Abstract
Background: Stigma is a major barrier to health care access and impacts the quality of life for individuals affected by tuberculosis (TB). Assessing TB stigma is essential to addressing health disparities. However, no such instrument was available in Mexico at the time of our study. This study examined the adaptability of the TB and human immunodeficiency virus (HIV) stigma scales previously used in Thailand.
Methods: The original scale, developed in English, was linguistically adapted to Spanish and administered to 217 individuals affected by TB in five states in Mexico. The TB-HIV stigma subscales were designed to assess individual and community perspectives. Additional data collected included general information and socio-demographics. Assessment of psychometric properties included basic statistical tests, evaluation of Cronbach's alpha and factor analysis.
Results: We found no significant statistical differences associated with higher stigma scores by location, age, marital status, education and stigma scores. Factor analysis did not create any new factors. Internal consistency reliability coefficients were satisfactory (Cronbach α = 0.876–0.912).
Conclusion: The use of the stigma scales has implications for 1) health improvements, 2) research on stigma and health disparities, and 3) TB and HIV stigma interventions. Further research is needed to examine transferability among larger and randomly selected Spanish-speaking populations.
Keywords: tuberculosis, stigma, measurement, Mexico
Abstract
Contexte : La stigmatisation est un obstacle majeur à l'accès aux soins de santé et elle altère la qualité de vie des personnes affectées par la tuberculose (TB). L'évaluation de cette stigmatisation relative à la TB a un rôle crucial dans la lutte contre les disparités sanitaires. Cependant, aucun instrument de mesure n'était disponible au Mexique à l'époque de notre étude. Cette étude a examiné l'adaptabilité des échelles de stigmatisation de la TB et du virus de l'immunodéficience humaine (VIH) utilisées jusqu'alors en Thaïlande.
Méthodes : L'échelle originale, élaborée en anglais, a été adaptée à la langue espagnole et soumise à 217 personnes affectées par la TB dans cinq états du Mexique. Les sous-échelles de stigmatisation relatives à la TB et au VIH ont été conçues afin d'évaluer les perspectives des individus et de la communauté. Des données supplémentaires générales et sociodémographiques ont été recueillies. L'évaluation des propriétés psychométriques incluaient les tests statistiques de base, l'évaluation du coefficient alpha de Cronbach et l'analyse factorielle.
Résultats : Nous n'avons pas trouvé de différence statistiquement significative associée à une stigmatisation plus importante en fonction du lieu, de l'âge, du statut marital, du niveau d'instruction et des scores de stigmatisation. L'analyse factorielle n'a pas créé de nouveaux facteurs. Les coefficients de fiabilité de la cohérence interne ont été satisfaisants (Cronbach α = 0,876 à 0,912).
Conclusion : L'utilisation des échelles de stigmatisation a des implications pour 1) l'amélioration de la santé ; 2) la recherche relative à la stigmatisation et aux disparités en matière de santé ; et 3) des interventions relatives à la stigmatisation du VIH et de la TB. D'autres recherches sont requises afin d'étudier la possibilité de transférer cette méthode dans des populations hispanophones plus importantes et sélectionnées au hasard.
Abstract
Antecedentes: El estigma es un gran obstáculo para el acceso a la salud y afecta la calidad de vida de las personas con tuberculosis (TB). Evaluar el estigma relacionado con la TB es esencial para abordar las desigualdades. Dicho instrumento no estaba disponible en México en el momento del estudio. Se examinó la adaptabilidad de las escalas de estigma de TB y del virus de la inmunodeficiencia humana (VIH) utilizadas anteriormente en Tailandia.
Métodos: La escala original, desarrollada en inglés, fue lingüísticamente adaptada al español y administrada a 217 personas afectadas por la TB en cinco estados de México. Las sub-escalas fueron diseñadas para evaluar las perspectivas individuales y comunitarias. Recopilación de datos generales, evaluación de propiedades psicométricas y alfa de Cronbach, pruebas estadísticas básicas, y análisis factorial.
Resultados: No encontramos diferencias estadísticas significativas asociadas con valores altos de estigma por ubicación, edad, estado civil, educación y calificaciones de estigma. El análisis factorial no creó nuevos factores. Los coeficientes de confiabilidad de consistencia interna fueron satisfactorios (Cronbach α = 0.876 a 0.912).
Conclusión: Las implicaciones de uso de las escalas de estigma para: 1) mejoras de salud; 2) investigación en estigma; e 3) intervenciones. Se necesitan investigaciones adicionales para examinar la transferibilidad entre las poblaciones de habla hispana en una muestra mayor al azar.
