Abstract
Background
Pharmacovigilance concerns the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems. Consumer pharmacovigilance is the involvement of consumers in adverse drug reaction (ADR) reporting. Assessing healthcare professionals’ (HCPs) knowledge of and attitude towards pharmacovigilance and consumer pharmacovigilance is integral to strengthening adverse drug reaction reporting systems.
Aims
To study knowledge of and attitude towards pharmacovigilance and consumer pharmacovigilance among HCPs from KIST Medical College, Lalitpur, Nepal, and to plan an appropriate educational intervention to address deficiencies noted.
Method
The study was conducted from February 2013 to December 2013 at KIST Medical College using a self-administered, pretested, structured questionnaire. The maximum possible scores for knowledge, attitude, and total were 100, 95, and 195, respectively. Baseline knowledge and attitude were studied. Two months after the questionnaire, an intervention that used a combination of methods about pharmacovigilance and consumer pharmacovigilance was undertaken. Knowledge and attitudes were studied immediately after the intervention. Scores before and after the intervention were compared using Wilcoxon signed-rank test.
Results
A total of 105 HCPs participated. The median (interquartile range) knowledge, attitude, and total scores before the intervention were 56 (7), 72 (9), and 127 (16), respectively. After the intervention the scores increased significantly to 72 (8), 75 (11.5), and 146 (16.5) (p<0.001), respectively.
Conclusion
The intervention was effective in improving HCPs’ knowledge of and attitude towards pharmacovigilance and consumer pharmacovigilance. More studies on this topic among HCPs at other institutions and in the community are required.
Keywords: Attitude, pharmacovigilance, consumer pharmacovigilance, healthcare professionals, Nepal
What this study adds:
-
What is known about this subject?
In developing countries, consumers are involved in adverse drug reaction (ADR) reporting with significant benefits. Pilot studies involving consumers in pharmacovigilance have also been conducted in certain developing countries.
-
What new information is offered in this study?
This study offers insight into healthcare professionals’ knowledge of and attitude towards pharmacovigilance and consumer pharmacovigilance at a regional pharmacovigilance centre in Nepal. It also highlights how an educational intervention improved the HCPs’ knowledge and attitude.
-
What are the implications for research, policy, or practice?
There is an urgent need for developing guidelines to initiate an improvement in consumer pharmacovigilance in Nepal with respect to attitudes towards and reporting of ADRs.
Background
Adverse drug reactions (ADRs) are a major cause for morbidity and mortality globally.1,2 The World Health Organization (WHO) defines an ADR as “a response to a drug which is harmful and unintended, and which occurs at doses normally used in man for the prophylaxis, diagnosis, or therapy of disease or for the modification of body functions”.3 ADRs can be a big threat to the health of people in Nepal given the variety of allopathic, traditional, homeopathic, and ayurvedic medicines available on the market. Hence, reporting of ADRs should be a priority area.
Underreporting of ADRs remains a big problem worldwide.4 A systematic review published in 2006, which analysed the causes of underreporting, mentions that only 5–10 per cent of ADRs are reported.5 This review had examined studies estimating underreporting of ADRs.5 The underreporting rate of ADRs by general practitioners ranged from 36 per cent to more than 99 per cent, while in the hospital setting underreporting rates ranged from 59 per cent to 100 per cent. Many factors contribute to underreporting by Healthcare Professionals (HCPs);6–8 however, their knowledge of and attitudes towards ADR and ADR reporting is an important factor.8
Spontaneous reporting by healthcare professionals is the most common method used to report ADRs.9 HCPs in Nepal are medical doctors that have an undergraduate medical degree (MBBS) or advanced qualifications, dental surgeons that have a Bachelor in Dental Surgery, pharmacists, and paramedical professionals such as health assistants (HAs), community medicine auxiliaries (CMAs), auxiliary nursing midwives (ANMs), and community health workers (CHWs).10 Upon completing 10 years of schooling, HAs and CMAs undergo basic medical training of 36 months and 18 months, respectively. HAs and CMAs receive training to diagnose and treat common illnesses and can refer patients for more specialised care as required.10 They can treat patients suffering from minor illnesses and prescribe a few select medicines. After 10 years of schooling, auxiliary nursing midwives obtain basic nursing training of 18 months; they assist in the delivery of babies.
Physicians, pharmacists, and nurses have a major role in pharmacovigilance programmes. Nurses are among the first HCPs to observe patients admitted for treatment. They can educate patients and their families and/or care providers for the signs and symptoms that should be reported immediately.11 Similarly, pharmacists have a diverse role that includes the promotion, development, maintenance, and ongoing evaluation of a programme to reduce the risk of ADRs. Pharmacists can also educate physicians and nurses, and can encourage compliance with the ADR reporting programme.12
Pharmacovigilance activities in Nepal
Nepal’s drug regulatory authority is the Department of Drug Administration (DDA) within the Ministry of Health. It was formed as per the Drug Act of 1978. DDA regulates the manufacture, import/export, sales, distribution, and storage of drugs in Nepal, and also houses the National Centre for Pharmacovigilance established in 2004.13
Nepal became a member of the International Pharmacovigilance Programme in 2007.14 KIST Medical College joined the programme as a regional centre in July 2008.15 Presently, there are seven regional pharmacovigilance centres in Nepal reporting ADRs to the national centre, which sends reports to the Uppsala Monitoring Centre in Sweden, a centre for international service and scientific research towards patient safety.16
Nepal’s existing ADR reporting system relies on voluntary reporting as the main source of information.17 The national centre has designed a national ADR reporting form for HCPs. Different regional centres have their own ADR forms based on the national form, however, approximately 40 per cent of healthcare professionals who could play an important role in reporting ADRs both inside and outside the regional pharmacovigilance centres are unaware of the form’s existence and its intended use as a reporting mechanism for suspected ADRs.18 To date, consumers are not involved in Nepal’s ADR reporting system.
