Abstract
Objectives
To assess patient preferences regarding side effects associated with cervical cancer treatment.
Methods/Materials
The visual analog scale (VAS) and modified standard gamble (SG) were used to elicit preferences of women with no evidence of disease following primary treatment for cervical cancer. Higher scores on VAS and SG indicated more favorable ratings for a given health state (HS). HS included: vaginal shortening (VAG), diarrhea, dietary changes (DIET), menopause, moderate nausea/vomiting (NV), rectal bleeding, sexual dysfunction, and urinary self-catheterization (USC). Descriptive statistics, Kruskal-Wallis, Mann Whitney U, Wilcoxon signed-ranks tests and correlation coefficients were used for statistical analysis.
Results
78 patients participated in the study. Median age was 44.1 years (range 24.9–67.8). Median time since treatment completion was 31.2 months (range 1.0–113.3). The health states rated as most favorable by VAS were also rated as most favorable by SG. Increasing age was associated with higher VAS scores for menopause and VAG (p=0.04 and 0.036). African-Americans had higher VAS scores for DIET (p=0.05), sexual dysfunction (p=0.028), and diarrhea (p=0.05) when compared to Hispanic and non-Hispanic white patients. Women receiving radiation had more favorable VAS scores for menopause compared to women undergoing radical hysterectomy (p=0.05). Women receiving chemotherapy rated USC less favorably by VAS score compared to those not receiving chemotherapy (p=0.045).
Conclusions
Multiple demographic and clinical factors influence the severity of treatment-related adverse effects perceived by women surviving cervical cancer. A better understanding of factors influencing patient preferences regarding treatment side effects will allow providers to formulate care better tailored to the individual desires of each patient.
Keywords: Preferences, Quality of life, Cervical Cancer
INTRODUCTION
Despite effective screening strategies and preventative vaccines, cervical cancer continues to afflict women in the United States. An estimated 12,360 new cases of cervical cancer will be diagnosed in the United States during 2014 with 4,020 associated deaths (1). Cervical cancer is initially treated surgically or with chemoradiation depending on stage of the cancer at diagnosis. Detrimental side effects may range from urinary dysfunction to sexual dysfunction (2, 3). Although many patients will be cured, the acute and late effects of treatment may have substantial negative impact on quality of life (QOL) (4–6). It is essential that healthcare providers have an understanding of patient preferences regarding treatment side effects in order to provide care tailored to the individual’s desires.
Patient preferences reveal how patients perceive health states, such as specific treatments or associated side effects. Researchers utilize preference assessment measures to evaluate the strength of the patient’s preference for health states (7). Scores range from 0 to 1, where 0 represents “least preferred” and 1 represents “most preferred.” Results of preference assessment studies increase providers’ understanding of how patients interpret the risks and benefits of a given treatment. Additionally, preference data are used in cost-effectiveness studies to evaluate the cost per quality-adjusted life-year.
Preference studies related to cervical abnormalities largely focus on the management and surveillance of cervical dysplasia (8, 9). Limited research has examined preferences among patients with invasive cervical cancer (10, 11). These studies demonstrate that patients prefer minimally invasive surgery for the management of early stage, high-risk cervical cancer and consider health states such as small bowel obstruction and ureteral obstruction as less tolerable than health states such as lymphedema or radiation cystitis (10, 11). Interestingly, patients and health-care providers have differing views on the impact of treatment side effects on patients’ QOL (11). Patients rate certain side effects as severely impacting their QOL whereas providers rate the same side effects as minimally impacting the patient’s QOL, suggesting that the perceptions of patients and their providers regarding treatment complications differ significantly.
Knowledge of patient preferences allows providers to “tailor” or “personalize” treatment planning to focus on each patient’s individual desires and goals for treatment. Additionally, patient preferences data may be used to determine quality-adjusted clinical outcomes that may be used to compare the effectiveness of different treatment strategies. As our current health-care system evolves, such evaluations are becoming increasingly important. Accordingly, the primary objective of our study was to assess patient preferences for side effects of cervical cancer treatment. A secondary objective was to explore whether demographic and clinical factors influenced preference scores.
MATERIALS AND METHODS
This study was approved by the IRB of The University of Texas MD Anderson Cancer Center. Eligible women were seen at our institution, were at least 18 years of age, had completed primary therapy for cervical cancer, were currently with no evidence of disease, and spoke either English or Spanish. Patients were identified from weekly clinic rosters and invited to participate. A trained research coordinator conducted individual 30-minute study interviews consisting of preference assessments and a QOL survey. A certified translator translated for patients who spoke only Spanish. Written informed consent was obtained from all enrolled patients.
Preference assessments
Eight health states were included in this study: diarrhea, dietary changes, menopause, nausea and vomiting, rectal bleeding, sexual dysfunction, urinary self-catheterization, and vaginal length shortening. Health states were selected based on input from physicians who frequently care for cervical cancer patients. The health state descriptions were written based upon input from cervical cancer patients and physicians. These descriptions were reviewed by other patients and women without a cancer diagnosis to ascertain face validity before being used in this study.
