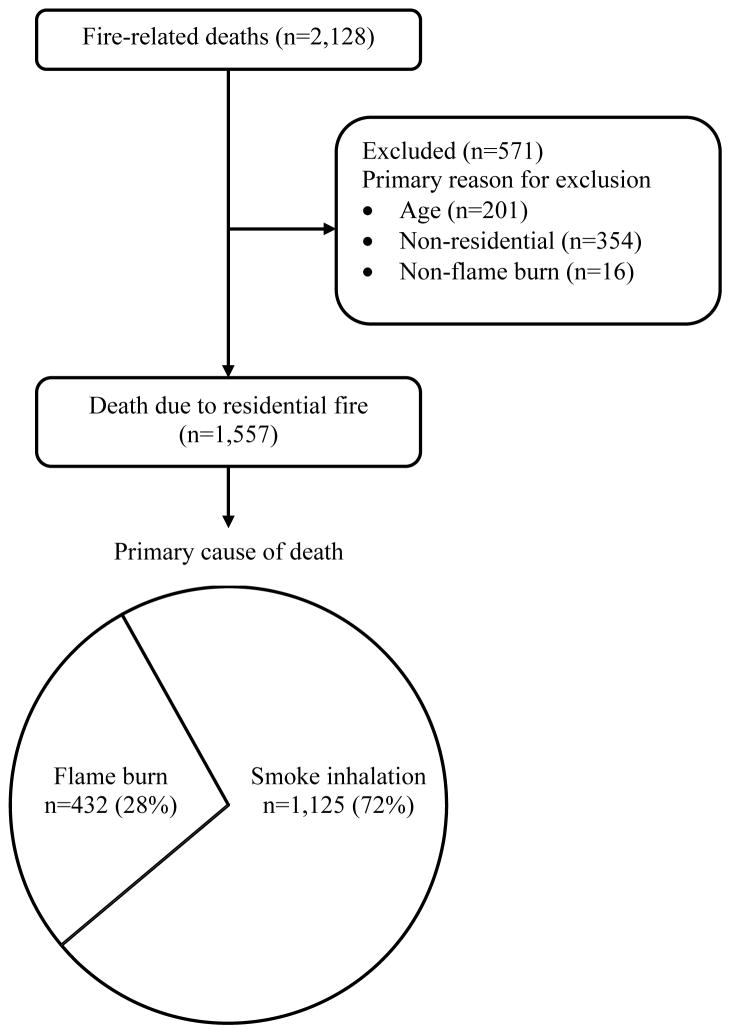
The Office of the Chief Coroner investigated a total of 2,128 fire-related deaths in our province over the 17-year period. There were 1,557 (73%) deaths that met inclusion criteria; the average age was 55 years (SD=20). The primary cause of death was smoke inhalation for 1,125 (72%) people (Figure 1).
Figure 1.
Fire-related deaths province-wide
There were 3,401 admissions to our burn centre during the 17-year study period, of which 1,139 (34%) met inclusion criteria (Figure 2). Patient characteristics and outcomes are summarized in Table 1. The average cost for a burn patient’s stay in hospital was CAN$84,678 per patient. As expected, average cost varied with burn severity and generally increased for those with larger burns (Table 2). The only exception was among those who died within 24 hours, as they tended to have lower average cost per patient (Table 2). Burn center costs totaled CAN$96,448,194 (Table 2).
Figure 2.
Burn center patient flow diagram
Table 1.
Patient characteristics and outcomes
| Variable | n=1,139 |
|---|---|
| Percent total body surface area burned | 22 ± 22 |
| Age (years) | 47 ± 19 |
| Hospital length of stay (days) | 19 ± 27 |
| Inhalation injury (%) | 284 (25) |
| Mortality (%) | 170 (15) |
Data presented as mean ± SD or number (%)
Table 2.
