Abstract
Aim: Persistent or recurrent pain after hysterectomy is one of the most frustrating clinical scenarios in benign gynaecology. We attempt to review the current evidence regarding the recurrence of pelvic pain after hysterectomy for endometriosis. The impact of ovarian conservation, type of hysterectomy and the extent of surgical excision were analysed.
Methods: Peer reviewed published manuscripts in the English language in the period between 1980 and 2014 were reviewed using Pubmed and science direct regarding the incidence, causes and recurrence of endometriosis.
Results: Sixty-seven articles were identified. Incomplete excision of endometriosis is the most predominant reason in the literature for the recurrence of endometriosis, and the type of Hysterectomy affects the recurrent symptoms mainly by impacting the extent of excision of the lesion. Ovarian cyst drainage is associated with the highest rate of ovarian cyst reformation within three to six months after surgery. The use of hormone replacement therapy is associated with recurrence of pelvic pain in 3.5% of cases. No studies addressed the recurrence of endometriosis after standard vs robotic assisted hysterectomy.
Conclusion: A high recurrence rate of 62% is reported in advanced stages of endometriosis in which the ovaries were conserved. Ovarian conservation carries a 6 fold risk of recurrent pain and 8 folds risk of reoperation. The decision has to be weighed taking into consideration the patient’s age and the impact of early menopause on her life style. The recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease. Surgical effort should always aim to eradicate the endometriotic lesions completely to keep the risk of recurrence as low as possible.
Keywords: Endometriosis, hysterectomy, pelvic pain, recurrence, reoperation
Introduction
Worldwide, approximately 176 million women between the ages of 15 and 49 are affected by endometriosis (Taylor et al., 2012). Endometriosis manifests clinically with pelvic pain, infertility, and pelvic mass. Treatment is aimed primarily at symptomatic relief of the chronic and potentially debilitating pain. In women who wish to preserve future fertility, advanced conservative laparoscopic options include excision of ovarian endometrioma, peritoneal endometriosis and endometriosis in the rectovaginal septum.
In women who completed childbearing period, hysterectomy with or without bilateral salpingopherectomy is commonly considered the definitive option (MacDonald et al., 1999; Chalermchockchareonkit et al., 2012). Many women who elect for hysterectomy often view the procedure as a permanent solution to their symptoms caused by endometriosis. In this manuscript, the incidence, symptoms, causes of recurrence of endometriosis following hysterectomy will be reviewed and insights into future options will be contemplated.
Incidence of endometriosis recurrence
In the United States, over 100,000 hysterectomies are performed each year for a primary diagnosis of endometriosis, and approximately 12% of women with endometriosis will eventually require a hysterectomy (Lepine et al., 1997; Rizk and Abdalla, 2003). Anecdotal clinical experience suggests that patients achieve a satisfactory alleviation of endometriosis-associated pain with definitive surgery. However, patients should be informed that there is an approximate 15% probability of persistent pain after standard hysterectomy with a 3-5% risk of worsening pain or new symptom development (Vercellini et al., 2009). Only a few studies have looked at the advantages and disadvantages of definitive surgery for symptomatic endometriosis (MacDonald et al., 1999; Namnoum et al., 1995; Fedele et al., 2005; Shakiba et al., 2008). These studies can be used to glean information about recurrence, although each study reports different rates with different follow-up times.
Namnoum et al. compared the outcome of hysterectomy for symptomatic endometriosis with and without ovarian preservation (Namnoum et al., 1995). One hundred and thirty-eight women underwent hysterectomy, 29 of which had some ovarian tissue preserved, while the other 109 women underwent an accompanying bilateral oophorectomy. Symptomatic recurrence occurred in 18 (62%) of the women with ovarian preservation, of which 9 (31%) required re-operation. In the group with complete ovarian removal, 11 (10%) developed recurrent symptoms, and 4 (3.7%) required re-operation. The study concluded that ovarian conservation carries a 6.1 fold risk of recurrent pain and 8.1 fold risk of re-operation.
Shakiba et al. (2008) also assessed the need for re-operation after hysterectomy for endometriosis-associated symptoms with and without ovarian preservation. At least one ovary was preserved in 47 patients. Of these, 9 (19.2%) required re-operation. The 2, 5, and 7-year re-operation-free percentages were 95.7%, 86.6%, and 77.7%, respectively. Of the 50 patients who underwent bilateral oophorectomy, 4 (8%) required re-operation, and the 2, 5, and 7-year re-operation-free percentages were 96.0%, 91.7%, 91.7%, respectively.
Fedele et al. (2005) compared the outcome of standard extrafascial hysterectomy (n = 26) with that of a modified radical hysterectomy (n = 12) that included removal of all deeply infiltrating lesions. All patients in the post-operative course received transdermal estradiol. Eight patients (31%) in the standard hysterectomy group reported symptomatic recurrence after a minimum follow-up time of 2 years, while none in the modified radical hysterectomy group reported symptomatic recurrence, arguing for the complete removal of all deep lesions.
Symptoms of endometriosis recurrence
Accurate diagnosis of recurrence is difficult and only confirmed by second look laparoscopy, which poses particular risk to patients with prior surgery. Diagnosis of recurrence on the basis of symptoms or diagnostic imaging can be challenging. Pelvic pain and dyspareunia are the most common presenting symptoms of recurrent endometriosis after hysterectomy, although vaginal and rectal bleeding as well as low back and rectal pain may also occur (Hasty et al., 1995; Clayton et al., 1999). Painful defecation and severe dyspareunia may indicate deeply infiltrating lesions (Chapron et al., 2005). For these patients, it can be difficult to identify the exact cause of pain, because the differential diagnosis is broad, including ovarian remnant syndrome, post-surgical adhesions, and recurrent endometriosis (Hasty et al., 1995).
