Abstract
Women aged 15–24 years have an HIV infection rate twice that of men the same age. This study examined reasons why HIV-infected women taking antiretroviral therapy (ART) report missing HIV medications. Women (N= 206) on ART were 2.2 times more likely to endorse reasons pertaining to forgetfulness versus reasons pertaining to problems taking pills (OR= 2.2, 95% CI: 1.63, 2.94, p<0.001). There was a difference between the adherent and non-adherent groups in types of reasons overall, (p<. 001, 95%CI −3.82, −2.03). Using a patient-centered approach to understand type of nonadherence (intentional vs. unintentional) may support development of novel interventions.
Across the world, an estimated 2.2 million persons were infected with HIV in 2011. Of these, 1.2 million were women and girls and those aged 15–24 years have an infection rate twice that of men the same age (UNAIDS, 2012). In 2009, nearly twenty-five percent of newly diagnosed cases of HIV in the United States were women, and most of those infected were minorities and of low socioeconomic status (Centers for Disease Control and Prevention, 2011). Women living with HIV and AIDS (WLHA) taking antiretroviral therapy (ART) are more likely to have lower rates of medication adherence when compared to men (Arnsten, et al., 2002; Lopez, Jones, Villar-Loubet, Arheart & Weiss, 2010; McNabb et al., 2001). Consequently, adherence to ART remains a critical concern in this population. HIV medication adherence literature often reports ‘forgetting’ as one of the most common reasons why people miss their HIV medications (Chesney, 2003; Gay et al, 2011; Heckman, Catz, Heckman, Miller & Kalichman, 2004; Kyser et al., 2011; Sullivan, Campsmith, Nakamura, Begley, Schulden & Nakashima, 2007), yet this understanding has done little to inform effective interventions. Decades of research has identified and described predictors of nonadherence and strategies for people to reach optimal adherence levels, but adherence continues to be a challenge for most people living with HIV and AIDS (PLWHA).
One problem with current strategies to understand and improve adherence is the failure to address adequately the multidimensional nature of nonadherence. Adherence is a result of a set of conscious and subconscious decisions and triggers, and nonadherence can be intentional or unintentional. Gaining an understanding and appreciation of the reasons women forget to take their ART and otherwise do not adhere to their prescribed regimens may inform improved strategies for WLHA’s medication adherence. To improve adherence, providers caring for WLHA need novel evidence-based strategies that can accommodate the unique experience of the context of women’s lives, including condition specific factors (i.e., physical and social environments, family/individual characteristics, knowledge beliefs, social facilitation). Wilson (2010) highlights that approaches such as patient-centered, adult learning theory and motivational interviewing have been growing in the management of adherence in PLWHA. Others emphasize the need for enhanced communication strategies, individualized solutions, and patient-centered approaches to improve ART adherence management (Rochon et al., 2011; Saberi, Comfort, & Johnson, 2012; Saha, Beach, & Cooper, 2008; Wilson, 2010). Patient satisfaction, adherence and positive health outcomes have all been linked to patient-centered communication (Stewart, 1995).
There are limited studies describing the reasons why women in particular, miss taking their medications. The purpose of this study was to examine and gain an appreciation of the reasons why WLHA in Northeast, OH and the San Francisco Bay Area of California report missing their HIV medications, and how the results can influence a new trajectory of patient-centered HIV adherence research. The researchers conducted this secondary analysis investigation to support the international and interdisciplinary HIV community. The range of persons working with, engaging with and interacting with people living with HIV/AIDS is vast. The importance of women, HIV and nonadherence internationally has a significant impact into not only the lives of women but also their family and community. HIV continues to infect and affect women worldwide; gaining a clearer understanding of the dynamic and individual nature of nonadherence in women has the potential to improve the lives of women globally.
Self-Management Framework
Women living with HIV are often managing several co-occurring chronic conditions and balancing multiple social and family roles. Self-management behaviors improve health outcomes, but not all researchers, academics, and providers agree on the components and how best to incorporate them in order to improve health. Ryan & Sawin (2009) present a mid-range theory to organize the similar and divergent ideas. They propose that self-management is a complex dynamic phenomenon consisting of three dimensions: context, process and outcomes. The context dimension consists of condition-specific factors, physical and social environments, and individual and family characteristics. The concepts of the process dimension are based in health behavior theories, research and practice. The concepts include: knowledge and beliefs, self-regulation, skills and abilities, and social facilitation. The outcomes dimension is inclusive of proximal and distal outcomes. The proximal outcomes are self-management behaviors and cost of health care services, while distal are health status, quality of life and cost of health. Incorporating the many factors affecting adherence into a self-management framework can provide a lens to view the dynamic nature of adherence. Integration of the dimensions supported our study analysis. A self-management framework can provide the flexibility that will allow for the adaptation to individuals with common and unique barriers to adherence.
Literature on Reasons for Nonadherence
In 1992 Samet and colleagues first documented ‘simply forgetting’ as the main reason PLWHA taking monotherapy missed their HIV medications, and forgetting has consistently been documented in the top five reasons for nonadherence ever since (Barfod, Sorensen, Nielsen, Rodkjaer, & Obel, 2006; Gay et al., 2011; Heckman, Catz, Heckman, Miller & Kalichman, 2004; Hill, Kendall, & Fernandez, 2003; Kalichman, Catz & Ramachandran, 1999; Sullivan, Campsmith, Nakamura, Begley, Schulden & Nakashima, 2007). Research exploring the reasons for nonadherence and degree of adherence has expanded. Catz et al. (2000) found differences between adherent and non-adherent persons regarding knowledge of regimens, number and appearance of pills, instructions, and benefits of taking medications. Kalichman et al. (2001) explored adherent vs. non-adherent women (missed at least one dose in the past week) and compared the groups on HIV treatment knowledge, intentions to adhere, and self-efficacy for HIV treatment adherence. Non-adherent women demonstrated less intention to adhere to medication and less HIV treatment self-efficacy than those who were classified as adherent. Interestingly, improvements in adherence in women did not result from the implementation of “reminder” adherence enhancement strategies such as timers, beepers, pillboxes, and reminder notes. Barfod, Sorensen, Nielsen, Rodkjaier & Obel (2006) examined patients’ self-reported reasons for missing doses of ART in 840 Danish adults (79% male) living with HIV. They compared reasons between those participants classified as low adherers (missing a dose within the preceding four days) and high adherers. “Simply forgot” was the most frequently stated reason, regardless of degree of adherence. Ferguson et al. (2002) examined 25 reasons for nonadherence and found that women were more likely to report forgetting to refill medications than men, and lacked understanding of how to take the medications properly. Despite the many efforts to integrate reminder devices and strategies into a PLWHA’s daily routine, forgetting continues to be the most frequently stated reason for nonadherence (Gay et al, 2011; Kyser et al., 2011). Yard, Huh, King and Simoni (2011) examined 34 patient-level characteristics, inclusive of mental health, sociodemographic and interpersonal factors as moderators of two ART adherence interventions (peer support and pager reminders) in 224 men and women and found none of the 34 significantly moderated either intervention. Saberi & Johnson, (2011) conducted a recent systematic review, they examined 36 publications, (a mix of quantitative and qualitative studies) and found a clear pattern favoring individually tailored multi-functional technologies rather than solely electronic reminder devices.
