Abstract
Objectives
The aim of this study is to investigate the association between serum uric acid level and metabolic syndrome according to menopausal status in Korean women.
Methods
A total of 2,241 women who visited to the health promotion center at Pusan National University Hospital from 2010 to 2014 were included in this cross-sectional study. Self-report questionnaires and interviews with healthcare providers were used to assess disease history, medication history, menstrual history and body size measuring. Anthropometric measurements and laboratory results were compared as presence of metabolic syndrome and menopausal status by student-t test. Logistic regression analysis was performed between presence of metabolic syndrome and presumable predictive factors, such as age, menopause and serum uric acid.
Results
The prevalence rate of metabolic syndrome were 7.45% (63/846) in pre-menopausal group and 23.87% (333/1395) in menopausal group. Serum uric acid level was higher in menopausal women than premenopausal women (4.6 ± 1.1 vs. 4.3 ± 0.9. P = 0.000). And, its concentration was also higher in metabolic syndrome than normal women regarding of menopausal statue (premenopause 4.7 ± 1.1 vs. 4.2 ± 0.8, P = 0.001, menopause 4.9 ± 1.3 vs. 4.5 ± 1.0, P = 0.000). Multiple logistic regression analysis showed serum uric acid and age have relationship with metabolic syndrome (OR: 1.453, 95% confidence interval [CI]: 1.074-1.111, P = 0.000; OR: 1.092, 95% CI: 1.305-1.619, P = 0.000).
Conclusion
We could find out some potential of uric acid as predictive factor for metabolic syndrome in premenopausal and menopausal group. Further investigation is required to clarify the relationship between serum uric acid, menopause and metabolic syndrome.
Keywords: Menopause, Metabolic syndrome X, Uric acid
Introduction
Metabolic syndrome is a risk factor of cardiovascular diseases and diabetes, these show high morbidity and are one of the main causes of mortality in the modern society.1,2,3 Because of this high morbidity and mortality rate, early diagnosis through screening test and aggressive treatment have been emphasized.
Many studies showed that serum uric acid was highly related to hypertension,4,5,6,7,8 dyslipidemia,6,7,9,10 insulin resistance (IR),5,6,7,8,10 and obesity.6,7 Based on these results, there were some studies to use the concentration of serum uric acid as an indi cator for IR and metabolic syndrome.11,12
However, there were some limitations to use serum uric acid as an indicator. Firstly, antioxidative characteristic of uric acid showed paradoxical value depending on blood concentration.13 At normal concentration, it showed antioxidative value, but hyperuricemia, high concentration of uric acid, was known as strong independent precursor for the metabolic syndrome.11 Secondly, serum uric acid concentration differed between men and women, which should be taken into account clearly before using serum uric acid as an indicator of metabolic syndrome. The serum uric acid concentration was higher in men than women because of the difference in renal clearance rate.14,15,16 Also, high estradiol concentration was assumed to be one of reasons for lower concentration in women, but the exact mechanism had not yet been clarified.16,17,18 In addition, there was different result of serum uric acid level between pre-menopause and menopause women, because blood estradiol level was changed rapidly during menopausal transition period. This is an important limiting factor for clinical use of serum uric acid as a metabolic marker.
There was a report that serum uric acid increase after menopause,19,20 but it was hard to find a report about correlation of serum uric acid with metabolic syndrome with menopause, especially on Korean population. So, we investigated the possibility of serum uric acid as a predictive marker of metabolic syndrome through clarifying the relationship between uric acid level and metabolic syndrome according to menopausal status for women visited hospital for physical check-up.
Materials and Methods
1. Study population
A total 2,241 women who visited to the health promotion center at Pusan National University hospital between January 2010 and January 2014, were included in this cross-sectional study. Eight hundreds forty six premenopausal and 1,395 menopausal women included. Demographic data were collected at the time of visit. Information on disease history and medication history were obtained with self-report questionnaires and interviews with healthcare providers. We included patients answered questionnaires without exception and excluded patients who had taking a steroid medicine for asthma, arthritis, rheumatic disease. Menopause was defined as patients with history of both ovarian resection and whose last menstrual period was elapsed over one year. In the patients with previous hysterectomy, serum follicle stimulating hormone (FSH) level over 40 mIU/mL was defined as menopause state. All the medical records used for this study were agreed by each patient with consent from at the time of health examination.