Causes of endometriosis recurrence
Endometriotic lesions detected at the time of the second look surgery
Endometriotic lesions are likely responsible for the majority of recurrent symptoms, in cases where the uterus and ovaries are removed, but deep endometriotic lesions are left behind. This was the standard of practice for many years, as it was noted early that endometriosis would atrophy in the absence of estrogenic stimulation (Sampson, 1921; 1922). However, it has never been definitively shown that endometriosis completely regresses in the presence of menopausal levels of estrogen, whether surgically induced or physiologic (Redwine, 1994). Moreover, in the current era of HRT, it has become increasingly important to make an effort to remove all deep lesions as they carry a risk for symptomatic recurrence and rarely malignant transformation. The most recent guidelines on the management of endometriosis reflect this change in thought (ACOG practice bulletin, 2010).
A major challenge may lie in the visual diagnosis of endometriosis. It has been estimated that two-thirds of patients have some visual disease that many clinicians have not been trained to recognize, and this may be the only manifestation of disease (Redwine, 1990). Some lesions may appear atypically or non-pigmented (Martin et al., 1989a; Jansen and Russell, 1986). Deep endometriotic lesions located in the subperitoneal space may go completely unrecognized or be particularly difficult to visualize during laparoscopy or to access during surgery. Additionally, lesions can be hidden by peritoneal adhesions of the pouch of Douglas (Kinkel et al., 1999).
The most common sites of recurrent (likely persistent) lesions after hysterectomy and oophorectomy are the large and small bowel (ACOG practice bulletin, 2010). Redwine (1994) presents a prospective, longitudinal observational study looking at the anatomical distribution of disease upon re-operation following bilateral oophorectomy, with or without hysterectomy. Patients were more likely to have intestinal involvement of their disease (RR 1.3, 95% CI 0.94-1.8), when compared with conservative treatment. In over half of these patients, disease was described at the time of oopherectomy, but was not treated, giving credence to the idea of persistent over recurrent disease. The authors conclude that invasive disease of the uterosacral ligaments or intestinal tract is more likely to remain symptomatic following oopherectomy with retention of disease and that it is illogical to leave endometriosis surgically untreated at the time of hysterectomy. Both Redwine and Clayton report satisfactory results post-operatively after excisional removal of the residual disease, although there were no formal long-term follow-up studies (Clayton et al., 1999; Redwine, 1994).
Microscopic foci
Some have proposed that microscopic foci of disease (invisible at the time of surgery) could progress and under suitable conditions give rise to clinically significant disease, which is interpreted as new disease (Guo, 2009). The concept of microscopic endometriosis began in the mid-1980s when endometriotic lesions were documented by electron microscopy from biopsies of seemingly normal appearing peritoneum upon laparotomy (Vasquez et al., 1984; Murphy et al., 1986). Researchers estimated that upwards of 25% of patients could have microscopic foci (Murphy et al., 1986). More recent studies done with laparoscopy report an incidence of 0-13% (Redwine, 1988; Redwine and Yocom, 1990b; Jansen and Russel, 1986b; Nezhat et al., 1991; Balasch et al., 1996; Walter et al., 2001). Some propose that the incidence of microscopic foci is directly related to the power of magnification used to select peritoneum for biopsy, and that increasing magnification at surgery allows for the visualization of almost all endometriotic lesions. However, it has not been demonstrated that these microscopic foci will actually progress into clinically significant disease (Redwine, 2003). Therefore, microscopic foci of disease do not represent a significant mechanism of recurrence after surgery.
Development of Endometriosis in patients who underwent hysterectomy for endometriosis
There have been few reported cases of the development of endometriosis after hysterectomy in patients on HRT with no previous history of endometriosis (Goumenou et al., 2003; Bellina and Schenck, 2000). These cases are exceedingly rare and the mechanism is unknown.
Lymphovascular invasion
Lymph node involvement in endometriosis is considered to be uncommon, and the exact incidence of lymphatic involvement is unknown, as lymph node dissection is not routinely performed for a benign disease. It is possible that lymphatic spread may contribute to endometriosis recurrence. Lymph node involvement has been reported in cases of extra-pelvic endometriosis (Insabato and Pettinato, 1996; Lorente et al., 2003; Sheikh et al., 2005; Thomakos et al., 2006). Lymphatic involvement has been studied more closely in cases of rectosigmoid endometriosis because of the relative ease of accessibility of the regional lymph nodes. Lymph node involvement is reportedly involved in 25-40% of rectosigmoid endometriosis (Noël et al., 2008; Abrao et al., 2006). Further, lymphatic involvement correlated with the size and wall layers affected by endometriosis, number of lymph nodes retrieved, and presence of D2-40, a marker of lymphovascular invasion (Noël et al., 2008). It is unclear whether lymphatic involvement is the result of an invasive process, or simply the result of regional lymphatic drainage from endometriotic lesions. There is some evidence that deeply infiltrating endometriosis can behave in a malignant manner, invading adjacent tissue, but further research must be conducted (Thomas and Campbell, 2000).
Ovarian preservation
Removal of endogenous estrogen production may be an effective strategy in reducing symptomatic endometriosis. The issue of ovarian preservation is of particular importance, since many patients undergoing hysterectomy for endometriosis-associated pain are young women in whom an effort should be made to preserve at least one ovary. At least 10,000 women per year in the United States between the ages of 25-29 undergo a hysterectomy for a primary diagnosis of endometriosis (Lepine et al., 1997). It is unclear whether ovarian preservation improves or worsens clinical outcomes in endometriosis, as no randomized controlled trials have addressed this issue.