Research specifically focused on women and ART adherence is continuing to grow and expand not only in regard to reasons women are nonadherent, but also in regard to predictors of adherence. Lazo et al. (2007) examined patterns and predictors of changes in adherence to ART over a 5-year period. Among the factors associated with decreasing adherence in women was a history of an AIDS diagnosis and a protease inhibitor (PI) based regimen. Amico (2007) recruited 72 PLWHA from Mississippi and found different adherence patterns among women and individuals with moderate to severe depression. Feeling sick and wanting to take a break from the medications were common reasons cited in both groups. Although participants cited multiple reasons for nonadherence, the researchers found that adherence was not correlated with total number of reasons for missed medications. Vyavaharkar et al. (2007) demonstrated in a cohort of 224 women with depression, denial/avoidance coping and increased numbers of children were positive predictors of reporting more reasons for missed medications.
Intentional and Unintentional Adherence
Roberts and Mann (2003) explored the idea of intentional versus unintentional nonadherence. Intentional nonadherence refers to the deliberate aim not to take medications, and it occurs when patients who are knowledgeable about the medications choose not to adhere. To study this, they recruited 20 women between the ages of 25 and 54 living with HIV in the US, and collected women’s own perceptions in diary format to better understand why these women intentionally fail to adhere to their ART. The researchers provided insight into the world of intentional nonadherence and the results underscore the need for routine provider-patient adherence communication due to the emotional and social ramifications intentional nonadherence has for women. Roberts and Mann (2003) call attention to the fact that if interventions are to improve adherence, they must address both intentional and unintentional nonadherence. Both intentional and unintentional nonadherence has been studied in patients with chronic illness including: asthma, lupus, hypertension, and breast cancer (Atkins & Fallowfield, 2006; Daleboudt, Broadbent, McQueen & Kaptein, 2010; Lehane & McCarthey, 2007; Lowry, Dudley, Oddone & Bosworkth, 2005; Wroe, 2002). This area of study has been limited in PLWHA (Mo & Mak, 2009; Norton et al., 2010; Wroe & Thomas, 2003). Mo and Mak (2009) investigated factors associated with adherence, intentional nonadherence, and unintentional nonadherence among PLWHA in Hong Kong. Their findings that intentional and unintentional nonadherence are separate types of adherence and associated with different factors support the need for a comprehensive measurement of adherence and further study with intentional and unintentional nonadherence.
Gaining a clearer understanding of the type of nonadherence can assist providers in gaining a perspective into a patient’s unique situation, support joint decisions to possibly change patient regimens and/or provide additional resources. Distinguishing between intentional and unintentional nonadherence may assist in categorizing whether the reasons fall into a certain theme, which can be a foundation for developing effective interventions. Wayson Locher, Pargament and Duggan (2007) conducted seven qualitative interviews with HIV positive women of color on the lived experience of ART. Three themes emerged: trust and mistrust (of medicines, clinicians, friends); motivation of approach/avoidance; and feeling constantly tethered. They discuss this concept of ‘constantly tethered’ as derived from having to take pills every day, fear of forgetting, needing to create new routines and the constant reminder of HIV that having to take the medication created. Not all health care providers and adherence supporters are able to interview their patients in order to break through to a theme, but Wayson Locher, Pargaement and Duggan (2007) draw attention to the fact that the repeated findings of forgetting or sleeping through a dose may possibly be a manifestation of rebellion or denial against a life tethered to ART. Forgetting, being away from home, being busy, and sleeping through doses are uncomplicated answers that fail to explain the underlying reasons for missing medications.
The literature provides a lens highlighting the need to be mindful of synthesizing adherence literature, incorporating lessons learned, and understanding the needs of individual patients. Placing patients into a subgroup or box of nonadherence predictors can potentially disengage and seemingly ignore the individual. Identifying a common profile is a starting point, and then gaining an appreciation for the individuals’ needs and barriers can support adherence in people taking ART. This evidence suggests a need for new adherence strategies that are more dynamic and can easily respond to an individual’s unique situation. The type of ART regimen, treatment for other non-AIDS defining complications, and other contextual factors play a vital role in understanding how adherence is integrated into an individual’s life.
Methods
Participants and Procedure
A cross-sectional, descriptive study was conducted from October 2010 through March 2011 in Cleveland, Ohio, and in San Francisco and Oakland, California. Biologically female, English-speaking women aged 18 years or older with confirmed HIV-diagnosis, who were able to provide informed consent and self administer the questionnaire packet were eligible for the study. Participants were recruited via flyers posted at medical clinics and community support organizations. Case Western Reserve University (CWRU) and the University of California San Francisco (UCSF) Institutional Review Boards approved the study protocol. All participants provided written informed consent. The questionnaire packet took participants 45–60 minutes to complete; participants were paid for their participation. The main study aim was to develop and validate a measure of self-management for women living with HIV and AIDS (Webel et al., 2012). This secondary analysis on HIV adherence focused on reasons for missing ART.
Measures
Demographic, clinical characteristics and instruments
The self-administered questionnaire included demographic and clinical background items. Basic demographics included age, race, children, marital status, education level, annual income, housing, and insurance. Self-reported medical information included year diagnosed with HIV, antiretroviral status, HIV medications, AIDS diagnosis, viral load, CD4+ T-cell count and co-morbidities. Chart abstraction was completed at the Ohio clinic sites for viral load, CD4+ T cell count and year diagnosed with HIV. The scales and instruments gathered information on pregnancy history, access to care, social capital, chronic disease self-efficacy, health care provider engagement, self-management, quality of life and stigma. Adherence was measured using a visual analog self-report adherence scale, and the AIDS Clinical Trials Group Revised (ACTGrev) reasons for missed medications was used to assess reasons for nonadherence.