2. Anthropometric measurements and laboratory analysis
Height, weight, and abdominal circumference were measured separately and body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Blood pressure (BP) was measured with automatic machine (BP-203 RVII; Colin Corp., Aichi, Japan) in sitting position after taking 10 min break. Systolic and diastolic pressure were measured once and recorded. The blood test was done after 8 hr of overnight fasting. Total cholesterol and uric acid were measured by using Toshiba TBA200FR (TOSHIBA Co., Tokyo, Japan) with enzymatic colorimetric method. Intra-assay and inter-assay coefficients of variation of uric acid were 1.0% and 1.3%. Low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol were directly measured by using Toshiba TBA200FR. Fasting glucose was measured by using glucose oxidase (LX-20; Beckman Coulter, Brea, CA, USA). Coat-A-Count® Insulin was used to measure insulin concentration by solid-phase 125I radioimmunoassay. Thyroid stimulating hormone (TSH) was measured by Coat-A-Count TSH immunoradiometric assay (IRMA), Siemens, and free thyroxine (FT4) was measured by using Coat-A-Count FT4, Siemens. Homeostasis model assessment (HOMA)-IR was calculated by using glucose and insulin level (HOMA-IR = [glucose × insulin] / 405).
3. Diagnostic criteria
As the National Cholesterol Education Program reported in Adult Treatment Panel III, the metabolic syndrome can be defined by applying of three or more inclusion criteria of 5 diagnostic criteria. The diagnostic criteria are; 1) abdominal circumference over 80 cm (for Asian women), 2) Triglyceride level over 150 mg/dL, 3) HDL cholesterol less than 50 mg/dL, 4) fasting blood glucose (FBG) over 110 mg/dL or diabetes-mellitus (DM), and 5) BP over 130/85 or hypertension medication.21
4. Statistical analysis
Statistical Package for Social Sciences (SPSS) for Windows 18.0 program (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. All data were presented as mean ± standard deviation (SD). Student t-test was used for comparison of clinical characteristics in premenopausal and menopausal women, differences of clinical factor according to presence of metabolic syndrome and menopausal status, serum uric acid level in patients with metabolic syndrome and metabolic syndrome components. The correlation between metabolic syndrome and menopause status, age, and serum uric acid were analyzed by multiple logistic regression analysis. Two-sided values of P < 0.05 were considered as statistically significant.
Results
1. Comparisons of clinical characteristics according to menopausal status and metabolic syndrome
There were statistically significant differences in all parameters except TSH between pre-menopausal and menopausal groups (Table 1). Serum uric acid was significantly higher in menopausal group (4.3 ± 0.9, vs. 4.6 ± 1.1, P = 0.00). In menopausal group, 52 patients were current users of hormone therapy.
Table 1.