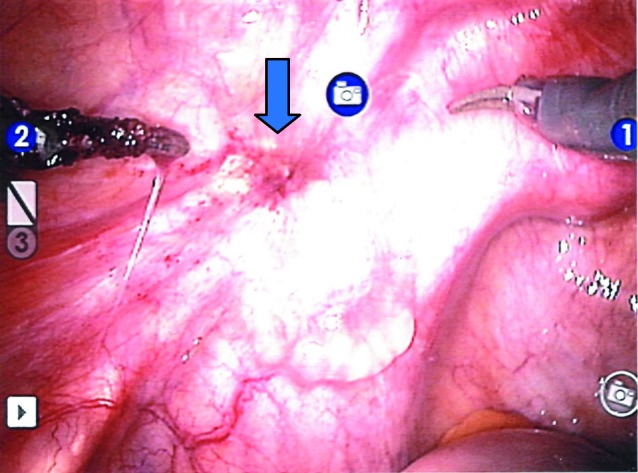
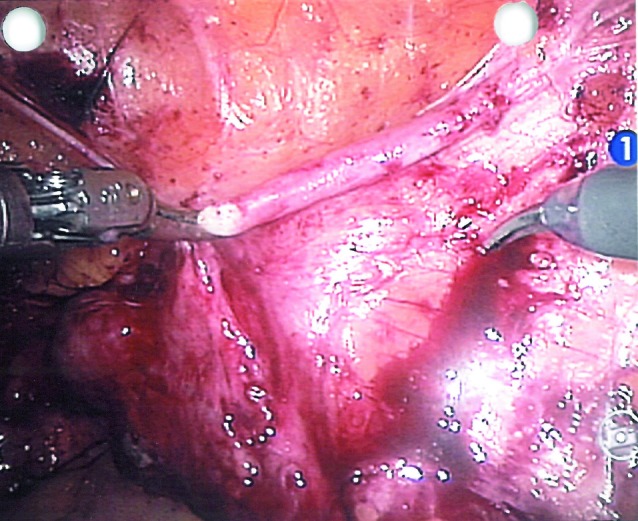
Fig. 1. Peritoneal endometriosis visualized along the course of left ureter causing persistent pain after laparoscopic hysterectomy.
Data suggest that ovarian conservation with hysterectomy is associated with increased symptom recurrence and higher rates of re-operation. As mentioned previously, Namnoum et al.’s study on women undergoing hysterectomy for symptomatic endometriosis concluded that ovarian conservation carried a 6.1 fold risk of recurrent pain and 8.1 fold risk of re-operation (Namnoum et al., 1995). Similarly, Shakiba et al. (2008) reported that preservation of both ovaries at hysterectomy for symptomatic endometriosis increased the risk of re-operation by 2.44 times, regardless of the age of patient, although these results did not reach statistical significance (CI 0.65–9.1). Further, they found that in women between 30-39 years, oophorectomy did not significantly change the time interval to re-operation. Taken together, these studies indicate that women undergoing hysterectomy with bilateral oophorectomy are less likely to require further surgery because of recurrent symptomatic disease (Vercillini et al., 2009). However, ovarian conservation is a viable option for some women, especially those under 40 years with advanced endometriosis.
Bilateral oophorectomy, and the induction of early menopause, has been associated with increased all-cause mortality and causes specific deaths from coronary heart disease (Parker et al., 2007).
An additional consideration, especially for younger women, is the widespread effect of estrogen deficiency on psychosexual health. Although MacDonald et al. (1999) showed that younger women (< 30 years) reported a lower incidence of recurrent endometriosis-related symptoms after hysterectomy with oophorectomy than older women (> 40 years), the younger women were more likely to report a sense of loss, and to report more disruption from pain in different aspects of their lives. Further, observational studies have shown that women who have had an oophorectomy more consistently report dissatisfaction with their sexual life post-operatively, when compared to women who have had only a hysterectomy or who have reached physiologic menopause (Nathorst-Boos and Van Schoultz, 1992).
Thus, the physician and patient must carefully weigh the risks and benefits of hysterectomy with and without ovarian preservation.
Ovarian Remnant Syndrome
Recurrent endometriosis has been associated with the presence of residual ovarian tissue following oophorectomy (Dmowski et al., 1988). Reactivation of disease secondary to endogenous hormone secretion from this ovarian tissue is the so called ‘ovarian remnant syndrome.’ The incidence of ovarian remnant syndrome in endometriosis recurrence following definitive surgery is not known, and hormone replacement therapy may blur the lines clinically in distinguishing it from disease recurrence. Dense pelvic adhesions, inflammatory conditions, such as endometriosis, peri-operative bleeding, and ovaries which are partially or wholly retroperitoneal, can all contribute to the unintentional preservation of ovarian fragments (Kho and Abrao, 2012). For this reason, care should be taken to meticulously remove ovarian tissue during the initial oophorectomy with clear surgical margins.
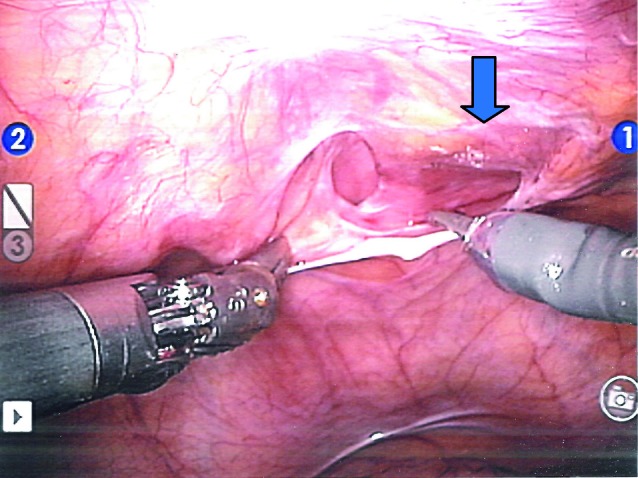
Fig. 2. Vaginal vault endometriosis infiltrating deep between vaginal canal and rectum.
Pre-menopausal levels of serum FSH and estradiol in a patient after definitive surgery for endometriosis may indicate the existence of a functional ovarian remnant (Kho and Abrao, 2012). Of course, HRT must be stopped for at least ten days prior to testing. Menopausal levels of FSH and estradiol do not preclude ovarian remnants, however, as some are less functional than others. Ultimately, histological confirmation of the ovarian tissue is needed to confirm the diagnosis (Rizk and Abdalla, 2003). If imaging demonstrates residual ovarian tissue, surgical removal with histological confirmation is recommended. If not, pharmacological suppression of ovarian function can be attempted with GnRH agonists, danazol, or progesterone.