Reasons, Adherence Level and Regimen
The ACTGrev Reasons for Missing Medications revised instrument (Holzemer et al., 2006) was used to capture reasons for missed medication in the past month. This nine-item, self-report measure uses a four-point Likert ordinal scale that allows participants to respond on the frequency of missing their medications (never, rarely, sometimes or often). The first five items cluster into one factor “problems taking pills” and include: (1) wanted to avoid side effects, (2) felt sick or ill, (3) too many pills to take, (4) felt depressed/overwhelmed and (5) problems taking pills at specified times. The other four items cluster into the second factor “forgetfulness” and include: (1) too busy with other things, (2) away from home, (3) simply forgot, and (4) fell asleep/slept through the dose. The Cronbach’s α reliability coefficient for this study was 0.93, and in previous studies it has ranged from .85 to .89 (Gay et al., 2011, Holzemer et al., 2006).
Self-reported adherence was measured on a visual analogue scale based on one’s adherence level over three days. The scale is based on Walsh, Mandalia, & Gazzard’s (2002) 30-day adherence assessment. Participants marked their level of adherence with an ‘X’ on the line indicating zero to 100 percent in the last three days. If a participant indicated an ‘X’ at 100% they were defined as adherent. Nonadherence was defined as anything less than 100% adherence. Over-reporting of adherence is a concern with self-reported measures, which is why the authors choose a conservative cut off of anything less than 100% as non-adherent. Participants indicated from a chart listing 32 FDA approved HIV medications which ones they were currently taking. Regimen data was categorized into a protease inhibitor (PI) based regimen and a non-PI based regimen.
Analysis
We calculated descriptive statistics to summarize demographic and clinical characteristics; and performed chi-square and t-tests to determine differences between the adherence level (adherent vs. non-adherent) groups and regimen (PI based vs. non-PI based) groups. The data from the ACTGrev instrument was dichotomized into persons who reported never missing their medication for that reason and those who ever missed (included rarely, sometimes, and often) for that reason. A ranking was calculated on the percent of persons documenting ever missing their medication for each of the nine reasons, by adherence level and regimen. Additionally, chi-square tests were performed for each reason by adherence level and regimen. Rankings and chi-square testing were also completed with the following subgroups: (1) PI and adherence level, and (2) Non-PI and adherence level. We also conducted multi-level regression analysis to determine the overall difference between adherence level groups in reasons given and between regimen groups. An overall main effect with grouping reasons into the factors (Problems Taking Pills and Forgetfulness) and an interaction between regimen group and factors (Problems Taking Pills and Forgetfulness) was analyzed. We conducted our analysis with STATA version 11.0 (Stata corporation, College Station, TX).
Results
Participants
The sample included 266 women, 131 women from the Cleveland site and 135 from the San Francisco Bay Area site. The mean age for all participants was 46 (SD: 9.3, range 22–71). Our analysis focused on the 206 (77%) women on ART (mean age of 47 years [SD: 9.2]) (see Table 1). Thirty percent of these women had less than a high school education, 64% were African American, 59% single, 88% had children, 22% were working, 46% reported receiving an AIDS diagnosis and there was a mean self-reported adherence level of 87%. Fifty-six percent (n=115) documented 100% adherence in the last three days and 48% of the women in the sample (n=99) were taking a PI regimen. The median CD4+ T cell counts for the adherent and non-adherent groups were 515 cells/mm3 (IQR: 266–798) and 487 cells/mm3 (244–714), respectively. Viral load (VL) was available for 66% of the sample and both the non-adherent group and PI based regimen group had a greater percentage of women with detectable viral loads. The women on a PI regimen had lower CD4+ T cell counts, more detectable viral loads, and a greater percentage of ever having an AIDS diagnosis. Chi-square tests revealed statistically significant results between: African American race and PI versus non-PI regimen (p=. 001), and self- reported adherence versus PI and non-PI regimen (p=. 010) (not documented in Table 1).
Table 1.
Demographic and clinical characteristics: Overall and by Adherence level and Regimen
| Characteristics | Sample | Adherent 100% in past 3 days |
Nonadherent Less than 100% in past 3 days |