Visual Analog Scale (VAS)
Patients were asked to read the eight health states and rank them in order from most- to least-preferred using a visual analog scale (VAS). The VAS used in this study was a “feeling thermometer,” Figure 1, in which patients rated each health state on a scale from 0 to 100 (0=worst; 100=best). VAS was chosen as one of the preference assessment measures for this study because it presents the least amount of patient burden (in terms of time and intellectual output) and is the easiest and most intuitive preference assessment measure to understand (7).
Figure 1. Visual analog scale (VAS) Thermometer.
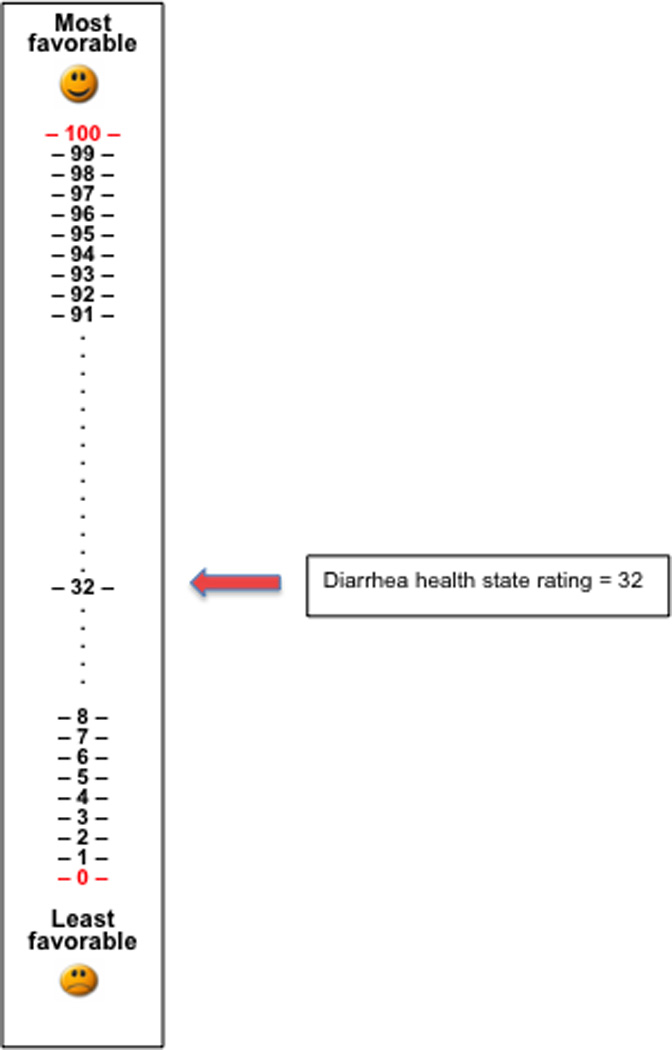
This VAS scale was used in the current study. Patients were asked to rate a health state, “diarrhea” on the scale. A higher score indicated a more favorable rating for the given health state.
Standard Gamble (SG)
Patients were also asked to evaluate eight health states using the standard gamble (SG), a choice-based method of evaluating preferences under conditions of uncertainty. The traditional framework asks subjects to choose between life in a compromised health state, or participating in a gamble of X% chance of perfect health and (1–X)% chance of immediate and painless death (12). Probabilities are systematically varied until the respondent is indifferent to the choice or prefers the health state being evaluated. The probability X at this point is the SG preference score for the health state being evaluated.
The SG was chosen as one of the preference assessment measures for this study because it is considered the gold standard for asking patients to assess preferences since it measures their willingness to accept risk (7, 13). Because the SG involves an element of uncertainty surrounding potential outcomes it closely mirrors what patients must take into account when deciding whether to undergo a given cancer treatment.
Previous experience with our patient population suggested that, because of the temporary nature of many side effects, women with cervical cancer would not be willing to consider death as a possible SG outcome. Similar to other investigators, we therefore used a modified SG by incorporating a non-death health state as the worst outcome (anchor) (14). We chose “severe nausea and vomiting resulting in bedrest” because our prior research showed that preference scores for severe nausea and vomiting approximate scores for death (15).
Accordingly, a modified SG score was obtained in the following manner: for each health state, patients were given a choice between two hypothetical treatments, Treatment 1 and Treatment 2. Treatment 1 would result in immediate clinical remission with no side effects in X% of patients, but the remaining (1–X)% of patients would experience the worst health state (severe nausea and vomiting resulting in bed rest) followed by clinical remission. Treatment 2 would result in the patient experiencing the health state in question (e.g., diarrhea) followed by clinical remission. The probability X began at 100% and decreased in 10% increments until the patient chose Treatment 2. This X value was the SG score for the patient. The SG framework is shown in Figure 2.
Figure 2. Standard gamble (SG) algorithm comparing treatment 1 to treatment 2.
