Abstract
Background:
Intraoperative frozen section (FS) diagnostics is an important diagnostic tool in neurosurgery, but agreement with final histopathology diagnoses may vary. In the present study we assess the diagnostic properties of intraoperative FSs in suspected intracranial tumors.
Methods:
Retrospective single-center review of consecutive patients with suspected intracranial brain tumors from January 2008 to December 2012. We included all cases were both an intraoperative FS and a formalin-fixed paraffin-embedded (FFPE) section had been acquired. Agreement with final diagnosis, sensitivity, specificity, and predictive values were explored. Time between date of surgery and first final diagnosis based on FFPE section, whether the patients had undergone previous brain surgery and/or prior cerebral radiotherapy were also registered.
Results:
Agreement between FS diagnoses and final FFPE section diagnoses was seen in 504/558 (90.3%), while there was lack of agreement in 54/558 (9.7%). In 20 cases, agreement was not classifiable. Agreement was lower in low-grade gliomas (82.5%) than in high-grade gliomas (93.2%). Agreement between FS and FFPE was significantly higher in primary operations (92.1%) than in re-do operations (81.5%) (P = 0.001). Sensitivity of FS ranged from 30.8% in lymphomas to 94.6% in meningiomas.
Conclusions:
Intraoperative FS diagnoses demonstrate high diagnostic accuracy. However, agreement varies among histopathological entities and is lower in low-grade tumors than in high-grade tumors. Sensitivity for diagnosing CNS lymphomas is low. A variable degree of reservation is always necessary when interpreting and communicating FS diagnoses.
Keywords: Brain tumor, frozen section, histology, sensitivity, specificity
INTRODUCTION
Today's neurosurgeons usually have a good idea about the probable nature of the lesions they are to operate. Magnetic resonance imaging (MRI) may display anatomical involvement, speed and patterns of growth, effect on the blood–brain-barrier (i.e., contrast enhancement), edema, necrosis, and to some extent the density and vascularity of the lesions. Special image sequences such as diffusion-weighted imaging (DWI), and magnetic resonance spectroscopy (MRS) can also be helpful in the differential diagnostics.[2,14,18] A study from 2006 compared MRI classification of brain tumors with final histopathological diagnoses in 393 patients. The reported specificity for MRI diagnoses was higher (85.2–100%) than sensitivity. Sensitivity was still high in the recognition of broad diagnostic categories (i.e. neuroepithelial vs meningiothelial tumors).[12] Another study compared computed tomography (CT), MR and angiography with final diagnoses and found high specificity (95–100%) but a lower sensitivity of diagnoses based on neuroimaging.[8] Intraoperative frozen section (FS) of suspected intracranial tumors still remains an important diagnostic tool for the neurosurgeon to confirm that the targeted lesion is tumor tissue and to decide on the most appropriate surgical strategy. Also, while awaiting the final histopathological diagnosis, the FS diagnosis may be important both for informing patients and planning follow-up or adjuvant therapy. Thus, knowledge about the diagnostic properties of FSs is useful for clinicians. Previous studies have reported a diagnostic accuracy in brain tumors to be greater than 85%.[3,19,21,23,28] However, there are few large studies, and to our knowledge no studies have compared intraoperative diagnosis based on FS with final diagnosis based on formalin-fixed paraffin-embedded (FFPE) section after the new World Health Organization (WHO) classification of tumors of the central nervous system (CNS) from 2007. Earlier studies also do not present sensitivities, specificities, and predictive values. In the present study, we aimed to assess the diagnostic properties of intraoperative FSs in suspected intracranial tumors.
MATERIALS AND METHODS
Patient selection, laboratory routines, and study variables
The patients were included from St. Olavs University Hospital, Trondheim, Norway. We retrospectively reviewed surgical records for consecutive patients operated (diagnostic biopsy or tumor resection) for suspected brain tumor in the period from January 2008 through December 2012. We included all operations were both an FS and a FFPE section had been acquired (n=578). We only assessed the FS diagnoses given intraoperatively; later reviews of FS samples were therefore ignored. For the final histopathological diagnosis, we identified the first final diagnosis. Later histopathological reviews as a part of other studies or quality control were overlooked since these did not form basis for clinical decision making at the time. For diagnostic biopsies navigated biopsy forceps provides were used to obtain tissue samples of approximately 1 mm in diameter. Typically 4–5 biopsies were sent for FFPE diagnostics and 1–2 samples were taken for FS. Larger forceps were used for tissue samples during open resections. Targeted image-guided bipopsies were guided only by conventional MRI sequences and three dimensional (3D) ultrasound, and metabolic hot spots were generally not assessed. All FFPE diagnoses and most FS diagnoses were made by an experienced neuropathologist (SHT), and in accordance to the current WHO classification system.[13] In more difficult cases, including most low-grade gliomas, or cases where other pathologists were uncertain, the experienced neuropathologist is usually involved in the FS diagnostics. No preliminary answers based on hematoxylin and eosin (H and E) alone are given out, and final FFPE diagnoses are always supported by immunohistochemistry staining. Tumor genetics were not routinely assessed in the study period (e.g. 1p19q deletion status). Confirmatory second opinions from experienced colleagues at other university hospitals are frequently sought. Patient age, time between date of surgery and first final diagnosis based on FFPE section and whether patients had undergone previous brain surgery and/or cerebral radiotherapy were also registered.
