Abstract
Purpose: Ureteral stent removal is a source of patient morbidity. We surveyed 599 patients to evaluate their experiences and identify the preferred method of stent removal.
Materials and Methods: Visitors to a kidney stone website were invited to participate. Respondents were asked how their ureteral stent was removed? Pain during and after the procedure, patient experiences, and preferences regarding stent removal were queried. Chi-square and ANOVA tests were used to identify significant differences among removal methods.
Results: Five hundred seventy-one respondents were included in the study. The majority of stents (44%) were removed by office cystoscopy while 39% had their stents removed by string. Mean pain during stent removal was 4.8 out of 10 with 57% reporting moderate-to-severe pain levels of 4 or more. Removal by office cystoscopy resulted in the highest experienced pain (5.3). Thirty-two percent reported delayed severe pain after stent removal, including 9% who returned for emergency care. Removal by string resulted in more emergency room visits when compared to cystoscopy. Willingness to undergo the same removal technique was lowest for those who underwent office cystoscopy and highest for operating room cystoscopy. Being informed of why a stent was placed and the removal process was of high priority for respondents.
Conclusions: The majority of patients report moderate-to-severe pain with stent removal and a third report delayed significant pain after stent removal. Variations exist in the patient experience with stent removal based on the method used. More research is needed to identify effective ways to prevent or manage stent-removal-related adverse events.
Introduction
Urinary tract stone disease affects ∼10.6% of men and 7.1% of women in the United States.1 Many of these patients ultimately require surgical intervention.2 Stent placement is commonplace at the time of stone surgery, particularly in the setting of ureteroscopy and extracorporeal shockwave lithotripsy. Among patients in the National Health Service (NHS), Hughes and colleagues reported that 74% of patients had some form of ureteral drainage placed after uncomplicated ureteroscopy. In patients who had ureteral stents already in place preoperatively, the majority still had stents placed afterward (65%), only slightly less often than in patients who did not have stents preoperatively.3 A separate study performed by Mangera and Parys found similar results.4 Practice patterns in the United States are similar. Auge and colleagues reported that in a survey of 173 urologists, 80% of urologists placed a stent 50% to 100% of the time after ureteroscopy.5
Ureteral-stent-related morbidity has been extensively reported6–8 but few studies have examined the morbidity related to their removal. As the incidence of stones increases, including in the pediatric population,9–11 urologists need to better understand patients' perception of stent removal in order to minimize its morbidity. We performed a study to help address these questions by comparing the experiences of patients with various methods of stent removal.
Materials and Methods
Visitors to the website www.kidneystoners.org in 2013 were invited to participate in an anonymous survey (Fig. 1). Respondents reported method of stent removal from four choices, including “I pulled it out myself with the dangling string” (self-string); “My physician's office pulled out the stent with the dangling string” (doctor-string); “I had cystoscopy in the clinic to have my stent removed” (office-cysto); or “I had cystoscopy in the operating room to have my stent removed” (OR-cysto). Additional questions examined pain occurring during and after the stent removal procedure, willingness to undergo the same procedure again, and a comparison of the experience to their expectations. Preoperative counseling was assessed by querying preferences regarding being informed about the stent's purpose, the process of stent removal, and whether a video or diagram of stent removal was beneficial. The survey was hosted using Polldaddy.com. Geographic location of respondents was recorded as country from where the survey was accessed. Demographic information was otherwise not obtained in the anonymous survey.
FIG. 1.
Mean pain and recurrent pain, all methods.
Data were summarized with means and proportions. Chi-square and ANOVA tests were used to identify significant associations between responses and removal methods. Analysis was performed using STATA 12.1 (StataCorp, College Station, TX). Overall website activity was obtained using Google Analytics software (Google, Inc., Mountain View, CA). Estimates of demographic information for overall visitors to the website were obtained using Quantcast software (Quantcast Corporation, San Francisco, CA) for the last month of survey participation, December 2013. Quantcast reports that it generates demographic estimates using a combination of a javascript tag that tracks visitors anonymously and an “inference model” to characterize audiences.