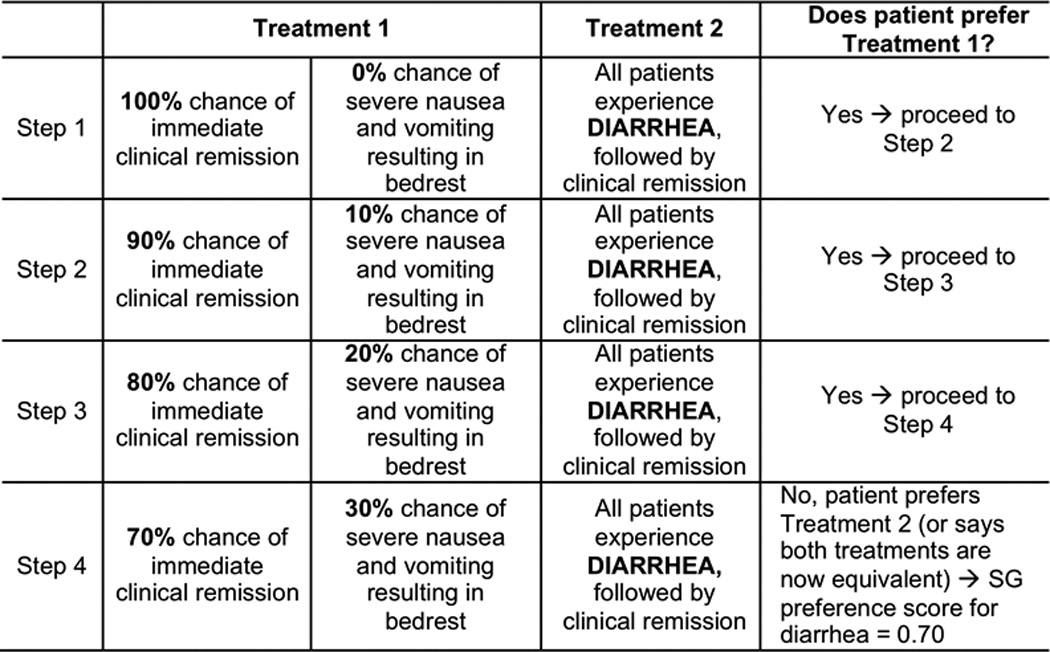
This algorithm was used to assess the patient’s SG score. The research nurse started at step 1 by asking the patient if she would prefer treatment 1, which would result in 100% clinical remission and a 0% chance of nausea/vomiting, or treatment 2 which would result in all patients experiencing diarrhea (the health state being tested) followed by complete clinical remission. The research nurse would continue going through each outlined step until the patient stated that treatment 2 was better than treatment 1 or that the patient considered both treatment options to be equal.
Statistical considerations
Characteristics of the study population were summarized using descriptive statistics, including median and range for continuous variables and percentage for categorical variables. Kruskal-Wallis and Mann Whitney U tests were used to evaluate the differences between groups for preference scores and quality of life scores. The Wilcoxon signed-ranks test was used to compare VAS and SG scores in a pairwise fashion.
RESULTS
Patients’ characteristics
Seventy-eight women were enrolled in the study. Demographic and clinical characteristics are shown in Table 1. All patients received some form of radiation therapy and 27 patients (35%) received chemoradiation. Twenty-four patients (24%) underwent radical hysterectomy.
Table 1.
Demographic and clinical characteristics (N=78)
| Median age, years (range) | 44.1 (24.9–67.8) |
| Median time since diagnosis, months (range) | 32.5 (1.9–112.8) |
| Characteristic | n (%) |
| Race | |
| Non-Hispanic white | 21 (26.9) |
| Black | 25 (32.1) |
| Hispanic | 32 (41.0) |
| Marital status | |
| Single | 23 (29.5) |
| Married | 35 (44.9) |
| Divorced | 16 (20.5) |
| Other | 4 (5.1) |
| Has children | 71 (91.0) |
| Menopause status | |
| Yes | 65 (83.3) |
| No | 13 (16.7) |
| Smoking status | |
| Yes (Ever) | 44 (56.4) |
| No | 34 (43.6) |
| Language | |
| English | 63 (80.8) |
| Spanish | 15 (19.2) |
| Education | |
| Less than high school | 25 (32.1) |
| High school or technical school | 30 (38.5) |
| Some college | 11 (14.1) |
| College degree or higher | 11 (14.1) |
| Uninsured or received Medicaid | |
| Yes | 35 (46) |
| No | 43 (54) |
| Stage | |
| IA1 or IA2 | 5 (6.4) |
| IB1 | 29 (37.2) |
| IB2 | 25 (32.1) |
| IIA or IIB | 13 (16.7) |
| IIIB | 5 (6.4) |
| IVA or IVB | 1 (1.3) |
| Histologic type | |
| Squamous cell | 63 (80.80) |
| Adenocarcinoma | 10 (12.8) |
| Adenosquamous cell | 1 (1.3) |
| Other | 4 (5.1) |
VAS and SG Preferences
VAS and SG preference scores are listed in Table 2. High VAS scores reflect favorable ratings, and low VAS scores are unfavorable. Similarly, high SG scores indicate that patients are more willing to accept the specific health state being evaluated (e.g. diarrhea), and less willing to accept the chance of experiencing the worst health state (being bedridden due to severe nausea and vomiting).
Table 2.