Overall agreement
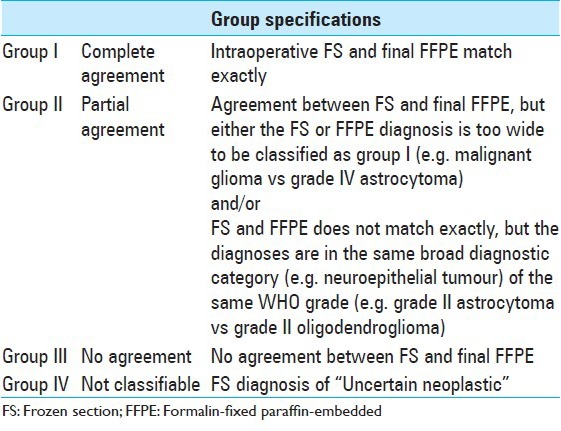
Agreement between FS diagnoses and FFPE section diagnoses was classified into four categories, as presented in Table 1. We further dichotomized results into “agreement” (groups I and II) or “no agreement” (group III). Lesions that were not classifiable in FSs (group IV) were excluded from agreement calculations.
Table 1.
Definitions of agreement between frozen section diagnosis and final histopathological diagnosis
Statistics
The statistical analyses were made using the IBM SPSS statistics program version 20. Statistical significance was defined as P <0.05. The Pearson's Chi-square test was used for determination of statistical significance in contingency tables. All tests are two-sided. Central tendencies are presented as medians with range if skewed. Sensitivity, specificity, positive predictive values, and negative predictive values were calculated using 2×2 tables, as shown in Table 2. Final histopathology FFPE diagnoses that formed basis for clinical decision making and adjuvant treatments at the time were considered the golden standard. Binary multivariate logistic regression was used to adjust for possible predictors of nonagreement.
Table 2.
Sensitivity=A/(A;C). Specificity=D/(D;B). Positive predictive value=A/(A;B). Negative predictive value=D/(D;C)

Ethical statement
The study was approved by the medical faculty of the Norwegian University of Science and Technology as a student project. The regional ethics committee signed a waiver for formal ethical review. The Data Protection Official for Research at St. Olavs University Hospital approved the study.
RESULTS
Median age of included patients was 57 years (range 2 months to 91 years); 25 (4.3%) were children (<16 years) and 153 (26.4%) were elderly (>65years). A total of 478 (82.7%) of FSs were from primary operations. A total of 63 (10.9%) of FS were from patients who had undergone cerebral radiotherapy.
Median time between date of surgery and date of final diagnosis based on FFPE sections was 9 days (range 2–54 days).
Agreement
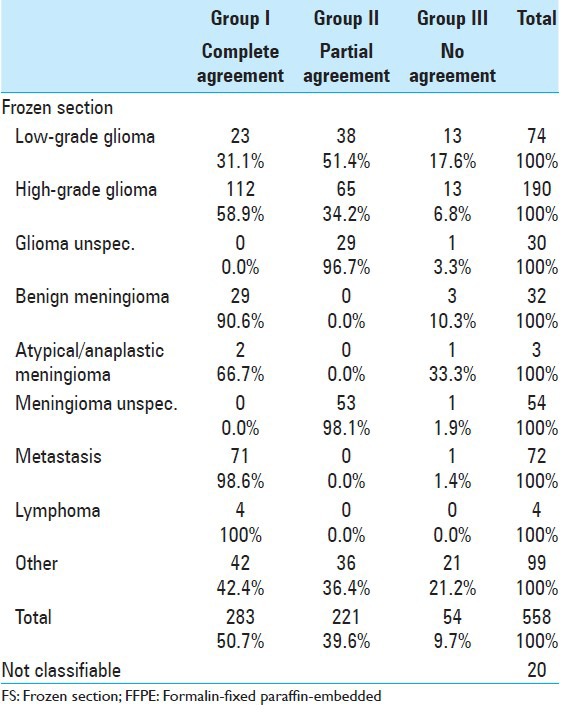
As seen from Table 3, FS and FFPE matched exact in 50.7% of cases. Partial agreement was seen in 39.6%. Thus, overall agreement was 90.3%. No agreement was seen in 54 cases (9.7%). Agreement ranged from 66.7% in atypical/anaplastic meningiomas to 100% in lymphomas.
