Abstract
Background:
The efficacy and safety of cervical laminoforaminotomy (FOR) in the treatment of cervical radiculopathy has been demonstrated in several series with follow-up less than a decade. However, there is little data analyzing the relative effectiveness of FOR for radiculopathy due to soft disc versus osteophyte disease. In the present study, we review our experience with FOR in a single-center cohort, with long-term follow-up.
Methods:
We examined the charts of patients who underwent 1085 FORs between 1990 and 2009. A cohort of these patients participated in a telephone interview designed to assess improvement in symptoms and function.
Results:
A total of 338 interviews were completed with a mean follow-up of 10 years. Approximately 90% of interviewees reported improved pain, weakness, or function following FOR. Ninety-three percent of patients were able to return to work after FOR. The overall complication rate was 3.3%, and the rate of recurrent radiculopathy requiring surgery was 6.2%. Soft disc subtypes compared to osteophyte disease by operative report were associated with improved symptoms (P < 0.05). The operative report of these pathologic subtypes was associated with the preoperative magnetic resonance imaging (MRI) interpretation (P < 0.001).
Conclusions:
These results suggest that FOR is a highly effective surgical treatment for cervical radiculopathy with a low incidence of complications. Radiculopathy due to soft disc subtypes may be associated with a better prognosis compared to osteophyte disease, although osteophyte disease remains an excellent indication for FOR.
Keywords: Cervical radiculopathy, laminoforaminotomy, posterior cervical foraminotomy, surgical outcomes
INTRODUCTION
Cervical radiculopathy, seen in primary care settings and spine clinics, has an annual incidence of approximately 0.1%.[5,21] Cervical laminoforaminotomy (FOR) is a well-known surgical option to treat cervical radiculopathy and has been associated with short-term clinical success rates of 85-100%. Reported complication rates vary from 0 to 10%.[6,12,13,16,17,18,21,24,26,28,30,31,33] Although the principal surgical alternative, anterior cervical discectomy and fusion (ACDF), is commonly employed to treat radiculopathy, FOR has important advantages. For example, ACDF carries risks of injury to the carotid artery, esophagus, and trachea, and there are risks associated with instrumented fusion, including pseudarthrosis, graft or plate extrusion or fracture, and adjacent level disease. The presence of soft disc rather than osteophyte has been associated with greater success rates for FOR, but this premise needs to be reexamined.[16,19,24]
Between 1990 and 2009, the authors performed 1085 FORs for cervical radiculopathy. Long-term outcomes were assessed in a subset of 319 patients (338 cases) available for interviews who had been followed for an average of 10 postoperative years. Our primary hypothesis was that FOR was nearly equally successful for patients with underlying soft disc protrusions versus osteophytes.
METHODS
Patient population
We reviewed patient records at our hospital using the International Classification of Diseases procedural code for cervical FOR. This study was approved by our institutional review board (IRB), and patients gave their verbal informed consent. Surgeries were performed in 1990-2009 by three senior authors (FS 950, SD 128, and WW 7). Our statistical analysis revealed no significant association between surgeon and principal outcomes. Thus, all patients were analyzed as a single cohort. Our initial search included all patients who underwent FOR for the treatment of pain or weakness caused by C3-C8 radiculopathy. Those with myelopathy, previous cervical fusion at the same level, or spinal neoplasm were excluded. Our search yielded 1085 FOR surgeries performed among 1039 patients. Of these, 319 patients (338 cases) were available for interviews. They had been followed for an average of 10 postoperative years. The surgical approach has been described elsewhere.[10,19,23,25,26]
Chart review
Data including demographic information, comorbidities, presenting symptoms, previous non-surgical treatments, previous and subsequent spine surgeries, diagnostic studies, surgical level and side, operative findings, and complications were collected, entered into a database, and reviewed for our analyses. All patients were seen for routine follow-up approximately 30 days after their surgery, and in our review, the office notes from these follow-up appointments were examined for mention of residual symptoms.
Magnetic resonance imaging (MRI) reports were reviewed given the large majority of images were unavailable. Although the term “soft disc” was not typically used in imaging reports, MRI was frequently able to differentiate between disc and osteophyte etiologies. Operative reports consistently used the term “soft disc,” and thus we chose to categorize patients according to these variables throughout this study.
