Abstract
Magnetic Resonant Imaging (MRI) has demonstrated that we can differentiate the uterus in 3 important functional areas. Exploration of the uterus in the infertile patient should implement the evaluation of the endometrium, the Junctional zone myometrium (JZ), the outer myometrium and the cervical canal. Especially the JZ myometrium should receive our close attention in the exploration and treatment of the infertile patient.
MRI cannot be implemented as a screening examination but also limiting the imaging of the womb to a 2 or 3 D ultrasound exam only does not meet the scientific requirements of sensitivity and specificity.
Modern ambulatory uterine diagnosis in a one-stop approach includes transvaginal ultrasound, fluid mini Hysteroscopy, contrast sonography and endomyometrial tissue sampling.
Transvaginal Ultrasound being the gold standard for global uterine screening has a cardinal importance for diagnosis of myometrial disorders and uterine congenital malformations whereas hysteroscopy remains the gold standard for the evaluation of the endometrium and cervical canal. The major challenge remains to perform a tissue sampling of the endo-myometrium in an ambulatory, patient friendly and reliable way for which the newly designed Trophy hysteroscope provide a satisfactory answer.
This one-stop approach opens a total new and advanced dimension to the screening, diagnosis and treatment of uterine pathology in the infertile patient.
Keywords: Ambulatory, diagnosis, hysteroscopy, infertility, MRI, one-stop approach, tissue sampling, sonography, ultrasound
Introduction
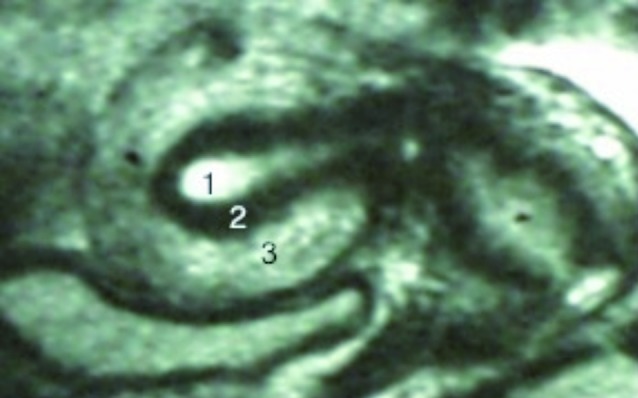
An important challenge in the management of the infertile patient is the evaluation of the uterine capacity for reproduction. MRI has demonstrated that the uterus is divided in 3 functional areas, the endometrium, the sub-endometrial myometrium or junctional zone myometrium (JZ) and the outer myometrium (Fig. 1) (Brosens et al., 1995; Novellas et al., 2011).
Fig. 1. Magnetic resonance imaging demonstrating the 3 functional zones of the uterus.(1) Endometrium, (2) Junctional zone myometrium, (3) Outer myometrium.
The challenge is to evaluate those functions in an ambulatory setting with accessible diagnostic methods. Especially changes in the JZ myometrium seems of major interest to the reproductive health care researchers.
Hysteroscopy is without any doubt the gold standard for the diagnosis of cervical and intrauterine pathology and could play a major role in the evaluation of JZ myometrial pathology (Campo et al., 1999; Bakour et al., 2006; Molinas and Campo, 2006; RCOG, 2011). Although for a broad implementation we have to be able to organise the hysteroscopic diagnostic exam with the same simplicity as a transvaginal ultrasound and with comparable patient compliance.
Transvaginal 2 and 3 D ultrasound are the gold standard for the global uterine screening and with a cardinal importance for diagnosis of myometrial disorders and uterine congenital malformations. But it is demonstrated that in normal ultrasound findings still pathology of possibly importance for the reproduction is detected at hysteroscopy (El-Toukhy et al., 2014).
By combining both examinations, a complete uterine diagnosis in a one-stop session can be done. With the new generation of instruments, it is possible today to perform this one-stop diagnosis, in a most comfortable and accurate way. Without the necessity to use speculum or analgesia, ultrasound, hysteroscopy, contrastsonography and even the hysteroscopic or ultrasound guided endo-myometrial tissue sampling can be performed (Campo et al., 1999, 2005).
This one stop approach provides with a high patient compliance, all necessary information to make an accurate diagnosis and to plan the correct therapeutic approach.
One-stop uterine diagnosis
The one-stop uterine diagnosis is an attractive idea for both patients and clinicians, but to implement we have to solve the drawbacks of hysteroscopy.