Visual Analog Scale (VAS) and modified Standard Gamble (SG) scores for all patients (N=78).
| VAS Score | SG Score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Health state | Median | Range* | Mean | SD** | Median | Range* | Mean | SD** | ||
| Menopause | 0.45 | 0.00 – 1.00 | 0.45 | 0.33 | 0.90 | 0.00 – 1.0 | 0.78 | 0.24 | ||
| Dietary changes | 0.42 | 0.00 – 1.00 | 0.44 | 0.29 | 0.90 | 0.00 – 1.00 | 0.75 | 0.25 | ||
| Urinary self-catheterization | 0.33 | 0.00 – 1.00 | 0.37 | 0.30 | 0.70 | 0.00 – 1.0 | 0.62 | 0.29 | ||
| Sexual dysfunction | 0.30 | 0.00 – 1.00 | 0.37 | 0.30 | 0.90 | 0.00 – 1.0 | 0.72 | 0.29 | ||
| Vaginal length shortening | 0.26 | 0.00 – 0.95 | 0.33 | 0.27 | 0.90 | 0.10 – 1.0 | 0.75 | 0.24 | ||
| Diarrhea | 0.25 | 0.00 – 1.00 | 0.34 | 0.29 | 0.70 | 0.00 – 0.98 | 0.64 | 0.29 | ||
| Nausea and vomiting | 0.25 | 0.00 –0.94 | 0.33 | 0.28 | 0.70 | 0.00 – 1.0 | 0.63 | 0.28 | ||
| Rectal bleeding | 0.20 | 0.00 – 0.97 | 0.25 | 0.24 | 0.60 | 0.00 – 1.0 | 0.58 | 0.32 | ||
Scores range from 0.0=least favorable to 1.0=most favorable.
SD, standard deviation
Using the diarrhea health state as an example, a median SG score of 0.95 would mean that patients will accept a 5% chance of the worst health state (becoming bedridden due to severe nausea and vomiting) in order to not have to experience diarrhea. However, if the chance of being bedridden due to severe nausea and vomiting exceeds 5%, patients would rather experience diarrhea. Median VAS and SG preference scores are shown in Table 2.
The health states most highly ranked by VAS were menopause and dietary changes (median scores of 0.45 and 0.42, respectively). These were followed by urinary self-catheterization, sexual dysfunction, vaginal length shortening, diarrhea, and nausea and vomiting. Rectal bleeding was the least favorable health state (median score of 0.20). By SG, four health states tied for most favorable score with median scores of 0.90: menopause, dietary changes, sexual dysfunction, and vaginal length shortening. Rectal bleeding was the least favorable health state by SG (median of 0.60). The remaining health states received median SG scores of 0.70. Overall, health states patients rated as most favorable by VAS were also the health states rates as most favorable by SG.
Age
Increasing age was associated with higher (more favorable) VAS scores for menopause and vaginal length (r=0.233, p=0.04 and r=0.239, p=0.036). When evaluating preferences by SG score this association was not seen, and increasing age was associated with lower (less favorable) scores for menopause (r= −0.359, p=0.002).
Race
African-American patients had higher VAS scores than Hispanic and non-Hispanic white patients for dietary changes (p=0.05), sexual dysfunction (p=0.028), and diarrhea (p=0.05). African-American patients had higher SG scores than Hispanic and non-Hispanic white patients for menopause (p=0.046). Median VAS and SG preference scores by race are shown in Figures 3 and 4.
Figure 3. Median visual analog scale (VAS) scores by ethnicity.
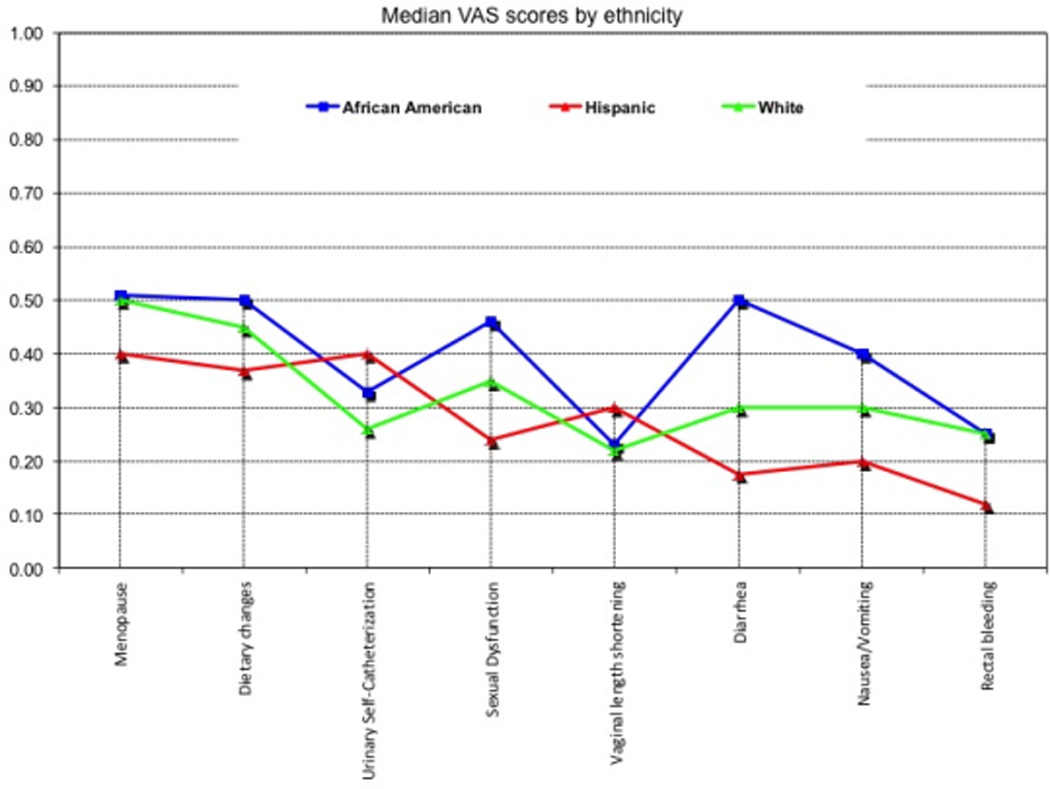
Median VAS scores for each health state are outlined by race/ethnicity. Higher score indicates a more favorable view of the health state for that race/ethnicity.
