Abstract
STUDY DESIGN
Longitudinal cross-sectional study.
BACKGROUND
In the early stages after total knee arthroplasty (TKA), quadriceps strength of the operated limb decreases and is substantially less than that of the nonoperated limb. This asymmetry in strength is related to asymmetrical movement patterns that increase reliance on the nonoperated limb. Over time, quadriceps strength in the operated limb increases but remains less than that in age-matched controls without knee pathology, whereas the quadriceps strength in the nonoperated limb gradually decreases. The purpose of this study was to investigate the changes in quadriceps strength and function of both limbs up to 3 years after TKA and to evaluate change in interlimb kinematic and kinetic parameters over time compared to that in age-matched individuals without knee pathology.
METHODS
Fourteen individuals after TKA and 14 healthy individuals matched for age, weight, height, and sex participated in the study. Outcome measures included kinematics, kinetics, quadriceps strength, and functional performance.
RESULTS
In participants who underwent TKA, quadriceps strength was significantly different between limbs at 3 months and 1 year after TKA, but not at 3 years after TKA. In this group, there was also a significant improvement in self-reported function between 3 months and 1 year after TKA, but a significant decrease between years 1 and 3 for the physical component summary score of the Medical Outcomes Study 36-Item Short-Form Health Survey. In the TKA group, there were few interlimb differences in joint kinematics and kinetics 3 years after TKA, which may be attributed to a combination of worsening in the nonoperated limb, as well as improvement in the operated limb. Differences between participants without knee pathology and those 3 years after TKA still existed for kinematic, kinetic, and spatiotemporal variables.
CONCLUSION
As interlimb differences in quadriceps strength decrease after TKA, there are concomitant symmetrical improvements in temporospatial and kinetic gait parameters. The symmetry 3 years after TKA in quadriceps strength is primarily the result of progressive weakness in the nonoperated limb.
Keywords: biomechanics, joint replacement, walking
Knee osteoarthritis is a common degenerative condition that is typified by joint pain, quadriceps weakness, and altered movement patterns. Total knee arthroplasty (TKA), which improves functional ability, reduces pain, and restores anatomical alignment of the tibiofemoral joint, is the most common surgical intervention for end-stage knee osteoarthritis.8,9,16,24 Despite these improvements, quadriceps weakness of the operated limb persists after surgery. Compared to the nonoperated limb, quadriceps strength has been shown to reduce by 40% 1 month after TKA, and patients during this time have demonstrated a 17% activation deficit.19 The disparity in quadriceps strength between limbs decreases 1 to 2 years after TKA, but this apparent symmetry in strength between limbs is a result of not only increased quadriceps strength in the operated limb but also a progressive decline of quadriceps strength in the nonoperated limb.33
Differences in strength between limbs also result in asymmetrical movement patterns during dynamic activities. After TKA, patients adopt asymmetrical movement patterns that result in attenuated motion in the operated limb and potentially increased loads in the nonoperated limb.1 These asymmetrical movement patterns are most apparent in the early recovery phase, and the extent of these alterations is dependent on the weakness of the operated limb, with greater weakness contributing to greater asymmetries.32 Three months after TKA, patients continue to demonstrate differences in strength,19 ambulate with less knee flexion excursion on the operated limb, and place higher loads on the nonoperated limb during sit-to-stand movements.8,20 However, when quadriceps strength equalizes 1 year after TKA, joint excursions and movement patterns become more symmetrical between limbs.32 Despite this improved symmetry over time, the gait patterns of persons following TKA still differ from those of age-matched healthy individuals.17,25
After TKA, the decline in strength of the nonoperated limb occurs faster than that attributable to age alone.7 This loss of strength is exemplified by a reduction in the contribution of the knee extensor moment during loading response in the nonoperated limb by 1 year after TKA.32 As a result, bilateral strength deficits may underlie the gait abnormalities in patients after TKA compared to age-matched healthy individuals.
Therefore, the purpose of this study was 2-fold. The first aim was to determine whether kinematic and kinetic differences between limbs are resolved as quadriceps strength becomes more symmetrical over time in subjects after TKA. The second aim was to compare gait patterns in patients after TKA to those in healthy individuals matched for age, sex, weight, and height.
First, we hypothesized that individuals who had TKA would demonstrate significantly different kinematic and kinetic gait parameters between limbs 3 months postsurgery, but that these differences would not be present 3 years after TKA. Second, we hypothesized that individuals after TKA would demonstrate significant improvements in movement patterns of the operated limb as quadriceps strength increased over time, whereas movement patterns of the nonoperated limb 3 years after TKA would be significantly different from those of control subjects, as quadriceps weakness after TKA in the nonoperated limb advances faster than weakness associated with age alone.
METHODS
Subjects
Patients who underwent primary unilateral TKA (not revision) were recruited from a group of local orthopaedic surgeons. Potential candidates were 50 to 85 years of age. Exclusion criteria were (1) evidence of musculoskeletal impairments other than the TKA that affected functional daily activities, (2) body mass index (BMI) greater than 40 kg/m2, (3) uncontrolled hypertension, (4) diabetes mellitus, (5) neoplasms, (6) neurological disorders, (7) knee flexion contracture greater than 5°, (8) inability to actively flex the operated knee to 75° at 3 months after the surgery, and (9) a symptomatic contralateral limb, operationally defined as self-reported maximal daily knee pain of 4 or more on a 0-to-10 verbal rating scale, pain that interfered with daily activity, or plans for a knee surgery.
A control group of healthy individuals between the ages of 50 and 85 years, without evidence of neurological or musculoskeletal impairments on either lower limb, was recruited from the same geographic region as those with TKA. Three months post-TKA, control subjects were individually matched to those with TKA based on age (±5 years), sex, height (±5%), and body weight (±5%). In the control subjects, the lower extremity considered the “operated limb” corresponded to the side (left or right) of the TKA on the matched subjects.
The subjects in the TKA group were assessed, including motion analysis, at baseline (3 months post-TKA) and at 1 year and 3 years after TKA. Healthy subjects were tested at baseline and at a follow-up session 2 to 3 years later. All subjects signed a written informed consent form approved by the Human Subjects Review Board of the University of Delaware prior to participation in any facet of the study. Weight and height, measured on the same annually calibrated scale, and BMI were recorded for each subject. The University of Delaware Osteoarthritis Profile was used to assess function, strength, and range of motion.18 This battery of tests includes self-report of function questionnaires, clinical tests of strength and motion, and objective functional measures, which are described in detail below. Postoperative rehabilitation for all individuals in the TKA group consisted of 8 weeks of physical therapy intervention that commenced approximately 1 month after surgery.23 The focus of the rehabilitation program was on progressive quadriceps strengthening, modalities to reduce pain and inflammation, manual therapy to improve joint range of motion, and functional retraining.23 All patients in the TKA group were treated in the same physical therapy clinic by therapists who adhered to the standardized and progressive rehabilitation protocol.
Clinical Assessments
The Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) is a questionnaire used to measure health-related quality of life. The physical component summary (PCS) of the SF-36 measures the physical status of the patient, whereas the mental component summary measures the mental status of the patient.12,29 The SF-36 is a normative test, so a score of 50 represents the average score of the US population in 1998.13 The activities of daily living subscale of the Knee Outcome Survey (KOS-ADL) is a knee-specific questionnaire that evaluates self-reported functional ability during daily activities.11 It is a 14-item Likert-scale questionnaire that is reported as a percentage, with 100% being the highest possible score.
