Abstract
Background
Oxytocin (OT), a hormone most commonly associated with parturition and lactation, may have additional roles in diabetes complications. We determined OT levels in premenopausal women with type 1 diabetes mellitus (T1DM) compared to nondiabetic controls; and examined associations of OT with health behaviors, clinical factors, biomarkers, kidney function, and bone health. Lower OT was hypothesized for T1DM.
Methods
Cross-sectional study of premenopausal women with T1DM (n=88) from the Wisconsin Diabetes Registry Study, a population-based cohort of incident T1DM cases, and matched nondiabetic controls (n=74).
Results
Women with T1DM had lower OT levels than controls adjusting for caffeine and alcohol use (p=0.03). Health behaviors associated with OT differed between women with and without T1DM: OT was negatively associated with hormonal contraceptive use (quantified as lifetime contraceptive estrogen exposure) in women with T1DM (p=0.003) while positively related to hormonal contraceptive use (quantified as never/former/current) in controls (p<0.001). OT had a positive association with adiposity (waist-to-hip ratio and leptin) in women with T1DM and a negative relationship with adiposity (weight gain) in controls. In T1DM only, OT was positively associated with caffeine intake (p=0.01) and negatively associated with alcohol use (p=0.01). OT was not related to glycemic control, kidney function, or bone health in T1DM.
Conclusions
OT levels are lower in women with T1DM than matched controls. OT also has opposing associations with hormonal contraceptives and adiposity in women with and without T1DM. Research is needed to determine if the altered OT milieu in T1DM is associated with other health outcomes.
Key Terms: Oxytocin, Type 1 Diabetes, Hormonal Contraceptives, Adiposity
Introduction
Oxytocin (OT), a hormone known for its association with parturition and lactation, has evolutionary and pharmacological actions. OT is synthesized primarily by neurons in the supraoptic and paraventricular nuclei of the hypothalamus and released from the posterior pituitary. Centrally, OT is associated with maternal, sexual, social, and stress-related behaviors [1]; peripherally, OT is most commonly associated with smooth muscle contraction in both the female and male reproductive tract [1]. There is increasing evidence that OT also has diverse effects on fat and bone tissue, as well as on the pancreas, heart, and kidney [2,3]. For example, OT is negatively associated with body fat mass [4–6] in the absence of chronic disease.
Type 1 diabetes mellitus (T1DM) is an autoimmune disorder causing destruction of the insulin producing β-cells of the pancreas. T1DM accounts for 5–10% of those with diabetes and is characterized by an absolute insulin deficiency due to β-cell destruction [7]. Few studies have investigated OT in humans with T1DM. One study examined OT’s role in glucose counter-regulation during hypoglycemia and found that circulating OT concentrations after insulin-induced hypoglycemia were higher in individuals with T1DM than controls [8]. In another study of individuals with T1DM, there was a significant elevation of plasma glucagon after OT treatment in both the basal condition and during insulin-induced hypoglycemia, enhancing glucose recovery [9]. Although these studies have small sample sizes, they demonstrate a potential role of OT to increase glucose levels in response to hypoglycemia in T1DM. In contrast, OT and OT analogs have been studied in streptozotocin treated mice (model of T1DM) and demonstrated enhanced insulin secretion and lower glucose [10]. Since people with T1DM avoid insulin-induced hypoglycemia and have an absolute insulin deficiency, it is unclear if the results of these tightly controlled studies can be generalized to individuals living with T1DM. However, these studies taken together may suggest that OT maintains glucose levels within an optimal range via glucagon and insulin secretion in the context of glucose variability.
Recently, observational studies have been conducted examining OT and its relationship to diabetes complications. In studies including both T1DM and type 2 diabetes participants, lower levels of OT were associated with both cardiomyopathy [11,12] and gastroparesis [13]. OT has also been associated with mental health complications, such as depression, in people with type 2 diabetes [14]. The relationship of OT with other diabetes complications has not yet been examined.
Therefore, the current study determined OT levels in premenopausal women with T1DM from a population-based cohort and compared levels to those in matched controls without diabetes. We hypothesized women with T1DM would have lower levels of OT because of OT’s negative association with complications. Factors associated with OT were also examined in both groups of women, including health behaviors and clinical factors (e.g., diet, adiposity, and medications), glycemic control, biomarkers, kidney function and bone health.
Materials and Methods
Participants
The Wisconsin Diabetes Registry Study (WDRS) is a longitudinal study of a population-based cohort of incident cases with T1DM whose ascertainment and recruitment methods have been previously published [15,16]. Briefly, the WDRS included individuals (n=597) with T1DM diagnosed ≤ 30 years of age, between May 1987 and April 1992, who lived in 28 contiguous counties in south-central Wisconsin. T1DM was defined by the presence of polyuria and polydipsia with initiation of exogenous insulin use.
Of the original 288 female WDRS participants, 191 met the preliminary enrollment criteria in 2005 for an ancillary study on bone health in women with T1DM (continued participation in WDRS, 18–50 years of age, premenopausal, and living in Wisconsin) [15]. After recruitment, 89 eligible women with T1DM participated. The women were asked to identify a matched control (in priority order) as a full or half-sister, female cousin, niece/aunt, or female friend without diabetes, of the same race/ethnicity and within five years of age, up to 10 years if needed. Consequently, both groups potentially shared unmeasured genetic and lifestyle factors. Seventy-six controls participated.
The study was approved by the Institutional Review Boards at the University of Wisconsin-Madison and the University of Illinois at Chicago. Participants provided written informed consent at enrollment, at all subsequent study visits, and for the analysis of archived blood samples.