Burn center costs
| n | Average cost per day (CAN$) | Average cost per patient (CAN$) | Total cost (CAN$)* | |
|---|---|---|---|---|
| Burn severity | ||||
| <20% | 617 | 3,411 | 52,873 | 32,622,804 |
| 20–40% | 164 | 4,732 | 176,152 | 28,888,860 |
| >40% | 82 | 6,614 | 361,754 | 29,663,790 |
| Mortality<24 h | 81 | 7,620 | 7,620 | 617,220 |
| Reconstruction | 195 | 4,392 | 23,874 | 4,655,520 |
| Total | 1,139 | 84,678 | 96,448,194 | |
Total costs were calculated by multiplying the average cost per day by length of stay in days
Of the 1,139 admissions, 849 (75%) required ambulance services (CAN$240 for each land ambulance trip) for a total cost of CAN$203,760 (Table 3). The rehabilitation program subsequently admitted 164 patients during the study period, with an average cost of CAN$22,779 per patient and a total cost of CAN$3,735,756 (Table 3). There were 109,678 fires and 8,224 injuries that were reported to the OFMEM during the study period with property loss of $3,505,387,490 (Table 3). The total calculated costs of calculated resources and loss of property was 3,605,775,200 (Table 3).
Table 3.
Calculated cost of burns
| Resource | n | Total (CAN$) |
|---|---|---|
| Land ambulance transport | 849 | 203,760 |
| Burn center | 1,139 | 96,448,194 |
| Rehabilitation | 164 | 3,735,756 |
| Property loss | 109,678 | 3,505,387,490 |
|
| ||
| Total | 3,605,775,200 | |
Discussion
This study suggests that fires in residential dwellings lead to preventable burn injuries and burn deaths, substantial healthcare costs, and avoidable property loss. Costs incurred directly and indirectly from burn injury result in a considerable economic burden. Resource utilization in the highly specialized field of burn care is substantial in the acute phase and may require follow-up for years after injury, involving reconstructive surgery, rehabilitation, and psychological support.13–14
The 2014 National Burn Repository Report of the American Burn Association showed that the average hospital costs per burn patient was US$93,147 ± 963.15 One study investigating the cost of burns in adult patients found an average cost of US$73,532 while another was £5,337.16–17 However, the average TBSA for the former study was 19.55% and the latter was 6.2%. This demonstrates our average burn care costs (CAN$84,678 per patient) relative to TBSA are in line with other centers.
A review of fatal commercial and residential fire data over a three-year period in Ontario reported that out of 52,990 fires, 43% did not have a working smoke alarm.3 Smoke alarms are essential, but automatic sprinklers provide an intervention to extinguish a fire that can prevent deaths in house fires. Comparatively, smoke alarms are a more active strategy and require a greater conscious effort from the individual to be effective i.e. remember to replace batteries or install the smoke alarm in the correct location. Passive and active strategies are most effective when used jointly as part of a comprehensive prevention strategy by injury prevention practitioners.18
In addition to helping the victims, automatic fire sprinklers also protect and reduce fire fighter injury and respective costs.12 A study in British Columbia, Canada showed the injury rate for fire fighters was doubled in buildings that did not have automated fire sprinklers.6 Sprinklers might also help to mitigate higher call volumes that lead to increased response times, more emergency personnel, and potential fire department resources.19
A number of jurisdictions in the United States have residential sprinkler ordinances for effective life-safety and property preservation. In Canada, only a few municipalities in British Columbia have implemented mandatory fire sprinklers in new family dwellings.19 The enormous cost of residential fires and associated burn injuries on the healthcare system justifies implementation of even expensive burn prevention strategies. While the average cost of the installation of automatic fire sprinklers is only CAN$1.49 (US$1.35)20 per sprinklered square foot in a new home, they are estimated to be installed in a mere 1% of homes affected by fire.21 A targeting strategy for installation of automatic fire sprinklers is imperative. Focusing on new homes first is effective because installation of automatic fire sprinklers is less costly than retrofitting a home. If automatic fire sprinklers were mandatory, rather than optional, the result would be a lower markup due to the cost being included in the price of the home. In the 2011 Ontario census households numbered just over 4 million,22 if all of the homes built from 1995–2012 had been fitted with automatic sprinklers, approximately 1,200,000 (30%)23 of the homes in Ontario would already have been sprinklered. In that same time period, injuries occurred in 8% of fires or at a rate of 1 in every 13 fire. In the province of Ontario, it has been projected that 55,400 new homes would be built in 2014 and 56,600 new homes in 2015.24 The second phase would be retrofitting older homes to protect groups most at risk from being injured in a house fire, such as children, elderly, and people with disabilities. The cost of retrofitting homes can range from US$3.00 to 8.00 per sprinklered square foot,25 but there are economic savings that can recoup the cost of retrofitting for homeowners, such as government incentive programs (e.g., reduced property taxes) and insurance premiums reductions.26
There were limitations with the study. The measure of expenses was limited due to the scope of charge data available. Items of interest not presently included are air ambulance, telemedicine, admissions to other hospitals, and long-term post-discharge costs (such as physical therapy, psychological therapy, prescription drugs, and home care). Additionally, there are greater consequences for the patient and society such as pain and suffering, loss of productivity, and potential life years lost that are difficult to quantify in terms of cost. The addition of these factors would only increase the expense of burn injuries and further strengthen the need for burn prevention strategies.