Telephone interview
Over a 45-day period, all patients who met the inclusion criteria were telephoned. Of those called, 338 cases were included in our primary analysis as patients were available to participate in a 5-min structured interview regarding their symptoms and function since surgery. Patients who had multiple FORs performed were asked the same questions for each surgery. In order to ensure the highest possible response rate, the telephone numbers were checked using multiple sources, and the patients were called on at least two separate occasions. Among those who could be reached, the mean follow-up was 10.0 years (median = 9.9 years, range = 2.5-19.4 years). Patients were queried regarding additional treatments, subjective improvement in symptoms and level of function, and they rated their original and subsequent postoperative pain on a scale of 0-10 [Figure 1].
Figure 1.
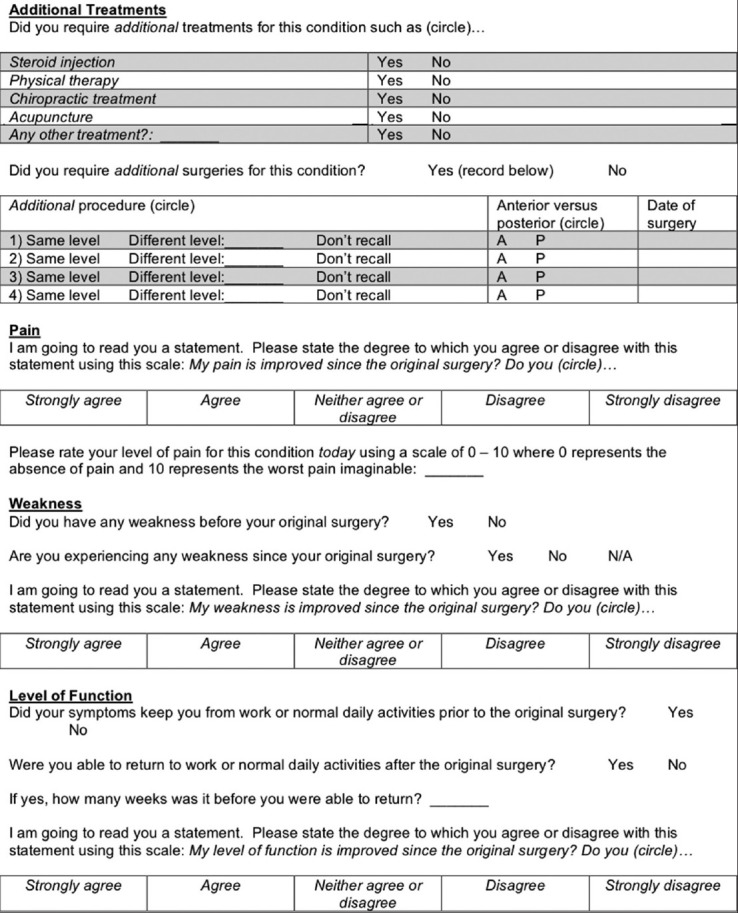
Structured telephone interview
Statistical analysis
Key exposure variables were determined by the chart review and telephone interview. The principal outcome variables included patients’ ratings of pain, weakness, and functional improvement, as well as current ratings of original preoperative pain (0-10) and ability to return to work or normal daily activities. The subset of patients who completed the interview was included in an analysis designed to test for associations between exposure and outcome variables. Chi-square, Fisher's exact test, general linear regression, and logistic regression were used to test for associations between exposure and outcome variables. The data analysis was performed using SAS/STAT software, Version 9.2, of the SAS System for Windows (SAS Institute Inc., Cary, NC, USA). A P < 0.05 was considered statistically significant.
RESULTS
Interview outcomes
We interviewed 319 patients who completed the questionnaire for 338 surgical cases. Thirteen of these patients underwent two FORs and three underwent three FORs. Patients answered the questionnaire items for each surgery. The mean age at interview was 60.1 years (range = 36-92 years), and the mean follow-up was 10.0 years (median = 9.9 years, range = 2.6-19.4 years). The group of interviewees was comparable to non-interviewees for all exposure and outcome variables (P < 0.05), except that the interviewees were older than the non-interviewees (50.2 vs 47.7 years, P < 0.001). There were also small differences in sex (52.4% of interviewees vs 59.2% of non-interviewees were male, P = 0.036), arm pain at presentation (93.4% of interviewees vs 96.5% of non-interviewees, P = 0.022), and year of surgery (49.4% of interviewees vs 63.5% of non-interviewees before the year 2000, P = 0.001).
