Abstract
Objectives
To evaluate the effects of transdermal estrogen therapy on bone mineral density (BMD) in postmenopausal Korean women.
Methods
A total of 149 healthy postmenopausal women were retrospectively evaluated: 100 were on hormone therapy (HT) and 49 were the control group. For the HT group, 54 applied estrogen transdermally using either a patch (n = 21) or gel (n = 33), and 46 took estrogen orally (conjugated estrogen 0.625 mg or equivalent). Demographic profiles and changes in BMD over two years were compared according to the route of the estrogen.
Results
No differences were found in age, age at menopause, parity, body mass index, and type of menopause among the oral, transdermal and control groups. Compared with controls, HT significantly increased BMD after 2 years in both the lumbar spine and the total hip. The increases in BMD at both lumbar spine and hip were comparable between the oral and transdermal groups. There were also no differences in BMD changes according to progestogen addition in either the oral or transdermal groups.
Conclusion
Transdermal estrogen therapy increases BMD, comparable to oral estrogen, in postmenopausal Korean women.
Keywords: Administration cutaneous, Bone density, Hormone replacement therapy, Postmenopause
Menopause, the permanent cessation of menstruation, occurs at the mean age of 49.7 years in Korea.1 Although the age at menopause has remained remarkably constant, the postmenopausal period has been enlongated due to the great increase in the life expectancy of women. In this circumstance, osteoporosis is becoming a major health problem which affects one third of women aged over 50.2 Meanwhile, osteoporosis can lead to increased medical and social costs, impaired quality of life and higher mortality rate related to fractures.
After menopause, estrogen deficiency results in the accelerated bone loss and increased the risk for fractures. Hormone therapy (HT) has established beneficial effect on bone loss as well as relief of menopausal symptoms.3,4,5,6,7 Although oral route is most commonly used for administration of HT, several adverse effects could be a barrier for the treatment, since oral estrogen affects liver function, increases clotting factors or inflammatory markers, and may cause gastrointestinal problems.8,9,10 In these aspects, there have been attempts to use non-oral route for estrogen administration. Since transdermal route bypasses the gastrointestinal tract and first hepatic metabolism in contrast to oral route,9,10 it maintains more constant level of serum estrogen, and alters liver function, clotting, and inflammatory markers less than oral estrogen.8,9,10
Previous studies demonstrated comparable effects of transdermal estrogen over oral administration on relief of vasomotor symptoms and protection of bone loss in postmenopausal women.11,12 However, in Korea, there have been only a few reports on effects of transdermal estrogen in postmenopausal women, and most of them were regarding the effects on symptom relief or lipid metabolism, and skeletal protective effect was rarely addressed.13,14,15,16,17,18 The aim of the present study was to compare the effects of estrogen on bone according to route of administration in postmenopausal Korean women.
Materials and Methods
This retrospective study included 149 healthy postmenopausal women: 100 women who received HT at Samsung Medical Center Menopause Clinic, and 49 women who had annual routine checkups at Samsung Medical Center for Health Promotion. Women without menstruation for at least 12 months or those with serum level of follicle stimulating hormone over 40 mIU/mL were defined as postmenopausal. Only women with baseline and annual follow up results of bone mineral density (BMD) for two years were eligible for this study. Exclusion criteria were prior exposure to HT within 6 months from the baseline and a history of diseases or medications that can affect BMD. In addition, women who changed the route of estrogen administration during the follow up were also excluded.
Women in HT group were treated with either oral (n = 46) or transdermal estrogen (n = 54). Oral estrogens were conjugated equine estrogen (CEE) 0.625 mg or equivalent, and transdermal estrogens were a patch (estradiol 1.5 mg patch, Estran-50 patch, [Handok Inc., Seoul, Korea] twice a week, n = 21) or gel (0.1% estradiol gel, Estreva gel [Samil Pharm Co., Ltd., Seoul, Korea] 1.5 mg once daily, n = 33). In oral estrogen group, 16 were treated with estrogen alone, 30 with estrogen combined with progestogen. In transdermal estrogen group, 15 were treated with estrogen alone, and 39 wi th estrogen combined with progestogen.