Stigma associated with tuberculosis (TB) has been identified as a major barrier to health care and quality of life in TB management.1 Stigma is a social process that exists when elements of labeling, stereotyping, separation, loss of status, and discrimination occur in a power situation that allows them.2,3 Falk distinguishes between two types of stigmatization conditions based on the ‘cause or root’: ‘existential’ is when the individual did not cause the stigma or has little or no control over it, and ‘achieved’ is when a person earns the stigma because of conduct or because the individual contributed to attaining it.4
Stigma is increasingly recognized as having a major impact on public health interventions and a tendency to produce social inequality.5,6 Occasionally, the impact of stigma is positive, especially when individuals being stigmatized successfully adopt an ‘empowerment’ model as opposed to a ‘coping’ model.7 Stigma and fear of discrimination usually lead to delay in seeking health services, prolonged risk of transmission, poorer adherence and increased risk of disability, and drug resistance, with women bearing the highest burden of avoiding behaviors.8,9 Stigma and discrimination are created by multiple forces, including a lack of understanding of the disease, myths about transmission, prejudice, irresponsible media reporting, and the link between the human immunodeficiency virus/acquired immune-deficiency syndrome (HIV/AIDS) and TB, as well as a fear of relating the illness to disability and death.3,10
Prejudice and discrimination by health personnel or society may result in isolation and decreased self-esteem of the individual affected by TB, thereby impeding that person's potential for empowerment.11,12 Stigma and discrimination related to TB can take different forms and are manifested at different levels — societal, community and individual — and in different contexts. Health stigma remains a difficult concept to measure. It involves interaction between those who are healthy and those who are infected or appear to be infected.13,14
Measurement of health-related stigma
Much of the literature cites the complexity of stigma related to TB and other health conditions such as HIV/AIDS and its diversity in cultural settings as the core reason for the limited response to the phenomenon.15,16 Van Rie and colleagues noted that the cross-cultural generalizability of TB and HIV/AIDS stigma scales used in Thailand may be limited.17 They further hypothesized that the difference in the concept of stigma across cultural contexts is more reflective of ‘nuances and degree rather than substance’. TB in Mexico is not different from TB in Thailand. In a systematic review of the psychometric assessment of stigma instruments, Van Rie et al.'s scale rated positively on content validity, internal consistency, reliability, and floor and ceiling effects.18 We therefore decided to assess TB stigma using Van Rie et al.'s TB and HIV/AIDS stigma scales, with their approval, to evaluate for potential cross-cultural adaptation in Mexico.
METHODS
This study is a cross-sectional analysis of a convenience sample of 217 individuals of both sexes affected by TB and on treatment or who had completed treatment in the past 6 months in five study locations in Mexico. The study focused on persons affected by TB, regardless of their HIV status.
Ethics
Approval for this study was obtained from the Institutional Review Board of the University of Texas at El Paso.
Study setting
Mexico has a population of 112 337 000, with a male/female ratio of 95.4:100 and a median age of 26 years.19 The incidence rate of pulmonary TB in 2013 in Mexico was 13.6 per 100 000 population.20 TB and HIV co-morbidity is well documented globally. The incidence rate of HIV/AIDS and TB co-infection in 2010 was 8.7/100 000.21
Experienced, trained interviewers conducted face-to-face interviews using the TB and HIV/AIDS stigma scales that had been linguistically adapted to Spanish from the English version by Van Rie et al.17 The criteria for selecting five sites included highest risk of TB, higher prevalence of TB than national rates, and presence of the SOLUCION TB Project. The locations included three cities in the north (Tijuana, Ciudad Juarez, and Reynosa), one in the central region (Guadalajara), and one in the south (Tuxtla Gutierrez).
Inclusion criteria
The focus of the study is on TB. Participants consisted of individuals aged ⩾18 years of both sexes on treatment for TB, who had completed treatment in the past 6 months, regardless of their HIV status. Participation was voluntary. Participants with active TB were not interviewed due to the risk of exposing themselves or others to additional risk during the interview.
Sample
The sample size for this study was obtained using Epi Info v6 software (Centers for Disease Control and Prevention, Atlanta, GA, USA, 2014). Systematic sampling was used based on the assumption that the TB cases represent each of the three geographical regions in Mexico from which all the cases came. The sample was increased by 18% based on assumptions, non-response of 5%, and non-participation of 10%. The sample for each location varied, based on prevalence rates and case number.
Instrument
The standardized questionnaire included general and socio-demographic data, perception of support during treatment and the sub-scales of Van Rie et al. These scales were first linguistically adapted into Spanish, back-translated by the University Department of Linguistics and field-tested for comprehension among a sample of 30 individuals affected by TB and recruited by the SOLUCION TB Project.
Interview locations and schedule
The scales were administered at a health clinic or TB program office. The questionnaires were administered between January and February 2009.