Table 3.
Agreement between FS and FFPE diagnoses in tumour categories
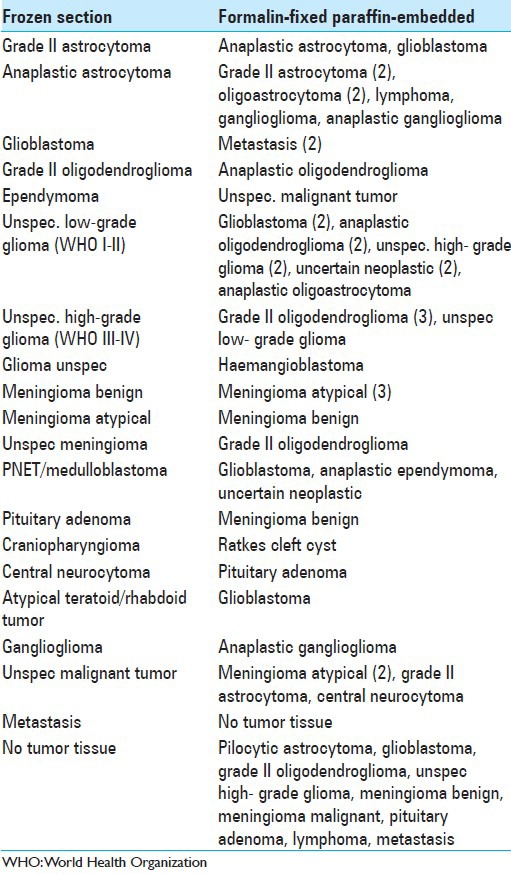
FS and final FFPE sections from the 54 cases with discrepant diagnoses are presented in Table 4. A total of 18 (33.3%) of these discrepancies were in WHO grading of gliomas. Wrong WHO grading of meningiomas was seen in four cases, while in nine cases the FS diagnose was “no tumor tissue,” but later FFPE section confirmed a tumor diagnose.
Table 4.
Discrepant diagnoses
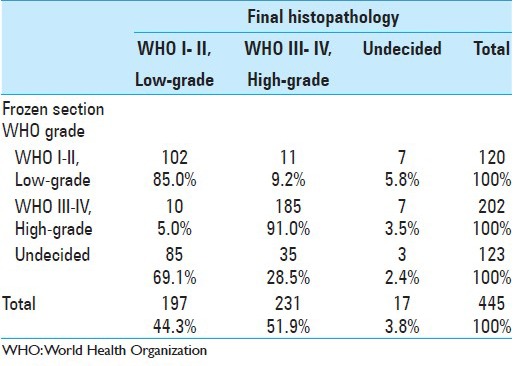
As seen in Table 5, agreement between FS and final diagnosis in low-grade (WHO I-II) lesions was 85.0%. In 9.2% of cases with WHO low-grade FS diagnoses the final diagnose was a WHO high-grade tumor. When the FS diagnosis was WHO high-grade (III- IV), this was confirmed as the final diagnose in 91.0%. In 5.0% the high-grade FS diagnoses were later downgraded to WHO low-grade lesions as the final diagnosis.
Table 5.
Frozen section WHO grade compared to final WHO grade
Tissue samples were from diagnostic biopsies alone in 70/578 (12.1%). There was an overall agreement between FS results and the final histopathology reports in 448/501 (88.2%) of resection cases as compared with 53/70 (75.7%) in cases undergoing biopsies only, a significant difference (P =0.004). However, these two groups are not necessarily comparable since biopsy alone, for example, was an uncommon strategy in meningiomas and far more common in lymphomas. In glioma patients there was agreement between FSs and the final histopathology reports in 233/262 (89.3%) after surgical resections as compared with 29/32 (90.6%) in biopsy cases (P =0.814).