BMDs were measured annually using dual energy X-ray absorptiometry (DXA) at the lumbar spine (L2-4) and the total hip. Since there were two types of scan system used for DXA at our center, Hologic system (Hologic Inc., Bedford, MA, USA), and Lunar DXA system (GE Healthcare, Madison, WI, USA), standardized BMD were calculated by universal BMD standardization equations to compare BMDs from different system. The equation that used in the present study as follows: sBMD at the spine = 1.0550 X (BMD measured by Hologic system - 0.972) + 1.0436 = 0.9683 X (BMD measured by Lunar system - 1.1 ) +1.0436; sBMD at the total hip = (1.008 × BMD measured by Hologic system) +0.006 = (0.979 × BMD measured by Lunar system -0.031).19,20,21
Baseline characteristics in oral estrogen, transdermal estrogen and control groups were compared by one-way analysis of variance (ANOVA) for continuous variables and Pearson's chi-square test for categorical variables. BMD changes during the follow up period were compared by repeated measures ANOVA. In addition, independent-sample t test was used to compare the differences between the groups at each time point. Data were analysed with a standard statistical package (PASW 18.0; SPSS, Inc., Chicago, IL, USA), and P values less than 0.05 were regarded as statistically significant.
Results
Table 1 presents clinical characteristics at the baseline. There were no differences in age, age at menarche, age at menopause, parity, body mass index (BMI), and type of menopause among the oral or transdermal estrogen, and the control groups. Standardized baseline BMD at both the lumbar spine and the total hip also did not differ by group (Table 1).
Table 1.
Baseline characteristics of the study participants
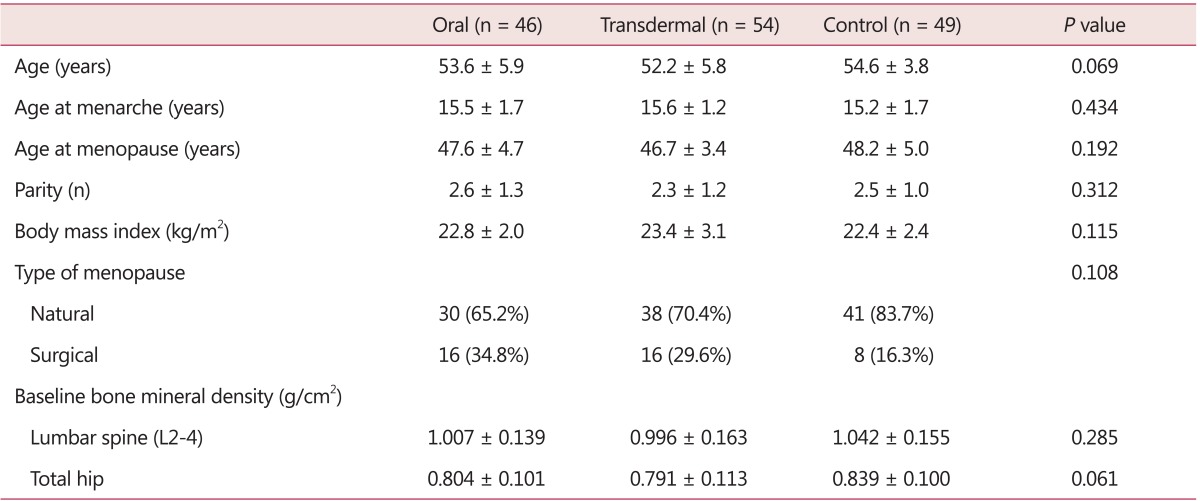
Data are presented as mean ± standard deviation (SD)
(P values by one-way analysis of variances) or n (%) (P values by Pearson's chi-square test)
BMD increased after HT (oral or transdermal), while it decreased in control group during the follow up period, showing significant differences at both the lumbar spine and the total hip, respectively (P < 0.05 and P < 0.01; Fig. 1).
Fig. 1.
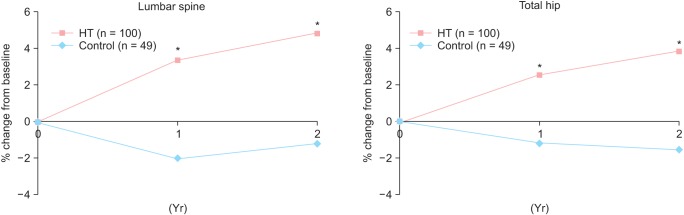
Bone mineral density changes between hormone therapy and control groups. HT: hormonal therapy. *P < 0.05, †P < 0.01 by independent sample t test.
In women who received estrogen alone (n = 31), the changes of BMD were not significantly different between the oral (n = 16) and tarnsdermal (n = 15) orute (Fig. 2).