Data entry
Data entry was conducted using SPSS Version 15.0.1.1 (SPSS, Chicago, IL, USA, 2007). The 45 stigma scale items were scored on a four-point Likert scale.22 The raw scores were mathematically computed into a standardized summary score (SS50) so that the level of stigma on each of the subscales would be between 0 and 50, with the highest scores representing higher stigma.
Statistical analysis
The descriptive data analysis focused on frequencies and cross-tabulations of key variables, which were used to detect relationships between the dependent variable (stigma) and the independent variables being surveyed (e.g., site, age, sex, education, and occupation). A factor analysis was performed for the 45 items of the scales. No items were excluded using SPSS V15.
A factor analysis was conducted using the principal component factor extraction method on the selected set of items to identify the factors and factor loadings.17,23 The oblique rotation method was used when the correlation between factors was > 0.40, and the orthogonal rotation method in situations where the loading factors were <0.40. The first round of un-rotated factor analysis yielded screen plots to determine the number of factors underlining the TB and HIV/AIDS stigma scales, followed by rounds of factor analysis, with rotations to provide a relationship among these items for each factor. Items with absolute value loading of ⩾0.40 were identified. Estimates were conducted of the correlation among the variables of the four stigma scales by means of the internal consistency of the variables, using the Cronbach's α statistic. A scale α ⩾0.7 was considered to have a good to excellent reliability.24 We assumed that the 45 items in the four scales were linearly related to the total score. Tukey's test of non-additivity was used to assess that there was no interaction between the cases and the items at the 0.95% level.
RESULTS
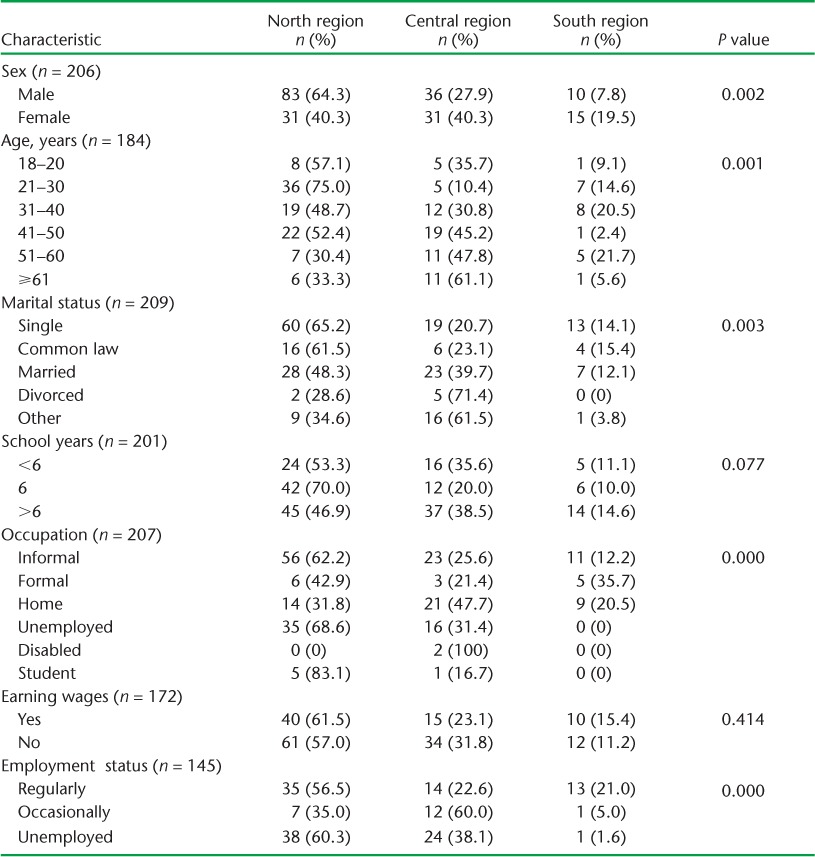
The distribution of the characteristics across participants by region with their respective probability values (P values) are shown in Table 1. The following participant characteristics show statistically significant differences (P < 0.05): perceived health status at the time of interview, health insurance type, employment status, occupation, marital status, age group, and sex.
TABLE 1.