PI based regimen | Non-PI based regimen |
|---|---|---|---|---|---|
| n=206 | n=115 | n=91 | n=99 | n=107 | |
| n (%) | n (%) | n (%) | n (%) | n (%) | |
|
| |||||
| Age in years: Mean (SD) | 47 (9.2) | 47 (9.9) | 46 (8.3) | 47 (8.8) | 47 (9.7) |
|
| |||||
| Race | |||||
| AA | 129 (64) | 70 (63) | 59 (67) | 50 (53) | 79 (75) |
| Hispanic | 17 (9) | 9 (8) | 8 (9) | 13 (14) | 4 (4) |
| White | 38 (19) | 24 (21) | 14 (16) | 22 (23) | 16 (15) |
| Other | 16 (8) | 9 (8) | 7 (8) | 10 (10) | 6 (6) |
|
| |||||
| Education | |||||
| 11 grade or less | 59 (30) | 32 (29) | 27 (30) | 29 (31) | 30 (29) |
| High School Diploma or General Education | 83 (42) | 42 (38) | 41 (46) | 38 (40) | 45 (43) |
| Degree | |||||
| 2 years college | 42 (21) | 26 (23) | 16 (18) | 22 (23) | 20 (19) |
| 4 yrs/MS/PhD | 15 (7) | 11 (10) | 5 (6) | 6 (6) | 10 (9) |
|
| |||||
| Marital status | |||||
| Married | 25 (13) | 16 (15) | 9 (10) | 14 (15) | 11 (11) |
| Single | 118 (59) | 59 (54) | 59 (66) | 59 (61) | 59 (57) |
| Separated/divorced | 38 (19) | 23 (21) | 15 (17) | 16 (17) | 22 (21) |
| Other | 18 (9) | 12 (10) | 6 (7) | 7 (7) | 11 (11) |
|
| |||||
| Have children1 | 147 (88) | 84 (88) | 63 (89) | 73 (89) | 74 (87) |
|
| |||||
| Currently employed | 44 (22) | 26 (23) | 18 (20) | 19 (19) | 25 (24) |
|
| |||||
| Permanent housing | 170 (84) | 96 (85) | 74 (82) | 79 (80) | 91 (88) |
|
| |||||
| HIV medication adherence in past 3 days: Mean (SD) | 87 (22.71) | 100 (0) | 71(26.5) | 83 (26.5) | 91(17.7) |
|
| |||||
| CD4+ T cell count2: cell/mm3 Median (IQR) | 500 (250–772) | 515 (266–798) | 487 (244–714) | 430 (233–700) | 585 (297–839) |
|
| |||||
| Detectable HIV Viral Load3 (> 75 copies/mL) | 38 (26) | 18 (24) | 20 (33) | 22 (33) | 16 (23) |
|
| |||||
| Ever told had AIDS | 92 (46) | 46 (41) | 46 (52) | 52 (53) | 40 (40) |
78–81% of sample responded
73–85% of sample responded
66–67% of sample responded
Reasons for Missed Medications
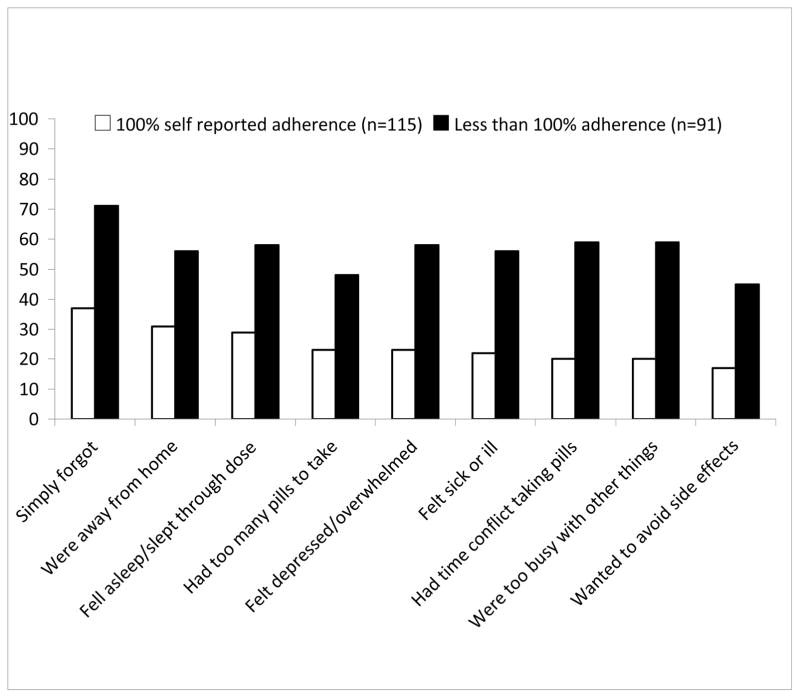
‘Simply forgot’ was the dominant reason for missing medications in both the adherent and non-adherent groups in this sample. ‘Away from home’ and ‘fell asleep’ were the second and third most frequent reasons for missed medications in the adherent group, and ‘problems taking pills at a specified time’ and ‘too busy with other things’ ranked second and third in the non-adherent group. ‘Wanted to avoid side effects’ was the least frequent reason reported for missed medication in both groups. For each reason, a statistically significant difference among the frequency reporting was found between the adherent and non-adherent groups (Figure 1). Additionally, among those in the adherent group, 9% reported all nine reasons for ever missing a medication compared to 25% of the non-adherent group who listed all nine.
Figure 1.
Reasons for missed medications in the last month according to self reported adherence in the last 3 days (n=206)
χ2 test of significance between those with 100% adherence and those with less than 100% adherence had a p-value = 0.001
Using multi-level logistic regression analysis, we found a difference between the reasons-related factors, (Problems Taking Pills vs. Forgetfulness); women were 2.2 times more likely to document the reasons falling under the Forgetfulness factor than the reasons falling under the Problems Taking Pills factor (OR= 2.2, 95% CI: 1.63, 2.94, p<0.001). There was also a difference between the adherent and non-adherent groups in reasons for missed medications given overall, (p<.0001, 95%CI −3.82, −2.03), but we did not find a difference between those on a PI based versus a non-PI based regimen across all reasons given for missed medication overall (p=.35, 95%CI −0.492, 1.389). When testing for an interaction between regimen group (PI vs. non-PI) and factors (Problems Taking Pills AND Forgetfulness), we did not find a statistically significant difference (OR= 1.71, 95% CI: 0.624, 4.68, p=0.296).
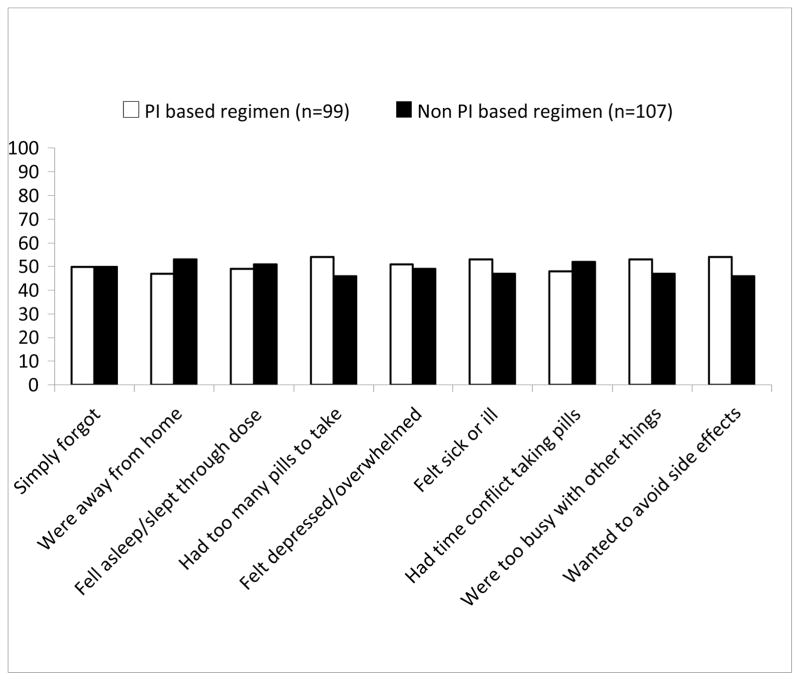
In comparing reasons for missed medication by ART regimen (PI vs. non-PI), the top four reasons for having missed medication in the PI and non-PI groups differed. Among those in the PI group, ‘wanted to avoid side effects’, ‘too many pills to take’, ‘too busy with other things’ and ‘felt sick’ were the four most frequent reasons, (three of these fall into the Problems Taking Pills factor). For those in the non-PI group, the most frequent reasons given for missing medications included ‘being away from home’, ‘problems taking pills at specified times’, ‘fell asleep’ and ‘forgot’, (three of these fall into the Forgetfulness factor). We did not find a significant difference between the reasons given between the two regimen groups (See Figure 2).