Knee flexion and extension range of motion were measured using a standard long-arm goniometer, with the subjects in the supine position. A soft block was placed under the heel during knee extension measurements to allow full range of motion.19
Performance-based functional testing included the timed up-and-go test (TUG), the stair-climbing test (SCT), and the 6-minute walk test (6MW). The TUG is a measure of the time it takes to rise from an arm chair (seat height, 46 cm), walk 3 m, turn, and return to sitting in the same chair. Subjects were asked to walk as quickly as possible, while remaining safe and comfortable. The average of 2 trials was recorded, and the subjects were allowed to use the arms of the chair if needed. The TUG is a reliable and valid tool for quantifying the functional mobility of patients after TKA.2,3,15,19,31 The SCT measures the time it takes to ascend and descend a flight of 12 seven-in (17.78-cm) steps. The subjects were asked to ascend and descend the flight of steps as quickly as possible, while remaining safe and using the rail if needed, starting at the investigator’s command. The average of 2 trials was recorded.23 The 6MW was originally an endurance test for patients with cardiopulmonary diseases; however, the use of this test has been shown to be reliable for testing general mobility in individuals after TKA.4–6,13–15,21–23 During the 6MW, subjects were asked to walk as far as possible for 6 minutes in a square course (1 lap was 157.27 m). Patients received verbal feedback on time elapsed at 2, 4, and 5 minutes.27 Previously reported minimum clinically important differences in these mobility tests are 2.49 seconds for the TUG, 5.49 seconds for 9 steps of the SCT, and 61.3 m for the 6MW.15
Quadriceps Strength and Muscle Activation Measurement
Maximal voluntary isometric contraction of the quadriceps femoris muscle was measured with a burst superimposition technique.26 Subjects were seated in a dynamometer (Kin-Com 500H; Isokinetic International, Chattanooga, TN), with the hip approximately flexed to 90° and the knee flexed to 75°. The seat was adjusted to align the axis of the dynamometer to the axis of the knee joint.26 The ankle attachment was placed 5 cm proximal to the lateral malleolus. Two 7.6 × 12.7-cm self-adhesive electrodes (ConMed Corporation, Utica, NY) were placed over the quadriceps femoris, near the motor points of the vastus medialis and proximal rectus femoris, to deliver the electrical stimulation (10 pulses, 100-pulse-per-second train, 600-microsecond pulse duration, 135 V) during maximal voluntary isometric contraction, via a grass stimulator (S48 Square Pulse Stimulator; Astro-Med, Inc, West Warwick, RI). Subjects performed practice sessions at 50%, 75%, and 100% of their maximum contraction, to become familiar with the testing procedure and to warm up. A rest of approximately 2 to 3 minutes was provided between practice trials to prevent fatigue. Data collection began after the practice trials and a 5-minute rest. On the investigator’s command, subjects were instructed to maximally contract the quadriceps muscle by pushing against the resistance pad of the dynamometer for several seconds. Verbal encouragement and visual representation of their force output target on the dynamometer were used to motivate the subjects to produce a maximum force at each trial. The knee extension force was measured and recorded using custom-written software (LabVIEW Versions 4.0.1 and 5.0; National Instruments Corporation, Austin, TX) at a 200-Hz sampling rate. If maximal voluntary force output was achieved (if there was no difference between the voluntary force and the stimulated superimposed burst force), then the testing session was completed for that limb; otherwise, a total of 3 trials were collected. The highest volitional force was used for analysis, with force (in Newtons) normalized to BMI to offset differences in anthropometry of individuals. The nonoperated limb was tested, followed by the operated limb. For the healthy subjects, the order of testing for the limbs was randomized. The central activation ratio was calculated as the force produced during the maximal voluntary isometric contraction, divided by the maximal force produced during the burst superimposition.
Gait Analysis
Gait analysis was performed with an 8-camera motion analysis system (Vicon Peak Version 5.1; OMG plc, Oxford, UK) with 2 force plates (Bertec Corporation, Columbus, OH). Kinematic and kinetic recordings were synchronized for simultaneous collection at 120 and 1080 Hz, respectively. Fourteen-millimeter retro-reflective markers were placed bilaterally on the head of the fifth metatarsal, lateral malleolus, lateral femoral condyle, greater trochanter, and iliac crest. Rigid thermoplastic shells with 4 markers oriented orthogonally were secured with elastic wraps (Fabrifoam SuperWrap; Isokinetics Inc, De Queen, AR) bilaterally to the shank and thigh to minimize movement artifact. To track pelvis movement, a triangular shell was placed at the midline over the sacrum. Two markers were located on the heel counter of the shoes, and a marker on the head of the fifth metatarsal was used to track the 3-D movement of the foot.
Standing calibration was performed prior to walking trials to identify joint centers with respect to the coordinate system of each segment. Following the standing calibration, the subjects practiced walking along a 10-m walkway at a self-selected pace until they could walk at a consistent velocity, as measured by 2 photoelectric cells placed 2.86 m apart. A total of 10 successful walking trials were recorded. A successful trial was defined as a trial in which the subjects contacted opposing force platforms with each foot, without evidence of targeting. Walking velocity was maintained between 95% and 105% of the average gait speed measured during practice trials.
Marker trajectories were filtered at 6 Hz, and kinetic data were low-pass filtered at 40 Hz. Sagittal plane hip, knee, and ankle angles were calculated using rigid-body analysis employing Euler angles, and joint kinetics were calculated based on inverse dynamics and expressed as net internal moments normalized to body weight times height (kg × m). Calculations were performed in Visual3D Version 3.79 (C-Motion, Inc, Germantown, MD). For each trial, stance phase was normalized to 100 points, calculated from the point at which the vertical component of the ground reaction force crossed a threshold of 20 N. Loading response was defined as the time from heel strike to peak knee flexion on the limb during stance. Gait speed, step width, double support time, stride length, cadence, and percentage of stance phase normalized to a gait cycle were analyzed as the temporospatial parameters. To assess gait patterns during loading response, the following were also analyzed: hip, knee, and ankle joint angles at both initial contact and peak knee flexion; hip, knee, and ankle internal moments at peak knee flexion; and the first peak vertical ground reaction force.
Statistical Methods
The G*Power calculator (Heinrich Heine University, Düsseldorf, Germany) was used to determine sample-size estimates based on means and standard deviations of a previous study.32 For clinical assessment and gait analysis outcome measures, the alpha level was set at .05 and the power at 80%. Based on our power analysis, 12 and 10 subjects in each group were necessary for aims 1 and 2, respectively. To address the first aim (interlimb differences over time in the subjects after TKA), differences between limbs over time were assessed using 2-by-3 (limb-by-time) 2-way repeated-measures analysis of variance (ANOVA). The factor of limb had 2 levels (operated limb and nonoperated limb) and the factor of time had 3 levels (baseline [3 months], 1 year, and 3 years post-TKA). The Mauchly test was applied prior to the main ANOVA to detect whether the variances at each testing time were equal. When the assumption of sphericity was violated, Huynh-Feldt corrections were applied. In the presence of a significant interaction effect, follow-up paired t tests were used for post hoc analysis to compare differences between limbs and time points. In the absence of significant interaction, main effects of limb and time were assessed. Metrics that were not limb-specific (SF-36, KOS-ADL, TUG, SCT, 6MW, knee range of motion, gait speed, step width, and double support time) were evaluated using a 1-way repeated-measures ANOVA to determine changes over time.
To address the second aim of the study, differences between the TKA group and control group were assessed using 2-by-2 (time-by-group) 2-way mixed-model ANOVAs. The within-group factor of time had 2 levels (baseline [3 months] and 2 to 3 years post-TKA), and the between-group factor of group had 2 levels (TKA and control). To detect changes for gait patterns, quadriceps strength, and muscle activation in each limb (the surgical side in the TKA group and the matched side in the control group; the nonsurgical side in the TKA group and its matched side in the control group), separate ANOVAs were performed. In the presence of a significant interaction, follow-up t tests were used for post hoc analysis. Main effects of group and time were tested when there was no significant interaction.