Data Collection and Variables
Health Behaviors and Clinical Characteristics
Height, weight, body mass index (BMI), and waist and hip circumferences were measured using standard methods previously published [15]. Information collected by questionnaire included: demographics; health behaviors such as smoking history, current supplement and medication use, and weight change within the last year; reproductive history such as age at menarche, average length of menstrual cycles, pregnancy history, and hormonal contraceptive use; and diabetes-related factors such as disease duration, insulin dose, insulin pump use, and frequency of blood glucose monitoring. Daily dietary intake of calcium, vitamin D, caffeine and alcohol were determined via a brief food frequency questionnaire [17]. Physical activity was measured using the Five-City Project physical activity assessment, and quantified as daily total energy expenditure. Vigorous physical activity was defined as activity of at least six metabolic equivalents [18].
OT, Bone Markers, and Biomarkers
Study visits were scheduled during days 20–24 of the menstrual cycle (luteal phase), and blood was drawn without regard to fasting, time of day, or time of year. To rule out hypoglycemia before blood was drawn, a random glucose level was measured in the women with T1DM using the study glucometer and was 60 mg/dl or higher in all women. The serum was immediately separated onsite and frozen in a portable −80°C freezer. The following biomarkers were measured within four months of collection. Osteocalcin (bone formation marker) was analyzed by Fairview Diagnostic Labs (Minneapolis, MN) using a chemiluminescent immunoassay. N-terminal cross-linked telopeptides (NTx; bone resorption marker) were measured by Dynacare Labs (Milwaukee, WI) with an enzyme immunoassay. The intra- and inter-assay coefficients of variation (CVs) were ≤9% for osteocalcin and ≤14% for NTx. Bioavailable (free and albumin-bound fractions) and total (bioavailable and sex-hormone-binding globulin-bound fractions) 17β-estradiol were measured in serum by the Inter Science Institute (Inglewood, CA). Total estradiol was determined by radioimmunoassay utilizing a specific antibody directed against estradiol conjugated to bovine serum albumin. The bioavailable portion was determined by radio partition chromatography. The intra-assay CVs were 13% for both; the inter-assay CV was ≤17% for total and ≤25% for bioavailable estradiol.
Serum and plasma samples frozen at −80°C for five years were used to determine the following biomarkers; one control did not consent to archive samples for future analysis. Plasma OT was analyzed at the University of Illinois at Chicago (UIC) by enzyme immunoassay with kits from Enzo Life Sciences (Plymouth Meeting, PA). The intra- and inter-assay CVs were ≤14.5%. OT levels were not able to be quantified in one woman with T1DM and one control. As OT was the dependent variable of interest, the final sample size for the current analysis therefore included those with OT data, n=88 T1DM cases and n=74 controls. Serum bone-specific alkaline phosphatase (BAP; bone formation marker) and tartrate-resistant acid phosphatase (TRAP5b; bone resorption marker) were measured by Northwestern University’s Comprehensive Center on Obesity: Metabolic Hormone Core Lab (Evanston, IL) by enzyme immunoassay with kits from Quidel Corporation (San Diego, CA). The intra- and inter-assay CVs were ≤7.6% for BAP and ≤3.0% for TRAP5b. Serum receptor activator of nuclear factor κβ ligand (RANKL) and osteoprotegerin (OPG; both markers of bone cell signaling) were measured by the Research Resource Core at UIC by fluorescently labeled microsphere beads from Millipore (St. Charles, MO). The intra- and inter-assay CVs were ≤6.0% for RANKL and ≤6.5% for OPG. The manufacturer’s insert for RANKL indicates that the kit can reliably detect values below 4.8 pg/ml using extrapolation. For this analysis, values ≥1.1 pg/ml were included as measured; for 13 women (eight controls and five women with T1DM) with values <1.1 pg/ml, the value was set at 1.1 pg/ml [19]. One T1DM woman did not have enough archived serum for BAP, TRAP5b, RANKL, and OPG; and two T1DM women had OPG values excluded because of extremely high levels (>6,700 pg/ml). Plasma adiponectin and leptin concentrations were quantified at UIC using high-sensitivity enzyme immunoassay kits (R&D Systems, Minneapolis, MN). Intra-assay CVs of adiponectin and leptin were 4.3% and 4.9%, respectively. There was insufficient archived plasma from one control for adiponectin and leptin determination.
Glycemic Control
Whole blood samples were analyzed for hemoglobin A1C (A1C) within seven days of collection by Fairview Diagnostic Labs (Minneapolis, MN). Automated high-performance liquid chromatography was used following the Diabetes Control and Complications Trial reference method [20]. The non-diabetic range for this assay is 4.3–6.0%. The intra-assay CV was 0.6%; the inter-assay CV was ≤3.3%.
Kidney Function
Cystatin-C was measured in archived serum using the Milliplex Human Kidney Toxicity Panel 2 kit (Millipore Corp., St. Charles, MO) with the Luminex system by the Research Resource Core at UIC. Cystatin-C was not able to be determined for two T1DM women due to insufficient archived sample. The intra- and inter-assay CVs were ≤9%. Estimated glomerular filtration rate (eGFR) was calculated using the CKD-EPI equation [21]: eGFR=127.7 × (Cystatin-C (pg/ml)/1000)−1.17 × age−0.13 × 0.91.
Bone Mineral Density (BMD)
Bilateral heel (calcaneus) and forearm (distal radius/ulna) BMD was measured in all participants by dual-energy X-ray absorptiometry (DXA) using the Peripheral Instantaneous X-Ray Imager (PIXI, GE Lunar, Madison, WI). Means of bilateral heel and forearm measurements were analyzed. All measurements were performed by one technologist. CVs of repeated measurements with repositioning were ≤3% at both sites.