Hormone replacement therapy after hysterectomy
There is no clear recommendation on the initiation of hormonal replacement therapy (HRT) following hysterectomy with oophorectomy for women with a history of endometriosis, but the general consensus is that the benefits outweigh the risks. The most recent guidelines state only that HRT is not contraindicated, as there is insufficient outcome-based evidence to support recommending HRT after definitive surgery (ACOG practice Bulletin, 2010). The risk of HRT is two-fold: (1) disease recurrence and (2) malignant transformation of residual disease foci; but these risks have not been clearly defined (Oxholm et al., 2007).
The exact incidence of disease recurrence with HRT is not known. Matorras et al. (2002) conducted a prospective, randomized study to estimate the risk of recurrence associated with the use of combined HRT (n = 115) vs. no HRT (n = 57) for patients who underwent bilateral salpingo-oophorectomy, with or without hysterectomy (91.8% had hysterectomy), for endometriosis. The mean follow-up time was 45 months. The recurrence rate was 3.5% (4 of 115) in women receiving HRT, or 0.9% per year. Two of these patients required re-operation. There was no recurrence in women who did not receive HRT. The authors identified two risk factors for recurrence in the women who received HRT: peritoneal involvement > 3 cm (2.4% recurrence per year vs 0.3%) and incomplete surgery (22.2% per patient vs 1.9%). They concluded that the risk of recurrence is low, but additional care should be taken in cases of peritoneal involvement.
Soliman and Hillard (2006) performed a thorough review of the literature on HRT after surgery for symptomatic endometriosis and recommend the use of continuous tibolone or combined estrogen and progesterone beginning immediately post-operatively, though they note that a strong evidence base for their recommendation is lacking.
Combined estrogen and progesterone therapy should be considered when there is documented residual endometriosis after radical surgery, in cases of severe disease, and in obese patients with higher levels of endogenous estrogen. The addition of progestin is hypothesized to reduce the chance of hyperplasia or malignant transformation in residual disease foci, as endometriotic tissue has both estrogen and progesterone receptors (Nisolle et al., 1994). It should be noted, however, that the addition of progestin long-term hormone therapy might increase the risk of post-menopausal breast cancer (Rossouw et al., 2002; Anderson et al., 2004). The advice is that the lowest dose of HRT be used (Soliman and Hillard, 2006).
Tibolone is a gonadomimetic, which shows promise in preventing recurrent endometriosis after pelvic clearance. Its active metabolite causes atrophy of the endometrial tissue and theoretically has the same effect on ectopic endometriotic tissue as well (Soliman and Hillard, 2006). Twenty-one women with residual pelvic endometriosis after bilateral oophorectomy were randomized to receive either tibolone (n = 11) or transdermal estrogen with medroxyprogesterone acetate (n = 12), and were followed for 12 months for symptom recurrence. Only 1 patient (9%) in the tibolone group reported symptomatic recurrence, compared with 4 (40%) in the combined HRT group (Fedele et al., 1999).
It should be noted that there is currently no evidence to suggest that combined HRT or tibolone reduces the risk of endometrioid adenocarcinoma. Moreover, some data link combined HRT and tibolone with recurrent endometriosis as well (Sundar et al., 2007).
Soliman and Hillard (2006) recommend initiating HRT immediately post-operatively. Early HRT minimizes hypoestrogenic symptoms (menopausal symptoms, urogenital atrophy, loss of libido, and bone loss), and there is evidence that early initiation does not increase the incidence of symptom recurrence following definitive surgery for endometriosis when compared to late initiation. A retrospective cohort study of 95 women who underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy for endometriosis compared the recurrence of pain in 60 women who began estrogen replacement therapy within 6 weeks of surgery and 35 women who began therapy more than 6 weeks after surgery (Hickman et al., 1998). Four (7%) of the women who began hormone replacement immediately had recurrent pain, compared with 7 (20%) of the women who delayed hormone replacement. After controlling for length of follow-up (average 57 months), there was no significant difference between the two groups. Further, after adjusting for covariates, the group who delayed hormone replacement had a relative risk of 5.7 for pain recurrence (95% CI, 1.3-25.2).
Aromatase enzyme activity
Other factors involved in disease persistence may be the local expression of aromatase activity and the varying activity of estrogen and progestin receptors in both primary and recurrent endometriotic tissue. It has been shown that eutopic endometrial tissue and endometriotic implants express aromatase, which may lead to autologous estrogen production to promote self-growth (Noble et al., 1996). Some hypothesize that the abnormal hormonal responsiveness of endometrial implants plays a role in the recurrence of endometriosis after hysterectomy. Endometriotic tissue contains a lower concentration of estrogen and progesterone receptors than normal endometrium, and the regulation of these receptors is dissimilar as well (Bergqvist et al., 1981; Janne et al., 1981). Recurrent endometriosis has still different levels in estrogen and progesterone receptors, which suggests different hormonal regulation (Bergqvist and Ferno, 1993). It is not surprising, then, that endometriosis recurring or persisting after hysterectomy occurs in a relatively unpredictable manner.
Aggressive, hormone-resistant endometriosis arising after hysterectomy and oophorectomy has been documented (Metzger et al., 1991). Further histological characterization of the tissue showed elevated progesterone receptor content, despite administration of large amounts of depo-medroxyprogesterone acetate. The lack of down-regulation points toward the undiscovered alterations in regulatory response in these recurrent lesions.
Alternatively, poor vascularity, fibrosis, or exposure to various inflammatory cells may contribute to the non-responsiveness of some endometrial implants (Berlanda et al., 2010).
Types of hysterectomy
Supracervical hysterectomy
Endometriosis has been reported after laparoscopic supracervical hysterectomy (LSH) with morcellation of the uterine corpus (Schuster et al., 2012; Hilger and Margina, 2006; Sepilian and Della Badia, 2003; Lieng et al., 2008; Lyons, 2007; Donnez et al., 1997). In LSH, the uterus is morcellated and removed from the pelvis while the cervical stump remains. Many surgeons prefer LSH because of its technical ease, reduced blood loss, reduced operating room and recovery time (Schuster et al., 2012; Lieng et al., 2008). Some propose that morcellation of the uterus in the abdomen seeds the peritoneal cavity with endometrial tissue, predisposing the patient to new onset or recurrent endometriosis (Hilger and Margina, 2006; Sepilian and Della Badia, 2003). Others hypothesize that retrograde flow of residual endometrial tissue from the retained cervical stump leads to endometriosis following LSH (Schuster et al., 2012; Hilger and Margina, 2006). Further, one cannot exclude that endometriosis may have been present, but not well visualized at the time of the original surgery; and onset of symptoms only represents worsening of the original disease.