RESULTS
Between-Limb Comparisons Over Time in the TKA Group (Aim 1)
Functional Performance Metrics
Thirteen subjects after TKA completed all testing sessions. One subject did not return for the 1-year follow-up testing session (TABLE 1). The SF-36 PCS showed a significant change over time (F2,23 = 5.396, P = .012). Follow-up testing revealed that the SF-36 PCS significantly improved between 3 months and 1 year after TKA (P = .008) and decreased between 1 year and 3 years following TKA (P = .040). The KOS-ADL score significantly increased over time (F2,23 = 3.993, P = .032), but follow-up testing revealed that this change was only significant between 3 months and 1 year (P = .011). There was no significant difference in 6MW scores over time (F2,23 = 0.366, P = .358); however, the TUG and SCT times became significantly faster between 3 months and 1 year after TKA (TUG, P = .010; SCT, P = .001), with no further changes between 1 and 3 years (TUG, P = .263; SCT, P = .070).
TABLE 1.
Subject Information for Aim 1 (n = 13)*
| 3 mo | 1 y | 3 y | |
|---|---|---|---|
| Height, m | 1.72 ± 0.08 | … | … |
| Weight, kg | 91.9 ± 10.6 | 91.1 ± 10.9 | 89.9 ± 10.9 |
| BMI, kg/m2 | 31.0 ± 4.1 | 30.8 ± 4.2 | 30.4 ± 4.0 |
| SF-36 PCS | 45.2 ± 8.0 | 52.2 ± 4.4† | 46.0 ± 8.7‡ |
| SF-36 MCS | 58.0 ± 5.3 | 58.2 ± 4.4 | 56.9 ± 4.2 |
| KOS-ADL | 0.81 ± 0.10 | 0.88 ± 0.09‡ | 0.88 ± 0.09 |
| TUG, s | 7.4 ± 1.3 | 6.9 ± 1.4† | 7.0 ± 11.3 |
| SCT, s | 11.3 ± 3.0 | 10.1 ± 2.3† | 10.2 ± 2.1 |
| 6MW, m | 581.1 ± 109.5 | 580.2 ± 172.8 | 615.2 ± 113.8 |
| Knee e-AROM, deg§ | 1.6 ± 2.4 | –0.2 ± 3.4‡ | –2.1 ± 3.7 |
| Knee f-AROM, deg | 119.5 ± 8.9 | 124.7 ± 6.9‡ | 128.5 ± 8.3‡ |
| MVIC, N/BMI | |||
| Operated | 18.4 ± 7.4‖ | 21.2 ± 9.2‡¶ | 19.8 ± 7.5 |
| Nonoperated | 27.8 ± 9.7 | 25.9 ± 11.2 | 21.5 ± 9.8‡ |
| CAR, % | |||
| Operated | 92.5 ± 4.7 | 93.2 ± 7.1 | 90.6 ± 9.8 |
| Nonoperated | 92.2 ± 6.2 | 90.4 ± 6.5 | 89.0 ± 8.8 |
Abbreviations: 6MW, 6-minute walk test; BMI, body mass index; CAR, central activation ratio; e-AROM, extension active range of motion; f-AROM, flexion active range of motion; KOS-ADL, Knee Outcome Survey activities of daily living subscale; MCS, mental component summary; MVIC, maximum voluntary isometric contraction; PCS, physical component summary; SCT, stair-climbing test; SF-36, Medical Outcomes Study 36-Item Short-Form Health Survey; TUG, timed up-and-go test.
Values are mean ± SD.
Significant difference from the previous session (P<.01).
Significant difference from the previous session (P<.05).
Negative direction of e-AROM indicates hyperextension of the knee.
Significant difference from the nonoperated limb (P<.01).
Significant difference from the nonoperated limb (P<.05).
Range of Motion and Strength
Knee extension range of motion (TABLE 1) on the operated limb significantly increased over time (F2,23 = 7.087, P = .004), with the changes being significant between 3 months and 1 year after TKA (P = .017) and nonsignificant from 1 year to 3 years after TKA (P = .129). Significant improvements were found for knee flexion range of motion of the operated limb over time (F1.4,16.3 = 7.606, P = .009), and these improvements were significant between 3 months and 1 year (P = .032) and between 1 year and 3 years (P = .028) after TKA.
There was a significant time-by-limb interaction for quadriceps strength (F2,23 = 10.840, P<.001). Compared to the nonoperated limb, the quadriceps in the operated limb was significantly weaker at 3 months and 1 year after TKA (3 months, P<.001; 1 year, P = .014), but not at 3 years after TKA (P = .064). After TKA, quadriceps strength in the operated limb significantly increased by 13% between 3 months and 1 year (P = .035), but there was no significant change between 1 year and 3 years (P = .492). Quadriceps strength on the nonoperated limb significantly decreased by 17% between 1 year and 3 years after TKA (P = .007). There was no significant interaction effect (F1.5,18.2 = 0.434, P = .653), main effect over time (F1.6,19.2 = 0.805, P = .436), or main effect between limbs (F1,12 = 2.462, P = .143) for the central activation ratio (TABLE 1).
Motion Analysis
There were no significant differences over time for gait speed (F2,23 = 0.010, P = .358), step width (F2,18 = 0.699, P = .510), and double support time (F2,22 = 0.524, P = .599) (TABLE 2). There was a significant time-by-limb interaction effect for stance phase (F2,22 = 5.971, P = .008). Stance phase on the operated limb was shorter compared to the nonoperated limb at the 3-month testing session only (P = .013).
TABLE 2.
Temporal and Spatial Results From Aim 1*
| 3 mo | 1 y | 3 y | |
|---|---|---|---|
| Gait speed, m/s | 1.35 ± 0.11 | 1.36 ± 0.16 | 1.35 ± 0.15 |
| Step width, m | 0.14 ± 0.02 | 0.13 ± 0.02 | 0.14 ± 0.03 |
| Double support time, s | 0.27 ± 0.04 | 0.27 ± 0.04 | 0.26 ± 0.05 |
| Stance (percent gait cycle) | |||
| Operated | 60.97 ± 3.57† | 62.99 ± 1.53 | 62.75 ± 1.84 |
| Nonoperated | 63.56 ± 1.82 | 62.82 ± 2.08 | 63.17 ± 1.76 |
Values are mean ± SD.
Significant difference compared to the nonoperated limb (P<.05).
There were no significant time-by-limb interactions and differences between limbs for knee flexion angles at initial contact (interaction: F2,22 = 1.285, P = .297; limb: F1,11 = 1.939, P = .191; time: F2,10 = 0.448, P = .651) and at peak knee flexion (interaction: F2,22 = 0.218, P = .806; limb: F1,11 = 0.239, P = .635; time: F2,10 = 0.006, P = .994) (TABLE 3). Similarly, there was no significant time-by-limb interaction for knee flexion excursion during loading response (F1.1,12.2 = 1.772, P = .209), main effect between limbs (F1,11 = 4.187, P = .065), and main effect over time (F2,10 = 0.386, P = .690).
TABLE 3.