The experienced neuropathologist (SHT) read 280/578 (48%) of all FSs. Overall agreement was 83.6% when FS were read by the experienced neuropathologist, and 89.9% when FS were read by other pathologists. However, gliomas were less common in the samples read by the other pathologists (46%) as compared with the samples read by the experienced neuropathologist (63%). It is nevertheless likely that experience helps. For example, for low grade gliomas, complete agreement with FFPE was seen in 18 (29.5%) of 61 patients where the experienced neuropathologist read FS. For comparison, complete agreement with FFPE was seen in only 4 (14.8%) of 27 low-grade glioma patients where other pathologists read FS. However, since the neuropathologist is usually involved in the more difficult cases, such subgroup analyses are not necessary valid.
Gliomas
As seen in Table 6, when the intraoperative FS diagnosis was low-grade glioma this was later confirmed as the final diagnosis in 58/74 (78.4%). 10/74 (13.5%) of the low-grade glioma FS diagnoses were later upgraded to WHO high-grade gliomas. In 3/74 (4.1%) with a low-grade glioma FS diagnosis a definite malignancy grade was undecided for the final diagnosis (i.e. unspecified gliomas). Sensitivity for detecting low-grade gliomas from FS was 64.4% while specificity was 96.7%. Positive predictive value was 78.4% while negative predictive value was 93.7%.
Table 6.
Diagnostic properties of glioma as frozen section diagnosis
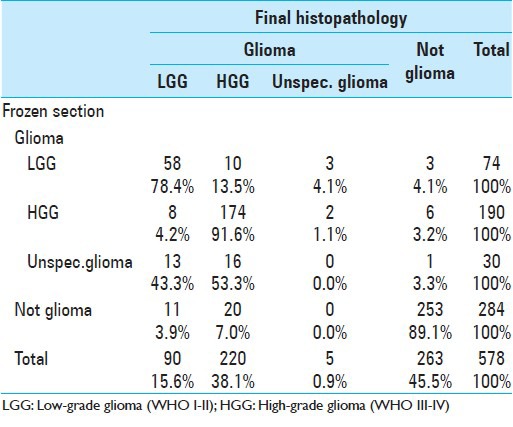
When the intraoperative FS diagnosis was a high-grade glioma, this was later confirmed as the final diagnosis in 174/190 (91.6%). In 8/190 (4.2%) cases, the final diagnoses were downgraded from high- to low-grade gliomas. Sensitivity for detecting high-grade gliomas with FS was 79.1% while specificity was 95.5%. The positive predictive value was 91.6% while the negative predictive value was 88.1%.
No WHO grade was given of in 30 FS glioma diagnoses (i.e. unspecified glioma). In 13/30 (43.3%) of these, the final WHO grade was a low-grade glioma, and in 16/30 (53.3%) the final diagnosis was a high-grade glioma.
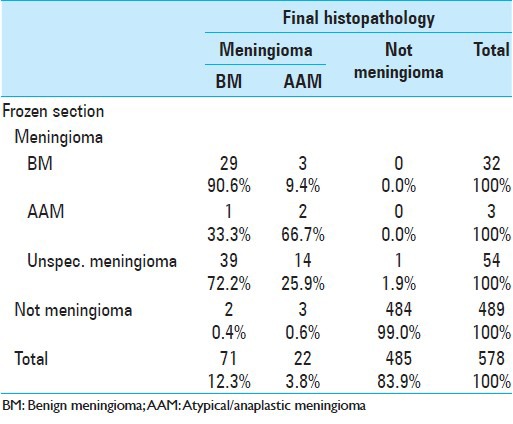
Meningiomas
In 89 cases, the FS section diagnosis was meningioma. As may be summed from Table 7, this was confirmed as the final diagnosis in 88 cases. The sensitivity for detecting meningioma from FS was 94.6%, while specificity was 99.8%. The positive predictive value was 98.9% while negative predictive value was 99.0%. In 32 FSs, the diagnosis was WHO grade I meningioma. This was confirmed as the final diagnoses in 29/32 (90.6%). In 3/32 (9.4%) the final diagnoses were upgraded to atypical or malignant meningiomas. Only three FSs diagnoses were atypical or malignant meningioma. Two were confirmed with the final FFPE diagnosis, and one was downgraded to a benign meningioma.
Table 7.