Fig. 3. Normal cystoscopy after excision of endometriosis along the course of the ureter in a patient who had previously underwent hysterectomy for endometriosis.
Schuster et al. (2012) conducted a single centre case control study, including 464 women who either underwent a LSH (n = 277) or a total abdominal or laparoscopic transvaginal hysterectomy (control group, n = 187), the largest cohort to date looking at the incidence of endometriosis after LSH with morcellation. One hundred and two patients had endometriosis at the time of hysterectomy, 60 in the LSH group and 42 in the control group. The incidence of newly diagnosed endometriosis was 1.4% for both the LSH group (3/217) and the control hysterectomy group (2/145). Recurrent endometriosis following LSH occurred in 3.3% (2/42), while no recurrent endometriosis was found in the control group (p = 0.34). At conclusion, the group states that it is inconclusive whether or not uterine morcellation leads to a higher recurrence rate of endometriosis as compared to total hysterectomy, as their results did not reach statistical significance. We await prospective, randomized clinical trials for further evaluation of this surgical technique and its effect on endometriosis recurrence.
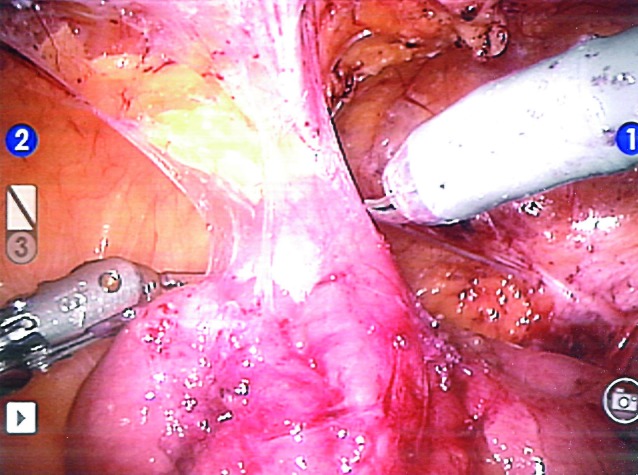
Fig. 4. Laparoscopic view of adhesions between bowel and pelvic wall in a patient with pelvic endometriosis.
MacDonald et al. (1999) compared the outcome of hysterectomy for endometriosis-associated pain in women less than 30 years old (n = 16) at the time of operation with women older than 40 years (n = 27). 20 % of younger women had persistent symptoms at a mean follow-up time of 4 years, while 13% of older women had persistent symptoms at a mean follow-up time of 9 years. Additionally, younger women were more likely to report a sense of loss, and to report more disruption from pain in different aspects of their lives.
How extensive should the hysterectomy be in women with deeply infiltrating endometriosis?
Fedele et al. (2005) coined the term modified radical hysterectomy to describe a tailored hysterectomy to the specific anatomic findings when removing deeply infiltrating nodules of the rectovaginal and/or vesicovaginal septum. The tailored radical hysterectomy included removal of the uterus, adnexa, posterior and anterior parametria, including endometriotic lesions and upper one-third of the vagina with lesions of lateral and posterior vaginal epithelium. There was no symptom recurrence 6-18 months after surgery and HRT, compared to 30% recurrence with standard extra-fascial hysterectomy and HRT. Tailored radical hysterectomy was associated with a 60 minute increase in operating room time and 1.7 day increase in mean post-operative hospital stay, which may make surgeons more reluctant to choose this option. However, the overall benefit may be in reduced rates of re-operation, although this was not explicitly studied.
Fig. 5. Laparoscopic view of adhesions between ovary and pelvic wall in a patient with pelvic endometriosis.
Management of endometriosis recurrence
Perhaps the best management for recurrence is prevention accomplished by thorough removal of all endometriotic lesions at the time of hysterectomy, including deep lesions of the pouch of Douglas, anterior pouch, and ureter. Although, this is more technically demanding, and requires longer surgery and post-operative stay, there is less recurrence even with HRT (Fedele et al., 2005).
In the case of symptomatic recurrence following hysterectomy, the clinician must have a high suspicion for deep or obstructing lesions. Therefore, it may be necessary to perform barium enema and sigmoidoscopy if a stricture is suspected, fat-suppressed MRI to identify deep disease, and intravenous urogram for hydronephrosis and hydroureter (Clayton et al., 1999).
The use of GnRH agonists is controversial in the case of recurrence following definitive surgery. If the ovaries have been removed, gonadotropin suppression should not induce hypoestrogenemia. However, endometrial tissue has been shown to have gonadotropin receptors, and some authors report success with early diagnosis, cessation of HRT, and a 3-month trial of GnRH agonist (Matorras et al., 2002; Vignali,1998).
If surgery is deemed necessary, laparoscopic excision should be performed using sharp dissection or monopolar electroexcision, as endometriosis be invasive (Martin et al., 1989b). All visible endometriosis should be removed. Robotic-assisted laparoscopy is of tremendous value in the visualization of lesions and in the meticulous resection (Fig. 1, Fig. 2). It is also important to make sure interstitial cystitis is excluded as a cause of pelvic pain (Fig. 3). Bowel and ovarian adhesions are frequently encountered in patients with pelvic endometriosis after hysterectomy performed for pelvic endometriosis (Fig. 4, Fig. 5). Laparotomy, partial, full-thickness or segmental bowel resections, or ureteric stenting may be necessary as well. Patients should be given a bowel preparation before the procedure.