Statistics
Analyses were performed using SPSS Version 17.0 (IBM Corporation, Somers, NY) and SAS Version 9.2 (SAS Corporation, Cary, NC). Skewed biomarkers (e.g., OT) were log-transformed. Independent variables with outliers were categorized into quartiles (e.g., alcohol intake) or using clinically relevant cut-points (e.g., change in weight). Statistical tests were considered significant at p<0.05.
To account for the matching between women with and without T1DM (i.e., the non-independence of the two groups), comparisons of variables between the two groups used linear (PROC MIXED to compare means) and non-linear (PROC GLIMMIX to compare proportions) mixed regression models with a random intercept, specifying the matched pair number in the subject option. Linear mixed regression models accounting for matching were then used to examine the difference in OT between women with and without T1DM; potential confounding was explored by individually entering covariates and assessing for a 10% change in the regression coefficient quantifying the difference in OT between the two groups. All covariates were tested as potential confounders, as there is limited information on factors associated with OT in diabetes. Confounders were retained in the final adjusted model of the difference in OT between the two groups.
Pearson correlation coefficients were used to determine bivariate associations of OT with covariates after stratification by T1DM status. Multivariable linear regression models estimating OT, stratified by T1DM status, were then built by entering all covariates with p≤0.15 from the Pearson correlations, and using a backwards stepwise approach to remove the non-significant covariates. Potential interactions between remaining covariates were tested, and reported if significant. Any covariate with a significant association with OT in women with T1DM but not controls, and vice versa, was tested for effect modification by diabetes status using linear mixed regression modeling accounting for the matching in the combined sample, and reported when significant.
Results
Participants
Clinical characteristics of the sample are presented in Table 1. The sample was 97% non-Hispanic White. In comparison to controls, those with T1DM had significantly higher caffeine intake, lower alcohol consumption, longer menstrual cycles, were more likely to be receiving thyroid replacement therapy, had higher A1C values and adiponectin levels, and lower levels of osteocalcin and heel and forearm BMD.
Table 1.
Sample Characteristics Stratified by T1DM
| Control (n=74) | T1DM (n=88) | |
|---|---|---|
| Age (years) | 28.4 ± 8.2 | 27.9 ± 6.8 |
| BMI (kg/m2) | 27.1 ± 6.1 | 28.1 ± 6.0 |
| Waist-to-hip ratio | 0.77 ± 0.05 | 0.78 ± 0.06 |
| Caffeine intake (quartiles of mgs/day), n (%) | ||
| 1st: 0 – 33.6 | 22 (30) | 17 (19)* |
| 2nd: 33.7 – 94.4 | 24 (32) | 18 (20) |
| 3rd: 94.5 – 171.3 | 13 (18) | 27 (31) |
| 4th: 171.4 – 709.1 | 15 (20) | 26 (30) |
| Alcohol intake (quartiles of grams/day), n (%) | ||
| 1st: 0 – 1.08 | 12 (16) | 31 (35)** |
| 2nd: 1.09 – 3.11 | 17 (23) | 20 (23) |
| 3rd: 3.12 – 8.64 | 20 (27) | 21 (24) |
| 4th: 8.65 – 79.18 | 25 (34) | 16 (18) |
| Taking calcium supplement, n (%) | 36 (49) | 38 (43) |
| Weight change in last year, n (%) | ||
| Lost ≥ 10 pounds | 19 (26) | 15 (17) |
| Maintained ± 9.9 pounds | 43 (58) | 59 (67) |
| Gained ≥ 10 pounds | 12 (16) | 14 (16) |
| History of smoking, n (%) | 43 (58) | 51 (58) |
| Vigorous physical activity (kcalories/kg/day), n (%) | ||
| None | 28 (38) | 39 (44) |