Diagnostic properties of meningioma as frozen section diagnosis
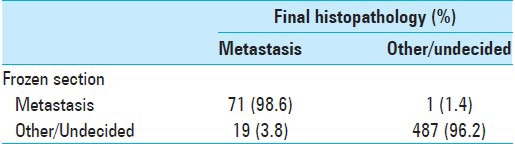
Metastasis
In 72 operations, the FS diagnosis was metastasis. This was confirmed as the final diagnosis in 71(98.6%). As may be calculated from Table 8, the sensitivity and specificity for metastasis as a FS diagnosis was 78.9% and 99.7%, respectively. The positive predictive value of FS with metastasis was 98.6% while the negative predictive value was 96.2%.
Table 8.
Metastasis
Lymphomas
In only four patients the FS diagnosis was lymphoma. As can be calculated from Table 9, the sensitivity for detecting lymphomas with FSs was 30.8% while the specificity was 100%. The positive predictive value was 100% and the negative predictive value was 98.4%.
Table 9.
Lymphoma

Primary surgery or previous radiotherapy
Agreement between FS and FFPE was significantly higher in primary operations (92.2%) than in re-do operations (81.4%) (P =0.001). In 42/75 (56.0%) of reoperations the patients had previously undergone radiotherapy. There was a trend toward poorer agreement between FS and final histopathology if patients had undergone radiotherapy (83.6% vs. 91.1%), P =0.06. However, in multiple logistic regression analyses with prior surgery and prior radiotherapy as variables, only prior brain surgery (P =0.007) was significantly associated with poorer agreement between FS and final histopathology. For the 36 high- and low-grade gliomas that had previously undergone surgery and radiotherapy overall sensitivity of FS for was 75%.
DISCUSSION
In consecutive FS samples from suspected intracranial tumors we found 90.3% overall agreement with the final FFPE section diagnosis. Agreement varied between histopathological entities and was lower in low-grade tumors than in high-grade tumors. Agreement was significantly higher in primary operations than in re-do operations. Sensitivity and specificity varies among entities, but does not reach 100%, even for meningiomas. A variable degree of reservation is therefore always necessary when interpreting and communicating FS diagnoses.
The present study is the first study in this topic after the new WHO classification system from 2007. The newest version of the WHO classification includes several changes, including grading changes for anaplastic oligoastrocytoma, meningioma, choroid plexus tumors, pineal parenchymal tumors, ganglioglioma, cerebellar liponeurocytoma, and hemangiopericytoma. Results from our study are nevertheless much in line with previous reports. Plesec and Prayson included 2156 cases with a CNS tumor diagnosis and reported less than 3% discrepancy between FS diagnoses and final histopathology.[19] Regragui et al. studied diagnostic accuracy of FS in 1315 CNS tumor cases, and report agreement with final diagnoses in 87.6% of cases.[21] Some smaller studies report agreement between FS and final histopathological diagnoses between 88% and 99%.[3,15,23,26,28] There may be several explanations behind the range of agreement reported from such studies. First, most assess agreement, but definitions of agreement often differ. We attempted to analyze our data pragmatically to reflect how we use FSs clinically. We defined “partial agreement” as when FS diagnoses were too wide to be classified as complete agreement (e.g. malignant glioma vs grade IV astrocytoma) and when diagnoses were in the same broad diagnostic category (e.g. neuroepithelial tumor) of the same WHO grade (e.g. grade II astrocytoma vs grade II oligodendroglioma). Still, the present and other definitions of agreement can be discussed. Further, due to the known interobserver variability in histopathological diagnoses for various CNS tumors,[1,17,20,29] agreement is presumably higher if FS and final diagnoses are given by the same pathologist. In the present study most, but not all diagnoses, were given by the same experienced neuropathologist. It is important to remember that results can be influenced by inter- and intraobserver variability, but these factors have not been controlled for by our study design. Also, many brain tumors, especially neuroepithelial tumors, are often heterogeneous. Since tissue samples for FS may be taken from a different region than tissue for FFPE sections, the lack of agreement observed may not only reflect the diagnostic limitation of FSs, but also the possible local variation within a single lesion. Some hospitals use smears and imprints in addition to or in place of FS. FS is still the gold standard in intraoperative lesion diagnostics.[25] One advantage of FS is the ability to preserve tissue architecture[19] and appear more similar to FFPE sections than cytological preparations.[5] However, as demonstrated, FSs are not always accurate, and such preliminary diagnoses should be held up against image findings and intraoperative findings until the final histopathological diagnosis is settled. A strength of the present study is the consecutive and fairly large patient sample. To enhance perception of the diagnostic properties of FS, we also report sensitivity, specificity, and predictive values, in addition to agreement. However, of note, predictive values will depend on the prevalence of disease. Thus, local routines for obtaining FSs will affect predictive values. One should also keep in mind that this study is performed in a single university hospital and FS routines and study results may not necessarily be representative for other centers. Another limitation is that we did not include neuroimaging findings, clinical, diagnostic or prognostic biomarkers in the present study. The tissue sampling techniques and sample volumes may depend on lesion volumes, tumor location and can differ between biopsies or resection procedures, possibly affecting the observed diagnostic accuracies of FS.