Fig. 2.
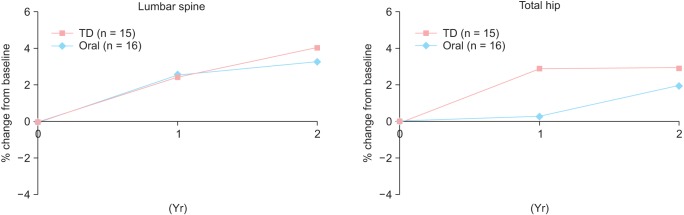
Changes in bone mineral density in women taking estrogen-alone according to route of administration. TD: transdermal.
Changes in BMD were compared according to the addition of progestogen. Figure 3 shows the changes in BMD between estrogen alone and estrogen combined with progestogen groups within oral HT group. BMDs increased in both groups without significant differences. In addition, within transdermal estrogen group, the pattern of BMD changes was also not different between estrogen alone and estrogen combined with progestogen groups (Fig. 4). Based on these findings, data on estrogen alone and estrogen combined with progestogen were pooled in the subsequent analysis, and comparisons were made only according to the route of estrogen administration.
Fig. 3.
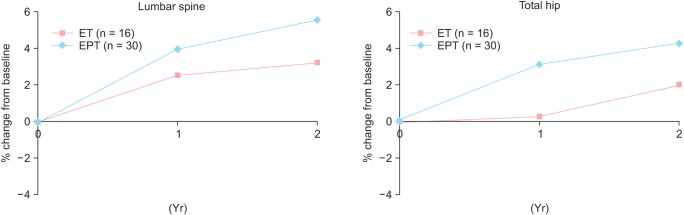
Changes in bone mineral density in women taking receiving hormone therapy using through oral estrogen. ET: estrogen therapy, EPT: estrogen plus progestogen therapy.
Fig. 4.
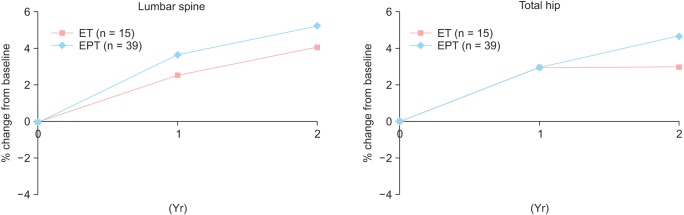
Changes in bone mineral density in women taking hormone therapy using transdermal estrogen. ET: estrogen therapy, EPT: estrogen plus progestogen therapy.
Figure 5 shows the changes in BMD after 2 years of HT. BMD at the lumbar spine increased by 4.8% in the oral estrogen group (n = 46) and 4.9 % in the transdermal estrogen group (n = 54) after 2 years of treatment. At the total hip, the BMD increased by 3.5 % in the oral estrogen group and 4.2 % in the transdermal estrogen group after 2 years. The changes in BMD at both the lumbar spine and the total hip according to the route of estrogen were comparable.
Fig. 5.
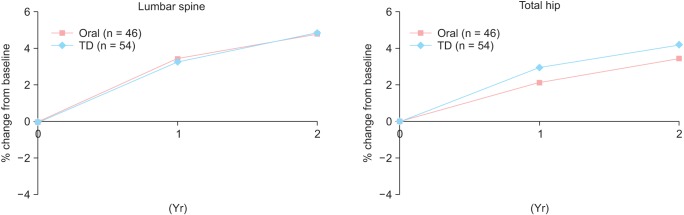
Changes in bone mineral density in women taking hormone therapy according to the route of estrogen administration - pooled analysis. TD: transdermal.
In addition, within transdermal group, the changes of BMD were not different according to the type of transdermal estrogen - gel or patch (data not shown).
Discussion
The present study compared changes in BMD according to the route of estrogen in postmenopausal Korean women, and demonstrated a positive effect of transdermal estrogen therapy on BMD, which was comparable to that of oral estrogen therapy.