Results
During the period of the survey, there were 283,690 unique visitors to the website overall, with 69% from the United States, 7% from the United Kingdom, 6% from India, 5% from Canada, and the remainder from others. Quantcast demographic information for U.S. visitors in December 2013 estimated that visitors to the website were 68% female, 83% Caucasian, and 59% at least college educated. Ages <18 years comprised 17% of visitors, those aged 18 to 24 years were 10%, 25 to 34 years were 19%, 35 to 44 years were 23%, 44 to 54 years were 17%, 55 to 64 years were 9%, and 65+ years were 4%. In terms of household income, $0 to $50k comprised 46% of visitors, $50 to $100k 32%, $100 to $150k 12%, and $150k+ 10%.
Overall survey results
Five hundred ninety-nine individuals responded to the survey between May 15, 2013, and December 30, 2013. Responses that were incomplete were discarded, leaving 571 surveys available. Office-cysto was the most common approach, reported by 44.3% of respondents. OR-cysto was reported by 16.8%, doctor-string was by 27%, and self-string was by 11.9%. The majority of respondents reported being told beforehand that they would have a stent (85.3%) (Table 1).
Table 1.
Respondent Characteristics
| Participant country | ||
| United States | 437 | 77% |
| Canada | 43 | 8% |
| United Kingdom | 31 | 5% |
| Australia/New Zealand | 22 | 4% |
| Asia | 9 | 2% |
| Other European | 11 | 2% |
| Other/unknown | 18 | 3% |
| Total | 571 | |
| Method | ||
| Cystoscopy in clinic | 253 | 44% |
| Doctor's office pulled string | 154 | 27% |
| Cystoscopy in the OR | 96 | 17% |
| I pulled string myself | 68 | 12% |
