Abstract
Background:
The increased incidence of autoimmune thyroid disease with increasing dietary iodine intake has been demonstrated both epidemiologically and experimentally. The hypothyroidism that occurs in the first year following radioactive iodine therapy is probably related to the destructive effects of the radiation and underlying ongoing autoimmunity.
Objective:
To study the outcomes at the end of six months after fixed dose I, 131therapy for Graves’ disease followed by an iodine restricted diet for a period of six months.
Materials and Methods:
Consecutive adult patients with Graves’ disease planned for I131 therapy were randomized either to receive instructions regarding dietary iodine restriction or no advice prior to fixed dose (5mCi) I131 administration. Thyroid functions and urinary iodine indices were evaluated at 3rd and 6th month subsequently.
Results:
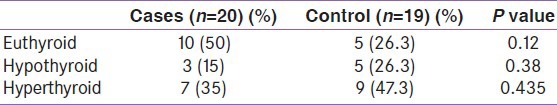
Forty seven patients (13M and 34F) were assessed, 2 were excluded, 45 were randomized (Cases 24 and Controls 21) and 39 patients completed the study. Baseline data was comparable. Median urinary iodine concentration was 115 and 273 μg/gm creat (p = 0.00) among cases and controls respectively. Outcomes at the 3rd month were as follows (cases and controls); Euthyroid (10 and 6: P = 0.24), Hypothyroid (3 and 5: P = 0.38) and Hyperthyroid (7 and 8: P = 0.64). Outcomes at the end of six months were as follows (cases and controls); Euthyroid (10 and 5: P = 0.12), Hypothyroid (3 and 5: P = 0.38) and Hyperthyroid (7 and 9: P = 0.43). Of the hypothyroid patients 5 (cases 1 and controls 4: P = 0.13) required thyroxine replacement.
Conclusions:
There was no statistical significant difference in the outcome of patients with dietary iodine restriction following I131 therapy for Graves’ disease.
Keywords: Dietary iodine restriction, graves’ disease, radioactive iodine, urinary iodine/creatinine ratios
INTRODUCTION
Radioactive 131Iodine (RAI) is widely used to treat hyperthyroid Graves’ disease. Treatment with radioactive I131 is safe and highly effective and the only significant complication of this therapy is the development of permanent hypothyroidism.[1] In addition to permanent hypothyroidism, transient hypothyroidism may occur 2 to 5 months after I131 therapy and then spontaneously remit over the next few months.[2,3] Over 50% of patients who developed hypothyroidism within six months after I131 treatment recover spontaneously. The mean time to develop permanent hypothyroidism is shorter in patients with transient hypothyroidism than in patients who do not develop transient hypothyroidism.[4]
The hypothyroidism that occurs in the first year following radioactive iodine therapy is probably related to the destructive effects of the radiation, while the subsequent occurrence of hypothyroidism is due to a combination of radiation injury and underlying and ongoing autoimmunity.[5] Hypothyroidism would probably occur in all patients if they lived long enough.[6,7] The development of transient hypothyroidism with recovery of thyroid function has been related by some to ongoing autoimmunity. The enduring presence of thyroid stimulating antibody in patients with transient hypothyroidism may play a role in the recovery of thyroid function in this group of patients.[4]
Among various population groups, epidemiological studies have shown increasing incidence of thyroid autoimmunity with increasing iodine content.[8,9,10] Clinical studies have also suggested a relationship of increased iodine intake in autoimmune thyroid disease.[11,12,13] This effect was however only observed in genetically susceptible individuals.[14] Many mechanisms have been suggested to explain the association of iodine intake and autoimmune thyroid disease. They include damage by generation of free radicals, direct injury to thyrocytes and pharmacological inhibition of the iodine pump. The most important mechanism is probably the promotion of thyroid autoimmunity by the increased iodine content of thyroglobulin.[15]
In this study, we are looking at the role of dietary iodine in the development of transient and permanent hypothyroidism in patients with Graves’ disease treated with radioactive iodine over a six months period. The aim of the study was to compare the incidence of permanent and transient hypothyroidism following fixed dose radioactive iodine among patients randomized to dietary iodine restriction and those on a normal iodine diet.