Clinical characteristics of the subjects
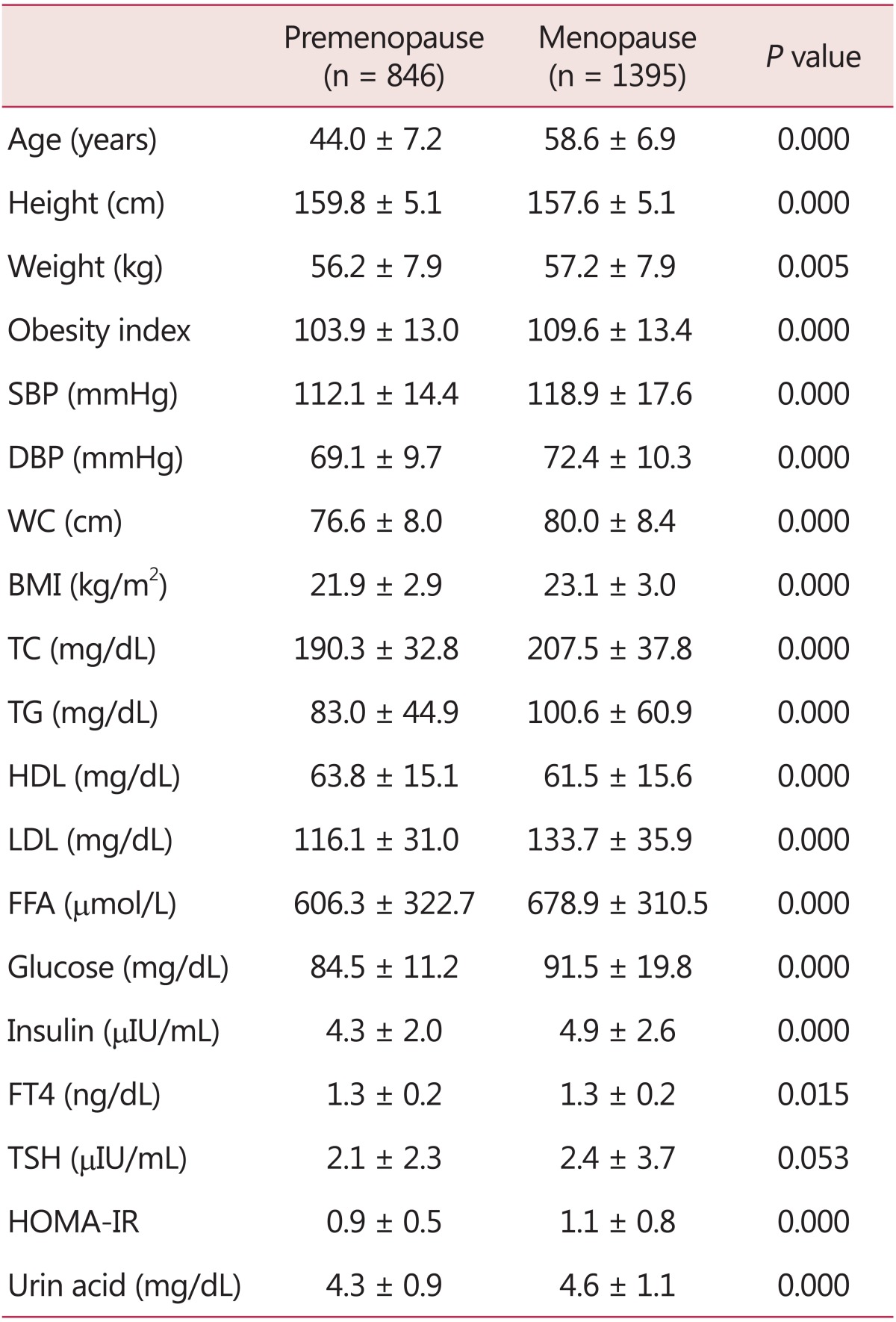
Data are presented as the means ± standard deviation (SD)
P value by student t-test
SBP: systolic blood pressure, DBP: diastolic blood pressure, WC: waist circumference, BMI: body mass index, TC: total cholesterol, TG: triglyceride, HDL: high-density lipoprotein, LDL: low-density lipoprotein, FFA: free fatty acid, FT4: free thyroxine, TSH: thyroid stimulating hormone, HOMA-IR: homeostasis model assessment-insulin resistance
Table 2 shows the differences of parameters according to presence or absence of metabolic syndrome in both groups. Also it presents the differences of parameters of metabolic syndrome patients according to menopause status. In premenopausal group, 63 patients had metabolic syndrome and the prevalence rate was 7.45%. Menopausal group showed higher percentage of metabolic syndrome patients than pre-menopausal group. The prevalence rate of metabolic syndrome in menopause group was 23.87%. There was no significant difference in thyroid hormone, but uric acid was significantly higher in the patients with metabolic syndrome in both groups. However serum uric acid level was not significantly different between premenopausal and menopausal groups in metabolic syndrome patients.