Discrepancies between FS and FFPE diagnoses seldom have direct consequences for the treatment of the patient. However, there can be exceptions. Surgical strategies, that is, aggressiveness can be different depending on the type of lesion. For example, in meningiomas, aggressive removal of underlying bone and associated dura may perhaps be less important benign lesions,[27] but this may be warranted in atypical lesions.[9] Although, there was usually agreement between FS and final diagnosis in WHO grading, the WHO low-grade FS diagnosis was later upgraded to a WHO high-grade final diagnosis in 1 in 10 cases. In some neuroepithelial tumors, the cost–benefit ratio of the most aggressive of the surgical strategies may depend on histopathology. Acquired neurological deficits due to aggressive resections in low-grade glioma may perhaps be more acceptable than in high-grade lesions since there are clear survival benefits of resection[10] and since early postoperative deficits often will improve much with rehabilitation and time.[4] However, new deficits are associated with reduced short-term quality of life[11] and in high-grade gliomas acquired deficits are associated with reduced survival.[6,16] Depending on laboratory resources and diagnostic routines, such as for awaiting immunohistochemistry staining or second opinions before diagnoses are given out, the time between the FS and FFPE diagnose may vary. In our center, the final diagnose is settled after median 9 days. Since most patients may be discharged before final histopathology diagnoses are ready, many patients will unfortunately leave the hospital with some uncertainly regarding the further follow-up, treatment and nature of their disease.
As seen, the positive predictive value of FS is high in high-grade gliomas (91.6%). FS is not optimal when there is much edema because of freezing artefacts. As a consequence of artefacts, FS do not always show the histological characteristic needed to sub-classify high-grade gliomas. It may, for example, be particularly difficult to distinguish between oligodendroglioma and astrocytoma from FS.[7] However, such minor sub-classification discrepancies do not have clinical implications in the waiting period for the final diagnosis. For low-grade gliomas, the positive predictive value was lower (78.4%) and several low-grade glioma FS diagnoses were later upgraded to high-grade gliomas. This may reflect the fact that a high proportion of the gliomas are heterogeneous, and the tissue samples sent to FS might not always represent the most aggressive part of the tumor.[19]
FS is good for distinguishing meningioma from other entities. If we also consider the fact that meningiomas often are diagnosed with quite good trustworthiness from neuroimaging,[24] the meningioma diagnosis is most often quite certain during surgery. Our results also show quite good accuracy in the cases where the meningiomas were given WHO grades from FS. However, the majority of the meningiomas were classified as “unspecified meningioma” on FS, even though the pathologists strive to provide a WHO grade.
In metastases the positive predictive value of FS is high and neurosurgeons can be quite sure that the final diagnosis will agree with the intraoperative diagnosis. In later confirmed metastases that were not diagnosed with FS, about 80% was classified as “unspecified malignant tumor” on FS. In many cases, a primary tumor outside the CNS is known and neuroimaging characteristics can also indicate metastases. Thus, “unspecific malignant tumor” as the FS diagnosis presumably seldom causes much confusion.
For CNS lymphomas, fast diagnostics is important as early chemotherapy is warranted and surgical resection will likely increase morbidity.[22] The positive predictive value for lymphoma was 100%, but in 9/13 cases of lymphoma, the FS did not give the right diagnosis, thus sensitivity of FS is low. This may lead to wrong surgical treatment (i.e. resection instead of biopsy) or treatment delays. Lymphomas may be imitators in both neuroradiology and histopathology. It is well known that glioblastomas and metastatic carcinomas histologically can mimic lymphomas. It is important that pathologists and clinicians communicate well when the FS diagnose does not fit with the clinical or radiological picture. Close communication between neurosurgeons, neuropathologists, and neuroradiologists may be the key to avoid potential pitfalls in lymphoma diagnostics.
We found lower diagnostic accuracy of FS if patients had undergone previous brain surgery. There are more diagnostic pitfalls for both radiologists and neuropathologists (pseudoprogression, radiation gliosis/necrosis, enhancement due to small peritumoral infarctions following first surgery or radiation, etc.) in reoperations. Also, re-do operations are common in cases with suspected malignant transformation. Such lesions may be particularly associated with sampling error as they contain both low- and high-grade tissue. Even if FS diagnoses may be less accurate in re-do operations, these patients already have a diagnosis from their last operation and a wrong FS diagnosis will perhaps usually not have clinical consequences for the treatment given. Still, for both patients and clinicians, it can be important to know if the new lesion is just radiation gliosis or pseudo-progression, and not a tumor relapse.