MATERIALS AND METHODS
Recruitment of the study cohort was done from the Endocrinology outpatient department of a university affiliated teaching hospital. The research proposal was informed to the Institutional Review Board and was ratified by the Committee prior to beginning of the study. All adult patients (≥18 years) presenting with autoimmune thyroid disease and thyrotoxicosis who were willing to undergo radioactive I131 treatment for thyrotoxicosis were assessed for inclusion into the study. Women in the reproductive age group planning on conception in the next 12 months, patients with cardiac decompensation, patients with active Graves’ ophthalmopathy (activity index over 4) and those prescribed iodine containing drugs were excluded from the study.
After explaining the study procedure the patients were provided informed consent forms in English. Randomization was done through the “block randomization technique” taking blocks of four patients each. All patients had baseline investigations including serum thyroid stimulating hormone (TSH), serum total and free thyroxine levels (TT4 and FT4) and radioactive 131I uptake scan at 2h and 24h. Urine was collected at baseline for estimation of Urine iodine/creatinine ratio. All study patients underwent Radioactive Iodine ablation in the Nuclear Medicine Department of our hospital at a fixed dose of 5 MCi (Millicurie). Patients were reassessed by the physician in the nuclear medicine department regarding eligibility for radioactive ablation.
After ablation the patients randomized as cases received instruction for minimizing iodine content in the diet. The following points were emphasized in the diet.
Avoidance of iodized salt and use of locally available non iodized crystal salt.
Avoiding cough mixtures and other over the counter medications without consulting the Investigator.
Avoiding sea fish and egg yolk.
Avoiding chocolate and commercial bakery products.
Avoiding canned meat and vegetable products.
Patient randomized as controls were given general dietary advice and encouraged to use iodized salt.
Serum TSH measurements were done on IMMULITE® 2000 (Siemens Healthcare Diagnostics Inc, Deerfield, IL, USA) which is a solid-phase, two-site chemiluminescent immunometric assay. The assay has an analytic sensitivity of 0.04μIU/L and a coefficient of Variation (CV) of 4.6-12.5%. Serum Total T4 and Free T4 were also performed on IMMULITE® 2000 (Siemens Healthcare Diagnostics Inc, Deerfield, IL, USA). The assays have an analytic sensitivity of 3.86pmol/L and 3.86pmol/L respectively with a CV of 5.6-11.7% for the total T4 assay and a CV of 4.8-9.0% for the free T4 assay. Urine creatinine measurements for estimating the urine iodine/creatinine ratio was done with Hitachi 912 Auto analyzer (F. Hoffmann-La Roche AG, Basel.) using kinetic in vitro assay. Urine Iodine measurements were done manually using the Sandell- Kolthoff reaction.
Statistical analysis was carried out using Statistical Package for Social Sciences Ver 11.0. To determine statistical significance we used Fishers’ exact test and Chi Square.
Patients were classified as euthyroid on visit -2 (three months after ablation) and visit-3 (six months after ablation) if FT4 levels were in the normal range for the laboratory. TSH normalization was not considered as patients may require more time for the recovery of central hypothyroidism. Patients were classified as hyperthyroid in visit -2 (three months after ablation) and visit-3 (six months after ablation) if FT4 levels were above the normal range for the laboratory. If patients received anti thyroid medications at visit-3 for symptoms then they were considered to be hyperthyroid at six month. Patients were classified as hypothyroid on visit -2 (three months after ablation) and visit-3 (six months after ablation) if FT4 levels were below the normal range for the laboratory. Additionally patients with normal FT4 levels and elevated TSH levels were considered to be hypothyroid. Hypothyroid patients were further classified as central, subclinical or primary hypothyroidism. Patients requiring replacement therapy at three months were classified as having primary hypothyroidism at six months.