Kinematic and Kinetic Results From Aim 1*
| 3 mo | 1 y | 3 y | |
|---|---|---|---|
| Initial contact | |||
| Hip flexion angle, deg | |||
| Operated | 25.67 ± 5.52 | 22.41 ± 10.15 | 23.96 ± 9.11 |
| Nonoperated | 24.77 ± 8.59 | 27.04 ± 8.39 | 24.72 ± 5.96 |
| Knee flexion angle, deg | |||
| Operated | 7.73 ± 4.14 | 6.38 ± 5.74 | 5.10 ± 6.40 |
| Nonoperated | 4.63 ± 5.55 | 4.58 ± 6.36 | 4.92 ± 5.38 |
| Ankle plantar flexion angle, deg | |||
| Operated | −0.10 ± 3.68 | 5.53 ± 16.45 | 0.16 ± 2.98 |
| Nonoperated | 1.64 ± 5.27 | 4.63 ± 16.27 | −0.39 ± 3.16 |
| Knee flexion excursion, deg | |||
| Operated | 10.5 ± 5.67 | 11.5 ± 5.4 | 13.7 ± 5.01 |
| Nonoperated | 14.8 ± 8.52 | 14.8 ± 4.6 | 13.7 ± 4.07 |
| At peak knee flexion | |||
| Hip flexion angle, deg | |||
| Operated | 15.88 ± 6.24 | 17.50 ± 10.25 | 15.60 ± 8.97 |
| Nonoperated | 16.55 ± 5.89 | 18.34 ± 7.99 | 14.42 ± 7.71 |
| Peak knee flexion angle, deg | |||
| Operated | 18.25 ± 7.78 | 17.88 ± 7.03 | 18.76 ± 9.51 |
| Nonoperated | 20.42 ± 8.94 | 19.39 ± 8.15 | 18.61 ± 5.46 |
| Ankle dorsiflexion angle, deg | |||
| Operated | −4.93 ± 3.47 | 1.02 ± 14.97 | −3.75 ± 3.55 |
| Nonoperated | −2.43 ± 2.22 | 0.71 ± 16.16 | −4.31 ± 3.23 |
| Hip extensor moment, Nm/BW × HT | |||
| Operated | 0.21 ± 0.21 | 0.15 ± 0.21 | 0.09 ± 0.17 |
| Nonoperated | 0.22 ± 0.21 | 0.22 ± 0.21 | 0.12 ± 0.18 |
| Knee extensor moment, Nm/BW × HT | |||
| Operated | 0.12 ± 0.18 | 0.15 ± 0.15 | 0.23 ± 0.18 |
| Nonoperated | 0.22 ± 0.18 | 0.20 ± 0.20 | 0.23 ± 0.17 |
| Ankle plantar flexor moment, Nm/BW × HT | |||
| Operated† | 0.06 ± 0.14 | 0.03 ± 0.08 | 0.08 ± 0.07 |
| Nonoperated | 0.11 ± 0.08 | 0.09 ± 0.12 | 0.15 ± 0.13 |
| Ground reaction forces | |||
| First peak vertical, N/BW | |||
| Operated | 1.05 ± 0.05‡ | 1.11 ± 0.11§‖ | 1.12 ± 0.10 |
| Nonoperated | 1.16 ± 0.12 | 1.16 ± 0.14 | 1.13 ± 0.10 |
Abbreviations: BW, body weight; HT, height.
Values are mean ± SD.
Significant difference between limbs across time (P<.001).
Significant difference from the nonoperated limb (P<.01).
Significant difference from the previous session (P<.05).
Significant difference from the nonoperated limb (P<.05).
There was no significant time-by-limb interaction (F2,24 = 0.545, P = .588), difference between limbs (F1,11 = 1.962, P = .189), or difference over time (F2,10 = 1.285, P = .319) for peak knee extensor moments at peak knee flexion. There was a significant time-by-limb interaction in the peak vertical ground reaction force (F2,22 = 4.432, P = .024), and follow-up paired t tests revealed that peak vertical ground reaction force of the operated limb was significantly less than that of the nonoperated limb 3 months and 1 year after TKA (P = .003 and P = .020, respectively), but not at 3 years after TKA (P = .723), with a significant increase of the operated limb between 3 months and 1 year after TKA (P = .046).
Comparisons Between the TKA and Control Groups Over Time (Aim 2)
Functional Performance Metrics
Thirteen patients from the first experimental aim and 1 patient who was tested at the 2-year follow-up instead of the 3-year follow-up were analyzed and compared to 14 matched healthy participants (TABLE 4). There was no significant group-by-time interaction (F1,25 = 1.290, P = .267) or main effect of time (F1,25 = 0.007, P = .933) for the SF-36 PCS. For the group main effect, the SF-36 PCS score in the TKA group was 4.8 points lower than the healthy control subjects over time, although this difference was not statistically significant (F1,25 = 4.023, P = .056). There was a significant time-by-group interaction for the KOS-ADL score (F1,26 = 9.435, P = .005), and follow-up testing revealed significant improvements in the TKA group between the 2 sessions (P = .045), whereas the score of the healthy subjects significantly decreased between sessions (P = .048). Follow-up testing between groups revealed that the KOS-ADL score was significantly lower in the TKA group at baseline (P<.01), yet there was no difference between groups at follow-up testing (P = .071). There was no significant time-by-group interaction (F1,26 = 2.577, P = .121), difference between groups (F1,26 = 0.579, P = .453), or difference over time (F1,26 = 0.027, P = .871) for the TUG. There was a significant time-by-group interaction for the SCT (F1,26 = 15.061, P = .001), because the healthy subjects demonstrated a significant increase in SCT time at the follow-up session (P = .001), whereas there were no significant changes for the TKA group (P = .063). The healthy controls demonstrated significantly shorter SCT times compared to the TKA group at baseline (P = .012) but not at follow-up (P = .788). There was no time-by-group interaction, difference between groups (F1,26 = 3.830, P = .061), or difference over time (F1,26 = 0.114, P = .738) for the 6MW.
TABLE 4.
Subject Information for Aim 2*
| TKA (n = 14) | Age-Matched Healthy (n = 14) | |||
|---|---|---|---|---|
| 3 mo | 2–3 y | Baseline | Follow-up | |
| Height, m | 1.7 ± 0.1 | … | 1.8 ± 0.1 | … |
| Weight, kg | 90.4 ± 11.6 | 88.6 ± 10.7 | 93.0 ± 17.2 | 91.7 ± 15.9 |
| BMI, kg/m2 | 30.8 ± 4.0 | 30.3 ± 3.9 | 30.6 ± 5.7 | 29.9 ± 4.9 |
| SF-36 PCS | 45.7 ± 7.8 | 46.9 ± 9.0 | 52.3 ± 5.7 | 49.9 ± 7.5 |
| SF-36 MCS | 58.2 ± 5.1 | 56.5 ± 4.3 | 58.1 ± 1.9 | 56.9 ± 4.1 |
| KOS-ADL | 0.79 ± 0.11† | 0.88 ± 0.01‡ | 0.99 ± 0.02 | 0.94 ± 0.09‡ |
| TUG, s | 7.5 ± 1.3 | 7.1 ± 1.1 | 6.8 ± 1.0 | 7.2 ± 1.1 |
| SCT, s | 11.5 ± 3.0† | 10.5 ± 2.3 | 9.1 ± 1.2 | 10.3 ± 1.3§ |
| 6MW, m | 577.7 ± 105.9 | 610.6 ± 110.7 | 652.5 ± 129.9 | 629.3 ± 104.8 |
| Knee e-AROM, deg‖ | 1.5 ± 2.4 | −1.9 ± 3.6 | −0.4 ± 2.1 | −2.2 ± 3.1 |
| Knee f-AROM, deg | 119.1 ± 8.7† | 126.8 ± 9.4‡ | 133.6 ± 8.2 | 131.9 ± 8.4 |
| MVIC, N/BMI | ||||
| Operated | 18.5 ± 7.1† | 20.0 ± 7.2§ | 28.8 ± 7.5 | 22.4 ± 8.4§ |
| Nonoperated¶ | 27.8 ± 9.3 | 21.8 ± 8.5 | 27.8 ± 5.8 | 23.2 ± 7.6 |
| CAR, % | ||||
| Operated | 93.2 ± 4.6 | 91.1 ± 9.6 | 91.5 ± 6.4 | 88.8 ± 8.9 |
| Nonoperated | 92.2 ± 6.1 | 89.4 ± 8.6 | 90.0 ± 6.2 | 88.1 ± 11.6 |
Abbreviations: 6MW, 6-minute walk test; BMI, body mass index; CAR, central activation ratio; e-AROM, extension active range of motion; f-AROM, flexion active range of motion; KOS-ADL, Knee Outcome Survey activities of daily living subscale; MCS, mental component summary; MVIC, maximum voluntary isometric contraction; PCS, physical component summary; SCT, stair-climbing test; SF-36, Medical Outcomes Study 36-Item Short-Form Health Survey; TKA, total knee arthroplasty; TUG, timed up-and-go test.