The national pharmacovigilance centre encourages ADR reporting by HCPs, but according to DDA statistics, by the end of 2013 only 523 ADRs had been reported.19 The WHO indicates that fully functional pharmacovigilance systems should expect to receive 200 ADR reports per year per million population; for Nepal, that equates to 6,097 ADR reports per year for its population of 30.5 million.20
Nepal, being a developing country, has to overcome many obstacles to develop a strong pharmacovigilance programme. Many factors, including lack of full-time dedicated staff responsible for pharmacovigilance activities, lack of public awareness programmes, and lack of standard guidelines for pharmacovigilance, have been found to cause underreporting of ADRs.17 One of the most important limitations of Nepal’s existing pharmacovigilance programme is lack of dedicated personnel responsible for managing the pharmacovigilance programmes in the regional centres.17 Currently, there is also only one person in the national pharmacovigilance centre that coordinates pharmacovigilance activities.21
Common reasons cited for underreporting by HCPs were ignorance and insecurity,5 indifference or lack of interest in registering ADRs, and lack of time due to competing demands in the clinical routine. Another study conducted in India described lack of time to fill in a report, lack of time to actively look for ADRs, and lack of confidence as common factors for underreporting.22 Certain HCPs may be interested in reporting ADRs because of their professional interest to inform others.5 In a recent study in Nepal, the prevalence of ADRs was found to be 0.86 per cent, with a male-to-female ADR prevalence ratio of 0.85 and proportion of severe ADRs as 10.81 per cent. These findings, demonstrating the high rate of ADR in this country, underpin the necessity to further examine the causes and consequences of ADRs in Nepal.23
Rationale of the study
Studies have revealed major lack of awareness and perceptions about pharmacovigilance and consumer pharmacovigilance among HCPs.12,17,24,25 As HCPs play an important role in educating their patients and are respected persons in local communities, it is important that they provide proper medical care to patients as their knowledge about pharmacovigilance can be transferred to patients, patients’ families, and society.
There have been no previous pre-post comparison studies analysing the knowledge of and attitude towards pharmacovigilance and consumer pharmacovigilance among HCPs following an educational intervention in Nepal. The present study was planned to evaluate the knowledge of and attitude towards pharmacovigilance among HCPs. The association of knowledge and attitude scores with demographic factors, if noted, would help to identify subsections of HCPs who may have deficiencies in this area and require extra educational programmes. This study also explores the current status of consumer pharmacovigilance in different countries, to provide comparison and foundation for initiating a programme in Nepal. Therefore, this study was carried out with the following objectives:
To obtain information regarding the knowledge of and attitude towards pharmacovigilance and consumer reporting of ADRs among healthcare professionals from KIST Medical College in Lalitpur District.
To note the association of knowledge and attitude with demographic and other characteristics of healthcare professionals and compare the scores for knowledge and attitude before and after an educational intervention.
Method
Study site and study period
This study was conducted from February 2013 to December 2013 in a medical school located at Lalitpur, one of Nepal’s 75 districts. According to the 2011 census, the population of Kathmandu Valley was 466,784.27 The valley includes three districts: Lalitpur, Kathmandu, and Bhaktapur.
Study design
The design was cross-sectional: one-group pre-test–post-test (quasi experimental) design. The study population comprised healthcare professionals working at KIST Medical College, Lalitpur District, Nepal.
Sampling method
The method used was random sampling and was conducted among medical doctors, dentists, nursing staff, and other HCPs. From the 235 HCPs employed at KIST Medical College, 105 were included in the study. Only 105 respondents were included because the HCPs were advised not to hamper their important duties, so some could not take time off to participate.
Sample size calculation
For sample size calculation, we assumed that the knowledge should be about 40 per cent in our population of HCPs. This was obtained from the results of the pilot test and also from the literature review.27
Knowledge = 40%, P=0.4, Q=1-P=0.6
N=Zα2xPxQ/(M.E.)2
Where Zα = 1.96 from normal table, two tailed
P = Population proportion
M.E.= Margin of error = 10%
-
Now, n = (1.96)2 x (0.4) x (0.6)/(0.1)2
= 92
Non-response correction = 10%
Total sample size needed with provision for drop outs from the study = 92 + 10% of 92 = 101
The hospital management supported the study and all interested HCPs working at KIST Medical College were included in it. The hospital management allotted a certain time period where the authors could interact with the doctors, dentists, nurses, HAs, and CMAs. This was arranged during one of the clinico-investigative conferences, which is a regular academic activity. This arrangement allowed the authors to have enough time to introduce the study to the respondents and answer their queries. Knowledge and attitude regarding pharmacovigilance and consumer pharmacovigilance were studied using a questionnaire.
Demographics
Information like gender, age, ethnic/caste group, working experience, and educational qualifications of the respondents was noted. Participants’ knowledge and attitudes were measured by noting their agreement with a set of 39 statements using a Likert-type scale.
Scoring system
The scoring system used was: 5=strongly agree, 4=agree, 3=neutral, 2=disagree, and 1=strongly disagree. There were 20 statements for assessing knowledge with a maximum possible score of 100 and 19 statements for attitude with a maximum possible score of 95. The total scores before and after the module were obtained by adding the “Knowledge” and “Attitude” scores. The maximum total score was 195. The median and interquartile range was calculated for “Knowledge”, “Attitude”, and “total” scores. The questionnaire addressed different aspects of pharmacovigilance and consumer pharmacovigilance. The topics to be included in the questionnaire were developed on the basis of review of the literature and the authors’ experiences of important issues related to pharmacovigilance in Nepal.12,17,24,25 Inputs were also obtained from other experts in this field. To avoid bias, certain statements were negative and their scores were reversed while calculating the total score. Knowledge, attitude, and total scores were compared before and after the educational intervention.
Development of the questionnaire
The questionnaire included questions about knowledge of and attitude towards pharmacovigilance and consumer pharmacovigilance based on previous studies. The topics covered were the origin of pharmacovigilance in Nepal, progress and status of pharmacovigilance, and the country’s present system of pharmacovigilance. Information about reporting ADRs, who can report ADRs, and location and functions of the national pharmacovigilance centre were also covered.