Table 2.
Differences of clinical factor according to presence of metabolic syndrome and menopausal status
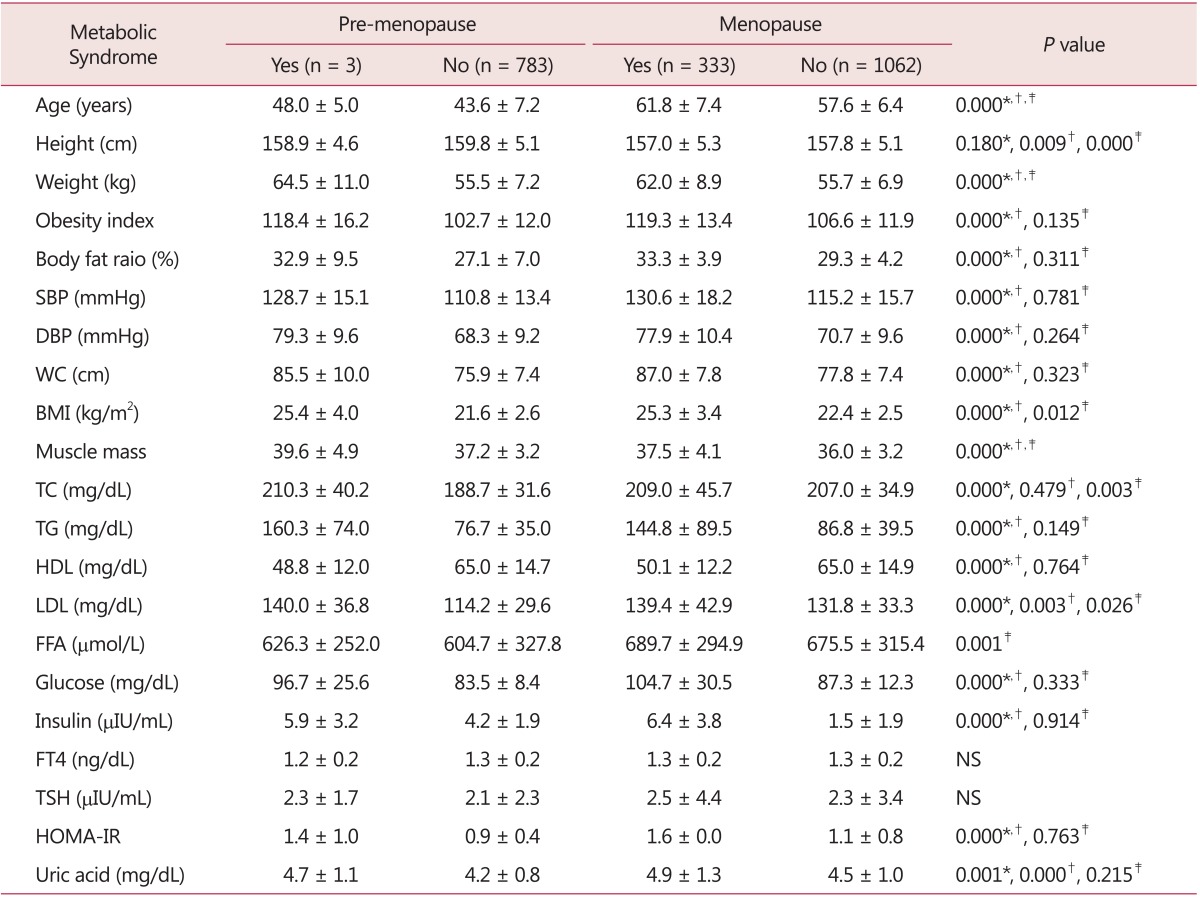
Data are presented as the means ± standard deviation (SD)
P value by student t-test
*between premenopausal groups, †between menopausal groups, ‡between metabolic syndrome groups.