RESULTS
Baseline data
Forty seven patients were assessed for the study, there were 13 male and 34 females. The mean age was 41 years and median was 40 years. The average duration of symptoms at presentation was over 22 months with a median duration of symptoms at presentation of 12 months. Details of patient enrollment, randomization and study completion is given in Figure 1. Comparison of important baseline values among cases and controls of the 39 patients who completed the study are given in Table 1. The adequacy of dietary iodine restriction among cases is illustrated in Table 2.
Figure 1.
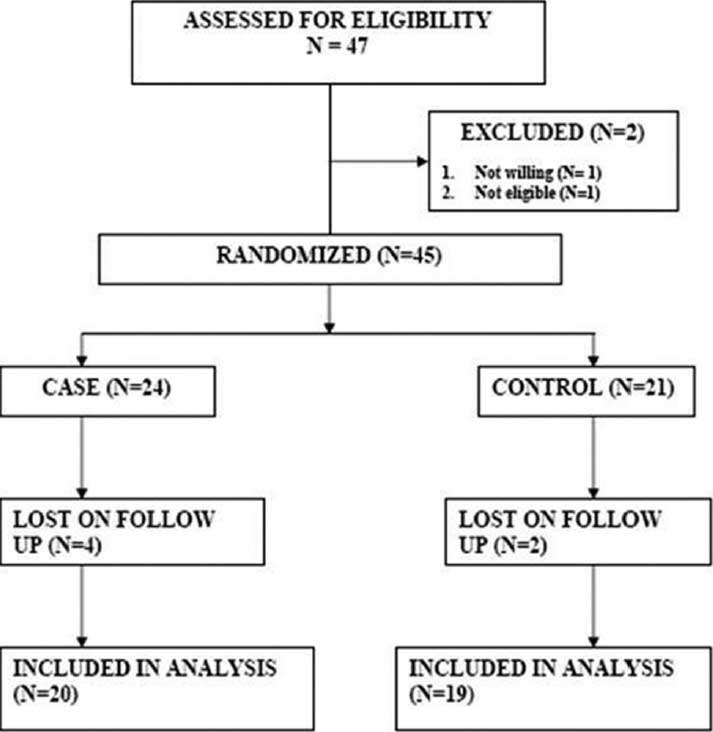
Details of study enrollment, randomization and completion
Table 1.
Baseline variables
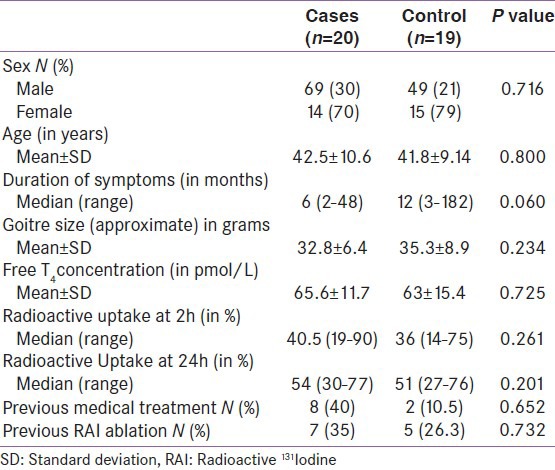
Table 2.
Urinary Iodine creatinine ratio and urinary iodine excretion in cases and controls
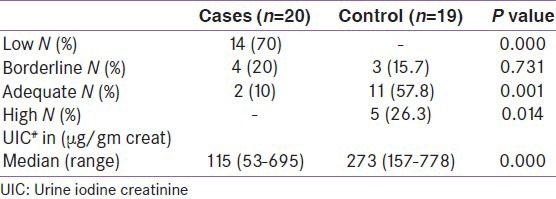
Outcome in patients at third and sixth month
The outcomes of thyroid function tests for patients at third and sixth month of follow up was classified into hypothyroid, euthyroid and hyperthyroid based on the definitions previously given. The details are in Table 3 and 4.