Changes of BMD did not differ by addition of progestogen in both oral and transdermal estrogen groups, which is consistent with the results of a previous study showing no significant differences in BMD according to progestogen addition.11 Checa and colleagues22 also reported comparable odds ratios for bone loss in both the estrogen and estrogen-progestogen therapy. However, there are still conflicting results about the effect of progestogen addition on bone mass. A previous randomized trial reported that addition of medroxyprogesterone acetate (MPA) to CEE showed greater increase in spine BMD than CEE-alone.23 In addition, another randomized trial also showed additional gain in BMD within the group of CEE 0.625 mg combined with MPA 2.5 mg daily,24,25 and Dresner-Pollak and colleagues26 demonstrated positive effects on bone when norethindrone acetate was added to estradiol in postmenopausal women. To determine the effects of progestogen on bone, further studies are needed
Several studies have proposed ethnic differences on estrogen metabolism. Kim et al.27 reported different levels of sex hormones in postmenopausal women in different ethnicities. In addition, Caucasian women had higher bioavailable estradiol levels than African-American or Hispanic women, and the changes in estradiol levels among estrogen users were larger in Caucasian women than in African-American women. Huddleston and colleagues28 reported higher serum estradiol level in Asian after transdermal estradiol, which also suggests differences in metabolic clearance of sex hormones in different ethnic groups. In a similar way, bone metabolism also can be difefrent according to the ethnicity.29,30,31 Elevation of bone resorption marker was greater in Japanese women than in African-American or Caucasian women,32 and BMDs in postmenopausal Caucasian women were higher than those in Asian women at the total hip and spine, but lower than those in African-American women at the hip.29,33 Consequently, the prevalence of osteoporosis (37.0%) in Korea is higher than in Caucasian women.34,35 However, fracture rates were lower in Asian women than Caucasian women, and this discrepancy might also be explained by ethnic differences in bone microarchitecture or thickness and density of cortex.36,37
In spite of ethnic differences in bone metabolism, there have been limited reports regarding transdermal estrogen in Korean women. Transdermal estrogen was effective for relief of menopausal symptoms, and improvement of lipid profiles,15,16,17,18 but only few reports showed the increase in BMD with transdermal estrogen. A previous study evaluated the effects of transdermal estrogen in 30 postmenopausal Korean women, and reported 4.8% gain of BMD at the lumbar spine, showing consistency with our results. However, effects was not compared according to the route.16 To the best of our knowledge, this is the first report that compared beneficial effect of transdermal estrogen on bone with oral route in postmenopausal Korean women.
Nevertheless, the present study has some limitations mostly stemming from small sample size and retrospective design. In addition, fracture risk was not assessed. Use of two different DXA systems might affect precise comparisons, although BMD measurement was converted into standardized BMD for comparison.19,20,21
In conclusion, transdermal estrogen therapy increases BMD, to a similar degree with oral estrogen in postmenopausal Korean women.
Acknowledgement
This work has been supported in part by Sungkyunkwan University Foundation for Corporate Collaboration (S-2010-0228-000) and Samsung Medical Center Research Fund (PH01040831 and PH01095801).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Choi H, Lee HK, Park HM. The Korean menopausal womens attitudes and awareness on menopause: results of Korean gallup epidemiologic survey on menopause and HRT. J Korean Soc Menopause. 2003;9:36–43. [Google Scholar]
- 2.Iki M, Kagamimori S, Kagawa Y, Matsuzaki T, Yoneshima H, Marumo F. Bone mineral density of the spine, hip and distal forearm in representative samples of the Japanese female population: Japanese Population-Based Osteoporosis (JPOS) Study. Osteoporos Int. 2001;12:529–537. doi: 10.1007/s001980170073. [DOI] [PubMed] [Google Scholar]