NS: not significant, SBP: systolic blood pressure, DBP: diastolic blood pressure, WC: waist circumference, BMI: body mass index, TC: total cholesterol, TG: triglyceride, HDL: high-density lipoprotein, LDL: low-density lipoprotein, FFA: free fatty acid, FT4: free thyroxine, TSH: thyroid stimulating hormone, HOMA-IR: homeostasis model assessment-insulin resistance
2. Serum uric acid level of patients with metabolic syndrome and metabolic syndrome components
The differences of serum uric acid level according to each metabolic syndrome diagnostic criteria in patients of metabolic syndrome were described in Table 3. There was no statistical difference between premenopausal and menopausal groups.
Table 3.
Serum uric acid level in patients with metabolic syndrome and metabolic syndrome components
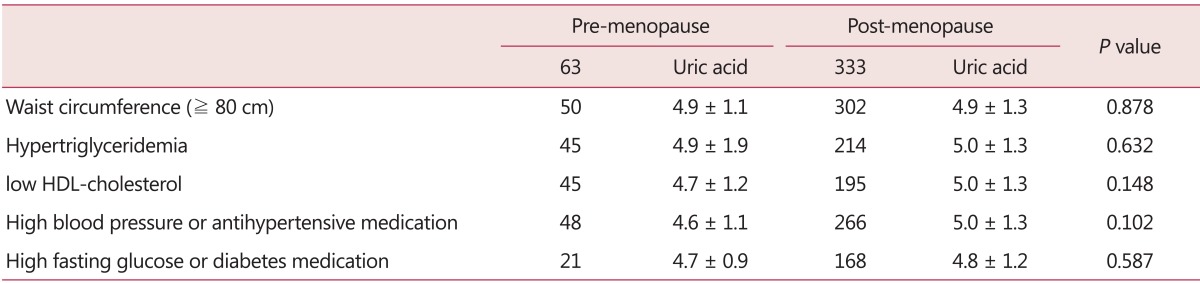
Data are presented as the means ± standard deviation (SD)
P value by student t-test
HDL: high-density lipoprotein
3. Multiple logistic regression analysis of the possible correlates for metabolic syndrome
Serum uric acid, menopause, and age were analyzed by multiple logistic regression analysis. There was no correlation with menopause (odds ratio [OR]: 0.980, 95% confidence interval [CI]: 0.677-1.417, P = 0.913), but age (OR: 1.092, 95% CI: 1.305-1.619, P = 0.000) and serum uric acid (OR: 1.453, 95% CI: 1.074-1.111, P = 0.000) were showed positive correlation with metabolic syndrome (Table 4).
Table 4.
Multiple logistic regression analysis results of the possible correlates for metabolic syndrome
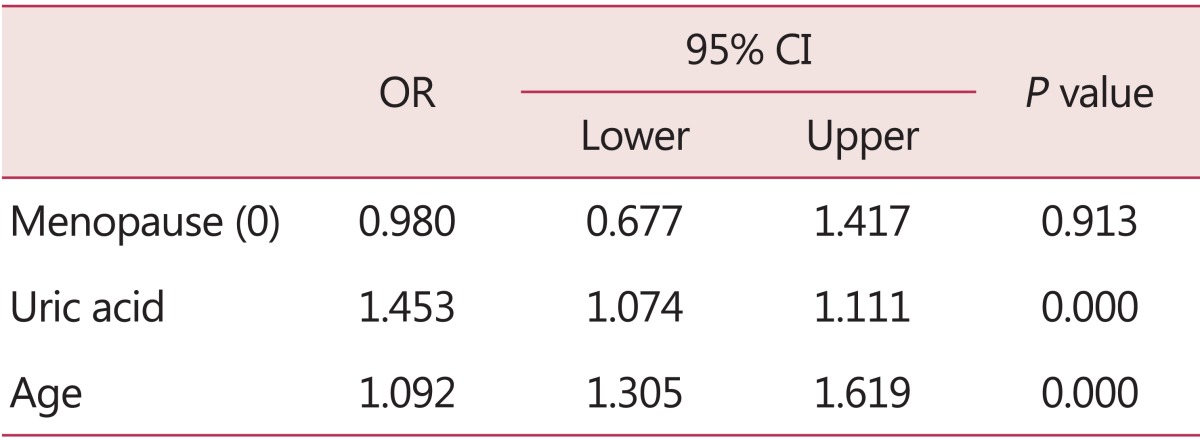
P value by multiple logistic regression
OR: odds ratio, 95% CI: 95% confidence interval
Discussion
This study shows that the prevalence of metabolic syndrome of the premenopausal women was 7.45% (63/843), and that of the menopausal women was 23.87% (333/1,395). These results were similar with the study that investigated the prevalence of metabolic syndrome from 2006 to 2010, which was included 2,832 women who visited Health Promotion Center in Pusan National University Hospital: premenopausal women showed 8.69%, and menopausal women showed 21.85%.22 The prevalence rate of metabolic syndrome from this study was markedly lower than the prevalence of previous study which were 13.0% in Korean premenopausal women23 and 31.2-54.6% in menopausal women.24,25 This was thought to have reflected that since the data of the study was from the health promotion center and the women included in this study could be relatively healthy women or who concerned about their health. The prevalence rate of metabolic syndrome markedly increases for the menopausal women. But since there was a large difference in age between the premenopausal (44.0 ± 7.2 years) and menopausal (58.6 ± 6.9 years) women, analyzing with subdivided aging groups is needed to evaluate factors that affects to the incidence of metabolic syndrome.