Figure 2.
Reasons for missed medication in the last month according to regimen (n=206)
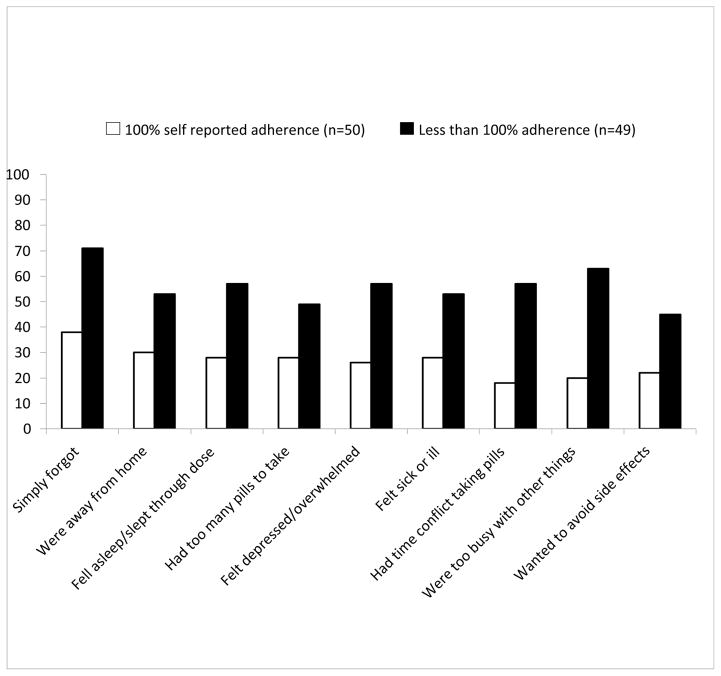
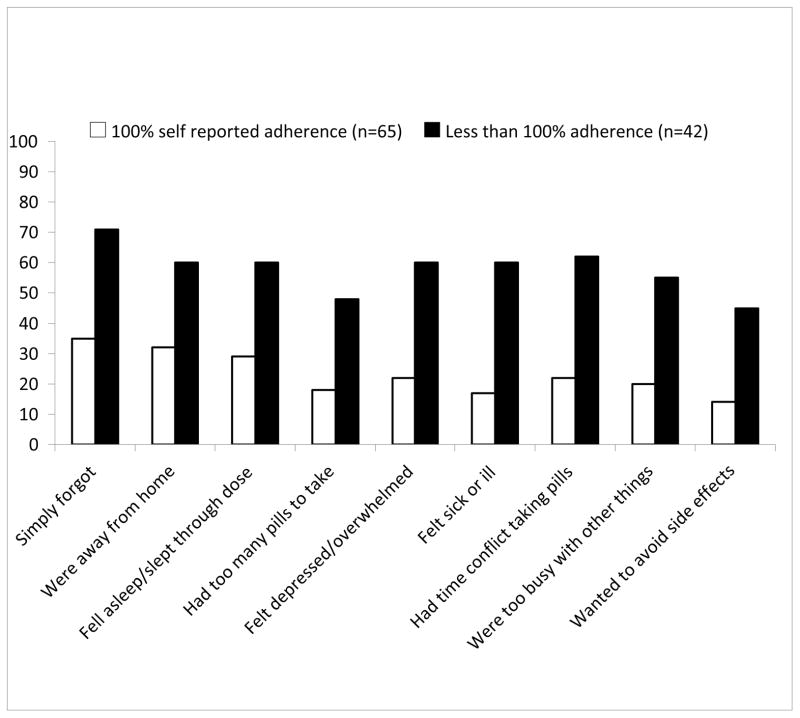
In sub group analyses, ‘simply forgot’ was the top ranked reason for not taking medications in the PI based regimen (n=99) among the adherers (n=50) and nonadherers (n=49). The top three reasons reported by both the adherers and nonadherers fell in the Forgetfulness factor. For those participants in the non-PI based group (n=107), the adherers (n=65) and nonadherers (n=42) had the same top five reasons for missing medication, with the most common being ‘simply forgot’ and the last ranked being ‘wanted to avoid side effects’. Refer to Figure 3 and 4.
Figure 3.
Reasons for missed medications in the last month according to self reported adherence in the last three days for those taking a PI based regimen (n=99)
Figure 4.
Reasons for missed medictions in the last month according to self reported adherence in the last 3 days for those taking a Non PI regimen (n=107)
Discussion
In this sample with substantial representation of single, African American women with children, the mean adherence level was 87%, and participants were 2.2 times more likely to document reasons pertaining to forgetfulness than problems taking pills. Fifty-six percent of the women in the sample self-reported 100% HIV medication adherence in the past three days. Researchers have consistently demonstrated that forgetfulness is the leading reason people cite for nonadherence (Gay et al., 2011; Kyser et al., 2011). The researchers of this study also found this in our all-female sample. However, it is important to note that an overall difference was found in the type of reasons given between the adherent group (56% of the sample) and the non-adherent group. In 2006, Barfod and colleagues hypothesized that reasons for missed medications are different between adherers and nonadherers, and that forgetfulness is not as prominent in nonadherers, and may explain why reminder devices are not as effective for those who are nonadherers (Mannhiemer et al., 2006). And although simply forgetting was reported as the number one ranked reason irrespective of adherence level by both Barfod and colleagues and participants in our study, we also found that the overall reasons for missed medications between adherers and nonadherers differed as did the frequency of reasons between these two groups. This evidence suggests that it is not just about simply forgetting, but highlights the importance of appreciating the reasons for nonadherence. Nonadherence is complex. Reasons for nonadherence are at times based on conscious decision-making (intentional nonadherence) and at other times based on situation or the subconscious (unintentional nonadherence). Understanding the complex nature of nonadherence, and appreciating the multifaceted nature of this phenomenon can improve interventions promoting adherence.
The research we carried out provides insight that nonadherers may have a complex profile that requires a careful, individualized assessment. The evidence suggests that the type of reason can impact adherence level. For providers discussing adherence with patients, a patient-centered approach that reviews type of reason, frequency of reasons and type of nonadherence (intentional vs. unintentional), as well as contextual factors surrounding the nonadherent behavior, may help elicit an individualized profile of nonadherence. As researchers and clinicians highlight the need for enhanced communication strategies, individualized solutions and patient-centered approaches to improve ART adherence management, (Rochon et al., 2011; Saberi, Comfort, & Johnson, 2012; Saha, Beach, & Cooper, 2008; Wilson, 2010) appreciating and acknowledging individuals’ nuanced reasons for missed medication can support these strategies, solutions and approaches for optimal medication adherence. As women continue to struggle with managing not only HIV/AIDS but additional chronic diseases, (Phillips, Neaton, & Lundgren 2008), family and other competing priorities, the importance of appreciating the reasons for nonadherence can assist in overcoming barriers to ART adherence.