Participant demographics by study location
Standardized stigma scores
The scores were distributed normally, with mean scores (± standard deviation [SD]) of 28.9 (±8.7) for community perspectives of TB; 28.3 (±8.2) for the person affected by TB; 29.4 (±9.0) for community perspectives of HIV/AIDS; and 34.3 (±7.5) for persons affected by TB perspectives toward HIV/AIDS scales. These results compared well to the study by Van Rie et al.17
Factor analysis
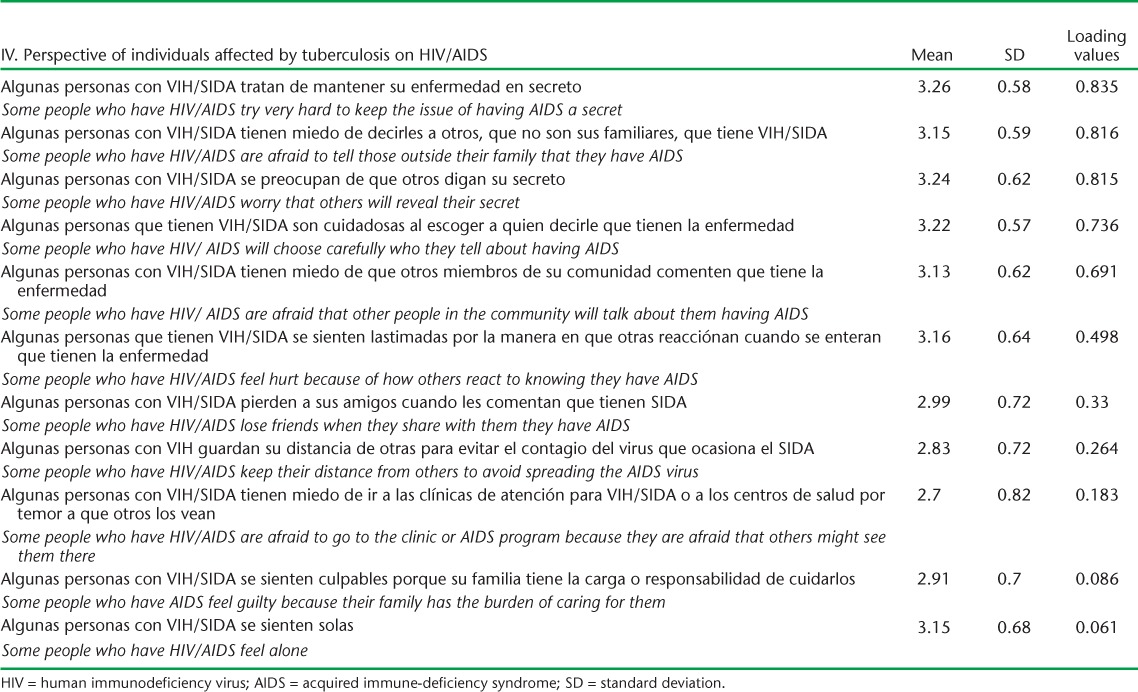
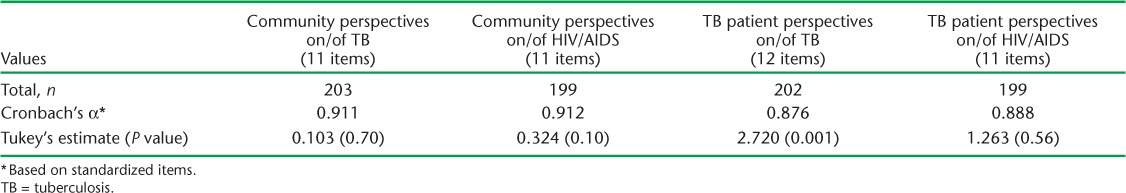
Factor analysis demonstrated high loadings of most items (⩾0.40). Items with an absolute value loading of ⩾0.40 have relatively greater importance.17,25,27 Tables 2–5 present the two stigma subscales.
TABLE 2.
Absolute loading values for TB stigma scales by item of importance
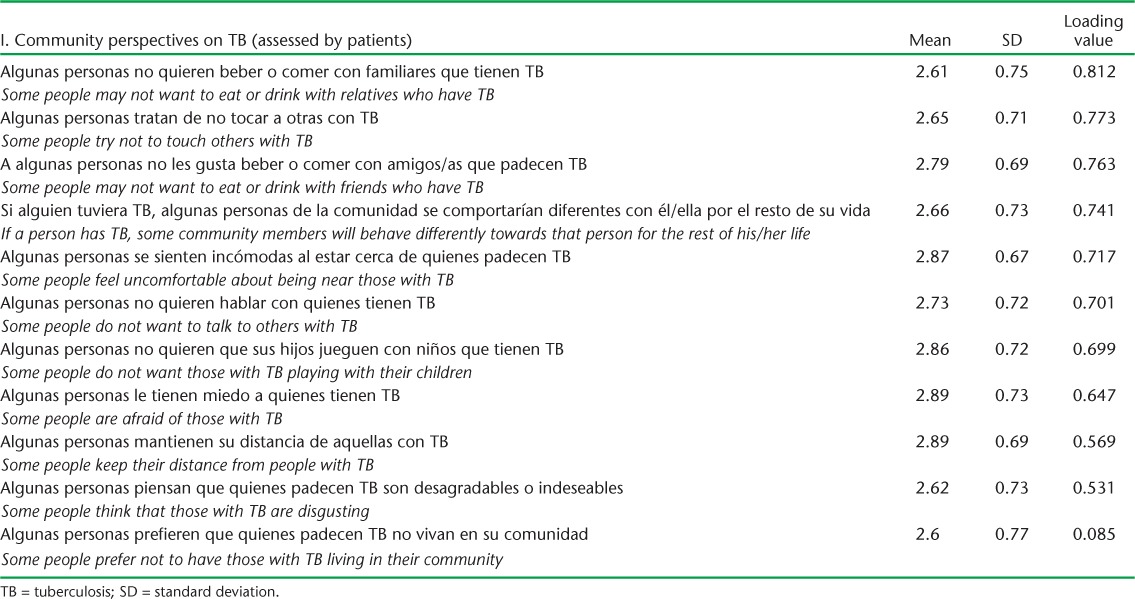
TABLE 3.
