INTRODUCTION
The terms “endemic” and “epidemic” were coined by hippocrates, who distinguished between diseases that were always present in a given population, and diseases which used to occur during certain periods of an year or during certain years.[1] These terms have now become an integral part of the medical etymology. Predominantly used to describe acute infectious diseases, the term “epidemic” is increasingly being utilized to describe the increasing prevalence of noninfectious, metabolic or chronic diseases. This communication tries to discuss the relevance and accuracy of these terms with relation to diabetes mellitus, suggests improvements in their usage, and proposes that diabetes can now be termed an endemic disease.
DEFINITIONS
Much debate surrounds the use of term “endemicity” in infectious illness. The definition of these concepts is still evolving and is open to debate. Endemic is currently being used only as an adjective, to describe an area, or a disease. The size of an area and the duration of endemicity of a condition, however, may vary. Various definitions, some disease-specific, have been proposed to explain the concept of endemicity. Many of the earlier definitions, such as those related to malaria, yellow fever, and plague have gone out of use.
One old (dating to 1948), clinically based definition proposed for cholera is still relevant. It states: “An endemic area is one in which over a number of years, these is practically continuous presence of clinical cholera with annual seasonal exacerbation of incidence.”[1] The Dictionary of Epidemiology defines an endemic disease as “the constant presence of a disease or infectious agent within a given geographic area or population group; may also refer to the usual prevalence of a given disease within such an area or group.”[2]
The term epidemic can be an adjective but is often used as a noun, e.g. the diabetes epidemic. While the word epidemic is almost universally prefixed to diabetes now, it seems to be used in a colloquial, rather than a scientific sense. The Dictionary of Epidemiology defines an epidemic as “the occurrence in a community or region of cases of an illness, specific health-related behavior, or other health-related events clearly in excess of normal expectancy.”[2] Based upon this, diabetes is certainly an epidemic in most countries.
Sometimes, public health professionals also fix criteria (of prevalence/incidence) to label a disease as endemic or epidemic on the basis of its significance as a public health problem. Such a criterion has been defined for endemicity/severity of goiter.[3,4] However, no such criteria have been proposed for diabetes mellitus or the many other chronic metabolic conditions so far.
DESCRIBING THE EPIDEMIOLOGY OF DIABETES MELLITUS
But when will be the syndrome of diabetes mellitus cease to become an epidemic, and be characterized as an endemic condition? Using the 1948 definition for cholera as a framework, India is now an endemic country for diabetes as, “over a number of years, there is practically continuous presence of clinical diabetes.”
If we try to approach this issue objectively, using prevalence data, or incidence rates, an even stronger picture emerges. Reasonably accurate data are available for the prevalence of diabetes over the past few decades. As we know, an epidemic term is used when the cases are “clearly in excess of normal expectancy.” We take the criteria of “more than 2 standard deviations (SD)” to assess whether cases are clearly in excess of normal expectancy or not. If the disease is not seasonal, we can compare the current prevalence with previous years’ prevalence (incidence in case of acute/communicable diseases). However, as diabetes develops slowly, it may be prudent to analyze decadal prevalence to assess whether the syndrome is epidemic or not. If the increase over a decade is more than 2 SD, diabetes is certainly epidemic. If it (the increase) ceases to be more than 2 SD and varies within 2 SD, it may be described as being endemic to a particular territory. Hence, if the change in decadal prevalence of diabetes is < 2 SD, it may cease to be an epidemic disease, and will be better characterized as an endemic syndrome. This is a simple way of determining endemicity/epidemicity.
INDICES OF ENDEMICITY AND EPIDEMICITY
We can extrapolate novel concepts, proposed by pioneers in the field, to refine this concept further. The term ‘endemic index’ was first used by Swaroop in 1957, in the context of infectious disease. He discussed the duration of time, or number of years, to be used while calculating an endemicity index, but did not put forward any mathematical equation.[1]
Deterministic and stochastic mathematical models are available to predict epidemicity and endemicity of infectious illnesses.[5] These use the basic reproduction number of an infectious agent to predict when an endemic illness will convert into an epidemic, or vice versa. With required modification, these models can be utilized to predict the endemicity of diabetes.