Values are mean ± SD.
Significant difference compared to the healthy control group (P<.05).
Significant difference compared to the previous session within a group (P<.05).
Significant difference compared to the previous session within a group (P<.01).
Significant change over time in both groups (P<.01). Negative direction of e-AROM indicates hyper-extension of the knee.
Significant change over time in both groups (P<.05).
Range of Motion and Strength
There was no significant interaction effect (F1,26 = 1.287, P = .267) or main effect of group (F1,26 = 1.929, P = .177), but there was a significant increase in knee extension range of motion over time (F2,26 = 12.961, P = .001) for both groups. There was a significant time-by-group interaction for knee flexion (F1,26 = 6.473, P = .017). Follow-up testing revealed significantly less knee flexion in the TKA group compared to the healthy control group at baseline (P<.0001) but not at follow-up (P = .140). There was a significant increase in knee flexion in the TKA group between the 2 sessions (P = .020), but no change for the control group (P = .467).
There was a significant time-by-group interaction for quadriceps strength of the operated limb (F1,26 = 15.750, P = .001), and follow-up paired t tests revealed that strength of the operated limb in the TKA group significantly increased between the 2 sessions (P = .002), whereas the quadriceps of the comparison limb in the healthy group became significantly weaker between the 2 sessions (P = .001). The strength of the operated limb in the TKA group was significantly less than that of the healthy control group at baseline (P = .001) but not at follow-up (P = .435). There was no group-by-time interaction in the strength of the nonoperated limb (F1,26 = 0.298, P = .590), but there was a significant main effect of time (F1,26 = 17.021, P<.001), with a significant decrease for both the TKA group (22%, P = .002) and control group (17%, P = .040) between testing periods. There was no significant group main effect for the strength of the nonoperated limb between groups (F1,26 = 0.077, P = .783). There were no time-by-group interactions, main effect over time, or main effect between groups for the central activation ratio of both the operated limb (interaction: F1,25 = 0.116, P = .736; over time: F1,25 = 1.368, P = .253; group: F1,25 = 2.126, P = .157) and nonoperated limb (interaction: F1,26 = 0.065, P = .801; over time: F2,26 = 1.510, P = .230; group: F1,26 = 0.462, P = .503).
Motion Analysis
There were no time-by-group interactions (F1,26 = 0.202, P = .657), differences between baseline and follow-up (F1,26 = 0.047, P = .829), or differences between groups for gait speed (F1,26 = 3.548, P = .071). There were no significant time-by-group interactions (F1,24 = 0.930, P = .344) or changes over time (F1,24 = 0.314, P = .580) for step width, but the TKA group had a significantly wider step compared to the healthy control group (F1,24 = 6.320, P = .019). There were no time-by-group interactions (F1,25 = 1.571, P = .222), differences between baseline and follow-up (F1,25 = 0.029, P = .867), or differences between groups for double support time (F1,25 = 0.052, P = .822). There were no significant time-by-group interactions (F1,25 = 0.630, P = .435) or differences between groups (F1,25 = 1.591, P = .219) for the stance phase of the operated limb, but there was a significantly longer stance time in the second session compared to the first session in both groups (F1,25 = 5.150, P = .032) (TABLE 5). There were no time-by-group interactions (F1,25 = 0.755, P = .393), differences between baseline and follow-up (F1,25 = 0.017, P = .899), or differences between groups for stance phase of the nonoperated limb (F1,25 = 0.300, P = .589).
TABLE 5.
Temporal and Spatial Parameter Results for Aim 2*
| TKA (n = 14) | Age-Matched Healthy (n = 14) | |||
|---|---|---|---|---|
| 3 mo | 2–3 y | Baseline | Follow-up | |
| Gait speed, m/s | 1.35 ± 0.10 | 1.35 ± 0.15 | 1.45 ± 0.15 | 1.43 ± 0.17 |
| Step width, m† | 0.14 ± 0.02 | 0.14 ± 0.03 | 0.12 ± 0.02 | 0.12 ± 0.02 |
| Double support time, s | 0.27 ± 0.04 | 0.26 ± 0.05 | 0.26 ± 0.05 | 0.27 ± 0.05 |
| Stance (percent gait cycle) | ||||
| Operated‡ | 60.82 ± 3.85 | 62.67 ± 1.78 | 62.20 ± 1.72 | 63.09 ± 1.73 |
| Nonoperated | 61.70 ± 7.00 | 62.84 ± 2.04 | 62.27 ± 2.08 | 60.73 ± 7.73 |
Values are mean ± SD.
Significant difference between groups over time (P<.05).
Significant change over time in both groups (P<.05).
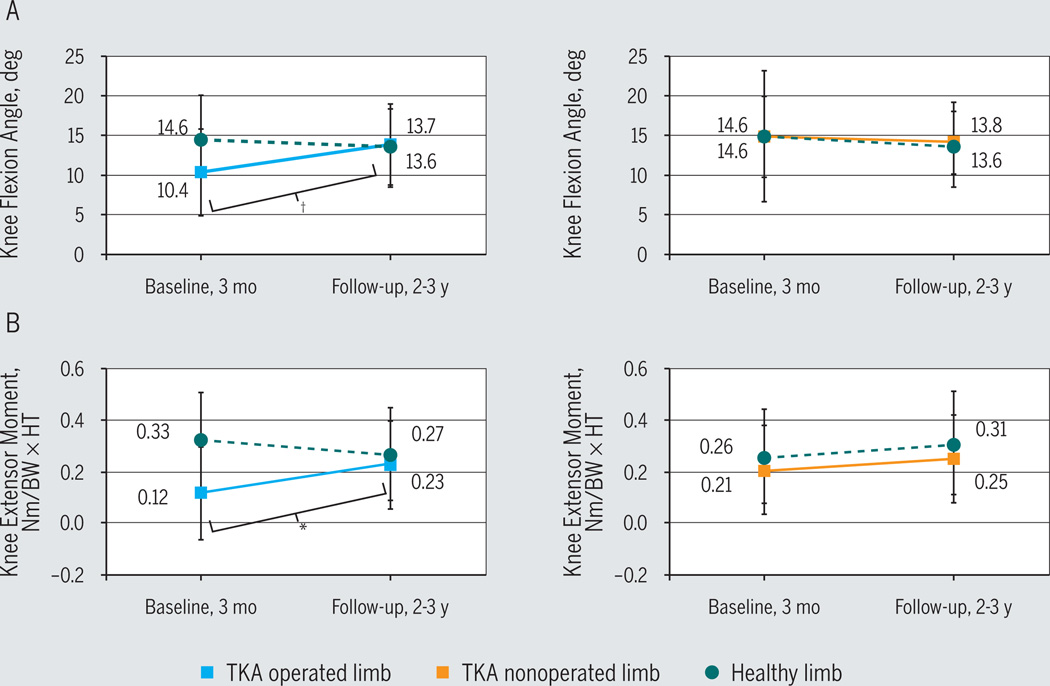
There were no time-by-group interactions (F1,25 = 1.238, P = .277), differences over time (F1,25 = 2.964, P = .097), or differences between groups (F1,25 = 0.031, P = .862) in knee flexion angle of the operated limb at initial contact. In the nonoperated limb, there were also no time-by-group interactions (F1,25 = 0.582, P = .453), differences over time (F1,25 = 0.574, P = .456), or differences between groups (F1,25 = 0.069, P = .795) in knee flexion angle at initial contact. There were no time-by-group interactions (F1,25 = 0.444, P = .511), differences over time (F1,25 = 0.708, P = .408), or differences between groups (F1,25 = 0.630, P = .435) in peak knee flexion angle of the operated limb. There were no time-by-group interactions (F1,25 = 0.376, P = .545), differences over time (F1,25 = 1.450, P = .240), or differences between groups (F1,25 = 0.057, P = .814) in peak knee flexion angle of the nonoperated limb. There was a significant time-by-group interaction in knee flexion excursion in the operated limb (F1,25 = 9.346, P = .005) but not in the nonoperated limb (F1,25 = 0.006, P = .940) (TABLE 6). The TKA group significantly increased knee flexion excursion of the operated limb between sessions (P = .001), whereas there was no change in knee flexion excursion of the healthy subjects (P = .350) (FIGURE). Knee flexion excursion in the TKA group was 4.4° less than the healthy control group at baseline (P = .047), but there was no difference at follow-up (P = .920). There was no difference over time (F1,25 = 0.391, P = .537) or between groups (F1,25 = 0.008, P = .929) for knee flexion excursion of the nonoperated limb.