Table 3.
Outcomes of patients at third month
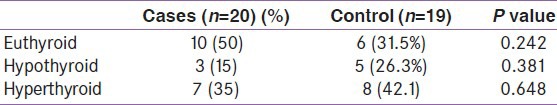
Table 4.
Outcomes of patients at sixth month
Details of hypothyroidism seen in cases and controls
A total of nine patients developed hypothyroidism. One patient had transient hypothyroidism with recovery of thyroid function at the second visit. Among the eight patients who were hypothyroid at six months all but one were hypothyroid at the Three month visit as well. Details are given in Table 5. Figure 2 represents patients with symptomatic primary hypothyroidism requiring Levo-thyroxine replacement among cases and controls during the period of study.
Table 5.
Details of patients who developed Hypothyroidism
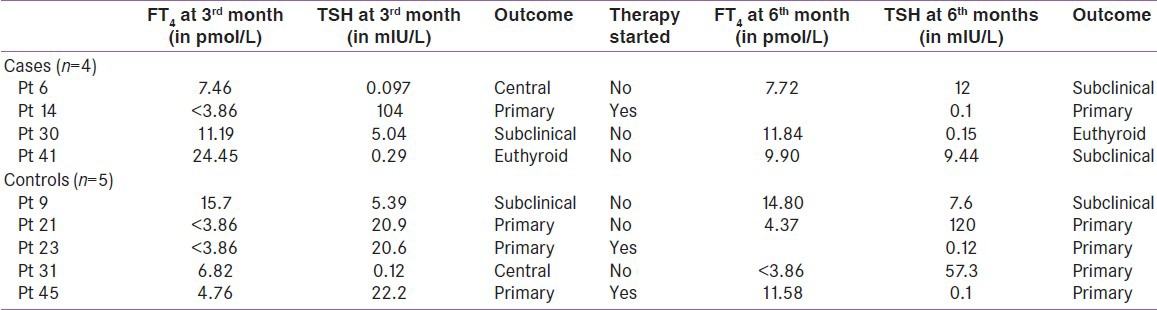
Figure 2.
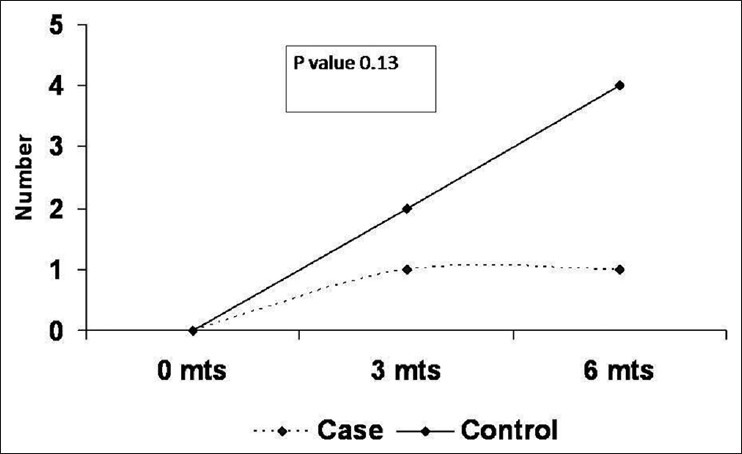
Development of primary hypothyroidism requiring levo-thyroxine in cases and controls
Correlation between serum TSH values at 6 months and urine iodine/creatinine ratios
Figure 3 shows the correlation between highest TSH values and the average urinary iodine excretion as estimated by the Iodine/creatinine ratio.
Figure 3.