Women in our sample taking a PI based regimen reported reasons falling under the Problems Taking Pills factor more often than those on a non-PI based regimen. Okonsky, (2011) also described the reasons for missed medication among 416 PLWHA taking ART using the ACTGrev instrument. In her study with 44% of PLWHA on a PI based regimen, (29% female), the Problems Taking Pills factor was associated with a PI regimen and the Forgetfulness factor was not. Additionally, PI based regimens have not only been shown to have a lower adherence but also decreases in adherence have been documented over time (Lazo et al., 2007, Mannheimer, Friedland, Matts, Child, & Chesney, 2002). In our study, we documented women on a PI based regimen had a mean adherence level of 79% compared to 91% for women on a non-PI based regimen. Walsh, Horne, Dalton, Burgess & Gazzard (2001) defined common reasons and frequency of reasons for non-adherent persons taking a PI based regimen. Those with lower adherence gave more reasons. Our study had similar findings: those grouped as non-adherent had a greater number of reasons documented (25 % vs. 9%). Twenty-five percent (23/91) of the sample in the non-adherent group listed all nine reasons for missing medication, while only 9% (10/115) in the adherent group listed all nine. Interestingly, Walsh et al., (2001) conducted a factor analysis of reasons and found that ‘low priority for medication’ and ‘unintentional nonadherence’ was independently associated with nonadherence. Continuing to explore and understand the type of nonadherence can illuminate the complexities in a patients’ unique situation that may have otherwise been concealed. Using a self-management framework is important in understanding one’s intentions and can support further exploration in adherence studies of women. Allowing for individuals’ own story regarding intentions may be a tipping point for nonadherence research. A dynamic patient-centered approach can facilitate an appreciation of the reasons for nonadherence in PLWHA.
The nature of this cross sectional study with self-reported data only allowed for a snapshot of what was happening at that specific time. However, adherence is a dynamic issue. Dichotomizing the data for ease of analysis can weaken the results. The ACTGrev was limited to nine reasons. Although the nine reasons listed are commonly cited in both qualitative and quantitative studies, there was no option for other, suggesting to participants to document only the reasons presented. Nonetheless, the ACTGrev is a quick translatable starting point for a patient-centered approach to assess the need for further adherence discussions. Demographics and clinical characteristics presented a profile of the women in this study, but we did not provide the patient’s regimen history, and other patient related factors such as substance abuse, depression, and social support that have been associated with adherence. Nevertheless, our findings contribute to a growing body of female-centered adherence research on the role of competing interests and their impact on adherence.
The implications our study has on practice, future research and policy are fundamental to the HIV community globally. Highlighting the need for appreciating the dynamic nature of adherence and types of nonadherence for women is a critical shift in adherence intervention development. The patient-centered approach and discussion specific to reasons for nonadherence in clinical practice can be viewed through a self-management lens and future research can focus not only the varied circumstances women are living in but also the varied environments. Moreover, the work of the researchers can help inform HIV policy guidelines through a growing body of literature on women and HIV nonadherence.
Conclusion
Forgetting has dominated the adherence literature as the leading reason people are not taking their medicines; and even with the influence of reminder devices and strategies, forgetting remains as the top reason. Not all PLWHA taking ART will be able to enroll in an experimental intervention or keep weekly or monthly appointments to complete an adherence intervention; and certain intervention strategies will not work for everyone due to the complex nature of adherence and the individual. As a community of providers, counselors, advocates, and social workers working with PLWHA, we need to meet our patients where they are and realize that their life circumstances change quickly. Our research findings parallel other studies in that forgetfulness is still the most common reason for nonadherence. The evidence suggests that ‘forgetting’ is an easy answer to a more complex problem not entirely addressed by a 9-item instrument. Forgetting, being away from home, being busy, and sleeping through doses are uncomplicated answers that may fail to explain the underlying reasons for missing medications. Our study discussion emphasizes the need to focus on patients’ unique situation in order to gain an appreciation for the type of nonadherence they are experiencing. It is vital that we are not complacent when patients say, “I simply forgot” but be proactive and support patients to discuss what forgetting actually means. Incorporating a self-management framework and moving toward integrating a patient-centered approach while appreciating the intentional and unintentional nonadherence a person is experiencing can influence a new body of literature that may spur new and innovative interventions that can support one owns unique situation and improve adherence.
Acknowledgments
The study team would like to thank the participants, Cleveland HIV clinic, Ward 86, UCSF Women’s HIV Program and WORLD.
Funding
This research was funded by grants from the National Institutes of Health (5KL2RR024990, 1UL1 RR024989, TL1 RR024129, T32NR007081 & P30 NR010676) in the United States.
Contributor Information
Jennifer G. Okonsky, Department of Community Health Systems, School of Nursing, University of California San Francisco, San Francisco, California, USA
Allison Webel, Bolten School of Nursing, Case Western Reserve University, Cleveland, Ohio, USA.
Carol Dawson Rose, Department of Community Health Systems, School of Nursing, University of California San Francisco, San Francisco, California, USA.
Mallory Johnson, Center for AIDS Prevention Studies, School of Medicine, University of California San Francisco, San Francisco, California, USA.
Alice Asher, School of Nursing, University of California San Francisco, San Francisco, California, USA.
Yvette Cuca, Department of Community Health Systems, School of Nursing, University of California San Francisco, San Francisco, California, USA.
Alphoncina Kaihura, School of Nursing, University of California San Francisco, San Francisco, California, USA.