| > 0 to 2.6 | 29 (39) | 26 (30) |
| > 2.6 | 17 (23) | 23 (26) |
| Mean menstrual cycle length, n (%) | ||
| 22 to 39 days | 69 (93) | 65 (74)** |
| 40 to 89 days | 2 (3) | 12 (14) |
| ≥ 90 days | 3 (4) | 11 (12) |
| Taking thyroid replacement medication, n (%) | 5 (7) | 17 (19)* |
| Estrogen contraceptive use, n (%) | ||
| Never | 15 (20) | 23 (26) |
| Former | 30 (41) | 33 (38) |
| Current | 29 (39) | 32 (36) |
| Diabetes-related | ||
| Hemoglobin A1C (%) | 5.0 ± 0.3 | 8.1 ± 1.7*** |
| Cystatin-C (log; ng/ml)a | 7.4 ± 0.8 | 7.4 ± 0.6 |
| eGFR (log; mL/min/1.73 m2)a | 3.8 ± 0.9 | 3.8 ± 0.7 |
| Diabetes duration (years) | 16.0 ± 1.5 | |
| Blood glucose monitoring (readings per day) | 3.7 ± 1.9 | |
| Use insulin pump, n (%) | 39 (44.3) | |
| Insulin dose (units/kg/day) | 0.79 ± 0.45 | |
| Bone mineral densities (g/cm2) | ||
| Heel | 0.532 ± 0.092 | 0.492 ± 0.093** |
| Forearm | 0.465 ± 0.052 | 0.441 ± 0.048*** |
| Bone turnover markers | ||
| Osteocalcin (ng/ml) | 4.6 ± 1.8 | 3.6 ± 1.6*** |
| BAP (U/L)a | 23.5 ± 9.1 | 24.8 ± 7.9 |
| NTx (log; nmol BCE/L) | 1.0 ± 0.1 | 1.0 ± 0.1 |
| TRAP 5b (U/L)a | 2.3 ± 0.9 | 2.4 ± 1.0 |
| RANKL (log; pg/ml)a | 1.2 ± 0.6 | 1.2 ± 0.6 |
| OPG (pg/ml)a | 1376.7 ± 837.4 | 1379.1 ± 560.8 |
| Biomarkers | ||
| OT (log; pg/ml) | 2.4 ± 0.4 | 2.3 ± 0.4 |
| Leptin (pg/ml)a | 22.1 ± 10.3 | 19.9 ± 11.0 |
| Adiponectin (ng/ml)a | 4155.6 ± 1822.4 | 8649.1 ± 4099.6*** |
| Total estradiol (pg/ml) | 295.7 ± 118.1 | 302.0 ± 137.7 |
| Bioavailable estradiol (pg/ml) | 65.2 ± 34.1 | 67.4 ± 34.1 |
Note. Continuous data are expressed as mean ± standard deviation. Categorical data are expressed as n (%). eGFR, estimated Glomerular Filtration Rate; BAP, Bone-specific Alkaline Phosphatase; NTx, N-Terminal cross-linked telopeptides; BCE, Bone Collagen Equivalent; TRAP5b, Tartrate-Resistant Acid Phosphatase 5b; RANKL, Receptor Activator of Nuclear factor κβ Ligand; OPG, Osteoprotegerin
T1DM: Cystatin-C and eGFR (n=86)
BAP, TRAP5b, and RANKL (n=87)
OPG (n=85)
Control: Leptin and Adiponectin (n=73)
p < 0.05
p < 0.01
p < 0.001
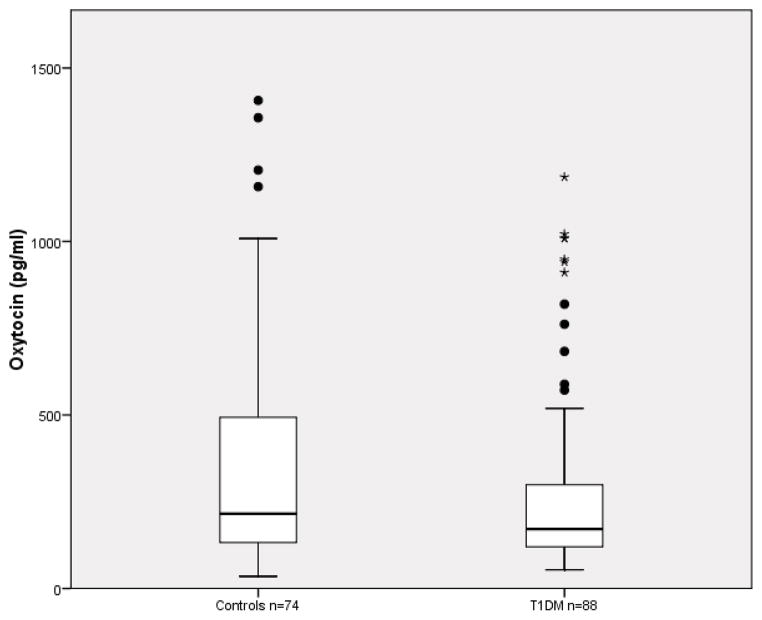
Oxytocin Levels
A box and whisker plot of the non-transformed OT levels for women with T1DM and controls is presented in Figure 1. Log-transformed OT levels (pg/ml) were lower in the T1DM women compared to controls (2.3 vs. 2.4, p=0.17; Table 1). After controlling for confounding by caffeine and alcohol use, the log-transformed OT levels were significantly lower in women with T1DM (2.2 vs. 2.4, p=0.03).
Figure 1.
Oxytocin Levels (pg/ml)
Mean ± Standard Deviation: Controls = 346.3 ± 324.2, T1DM = 280.7 ± 264.5
Median ± 25th to 75th Percentile: Controls = 215.2 ± 363.0, T1DM = 171.2 ± 182.0
Oxytocin (log OT) Models
Bivariate Associations
Health behaviors
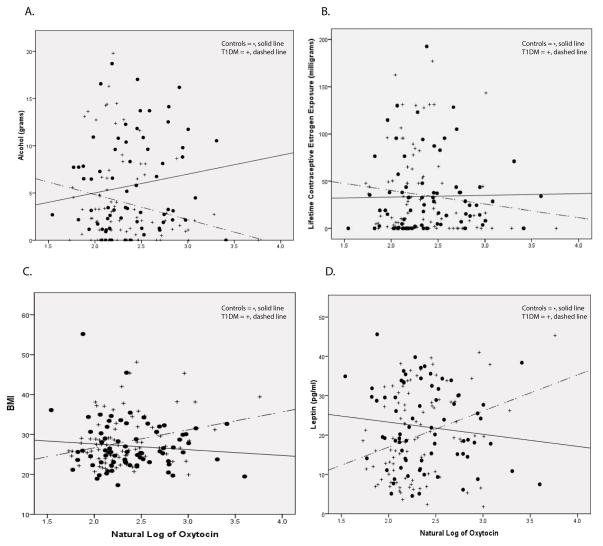
Caffeine consumption (quartiles) was positively associated with OT in T1DM (β=0.08, p=0.03) but not associated in controls. Alcohol intake (quartiles) was negatively associated with OT in T1DM (β=−0.08, p=0.03), but not associated in controls, and the interaction between alcohol intake and the presence of T1DM on OT was significant (p=0.008). Figure 2A is a plot of OT with alcohol intake as a continuous variable. Currently taking a calcium supplement was marginally positively associated with OT in T1DM (p=0.13) and was used in multivariable modeling. There were no significant associations for either group of OT with age, dietary calcium consumption, smoking, physical activity, or taking either anti-hypertensive or thyroid medications (all p>0.15).
Figure 2.