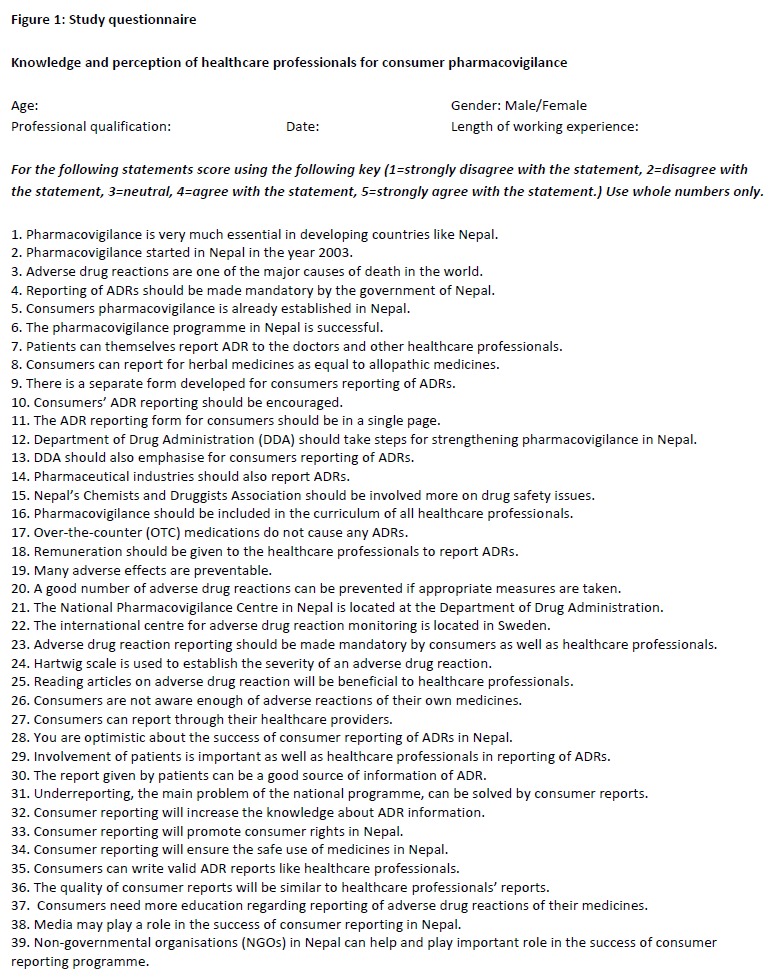
As a part of their professional role, HCPs are taught and trained to report ADRs; this training was enhanced by the educational intervention with an added emphasis on consumer reporting of ADRs. Manuscripts and published papers describing similar research and methodological issues were also studied to help us with designing the educational intervention. 12,17,24,25 The questionnaire was developed after discussion and deliberations among the researchers. After finalising the statements, these were further discussed with other faculty members of the department for their inputs. Inputs were also obtained from other researchers in the field. The questionnaire was developed in English (Figure 1) and was pilot tested.
Figure 1. Study questionnaire.
Pretesting of the questionnaire
The questionnaire was pretested for readability and ease of understanding among 12 HCPs (medical doctors, nurses, and pharmacists). The data obtained was not included in the study. Face validation was done by our departmental colleagues. Then, the questionnaire was sent to faculties of other departments for their input regarding readability and grammatical errors. Content validation was done by sending the questionnaire to the content experts of pharmacovigilance within Nepal. Internal consistency was measured by calculating Cronbach’s alpha value, which was 0.78, indicating good reliability.
Conduct of the study
This study was carried out in two phases. During the first phase, baseline knowledge and attitude of HCPs was studied so that strengths and deficiencies could be noted and an appropriate educational intervention planned. The second phase was done post-intervention with the same group. The time interval between the first phase of the study and the intervention was two months.
The subject areas covered during the educational session were those where participants had less knowledge and poor attitude as identified from their responses to the questionnaire. There was a presentation on important issues related to medicines, their effects on patient safety, as well as on the definition of pharmacovigilance and classification of ADRs, the WHO online database for reporting ADRs, and details about the ADR reporting form developed by the regional pharmacovigilance centre and the national ADR reporting form.
This was followed by a poster session where participants were provided with important information regarding pharmacovigilance. The posters focused on areas like different types of ADRs, reporting of ADRs, where to report and to whom to report, ADR reporting forms, and possible benefits of involving consumers in Nepal’s existing pharmacovigilance programme. These posters were obtained from the Department of Drug Administration. Several issues relating to medicine-use problems were also discussed; for example, “sound alike” and “look alike” (SALA) drugs, and management of ADRs. Inputs about the process to be followed and topics to be discussed during the intervention process were obtained from medical educators in the institution, other researchers working in the field of pharmacovigilance, and previous studies.12,17,24,25
Statistical analysis
After the intervention, scores for knowledge and attitude were again measured using the same questionnaire. The collected data was analysed using SPSS version 19.0 for Windows (SPSS Inc., Chicago, Illinois). The knowledge, attitude, and total scores before and after the educational intervention were tested for normality of distribution using one sample Kolmogorov-Smirnov test. The samples did not follow a normal distribution and the median was calculated as a measure of central tendency, interquartile range as a measure of variance, and non-parametric tests were used for comparison between different subgroups of respondents pre-intervention. Scores before and after the intervention were compared using the Wilcoxon signed-rank test. Median knowledge, attitude, and total scores were also compared among different subgroups of respondents both before and after the intervention across categories. A p value less than 0.05 was taken as statistically significant.
Ethical considerations
KIST Medical College’s Institutional Research Committee approved this study. All HCPs were informed about the aims and objectives of the study and invited to participate. Written informed consent was obtained from all participants.
Results
Respondent demographics
Details of the respondents’ demographic characteristics are shown in Table 1.