Ninety-seven (28.7%) cases used postoperative physical therapy for the original condition. Steroid injection was used in 29 (8.6%) instances, chiropractic treatment in 27 (8.0%), and acupuncture in 16 (4.7%). Patients were questioned about additional surgeries during the interview because they may change providers and undergo procedures not captured in our health system records. Among 338 interviews, one additional cervical surgery was performed in 37 (11.0%) instances. Two additional cervical surgeries were performed in eight (2.4%) instances and three additional cervical surgeries in one (0.30%) instance. Of these additional surgeries, 8 were FORs at the same level and side, 23 were FORs at a different level or side, 11 were ACDFs at the same level, 11 were ACDFs at a different level, 1 was a posterior fusion, and in one instance, the patient did not recall whether a subsequent ACDF was performed at the same level as the index FOR. Assuming this unknown case was performed at the same level, the total number of additional cervical surgeries involving the same level and side was 21 of 338 (6.2%), which we interpret as the rate of recurrence requiring additional surgery.
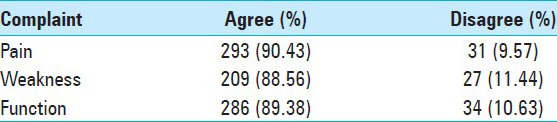
Patient ratings of improvement in symptoms and level of function are presented in Table 1. The mean 0-10 rating of the current pain related to the preoperative condition was 1.57 (SD = 2.28, median = 0, range = 0-9). There were 160 (64.3%) patients who had preoperative subjective weakness and no postoperative weakness, compared with 89 (35.7%) who had preoperative and at least some postoperative weakness. Two hundred and twenty-four (93.0%) patients who were unable to work or perform normal daily activities prior to surgery were able to return postoperatively.
Table 1.
Symptomatic and functional improvement at follow-up
Associations between exposure and outcome variables
Our regression analyses revealed a lack of association between our outcome variables and age (range 30-82 years). However, outcomes were associated with the presence of medical comorbidities. Cases with no medical comorbidities were associated with improvements in pain (χ2, P = 0.002, 93.2% vs 81.1%), subjective weakness (χ2, P = 0.001, 92.3% vs 76.4%), function (χ2, P = 0.027, 91.5% vs 82.4%), and ability to return to work (χ2, P = 0.012, 95.2% vs 85.2%).
Cases with subjective weakness at presentation versus those without subjective weakness experienced more residual weakness, pain, or both at 30-day follow-up (χ2, P = 0.0009, 97.7% vs 83.2%). Of note, 7.8% of patients with subjective weakness at presentation versus 1.0% of patients without subjective weakness at presentation were noted to have weakness at 30-day follow-up. However, this relationship was not significant for weakness on exam at presentation. Duration of symptoms prior to surgery was not associated with outcomes. Both prescription narcotic use and the number of previous cervical spine surgeries were not associated with outcomes. Additionally, the number of root decompressions per operation was not associated with outcomes or the rate of complications.
Preoperative MRI findings and operative findings differentiating soft disc and osteophyte pathologies were significantly associated (χ2, P < 0.001). Operative findings of soft disc protrusions compared with osteophyte disease were associated with significantly higher rates of improved pain postoperatively (χ2, P = 0.002, 95.3% vs 81.0%), reports of lower current pain at the time of telephone interview (general linear regression model, P = 0.022, 1.28 vs 2.10), improved weakness (χ2, P = 0.001, 95.7% vs 76.2%), eliminated weakness (χ2, P = 0.005, 75.8% vs 52.3%), and improved function (χ2, P = 0.009, 95.2% vs 83.6%). Patients with soft discs compared to those with osteophytes at surgery tended to report shorter durations of symptoms prior to surgery (P < 0.001, 20.5 vs 59.9 weeks). However, the associations between pathologic subtype and outcomes remained significant when controlling for duration of symptoms prior to surgery in multivariate regression analysis. Preoperative MRI findings of soft disc only versus osteophyte only were associated with the ability to return to work following surgery (χ2, P = 0.0021, 95.4% vs 75.0%).
The rate of complications was not statistically related to symptomatic and functional outcomes. There were no significant associations between year of surgery (length of follow-up) and the long-term outcomes, including the current rating of pain [Figure 2]. Likewise, all surgeons had similarly high success rates for each outcome measure, and there were no associations between individual surgeon and any of these outcomes.