Associations with OT in Controls (n=74) and T1DM (n=88)
A. Daily Alcohol Intake (grams): excludes influential outliers with alcohol intake >20 grams, controls=69, T1DM=85
B. Lifetime Contraceptive Estrogen Exposure (mgs)
C. BMI (kg/m2)
D. Leptin (pg/ml)
Reproductive history
There was a difference in the association of OT with contraceptive estrogen use between women with and without T1DM. History of estrogen contraceptive use (never/former/current) was positively associated with OT in controls (β=0.17, p=0.005), but was not associated in women with T1DM; T1DM significantly modified this association of history of estrogen contraceptive use and OT (p=0.003). Conversely, when hormonal contraceptive use was examined via a different variable, lifetime contraceptive estrogen exposure (quartiles), it was negatively associated with OT in women with T1DM (β =−0.08, p=0.02), and not associated in controls, with effect modification by T1DM (p=0.058). Figure 2B is a plot of OT with lifetime contraceptive estrogen exposure as a continuous variable. OT was not associated with length of menstrual cycles, history of pregnancy and breastfeeding, or circulating total and bioavailable estrogen in either group.
Adiposity
The association of OT with adiposity also differed between the two groups. In women with T1DM, positive associations with OT were found for BMI (β=0.02, p=0.01), waist-to-hip ratio (1/10th of a unit, β=0.15, p=0.02), and leptin (pg/ml, β=0.01, p=0.004). No association with OT was found in controls for BMI, waist-to-hip ratio, or leptin. BMI and leptin had significant interactions with T1DM on OT (p=0.01 and p=0.006, respectively) (Figures 2C and 2D). Change in weight (lost/maintained/gained) was marginally negatively associated with OT in controls (p=0.15) and was used in multivariable modeling. OT was not associated with adiponectin in either group.
Kidney function and bone health
OT was not related to either Cystatin-C or eGFR in women either with or without T1DM. However, OT and NTx (log; nmol bone collagen equivalents (BCE)/L) were positively associated in women with T1DM (β=0.54, p=0.04). There was no association of OT with NTx in controls. RANKL was marginally positively associated with OT in controls (p=0.11) and was used in multivariable modeling, but not associated in women with T1DM. OT was not associated with heel or wrist BMD, osteocalcin, BAP, TRAP5b, or OPG in either group.
Diabetes-specific factors
In women with T1DM, there was a positive association between OT and insulin dose (1/10th unit/kg/day, β=0.02, p=0.02). No associations were found for OT with A1C, random glucose, duration of T1DM, insulin pump use, or the number of blood glucose readings per day.
Multivariable Models
Regression models of OT for women with T1DM and controls are presented in Table 2. In the control model, OT was positively associated with current estrogen contraceptive use, negatively associated with weight gain, and positively associated with RANKL. In the T1DM model, OT was negatively associated with alcohol intake and lifetime contraceptive estrogen exposure; and positively with caffeine use, calcium supplement use, and leptin. There was an interaction between waist-to-hip ratio and insulin dose on OT in women with T1DM (p=0.02). For women with lower insulin doses, waist-to-hip ratio had no association with OT, but at higher doses, waist-to-hip ratio had a positive association with OT (Figure 3).
Table 2.
Multivariable Linear Regression Models Predicting OT (log; pg/ml) Stratified by T1DM
| Control (n=74) | T1DM (n=88) | |||
|---|---|---|---|---|
| Variables | β | p value | β | p value |
| Health Behaviors | ||||
| Quartiles of alcohol intakea | - | −0.08 | 0.007 | |
| Quartiles of caffeine intakeb | - | 0.09 | 0.005 | |
| Taking calcium supplementc | - | 0.14 | 0.04 | |
| Reproductive History | ||||
| Estrogen contraceptive used | 0.22 | 0.0004 | - | |
| Quartiles of lifetime contraceptive estrogen exposuree | - | −0.09 | 0.003 | |
| Adiposity | ||||
| Change in weightf | −0.14 | 0.046 | - | |
| Waist-to-hip ratio (1/10th unit) | - | −0.21 | 0.18 | |
| Leptin (pg/ml) | - | 0.01 | 0.02 | |
| Bone | ||||
| RANKL (log; pg/ml) | 0.18 | 0.02 | - | |
| Diabetes Specific Factors | ||||
| Insulin dose (1/10th unit/kg) | - | −0.34 | 0.02 | |
| Interaction | ||||
| Insulin dose * waist-to-hip ratio | - | 0.04 | 0.02 | |
| Adjusted R2 | 0.18 | 0.39 | ||
Note. RANKL, Receptor Activator of Nuclear factor κβ Ligand
0=0–1.08 grams/day, 1=1.09–3.11 grams/day, 2=3.12–8.64 grams/day, 3=8.65–79.18 grams/day
0=0–33.6 mgs/day, 1=33.7–94.4 mgs/day, 2=94.5–171.3 mgs/day, 3=171.4–709.1 mgs/day
0=no, 1=yes
0=never, 1=former, 2=current
0=0–0.93 mgs, 1=0.94–17.19 mgs, 2=17.20–47.78 mgs, 3=47.79–192.47 mgs
0=lost ≥ 10 pounds, 1=maintained (± 9.9 pounds), 2=gained ≥ 10 pounds
Figure 3.
Association of OT with Waist-to-Hip Ratio in T1DM (n=88) is Modified by Insulin Dose (interaction p=0.02). The figure is plotted using T1DM percentiles of waist-to-hip ratio (10th, 25th, 50th, 75th) and insulin dose (25th, 50th, 75th).