| Total | 571 | |
| Were you told that you would have a stent? | ||
| No, I was not told | 83 | 15% |
| Yes, I was told | 483 | 85% |
| Total | 566 | |
| Did you experience another episode of severe pain following your stent removal? | ||
| No everything was fine after the stent came out | 200 | 35% |
| Yes, I had a mild attack of pain later | 183 | 32% |
| Yes, I had a severe attack of pain later | 134 | 24% |
| Yes, the pain was bad enough that I went back to the ER | 48 | 8% |
| Total | 565 | |
| Comparing your expectations before your stent removal procedure to what you actually experienced | ||
| Not nearly as bad | 111 | 20% |
| Not as bad | 89 | 16% |
| About what I expected | 150 | 27% |
| A bit worse | 84 | 15% |
| Much worse | 131 | 23% |
| Total | 565 | |
ER=emergency room; OR=operating room.
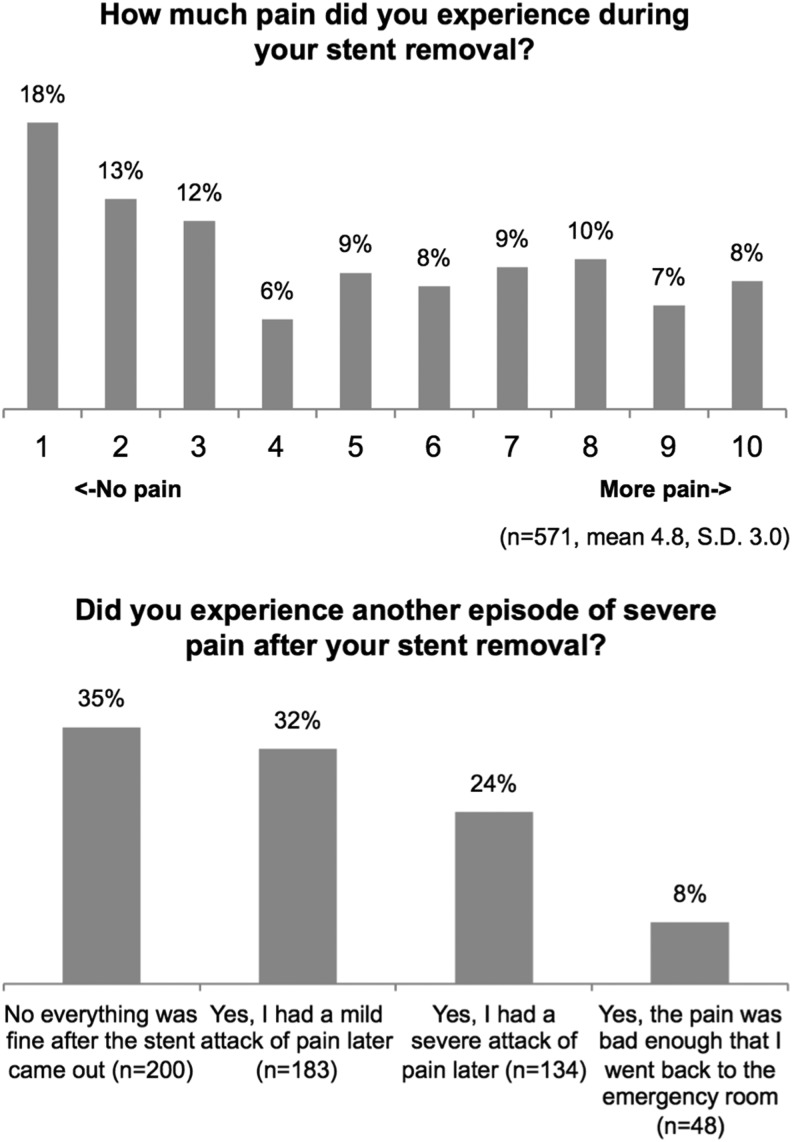
On a scale of 1 to 10, mean reported pain during stent removal was 4.8 (SD=3.0, range=1–10). A third of respondents (35.4%) reported no delayed pain after stent removal, a third (32.3%) reported mild delayed pain, 23.7% reported severe delayed pain, and 8.5% reported severe delayed pain bad enough to cause them to return to an emergency room (ER). Twenty percent reported the experience of stent removal being not nearly as bad as they expected, 16% reported it being not as bad, 27% reported it being about what they expected, 15% reported it being a bit worse, and 23% reported it being much worse (Fig. 1 and Table 1).
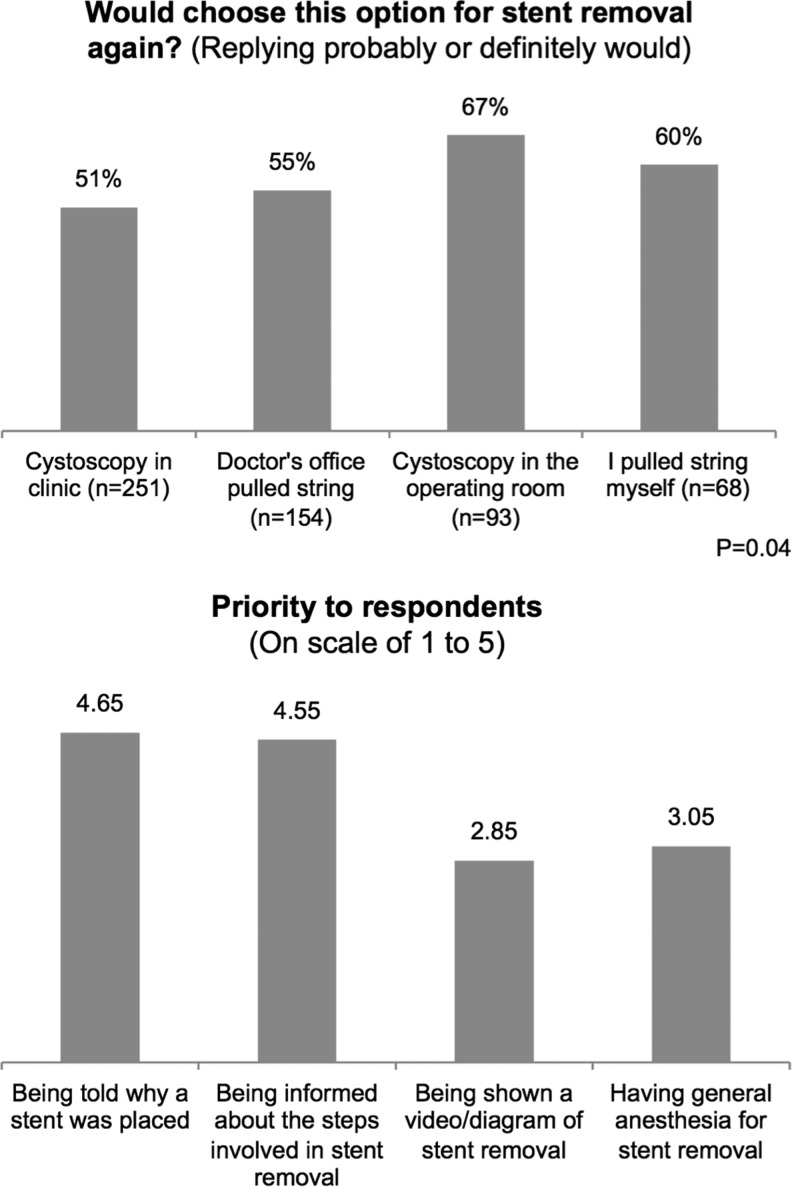