Jan E. Hanson, Departments of Anthropology and Public Health, Case Western Reserve University, Cleveland, Ohio, USA
Carmen J. Portillo, Department of Community Health Systems, School of Nursing, University of California San Francisco, San Francisco, California, USA
References
- Amico KR, Konkle-Parker DJ, Cornman DH, Barta WD, Ferrer R, Norton WE, et al. Reasons for ART nonadherence in the Deep South: adherence needs of a sample of HIV-positive patients in Mississippi. AIDS Care. 2007;19:1210–1218. doi: 10.1080/09540120701426516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. Journal of General Internal Medicine. 2002;17:377–381. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins L, Fallowfield L. Intentional and non-intentional nonadherence to medication amongst breast cancer patients. European Journal of Cancer. 2006;42:2271–2276. doi: 10.1016/j.ejca.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Balint E. The possibilities of patient-centered medicine. Journal of the Royal College of General Practitioners. 1969;17:269–276. [PMC free article] [PubMed] [Google Scholar]
- Barfod TS, Sorensen HT, Nielsen H, Rodkjaer L, Obel N. ‘Simply forgot’ is the most frequently stated reason for missed doses of HAART irrespective of degree of adherence. HIV Medicine. 2006;7:285–290. doi: 10.1111/j.1468-1293.2006.00387.x. [DOI] [PubMed] [Google Scholar]
- Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychology. 2000;19:124–133. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Women and Girls Awareness Day. Retrieved September 10, 2011 from http://www.cdc.gov/features/womengirlshivaids/
- Daleboudt GM, Broadbent E, McQueen F, Kaptein AA. Intentional and unintentional treatment nonadherence in patients with systemic lupus erythematosus. Arthritis Care Research (Hoboken) 2010 doi: 10.1002/acr.20411. [DOI] [PubMed] [Google Scholar]
- Ferguson TF, Stewart KE, Funkhouser E, Tolson J, Westfall AO, Saag MS. Patient-perceived barriers to antiretroviral adherence: Associations with race. AIDS Care. 2002;14:607–617. doi: 10.1080/0954012021000005434. [DOI] [PubMed] [Google Scholar]
- Gay C, Portillo CJ, Kelly R, Coggins T, Davis H, Aouizerat BE, Lee K. Self-reported medication adherence and symptom experience in adults with HIV. Journal of the Association of Nurses in AIDS Care. 2011;22:257–268. doi: 10.1016/j.jana.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman BD, Catz SL, Heckman TG, Miller JG, Kalichman SC. Adherence to antiretroviral therapy in rural persons living with HIV disease in the United States. AIDS Care. 2004;16:219–230. doi: 10.1080/09540120410001641066. [DOI] [PubMed] [Google Scholar]
- Hill Z, Kendall C, Fernandez M. Patterns of adherence to antiretrovirals: why adherence has no simple measure. AIDS Patient Care STDS. 2003;17:519–525. doi: 10.1089/108729103322494311. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Bakken S, Portillo CJ, Grimes R, Welch J, Wantland D, et al. Testing a nurse-tailored HIV medication adherence intervention. Nursing Research. 2006;55:189–197. doi: 10.1097/00006199-200605000-00005. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Catz S, Ramachandran B. Barriers to HIV/AIDS treatment and treatment adherence among African-American adults with disadvantaged education. Journal National Medical Association. 1999;91:439–446. [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, DiFonzo K, Simpson D, Austin J, Luke W, et al. HIV treatment adherence in women living with HIV/AIDS: research based on the Information-Motivation-Behavioral Skills model of health behavior. Journal of Association of Nurses in AIDS Care. 2001;12:58–67. doi: 10.1016/S1055-3290(06)60217-3. [DOI] [PubMed] [Google Scholar]
- Kyser M, Buchacz K, Bush TJ, Conley LJ, Hammer J, Henry K, Brooks JT. Factors associated with nonadherence to antiretroviral therapy in the SUN study. AIDS Care. 2011;23:601–611. doi: 10.1080/09540121.2010.525603. [DOI] [PubMed] [Google Scholar]
- Laws MB, Epstein L, Lee Y, Rogers W, Beach MC, Wilson IB. The association of visit length and measures of patient-centered communication in HIV care: A mixed methods study. Patient Education and Counseling. 2011 doi: 10.1016/j.pec.2011.04.013. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazo M, Gange SJ, Wilson TE, Anastos K, Ostrow DG, Witt MD, Jacboson LP. Patterns and predictors of changes in adherence to highly active antiretroviral therapy: longitudinal study of men and women. Clinical Infectious Diseases. 2007;45:1377–1385. doi: 10.1086/522762. [DOI] [PubMed] [Google Scholar]
- Lehane E, McCarthy G. An examination of the intentional and unintentional aspects of medication nonadherence in patients diagnosed with hypertension. Journal of Clinical Nursing. 2007;16:698–706. doi: 10.1111/j.1365-2702.2005.01538.x. [DOI] [PubMed] [Google Scholar]
- Lopez EJ, Jones DL, Villar-Loubet OM, Arheart KL, Weiss SM. Violence, coping, and consistent medication adherence in HIV-positive couples. AIDS Education and Prevention. 2010;22:61–68. doi: 10.1521/aeap.2010.22.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry KP, Dudley TK, Oddone EZ, Bosworth HB. Intentional and unintentional nonadherence to antihypertensive medication. Annals of Pharmacotherapy. 2005;39:1198–1203. doi: 10.1345/aph.1E594. [DOI] [PubMed] [Google Scholar]
- Mannheimer S, Friedland G, Matts J, Child C, Chesney M. The consistency of adherence to antiretroviral therapy predicts biologic outcomes for human immunodeficiency virus-infected persons in clinical trials. Clinical Infectious Diseases. 2002;34:1115–1121. doi: 10.1086/339074. [DOI] [PubMed] [Google Scholar]
- Mannheimer SB, Morse E, Matts JP, Andrews L, Child C, Schmetter B, Friedland GH. Sustained benefit from a long-term antiretroviral adherence intervention. Results of a large randomized clinical trial. Journal of Acquired Immune Deficiency Syndrome. 2006;43(Suppl 1):S41–47. doi: 10.1097/01.qai.0000245887.58886.ac. [DOI] [PubMed] [Google Scholar]
- McNabb J, Ross JW, Abriola K, Turley C, Nightingale CH, Nicolau DP. Adherence to highly active antiretroviral therapy predicts virologic outcome at an inner-city human immunodeficiency virus clinic. Clinical Infectious Diseases. 2001;33:700–705. doi: 10.1086/322590. [DOI] [PubMed] [Google Scholar]
- Mo PK, Mak WW. Intentionality of medication nonadherence among individuals living with HIV/AIDS in Hong Kong. AIDS Care. 2009;21:785–795. doi: 10.1080/09540120802511968. [DOI] [PubMed] [Google Scholar]