Conclusion
For women with endometriosis, hysterectomy is often viewed as a permanent solution to their chronic pelvic pain. For many women, this is the case. However, there will be a small number of women who will experience a recurrence of their symptoms after “definitive” surgery. Women who choose to keep one or both ovaries or start HRT after oophorectomy are at higher risk for recurrence, although the benefits of ovarian conservation or HRT in younger women likely outweigh the risk of disease recurrence.
Many theories have been proposed as to why endometriosis would recur after hysterectomy, including residual microscopic foci, hormonal factors, ovarian remnants, uterine morcellation, lymphovascular invasion, and de-novo disease. It is likely, however, that most cases of disease recurrence after hysterectomy are actually cases of disease persistence. It is hard to decipher from the studies that looked at the incidence of disease recurrence after hysterectomy whether or not thorough excision of all endometriotic lesions was performed at the time of the primary surgery. It has been shown that there is a lower rate of recurrence with complete removal of all endometriotic lesions at the time of hysterectomy, although this is a more technically demanding surgery. With this in mind, surgeons who are familiar and comfortable with the identification and excision of endometriosis should handle hysterectomy for the primary diagnosis of endometriosis. If this is not the case, the patient should be referred to a surgical centre with more expertise in endometriosis.
References
- Abrao MS, Podgaec S, Dias JA. Deeply infiltrating endometriosis affecting the rectum and lymph nodes. Fertil Steril. 2006;86:543–547. doi: 10.1016/j.fertnstert.2006.02.102. [DOI] [PubMed] [Google Scholar]
- ACOG Practice Bulletin. Practice bulletin no. 114: management of endometriosis. Obstet. Gynecol. 2010;116:223–236. doi: 10.1097/AOG.0b013e3181e8b073. [DOI] [PubMed] [Google Scholar]
- Anderson GL, Limacher M, Assaf AR, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: The Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701–1712. doi: 10.1001/jama.291.14.1701. [DOI] [PubMed] [Google Scholar]
- Balasch J, Creus M, Fábregues F, et al. Visible and non-visible endometriosis at laparoscopy in fertile and infertile women and in patients with chronic pelvic pain: a prospective study. Hum. Reprod. 1996;11:387–391. doi: 10.1093/humrep/11.2.387. [DOI] [PubMed] [Google Scholar]
- Bellina JH, Schenck D. Large postmenopausal ovarian endometrioma. Obstet Gynecol. 2000;96:846. doi: 10.1016/s0029-7844(00)00963-7. [DOI] [PubMed] [Google Scholar]
- Bergqvist A, Rannevik G, Thorell J. Estrogen and progesterone cytosol receptor concentration in endometriotic tissue and intrauterine endometrium. Acta Obstet Gynecol Scand. 1981;101(Suppl):53–58. doi: 10.3109/00016348109157813. [DOI] [PubMed] [Google Scholar]
- Bergqvist A, Fernö M. Estrogen and progesterone receptors in endometriotic tissue and endometrium: comparison according to localization and recurrence. Fertil Steril. 1993;60:63–68. [PubMed] [Google Scholar]
- Berlanda N, Vercellini P, Fedele L. The outcomes of repeat surgery for recurrent symptomatic endometriosis. Curr Opin Obstet Gynecol. 2010;22:320–325. doi: 10.1097/GCO.0b013e32833bea15. [DOI] [PubMed] [Google Scholar]
- Chalermchockchareonkit A, Tekasakul P, Chaisilwattana P, et al. Laparoscopic hysterectomy versus abdominal hysterectomy for severe pelvic endometriosis. Int J Gynecol Obstet. 2012;116:109–111. doi: 10.1016/j.ijgo.2011.09.022. [DOI] [PubMed] [Google Scholar]
- Chapron C, Barakat H, Fritel X, et al. Presurgical diagnosis of posterior deep infiltrating endometriosis based on a standardized questionnaire. Hum Reprod. 2005;20:507–513. doi: 10.1093/humrep/deh627. [DOI] [PubMed] [Google Scholar]
- Clayton RD, Hawe JA, Love JC, et al. Recurrent pain after hysterectomy and bilateral salpingo-oophorectomy for endometriosis: evaluation of laparoscopic excision of residual endometriosis. BJOG. 1999;106:74–74. doi: 10.1111/j.1471-0528.1999.tb08377.x. [DOI] [PubMed] [Google Scholar]
- Dmowski WP, Radwanska E, Rana N. Recurrent endometriosis following hysterectomy and oophorectomy: the role of residual ovarian fragments. Int J Gynecol Obstet. 1988;26:93–103. doi: 10.1016/0020-7292(88)90202-0. [DOI] [PubMed] [Google Scholar]
- Donnez J, Nissole M, Smets M, et al. Laparoscopic supracervical (subtotal) hysterectomy: a first series of 500 cases. Gynecol Endosc. 1997;6:73–76. [Google Scholar]
- Fedele L, Bianchi S, Raffaelli R, et al. Comparison of transdermal estradiol and tibolone for the treatment of oophorectomized women with deep residual endometriosis. Maturitas. 1999;32:189–193. doi: 10.1016/s0378-5122(99)00032-8. [DOI] [PubMed] [Google Scholar]
- Fedele L, Bianchi S, Zanconato G, et al. Tailoring radicality in demolitive surgery for deeply infiltrating endometriosis. Am J Obstet Gynecol. 2005;193:114–117. doi: 10.1016/j.ajog.2004.12.085. [DOI] [PubMed] [Google Scholar]