Table 1. Demographic characteristics of respondents (n=105).
| Characteristic | Number (%) |
|---|---|
| Gender | |
| Male | 54 (50.8) |
| Female | 51 (48.9) |
| Age | |
| <20 | 2 (1.9) |
| 21–30 | 62 (58.5) |
| 31–40 | 31 (29.2) |
| 41–50 | 10 (9.4) |
| Profession | |
| Doctor | 50 (47.2) |
| Nurse | 22 (20.8) |
| Paramedical | 14 (13.2) |
| Pharmacist | 6 (5.7) |
| Dentist | 10 (9.4) |
| Other | 3 (2.85) |
| Ethnic/Caste group | |
| Brahmin | 21 (19.8) |
| Chettri | 29 (27.4) |
| Newar | 42 (39.6) |
| Others | 13 (12.3) |
| Working experience | |
| 1–5 years | 38 (35.8) |
| 5–10 years | 34 (32.1) |
| >10 years | 16 (15.1) |
| Qualifications | |
| Below 10 class | 1 (0.9) |
| Intermediate | 6 (5.7) |
| Bachelor | 39 (36.8) |
| Master | 55 (51.9) |
| PhD | 4 (3.8) |
Fifty participants (47.2 per cent) were medical doctors, 22 (20.8 per cent) were nurses, 14 (13.2 per cent) were paramedicals, and 10 (9.4 per cent) were dentists. The majority of participants were Newars (42, 39.6 per cent), followed by Chettris (29, 27.4 per cent). Thirty-eight participants (35.5 per cent) had work experience between 1–5 years, and 34 (32.1 per cent) had work experience of 5–10 years. Fifty-five HCPs (51.9 per cent) had a doctor of medicine (MD) or master’s level of qualification, followed by 39 HCPs (36.8 per cent) with bachelor’s level of educational qualification. The total of different subgroups may not add up to 105 as certain respondents did not fill in all the required information.
Scores for knowledge and attitude
The median (interquartile range) knowledge and attitude scores before the intervention were 56 (7) and 72 (9), respectively, while the median total score was 127 (16). The median knowledge and attitude scores after the intervention were 72 (8) and 75 (11.5), respectively, while the total median score increased to 146 (16.5). The maximum possible knowledge and attitude scores were 100 and 95, respectively. On comparing pre- and post-intervention scores using the Wilcoxon signed-rank test, knowledge (p<0.001), attitude (p<0.001), and total scores (p<0.001) increased after the intervention (Table 2).
Table 2. Median knowledge, attitude, and overall scores before and after intervention.
| Characteristic | Median score (95% CI) | P value |
|---|---|---|
| Knowledge | ||
| Before Intervention | 56 (54–57) | <0.001 |
| After Intervention | 72 (70–74) | |
| Attitude | ||
| Before Intervention | 72 (71–75) | <0.001 |
| After Intervention | 75 (73-77) | |
| Total score | ||
| Before Intervention | 127 (125–131) | <0.001 |
| After Intervention | 146 (144–149) |
The scores before and after the intervention were compared using Wilcoxon signed-rank test.
The scores of certain statements from the questionnaire were low before the intervention but increased post-intervention. Examples include:
#3. Adverse drug reactions are one of the major causes of death in the world.
#10. Consumers’ ADR reporting should be encouraged.
#13. DDA should also emphasise for consumers’ reporting of ADRs.
#17. Over-the-counter medicines do not cause any ADRs.
#19. Many adverse effects are preventable.
#30. The report given by patients can be a good source of information of ADR.
Table 3 compares median total scores among various subgroups of respondents both before and after the intervention across each category of these independent variables.
Table 3. Comparison of median scores among different subgroups of respondents before and after intervention.
| Characteristic | Knowledge | P value | Attitude | P value | Total | P value | |||
|---|---|---|---|---|---|---|---|---|---|
| Before Median score (95%CI) | After Median score (95%CI) | Before Median score (95%CI) | After Median score (95%CI) | Before Median score (95%CI) | After Median score (95%CI) | ||||
| Gender a | |||||||||
| Male | 54 (52–56) | 70 (68–74) | <0.001 | 71 (69–73) | 76 (71–77) | <0.001 | 125 (121–129) | 144 (141–149) | <0.001 |
| Female | 57 (55–59) | 73 (71–75) | <0.001 | 74 (72–75) | 74 (72–77) | 0.132 | 133 (127–136) | 146 (144–153) | <0.001 |
| Age (in years) | |||||||||
| <20 | 64 (64–65) | 72 (70–74) | 0.180 | 79 (75–84) | 67 (66–68) | 0.180 | 144 (139–149) | 139 (136–142) | 0.655 |
| 21–30 | 55 (53–57) | 72 (69–74) | <0.001 | 71 (69–73) | 73 (70–76) | <0.001 | 126 (122–129) | 145 (141–149) | <0.001 |
| 31–40 | 55 (53–59) | 71 (68–75) | <0.001 | 74 (72–77) | 77 (73–80) | 0.002 | 129 (124–135) | 146 (143–155) | <0.001 |
| 41–50 | 59 (54–61) | 76 (68–80) | 0.005 | 76 (64–81) | 76 (68–86) | 0.070 | 135 (119–139) | 153 (138–163) | <0.005 |
| Profession a | |||||||||
| Doctors | 55 (54–58) | 73 (69–75) | <0.001 | 72 (69–75) | 76 (73–78) | <0.001 | 126 (124–129) | 146 (144–153) | <0.001 |
| Nurses | 60 (57–63) | 75 (72–79) | <0.001 | 75 (73–81) | 71 (67–77) | 0.040 | 136 (131–139) | 147 (139–156) | <0.001 |
| Paramedicals | 54 (50–58) | 70 (68–74) | 0.001 | 70 (68–82) | 74 (72–87) | 0.001 | 125 (119–135) | 145 (140–155) | <0.001 |
| Pharmacist | 53 (51–58) | 70 (68–77) | 0.026 | 74 (58–79) | 78 (62–83) | 0.014 | 128 (110–134) | 150 (130–155) | 0.026 |
| Dentist | 52 (49–57) | 68 (64–72) | 0.005 | 70 (60–77) | 74 (64–82) | 0.004 | 131 (110–136) | 142 (130–157) | 0.005 |