On a scale of 1 to 5, with 5 being “very important,” being told why they had a stent (4.7) and how a stent would be removed (4.6) were both high priorities. Being shown a video or diagram of the stent removal and having the option of general anesthesia were moderate priorities (2.9 and 3.1, respectively) (Fig. 2).
FIG. 2.
Respondent preferences and priorities.
Results by method
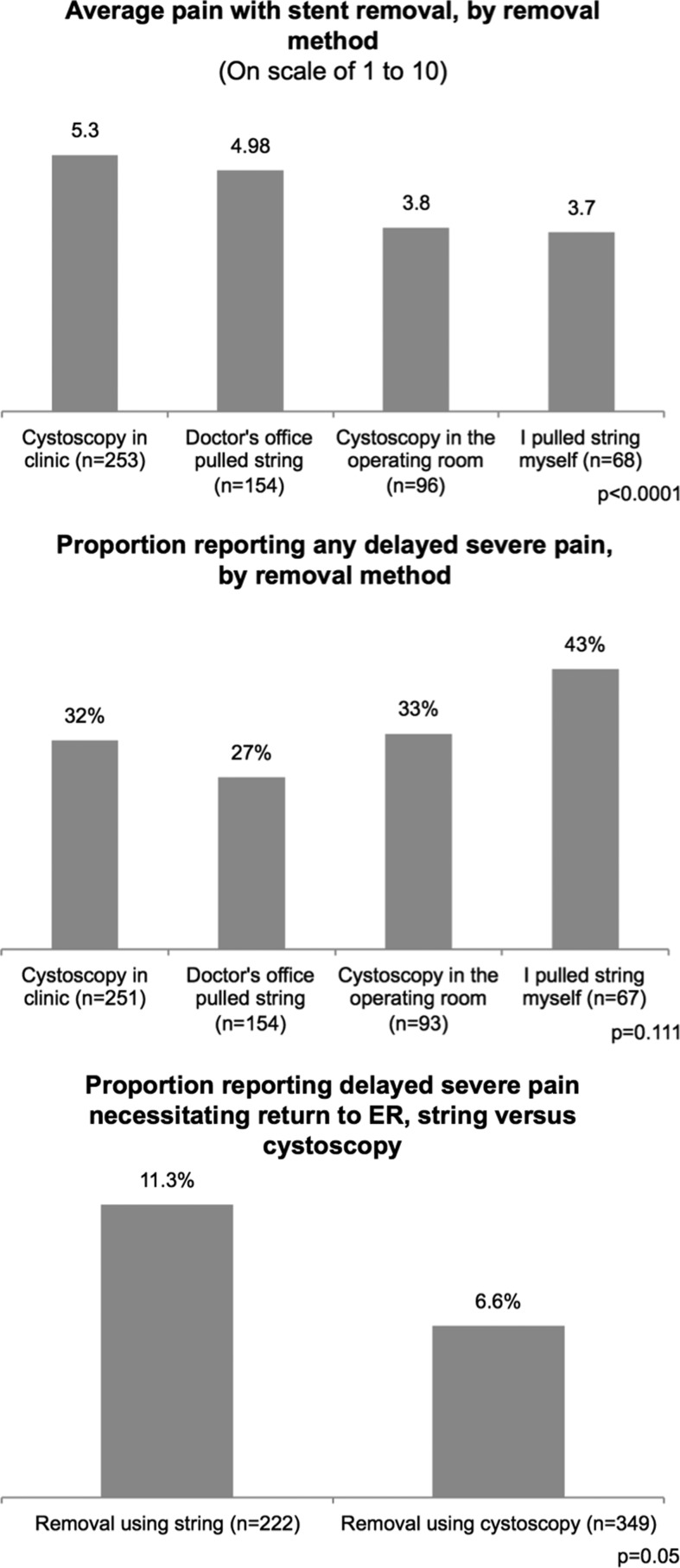
Mean reported pain varied with method of stent removal. Office-cysto was associated with the highest-reported mean pain (5.3), followed by doctor-string (5.0), OR-cysto (3.8), and self-string (3.7; p<0.0001). Many respondents reported minimal or no pain with their stent removal. This varied by procedure, with 36% of office-cysto, 60.4% of OR-cysto, 55.9% of self-string, and 41.6% of doctor-string respondents reporting minimal or no pain (p<0.0001) (Fig. 3).
FIG. 3.
Mean pain and delayed pain, by removal method.
Stent removal by string was more likely to result in severe pain prompting a trip to an emergency department than stent removal by cystoscopy (11.3% vs 6.6%; p=0.05). When examined individually, differences between the four different removal methods did not reach statistical significance. Patients who had their stents removed by self-string had the highest proportion of patients returning to the emergency department for pain (14.71%), followed by doctor-string (9.74%), office-cysto (7.51%), and OR-cysto (4.17%). Delayed episodes of severe pain occurring after stent removal were most frequently reported by those who used the self-string method (43.3%) and less frequently following OR-cysto (33.3%), office-cysto (32.3%), and doctor-string (26.6%). However, this trend did not reach statistical significance (p=0.111) (Fig. 2).