Figure 4. Median modified standard gamble (SG) scores by ethnicity.
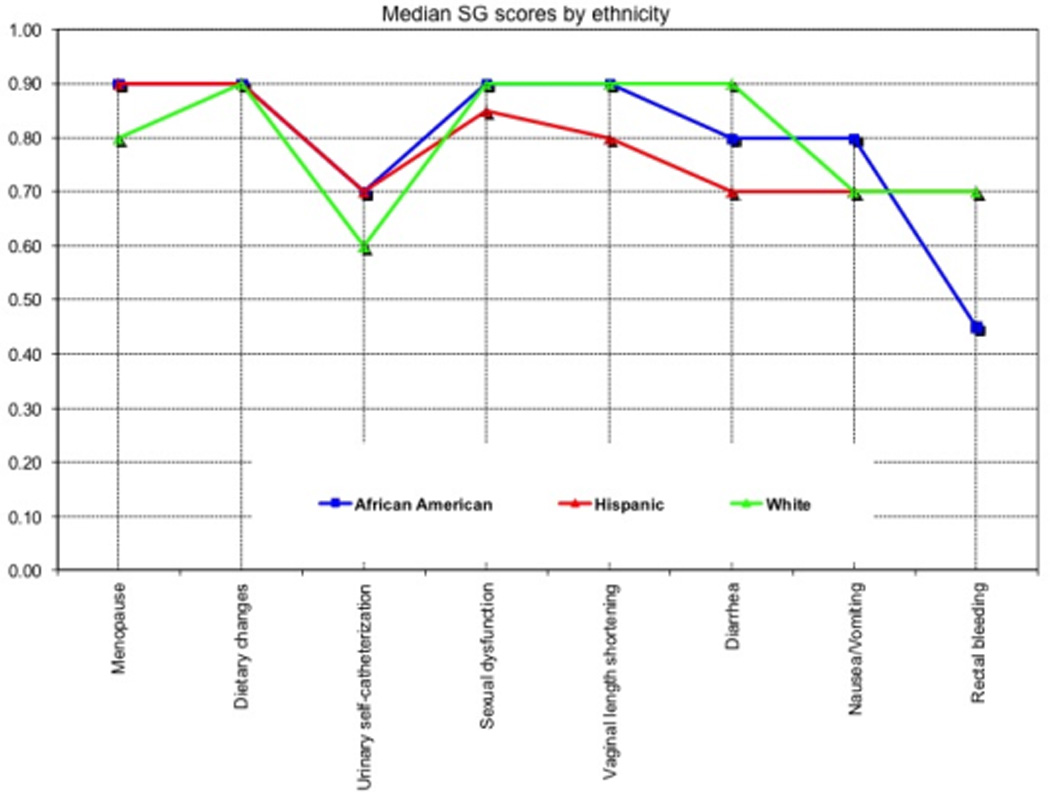
Median SG scores for each health state are outlined by race/ethnicity. Higher score indicates a more favorable view of the health state for that race/ethnicity.
Marital status and Presence of Children
Married women had less favorable VAS scores for menopause (p=0.01), dietary changes (p=0.04), sexual dysfunction (p=0.05), and nausea/vomiting (p=0.045). when compared to women who were not married. Women with children gave more favorable VAS scores for diarrhea (p=0.02) and nausea/vomiting (p=0.01), but worse scores for vaginal length shortening (p=0.042) when compared with women who did not have children. There were no statistically significant differences in SG preferences based on marital status or the presence of children.
Radiation Therapy
Compared with women who underwent radical hysterectomy, women who were treated with radiation and brachytherapy with ALTO rated menopause more favorably by VAS score (0.16 vs. 0.5 p=0.05). Women who had received radiation and brachytherapy with ALTO also rated urinary self-catheterization less favorably by VAS score, but this difference was not statistically significant (0.28 vs. 0.48, p=0.127) There were no statistically significant differences in SG preferences between women who had or had not received radiation therapy.