| Others | 51 | 72 (70–74) | 0.109 | 72 (71–75) | 75 (73–77) | 0.101 | 128 (125–131) | 136 (133–138) | 0.026 |
| Ethnic/Caste group a | |||||||||
| Brahmin | 55 (51–58) | 72 (67–75) | <0.001 | 70 (65–73) | 73 (67–76) | 0.001 | 125 (118–129) | 144 (139–150) | <0.001 |
| Chettri | 56 (53–58) | 71 (70–74) | <0.001 | 71 (68–79) | 75 (70–82) | <0.001 | 129 (121–136) | 147 (141–156) | <0.001 |
| Newar | 56 (53–58) | 73 (69–75) | <0.001 | 74 (73–76) | 77 (75–78) | 0.018 | 130 (126–135) | 148 (145–155) | <0.001 |
| Others | 57 (52–61) | 69 (66–77) | 0.001 | 69 (62–75) | 71 (62–80) | 0.045 | 126 (116–135) | 140 (132–145) | 0.001 |
| Working experience a | |||||||||
| < 1 year | 54 (52–56) | 71 (67–74) | <0.001 | 69 (65–71) | 71 (68–75) | <0.001 | 122 (118–127) | 142 (138–147) | >0.001 |
| 1–5years | 55 (52–58) | 71 (68–74) | <0.001 | 74 (72–76) | 77 (73–79) | 0.000 | 130 (126–135) | 146 (144–153) | <0.001 |
| 5–10 years | 56 (54–62) | 72 (70–79) | <0.001 | 74 (68–80) | 75 (70–83) | 0.231 | 133 (124–135) | 149 (139–158) | <0.001 |
| >10 years | 59 (52–61) | 76 (68–78) | <0.001 | 75 (71–81) | 76 (71–82) | 0.171 | 135 (124–139) | 150 (142–161) | 0.001 |
| Qualifications a | |||||||||
| Intermediate | 52 (62–68) | 68 (66–75) | 0.024 | 73 (58–79) | 77 (62–83) | 0.014 | 125 (110–134) | 145 (130–155) | 0.024 |
| Bachelor | 56 (52–57) | 72 (68–74) | <0.001 | 71 (68–75) | 73 (68–76) | <0.001 | 128 (120–131) | 145 (139–152) | <0.001 |
| Master | 56 (54–59) | 73 (70–75) | <0.001 | 73 (71–75) | 75 (73–77) | <0.001 | 127 (125–135) | 148 (144–153) | <0.001 |
| PhD | 56 (51–61) | 71 (67–81) | 0.066 | 72 (62–88) | 76 (65–91) | 0.063 | 128 (114–148) | 150 (132–167) | 0.068 |
The scores before and after were compared using Wilcoxon signed-rank test.
The scores of different subgroups of respondents before the intervention
The median (IQR) knowledge scores improved significantly among females compared to males from 57 (8) to 73 (9) (p<0.001). Similarly, the scores significantly improved from 55 (7) to 72 (8) for respondents from the age group 21–30 years (p<0.001), and from 55 (8) to 71 (8) for participants from the age group 31–40 years (p<0.001). The scores improved significantly for doctors and nurses among other HCPs after the educational intervention 55 (7) to 73 (9), (p<0.001), and 60 (7) to 75 (8), (p<0.001), respectively.
There was a significant improvement in knowledge scores for participants from all ethnic groups. Similarly, scores improved significantly from 56 (8) to 73 (9), (p<0.001) for professionals having MD/master’s degree, and bachelor level of education from 56 (7) to 72 (8), (p<0.001). There was no significant difference in knowledge scores for professionals having intermediate level of qualification. Intermediate level means a diploma-level course, which is done after passing class 10 and is usually of two years duration. After completing the course, a student can get admission in related bachelor level courses in Nepal. There was no significant difference in knowledge scores among pharmacists and other HCPs post-intervention.
Attitude towards pharmacovigilance and consumer pharmacovigilance among different subgroups post-intervention
Males showed a significant improvement in their attitude towards pharmacovigilance post-intervention. Respondents from all age groups showed an improvement in scores, but those aged 21–30 showed a statistically significant improvement from 71 (11) to 73 (11), (p<0.001). Similarly, professionals from all ethnic backgrounds showed a significant improvement in scores post-intervention. Medical doctors showed significant improvement in attitude scores post-intervention, from 72 (10) to 76 (11), (p<0.001). Professionals having less than one year experience and bachelor level of educational qualification showed significant improvement from 69 (9) to 71(10), (p<0.001) and 71 (12) to 73(13), (p<0.001). There was no significant difference in attitude scores among pharmacists and other HCPs post-intervention.
Discussion
Reporting of ADRs is a very important and essential component of pharmacovigilance systems worldwide and is an essential part of the safety surveillance of marketed drugs. Spontaneous reporting remains an important tool for detecting and reporting ADRs. Studies have been done previously to evaluate HCPs’ knowledge of and attitude towards pharmacovigilance, but the concept of consumer pharmacovigilance is a new concept in developing countries like Nepal.17 To the best of our knowledge this is among the first studies to be done in Nepal among HCPs assessing knowledge of and attitude toward pharmacovigilance and consumer pharmacovigilance before and after an educational intervention. The overall median knowledge, attitude, and total scores improved significantly post-intervention. Differences in scores for knowledge and attitude were noted among certain groups of respondents both before and after the intervention. Pharmacovigilance and consumer pharmacovigilance should be emphasised during continuing professional education programmes and the educational intervention should be carried out at least twice a year for new HCPs joining the institution.