This study shows the high cost of burn injuries occurring in homes and the resulting property loss that may be preventable with the implementation of automatic fire sprinklers.
Acknowledgments
Source of Funding
This project was supported by:
Canadian Automatic Sprinkler Association
Canadian Association of Fire Chiefs
Canadian Institutes of Health Research # 123336.
CFI Leader’s Opportunity Fund: Project # 25407
Fire Marshal’s Public Fire Safety Council
NIH RO1 GM087285-01
Ontario Municipal Fire Prevention Officers Association
Physicians’ Services Incorporated Foundation - Health Research Grant Program
The Co-operators Insurance Group
Footnotes
Abstract presented at the 46th Annual Meeting of the American Burn Association, Boston, MA, USA
Conflicts of Interest
None of the authors declared any conflict of interest.
The funding organizations had no role in the design or conduct of the study; collection, management, analysis or interpretation of the data; or the preparation, review or approval of the manuscript.
Disclaimer: The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources.
References
- 1.Runyan CW, Casteel C. The state of home safety in America: Facts about unintentional injuries in the home. 2. Washington, D.C: Home Safety Council; 2004. [Google Scholar]
- 2.SMARTRISK. The economic burden of injury in Canada. SMARTRISK; Toronto, ON: 2009. [Google Scholar]
- 3.Ontario Association of Fire Chiefs. Position paper: Residential fire sprinklers. [Accessed January 2014];Ontario Association of Fire Chiefs. 2011 Available from http://www.oafc.on.ca/oafc-position-paper-residential-sprinklers.
- 4.The Office of the Fire Marshal and Emergency Management. Ontario Residential Fires: 2008 to 2012. Ministry of Community Safety and Correctional Services; [Accessed May 2014]. Available from http://www.mcscs.jus.gov.on.ca/english/FireMarshal/MediaRelationsandResources/FireStatistics/OntarioFires/HomeFires-Injuries/stats_injuries_res.html. [Google Scholar]
- 5.Ahrens M. Smoke alarms in US home fires. National Fire Protection Association; Quincy, MA: 2011. [Google Scholar]
- 6.Garis L, Clare J. Sprinkler systems and residential structure fires: Exploring the impact of sprinklers for life safety and fire spread. Centre for Public Safety and Criminal Justice Research, School of Criminology and Criminal Justice, University of the Fraser Valley; 2013. [Google Scholar]
- 7.Wieczorek CJ, Ditch B, Bill RG. Environmental impact of automatic fire sprinklers. FM Global Research Division; 2010. [Google Scholar]
- 8.Jakubowski G. Communities with home fire sprinklers: The experience in Bucks County. Pennsylvania: Home Fire Sprinkler Coalition; 2011. [Google Scholar]
- 9.Weatherby S. Benefits of residential fire sprinklers: Prince George’s County 15-year history with its single-family residential dwelling fire sprinkler ordinance. Home Fire Sprinkler Coalition. 2009 [Google Scholar]
- 10.Ford J. Saving Lives, Saving Money: Automatic Sprinklers: A 10 year study. Scottsdale, Ariz. City of Scottsdale: Rural/Metro Fire Department, Home Fire Sprinkler Coalition; 1997. [Google Scholar]
- 11.Ford J. Years of Built-in Automatic Fire Sprinklers: The Scottsdale Experience. Scottsdale, Arizona. City of Scottsdale, AZ: Rural/Metro Fire Department and the Home Fire Sprinkler Coalition; 1997. [Google Scholar]