Chemotherapy
Women who had received chemotherapy rated urinary self-catheterization less favorably by VAS compared to those who had not (0.13 vs 0.4, p=0.045). Women who had received chemotherapy also gave lower VAS scores to nausea/vomiting compared to those who had not, but this difference was not statistically significant (0.18 vs. 0.27, p=0.13). There were no statistically significant differences in SG preferences between women who had or had not received chemotherapy.
DISCUSSION
Studies of patient preferences give us a better understanding of our patient’s desires regarding the treatment of their disease. Prior preference studies among women with cervical cancer predominately focused on preferences regarding method of treatment and surgical or radiation complications (10, 11). Our study examined common health states associated with surgical, radiation, and chemotherapeutic treatment of cervical cancer in an effort to obtain a better understanding of the impact these treatments have on the patient. By identifying factors that influence patient preferences, we hope not only to customize treatment plans to the individual patient, but also to encourage increased exploration of quality-adjusted clinical outcomes. This study demonstrates that preferences for treatment side effects among women with cervical cancer vary depending upon multiple demographic, disease, and treatment factors.
Among our patients, VAS scores were lower than SG scores for each health state. This variation between VAS and SG scores is expected due to the differences in the construction of the two instruments (7). VAS scores are generally lower than SG scores because the VAS asks patients for their ordinal rating of each health state. Accordingly, there is no personal risk associated with the patients’ VAS scores. In contrast, the SG requires patients to associate some level of personal risk with their score. Our findings confirm those of previous studies regarding the general trend of scores for each instrument (11, 16–19).
Age
Prior research has shown mixed results for the role of age and patient preferences (20). Our study found an association between increasing age and more favorable VAS scores for menopause and shortened vaginal length. This suggests that these side effects were less bothersome in older women.
However, when SG scores were assessed, increasing age was associated with a decreased willingness to undergo menopause. Initially, this may appear to contradict our VAS results; however, several factors may have affected these scores among older women. First of all, the SG offers the patient a choice, whereas the VAS does not. This may result in lower SG scores due to patient willingness to accept an increased risk of the worst-case SG health state (severe nausea and vomiting resulting in bed rest) in order to avoid the primary health state (menopause). Secondly, the worst-case SG health state used in our model is temporary, whereas menopause is permanent.
The temporary nature of the worst-case health state (nausea and vomiting resulting in bedrest) may have impacted SG scores among older, menopausal patients because these women may have been more willing than younger, pre-menopausal women to accept the temporary worst health state in order to avoid the permanent state of menopause. This suggests that older women are able to better understand the significance and permanence of menopause when compared to younger women. However, when not given a choice to forgo menopause (via the VAS), older women appear less bothered by menopause. This suggests that older women, despite greatly appreciating the significance of menopause, are more willing than younger women to undergo treatments with a high likelihood of menopause. Perhaps this willingness occurs because older women have either already gone through menopause or expect to go through it in the near future.
Race
Racial differences may alter treatment preferences (21, 22). Despite this, the role of race for preferences of treatment side effects has not been previously evaluated. Our data suggest that African-American women had more favorable views by VAS for dietary changes, sexual dysfunction, and diarrhea than did non-Hispanic white and Hispanic women. The SG did not demonstrate these same differences in preferences. Using the SG, the only statistically significant difference noted was that African-American women viewed menopause more favorably than non-Hispanic white and Hispanic women. This suggests that African-American women were less bothered by menopause than non-Hispanic white and Hispanic women.
Treatment experience
Patients’ previous experiences are key determinants of their preferences (7, 23). Patients tend to give favorable preference scores for treatments that they have already received because they are less fearful of side effects that they have already experienced. In our study, women who received prior radiation therapy gave more favorable VAS scores to menopause, when compared to those undergoing surgery. A possible reason is that, thus far, these women have had good clinical outcomes without the morbidity associated with surgery, thus reinforcing the notion that this treatment (and resulting side effects) was worthwhile to them. This phenomenon is known as “response shift” and involves an internal change of patients’ standards or adaptation in patients with a disability; these changes may result in a “valuation shift” or higher values for adverse health states (7, 24).
One exception to response shift is nausea and vomiting, which has consistently been reported as one of the most dreaded side effects of chemotherapy (25–30). In our study, women who previously had chemotherapy gave the lowest VAS scores to nausea and vomiting. While not statistically significant, this trend suggested that women who had previously experienced chemotherapy induced nausea and vomiting were more likely to view it unfavorably. These preferences are consistent with results of our previous study, in which preferences for nausea and vomiting actually worsened after patients completed treatment (15). This suggests that experiencing this side effect results in a negative valuation shift.
Limitations
Interpretation of SG data may be limited by our use of a non-death health state as an anchor. Since this was our first preference assessment study with cervical cancer patients, we chose this state because we wanted to minimize potential emotional burden on our patients. Other investigators have also acknowledged this need when conducting patient preferences in gynecologic oncology settings (16).