- Goumenou AG, Chow C, Taylor A, et al. Endometriosis arising during estrogen and testosterone treatment 17 years after abdominal hysterectomy: a case report. Maturitas. 2003;46:239–241. doi: 10.1016/s0378-5122(03)00081-1. [DOI] [PubMed] [Google Scholar]
- Guo SW. Recurrence of endometriosis and its control. Hum Reprod Update. 2009;15:441–461. doi: 10.1093/humupd/dmp007. [DOI] [PubMed] [Google Scholar]
- Hasty LA, Murphy AA. Management of Recurrent Endometriosis After Hysterectomy and Bilateral Salpingo-Oophorectomy. Endometriosis. 1995;18:189–192. [Google Scholar]
- Hickman TN, Namnoum AB, Hinton EL, et al. Timing of estrogen replacement therapy following hysterectomy with oophorectomy for endometriosis. Obstet Gynecol. 1998;91:673–677. doi: 10.1016/s0029-7844(98)00071-4. [DOI] [PubMed] [Google Scholar]
- Hilger WS, Margina JF. Removal of pelvic leiomyomata and endometriosis five years after supracervical hysterectomy. Obstet Gynecol. 2006;108:772–774. doi: 10.1097/01.AOG.0000209187.90019.d3. [DOI] [PubMed] [Google Scholar]
- Insabato L, Pettinato G. Endometriosis of the bowel with lymph node involvement. A report of three cases and review of the literature. Pathol Res Pract. 1996;192:957–962. doi: 10.1016/S0344-0338(96)80079-3. [DOI] [PubMed] [Google Scholar]
- Jansen RP, Russell P. Nonpigmented endometriosis: clinical, laparoscopic, and pathologic definition. Am J Obstet Gynecol. 1986;155:1154–1159. doi: 10.1016/0002-9378(86)90136-5. [DOI] [PubMed] [Google Scholar]
- Kho RM, Abrao MS. Ovarian remnant syndrome: etiology, diagnosis, treatment and impact of endometriosis. Curr Opin Obstet Gynecol. 2012;24:210–214. doi: 10.1097/GCO.0b013e3283558539. [DOI] [PubMed] [Google Scholar]
- Kinkel K, Chapron C, Balleyguier C, et al. Magnetic resonance imaging characteristics of deep endometriosis. Hum Reprod. 1999;14:1080–1086. doi: 10.1093/humrep/14.4.1080. [DOI] [PubMed] [Google Scholar]
- Lepine LA, Hillis SD, Marchbanks PA, et al. Hysterectomy surveillance – United States, 1980-1993. MMWR CDC Surveill Summ. 1997;46:1–15. [PubMed] [Google Scholar]
- Lieng M, Qvigstad E, Istre O, et al. Long-term outcomes following laparoscopic supracervical hysterectomy. BJOG. 2008;115:1605–1610. doi: 10.1111/j.1471-0528.2008.01854.x. [DOI] [PubMed] [Google Scholar]
- Lorente-Poyatos R, Palacios-Perez A, Bravo-Bravo F, et al. Rectosigmoid endometriosis with lymph node involvement. Gastroenterol Hepatol. 2003;26:23–25. [PubMed] [Google Scholar]
- Lyons T. Laparoscopic supracervical versus total hysterectomy. J Minim Invasive Gynecol. 2007;14:275–277. doi: 10.1016/j.jmig.2006.10.032. [DOI] [PubMed] [Google Scholar]
- MacDonald SR, Klock SC, Milad MP. Long-term outcome of nonconservative surgery (hysterectomy) for endometriosis-associated pain in women < 30 years old. Am J Obstet Gynecol. 1999;180:1360–1363. doi: 10.1016/s0002-9378(99)70020-7. [DOI] [PubMed] [Google Scholar]
- Martin DC, Hubert GD, Levy BS. Depth of infiltration of endometriosis. J Gynecol Surg. 1989;5:55–60. [Google Scholar]
- Martin DC, Hubert GD, Vander ZR, et al. Laparoscopic appearances of peritoneal endometriosis. Fertil Steril. 1989;51:63–67. doi: 10.1016/s0015-0282(16)60429-6. [DOI] [PubMed] [Google Scholar]
- Matorras R, Elorriaga MA, Pijoan JI, et al. Recurrence of endometriosis in women with bilateral adnexectomy (with or without total hysterectomy) who received hormone replacement therapy. Fertil Steril. 2002;77:303–308. doi: 10.1016/s0015-0282(01)02981-8. [DOI] [PubMed] [Google Scholar]
- Metzger DA, Lessey BA, Soper JT, et al. Hormone-resistant endometriosis following total abdominal hysterectomy and bilateral salpingo-oophorectomy: correlation with histology and steroid receptor content. Obstet Gynecol. 1991;78:946–950. [PubMed] [Google Scholar]
- Murphy AA, Green WR, Bobbie D, et al. Unsuspected endometriosis documented by scanning electron microscopy in visually normal peritoneum. Fertil Steril. 1986;46:522–524. doi: 10.1016/s0015-0282(16)49598-1. [DOI] [PubMed] [Google Scholar]
- Namnoum AB, Hickman TN, Goodman SB, et al. Incidence of symptom recurrence after hysterectomy for endometriosis. Fertil Steril. 1995;64:898–902. doi: 10.1016/s0015-0282(16)57899-6. [DOI] [PubMed] [Google Scholar]
- Boos J, Von Schoultz H. Psychological reactions and sexual life after hysterectomy with and without oophorectomy. Gynaecol Obstet Invest. 1992;34:97–101. doi: 10.1159/000292735. [DOI] [PubMed] [Google Scholar]
- Nezhat F, Allan CJ, Nezhat C, et al. Nonvisualized endometriosis at laparoscopy. Int J Fertil. 1991;36:340–343. [PubMed] [Google Scholar]
- Nisolle M, Roux F, Wyns C, et al. Immunohistochemical analysis of estrogen and progesterone receptors in endometrium and peritoneal endometriosis: a new quantitative method. Fertil Steril. 1994;62:751–759. doi: 10.1016/s0015-0282(16)57000-9. [DOI] [PubMed] [Google Scholar]
- Noble LS, Simpson ER, Johns A, et al. Aromatase expression in endometriosis. J Clin Endocrinol Metab. 1996;81:174–179. doi: 10.1210/jcem.81.1.8550748. [DOI] [PubMed] [Google Scholar]