Figure 2.
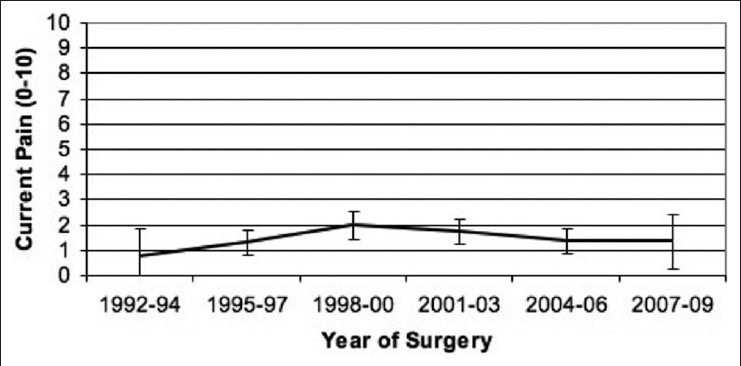
Rating of original preoperative pain at the time of interview by year of surgery. Patients were asked to rate their pain from 0 to 10. Bars represent the 95% confidence interval. There were similarly no associations between year of surgery and other outcome variables
Presentation, complications, and clinical follow-up
Although the focus of our study was the subset of patients who participated in the follow-up telephone interview, we briefly present overall information regarding demographics, presentation, evaluation, and treatment in Tables 2–6. We found no major statistically significant difference between the overall cohort and the interviewed subset, indicating that the interviewed subset is largely representative of the whole. Overall, 57.2% were male and 42.8% were female. Mean age at surgery was 48.5 years (range 19-82 years). The mean duration of symptoms prior to surgery was 39.8 weeks (median = 12 weeks, range = 0.29-1040 weeks).
Table 2.
Presenting symptoms
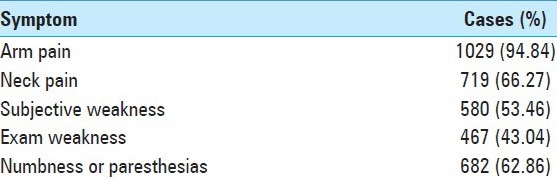
Table 6.
Distribution of surgically treated nerve roots
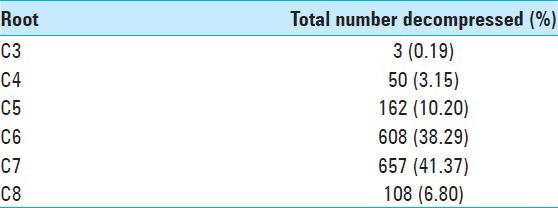
Table 3.
Preoperative non-surgical treatments
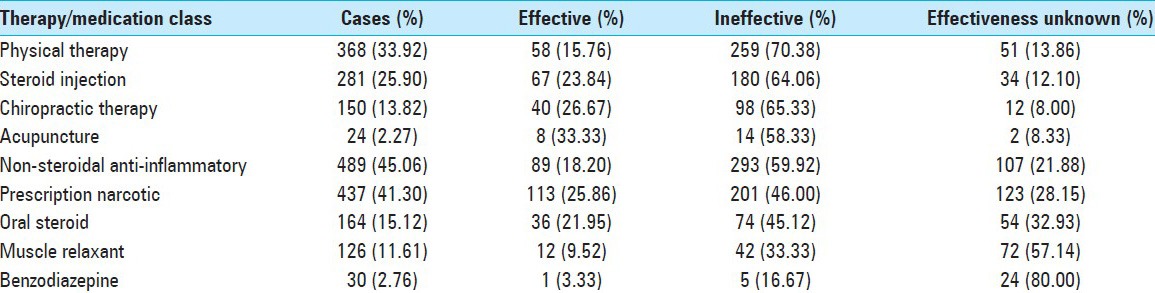
Table 4.