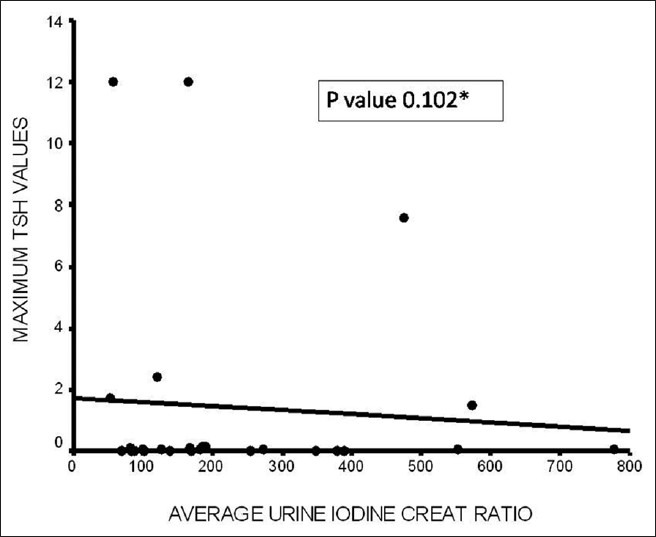
Correlation between Highest TSH values and the average urinary iodine excretion as estimated by the Iodine/creatinine ratio (*One patient with TSH value of 48 IU (outlier) was excluded from the graph)
DISCUSSION
The essential goal in the management of thyrotoxicosis of Grave's disease is to reduce hyper secretion of thyroid hormone. One of the three forms of therapy available, the use of radioactive Iodine is associated with the development of hypothyroidism in a large majority of patients. In this study we could not find any significant benefit of restricting iodine in the diet of patients undergoing radioactive iodine therapy. There were no differences in the development of hypothyroidism at three and six month post I 131ablation or in the overall cure rates among patients who underwent iodine restriction compared to the controls.
In the study, subject iodine intake was restricted in the diet predominantly by changing over from packed iodized salt to locally prepared unpacked crystal salt. Avoidance of other dietary sources of iodine was stressed; however these sources were not important in most patients. The adequacy of the dietary restriction was reflected in the subsequent measurements of urine iodine creatinine (UIC) ratio. The UIC ratio has good co-relation with the 24 hour Iodine excretion estimation in adults.
Transient hypothyroidism
The phenomenon of transient hypothyroidism which was the basis of this study was observed in only one patient in the study. All other patients detected to be hypothyroid at three months continued to be hypothyroid at six month. This is in contrast to Aizawa et al.,[4] who retrospectively looked at 260 patients treated with radioactive therapy and found that 39 (15%) patients had transient hypothyroidism. Transient hypothyroidism was diagnosed when the patients were noted to be hypothyroid at any time during the initial six months and subsequently was found to be euthyroid at the end of the first year. From their study we would expect 36% of patients to develop hypothyroidism in the first six months of whom around 2/3rd would be euthyroid at the end of the year. In our study, only 20% of patients developed hypothyroidism in the first six months. Within this limited period only one patient showed recovery of thyroid functions. There could be two reasons for the failure to demonstrate more patients with transient hypothyroidism. Firstly the overall rates of development of hypothyroidism in the first six months are much less in this series compared to the previous series (36% vs. 20%). This in turn could be related to the lower doses of radioactive iodine used in this study. Secondly, the limited follow-up of six months would miss out the patients who recover thyroid functions over the next six months.