Those who underwent office-cysto were least willing to undergo the same procedure again, with 22.7% reporting “not a chance” in contrast to doctor-string (16.2%), OR-cysto (12.8%), and self-string (11.8%) (p=0.002) (Fig. 3).
Regional variations
The majority of respondents originated from the United States (n=437, 76.5%). Others were from Canada (n=43, 7.5%), United Kingdom (n=31, 5.4%), Australia/New Zealand (n=22, 3.9%), other European (n=11, 1.9%), Asia (n=9, 1.6%), and other/unknown (n=18, 3.2%). The last three groups were combined for analysis due to the small numbers in each (Table 1).
Mean reported amount of pain with stent-removal did not differ in a significant fashion between regions (4.8, 4.3, 4.4, and 5.1; ANOVA p=0.56 for United States, Canada, United Kingdom, and “other” countries). The approach to stent-removal reported by respondents varied significantly by country. Patients in the United States and United Kingdom were more likely to undergo office-cysto for stent removal (47.6% and 51.6%) as compared with Canada and “other” countries (23.3% and 31.7%). Stent-removal in the OR was performed most often in the United Kingdom and “other” countries (41.9% and 40%). Canada and the United States had significantly smaller rates (23.3% and 11.2%). Self-string was most common in Canada (25.6%), followed by the United States (12.6%). It was rare in “other” countries (3.3%) and was not reported by respondents from the United Kingdom (0%). Doctor-string was rare in the United Kingdom (6.5%) but was more common in the other regions (28.6%, 27.9%, and 25% in the United States, Canada, and “other” countries, respectively).