- Noël J, Chapron C, Fayt I, et al. Lymph node involvement and lymphovascular invasion in deep infiltrating rectosigmoid endometriosis. Fertil Steril. 2008;89:1069–1072. doi: 10.1016/j.fertnstert.2007.05.011. [DOI] [PubMed] [Google Scholar]
- Oxholm D, Knudsen UB, Baggesen N, et al. Postmenopausal endometriosis. Acta Obstet Gynecol Scand. 2007;4:1–7. doi: 10.1080/00016340701619407. [DOI] [PubMed] [Google Scholar]
- Parker WH, Broder MS, Liu Z, et al. Ovarian conservation at the time of hysterectomy for benign disease. Clin Obstet Gynecol. 2007;50:354–361. doi: 10.1097/GRF.0b013e31804a838d. [DOI] [PubMed] [Google Scholar]
- Parker WH, Broder MS, Chang E, et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses’ health study. Obstet Gynecol. 2009;113:1027–1037. doi: 10.1097/AOG.0b013e3181a11c64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redwine DB. Is “microscopic” peritoneal endometriosis invisible? Fertil Steril. 1988;50:665–666. doi: 10.1016/s0015-0282(16)60205-4. [DOI] [PubMed] [Google Scholar]
- Redwine DB. The visual appearance of endometriosis and its impact on our concepts of the disease. Prog Clin Biol Res. 1990;323:393–412. [PubMed] [Google Scholar]
- Redwine DB. Endometriosis persisting after castration: clinical characteristics and results of surgical management. Obstet Gynecol. 1994;83:405–413. [PubMed] [Google Scholar]
- Redwine DB. Invisible” microscopic endometriosis: a review. Gynecol Obstet Invest. 2003;55:63–67. doi: 10.1159/000070176. [DOI] [PubMed] [Google Scholar]
- Redwine DB, Yocom LB. A serial section study of visually normal pelvic peritoneum in patients with endometriosis. Fertil Steril. 1990;54:648–651. doi: 10.1016/s0015-0282(16)53823-0. [DOI] [PubMed] [Google Scholar]
- Rizk B, Abdalla H. Fast Facts: Endometriosis. (2nd ed.) Oxford: Health Press; 2003. [Google Scholar]
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- Sampson JA. Perforating hemorrhagic (chocolate) cysts of the ovary. Arch Surg. 1921;3:245–323. [Google Scholar]
- Sampson JA. Ovarian hematomas of endometrial type (perforating hemorrhagic cysts of the ovary) and implantation adenomas of the endometrial type. Boston Med Surg J. 1922;186:445–456. [Google Scholar]
- Schuster MW, Wheeler TL, Richter HE. Endometriosis after Laparoscopic Supracervical Hysterectomy with Uterine Morcellation: A Case Control Study. J Minim Invasive Gynecol. 2012;19:183–187. doi: 10.1016/j.jmig.2011.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepilian V, Della Badia C. Iatrogenic endometriosis caused by uterine morcellation during a supracervical hysterectomy. Obstet Gynecol. 2003;102:1125–1127. doi: 10.1016/s0029-7844(03)00683-5. [DOI] [PubMed] [Google Scholar]
- Shakiba K, Bena JF, McGill KM, et al. Surgical treatment of endometriosis: a 7-year follow-up on the requirement for further surgery. Obstet Gynecol. 2008;111:1285–1292. doi: 10.1097/AOG.0b013e3181758ec6. [DOI] [PubMed] [Google Scholar]
- Sheikh HA, Krishnamurti U, Bhat Y, et al. A 42-year-old woman with a 7-month history of abdominal pain. A, endometriosis involving ileocecal junction and 2 pericolonic lymph nodes; B, intranodal benign glandular inclusions. Arch Pathol Lab Med. 2005;129:e218–e221. doi: 10.5858/2005-129-e218-AYWWAM. [DOI] [PubMed] [Google Scholar]
- Soliman NF, Hillard TC. Hormone replacement therapy in women with past history of endometriosis. Climacteric. 2006;9:325–335. doi: 10.1080/13697130600868711. [DOI] [PubMed] [Google Scholar]
- Sundar SS, Gornall RJ, Kerr-Wilson R. A case report of recurrent endometriosis following Tibolone hormone replacement therapy. J Obstet Gynaecol. 2007;27:433–434. doi: 10.1080/01443610701362914. [DOI] [PubMed] [Google Scholar]
- Taylor RN, Hummelshoj L, Stratton P, et al. Pain and endometriosis: Etiology, impact and therapeutics. Middle East Fertil Soc J. 2012;17:221–225. doi: 10.1016/j.mefs.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomakos N, Rodolakis A, Vlachos G, et al. A rare case of rectovaginal endometriosis with lymph node involvement. Gynecol Obstet Invest. 2006;62:45–47. doi: 10.1159/000091998. [DOI] [PubMed] [Google Scholar]
- Thomas EJ, Campbell IG. Evidence that endometriosis behaves in a malignant manner. Gynecol Obstet Invest. 2000;50(Suppl 1):2–10. doi: 10.1159/000052872. [DOI] [PubMed] [Google Scholar]
- Vasquez G, Cornillie F, Brosens IA. Peritoneal endometriosis: scanning electron microscopy and histology of minimal pelvic endometriotic lesions. Fertil Steril. 1984;42:696–703. doi: 10.1016/s0015-0282(16)48193-8. [DOI] [PubMed] [Google Scholar]
- Vercellini P, Barbara G, Abbiati A, et al. Repetitive surgery for recurrent symptomatic endometriosis: what to do? Eur J Obstet Gynecol Reprod Biol. 2009;146:15–21. doi: 10.1016/j.ejogrb.2009.05.007. [DOI] [PubMed] [Google Scholar]
- Vignali M. Molecular action of GnRH analogues on ectopic endometrial cells. Gynecol Obstet Invest. 1998;45(Suppl 1):2–5. doi: 10.1159/000052845. [DOI] [PubMed] [Google Scholar]
- Walter AJ, Hentz JG, Magtibay PM, et al. Endometriosis: correlation between histologic and visual findings at laparoscopy. Am J Obstet Gynecol. 2001;184:1407–1413. doi: 10.1067/mob.2001.115747. [DOI] [PubMed] [Google Scholar]