Frequencies of patients who underwent previous and subsequent spine surgeries based on chart review
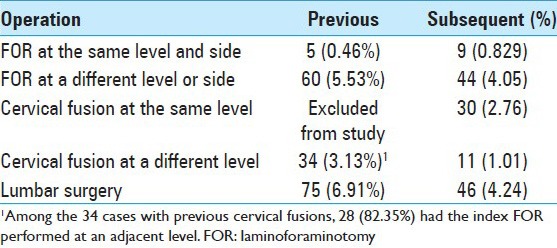
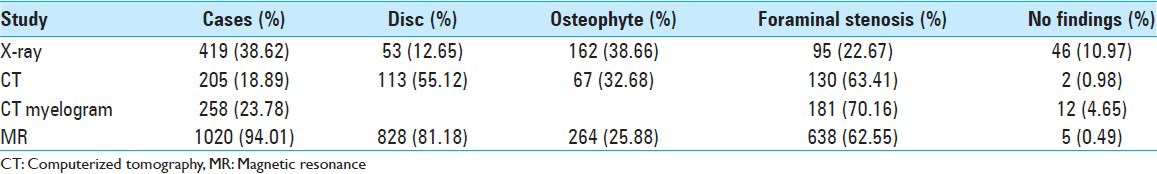
Table 5.
Preoperative diagnostic studies and findings
The overall number of complications was 36 (3.3%). Of these, there were 19 (1.8%) surgical site infections. Fourteen of these cases required reoperation for incision and drainage, while the remaining infections were effectively treated with antibiotics. There were seven (0.7%) dural breaches, five of which resulted in CSF leaks. Three of these leaks required reoperation for repair. Following surgery, six (0.6%) patients developed a new focal sensory disturbance and three (0.3%) developed new focal weakness. One patient suffered a temporal scalp laceration due to misplacement of the Mayfield head holder. No association was found between the occurrence of a complication and patients’ outcomes.
Review of 30-day follow-up notes revealed residual arm pain in 20 of 630 (3.2%) visits, arm weakness in 26 of 630 (4.1%) visits, and both pain and weakness in 3 of 630 (0.5%) visits. In every case, residual symptoms had been present preoperatively. There were no new symptoms reported. In 581 of 630 (92.2%) visits, there was no mention of residual symptoms. Among the 49 of 630 (7.8%) visits with residual pain or weakness at follow-up, some degree of improvement was noted in 29 (59.2%).
DISCUSSION
FOR in the treatment of cervical radiculopathy
This study reports long-term follow-up in a large cohort, shown to be representative of over 1000 cases of FOR for cervical radiculopathy. FOR was successful in relieving symptoms in 90% of patients, which is similar to the rate reported in other studies.[12,13,16,17,30,31] Furthermore, approximately 93% of patients who were unable to work or perform normal daily activities were able to return to these activities following FOR. The overall complication rate in our analysis was just over 3% and is also similar to the rates reported in previous series.[1,6,12,13,16,17,18,24,26,28,30,31,33] The rate of recurrence of symptoms requiring additional surgery in the present study was 6.2% based on our telephone interviews. This rate is slightly higher than that reported by others. However, this difference may, at least in part, be the result of longer mean follow-up in our study.
Pathologic subtype and FOR outcomes
Previous reports have shown a higher incidence of soft disc protrusions (60-80%) associated with cervical radiculopathy compared to osteophytic disease (15%).[17,23] These distributions are roughly concordant with our operative findings of 62.2% soft discs and 32.0% osteophytes. Six percent of our cases were reported to have combined features. The distribution based on MRI was similar, and pathologic subtype findings by operative report correlated with the findings on MRI. Of note, soft disc material as defined intraoperatively compared with osteophytic disease was associated with better results for nearly every outcome measured. Although patients with soft discs tended to report shorter durations of symptoms prior to surgery, duration of symptoms itself did not appear to affect outcomes. Results in the osteophyte group were quite good, as they have been in previous studies.[18] Thus, radiculopathy due to osteophyte disease is still an excellent indication for FOR, and the results are similar to other forms of radiculopathy surgery.[4]
Additional findings
Perhaps not surprisingly, patients without medical comorbidities appeared to have superior outcomes compared to those patients with comorbidities. Preoperative subjective weakness was associated with increased residual weakness and pain at 30-day follow-up compared to no preoperative subjective weakness. This weakness may represent irreparable nerve injury. However, this association was not found for weakness detected on preoperative physical examination, emphasizing the importance of a thorough history as well as physical examination. In addition, the duration of symptoms preoperatively was not directly associated with worse outcomes.