Discussion
OT in humans with T1DM and type 2 diabetes has previously been examined in the context of gastric and cardiac complications [11–13], and in basal conditions and insulin-induced hypoglycemia [8,9]. In mice with streptozotocin induced diabetes, OT treatment has been associated with improved insulin secretion [10]. This is the first study to our knowledge to report that circulating OT levels may be lower in premenopausal women with T1DM compared to matched controls. OT has been widely studied in the context of social behaviors, including OT’s inverse association with stress and depression [22]. The increased stress and higher levels of depression found in individuals with T1DM [23,24] may explain the lower OT levels in our sample of T1DM women. Young women with anorexia nervosa, a disease similarly characterized by co-morbid anxiety and depression, have also been found to have lower levels of OT [25]. Interestingly, research in animal models of T1DM has demonstrated that OT levels in the hypothalamus are higher in the presence of diabetes [26]. This, in addition to evidence that there is a disturbance in the Hypothalamic-Pituitary-Adrenocortical (HPA) Axis in animal models of T1DM [27], might suggest an alteration in the release of OT into the peripheral circulation as another explanation for the lower levels of OT in T1DM. OT levels were not associated with diabetes management, glycemic control, random glucose level, or kidney or bone complications in our sample of young women with T1DM.
Adiposity/Leptin
Figure 4 represents a summary of the multivariable associations found in this study for controls (Figure 4A) and women with T1DM (Figure 4B). Similar to previous research on the association of OT with eating behaviors and weight gain [4,28], we found an association of low OT with weight gain in the last year for controls. Though there are limited data on the association of circulating OT with leptin in humans [29], our results demonstrating no association of circulating OT with leptin or fat mass (e.g., BMI, waist-to-hip ratio) in controls is consistent with a previous study in women [30].
Figure 4.
Multivariable Models for Oxytocin
A. Controls
B. T1DM
In contrast, the positive associations of OT with waist-to-hip ratio and leptin in the women with T1DM are novel findings; indeed the effect modification by diabetes status on the association of OT with fat/leptin was statistically significant. Notably, in the women with T1DM, the positive association between OT and waist-to-hip ratio became stronger with higher daily insulin dosing. Previous basic science research has demonstrated that the combined effect of OT and insulin on the function of adipocytes is very complex and depends on the levels of each in vitro [31]. Further research is needed to begin to elucidate the complex mechanisms involved between OT/fat/insulin in humans with T1DM. OT’s positive association with leptin in the women with T1DM is consistent with the strong relationship between fat and leptin in girls with T1DM [32].
Contraceptive Use
The positive association between OT and current contraceptive estrogen use in controls is consistent with previous literature on OT and contraceptive use [33,34]. It has also been reported that estradiol treatment promotes the activation of OT producing neurons, resulting in higher circulating OT levels [33,34]. In comparison, a novel finding in the current study was a negative association of OT with contraceptive estrogen exposure in our T1DM sample. Again, the effect modification by diabetes status on the association of OT with contraceptive estrogen use was statistically significant. The mechanism of this interaction is currently unknown, as there are no studies in animals or humans examining estrogen and OT levels in the presence of T1DM. Perhaps the OT neurons in women with T1DM are suppressed by estrogen as a function of HPA disruption in T1DM [27].
Other Factors
The positive relationship between OT and the bone cell signaling marker RANKL demonstrated in controls has been previously reported [6], and is consistent with the association between higher OT and greater BMD [30,35,36]. This is the first study to our knowledge to explore the relationship between OT and behavioral factors such as caffeine and alcohol use in T1DM; OT was positively associated with caffeine intake, and negatively associated with alcohol use, in women with T1DM. Perhaps the lower levels of OT in women with T1DM lead to lower energy levels, as has been shown in non-diabetic models [37], and women with T1DM may elect to use caffeine and avoid alcohol to improve their energy levels. This might explain the significant differences in daily intake of caffeine and alcohol compared with controls. Interestingly, alcohol’s negative association with OT is supported by literature in lactating women [38], which found lower levels of OT when alcohol was given during lactation. The positive relationship of OT with current calcium supplement use in women with T1DM is supported by previous basic science research demonstrating that the release of OT from the pituitary gland is greater with increasing calcium concentrations in vitro [39].
Limitations/Strengths
The sample included only females and was 98% non-Hispanic White. Therefore, the results may not be generalizable to males or other race/ethnicities. However, the homogeneity of the sample increases internal validity. The cross-sectional design limits interpretation of any associations as causal. Many of the variables are self-reported data, but validated questionnaires were used. The study strengths include the selection of matched controls, potentially accounting for unmeasured genetic and lifestyle factors, which is important in determining the independent association of T1DM with OT.
Conclusion
In the current study, we found that premenopausal women with T1DM have lower levels of OT compared to matched controls, and that there were no associations of OT with diabetes management or complications. This is the first study to our knowledge to report that the association of OT with adiposity, hormonal contraceptives, alcohol, and caffeine use may be different for women with T1DM than controls. How these lower levels and differential associations contribute to OT’s action in women with T1DM remains unknown. Research is needed to explore the possible mechanistic links of OT with clinical factors and behaviors in T1DM and type 2 diabetes, and whether the altered OT milieu impacts other health outcomes such as reproduction.
Acknowledgments
GRANT SUPPORT: Grant Number 1-05-CR-35 from the American Diabetes Association; Grant Number K12HD055892 from the National Institute of Child Health and Human Development (NICHD) and the National Institutes of Health Office of Research on Women’s Health (ORWH); Grant Number R01DK036904 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); and Grant Number UL1RR029879 from the National Center for Research Resources, National Institutes of Health.
We gratefully acknowledge the study participants and staff of the Wisconsin Women and Diabetes Study, the Wisconsin Diabetes Registry Study, the Osteoporosis Clinic Research Program, and Hossein Pournajafi-Nazarloo for performing the oxytocin immunoassays. We thank Chih-Hsiung Edward Wang and Carol J. Ferrans for providing feedback in the writing of this paper, and Kevin Grandfield and Rebecca Monson for editorial assistance. This study was previously published in abstract form at the 73rd Annual Meeting of the American Diabetes Association, June 2013.
Footnotes
DISCLOSURE STATEMENT: Authors have nothing to declare.