In this study, serum uric acid was higher in menopause women. The result of this study about the relationship of menopause and serum uric acid was coincided with the data from the National Health and Nutrition Examination Survey (NHANES III).26 The pathophysiology of higher serum uric acid level in menopausal women is not fully revealed. Some authors claimed that the change of fat distribution during menopausal transition is one of the reasons for increasing serum uric acid.27,28
Cremonini et al.28 reported that trunk body fat mass accumulation is independently associated with higher serum uric acid, and this association is confined to women in menopause.
However, serum uric acid level was not different between premenopausal and menopausal groups in metabolic syndrome patients. Serum uric acid level in pre-menopausal women with metabolic syndrome was 4.7 ± 1.1 mg/dL and in menopausal women with metabolic syndrome was 4.9 ± 1.3 mg/dL (P = 0.215). According to these results, we can assume that serum uric acid level is higher in women who have metabolic syndrome and serum uric acid could be used as the predictive factor of metabolic syndrome regardless of menopausal status.
Also, in the logistic regression analysis, metabolic syndrome had correlation with age and serum uric acid independently. So serum uric acid and age could be used as the predictive factors for metabolic syndrome. Moreover the odds ratio of serum uric acid was higher than that of age (OR 1.453 in serum uric acid and 1.092 in age). The basic mechanism of this relationship is unclear. However, we can postulate some theories. Hyperuricemia could occur in sodium metabolic disorder of kidney and cause injury of kidney. This injury can cause damage to blood vessel and rise of BP.29 Also, serum uric acid can cause increase of oxygen free radical in case of high serum concentration.13
For application of serum uric acid to predict metabolic syndrome in practice, several problems have to be solved. The cut-off value of serum uric acid must be determined. In this study, the prevalence rate of hyperuricemia was 11.11% (7/63) in premenopausal women with metabolic syndrome and 18.32% (61/333) in menopausal women with metabolic syndrome (data was not shown). The predictive value for metabolic syndrome is very low in case of applying hyperuricemic level. So, wider and detailed analyses are needed for determining cut-off value of serum uric acid in each age group.
This study has several limitations. First, the history about pregnancy, lactation, gestational diabetes and polycystic ovary syndrome were not investigated. These factors are related with onset of metabolic syndrome in women.30 There are another limitations in study design and population. It was conducted retrospectively and based questionnaires. Women who visited a health care center in only single institution were included and the prevalence rate of metabolic syndrome was relatively lower than other studies. Also, who taking hormone therapy in menopausal group was not considered in analyzing data. So, it may not be proper to adapt the result to general population.