Canadians and respondents from the United Kingdom were less likely to report that being told why they had a stent was “very important” (60.5% and 63.3% vs 72% and 80% for the United States and “other” countries; p=0.002). Canadians were less likely to report that having the option of general anesthesia for stent removal was “very important” (16.3% for Canada vs 28.7%, 34.5%, and 36.7% for United States, United Kingdom, and “other” countries; p=0.014). There were no significant regional variations in priorities of being told how a stent is removed or being shown a diagram or video of stent removal.
Discussion
Although studies have previously called into question the necessity of ureteral stenting after uncomplicated lithotripsy,8,12 postoperative stent placement remains common and the question of whether to stent remains unresolved.13 The results of this survey identify the morbidity that can be associated with stent removal and provides insight into the experiences and preferences of urologic patients who undergo these procedures.
The majority of patients reported moderate-to-severe levels of pain with stent removal, with an overall mean pain of 4.8 on a scale of 1 to 10. Office cystoscopy resulted in the highest mean pain, followed by use of a dangler-string in the office. Although the presumption is that stent removal by string in the office is more benign than cystoscopy, our data do not support this notion, with both methods reporting similar pain levels. Methods that reported lowest mean pain were self-removal via dangler-string at home and OR cystoscopy. Across all the methods, there was also a significant proportion of respondents (43%) who reported minimal or no pain. Few prior studies have examined pain during stent removal. The studies that have been done have found no significant differences in pain between patients who had their stents removed by cystoscopy or extraction string. Kuehhas and colleagues reported that in their patients, pain during rigid cystoscopic stent removal was similar to that for office stent string removal.14 They did not evaluate self-removal or OR removal of stents. Barnes and colleagues reported similar findings in their study.15 In their prospective, randomized study, they found no difference in visual analog pain scores between patients who had stents removed by cystoscopy and those who had theirs removed by stent string.
In addition to examining pain, we assessed patient preferences. Removal of the stent by office-cystoscopy was the least-preferred method. Conversely, having patients pull out their own stent and operating room cystoscopy, with the patient receiving some form of anesthesia, had the highest proportion of patients reporting that they would be willing to undergo the same procedure. We recognize that the choice of a specific method can be influenced by multiple factors, including cost, resources, and the risk of accidental dislodgement when a string is left in place.12
Delayed pain after stent removal appears to be underappreciated by physicians. As a result, patients often report that they were not adequately counseled about this potential morbidity. We found that delayed pain occurring after removal of a ureteral stent was an important source of patient morbidity, with a third of patients surveyed reporting delayed severe pain after stent removal, including the 8% who reported having to return to an emergency department. Removal by stent-string was significantly more likely to result in a return trip. No studies have examined this difference but there is a possibility that the string itself may contribute to physiologic changes that lead to delayed pain after stent removal, such as trigonal edema. More studies are needed to examine this difference.
Investigators have started to examine how to prevent delayed pain in all patients who have stents removed. Tadros and colleagues previously examined poststent removal pain and found that NSAIDs may help in its prevention.16 In their randomized, double-blind controlled trial, they found a significant reduction in poststent removal pain with the administration of a COX-2 inhibitor prior to cystoscopy to remove the stent. Fifty-five percent of participants who were given the placebo experienced severe pain, while in the medicated group, no patients reported severe pain (p<0.01). Though the study used a small sample size, it establishes the foundation for larger studies to examine the utility of preventative measures.