Overall cure rates
An overall cure rate of 58% (23/39) was seen in this cohort at the end of six months with a radioactive iodine dose of 5mCi. This is similar to the results obtained from another center in India.[16] However; the optimal dose of radioactive iodine among Indian patients with Graves’ disease is still unclear. Nordyke and Gilbert analyzed 605 patients treated with radioactive iodine to find out the optimal dose to achieve cure. They concluded that cure was directly related to the dose of 131I administered. The study concluded that the optimal iodine dose for curing hyperthyroidism was approximated by using starting doses of 10mCi and increasing it for unusually large glands and special patient circumstances.[17] Kendall-Taylor et al., examined 225 patients with Graves hyperthyroidism treated with a standard dose of 15mCi of radioactive iodine and found 64% of the patients to be hypothyroid and 30% to be euthyroid at the end of one year.[18] In a similar study done by Alexander et al., they summarized that high dose iodine therapy with a treatment protocol that aimed to deliver 150 to 175Ci I 131/gm of thyroid tissue at 24 hour would be optimal. The average dose used in their study was approximately 8mCi assuming an average thyroid weight 50gms. Using this protocol the authors were able to get a cure rate of 86% in there group of 261 patients.[19] They summarized that high dose radioactive iodine therapy is an effective treatment for patients with Grave's hyperthyroidism. The approach using higher doses is safe, simple and avoids the need for long term follow up or later hypothyroidism. Many of these findings have been well accepted and the Royal College in its guidelines for the use of radioactive iodine in the management of hyperthyroidism recommend a dose in the range of 10mCi for standard case of Graves disease and increasing it for unusually large glands.[20]
The main drawbacks of this study are firstly, the lack of clarity as to what constitutes an adequate dose of radioactive iodine among Indian patients. The dosing used in this study resulted in cure rates much less than expected. Secondly, the limited follow up of six months might result in missing out patients with transient hypothyroidism who recovered thyroid functions after six months. A larger sample size of patients administered a higher dose of radioactive Iodine followed up for a period of one year may have been more appropriate.
In conclusion, there was no statistically significant difference in the development of overt primary hypothyroidism following Radioactive Iodine therapy for Graves’ disease with dietary Iodine restriction. Though a trend for better cure rates at 6 months was noted with dietary Iodine restriction the difference was not statistically significant.
ACKNOWLEDGEMENT
Mrs. Banu for help in patient recruitment and data entry.
Footnotes
Source of Support: UGC, Sri Lanka
Conflict of Interest: None declared.
REFERENCES
- 1.Staffurth JS. Hypothyroidism following radioiodine treatment of thyrotoxicosis. J R Coll Physicians Lond. 1987;21:55–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Dorfman S, Young RL, Carfetta RF. Transient hypothyroidism. Arch Intern Med. 1977;137:256–7. [PubMed] [Google Scholar]
- 3.Connell JM, Hilditch TE, McCruden DC, Alexander WD. Transient hypothyroidism following radioiodine therapy for thyrotoxicosis. Br J Radiol. 1983;56:309–13. doi: 10.1259/0007-1285-56-665-309. [DOI] [PubMed] [Google Scholar]
- 4.Aizawa Y, Yoshida K, Kaise N, Fukazawa H, Kiso Y, Sayama N, et al. The development of transient hypothyroidism after iodine-131 treatment in hyperthyroid patients with Grave's disease: Prevalence, mechanism and prognosis. Clin Endocrinol. 1997;46:1–5. doi: 10.1046/j.1365-2265.1997.d01-1737.x. [DOI] [PubMed] [Google Scholar]