Knowledge
The scores for awareness about ADRs and Nepal’s ADR reporting system was low among HCPs in our study, which is similar to other studies previously reported.14,27–30 Various studies from developed countries like the United Kingdom and the United States have shown a higher rate of ADR reporting and relatively higher awareness and knowledge about pharmacovigilance among HCPs.31–33 In the UK, most medical schools have included the yellow card ADR reporting scheme in the undergraduate syllabi and the skills for reporting ADRs are assessed.34 In this study, doctors and nurses had slightly higher scores than other HCPs. This was similar to that observed in a study done among HCPs at a medical college in Nepal.31 Differences in the extent of knowledge and awareness in developing countries may be due to non-inclusion of ADRs, reporting of ADRs, and the assessments for ADRs in the curriculum. In Nepal, certain medical schools have included these topics in their undergraduate syllabi for medical students, whereas many others medical schools in Nepal have still not done so.35 The same scenario is noted with paramedical and nursing syllabi.
Awareness can be increased among HCPs by disseminating information about ADRs in continuous professional education sessions and other training related to pharmacovigilance. This can be a periodic educational process done regularly to encourage HCPs to report ADRs. In previous studies, improvement in knowledge has been shown to be associated with respondents’ level of education.36 In a recent study conducted among pharmacists regarding knowledge of and attitudes toward herbal medicine, the median knowledge scores improved after the educational intervention.37
Attitude
Attitude improved among both male and female respondents. Similarly, HCPs from different ethnic backgrounds observed improvement in scores, but Chettris showed a significant improvement. This may be due to the changing scenario with people from different ethnic backgrounds now obtaining more resources for education in this area. In Nepal, there are various ethnic groups whose members share a common tradition, often consisting of a common language and culture, and a shared religion. The caste group is a system of social stratification in which communities are defined by thousands of traditional groups called jatis.38
Attitude can be one’s own idea to express an appropriate behaviour for treatment-seeking practices.39 Attitude can be proper/positive, or improper/negative. Improved practice can result from proper attitudes, whereas harmful effects may be associated with an improper attitude.40 In Nepal, there is no compulsory reporting of ADRs by HCPs. Professionals like medical doctors, dentists, pharmacists, nurses, and others can report ADRs if they wish to do so. Among different categories of HCPs, both knowledge and attitude improved significantly among medical doctors in our study. Research has shown that ADRs encountered by HCPs during their professional work are never or rarely reported. The reason for this may be very busy schedules and a heavy patient workload. Nurses have also shown an improvement in knowledge scores. A study done in China had shown that nurses had encountered the maximum number of ADRs as compared to other HCPs, but they had not reported any.41 In Nepal, there are 10,197 (3.64/10,000 population) medical doctors and dentists, 32,846 (11.71 /10,000 population) nursing and midwifery personnel, and 731 (0.261 /10,000 population) licensed pharmacists.10
The HCP-patient ratio is not adequate (3.64/10,000 population), and HCPs find it difficult to spare time for ADR reporting. Many respondents stated that they were unaware of the existence of ADR reporting forms and the reporting process. This reaffirms underreporting by HCPs as shown by various studies.17,42–43 Since our intervention was for a short duration it may not be sufficient for substantial improvement in participants’ overall knowledge and attitude. The educational intervention was conducted only once for two hours and was not repeated. Knowledge and attitudes were tested again immediately after the educational intervention. The effect of the intervention on retention of information was not assessed. Lack of continuous feedback and information sharing by the regional pharmacovigilance centre from where HCPs can obtain information and knowledge about ADRs and reporting of ADRs may be another limitation that could have influenced underreporting of ADRs.
Possible strategies for improving pharmacovigilance and consumer pharmacovigilance in Nepal
Regular meeting with all HCPs in regional pharmacovigilance centres and periodic dissemination of reported ADRs with their details to the reporting HCPs and others would encourage ADR reporting. In some developed countries, consumer reported began in the 1970s, while in others it did not start until the 1990s.17 The concept of consumer pharmacovigilance can encourage understanding about pharmacovigilance and safer use of medicine to manage different diseases. Consumer pharmacovigilance can help report unwanted drug effects, which have not been described previously.
Consumer reporting cannot go ahead alone, it should be a part of consumer education on rational drug use and health care.17 A strong collaboration between DDA and the National Health Education Information and Communication Centre (NHEICC) is needed to bring consumer education into action. NHEICC is a centre in the Ministry of Health and Population responsible for an integrated approach and one system for advocacy, community mobilisation, behaviour change communication, and health service programme and promotion activities. At present, there is a strong need to establish coordination of ADR reporting activities among all stakeholders in Nepal to promote consumer pharmacovigilance.44
Recommendations, strengths, and limitations of the study
This study emphasises the importance of an educational intervention for improved knowledge of and attitude towards pharmacovigilance among healthcare professionals for better patient safety. This study enables all HCPs to understand the importance of pharmacovigilance, including the process for ADR reporting, and involving consumers as an important stakeholder for promoting consumer pharmacovigilance in Nepal. Similar studies are required in other regional centres to provide a more valid conclusion on the state of pharmacovigilance across Nepal.
This study has some limitations. We were unable to include all healthcare professionals in the study. Furthermore, all HCPs relevant to this study could not be contacted for the pre-test process and some HCPs, particularly nurses, were unable to take time out of their busy schedules despite our best efforts to create convenient time slots for conducting the study.
Conclusion
An educational intervention using different methods facilitating better understanding of pharmacovigilance and consumer pharmacovigilance-related issues was found to be effective in significantly improving knowledge, attitude, and total scores. However, since the intervention was carried out only once, its effect on retention of knowledge was not measured. More resource-intensive educational sessions are needed to gather information on ADRs and reporting of ADRs by healthcare professionals and consumers in a developing country like Nepal. Short training sessions or workshops should be arranged specifically for healthcare professionals like doctors, nurses, pharmacists, dentists, and also to consumers like patients, and school and college teachers, to educate them about reporting ADRs within the wider community. Further studies among a larger population of healthcare professionals are required.