Limitations
Limitations of the present study are those intrinsic to a retrospective design. Most notably, follow-up was largely subjective and our telephone interviews were dependent on patients’ memory of events. Outcomes were based on patients’ recollection and accurate reporting of their current symptoms. Patients’ memory of details of additional surgeries, and our recurrence rate based on interview, is subject to this limitation. Thirty-day follow-up notes were limited, as no standardized outcome measures were administered during these visits. We assessed for responder bias by looking for differences between the group of telephone interviewees and those who were unable to be reached by telephone. Not surprisingly, interviewees’ surgery dates tended to be more recent. Interviewees were slightly older than non-interviewees. Overall, the groups appeared comparable.
FOR and ACDF
Degenerative cervical spine disease requiring surgery is a significant public health issue. Patil et al. reviewed data from the National Inpatient Sample Database utilizing ICD-9 codes, comparing the years 1990 and 2000.[20] The total number of cervical spine operations nearly doubled from 53,810 in 1990 to 112,400 in 2000. Anterior fusion procedures rose from 17.8 to 69.5% of cervical spine operations, while non-fusion decompressions declined from 70.5 to 24.6%. The inflation-adjusted hospital charges for these procedures rose by 48% to a total exceeding $2 billion in 2000. The cost of these operations should not only be measured in terms of healthcare expenditure, but also in terms of effectiveness to achieve full function postoperatively because, at least in the case of cervical radiculopathy, patients are expected to return to work promptly.
We did not include our experience with ACDF for cervical radiculopathy. Comparisons of outcomes between FOR and ACDF in the treatment of cervical radiculopathy are currently limited.[27,29] Furthermore, it is not uncommon for studies to define outcomes differently, making direct comparisons challenging. To assess the relative effectiveness of FOR versus ACDF in a controlled population with similar vocational requirements, Tumialán et al. studied 38 military personnel matched for age, treatment level, and surgeon.[27] Nineteen of these patients underwent FOR and the other nineteen underwent ACDF. Surgical results were comparable, as were operating room time, blood loss, and postoperative narcotic refills. The only complications were two cases of transient recurrent laryngeal nerve palsy in the ACDF group. Significantly, the average time to return to unrestricted full duty was 4.8 weeks (range 1-8 weeks) in the FOR group and 19.6 weeks (range 12-32 weeks) in the ACDF group, a difference of 14.8 weeks. Direct surgical costs were $3570 in the FOR group and $10,078 in the ACDF group. The difference in indirect costs based on time to return to active duty was greater in the ACDF group by $20,094–$30,553. Of note, the virtually universal use of instrumentation devices likely increases the direct costs of ACDF.
Another significant advantage of FOR is avoidance of fusion and potential adjacent segment degeneration, which may require additional surgery.[2,3,11,14,15,32] Although there is controversy over the exact incidence of adjacent disc degeneration, its existence is hardly in doubt. The proliferation of anterior arthroplasty devices, whose function is predominantly to prevent the expected adjacent disc degeneration by allowing motion at the operated segment, underscores our awareness of delayed adjacent complications. The more immediate complication of pseudarthrosis has been mitigated but not eliminated by the virtually universal use of anterior instrumentation devices, but as yet there is no treatment that successfully addresses adjacent disc degeneration, which seems to occur in a significant percentage of patients. Ishihara et al. followed 112 patients with anterior cervical interbody fusion for more than 2 years.[15] Nineteen percent developed symptomatic adjacent segment disease. Goffin et al. studied 181 patients treated with ACDF with an average follow-up of more than 8 years.[11] They developed anterior segment disc degeneration at a far greater rate than would be expected with normal aging, and 43% demonstrated radiographically moderate to severe changes. Hilibrand et al. showed that symptomatic adjacent segment disease, as defined by the presence of new radiculopathy or myelopathy referable to motion at an adjacent segment, may affect more than one-fourth of all patients within 10 years following cervical arthrodesis.[14] The study demonstrated an annual incidence of symptomatic disease of approximately 2.9% following the index procedure. In view of the fact that two roots were decompressed in one-third of cases in the present study, FOR offers freedom to explore and treat multiple roots without multiple fusions.