TABLE 6.
Kinematic and Kinetic Results for Aim 2*
| TKA (n = 14) | Age-Matched Healthy (n = 14) | |||
|---|---|---|---|---|
| 3 mo | 2–3 y | Baseline | Follow-up | |
| Initial contact | ||||
| Hip flexion angle, deg | ||||
| Operated | 26.10 ± 5.51 | 24.16 ± 8.79 | 24.53 ± 6.02 | 23.26 ± 9.01 |
| Nonoperated | 25.25 ± 8.40 | 25.22 ± 6.25 | 23.27 ± 5.14 | 20.24 ± 9.67 |
| Knee flexion angle, deg | ||||
| Operated | 8.33 ± 4.51 | 5.11 ± 6.11 | 6.63 ± 4.92 | 5.87 ± 6.24 |
| Nonoperated | 4.86 ± 5.38 | 4.95 ± 4.96 | 5.18 ± 3.71 | 3.72 ± 4.99 |
| Ankle plantar flexion angle, deg | ||||
| Operated | −0.49 ± 3.79 | 0.20 ± 3.90 | 0.43 ± 3.73 | −1.41 ± 2.97† |
| Nonoperated | 1.14 ± 5.35 | −0.43 ± 3.66 | 0.49 ± 4.35 | −1.38 ± 4.08† |
| Knee flexion excursion, deg | ||||
| Operated | 10.35 ± 5.46‡ | 13.68 ± 4.80† | 14.77 ± 5.48 | 13.67 ± 4.81 |
| Nonoperated | 14.64 ± 8.17 | 13.81 ± 3.92 | 14.60 ± 5.07 | 13.55 ± 5.28 |
| At peak knee flexion | ||||
| Hip flexion angle, deg | ||||
| Operated | 16.42 ± 6.29 | 15.83 ± 8.86 | 14.83 ± 6.24 | 10.60 ± 10.42 |
| Nonoperated | 17.23 ± 6.16 | 15.04 ± 7.50 | 14.30 ± 7.22 | 11.09 ± 10.25 |
| Peak knee flexion angle, deg | ||||
| Operated | 18.68 ± 7.62 | 18.53 ± 8.81 | 21.40 ± 6.01 | 19.48 ± 7.81 |
| Nonoperated | 19.50 ± 8.57 | 18.92 ± 5.11 | 19.78 ± 6.70 | 17.26 ± 7.70 |
| Ankle dorsiflexion angle, deg | ||||
| Operated | 5.30 ± 3.59 | 4.25 ± 3.56 | 0.96 ± 3.96 | 4.50 ± 2.73 |
| Nonoperated | 3.23 ± 3.60 | 4.39 ± 3.42 | 0.68 ± 4.65 | 5.62 ± 2.17 |
| Hip extensor moment, Nm/BW × HT | ||||
| Operated§ | 0.22 ± 0.21 | 0.11 ± 0.17 | 0.17 ± 0.13 | 0.08 ± 0.16 |
| Nonoperated§ | 0.25 ± 0.23 | 0.12 ± 0.17 | 0.15 ± 0.10 | 0.04 ± 0.13 |
| Knee extensor moment, Nm/BW × HT | ||||
| Operated | 0.12 ± 0.18‖ | 0.23 ± 0.17¶ | 0.33 ± 0.18 | 0.27 ± 0.18 |
| Nonoperated | 0.21 ± 0.17 | 0.25 ± 0.17 | 0.26 ± 0.18 | 0.31 ± 0.20 |
| Ankle plantar flexor moment, Nm/BW × HT | ||||
| Operated | −0.06 ± 0.13 | 0.07 ± 0.07 | 0.05 ± 0.06 | 0.07 ± 0.10 |
| Nonoperated | 0.10 ± 0.08 | 0.13 ± 0.13 | 0.03 ± 0.07 | 0.03 ± 0.06 |
| Ground reaction forces | ||||
| First peak vertical, N/BW | ||||
| Operated | 1.05 ± 0.05‖ | 1.13 ± 0.10† | 1.15 ± 0.10 | 1.16 ± 0.11 |
| Nonoperated | 1.15 ± 0.09 | 1.13 ± 0.09 | 1.13 ± 0.09 | 1.11 ± 0.07 |
Abbreviations: BW, body weight; HT, height; TKA, total knee arthroplasty.
Values are mean ± SD.
Significant improvement at the second session compared to the first session in the group (P<.01).
Significant difference compared to the healthy control group (P<.05).
Significant time effect in both groups between sessions (P<.05).
Significant difference compared to the healthy control group (P<.01).
Significant improvement at the second session compared to the first session in the group (P<.05).
FIGURE.
Knee kinematics and kinetics during loading response. (A) Knee flexion excursion during loading response. (B) Knee extensor moment at peak knee flexion. The operated limb improved over time in patients after total knee arthroplasty. *P<.05; †P<.01.
There was a significant time-by-group interaction in knee extensor moment of the operated limb (F1,24 = 5.474, P = .028). Knee extensor moment of the operated limb in the TKA group significantly increased by 92% between sessions (P = .045) (FIGURE), but there was no significant change in the control group over time (P = .057). Knee extensor moment in the TKA group was 63% less than the healthy control group at baseline (P = .007), but there were no significant differences at follow-up (P = .652). There were no time-by-group interactions (F1,23 = 0.001, P = .974), differences over time (F1,23 = 0.463, P = .503), or differences between groups (F1,23 = 1.387, P = .251) for knee extensor moment of the nonoperated limb.
There was a significant time-by-group interaction in the first peak of vertical ground reaction forces of the operated limb (F1,26 = 5.180, P = .031). The TKA group significantly increased the peak of vertical ground reaction forces of the operated limb by a mean of 7.6% between sessions (P = .007), whereas there was no significant change in the healthy subjects (P = .951). The vertical ground reaction forces in the operated limb of the TKA group were significantly less than those of the healthy subjects at baseline (P = .001) but not at the follow-up session (P = .508). There were no time-by-group interactions (F1,26 = 0.000, P = .997), changes over time (F1,26 = 2.031, P = .166), or differences between groups (F1,26 = 0.589, P = .450) in the peak vertical ground reaction forces of the nonoperated limb.