Nevertheless these limitations, our study has value to show the potential of serum uric acid as a predictive factor of metabolic syndrome. More detailed and large population based study can give us more data the relationship of serum uric acid and metabolic syndrome.
Acknowledgement
All authors have no conflict of interest. This work was supported by Pusan National University Hospital Research Grant 2014.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement Executive summary. Cardiol Rev. 2005;13:322–327. [PubMed] [Google Scholar]
- 3.Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 4.Perlstein TS, Gumieniak O, Williams GH, Sparrow D, Vokonas PS, Gaziano M, et al. Uric acid and the development of hypertension: the normative aging study. Hypertension. 2006;48:1031–1036. doi: 10.1161/01.HYP.0000248752.08807.4c. [DOI] [PubMed] [Google Scholar]
- 5.Nakanishi N, Okamoto M, Yoshida H, Matsuo Y, Suzuki K, Tatara K. Serum uric acid and risk for development of hypertension and impaired fasting glucose or Type II diabetes in Japanese male office workers. Eur J Epidemiol. 2003;18:523–530. doi: 10.1023/a:1024600905574. [DOI] [PubMed] [Google Scholar]
- 6.Tsouli SG, Liberopoulos EN, Mikhailidis DP, Athyros VG, Elisaf MS. Elevated serum uric acid levels in metabolic syndrome: an active component or an innocent bystander? Metabolism. 2006;55:1293–1301. doi: 10.1016/j.metabol.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt MI, Watson RL, Duncan BB, Metcalf P, Brancati FL, Sharrett AR, et al. Clustering of dyslipidemia, hyperuricemia, diabetes, and hypertension and its association with fasting insulin and central and overall obesity in a general population. Atherosclerosis Risk in Communities Study Investigators. Metabolism. 1996;45:699–706. doi: 10.1016/s0026-0495(96)90134-1. [DOI] [PubMed] [Google Scholar]
- 8.Yoo TW, Sung KC, Shin HS, Kim BJ, Kim BS, Kang JH, et al. Relationship between serum uric acid concentration and insulin resistance and metabolic syndrome. Circ J. 2005;69:928–933. doi: 10.1253/circj.69.928. [DOI] [PubMed] [Google Scholar]
- 9.Conen D, Wietlisbach V, Bovet P, Shamlaye C, Riesen W, Paccaud F, et al. Prevalence of hyperuricemia and relation of serum uric acid with cardiovascular risk factors in a developing country. BMC Public Health. 2004;4:9. doi: 10.1186/1471-2458-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vuorinen-Markkola H, Yki-Järvinen H. Hyperuricemia and insulin resistance. J Clin Endocrinol Metab. 1994;78:25–29. doi: 10.1210/jcem.78.1.8288709. [DOI] [PubMed] [Google Scholar]
- 11.Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metabolism. 2008;57:845–852. doi: 10.1016/j.metabol.2008.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen LK, Lin MH, Lai HY, Hwang SJ, Chiou ST. Uric acid: a surrogate of insulin resistance in older women. Maturitas. 2008;59:55–61. doi: 10.1016/j.maturitas.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Lippi G, Montagnana M, Franchini M, Favaloro EJ, Targher G. The paradoxical relationship between serum uric acid and cardiovascular disease. Clin Chim Acta. 2008;392:1–7. doi: 10.1016/j.cca.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 14.Wolfson WQ, Hunt HD, et al. The transport and excretion of uric acid in man; a sex difference in urate metabolism; with a note on clinical and laboratory findings in gouty women. J Clin Endocrinol Metab. 1949;9:749–767. doi: 10.1210/jcem-9-8-749. [DOI] [PubMed] [Google Scholar]