- 3.Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- 4.Cauley JA, Robbins J, Chen Z, Cummings SR, Jackson RD, LaCroix AZ, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women's Health Initiative randomized trial. JAMA. 2003;290:1729–1738. doi: 10.1001/jama.290.13.1729. [DOI] [PubMed] [Google Scholar]
- 5.Kiel DP, Felson DT, Anderson JJ, Wilson PW, Moskowitz MA. Hip fracture and the use of estrogens in postmenopausal women. The Framingham Study. N Engl J Med. 1987;317:1169–1174. doi: 10.1056/NEJM198711053171901. [DOI] [PubMed] [Google Scholar]
- 6.Marjoribanks J, Farquhar C, Roberts H, Lethaby A. Long term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst Rev. 2012;7:CD004143. doi: 10.1002/14651858.CD004143.pub4. [DOI] [PubMed] [Google Scholar]
- 7.Wimalawansa SJ. A four-year randomized controlled trial of hormone replacement and bisphosphonate, alone or in combination, in women with postmenopausal osteoporosis. Am J Med. 1998;104:219–226. doi: 10.1016/s0002-9343(98)00029-1. [DOI] [PubMed] [Google Scholar]
- 8.Carroll N. A review of transdermal nonpatch estrogen therapy for the management of menopausal symptoms. J Womens Health (Larchmt) 2010;19:47–55. doi: 10.1089/jwh.2008.1206. [DOI] [PubMed] [Google Scholar]
- 9.Goodman MP. Are all estrogens created equal? A review of oral vs. transdermal therapy. J Womens Health (Larchmt) 2012;21:161–169. doi: 10.1089/jwh.2011.2839. [DOI] [PubMed] [Google Scholar]
- 10.Stevenson JC. Type and route of estrogen administration. Climacteric. 2009;12(Suppl 1):86–90. doi: 10.1080/13697130903007389. [DOI] [PubMed] [Google Scholar]
- 11.Cetinkaya MB, Kökçü A, Yanik FF, Başoğlu T, Malatyalioglu E, Alper T. Comparison of the effects of transdermal estrogen, oral estrogen, and oral estrogen-progestogen therapy on bone mineral density in postmenopausal women. J Bone Miner Metab. 2002;20:44–48. doi: 10.1007/s774-002-8446-8. [DOI] [PubMed] [Google Scholar]
- 12.Ravn P, Warming L, Christgau S, Christiansen C. The effect on cartilage of different forms of application of postmenopausal estrogen therapy: comparison of oral and transdermal therapy. Bone. 2004;35:1216–1221. doi: 10.1016/j.bone.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 13.Cho S, Kim SR, Lee WY, Kho SK, Hwang SO, Kim MY. The effect of transdermal estrogen on pulsatility index of internal carotid artery in postmenopausal women - Effect of estrogen on arterial tone. Korean J Obstet Gynecol. 1999;42:2182–2186. [Google Scholar]
- 14.Choi DS, Lee DY, Yoon BK. Effects of transdermal estrogen gel in postmenopausal Korean women. J Korean Soc Menopause. 2012;18:113–118. [Google Scholar]
- 15.Choi YM, Park SY, Koo SY, Lee HS, Suh CS, Kim SH, et al. The clinical efficacy of transdermal estrogen[betadiol] in the treatment of postmenopausal symptoms. Korean J Obstet Gynecol. 1999;42:745–751. [Google Scholar]
- 16.Chung H, Choi KH, Lee CU, Kim HS, Yim CH, Han KO, et al. Effect of transdermal estrogen gel combined with oral progestogen replacement therapy in Korean postmenopausal women. J Korean Soc Menopause. 2001;7:47–53. [Google Scholar]
- 17.Lee BY, Jeong MJ, Park KH, Lee BS, Cho DJ, Hwang DH, et al. The effects of transdermal estrogen replacement therapy on lipid metabolism in postmenopausal women. Korean J Obstet Gynecol. 1993;36:1875–1881. [Google Scholar]
- 18.Weon JC, Cho S, Jeong KW, Choi B, Hwang SO, Koh SK, et al. The effects of oral and transdermal estrogen replacement therapy on the levels of serum lipids and lipoproteins in hysterectomized postmeonpausal women. Korean J Obstet Gynecol. 1997;40:2015–2020. [Google Scholar]
- 19.Lu Y, Fuerst T, Hui S, Genant HK. Standardization of bone mineral density at femoral neck, trochanter and Ward's triangle. Osteoporos Int. 2001;12:438–444. doi: 10.1007/s001980170087. [DOI] [PubMed] [Google Scholar]
- 20.Hui SL, Gao S, Zhou XH, Johnston CC, Jr, Lu Y, Glüer CC, et al. Universal standardization of bone density measurements: a method with optimal properties for calibration among several instruments. J Bone Miner Res. 1997;12:1463–1470. doi: 10.1359/jbmr.1997.12.9.1463. [DOI] [PubMed] [Google Scholar]
- 21.Osteaux M, Louis O. Standardization of bone mineral density measurements and the European multicentre studies. Eur J Radiol. 1995;20:170–172. doi: 10.1016/0720-048x(95)00648-a. [DOI] [PubMed] [Google Scholar]