Both the exam as the possibility of tissue sampling should be able to be performed as easy as a transvaginal ultrasound. Conventional hysteroscopy is mostly done under general anaesthesia using instruments of around 5 mm, which sometimes requires cervical dilatation using a speculum and tenaculum. This does not match with the required condition (Campo et al., 1999, 2005).
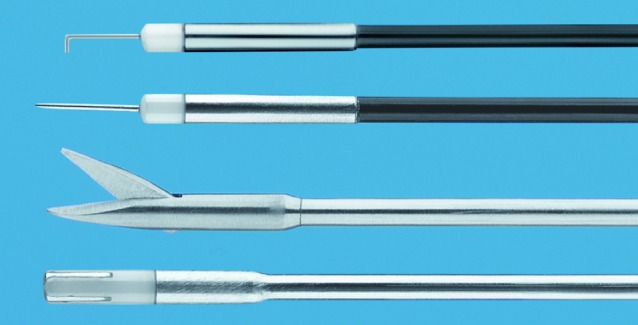
Today we have grade A evidence that only by reducing the total instrument diameter under 3.2 mm and by using the atraumatic vagino-cervico insertion technique with saline as a distension medium, everybody can learn to perform an ambulatory diagnostic hysteroscopy with high patient satisfaction and perfect visualization (Campo et al., 2005). Moreover, a recent prospective randomized multicentre controlled trial confirmed those findings as they did not report any access failure or complication in all hysteroscopies performed in the study (Campo et al., 2005). For this study a new compact 30° rigid 2.9 mm total diameter hysteroscope scope with a special designed instrument tip for atraumatic passage through the cervical canal was used and the hysteroscope is called after this study “Trophyhysteroscope”. The innovative feature of this hysteroscope is that it can be loaded with accessory sheaths in an active and passive position (Fig. 2). In this way we can start every hysteroscopy with a single flow 2,9 mm instrument, but if necessary the accessory sheet can be moved forward resulting in better closure of the cervical canal in case of leakage, double flow function to re-establish the view and in case of using the operative sheet, surgery with 5 French instruments is made possible (Fig. 3).
Fig. 2. Trophy hysteroscope (1) with diagnostic (2) and operative (3) accessory sheet. Diagnostic sheet in active position providing double flow after visual controlled dilatation (4).
Fig. 3. 5 French instruments used with the Trophy hysteroscope.
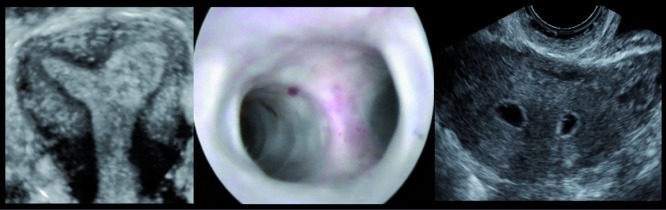
The one-stop uterine diagnosis starts with the transvaginal ultrasound (TvU), followed by a fluid Trophy hysteroscopy using the vagino-cervical atraumatic approach for which no speculum, tenaculum or cervical preparation is used, no analgesia or anaesthesia is necessary. Immediately after the hysteroscopy, a second TvU is performed, taking advantage of the intracavitary fluid for a contrast image of the uterus (Fig. 4).
Fig. 4. One stop uterine diagnosis.
In case of focal endometrial pathology one can use the 5 French instruments to remove the pathology. But an even more interesting feature is the possibility to perform a D&C with the Trophy curette without the need to place a speculum and with the possibility of visual control of the correct tissue removal has been taking place. If necessary the D&C can be repeated, as the accessory sheath stays in place, no discomfort of re-entering instruments through the cervix. This approach is unique and offers possibilities for interventions such as hysteroscopically guided embryo transfer or ultrasound guided endo-myometrial sampling.
In addition, the compatibility of the Trophy hysteroscope with a high-level biodegradable disinfection method, Tristel Fuse®, makes it easy and feasible to implement in the ambulatory environment with a high turnover of procedures.
Importance of hysteroscopy in the infertile patient
Uterine cavity abnormalities are seen as a cause of infertility in around 10% - 15 % of women. In women with recurrent implantation failure abnormalities are found in up to 50% of the women (Pundir and El-Toukhy, 2010).
The major advantage of the hysteroscopic evaluation is the information on the accessibility of the cavity, important for insemination or embryo transfer and the direct visualization of the endometrium and the cavity form. Findings are categorised into major or minor abnormalities according to their influence on the structural change of the cavity (Molinas and Campo, 2006).