References
- 1.Tom N, Assinder SJ. Oxytocin in health and disease. Int J Biochem Cell Biol. 2010;42(2):202–205. doi: 10.1016/j.biocel.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Lippert TH, Mueck AO, Seeger H, Pfaff A. Effects of oxytocin outside pregnancy. Horm Res. 2003;60(6):262–271. doi: 10.1159/000074243. [DOI] [PubMed] [Google Scholar]
- 3.Zingg HH, Laporte SA. The oxytocin receptor. Trends Endocrinol Metab. 2003;14(5):222–227. doi: 10.1016/s1043-2760(03)00080-8. [DOI] [PubMed] [Google Scholar]
- 4.Deblon N, Veyrat-Durebex C, Bourgoin L, Caillon A, Bussier AL, Petrosino S, Piscitelli F, Legros JJ, Geenen V, Foti M, Wahli W, Di Marzo V, Rohner-Jeanrenaud F. Mechanisms of the anti-obesity effects of oxytocin in diet-induced obese rats. PLoS One. 2011;6(9):e25565. doi: 10.1371/journal.pone.0025565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maejima Y, Iwasaki Y, Yamahara Y, Kodaira M, Sedbazar U, Yada T. Peripheral oxytocin treatment ameliorates obesity by reducing food intake and visceral fat mass. Aging (Albany NY) 2011;3(12):1169–1177. doi: 10.18632/aging.100408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beranger GE, Pisani DF, Castel J, Djedaini M, Battaglia S, Amiaud J, Boukhechba F, Ailhaud G, Michiels JF, Heymann D, Luquet S, Amri EZ. Oxytocin reverses ovariectomy-induced osteopenia and body fat gain. Endocrinology. 2014;155(4):1340–1352. doi: 10.1210/en.2013-1688. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36 (Suppl 1):S67–74. doi: 10.2337/dc13-s067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher BM, Baylis PH, Thornton S, Frier BM. Arginine vasopressin and oxytocin responses to insulin-induced hypoglycemia in type 1 (insulin-dependent) diabetes. J Clin Endocrinol Metab. 1989;68(3):688–692. doi: 10.1210/jcem-68-3-688. [DOI] [PubMed] [Google Scholar]
- 9.Paolisso G, Sgambato S, Giugliano D, Pizza G, Tesauro P, Varricchio M, D’Onofrio F. Effects of oxytocin delivery on counter-regulatory hormone response in insulin-dependent (type 1) diabetic subjects. Horm Res. 1989;31(5–6):250–255. doi: 10.1159/000181126. [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Wu C, Chen Q, Chen X, Xu Z, Wu J, Cai D. Treatment of obesity and diabetes using oxytocin or analogs in patients and mouse models. PLoS One. 2013;8(5):e61477. doi: 10.1371/journal.pone.0061477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Florian M, Jankowski M, Gutkowska J. Oxytocin increases glucose uptake in neonatal rat cardiomyocytes. Endocrinology. 2010;151(2):482–91. doi: 10.1210/en.2009-0624. [DOI] [PubMed] [Google Scholar]
- 12.Gutkowska J, Broderick TL, Bogdan D, Wang D, Lavoie J, Jankowski M. Downregulation of oxytocin and natriuretic peptides in diabetes: Possible implications in cardiomyopathy. J Physiol (Lond ) 2009;587 (Pt 19):4725–4736. doi: 10.1113/jphysiol.209.176461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borg J, Melander O, Johansson L, Uvnas-Moberg K, Rehfeld JF, Ohlsson B. Gastroparesis is associated with oxytocin deficiency, oesophageal dysmotility with hyperCCKemia, and autonomic neuropathy with hypergastrinemia. BMC Gastroenterol. 2009;9:17–25. doi: 10.1186/1471-230x-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kontoangelos K, Raptis AE, Papageorgiou CC, Tsiotra PC, Papadimitriou GN, Rabavilas AD, Dimitriadis G, Raptis SA. Oxytocin and psychological factors affecting type 2 diabetes mellitus. Exp Diabetes Res. 2012;2012:560864. doi: 10.1155/2012/560864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Danielson KK, Elliott ME, LeCaire T, Binkley N, Palta M. Poor glycemic control is associated with low BMD detected in premenopausal women with type 1 diabetes. Osteoporos Int. 2009;20(6):923–933. doi: 10.1007/s00198-008-0763-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palta M, LeCaire T, Daniels K, Shen G, Allen C, D’Alessio D. Risk factors for hospitalization in a cohort with type 1 diabetes. Wisconsin Diabetes Registry. Am J Epidemiol. 1997;146(8):627–636. doi: 10.1093/oxfordjournals.aje.a009328. [DOI] [PubMed] [Google Scholar]
- 17.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122(1):51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 18.Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS., Jr Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 19.Stern A, Laughlin GA, Bergstrom J, Barrett-Connor E. The sex-specific association of serum osteoprotegerin and receptor activator of nuclear factor kappaB legend with bone mineral density in older adults: the Rancho Bernardo study. Eur J Endocrinol. 2007;156(5):555–562. doi: 10.1530/eje-06-0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(4):977–986. doi: 10.1056/nejm199309303291401. [DOI] [PubMed] [Google Scholar]