CONCLUSION
In general, intraoperative FS diagnoses demonstrate high diagnostic accuracy. However, the agreement varies among histopathological entities and is lower in WHO low-grade tumors than in high-grade tumors. Sensitivity for diagnosing CNS lymphomas is low. A variable degree of reservation is always necessary when interpreting and communicating FS diagnoses.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/1/170/146153
Contributor Information
Kathrine Tofte, Email: oddnykat@stud.ntnu.no.
Cathrine Berger, Email: cathrbe@stud.ntnu.no.
Sverre Helge Torp, Email: sverre.torp@ntnu.no.
Ole Solheim, Email: ole.solheim@ntnu.no.
REFERENCES
- 1.Aldape K, Simmons ML, Davis RL, Miike R, Wiencke J, Barger G, et al. Discrepancies in diagnoses of neuroepithelial neoplasms: The San Francisco Bay Area Adult Glioma Study. Cancer. 2000;88:2342–9. [PubMed] [Google Scholar]
- 2.Clarke JL, Chang SM. Neuroimaging: Diagnosis and response assessment in glioblastoma. Cancer J. 2012;18:26–31. doi: 10.1097/PPO.0b013e318244d7c8. [DOI] [PubMed] [Google Scholar]
- 3.Colbassani HJ, Nishio S, Sweeney KM, Bakay RA, Takei Y. CT-assisted stereotactic brain biopsy: Value of intraoperative frozen section diagnosis. J Neurol Neurosurg Psychiatry. 1988;51:332–41. doi: 10.1136/jnnp.51.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: A meta-analysis. J Clin Oncol. 2012;30:2559–65. doi: 10.1200/JCO.2011.38.4818. [DOI] [PubMed] [Google Scholar]
- 5.Folkerth RD. Smears and frozen sections in the intraoperative diagnosis of central nervous system lesions. Neurosurg Clin N Am. 1994;5:1–18. [PubMed] [Google Scholar]
- 6.Gulati S, Jakola AS, Nerland US, Weber C, Solheim O. The risk of getting worse: Surgically acquired deficits, perioperative complications, and functional outcomes after primary resection of glioblastoma. World Neurosurg. 2011;76:572–9. doi: 10.1016/j.wneu.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 7.Gupta M, Djalilvand A, Brat DJ. Clarifying the diffuse gliomas: An update on the morphologic features and markers that discriminate oligodendroglioma from astrocytoma. Am J Clin Pathol. 2005;124:755–68. doi: 10.1309/6JNX-4PA6-0TQ5-U5VG. [DOI] [PubMed] [Google Scholar]
- 8.Hagen T, Nieder C, Moringlane JR, Feiden W, Konig J. Correlation of preoperative neuroradiologic with postoperative histologic diagnosis in pathological intracranial processes. Radiologe. 1995;35:808–15. [PubMed] [Google Scholar]
- 9.Hasseleid BF, Meling TR, Ronning P, Scheie D, Helseth E. Surgery for convexity meningioma: Simpson Grade I resection as the goal: Clinical article. J Neurosurg. 2012;117:999–1006. doi: 10.3171/2012.9.JNS12294. [DOI] [PubMed] [Google Scholar]
- 10.Jakola AS, Myrmel KS, Kloster R, Torp SH, Lindal S, Unsgard G, et al. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA. 2012;308:1881–8. doi: 10.1001/jama.2012.12807. [DOI] [PubMed] [Google Scholar]
- 11.Jakola AS, Unsgard G, Solheim O. Quality of life in patients with intracranial gliomas: The impact of modern image-guided surgery. J Neurosurg. 2011;114:1622–30. doi: 10.3171/2011.1.JNS101657. [DOI] [PubMed] [Google Scholar]
- 12.Julia-Sape M, Acosta D, Majos C, Moreno-Torres A, Wesseling P, Acebes JJ, et al. Comparison between neuroimaging classifications and histopathological diagnoses using an international multicenter brain tumor magnetic resonance imaging database. J Neurosurg. 2006;105:6–14. doi: 10.3171/jns.2006.105.1.6. [DOI] [PubMed] [Google Scholar]