Interestingly, we found that there were significant differences in pain between self-string and doctor-string removal. We suspect that increased anxiety or a heightened anticipation of pain in the presence of a practitioner may contribute to these differences. A similar phenomenon has been reported in patients who undergo prostate biopsy.17 Patients who had increased preprocedure anxiety experienced greater intraprocedural pain, due to a heightened adrenergic response causing hyperalgesia and hypersensitization of pain receptors.18,19 Conversely, in patients who remove their stents at home, the ability to remove the stents themselves may have a calming effect. However, these patients also reported the highest frequency of delayed episodes of severe pain, potentially due to less certainty about recurrent pain. Selection bias may also have a role in the difference observed with patients who have greater baseline anxiety electing to have their stents removed in the urologist office. Better counseling patients about what to expect after their stent self-removal and recommending premedication with an NSAID may help to allay this anxiety and prevent the pain.
We found variations in the method of stent removal by region. Patients were more likely to undergo office cystoscopy in the United States while in Canada removal by string was the preferred technique. In Austria, Kuehhas and colleagues reported that, in their experience of removing stents via rigid cystoscopy without anesthesia, the mean pain experienced was relatively low.14 In spite of these results, they have started to remove stents via string, signaling a potential paradigm shift toward the self-string method. Similar calls have been made in the United Kingdom.3
This study has several strengths, including a large sample size and by virtue of its website-based recruitment, a more diverse population geographically and in practice settings than would typically be available in an academic cohort of patients. This may make the results more reflective of the experiences of urology patients overall. There were also limitations. In this anonymous survey, we did not collect demographic data and therefore cannot assess whether stent-removal experiences differ by gender, age, and race. We also do not have data available on the length of time stents were in place or the reasons why stents were placed. We were not able to determine whether rigid or flexible cystoscopy was used during cystoscopic removal of stents or whether any adjunctive medications or local anesthesia was used. It is possible that reporting errors may exist for the method of stent removal. Respondents may not have understood the difference between an OR and a clinic procedure room or there may be variations in the use of these terms by region. These results may also have been influenced by response bias. Website visitors and respondents to the survey may not be representative of all patients who undergo stent removal. However, respondents to the survey aligned remarkably well with other existing research on stent removal that polled urologists instead, suggesting that the respondents are indeed representative. Auge and colleagues reported that U.S. urologists utilized office-cysto (42%), doctor-string (37%), and self-string (9%)5 while methods reported in this survey were office-cysto (44%), doctor-string (27%), OR-stent (17%), and self-string (12%). Despite these limitations, this study provides novel information on the morbidity of stent removal and the related preferences of patients. Most importantly, it identifies a need to address pain after the ureteral stent is removed in a significant portion of patients. This information can help guide patient counseling regarding stent removal and future studies.
Conclusions
There is moderate morbidity associated with ureteral stent removal and variations exist between different removal methods. When indicated, having patients remove their stent themselves via string can be associated with less procedural pain but may also be associated with a higher chance of severe delayed pain necessitating an ER visit. Properly counseling patients about why a stent needs to be placed, how it will be removed, and the risk of a delayed episode of pain occurring after stent removal may improve the experience of stent removal for patients. Additional research is necessary to identify optimal approaches to minimizing stent-removal morbidity.
Abbreviations Used
- ANOVA
analysis of variance
- ER
emergency room
- OR
operating room
- SD
standard deviation
Disclosure Statement
No competing financial interests exist.