We also acknowledge the limitations of evaluating only women without evidence of disease. These women generally were healthy and not currently experiencing the health states being evaluated. Specifically, they may have viewed certain health states more favorably compared to patients currently experiencing those health states as a result of active treatment. For example, a patient in our study may more favorably view the health state of nausea/vomiting compared to a patient currently undergoing chemotherapy and experiencing severe nausea/vomiting. Accordingly, the ability to generalize the results of our study to patients currently undergoing active treatment for cervical cancer is somewhat limited. Nonetheless, our study is one of the first to provide a cross-sectional side-effect preference profile for cervical cancer survivors.
Conclusions
Patient preference studies allow providers to gain insight into the aspects of care that are most important to the individual patient. Increased understanding of the factors influencing patient preferences will allow providers to formulate care that is tailored to the needs of each patient. Our study demonstrates that preferences in cervical cancer patients vary based on multiple demographic, disease and treatment factors. These results suggest that cervical cancer patients may prefer to undergo different primary and adjuvant treatments (with their associated side-effects) for their disease depending on their demographic characteristics and disease status. Accordingly, the results of this study may be used to help guide discussions with patients regarding their preferences for the treatment options available to them. Additionally, these results provide researchers with preferences data that can be incorporated into future quality-adjusted survival and cost-effectiveness analyses, ensuring that the outcomes reflect the preferences of cervical cancer patients.
Future studies should explore the role of age and whether patient preferences change over time, particularly with regard to sexual dysfunction, menopause, and fertility. As survivorship research in gynecologic oncology patients continues to grow, we need to develop a better understanding of how women perceive acute- and long-term treatment effects. Future management strategies can then be developed and implemented to prevent or minimize the impact of side effects on women’s lives during and after cancer treatment.
References
- 1.American Cancer Society Cancer Facts and Figures 2014. Available from: http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-041770.pdf.
- 2.Eifel PJ. Chemoradiotherapy in the Treatment of Cervical Cancer. Semin Radiat Oncol. 2006;16(3):177–185. doi: 10.1016/j.semradonc.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 3.Maher EJ, Denton A. Survivorship, Late Effects and Cancer of the Cervix. Clin Oncol. 2008;20(6):479–487. doi: 10.1016/j.clon.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 4.Frumovitz M, Sun CC, Schover LR, Munsell MF, Jhingran A, Wharton JT, et al. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol. 2005;23(30):7428–7436. doi: 10.1200/JCO.2004.00.3996. [DOI] [PubMed] [Google Scholar]
- 5.Korfage IJ, Essink-Bot M-L, Mols F, van de Poll-Franse L, Kruitwagen R, van Ballegooijen M. Health-Related Quality of Life in Cervical Cancer Survivors: A Population-Based Survey. Int J Radiat Oncol Biol Phys. 2009;73(5):1501–1509. doi: 10.1016/j.ijrobp.2008.06.1905. [DOI] [PubMed] [Google Scholar]
- 6.Barker CL, Routledge JA, Farnell DJ, Swindell R, Davidson SE. The impact of radiotherapy late effects on quality of life in gynaecological cancer patients. Br J Cancer. 2009;100(10):1558–1565. doi: 10.1038/sj.bjc.6605050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stiggelbout AM, de Haes JC. Patient preference for cancer therapy: an overview of measurement approaches. J Clin Oncol. 2001;19(1):220–230. doi: 10.1200/JCO.2001.19.1.220. [DOI] [PubMed] [Google Scholar]
- 8.Frederiksen ME, Lynge E, Rebolj M. What women want. Women's preferences for the management of low-grade abnormal cervical screening tests: a systematic review. BJOG. 2012;119(1):7–19. doi: 10.1111/j.1471-0528.2011.03130.x. [DOI] [PubMed] [Google Scholar]
- 9.Kuppermann M, Melnikow J, Slee C, Tancredi DJ, Kulasingam S, Birch S, et al. Preferences for surveillance strategies for women treated for high-grade precancerous cervical lesions. Gynecol Oncol. 2010;118(2):108–115. doi: 10.1016/j.ygyno.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jewell EL, Smrtka M, Broadwater G, Valea F, Davis DM, Nolte KC, et al. Utility scores and treatment preferences for clinical early-stage cervical cancer. Value Health. 2011;14(4):582–586. doi: 10.1016/j.jval.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 11.Einstein MH, Rash JK, Chappell RJ, Swietlik JM, Hollenberg JP, Connor JP. Quality of life in cervical cancer survivors: patient and provider perspectives on common complications of cervical cancer and treatment. Gynecol Oncol. 2012;125(1):163–167. doi: 10.1016/j.ygyno.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 12.Drummond M, O'Brien B, Stoddart G, Torrance G. Methods For The Economic Evaluation of Health Care Programmes. 2nd ed. New York: Oxford University Press; 1997. [Google Scholar]