- 13.Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109. doi: 10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maier SE, Sun Y, Mulkern RV. Diffusion imaging of brain tumors. NMR Biomed. 2010;23:849–64. doi: 10.1002/nbm.1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinez AJ, Pollack I, Hall WA, Lunsford LD. Touch preparations in the rapid intraoperative diagnosis of central nervous system lesions. A comparison with frozen sections and paraffin-embedded sections. Mod Pathol. 1988;1:378–84. [PubMed] [Google Scholar]
- 16.McGirt MJ, Mukherjee D, Chaichana KL, Than KD, Weingart JD, Quinones-Hinojosa A. Association of surgically acquired motor and language deficits on overall survival after resection of glioblastoma multiforme. Neurosurgery. 2009;65:463–9. doi: 10.1227/01.NEU.0000349763.42238.E9. [DOI] [PubMed] [Google Scholar]
- 17.Mittler MA, Walters BC, Stopa EG. Observer reliability in histological grading of astrocytoma stereotactic biopsies. J Neurosurg. 1996;85:1091–4. doi: 10.3171/jns.1996.85.6.1091. [DOI] [PubMed] [Google Scholar]
- 18.Morita N, Harada M, Otsuka H, Melhem ER, Nishitani H. Clinical Application of MR Spectroscopy and Imaging of Brain Tumor. Magn Reson Med Sci. 2010;9:167–75. doi: 10.2463/mrms.9.167. [DOI] [PubMed] [Google Scholar]
- 19.Plesec TP, Prayson RA. Frozen section discrepancy in the evaluation of central nervous system tumors. Arch Pathol Lab Med. 2007;131:1532–40. doi: 10.5858/2007-131-1532-FSDITE. [DOI] [PubMed] [Google Scholar]
- 20.Prayson RA, Agamanolis DP, Cohen ML, Estes ML, Kleinschmidt-DeMasters BK, Abdul-Karim F, et al. Interobserver reproducibility among neuropathologists and surgical pathologists in fibrillary astrocytoma grading. J Neurol Sci. 2000;175:33–9. doi: 10.1016/s0022-510x(00)00274-4. [DOI] [PubMed] [Google Scholar]
- 21.Regragui A, Amarti Riffi A, Maher M, El Khamlichi A, Saidi A. Accuracy of intraoperative diagnosis in central nervous system tumors: Report of 1315 cases. Neurochirurgie. 2003;49:67–72. [PubMed] [Google Scholar]
- 22.Reni M, Ferreri AJ. Therapeutic management of primary CNS lymphoma in immunocompetent patients. Expert Rev Anticancer Ther. 2001;1:382–94. doi: 10.1586/14737140.1.3.382. [DOI] [PubMed] [Google Scholar]
- 23.Reyes MG, Homsi MF, McDonald LW, Glick RP. Imprints, smears, and frozen sections of brain tumors. Neurosurgery. 1991;29:575–9. doi: 10.1097/00006123-199110000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Rogers L, Gilbert M, Vogelbaum MA. Intracranial meningiomas of atypical (WHO grade II) histology. J Neurooncol. 2010;99:393–405. doi: 10.1007/s11060-010-0343-1. [DOI] [PubMed] [Google Scholar]
- 25.Savargaonkar P, Farmer PM. Utility of intra-operative consultations for the diagnosis of central nervous system lesions. Ann Clin Lab Sci. 2001;31:133–9. [PubMed] [Google Scholar]
- 26.Shah AB, Muzumdar GA, Chitale AR, Bhagwati SN. Squash preparation and frozen section in intraoperative diagnosis of central nervous system tumors. Acta Cytol. 1998;42:1149–54. doi: 10.1159/000332104. [DOI] [PubMed] [Google Scholar]
- 27.Sughrue ME, Kane AJ, Shangari G, Rutkowski MJ, McDermott MW, Berger MS, et al. The relevance of Simpson Grade I and II resection in modern neurosurgical treatment of World Health Organization Grade I meningiomas. J Neurosurg. 2010;113:1029–35. doi: 10.3171/2010.3.JNS091971. [DOI] [PubMed] [Google Scholar]
- 28.Uematsu Y, Owai Y, Okita R, Tanaka Y, Itakura T. The usefulness and problem of intraoperative rapid diagnosis in surgical neuropathology. Brain Tumor Pathol. 2007;24:47–52. doi: 10.1007/s10014-007-0219-z. [DOI] [PubMed] [Google Scholar]
- 29.van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: A clinician's perspective. Acta Neuropathol. 2010;120:297–304. doi: 10.1007/s00401-010-0725-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