- 12.XE. [Accessed March 2014]; Available from http://www.xe.com/
- 13.Klein MB, Hollingworth W, Rivara FP, et al. Hospital costs associated with pediatric burn injury. J Burn Care Res. 2008;29:632–37. doi: 10.1097/BCR.0b013e31817db951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Griffiths HR, Thornton KL, Clements CM, et al. The cost of a hot drink scald. Burns. 2006;32:372–74. doi: 10.1016/j.burns.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 15.American Burn Association. [Accessed May 2014];National Burn Repository Report. 2014 Available from www.ameriburn.org/2014NBRAnnualReport.pdf.
- 16.Ahn C, Maitz PK. The true cost of burn. Burns. 2012;28:967–974. doi: 10.1016/j.burns.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 17.Jeevan R, Rashid A, Lympeopoulos NS, et al. Mortality and treatment cost estimates for 1075 consecutive patients treated by a regional adult burn service over a five year period: The Liverpool experience. Burns. 2013;40:214–22. doi: 10.1016/j.burns.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 18.Runyan CW, Baker SP. Preventing injuries by understanding energy damage. Bull World Health Organ. 2009;87:402–403. doi: 10.2471/BLT.09.063586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garis L. [Accessed May 2014];The impact of residential sprinklers on public fire protection. Available from http://www.surrey.ca/files/DCT_The_Impact_of_Residential_Sprinklers_on_Public_Fire_Protection.pdf.
- 20.Newport Partners. The Home Fire Sprinkler Cost Assessment. The Fire Protection Research Foundation; Quincy, MA: 2013. [Accessed January 2014]. Available from http://www.nfpa.org/~/media/Files/Research/Research%20Foundation/Research%20Foundation%20reports/Suppression/HomeFireSprinklerCostAssessment2013.pdf. [Google Scholar]
- 21.Butry DT. Comparing the performance of residential fire sprinklers with other life-safety technologies. Accid Anal Prev. 2012;48:480–94. doi: 10.1016/j.aap.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Statistics Canada. [Accessed July 2014];Private household by structural type of dwelling, by province and territory (2011 Census) Available from http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/famil55b-eng.htm.
- 23.Statistics Canada. [Accessed July 2014];Table 027-0008 Canada Mortgage and Housing Corporation, housing starts, under construction and completions, all areas quarterly (units) Available from http://www5.statcan.gc.ca/cansim/a05?lang=eng&id=0270008&pattern=0270008&searchTypeByValue=1&p2=35.
- 24.Canada Mortgage and Housing Corporation. [Accessed July 2014];Housing Market Outlook Ontario Region Highlights. Available from www.cmhc-schl.gc.ca/odpub/esub/65434/65434_2014_Q02.pdf.
- 25.Hansen RG. [Accessed July 2014];Thinking outside the box: a low cost retrofit design for residential fire sprinkler system installations in Pinellas Park, FL. 2008 Available from http://www.usfa.fema.gov/pdf/efop/efo42856.pdf.
- 26.Newport Partners LLC. Incentives for the use of residential fire sprinkler systems in US communities. The Fire Protection Research Foundation; Quincy, MA: 2010. [Accessed January 2014]. Available from http://www.nfpa.org/research/fire-protection-research-foundation/reports-and-proceedings/suppression/home-fire-sprinklers/incentives-for-the-use-of-residential-fire-sprinkler-systems. [Google Scholar]