DISCUSSION
The results from this study reflect the typical pattern of recovery in the first year after TKA.19 Between 3 months and 1 year after TKA, subjects in the TKA group demonstrated significant improvements in the SF-36 PCS, KOS-ADL, TUG, and SCT. Over the same time interval, the TKA group also demonstrated significant improvements in knee range of motion, strength, and vertical ground reaction force in the operated limb. When compared to control subjects, the operated limb of subjects in the TKA group also demonstrated improvements over time for knee joint kinematics and kinetics, as shown through a significant increase in knee extensor moment, knee flexion excursion, and vertical ground reaction force. At the follow-up session, these biomechanical variables in the TKA group were no different from the values of the control subjects. Despite improvements in the TKA group and a lack of differences between groups at follow-up for the majority of the outcome variables, both groups developed notable deficits between baseline and the 2-to-3-year follow-up. Although these may be attributed to impairments associated with aging, the persistence of deficits might have had more negative consequences in the TKA group, which started off with lower scores at baseline.
Although subjects in the TKA group demonstrated an increase in self-reported physical function, as evidenced by the significantly higher SF-36 scores at 1 year compared to baseline, this group subsequently demonstrated a significant decrease in SF-36 scores at the 3-year follow-up. This decrease in perception of functional ability occurred concomitantly with the statistically and clinically meaningful loss of strength in the nonoperated limb over the same period. There was no significant decrease in strength in the operated limb at 3 years (mean change, 0.4 N/BMI), whereas the loss of strength in the nonoperated limb over the same period was more than 10-fold greater (4.4 N/BMI). Previous reports have identified a strength change of 3.9 N/BMI as clinically meaningful.7 The nonoperated limb has been shown to be more painful and weaker 3 years after TKA, and the status of this limb is the best predictor of function at the same time point.7 The fact that subjects in the TKA group demonstrated a substantial loss of strength in the nonoperated limb may lend evidence to support the hypothesis that the nonoperated limb drives reduced functional ability in long-term follow-up after TKA. The bilateral loss of strength in the control group (mean, 19%) may also explain the decrease in functional ability, as shown by the significant increase in SCT time and significant reduction in KOS-ADL scores in this group between testing sessions. Future work should evaluate the relationship between change in strength and change in function, in both the TKA and healthy older adult population, to determine if the same impairments may underlie reductions in functional performance for both groups.
Three months after TKA, there were significant differences between limbs for quadriceps strength in the TKA group, and these differences persisted 1 year after TKA, with the operated limb being weaker than the nonoperated limb. However, 3 years after TKA, there were no significant or clinically meaningful differences between limbs with respect to quadriceps strength. The lack of differences between limbs 3 years after TKA was mainly attributed to the gradual loss of quadriceps strength in the nonoperated limb, not to a gradual increase in the strength of the operated limb. There was a 23% decrease in the strength of the nonoperated limb and only a 7% increase in the strength of the operated limb between 3 months and 3 years. Unfortunately, we did not measure other parameters that might have been related to the functional recovery or change in quadriceps strength over time, such as preoperative quadriceps strength values or postoperative physical activity levels. Future research should analyze the relationship between persistent gait asymmetries, abnormal loading related to quadriceps weakness, and disease progression, because it is possible that gait abnormalities that overload the nonoperated limb may contribute to osteoarthritis progression and weakness in this limb.
As the quadriceps strength equalized between limbs, there were concomitant improvements in symmetry for knee flexion excursion, knee flexor moment, and peak vertical ground reaction force in the TKA group, which supports our first hypothesis. In fact, in the TKA group, the values between limbs for these variables were nearly identical at the 3-year follow-up. It is also important to note that the differences between groups for these biomechanical outcomes in the operated limb were resolved at the follow-up period and that there were no between-group differences in these outcomes for the nonoperated limb. Therefore, it does not appear that the improvement in biomechanical symmetry in our sample is entirely reliant on strength loss in the nonoperated limb. Because significant improvements were seen for these biomechanical metrics in the operated limb of the TKA group and because our control group also demonstrated a significant weakening of both limbs, we cannot definitively conclude that the improvements in interlimb symmetry in our TKA group were solely a result of impairments that developed in the nonoperated limb. Therefore, our second hypothesis was not completely supported.
There was no difference between groups at follow-up for the majority of the biomechanical, clinical, and functional outcomes. This contrasts previous reports that have found persistent differences in stair-climbing time and gait speed at a 1-year follow-up evaluation after TKA.28 However, the differences between studies may be attributed to the shorter time of follow-up in the previous report, differences in study design, or differences in rehabilitation of the TKA sample. Walsh et al28 evaluated subjects 1 year after TKA and control subjects using a cross-sectional design (with no longitudinal assessment of the control group). Between the baseline and the follow-up assessments, we found a significant and clinically meaningful decline in strength and an increase in stair-climbing time in the control group. The development of these impairments in the control group partially explains why the TKA and control groups in our study had similar functional outcomes at the 3-year follow-up. All of the subjects following TKA in our study also underwent a structured and progressive rehabilitation protocol that specifically targeted muscle weakness and functional impairments, whereas specifics of postoperative care were not given in the previous study.23
Although this study is the first to report longitudinal clinical, biomechanical, and functional outcomes in subjects who underwent TKA compared to a control group evaluated over a similar period, there are several limitations that should be noted when interpreting the results. We powered this study on values for subjects after TKA, which provided a relatively small sample size. The change in values over time for the control group was an interesting finding but reduced our ability to identify interaction effects for most of our clinical metrics. The TKA group also consisted solely of individuals who were primarily nonsymptomatic in the nonoperated limb at the time of surgery. This might not have been reflective of the majority of patients who require TKA and might have underrepresented the potential negative changes that occur in the nonoperated limb. Although we did see a progressive decline in the strength of the operated limb, we found SF-36 scores decreasing only at the longer-term follow-up. It is possible that subjects with bilateral disease at baseline might demonstrate greater long-term deficits and more apparent impairments in the nonoperated limb over time. The strengths of this report lie in the longitudinal analysis of both groups and the use of a variety of self-reported and performance-based outcome measures. These outcome measures assess 2 different and distinct aspects of recovery, neither of which can be used individually to fully assess a patient’s functional recovery after TKA.10,18,30
CONCLUSION
As interlimb differences in quadriceps strength disappear after TKA, there are concomitant symmetrical improvements in temporospatial and kinetic gait parameters. The lack of differences in quadriceps strength between limbs 3 years after TKA is mostly attributable to a decline in the strength of the nonoperated limb, not to improvement in the strength of the operated limb, which supports our first hypothesis. Although there was a definitive loss of strength in the nonoperated limb of the TKA group and a significant reduction in the SF-36 over the same period, the control group also demonstrated significant reductions in strength and perception of function, and required increased time to complete functional activities. Additionally, biomechanical improvements were seen in the operated limb after TKA, and there were no differences between the TKA and control groups for most of the clinical, biomechanical, and functional outcome variables. It cannot be conclusively stated that these similarities are driven solely by the progressive weakness of the nonoperated limb in the TKA group alone, although it does appear that progressive weakness associated with aging may underlie functional changes in individuals with and without knee pathology.
KEY POINTS.
FINDINGS
Patients after TKA demonstrate an improvement in biomechanical symmetry at long-term follow-up; however, these individuals also demonstrate a progressive loss of strength in the nonoperated limb over time.
IMPLICATIONS
The decreased function during daily activity in individuals after TKA is contributed by the quadriceps weakness of the nonoperated limb.
CAUTION
This study exposes a plausible relationship between quadriceps strength and functional performance in individuals after TKA. These findings should be corroborated in a larger sample.