Absolute loading values for TB stigma scales by item of importance
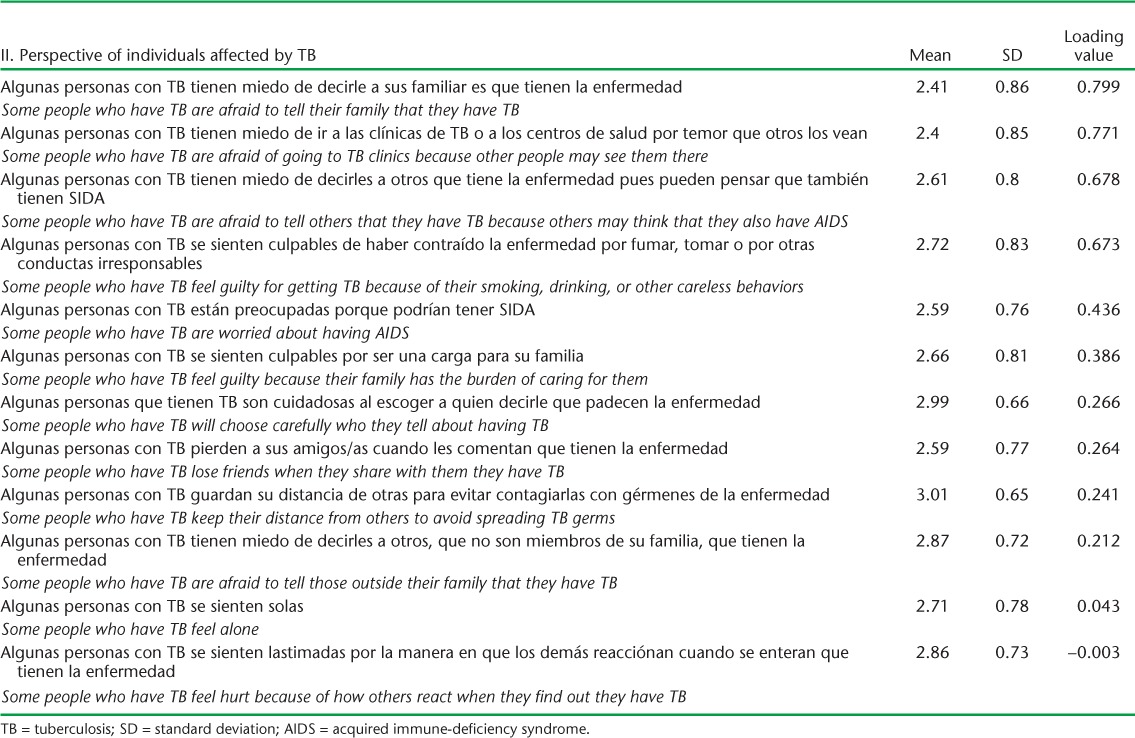
TABLE 4.