ACKNOWLEDGEMENTS
We thank the KIST Medical College management for allowing us to conduct the study among various healthcare professionals from the hospital. Authors acknowledge the help of Ms Shova for assisting in data collection. We would also like to thank Dr Nilam Thakur for helping us with data collection. Finally, we would like to thank everyone who participated in the study and our fellow colleagues in the department for their kind support.
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
ETHICS COMMITTEE APPROVAL
KIST Medical College Institutional Review Board. The approval reference number is KISTMC/IRB/2069/20, Study ID number 2013/02.
Please cite this paper as: Please cite this paper as: Jha N, Rathore DS, Rathore DS, Shankar PR, Gyawali S, Alshakka M, Bhandary S. An educational intervention’s effect on healthcare professionals’ attitudes towards pharmacovigilance. AMJ 2014;7(12):478–489.http//dx.doi.org/10.4066/AMJ.2014.2235
References
- 1.Davies EC, Green CF, Taylor S, Williamson PR, Pirmohamed M. Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLOS ONE. 2009;4:e4439. doi: 10.1371/journal.pone.0004439. DOI: 10.1371/journal.pone.0004439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies EC, Green CF, Mottram DR, Pirmohamed M. Adverse drug reactions in hospitals: a narrative review. Curr Drug Saf. 2007;2:79–87. doi: 10.2174/157488607779315507. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Requirements for adverse reaction reporting. Geneva, Switzerland: World Health Organization; 1975. [Google Scholar]
- 4.Bateman DN, Sanders GL, Rawlins MD. Attitudes to adverse drug reaction reporting in the Northern Region. Br J Clin Pharmacol. 1992;34:421–6. DOI:10.1046/j.1365-2125.2001.01306.x. [PMC free article] [PubMed] [Google Scholar]
- 5.Hazell L, Shaki SA. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006;29(5):385–6. doi: 10.2165/00002018-200629050-00003. [DOI] [PubMed] [Google Scholar]
- 6.Rehan H, Vaseudev K, Tripathi C. Adverse Drug Reaction Monitoring: Knowledge, attitude and practices of medical students and prescribers. Nat Med J India. 2002;15:24–6. [PubMed] [Google Scholar]
- 7.Biagic C, Montanaro N, Buccellato E, Roberto G, Vaccheri A, Motola D. et al. Underreporting in pharmacovigilance: an intervention for Italian GPs (Emilial – Romagna region) Eur J Clin Pharmacol. 2013;69(2):237–44. doi: 10.1007/s00228-012-1321-7. [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Gonzalez E, Herdeiro MT, Figueiras A. Determinants of underreporting of adverse drug reactions: a systematic review. Drug Saf. 2009;32:19–31. doi: 10.2165/00002018-200932010-00002. DOI:10.1007/S11096- 012-9675-6. [DOI] [PubMed] [Google Scholar]
- 9.Harmark L, van Grootheest AC. Pharmacovigilance: methods, recent developments and future perspectives. Eur J Clin Pharmacol. 2008;64:743–52. doi: 10.1007/s00228-008-0475-9. DOI: 10.1007/S00228-008-0475-9. [DOI] [PubMed] [Google Scholar]
- 10.Department of Health Services: Annual Report F/Y 2009/10. Government of Nepal, Kathmandu; 2011. [Google Scholar]
- 11.Eisenhauer LA. Adverse drug reactions: a concern for clinicians and patients. Clin Excell Nurse Pract. 2002;6:3–7. [Google Scholar]
- 12.Palain S, Izham M, Mishra P. Evaluation of the knowledge, attitude and practices on adverse drug reactions and pharmacovigilance among healthcare professionals in a Nepalese hospital: a preliminary study. Int J Pharmacol. 2007;6:1. [Google Scholar]
- 13.Nepal. Department of Drug Administration. Drug Act 2035. 1978. Available from: http://www.dda.gov.np/drugact.php. [Google Scholar]
- 14.Subish P, Mohamed I, Mishra P. Pattern of adverse drug reaction reported by community pharmacist in Nepal. Pharm Pract. 2010;8:201–7. doi: 10.4321/s1886-36552010000300008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jha N, Bajracharya O, Shrestha R, Thapa HS, Shankar PR. Starting a pharmacovigilance program within a teaching hospital: challenges and experiences from Lalitpur, Nepal. Southern Med Rev. 2009;2(1):7–10. [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Nepal joins programme. Uppsala Reports. 2007;36:5–6. Available from: http://who-umc.org/graphics/24365.pdf. [Google Scholar]
- 17.Jha N, Rathore DS, Shrestha PR, Thapa BB, Bhuju G, Alshakka M. Need for involving consumers in Nepal’s pharmacovigilance system. Australas Med J. 2014;7(4):191–5. doi: 10.4066/AMJ.2014.2011. DOI:10.4066/AMJ.2014.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Santosh KC, Pramote T, Edwards IR, Gorsanan S. Knowledge about adverse drug reactions reporting among healthcare professionals in Nepal. Inter J of Risk & Saf in Med. 2013;25:1–16. doi: 10.3233/JRS-120578. DOI:10.3233/JRS-120578. [DOI] [PubMed] [Google Scholar]
- 19.Santosh KC, Bhuju GB, Tragulpiankit P. Pattern of adverse drug reactions reported by Nepal regional pharmacovigilance centres [abstract] Drug Saf. 2010;33(10):940. [Google Scholar]
- 20.World Health Organization. Safety Monitoring of Medicinal Products. Uppsala,Sweden: Uppsala Monitoring Centre. 2000:28 p. Available from: http://apps.who.int/medicinedocs/en/d/Jh2934e/1.html. [Google Scholar]
- 21.Ministry of Health and Population in collaboration of WHO: Nepal pharmaceutical country profile. Kathmandu; September 27, 2011. Available from: http://apps.who.int/medicinedocs/en/m/abstract/Js19096en/ [Google Scholar]