Acknowledgments
This work was supported by the National Institutes of Health (R01HD041055-1 and T32HD07490) and was performed at the University of Delaware. The Human Subjects Review Board of the University of Delaware approved the study.
Footnotes
The authors have no other conflict of interest or financial involvement to report.
REFERENCES
- 1.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res. 2011;29:647–652. doi: 10.1002/jor.21323. http://dx.doi.org/10.1002/jor.21323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boonstra MC, De Waal Malefijt MC, Verdonschot N. How to quantify knee function after total knee arthroplasty? Knee. 2008;15:390–395. doi: 10.1016/j.knee.2008.05.006. http://dx.doi.org/10.1016/j.knee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Botolfsen P, Helbostad JL, Moe-Nilssen R, Wall JC. Reliability and concurrent validity of the Expanded Timed Up-and-Go test in older people with impaired mobility. Physiother Res Int. 2008;13:94–106. doi: 10.1002/pri.394. http://dx.doi.org/10.1002/pri.394. [DOI] [PubMed] [Google Scholar]
- 4.Crosbie J, Naylor JM, Harmer AR. Six minute walk distance or stair negotiation? Choice of activity assessment following total knee replacement. Physiother Res Int. 2010;15:35–41. doi: 10.1002/pri.453. http://dx.doi.org/10.1002/pri.453. [DOI] [PubMed] [Google Scholar]
- 5.Enright PL. The six-minute walk test. Respir Care. 2003;48:783–785. [PubMed] [Google Scholar]
- 6.Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med. 1998;158:1384–1387. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- 7.Farquhar S, Snyder-Mackler L. The Chitranjan Ranawat Award: the nonoperated knee predicts function 3 years after unilateral total knee arthroplasty. Clin Orthop Relat Res. 2010;468:37–44. doi: 10.1007/s11999-009-0892-9. http://dx.doi.org/10.1007/s11999-009-0892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farquhar SJ, Reisman DS, Snyder-Mackler L. Persistence of altered movement patterns during a sit-to-stand task 1 year following unilateral total knee arthroplasty. Phys Ther. 2008;88:567–579. doi: 10.2522/ptj.20070045. http://dx.doi.org/10.2522/ptj.20070045. [DOI] [PubMed] [Google Scholar]
- 9.Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA. Patient outcomes after knee replacement. Clin Orthop Relat Res. 1998:93–110. doi: 10.1097/00003086-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Hidding A, van Santen M, De Klerk E, et al. Comparison between self-report measures and clinical observations of functional disability in ankylosing spondylitis, rheumatoid arthritis and fibromyalgia. J Rheumatol. 1994;21:818–823. [PubMed] [Google Scholar]
- 11.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Keller SD, Majkut TC, Kosinski M, Ware JE., Jr Monitoring health outcomes among patients with arthritis using the SF-36 Health Survey: overview. Med Care. 1999;37:MS1–MS9. doi: 10.1097/00005650-199905001-00001. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy DM, Hanna SE, Stratford PW, Wessel J, Gollish JD. Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty. 2006;21:559–566. doi: 10.1016/j.arth.2005.07.010. http://dx.doi.org/10.1016/j.arth.2005.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kennedy DM, Stratford PW, Riddle DL, Hanna SE, Gollish JD. Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther. 2008;88:22–32. doi: 10.2522/ptj.20070051. http://dx.doi.org/10.2522/ptj.20070051. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. http://dx.doi.org/10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.König A, Walther M, Kirschner S, Gohlke F. Balance sheets of knee and functional scores 5 years after total knee arthroplasty for osteoarthritis: a source for patient information. J Arthroplasty. 2000;15:289–294. doi: 10.1016/s0883-5403(00)90532-1. [DOI] [PubMed] [Google Scholar]
- 17.McClelland JA, Webster KE, Feller JA. Gait analysis of patients following total knee replacement: a systematic review. Knee. 2007;14:253–263. doi: 10.1016/j.knee.2007.04.003. http://dx.doi.org/10.1016/j.knee.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Mizner RL, Petterson SC, Clements KE, Zeni JA, Jr, Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2011;26:728–737. doi: 10.1016/j.arth.2010.06.004. http://dx.doi.org/10.1016/j.arth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther. 2005;35:424–436. doi: 10.2519/jospt.2005.35.7.424. http://dx.doi.org/10.2519/jospt.2005.2036. [DOI] [PubMed] [Google Scholar]
- 20.Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23:1083–1090. doi: 10.1016/j.orthres.2005.01.021. http://dx.doi.org/10.1016/j.orthres.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 21.Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch Phys Med Rehabil. 2004;85:546–556. doi: 10.1016/j.apmr.2003.08.080. [DOI] [PubMed] [Google Scholar]
- 22.Ouellet D, Moffet H. Locomotor deficits before and two months after knee arthroplasty. Arthritis Rheum. 2002;47:484–493. doi: 10.1002/art.10652. http://dx.doi.org/10.1002/art.10652. [DOI] [PubMed] [Google Scholar]
- 23.Petterson SC, Mizner RL, Stevens JE, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183. doi: 10.1002/art.24167. http://dx.doi.org/10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 24.Ranawat CS, Ranawat AS, Mehta A. Total knee arthroplasty rehabilitation protocol: what makes the difference? J Arthroplasty. 2003;18:27–30. doi: 10.1054/arth.2003.50080. http://dx.doi.org/10.1054/arth.2003.50080. [DOI] [PubMed] [Google Scholar]
- 25.Smith AJ, Lloyd DG, Wood DJ. Pre-surgery knee joint loading patterns during walking predict the presence and severity of anterior knee pain after total knee arthroplasty. J Orthop Res. 2004;22:260–266. doi: 10.1016/S0736-0266(03)00184-0. http://dx.doi.org/10.1016/S0736-0266(03)00184-0. [DOI] [PubMed] [Google Scholar]
- 26.Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res. 2003;21:775–779. doi: 10.1016/S0736-0266(03)00052-4. http://dx.doi.org/10.1016/S0736-0266(03)00052-4. [DOI] [PubMed] [Google Scholar]
- 27.Vagaggini B, Taccola M, Severino S, et al. Shuttle walking test and 6-minute walking test induce a similar cardiorespiratory performance in patients recovering from an acute exacerbation of chronic obstructive pulmonary disease. Respiration. 2003;70:579–584. doi: 10.1159/000075202. [DOI] [PubMed] [Google Scholar]
- 28.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78:248–258. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 30.Wittink H, Rogers W, Sukiennik A, Carr DB. Physical functioning: self-report and performance measures are related but distinct. Spine (Phila Pa 1976) 2003;28:2407–2413. doi: 10.1097/01.BRS.0000085304.01483.17. http://dx.doi.org/10.1097/01.BRS.0000085304.01483.17. [DOI] [PubMed] [Google Scholar]
- 31.Yeung TS, Wessel J, Stratford PW, MacDermid JC. The timed up and go test for use on an inpatient orthopaedic rehabilitation ward. J Orthop Sports Phys Ther. 2008;38:410–417. doi: 10.2519/jospt.2008.2657. http://dx.doi.org/10.2519/jospt.2008.2657. [DOI] [PubMed] [Google Scholar]
- 32.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon) 2008;23:320–328. doi: 10.1016/j.clinbiomech.2007.10.008. http://dx.doi.org/10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zeni JA, Jr, Snyder-Mackler L. Early postoperative measures predict 1- and 2-year outcomes after unilateral total knee arthroplasty: importance of contralateral limb strength. Phys Ther. 2010;90:43–54. doi: 10.2522/ptj.20090089. http://dx.doi.org/10.2522/ptj.20090089. [DOI] [PMC free article] [PubMed] [Google Scholar]