Absolute loading values for HIV/AIDS related stigma scales by item of importance
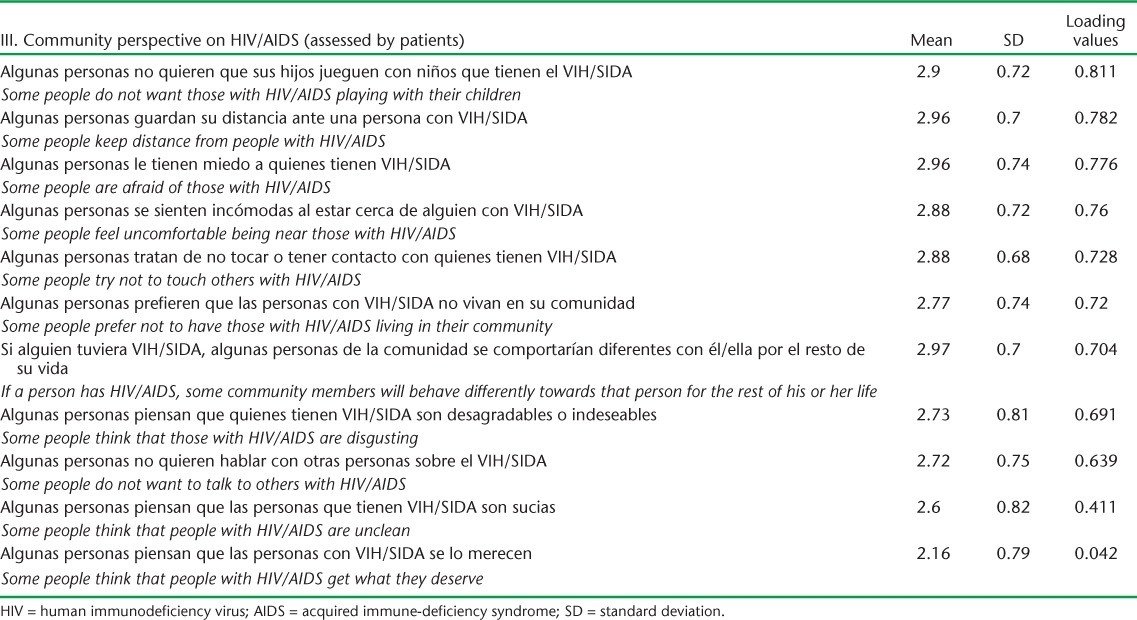
TABLE 5.
Absolute loading values for HIV/AIDS related stigma scales by item of importance
Factors associated with tuberculosis stigma
The effect measures of adjusted mean differences (MD) along with 95% confidence intervals (CI) from summed stigma scores are small, <1 in the relative scale; most of these effects are not consistent across the scales and few were statistically significant, as shown in Table 6. Table 2 illustrates the score distribution and Cronbach's α values for the subscales.
TABLE 6.
Score distributions and Cronbach's α values for communities and individuals affected by TB and HIV/AIDS stigma-related scales
DISCUSSION
The results of the study determined that the scales developed and validated by Van Rie et al. and linguistically adapted to Spanish for this study have good overall internal consistency, reliability, and psychometric characteristics among the sub-populations studied.
Similarities and differences between tuberculosis and HIV/AIDS stigma
Understanding stigma associated with HIV/AIDS and TB is essential to address the social exclusion of individuals and groups impacted and affected by HIV/AIDS and/or TB. HIV-related stigma is sometimes layered and compounded in addition to existing TB stigma. The results also identified some similarities between the stigma related to TB and HIV/AIDS. Items related to fear of infection through casual contact, such as eating or drinking with relatives and friends and touching others, were the most significant determinants of stigma in both TB and HIV/AIDS, based on the absolute loading factors. The item ‘Some people do not want those with HIV/AIDS playing with their children’ loaded third highest, which is interesting given the important differences in the modes of transmission between TB and HIV/AIDS. The investigation revealed that participants living with TB perceived that the community stigmatizes because of how TB is contracted and how persons affected with TB are perceived as vectors of a disease such as TB, and therefore they should be kept away to avoid infection or transmission. The item on TB patient perceptions toward HIV/AIDS, ‘Some people who have HIV/AIDS keep their distance from others to avoid spreading the AIDS virus’, loaded low. This can probably be explained by reflecting the knowledge and understanding of how HIV is transmitted. The results also identify some similarities between the stigma related to TB and HIV/AIDS. Items related to fear of infection through casual contact (eating or drinking with relatives and friends or touching others) were the most significant determinants of stigma in both TB and HIV/AIDS, based on the absolute loading factors. The same item for TB loaded high.
Disclosure and guilt
The dimension of disclosure or secrecy of either of the two conditions was prominent. In both the TB and the HIV/AIDS scales, the item ‘Some people who have TB (or HIV/AIDS) are afraid to tell their family (or those outside their family) that they have the condition’ loaded high. Maintaining the diagnosis of TB (or HIV/AIDS) confidential also rated very high. These perceptions indicate that moral judgment and fear of disclosure are associated with delayed care and stigmatization.
The concept of guilt was stated in the following items: ‘Some people who have TB feel guilty about getting the disease because of their smoking, drinking and other careless behaviors’ and ‘Some people think that those with TB (or HIV/AIDS) are disgusting.’ The HIV/AIDS scale item: ‘Some people prefer not to have those with HIV/AIDS living in their community’ indicated strong moral values and norms as well as punishment and judgment. Discrimination perceptions were also disclosed: ‘If a person has HIV/AIDS (or TB), some community members will behave differently toward the person for the rest of his/her life’ or ‘Some people do not want to talk to others with HIV/AIDS.’ Shame or guilt could be a root cause in delaying timely access to health services, as expressed in the following item: ‘Some people with TB are afraid of going to TB clinics because other people may see them there.’ This item suggests that there may be embarrassment and judgment involved in having TB and seeking care from a TB clinic.