- 5.Becker DV, McConahey WM, Dobins BM. Vol. 1. Vienna: G Gitsel Cie; 1971. The results of thyrotoxicosis therapy follow up study. Further advances in thyroid research; pp. 603–9. [Google Scholar]
- 6.Alevizaki CC, Alevizaki-Harhalaki MC, Ikkos DG. Radioiodine I-131 treatment of thyrotoxicosis: Dose required for and some factors affecting the early induction of hypothyroidism. Eur J Nucl Med. 1985;10:450–4. doi: 10.1007/BF00256589. [DOI] [PubMed] [Google Scholar]
- 7.Cevallos JL, Hagen GA, Maloof F, Chapman EM. Low-dosage 131-I therapy of thyrotoxicosis (diffuse goiters). A five-year follow-up study. N Engl J Med. 1974;290:141–3. doi: 10.1056/NEJM197401172900306. [DOI] [PubMed] [Google Scholar]
- 8.Beierwaltes WH. Iodine and lymphocyte thyroiditis. Bull All India Med Sci. 1969;3:145. [Google Scholar]
- 9.Hay ID. Thyroiditis: A clinical update. Mayo Clin Proc. 1985;60:836–43. doi: 10.1016/s0025-6196(12)64789-2. [DOI] [PubMed] [Google Scholar]
- 10.Weaver DK, Batsakis JG, Nishiyama RH. Relationship of iodine to “lymphocytic goiters”. Arch Surg. 1969;98:183–6. doi: 10.1001/archsurg.1969.01340080075014. [DOI] [PubMed] [Google Scholar]
- 11.Braverman LE, Ingbar SH, Vagenakis AG, Adams L, Maloof F. Enhanced susceptibility to iodide myxoedema in patients with Hashimoto's disease. J Clin Endocrinol Metab. 1971;32:515–21. doi: 10.1210/jcem-32-4-515. [DOI] [PubMed] [Google Scholar]
- 12.Roti E, Montermini M, Robuschi C, Gardini E, Salvo D, Gionet M, et al. Prevalence of hypothyroidism and Hashimoto's thyroiditis in two elderly populations with different dietary iodine intake. In: Pinchera A, Ingbar SH, McKenzie JM, Fenzi GF, editors. Thyroid Autoimmunity. New York: Plenum Press; 1987. p. 555. [Google Scholar]
- 13.Roti E, Minelli R, Gardini E, Bianconi L, Gavaruzzi G, Ugolotti G, et al. Iodine-induced subclinical hypothyroidism in euthyriod subjects with a previous episode of amiodarone-induced thyrotoxicosis. J Clin Endocrinol Metab. 1992;75:1273–7. doi: 10.1210/jcem.75.5.1331165. [DOI] [PubMed] [Google Scholar]
- 14.Koutras DA, Evangelopoulou K, Karaiskos KD, Boukis MA, Pperingos GD, Kitsopanides J, et al. Further data on iodine-induced autoimmunity. In: Pinchera A, Ingbar SH, McKenzie JM, Fenzi GF, editors. Thyroid Autoimmunity. New York: Plenum Press; 1987. p. 563. [Google Scholar]
- 15.Sundick RS, Bagchi N, Brown TR. The role of iodine in thyroid autoimmunity: From chickens to humans-A review. Autoimmunity. 1992;13:61–8. doi: 10.3109/08916939209014636. [DOI] [PubMed] [Google Scholar]
- 16.Sankar R, Sekhri T, Sripathy G, Walia RP, Jain SK. Radioactive iodine therapy in Graves's hyperthyroidism: A prospective study from a tertiary referral centre in north India. J Assoc Physicians India. 2005;53:603–6. [PubMed] [Google Scholar]
- 17.Nordyke RA, Gilbert FI. Optimal Iodine-131dose for eliminating hyperthyroidism in Graves’ disease. J Nucl Med. 1991;32:411–6. [PubMed] [Google Scholar]
- 18.Kendall-Taylor P, Keir MJ, Ross WM. Ablative radioiodine therapy for hyperthyroidism: Long term follow up study. Br Med J. 1984;289:361–3. doi: 10.1136/bmj.289.6441.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alexander EK, Larsen PR. High dose of (131) I therapy for the treatment of hyperthyroidism caused by Graves disease. J Clin Endocrinol Metab. 2002;87:1073–7. doi: 10.1210/jcem.87.3.8333. [DOI] [PubMed] [Google Scholar]
- 20.Guidelines for the use of radioiodine in the management of hyperthyroidism: A summary. Prepared by the radioiodine audit subcommittee of the Royal College of Physicians Committee on diabetes and endocrinology and the research unit of the Royal College of Physicians. J R Coll Physicians Lond. 1995;29:464–9. [PMC free article] [PubMed] [Google Scholar]