Despite the high success rate of FOR and the durability of this success for nearly 20 years in this study complemented by low complication rates, ACDF may be more effective than FOR in certain cases. For example, myelopathy or bilateral decompressions at the same level require the anterior approach. Concerns with FOR include same-level degeneration due to facet joint resection and persistent neck pain due to muscle stripping.[7] However, a recent radiographic follow-up study demonstrated a negligible rate of postoperative instability at an average 77 months follow-up among patients undergoing FOR.[16] Moreover, we did not observe persistent neck pain in our study, and minimally invasive FOR may reduce postoperative muscle pain.[22]
The anterior approach carries with it unique and potentially serious complications such as dysphagia or even esophageal injury and recurrent laryngeal nerve palsy.[8,9] Fountas et al. studied the complications from ACDF in 1015 patients and reported an overall morbidity of 19.3%.[9] Isolated postoperative dysphagia was seen in 9.5%, hematoma in 5.6% (2.4% required surgical intervention), symptomatic recurrent laryngeal nerve palsy in 3.1%, dural penetration in 0.5%, and esophageal perforation in 0.3%. The complications in our series were generally transient. In summary, multiple studies demonstrate the advantages of an operation for cervical radiculopathy that can produce equal results in terms of relief of arm pain yet avoid fusion. FOR offers moderately fewer immediate complications, significantly fewer long-term complications, a major reduction in direct costs (particularly if one uses anterior interbody arthroplasty devices), and a benefit to the patient and society due to earlier return to work.
ACKNOWLEDGMENTS
The authors wish to thank Dr. Lynne Taylor, PhD from the Department of Biostatistics and Epidemiology at the University of Pennsylvania for her assistance with the statistical analyses.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/16/536/148029
Contributor Information
Ephraim W. Church, Email: echurch@hmc.psu.edu.
Casey H. Halpern, Email: casey.halpern@uphs.upenn.edu.
Ryan W. Faught, Email: ryan.faught@uphs.upenn.edu.
Usha Balmuri, Email: usha.balmuri@uphs.upenn.edu.
Mark A. Attiah, Email: mark.attiah@uphs.upenn.edu.
Sharon Hayden, Email: sharon.hayden@uphs.upenn.edu.
Marie Kerr, Email: marie.kerr@uphs.upenn.edu.
Eileen Maloney-Wilensky, Email: eileen.maloney@uphs.upenn.edu.
Janice Bynum, Email: janice.bynum@uphs.upenn.edu.
Stephen J. Dante, Email: stephen.dante@uphs.upenn.edu.
William C. Welch, Email: william.welch@uphs.upenn.edu.
Frederick A. Simeone, Email: frederick.simeone@uphs.upenn.edu.
REFERENCES
- 1.Aldrich F. Posterolateral microdisectomy for cervical monoradiculopathy caused by posterolateral soft cervical disc sequestration. J Neurosurg. 1990;2:370–7. doi: 10.3171/jns.1990.72.3.0370. [DOI] [PubMed] [Google Scholar]
- 2.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993;18:2167–73. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Bartolomei JC, Theodore N, Sonntag VK. Adjacent level degeneration after anterior cervical fusion: A clinical review. Neurosurg Clin N Am. 2005;16:575–87. doi: 10.1016/j.nec.2005.07.004. v. [DOI] [PubMed] [Google Scholar]
- 4.Brigham CD, Tsahakis PJ. Anterior cervical foraminotomy and fusion. Surgical technique and results. Spine. 1995;20:766–70. [PubMed] [Google Scholar]
- 5.Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353:392–9. doi: 10.1056/NEJMcp043887. [DOI] [PubMed] [Google Scholar]
- 6.Davis RA. A long-term outcome study of 170 surgically treated patients with compressive cervical radiculopathy. Surg Neurol. 1996;46:523–30. doi: 10.1016/s0090-3019(96)00278-9. [DOI] [PubMed] [Google Scholar]
- 7.Fehlings MG, Gray RJ. Posterior cervical foraminotomy for the treatment of cervical radiculopathy. J Neurosurg Spine. 2009;10:343–4. doi: 10.3171/2009.1.SPINE08899. [DOI] [PubMed] [Google Scholar]
- 8.Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine. 1982;7:536–9. doi: 10.1097/00007632-198211000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32:2310–7. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 10.Frykholm R. Deformities of dural pouches and strictures of dural sheaths in the cervical region producing nerve-root compression; A contribution to the etiology and operative treatment of brachial neuralgia. J Neurosurg. 1947;4:403–13. doi: 10.3171/jns.1947.4.5.0403. [DOI] [PubMed] [Google Scholar]