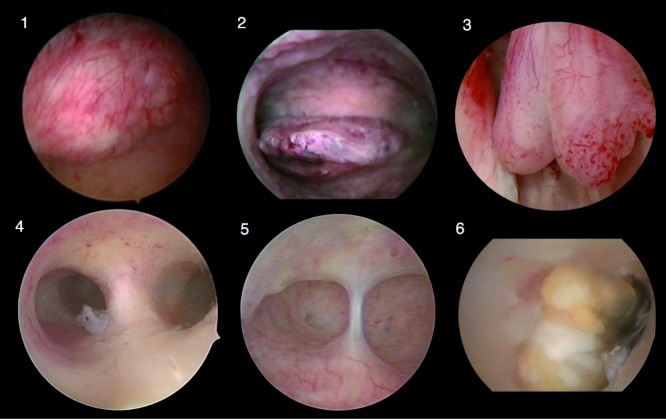
Major abnormalities are arbitrarily defined as those that structurally change the normal hysteroscopic uterine anatomy, like congenital malformations starting from U2 of the new ESHRE/ESGE classification, myoma, large polyps, adhesions and necrotic tissue (Fig. 5) (Grimbizis et al., 2013a, 2013b).
Fig. 5. Hysteroscopic findings, mayor pathologies. (1) Myoma, (2) (3) Endometrial polyp, (4) Uterine septum, (5) Intrauterine adhesions, (6) Placental remnants.
Minor abnormalities or subtle lesions are changes in the uterine cavity without significant anatomical deformation. The pathological significance of those findings still has to be proven, but for research purposes they should be handled differently than the normal and major findings. Examples are the diffuse polyposis, endometrial hypervascularization, strawberry pattern, mucosal elevation, endometrial defects and the subtle cavity malformation classified as U1 (Grimbizis et al., 2013a, 2013b).
A prospective randomized trial has demonstrated that the hysteroscopic findings in the infertile patients are significant different with those of abnormal uterine bleeding patients, not only for the major but also for the subtle lesions. The main findings in infertility patients are congenital malformation, polyps, necrotic tissue and adhesions for the major ones and congenital malformation U1, strawberry pattern, hypervascularisation and necrotic tissue for the subtle one (Fig. 6) (Molinas and Campo, 2006).
Fig. 6. Incidence of findings at hysteroscopy in the infertile and abnormal uterine bleeding patients. Subtle lesions clarification 1. Mucosal elevation, 2. Strawberry pattern, 3. Polyposis, 4. Necrotic tissue, 5. Synechiae.
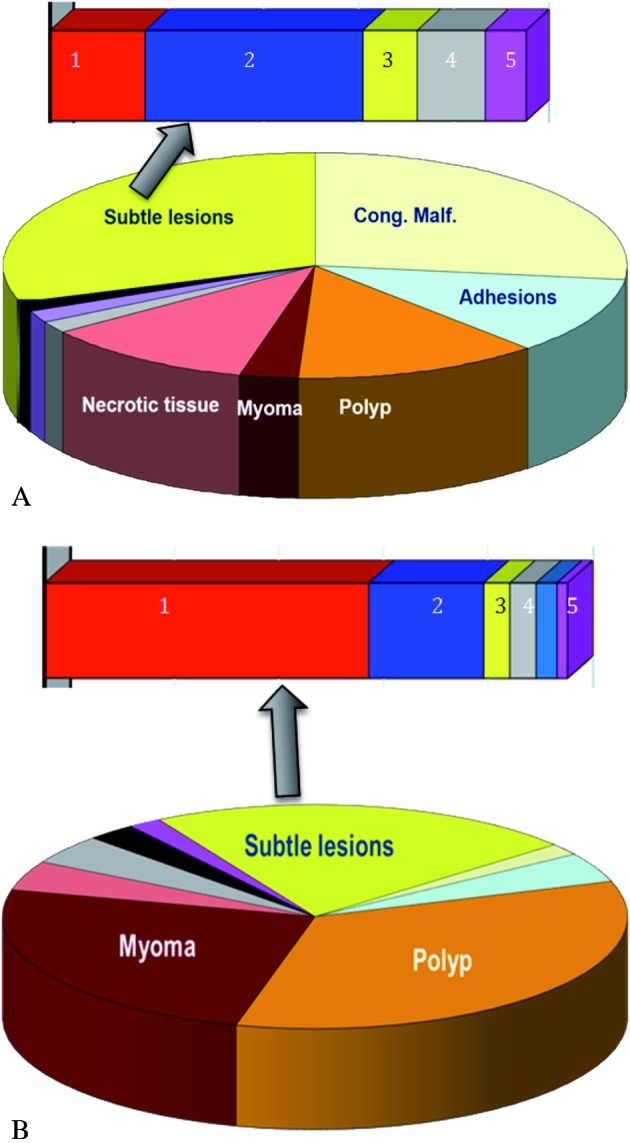
Abnormal uterine bleeding patients have mainly myoma and polyps as major pathology and mucosal elevation as subtle lesion.