- 22.Checa MA, Del Rio L, Rosales J, Nogués X, Vila J, Carreras R. Timing of follow-up densitometry in hormone replacement therapy users for optimal osteoporosis prevention. Osteoporos Int. 2005;16:937–942. doi: 10.1007/s00198-004-1806-z. [DOI] [PubMed] [Google Scholar]
- 23.The Writing Group for the PEPI. Effects of hormone therapy on bone mineral density: results from the postmenopausal estrogen/progestin interventions (PEPI) trial. The Writing Group for the PEPI. JAMA. 1996;276:1389–1396. [PubMed] [Google Scholar]
- 24.Thorneycroft IH, Lindsay R, Pickar JH. Body composition during treatment with conjugated estrogens with and without medroxyprogesterone acetate: analysis of the women's Health, Osteoporosis, Progestin, Estrogen (HOPE) trial. Am J Obstet Gynecol. 2007;197:137.e1–137.e7. doi: 10.1016/j.ajog.2007.05.042. [DOI] [PubMed] [Google Scholar]
- 25.Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Effect of lower doses of conjugated equine estrogens with and without medroxyprogesterone acetate on bone in early postmenopausal women. JAMA. 2002;287:2668–2676. doi: 10.1001/jama.287.20.2668. [DOI] [PubMed] [Google Scholar]
- 26.Dresner-Pollak R, Mayer M, Hochner-Celiniker D. The decrease in serum bone-specific alkaline phosphatase predicts bone mineral density response to hormone replacement therapy in early postmenopausal women. Calcif Tissue Int. 2000;66:104–107. doi: 10.1007/s002230010022. [DOI] [PubMed] [Google Scholar]
- 27.Kim C, Golden SH, Mather KJ, Laughlin GA, Kong S, Nan B, et al. Racial/ethnic differences in sex hormone levels among postmenopausal women in the diabetes prevention program. J Clin Endocrinol Metab. 2012;97:4051–4060. doi: 10.1210/jc.2012-2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huddleston HG, Rosen MP, Gibson M, Cedars MI, Fujimoto VY. Ethnic variation in estradiol metabolism in reproductive age Asian and white women treated with transdermal estradiol. Fertil Steril. 2011;96:797–799. doi: 10.1016/j.fertnstert.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 29.Nam HS, Kweon SS, Choi JS, Zmuda JM, Leung PC, Lui LY, et al. Racial/ethnic differences in bone mineral density among older women. J Bone Miner Metab. 2013;31:190–198. doi: 10.1007/s00774-012-0402-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Russell-Aulet M, Wang J, Thornton JC, Colt EW, Pierson RN, Jr Bone mineral density and mass in a cross-sectional study of white and Asian women. J Bone Miner Res. 1993;8:575–582. doi: 10.1002/jbmr.5650080508. [DOI] [PubMed] [Google Scholar]
- 31.Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger ML, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20:185–194. doi: 10.1359/JBMR.041007. [DOI] [PubMed] [Google Scholar]
- 32.Sowers MR, Zheng H, Greendale GA, Neer RM, Cauley JA, Ellis J, et al. Changes in bone resorption across the menopause transition: effects of reproductive hormones, body size, and ethnicity. J Clin Endocrinol Metab. 2013;98:2854–2863. doi: 10.1210/jc.2012-4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gourlay ML, Preisser JS, Hammett-Stabler CA, Renner JB, Rubin J. Follicle-stimulating hormone and bioavailable estradiol are less important than weight and race in determining bone density in younger postmenopausal women. Osteoporos Int. 2011;22:2699–2708. doi: 10.1007/s00198-010-1505-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Densitometry TISfC. Official positions of the international society for clinical densitometry. West Hartford, CT: The International Society for Clinical Densitometry; 2007. [Google Scholar]
- 35.Lee J, Lee S, Jang S, Ryu OH. Age-related changes in the prevalence of osteoporosis according to gender and skeletal site: The Korea national health and nutrition examination survey 2008-2010. Endocrinol Metab (Seoul) 2013;28:180–191. doi: 10.3803/EnM.2013.28.3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walker MD, Liu XS, Stein E, Zhou B, Bezati E, McMahon DJ, et al. Differences in bone microarchitecture between postmenopausal Chinese-American and white women. J Bone Miner Res. 2011;26:1392–1398. doi: 10.1002/jbmr.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clark P, Tesoriero LJ, Morton DJ, Talavera JO, Karlamangla A, Schneider DL, et al. Hip axis length variation: its correlation with anthropometric measurements in women from three ethnic groups. Osteoporos Int. 2008;19:1301–1306. doi: 10.1007/s00198-008-0572-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