- 11.Goffin J, van Loon J, Van Calenbergh F, Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995;8:500–8. [PubMed] [Google Scholar]
- 12.Grieve JP, Kitchen ND, Moore AJ, Marsh HT. Results of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathy. Br J Neurosurg. 2000;14:40–3. doi: 10.1080/02688690042898. [DOI] [PubMed] [Google Scholar]
- 13.Henderson CM, Hennessy RG, Shuey HM, Jr, Shackelford EG. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: A review of 846 consecutively operated cases. Neurosurgery. 1983;13:504–12. doi: 10.1227/00006123-198311000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–28. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4:624–8. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 16.Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: A single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 2009;10:347–56. doi: 10.3171/2008.12.SPINE08576. [DOI] [PubMed] [Google Scholar]
- 17.Krupp W, Schattke H, Müke R. Clinical results of the foraminotomy as described by Frykholm for the treatment of lateral cervical disc herniation. Acta Neurochir (Wien) 1990;107:22–9. doi: 10.1007/BF01402608. [DOI] [PubMed] [Google Scholar]
- 18.Kumar GR, Maurice-Williams RS, Bradford R. Cervical foraminotomy: An effective treatment for cervical spondylotic radiculopathy. Br J Neurosurg. 1998;12:563–8. doi: 10.1080/02688699844448. [DOI] [PubMed] [Google Scholar]
- 19.Murphey F, Simmons JC, Brunson B. Surgical treatment of laterally ruptured cervical disc. Review of 648 cases, 1939 to 1972. J Neurosurg. 1973;38:679–83. doi: 10.3171/jns.1973.38.6.0679. [DOI] [PubMed] [Google Scholar]
- 20.Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005;57:753–8. [PubMed] [Google Scholar]
- 21.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117:325–35. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 22.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: A prospective, randomized, controlled study. Spine. 2008;33:940–8. doi: 10.1097/BRS.0b013e31816c8b67. [DOI] [PubMed] [Google Scholar]
- 23.Scoville WB. Types of cervical disk lesions and their surgical approaches. JAMA. 1966;196:479–81. [PubMed] [Google Scholar]
- 24.Scoville WB, Dohrmann GJ, Corkill G. Late results of cervical disc surgery. J Neurosurg. 1976;45:203–10. doi: 10.3171/jns.1976.45.2.0203. [DOI] [PubMed] [Google Scholar]
- 25.Scoville WB, Whitcomb BB. Lateral rupture of cervical intervertebral disks. Postgrad Med. 1966;39:174–80. doi: 10.1080/00325481.1966.11696921. [DOI] [PubMed] [Google Scholar]
- 26.Silveri CP, Simpson JM, Simeone FA, Balderston RA. Cervical disk disease and the keyhole foraminotomy: Proven efficacy at extended long-term follow up. Orthopedics. 1997;20:687–92. doi: 10.3928/0147-7447-19970801-07. [DOI] [PubMed] [Google Scholar]
- 27.Tumialán LM, Ponton RP, Gluf WM. Management of unilateral cervical radiculopathy in the military: The cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusion. Neurosurg Focus. 2010;28:E17. doi: 10.3171/2010.1.FOCUS09305. [DOI] [PubMed] [Google Scholar]
- 28.Williams RW. Microcervical foraminotomy. A surgical alternative for intractable radicular pain. Spine. 1983;8:708–16. doi: 10.1097/00007632-198310000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Wirth FP, Dowd GC, Sanders HF, Wirth C. Cervical discectomy. A prospective analysis of three operative techniques. Surg Neurol. 2000;53:340–6. doi: 10.1016/s0090-3019(00)00201-9. [DOI] [PubMed] [Google Scholar]
- 30.Woertgen C, Holzschuh M, Rothoerl RD, Haeusler E, Brawanski A. Prognostic factors of posterior cervical disc surgery: A prospective, consecutive study of 54 patients. Neurosurgery. 1997;40:724–8. doi: 10.1097/00006123-199704000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Woertgen C, Rothoerl RD, Henkel J, Brawanski A. Long term outcome after cervical foraminotomy. J Clin Neurosci. 2000;7:312–5. doi: 10.1054/jocn.1999.0669. [DOI] [PubMed] [Google Scholar]
- 32.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: A 5- to 11-year radiologic and clinical follow-up study. Spine. 2005;30:2138–44. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 33.Zeidman SM, Ducker TB. Posterior cervical laminoforaminotomy for radiculopathy: Review of 172 cases. Neurosurgery. 1993;33:356–62. [PubMed] [Google Scholar]