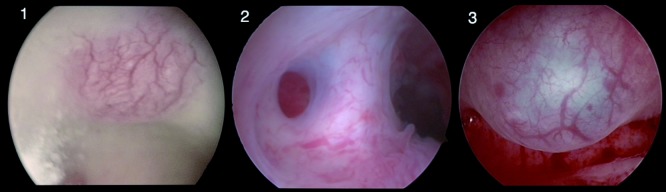
Although subtle lesions do not have a proven significance, they can be seen as either precursors of the pathology or a discrete sign of underlying pathology and as such a guide for sub-endometrial myometrial exploration. For example, focalised hypervascularisation, endometrium defects or cystic haemorrhagic lesions can be correlated with focal or diffuse adenomyosis and as such important for the further management of the infertile patient (Fig. 7) (Molinas and Campo, 2006).
Fig. 7. Subtle lesions.(1) Focal hypervascularization, (2) Cavity deformation, (3) Mucosal elevation.
Conclusion
The simplification of the hysteroscopic technique enlarges our spectrum for the ambulatory screening of the uterus. Hysteroscopy goes hand in hand with Ultrasound as a first-line diagnostic tool to evaluate the uterine reproductive capacities in the infertile patient. Especially the high patient compliance, low complication rate and the possibility of enlarging the visual procedure with eye-directed tissue sampling is seen as the most important progress in the modern hysteroscopic techniques.
The one-stop approach opens a total new and advanced dimension to the screening, diagnosis and treatment of uterine pathology, ensuring the normal structural and most optimal functional conditions of the uterus for embryo implantation and placentation.
References
- kour SH, Jones SE, Donovan P. Ambulatory hysteroscopy: evidence-based guide to diagnosis and therapy. Best Pract Res Clin Obstet Gynaecol. 2006;20:953–975. doi: 10.1016/j.bpobgyn.2006.06.004. [DOI] [PubMed] [Google Scholar]
- Brosens JJ, de Souza NM, Barker FG. Uterine junctional zone: function and disease. Lancet. 1995;346:558–560. doi: 10.1016/s0140-6736(95)91387-4. [DOI] [PubMed] [Google Scholar]
- Campo R, Van Belle Y, Rombauts L, et al. Office mini-hysteroscopy. Hum Reprod Update. 1999;5:73–81. doi: 10.1093/humupd/5.1.73. [DOI] [PubMed] [Google Scholar]
- Campo R, Molinas CR, Rombauts L, et al. Prospective multicentre randomized controlled trial to evaluate factors influencing the success rate of office diagnostic hysteroscopy. Hum Reprod. 2005;20:258–263. doi: 10.1093/humrep/deh559. [DOI] [PubMed] [Google Scholar]
- El Toukhy T, Khalaf Y, Coomarasamy A, et al. A multicentre randomised study of pre-IVF outpatient hysteroscopy in women with recurrent IVF-et failure – the trophy trial. Oral communication. Oral communication, ESHRE 30th Annual Meeting, Munich. 2014
- Grimbizis GF, Gordts S, Di Spiezio-Sardo A, et al. The ESHRE-ESGE consensus on the classification of female genital tract congenital anomalies. Gynecol Surg. 2013;10:199–212. doi: 10.1007/s10397-013-0800-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimbizis GF, Gordts S, Di Spiezio-Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. 28. 2013:2032–2044. doi: 10.1093/humrep/det098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molinas CR, Campo R. Office hysteroscopy and adenomyosis. Best Pract Res Clin Obstet Gynaecol. 2006;20:557–567. doi: 10.1016/j.bpobgyn.2006.01.019. [DOI] [PubMed] [Google Scholar]
- Novellas S, Chassang M, Delotte J, et al. MRI characteristics of the uterine junctional zone: from normal to the diagnosis of adenomyosis. AJR Am J Roentgenol. 2011;196:1206–1213. doi: 10.2214/AJR.10.4877. [DOI] [PubMed] [Google Scholar]
- Pundir J, El Toukhy T. Uterine cavity assessment prior to IVF. Women’s Health. 2010;6:841–848. doi: 10.2217/whe.10.61. [DOI] [PubMed] [Google Scholar]
- Royal College of Obstetricians and Gynaecologists. Best Practice in hysteroscopy. www.evidence.nhs.uk Green top guideline n. 59. 2011