- 21.Stevens LA, Coresh J, Schmid CH, Feldman HI, Froissart M, Kusek J, Rossert J, Van Lente F, Bruce RD, 3rd, Zhang YL, Greene T, Levey AS. Estimating GFR using serum cystatin C alone and in combination with serum creatinine: a pooled analysis of 3,418 individuals with CKD. Am J Kidney Dis. 2008;51(3):395–406. doi: 10.1053/j.ajkd.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bakermans-Kranenburg MJ, van I Jzendoorn MH. Sniffing around oxytocin: review and meta-analyses of trials in healthy and clinical groups with implications for pharmacotherapy. Transl Psychiatry. 2013;3:e258. doi: 10.1038/tp.2013.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berlin KS, Rabideau EM, Hains AA. Empirically derived patterns of perceived stress among youth with type 1 diabetes and relationships to metabolic control. J Pediatr Psychol. 2012;37(9):990–998. doi: 10.1093/jpepsy/jss080. [DOI] [PubMed] [Google Scholar]
- 24.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25(3):464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 25.Lawson EA, Donoho DA, Blum JI, Meenaghan EM, Misra M, Herzog DB, Sluss PM, Miller KK, Klibanski A. Decreased nocturnal oxytocin levels in anorexia nervosa are associated with low bone mineral density and fat mass. J Clin Psychiatry. 2011;72(11):1546–1551. doi: 10.4088/jcp.10m06617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saravia FE, Gonzalez SL, Roig P, Alves V, Homo-Delarche F, De Nicola AF. Diabetes increases the expression of hypothalamic neuropeptides in a spontaneous model of type I diabetes, the nonobese diabetic (NOD) mouse. Cell Mol Neurobiol. 2001;21(1):15–27. doi: 10.1023/A:1007165127420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beauquis J, Homo-Delarche F, Revsin Y, De Nicola AF, Saravia F. Brain alterations in autoimmune and pharmacological models of diabetes mellitus: focus on hypothalamic-pituitary-adrenocortical axis disturbances. Neuroimmunomodulation. 2008;15(1):61–67. doi: 10.1159/000135625. [DOI] [PubMed] [Google Scholar]
- 28.Olszewski PK, Klockars A, Olszewska AM, Fredriksson R, Schioth HB, Levine AS. Molecular, immunohistochemical, and pharmacological evidence of oxytocin’s role as inhibitor of carbohydrate but not fat intake. Endocrinology. 2010;151(10):4736–4744. doi: 10.1210/en.2010-0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lawson EA, Holsen LM, Santin M, Meenaghan E, Eddy KT, Becker AE, Herzog DB, Goldstein JM, Klibanski A. Oxytocin secretion is associated with severity of disordered eating psychopathology and insular cortex hypoactivation in anorexia nervosa. J Clin Endocrinol Metab. 2012;97(10):E1898–908. doi: 10.1210/jc.2012-1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Breuil V, Amri EZ, Panaia-Ferrari P, Testa J, Elabd C, Albert-Sabonnadiere C, Roux CH, Ailhaud G, Dani C, Carle GF, Euller-Ziegler L. Oxytocin and bone remodelling: relationships with neuropituitary hormones, bone status and body composition. Joint Bone Spine. 2011;78(6):611–615. doi: 10.1016/j.jbspin.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 31.Stephenson FA, Rogol AD. Oxytocin: Anti-insulin-like effects in isolated fat cells. Arch Biochem Biophys. 1984;234(1):230–234. doi: 10.1016/0003-9861(84)90344-8. [DOI] [PubMed] [Google Scholar]
- 32.Ahmed ML, Ong KK, Watts AP, Morrell DJ, Preece MA, Dunger DB. Elevated leptin levels are associated with excess gains in fat mass in girls, but not boys, with type 1 diabetes: longitudinal study during adolescence. J Clin Endocrinol Metab. 2001;86(3):1188–1193. doi: 10.1210/jcem.86.3.7320. [DOI] [PubMed] [Google Scholar]
- 33.Stock S, Karlsson R, von Schoultz B. Serum profiles of oxytocin during oral contraceptive treatment. Gynecol Endocrinol. 1994;8(2):121–126. doi: 10.3109/09513599409058033. [DOI] [PubMed] [Google Scholar]
- 34.Silber M, Almkvist O, Larsson B, Stock S, Uvnas-Moberg K. The effect of oral contraceptive pills on levels of oxytocin in plasma and on cognitive functions. Contraception. 1987;36(6):641–650. doi: 10.1016/0010-7824(87)90037-0. [DOI] [PubMed] [Google Scholar]
- 35.Elabd C, Basillais A, Beaupied H, Breuil V, Wagner N, Scheideler M, Zaragosi LE, Massiera F, Lemichez E, Trajanoski Z, Carle G, Euller-Ziegler L, Ailhaud G, Benhamou CL, Dani C, Amri EZ. Oxytocin controls differentiation of human mesenchymal stem cells and reverses osteoporosis. Stem Cells. 2008;26(9):2399–2407. doi: 10.1634/stemcells.208-0127. [DOI] [PubMed] [Google Scholar]
- 36.Tamma R, Colaianni G, Zhu LL, DiBenedetto A, Greco G, Montemurro G, Patano N, Strippoli M, Vergari R, Mancini L, Colucci S, Grano M, Faccio R, Liu X, Li J, Usmani S, Bachar M, Bab I, Nishimori K, Young LJ, Buettner C, Iqbal J, Sun L, Zaidi M, Zallone A. Oxytocin is an anabolic bone hormone. Proc Natl Acad Sci U S A. 2009;106(17):7149–7154. doi: 10.1073/pnas.0901890106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ho JM, Blevins JE. Coming full circle: contributions of central and peripheral oxytocin actions to energy balance. Endocrinology. 2013;154(2):589–596. doi: 10.1210/en.2012-1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mennella JA, Pepino MY, Teff KL. Acute alcohol consumption disrupts the hormonal milieu of lactating women. J Clin Endocrinol Metab. 2005;90(4):1979. doi: 10.1210/jc.2004-1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dicker SE. Release of vasopressin and oxytocin from isolated pituitary glands of adult and new-born rats. J Physiol. 1966;185(2):429–444. doi: 10.1113/jphysiol.1966.sp007994. [DOI] [PMC free article] [PubMed] [Google Scholar]