References
- 1.Scales CD, Jr., Smith AC, Hanley JM, Saigal CS. Urologic Diseases in America Project. Prevalence of kidney stones in the united states. Eur Urol 2012;62:160–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. In: Litwin MS, Saigal CS, eds. Washington, DC: US Government Printing Office, 2012, NIH Publication No. 12–7865 [Google Scholar]
- 3.Hughes B, Wiseman O, Thompson T, et al. The dilemma of post-ureteroscopy stenting. BJU Int 2014;113:184–185 [DOI] [PubMed] [Google Scholar]
- 4.Mangera A, Parys B. BAUS section of endourology national ureteroscopy audit: Setting the standards for revalidation. J Clin Urol 2013;45–49 [Google Scholar]
- 5.Auge BK, Sarvis JA, L'esperance JO, Preminger GM. Practice patterns of ureteral stenting after routine ureteroscopic stone surgery: A survey of practicing urologists. J Endourol 2007;21:1287–1291 [DOI] [PubMed] [Google Scholar]
- 6.Joshi HB, Stainthorpe A, MacDonagh RP, Keeley FX, Jr., Timoney AG, Barry MJ. Indwelling ureteral stents: Evaluation of symptoms, quality of life and utility. J Urol 2003;169:1065–1069; discussion 1069. [DOI] [PubMed] [Google Scholar]
- 7.Keeley FX, Jr., Timoney AG. Routine stenting after ureteroscopy: Think again. Eur Urol 2007;52:642–644 [DOI] [PubMed] [Google Scholar]
- 8.Pengfei S, Yutao L, Jie Y, et al. The results of ureteral stenting after ureteroscopic lithotripsy for ureteral calculi: A systematic review and meta-analysis. J Urol 2011;186:1904–1909 [DOI] [PubMed] [Google Scholar]
- 9.Routh JC, Graham DA, Nelson CP. Epidemiological trends in pediatric urolithiasis at united states freestanding pediatric hospitals. J Urol 2010;184:1100–1104 [DOI] [PubMed] [Google Scholar]
- 10.Bush NC, Xu L, Brown BJ, et al. Hospitalizations for pediatric stone disease in united states, 2002–2007. J Urol 2010;183:1151–1156 [DOI] [PubMed] [Google Scholar]
- 11.Kairam N, Allegra JR, Eskin B. Rise in emergency department visits of pediatric patients for renal colic from 1999 to 2008. Pediatr Emerg Care 2013;29:462–464 [DOI] [PubMed] [Google Scholar]
- 12.Bockholt NA, Wild TT, Gupta A, Tracy CR. Ureteric stent placement with extraction string: No strings attached? BJU Int 2012;110:E1069–E1073 [DOI] [PubMed] [Google Scholar]
- 13.Tang L, Gao X, Xu B, et al. Placement of ureteral stent after uncomplicated ureteroscopy: Do we really need it? Urology 2011;78:1248–1256 [DOI] [PubMed] [Google Scholar]
- 14.Kuehhas FE, Miernik A, Sharma V, et al. A prospective evaluation of pain associated with stone passage, stents, and stent removal using a visual analog scale. Urology 2013;82:521–525 [DOI] [PubMed] [Google Scholar]
- 15.Barnes KT, Bing MT, Tracy CR. Do ureteric stent extraction strings affect stent-related quality of life or complications after ureteroscopy for urolithiasis: A prospective randomised control trial. BJU Int 2014;113:605–609 [DOI] [PubMed] [Google Scholar]
- 16.Tadros NN, Bland L, Legg E, Olyaei A, Conlin MJ. A single dose of a non-steroidal anti-inflammatory drug (NSAID) prevents severe pain after ureteric stent removal: A prospective, randomised, double-blind, placebo-controlled trial. BJU Int 2013;111:101–105 [DOI] [PubMed] [Google Scholar]
- 17.Zisman A, Leibovici D, Kleinmann J, Siegel YI, Lindner A. The impact of prostate biopsy on patient well-being: A prospective study of pain, anxiety and erectile dysfunction. J Urol 2001;165:445–454 [DOI] [PubMed] [Google Scholar]
- 18.Tsivian M, Qi P, Kimura M, et al. The effect of noise-cancelling headphones or music on pain perception and anxiety in men undergoing transrectal prostate biopsy. Urology 2012;79:32–36 [DOI] [PubMed] [Google Scholar]
- 19.Khasar SG, McCarter G, Levine JD. Epinephrine produces a beta-adrenergic receptor-mediated mechanical hyperalgesia and in vitro sensitization of rat nociceptors. J Neurophysiol 1999;81:1104–1112 [DOI] [PubMed] [Google Scholar]