- 22.Ramesh A. Identifying the reasons for underreporting of ADR: a cross sectional survey. Res. J. Pharm., Biol. Chem. Sci. 2012;3:1379–86. [Google Scholar]
- 23.Jha N, Bajracharya O, Namgyal T. Prevalence of adverse drug reactions with commonly prescribed drugs in different hospitals of Kathmandu valley. Kath Univ Med J (KUMJ) 2007;5(4):504–10. [PubMed] [Google Scholar]
- 24.Alshakka MA, Izham MI, Azmi AH. Do health care professionals have positive perception towards consumers reporting adverse drug reactions? J Clin Diagn Res. 2013;7(10):2181–85. doi: 10.7860/JCDR/2013/5778.3464. DOI: 10.7860/JCDR/2013/5778.3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rajesh R, Vidyasagar S, Varma DM. An Educational Intervention to assess Knowledge Attitude Practice of pharmacovigilance among Health care professionals in an Indian tertiary care teaching hospital. Int .J. PharmTech Res. 2011;3(2):678–92. [Google Scholar]
- 26.Wikipedia. Lalitpur District, Nepal. Available from: http://en.wikipedia.org/wiki/Lalitpur_District,_Nepal. [Google Scholar]
- 27.Praveen S, Prakash RJ, Manjunath GN, Gautham MS, Kumar N. Adverse Drug Reaction reporting among medical and dental practitioners: a KAP study. Indian J Med Spec. 2013;4(1):10–15. [Google Scholar]
- 28.Pimpalkhute SA, Jaiswal KM, Sontakke SD, Bajait CS, Gaikwad A. Evaluation of awareness about pharmacovigilance and adverse drug reaction monitoring in resident doctors of a tertiary care teaching hospital. Indian J Med Sci. 2012;66:55–61. DOI:10.4103/0019-5359.110902. [PubMed] [Google Scholar]
- 29.Madhan R, Parthasarathi G. Adverse drug reactions reporting: Attitudes and perceptions of medical practitioners. Asian J Pharm Clin Res. 2009;2:10–4. [Google Scholar]
- 30.Oshikoya KA, Awobusuyi JO. Perceptions of doctors to adverse drug reaction reporting in a teaching hospital in Lagos, Nigeria. BMC Clin Pharmacol. 2009;9:14. doi: 10.1186/1472-6904-9-14. DOI: 10.1186/1472-6904-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palaian S, Ibrahim MI, Mishra P. Health professionals' knowledge, attitude and practices towards pharmacovigilance in Nepal. Phar Pract. 2011;9(4):228–35. doi: 10.4321/s1886-36552011000400008. DOI: 10.4321/S1886-36552011000400008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bateman DN, Sanders GL, Rawlins MD. Attitudes to adverse drug reaction reporting in the Northern Region. Br J Clin Pharmacol. 1992;34:421–6. [PMC free article] [PubMed] [Google Scholar]
- 33.Milstein JB, Faich GA, Hsu JP. Factors affecting physician reporting of adverse drug reactions. Drug Inf J. 1986;20:157–64. [Google Scholar]
- 34.Cox AR, Marriott JF, Wilson KA, Ferner RE. Adverse drug reaction teaching in UK undergraduate medical and pharmacy programmes. J Clin Pharm Ther. 2004;29:31–5. doi: 10.1046/j.1365-2710.2003.00533.x. [DOI] [PubMed] [Google Scholar]
- 35.Shankar PR, Subish P, Mishra P, Dubey AK. Teaching pharmacovigilance to medical students and doctors. Indian J Pharmacol. 2006;38(5):316–9. DOI: 10.4103/0253-7613.27698. [Google Scholar]
- 36.Elkalmi RM, Al-lela OQ, Jamshed SQ. Motivations and Obstacles for Adverse Drug Reactions Reporting among Healthcare Professionals from the Perspective of Lewin’s Force Field Analysis Theory: Analytic Approach. J Pharmacovigilance. 2014;2:130. DOI: 10.4172/2329-667.1000130. [Google Scholar]
- 37.Chang ZG, Kennedy DT, Holdford DA, Small RE. Pharmacists' knowledge and attitudes toward herbal medicine. Ann Pharmacother. 2000;34:710–15. doi: 10.1345/aph.19263. [DOI] [PubMed] [Google Scholar]
- 38.Lynn B, Dahal DR, Govindasamy PAV. Caste, ethnic and regional identity in Nepal: further analysis of the 2006 Nepal demographic and health survey. Calverton, Maryland, USA: Macro International Inc. 2008 Available from: http://measuredhs.com/pubs/pdf/FA58/FA58.pdf. [Google Scholar]
- 39.Good B. Medicine, rationality and experience: An anthropological perspective. Cambridge: Cambridge University Press. 1993 [Google Scholar]
- 40.Cleland J. A critique of KAP studies and some suggestions for their improvement. Stud Fam Plann. 1973;4:42–7. [PubMed] [Google Scholar]
- 41.Li Q, Zhang SM, Chen HT, Fang SP, Yu X, Liu D. Awareness and attitudes of healthcare professionals in Wuhan, China to the reporting of adverse drug reactions. Chin Med J (Engl) 2004;117:856–61. [PubMed] [Google Scholar]
- 42.Sharma N, Bhargava M, Mishra AK, Parakh R, Sharma D, Mahawari D. Current Scenario of pharmacovigilance amongst the health care professionals working in a teaching hospital in Rajsthan. Int J Cur Res Rev. 2014;6(9):93. [Google Scholar]
- 43.Ekman E, Backstrom M. Attitudes among hospital physicians to the reporting of adverse drug reactions in Sweden. Eur J Clin Pharmacol. 2009;65:43–6. doi: 10.1007/s00228-008-0564-9. [DOI] [PubMed] [Google Scholar]
- 44.Shrestha NP, Ludeman E. “Safety of Medicinal Products in Nepal: Pharmacovigilance Assessment and Performance.” Submitted to the US Agency for International Development by the Systems for Improved Access to Pharmaceuticals and Services (SIAPS) Program, Management Sciences for Health, Arlington, VA, USA. 2013 Feb; [Google Scholar]