- Norton WE, Amico KR, Fisher WA, Shuper PA, Ferrer RA, Cornman DH, Fisher JD. Information-motivation-behavioral skills barriers associated with intentional versus unintentional ARV nonadherence behavior among HIV+ patients in clinical care. AIDS Care. 2010;22:979–987. doi: 10.1080/09540121003758630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okonsky JG. Problems taking pills: understanding HIV medication adherence from a new perspective. AIDS Care. 2011 doi: 10.1080/09540121.2011.579944. Epub. [DOI] [PubMed] [Google Scholar]
- Ortego C, Huedo-Medina TB, Llorca J, Sevilla L, Santos P, Rodriguez E, Warren MR, Vejo J. Adherence to Highly Active Antiretroviral Therapy (HAART): A Meta-Analysis. AIDS and Behavior. 2011;15:1381–1396. doi: 10.1007/s10461-011-9942-x. [DOI] [PubMed] [Google Scholar]
- Phillips AN, Neaton J, Lundgren JD. The role of HIV in serious diseases other than AIDS. Aids. 2008;22:2409–2418. doi: 10.1097/QAD.0b013e3283174636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts KJ, Mann T. Adherence to antiretroviral medications in HIV/AIDS care: a narrative exploration of one woman’s foray into intentional nonadherence. Health Care for Women International. 2003;24:552–564. doi: 10.1080/07399330390199537. [DOI] [PubMed] [Google Scholar]
- Rochon D, Ross MW, Looney C, Nepal VP, Price AJ, Giordano TP. Communication strategies to improve HIV treatment adherence. Health Communication. 2011;26:461–467. doi: 10.1080/10410236.2011.554168. [DOI] [PubMed] [Google Scholar]
- Ryan P, Sawin KJ. The Individuval and Family Slef-Management Theory: Background and perspectives on context, process, and outcomes. Nursing Outlook. 2009;57:217–225. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saberi P, Comfort M, Johnson MO. The relationship between daily organization and adherence to antiretroviral therapy: a qualitative perspective. Journal of Acquired Immune Deficiency Syndrome. 2012;61(1):e3–e6. doi: 10.1097/QAI.0b013e318261faf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saberi P, Johnson MO. Technology-based self-care methods of improving antiretroviral adherence: a systematic review. PLoS One. 2011;6(11):e27533. doi: 10.1371/journal.pone.0027533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. Journal of the National Medical Association. 2008;100:1275–1285. doi: 10.1016/s0027-9684(15)31505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JH, Libman H, Steger KA, Dhawan RK, Chen J, Shevitz AH, Craven DE. Compliance with zidovudine therapy in patients infected with human immunodeficiency virus, type 1: a cross-sectional study in a municipal hospital clinic. American Journal of Medicine. 1992;92:495–502. doi: 10.1016/0002-9343(92)90746-x. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Amico KR, Smith L, Nelson K. Antiretroviral adherence interventions: translating research findings to the real world clinic. Curr HIV/AIDS Rep. 7(1):44–51. doi: 10.1007/s11904-009-0037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Campsmith ML, Nakamura GV, Begley EB, Schulden J, Nakashima AK. Patient and regimen characteristics associated with self-reported nonadherence to antiretroviral therapy. PLoS One. 2007;2(6):e552. doi: 10.1371/journal.pone.0000552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/201207_FactSheet_Global_en.pdf.
- Vyavaharkar M, Moneyham L, Tavakoli A, Phillips KD, Murdaugh C, Jackson K, Meding G. Social support, coping, and medication adherence among HIV-positive women with depression living in rural areas of the southeastern United States. AIDS Patient Care STDS. 2007;21(9):667–680. doi: 10.1089/apc.2006.0131. [DOI] [PubMed] [Google Scholar]
- Wayson Locher A, Pargament K, Duggan J. Antiretroviral therapy in the lives of women of colour with HIV. AIDS Care. 2007;19:1048–1051. doi: 10.1080/09540120701335253. [DOI] [PubMed] [Google Scholar]
- Walsh JC, Horne R, Dalton M, Burgess AP, Gazzard BG. Reasons for nonadherence to antiretroviral therapy: patients’ perspectives provide evidence of multiple causes. AIDS Care. 2001;13:709–720. doi: 10.1080/09540120120076878. [DOI] [PubMed] [Google Scholar]
- Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. Aids. 2002;16:269–277. doi: 10.1097/00002030-200201250-00017. [DOI] [PubMed] [Google Scholar]
- Webel AR, Asher A, Cuca Y, Okonsky JO, Burant C, Kaihura A, Hanson J, Dawson-Rose C, Salata R. Measuring HIV Self-Management in Women Living with HIV/AIDS: A Psychometric Evaluation Study of the HIV Self-Management Scale. Journal of Acquired Immune Deficiency Syndrome. 2012;60(3):e72–e81. doi: 10.1097/QAI.0b013e318256623d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson IB. Improving treatment adherence. John Hopkins Advanced Studies in Medicine. 2010;10:53–57. [Google Scholar]
- Wilson IB for the MACH 14 Investigators. A ‘honeymoon effect’ when initiating the use of electronic drug monitoring (EDM) in clinical studies: findings from MACH14. [Abstract # 62225]. Presented at: 5th International Conference on HIV Treatment Adherence; May 23–25, 2010; Miami, FL. 2010a. Abstract retrieved from: http://www.iapac.org/AdherenceConference/Downloads-ADC10/Adherence2010_Program_and_Abstracts%20book_051310.pdf. [Google Scholar]
- Wilson IB for the MACH 14 Investigators. Heterogeneity among studies in rates of declines of antiretroviral therapy (ART) adherence over time: findings from MACH14. [Abstract # 62221]. Presented at: 5th International Conference on HIV Treatment Adherence; May 23–25, 2010; Miami, FL. 2010b. Abstract retrieved from: http://www.iapac.org/AdherenceConference/Downloads-ADC10/Adherence2010_Program_and_Abstracts%20book_051310.pdf. [Google Scholar]
- Wroe A, Thomas M. Intentional and unintentional nonadherence in patients prescribed HAART treatment regimens. Psychology Health & Medicine. 2003;8:453–463. doi: 10.1080/1354850310001604595. [DOI] [PubMed] [Google Scholar]
- Wroe AL. Intentional and unintentional nonadherence: a study of decision making. Journal of Behavioral Medicine. 2002;25:355–372. doi: 10.1023/a:1015866415552. [DOI] [PubMed] [Google Scholar]
- Yard SS, Huh D, King KM, Simoni JM. Patient-Level Moderators of the Efficacy of Peer Support and Pager Reminder Interventions to Promote Antiretroviral Adherence. AIDS and Behavior. 2011 doi: 10.1007/s10461-011-0001-4. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]