Individuals aged ⩽21 years had lower TB and HIV stigma in both subscales than older people. Participants living in a marital or partnership relationship seemed to indicate lower stigma perceptions on all scales, consistent with other studies.27,28 Some studies have indicated that financial problems and economic distress were found to increase stigma.27,29 The less educated the participants, the more perceived stigma was found in this study. This finding has important implications for developing health literacy interventions to reduce stigma, primarily among orally literate participants.
This study served as groundwork for the first Tuberculosis Knowledge, Attitudes and Practices National Survey in Mexico (2010), which included the 23-item TB stigma subscale. The first author is currently working on these data, a sample of 1250 individuals (not affected by TB) in five locations in Mexico, to measure community members' perspective on TB.
Limitations
The study had some limitations. We focused on one particular population, namely those affected by TB, and captured affected individuals' self-perceived and individual forms and manifestations of stigma related to TB and not community perspectives. It is also possible that stigma is present in other sub-groups, such as persons affected by TB and not in treatment. We did not inquire about the participants' HIV status. We can only infer that a sample of those in the study was affected by HIV, due to the local data on incidence and prevalence of HIV. We encourage further understanding of stigma among those affected by HIV/AIDS. Second, there is no gold standard for measuring TB stigma. A more complete assessment of stigma would require the use of standardized, quantitative instruments, extensive interviews and qualitative analysis. The study does not offer sufficient data to assess the true meaning of the stigma scores of the scales. The sample was not randomly selected, which limits the ability to apply it to the general TB patient population or to draw conclusions about the impact of perceptions of stigma related to TB and HIV/AIDS in Mexico. Third, differences in language and culture need to be assessed.
CONCLUSIONS
The study findings will help move from understanding stigma to implementing reduction interventions to mitigate the impact of stigma and promote empowerment. TB and HIV/AIDS stigma are linked to the actions and attitudes of individuals and communities. To mitigate stigma, interventions should be multidimensional and address underlying social processes. Drawing on the experiences of advocacy, communication and social mobilization rather than individual behavior change is important. Strategies that focus on personal empowerment of marginalized groups are essential. Effective methods to mitigate stigma are those that engage the affected communities in addressing stigma, such as Photovoice projects, support groups, and media campaigns. The findings can serve as the basis for stigma measurement research with Spanish-speaking populations in other countries. Developing a generic set of stigma assessment instruments, given the similarity in the consequences of stigma in various cultural settings and crosscutting applicability, needs to be researched.
Acknowledgments
The authors thank the many people that made this research possible, in particular SOLUCION TB PCI, M C Joya, Director of the Mexico National TB Program, the local and state TB programs in the study locations, M Lush, R Lacson, and those affected by TB who participated in this study.
This study was supported by a grant from the University of Texas at El Paso College of Health Sciences Graduate Traineeship Program.
Footnotes
Conflicts of interest: none declared.
References
- 1.Courtwright A, Turner A N. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(Suppl):34–42. doi: 10.1177/00333549101250S407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Juniarti N, Evans D. A qualitative review: the stigma of tuberculosis. J Clinical Nurs. 2011;20:1961–1970. doi: 10.1111/j.1365-2702.2010.03516.x. [DOI] [PubMed] [Google Scholar]
- 3.Bond V, Nyblade L. The importance of addressing the unfolding TB-HIV stigma in high HIV prevalence settings. J Community Appl Soc Psychol. 2006;16:452–461. [Google Scholar]
- 4.Falk G. Stigma: how we treat outsiders. New York, NY, USA: Prometheus Books; 2001. [Google Scholar]
- 5.Deacon H. Towards a sustainable theory of health-related stigma: lessons from the HIV/AIDS literature. J Community Appl Soc Psychol. 2006;16:418–425. [Google Scholar]
- 6.Farmer P. California Series in Public Anthropology. Ewing, NJ, USA: University of California Press; 2005. Pathologies of power. Health, human rights, and the new war on the poor. [Google Scholar]