- 15.Scott JT, Pollard AC. Uric acid excretion in the relatives of patients with gout. Ann Rheum Dis. 1970;29:397–400. doi: 10.1136/ard.29.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicholls A, Snaith ML, Scott JT. Effect of oestrogen therapy on plasma and urinary levels of uric acid. Br Med J. 1973;1:449–451. doi: 10.1136/bmj.1.5851.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sumino H, Ichikawa S, Kanda T, Nakamura T, Sakamaki T. Reduction of serum uric acid by hormone replacement therapy in postmenopausal women with hyperuricaemia. Lancet. 1999;354:650. doi: 10.1016/S0140-6736(99)92381-4. [DOI] [PubMed] [Google Scholar]
- 18.Antón FM, García Puig J, Ramos T, González P, Ordás J. Sex differences in uric acid metabolism in adults: evidence for a lack of influence of estradiol-17 beta (E2) on the renal handling of urate. Metabolism. 1986;35:343–348. doi: 10.1016/0026-0495(86)90152-6. [DOI] [PubMed] [Google Scholar]
- 19.Wingrove CS, Walton C, Stevenson JC. The effect of menopause on serum uric acid levels in non-obese healthy women. Metabolism. 1998;47:435–438. doi: 10.1016/s0026-0495(98)90056-7. [DOI] [PubMed] [Google Scholar]
- 20.Rho YH, Woo JH, Choi SJ, Lee YH, Ji JD, Song GG. Association between serum uric acid and the Adult Treatment Panel III-defined metabolic syndrome: results from a single hospital database. Metabolism. 2008;57:71–76. doi: 10.1016/j.metabol.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 21.National Cholesterol Education Program Expert Panel on Detection Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 22.Joo JK, Son JB, Jung JE, Kim SC, Lee KS. Differences of prevalence and components of metabolic syndrome according to menopausal status. J Korean Soc Menopause. 2012;18:155–162. [Google Scholar]
- 23.Jeon SK, Hong HR, Yi KW, Park HT, Shin JH, Lee NW, et al. Relationship between metabolic syndrome and bone mineral density in middle-aged women. J Korean Soc Menopause. 2010;16:142–147. [Google Scholar]
- 24.Kim HM, Park J, Ryu SY, Kim J. The effect of menopause on the metabolic syndrome among Korean women: the Korean National Health and Nutrition Examination Survey, 2001. Diabetes Care. 2007;30:701–706. doi: 10.2337/dc06-1400. [DOI] [PubMed] [Google Scholar]
- 25.Cho GJ, Park HT, Shin JH, Kim T, Hur JY, Kim YT, et al. The relationship between reproductive factors and metabolic syndrome in Korean postmenopausal women: Korea National Health and Nutrition Survey 2005. Menopause. 2009;16:998–1003. doi: 10.1097/gme.0b013e3181a03807. [DOI] [PubMed] [Google Scholar]
- 26.Hak AE, Choi HK. Menopause, postmenopausal hormone use and serum uric acid levels in US women-the Third National Health and Nutrition Examination Survey. Arthritis Res Ther. 2008;10:R116. doi: 10.1186/ar2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ozbey N, Sencer E, Molvalilar S, Orhan Y. Body fat distribution and cardiovascular disease risk factors in pre- and postmenopausal obese women with similar BMI. Endocr J. 2002;49:503–509. doi: 10.1507/endocrj.49.503. [DOI] [PubMed] [Google Scholar]
- 28.Cremonini E, Bonaccorsi G, Bergamini CM, Castaldini C, Ferrazzini S, Capatti A, et al. Metabolic transitions at menopause: in post-menopausal women the increase in serum uric acid correlates with abdominal adiposity as assessed by DXA. Maturitas. 2013;75:62–66. doi: 10.1016/j.maturitas.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 29.Schachter M. Uric acid and hypertension. Curr Pharm Des. 2005;11:4139–4143. doi: 10.2174/138161205774913246. [DOI] [PubMed] [Google Scholar]
- 30.Han M. Metabolic syndrome emerging from menopause. J Korean Soc Menopause. 2011;17:127–135. [Google Scholar]