- 13.Read JL, Quinn RJ, Berwick DM, Fineberg HV, Weinstein MC. Preferences for health outcomes. Comparison of assessment methods. Med Decis Making. 1984;4(3):315–329. doi: 10.1177/0272989X8400400307. [DOI] [PubMed] [Google Scholar]
- 14.Sung L, Greenberg ML, Young NL, McLimont M, Ingber S, Rubenstein J, et al. Validity of a modified standard gamble elicited from parents of a hospital-based cohort of children. Journal of Clinical Epidemiology. 2003;56(9):848–855. doi: 10.1016/s0895-4356(03)00160-4. [DOI] [PubMed] [Google Scholar]
- 15.Sun C, Bodurka D, Donato M, Borden C, Rubenstein E. Nausea and vomiting side-effects of cancer therapies: preference assessments from patients, health care providers and healthy women. Supportive Care in Cancer. 2002;10(4):378. [Google Scholar]
- 16.Havrilesky LJ, Broadwater G, Davis DM, Nolte KC, Barnett JC, Myers ER, et al. Determination of quality of life-related utilities for health states relevant to ovarian cancer diagnosis and treatment. Gynecol Oncol. 2009;113(2):216–220. doi: 10.1016/j.ygyno.2008.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sung L, Young NL, Greenberg ML, McLimont M, Samanta T, Wong J, et al. Health-related quality of life (HRQL) scores reported from parents and their children with chronic illness differed depending on utility elicitation method. J Clin Epidemiol. 2004;57(11):1161–1166. doi: 10.1016/j.jclinepi.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Nease RF, Jr, Kneeland T, O'Connor GT, Sumner W, Lumpkins C, Shaw L, et al. Variation in patient utilities for outcomes of the management of chronic stable angina. Implications for clinical practice guidelines. Ischemic Heart Disease Patient Outcomes Research Team. JAMA. 1995;273(15):1185–1190. [PubMed] [Google Scholar]
- 19.Bass EB, Steinberg EP, Pitt HA, Griffiths RI, Lillemoe KD, Saba GP, et al. Comparison of the rating scale and the standard gamble in measuring patient preferences for outcomes of gallstone disease. Med Decis Making. 1994;14(4):307–314. doi: 10.1177/0272989X9401400401. [DOI] [PubMed] [Google Scholar]
- 20.Lloyd A, Nafees B, Narewska J, Dewilde S, Watkins J. Health state utilities for metastatic breast cancer. Br J Cancer. 2006;95(6):683–690. doi: 10.1038/sj.bjc.6603326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin MY, Pisu M, Oster RA, Urmie JM, Schrag D, Huskamp HA, et al. Racial variation in willingness to trade financial resources for life-prolonging cancer treatment. Cancer. 2011;117(15):3476–3484. doi: 10.1002/cncr.25839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Givens JL, Tjia J, Zhou C, Emanuel E, Ash AS. Racial and ethnic differences in hospice use among patients with heart failure. Arch Intern Med. 2010;170(5):427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jansen SJ, Otten W, Stiggelbout AM. Review of determinants of patients' preferences for adjuvant therapy in cancer. J Clin Oncol. 2004;22(15):3181–3190. doi: 10.1200/JCO.2004.06.109. [DOI] [PubMed] [Google Scholar]
- 24.Barclay-Goddard R, Epstein JD, Mayo NE. Response shift: a brief overview and proposed research priorities. Qual Life Res. 2009;18(3):335–346. doi: 10.1007/s11136-009-9450-x. [DOI] [PubMed] [Google Scholar]
- 25.Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, et al. On the receiving end--patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol. 1983;19(2):203–208. doi: 10.1016/0277-5379(83)90418-2. [DOI] [PubMed] [Google Scholar]
- 26.de Boer-Dennert M, de Wit R, Schmitz PI, Djontono J, v Beurden V, Stoter G, et al. Patient perceptions of the side-effects of chemotherapy: the influence of 5HT3 antagonists. Br J Cancer. 1997;76(8):1055–1061. doi: 10.1038/bjc.1997.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Griffin AM, Butow PN, Coates AS, Childs AM, Ellis PM, Dunn SM, et al. On the receiving end. V: Patient perceptions of the side effects of cancer chemotherapy in 1993. Ann Oncol. 1996;7(2):189–195. doi: 10.1093/oxfordjournals.annonc.a010548. [DOI] [PubMed] [Google Scholar]
- 28.Lindley C, McCune JS, Thomason TE, Lauder D, Sauls A, Adkins S, et al. Perception of chemotherapy side effects cancer versus noncancer patients. Cancer Pract. 1999;7(2):59–65. doi: 10.1046/j.1523-5394.1999.07205.x. [DOI] [PubMed] [Google Scholar]
- 29.Sun CC, Bodurka DC, Donato ML, Rubenstein EB, Borden CL, Basen-Engquist K, et al. Patient preferences regarding side effects of chemotherapy for ovarian cancer: do they change over time? Gynecol Oncol. 2002;87(1):118–128. doi: 10.1006/gyno.2002.6807. [DOI] [PubMed] [Google Scholar]
- 30.Sun CC, Bodurka DC, Weaver CB, Rasu R, Wolf JK, Bevers MW, et al. Rankings and symptom assessments of side effects from chemotherapy: insights from experienced patients with ovarian cancer. Support Care Cancer. 2005;13(4):219–227. doi: 10.1007/s00520-004-0710-6. [DOI] [PubMed] [Google Scholar]