- 7.Shih M. Positive stigma: examining resilience and empowerment in overcoming stigma. Ann Am Acad Polit Soc Sci. 2004;591:175–185. [Google Scholar]
- 8.Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11:353–363. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- 9.Kurspahić-Mujcić A, Hasanović A, Sivić S. Tuberculosis related stigma and delay in seeking care after the onset of symptoms associated with tuberculosis. Med Glas (Zenica) 2013;10:272–277. [PubMed] [Google Scholar]
- 10.Moya E, Lusk M. Tuberculosis stigma and perceptions in the US-Mexico border. Salud Publica Mex. 2013;55:498–507. doi: 10.21149/spm.v55s4.5155. [DOI] [PubMed] [Google Scholar]
- 11.Macq J, Solis A, Martinez G, Martiny P. Tackling tuberculosis patients' internalized social stigma through patient centred care: an intervention study in rural Nicaragua. BMC Public Health. 2008;8:154. doi: 10.1186/1471-2458-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gebremariam M K, Bjune G A, Frich J C. Barriers and facilitators of adherence to TB treatment in patients on concomitant TB and HIV treatment: a qualitative study. BMC Public Health. 2010;10:651–659. doi: 10.1186/1471-2458-10-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kipp A M, Pungrassami P, Nilmanat K et al. Socio-demographic and AIDS-related factors associated with tuberculosis stigma in southern Thailand: a quantitative, cross-sectional study of stigma among patients with TB and healthy community members. BMC Public Health. 2011;11:675. doi: 10.1186/1471-2458-11-675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang S H, Cataldo J K. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis. 2014;18:168–173. doi: 10.5588/ijtld.13.0181. [DOI] [PubMed] [Google Scholar]
- 15.Saad T, Tirkey A. Tuberculosis associated stigma among patients attending outpatient in Medical College Hospital in Sagar (Madhya Pradesh) in Central India. J Med Health Sci. 2014;3:126–131. [Google Scholar]
- 16.Tardin A, Dominicé Dao M, Ninet B, Janssens J P. Tuberculosis cluster in an immigrant community: case identification issues and a transcultural perspective. Trop Med Int Health. 2009;14:995–1002. doi: 10.1111/j.1365-3156.2009.02325.x. [DOI] [PubMed] [Google Scholar]
- 17.Van Rie A, Sengupta S, Pungrassami P et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: exploratory and confirmatory factor analyses of two new scales. Trop Med Int Health. 2008;13:21–30. doi: 10.1111/j.1365-3156.2007.01971.x. [DOI] [PubMed] [Google Scholar]
- 18.Stevelink S A, Wu I C, Voorend W, Brakel W. The psychometric assessment of internalized stigma instruments: a systematic review. Stigma Research and Action. 2012:2. [Google Scholar]
- 19.Instituto Nacional de Estadistica y Geografia. Censos y Conteos de Poblacion y Vivienda 2010. Mexico: Instituto Nacional de Estadistica y Geografia; 2014. [Google Scholar]
- 20.Castellanos M. Personal conversation on March 28, 2014. In: Moya E, editor. Mexico DF: CENAVESE; 2014. [Google Scholar]
- 21.Mexico National TB Program (CENAPRECE SdSeM) Data provided by Martin Castellanos Joya. In: Moya E, editor. El Paso, TX: University of Texas - El Paso; 2014. [Google Scholar]
- 22.Likert R. A theory for the measurement of attitudes. Archives of Psychology. 1932;140:1–55. [Google Scholar]
- 23.Harlow L L. Using multivariate statistics. Structural Equation Modeling Journal. (4th ed) 2002;9:621. [Google Scholar]
- 24.Nunnally J. Psychometric theory. New York, NY, USA: McGraw-Hill; 1978. [Google Scholar]
- 25.Raubenheimer J. An item selection procedure to maximise scale reliability and validity. SA Journal of Industrial Psychology. 2004;30:4. [Google Scholar]
- 26.Sengupta S, Pungrassami P, Balthip Q et al. Social impact of tuberculosis in southern Thailand: views from patients, care providers and the community. Int J Tuberc Lung Dis. 2006;10:1008–1012. [PubMed] [Google Scholar]
- 27.Weiss M G, Somma D, Thomas B E et al. Gender and socio-cultural determinants of TB-related stigma in Bangladesh, India, Malawi and Colombia. Int J Tuberc Lung Dis. 2008;12:856–866. [PubMed] [Google Scholar]
- 28.Gerrish K, Naisby A, Ismail M. The meaning and consequences of tuberculosis among Somali people in the United Kingdom. J Adv Nurs. 2012;68:2654–2663. doi: 10.1111/j.1365-2648.2012.05964.x. [DOI] [PubMed] [Google Scholar]
- 29.Murray E J, Bond V A, Marais B J, Godfrey-Faussett P, Ayles H M, Beyers N. High levels of vulnerability and anticipated stigma reduce the impetus for tuberculosis diagnosis in Cape Town, South Africa. Health Policy Plan. 2013;28:410–418. doi: 10.1093/heapol/czs072. [DOI] [PubMed] [Google Scholar]