Dowse et al. have described “diabetes epidemicity index (DEpI)” which is the ratio of impaired glucose tolerance (IGT) to total glucose intolerance (TGI) as an illustrative indicator of diabetes epidemic in a given population.[6] They suggested that the future prevalence of noninsulin dependent diabetes mellitus will depend on the prevalence of IGT, distribution of diabetes risk factors in the population and the mortality rates.[6]
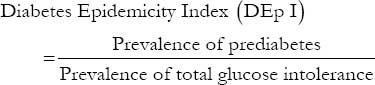
Jayawardena et al. have reported a high DEpI in Sri Lanka (52.8%), and relatively lower values in Bangladesh (33.1%), urban India (31.3%) and rural India (26.9%).[7] From an “epidemic perspective,” these values were suggested to predict a higher increase in the incidence of diabetes in Sri Lanka than its neighboring countries.[7] This, in turn, implies that a steep upward trend in the occurrence which is the defining feature of an epidemic will continue to occur in Sri Lanka, or any other country with a high DEpI.
The diabetes endemicity index
We propose looking at this data through an antipodal prism: Through that of an endemic. As suggested by Dowse et al., a low DEpI implies that the prevalence of diabetes will not change markedly.[6] New cases of diabetes (conversion from prediabetes to diabetes) will be balanced by the death of older cases of diabetes which will bring about an equilibrium in the prevalence.[6] To be accurate, detailed biostatistical analysis will require data related to conversion rate of prediabetes to diabetes, as well as mortality rates in people with diabetes. Such data, however, may be lacking for many populations.
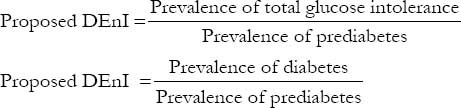
Simpler methods, therefore, can be utilized to assess endemicity. The reverse of DEpI, that is, ratio of TGI prevalence to prediabetes prevalence, can be used to calculate a diabetes endemicity index (DEnI). The ratio of diabetes to prediabetes may be another path to assessing DEnI. The higher the DEnI, the lesser the potential pool of cases which will convert to diabetes, and hence, the greater the justification of coining the term “diabetes endemia.”
In addition, the determinants of prevalence trends such as inflow and outflow of cases due to immigration, or deaths due to quality of health care facilities must be kept in mind while interpreting these indices or trends. Apart from this, surveillance programs which involve periodic surveys for risk factors of diabetes, and other chronic disorders facilitate timely decision making and corrective actions.[8]
Utility of diabetes endemicity index
Thus, these indices will help supplement predictions of future prevalence trends of diabetes, and facilitate decision-making regarding the epidemic or endemic nature of a given frequency of the disease. In a time, this concept may be extended to determine the endemicity of prediabetes as well as other diseases. As far as chronic diseases, especially diabetes, are concerned today, the term endemic seems preferable to that of the epidemic. Further research is required to focus on how the endemicity concept may be refined to understand the epidemiology of chronic diseases, including diabetes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Swaroop S. Index of endemicity. Bull World Health Organ. 1957;16:1083–101. [PMC free article] [PubMed] [Google Scholar]
- 2.Porta M, editor. 5th ed. New York: Oxford University Press; 2008. Dictionary of Epidemiology; pp. 78–9. [Google Scholar]
- 3.Koutras DA. Endemic goiter: An update. Hormones (Athens) 2002;1:157–64. doi: 10.14310/horm.2002.1163. [DOI] [PubMed] [Google Scholar]
- 4.Medani AM, Elnour AA, Saeed AM. Endemic goitre in the Sudan despite long-standing programmes for the control of iodine deficiency disorders. Bull World Health Organ. 2011;89:121–6. doi: 10.2471/BLT.09.075002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacquez JA, O’Neill P. Reproduction numbers and thresholds in stochastic epidemic models. I. Homogeneous populations. 1991;107:161–86. doi: 10.1016/0025-5564(91)90003-2. [DOI] [PubMed] [Google Scholar]
- 6.Dowse GK, Zimmet PZ, King H. Relationship between prevalence of impaired glucose tolerance and NIDDM in a population. Diabetes Care. 1991;14:968–74. doi: 10.2337/diacare.14.11.968. [DOI] [PubMed] [Google Scholar]
- 7.Jayawardena R, Ranasinghe P, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence and trends of the diabetes epidemic in South Asia: A systematic review and meta-analysis. BMC Public Health. 2012;12:380. doi: 10.1186/1471-2458-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Integrated Disease Surveillance Project: Operations manual for District Surveillance Unit. New Delhi: Government of India; 2004. Ministry of Health and Family Welfare. [Google Scholar]


