Abstract
IMPORTANCE
Follow-up with a primary care provider (PCP) in addition to the surgical team is routinely recommended to patients discharged after major surgery despite no clear evidence that it improves outcomes.
OBJECTIVE
To test whether PCP follow-up is associated with lower 30-day readmission rates after open thoracic aortic aneurysm (TAA) repair and ventral hernia repair (VHR), surgical procedures known to have a high and low risk of readmission, respectively.
DESIGN, SETTING, AND PARTICIPANTS
In a cohort of Medicare beneficiaries discharged to home after open TAA repair (n = 12 679) and VHR (n = 52 807) between 2003 to 2010, we compared 30-day readmission rates between patients seen and not seen by a PCP within 30 days of discharge and across tertiles of regional primary care use. We stratified our analysis by the presence of complications during the surgical (index) admission.
MAIN OUTCOMES AND MEASURES
Thirty-day readmission rate.
RESULTS
Overall, 2619 patients (20.6%) undergoing open TAA repair and 4927 patients (9.3%) undergoing VHR were readmitted within 30 days after surgery. Complications occurred in 4649 patients (36.6%) undergoing open TAA repair and 4528 patients (8.6%) undergoing VHR during their surgical admission. Early follow-up with a PCP significantly reduced the risk of readmission among open TAA patients who experienced perioperative complications, from 35.0% (without follow-up) to 20.4% (with follow-up) (P < .001). However, PCP follow-up made no significant difference in patients whose hospital course was uncomplicated (19.4% with follow-up vs 21.9% without follow-up; P = .31). In comparison, early follow-up with a PCP after VHR did not reduce the risk of readmission, regardless of complications. In adjusted regional analyses, undergoing open TAA repair in regions with high compared with low primary care use was associated with an 18% lower likelihood of 30-day readmission (odds ratio, 0.82; 95% CI, 0.71–0.96; P = .02), whereas no significant difference was found among patients after VHR.
CONCLUSIONS AND RELEVANCE
Follow-up with a PCP after high-risk surgery (eg, open TAA repair), especially among patients with complications, is associated with a lower risk of hospital readmission. Patients undergoing lower-risk surgery (eg, VHR) do not receive the same benefit from early PCP follow-up. Identifying high-risk surgical patients who will benefit from PCP integration during care transitions may offer a low-cost solution toward limiting readmissions.
At the time of discharge after high-risk surgery, patients are routinely counseled to follow-up with their primary care provider (PCP) as well as the surgeon who performed their procedure. Aside from representing a tradition in surgical practice, patients and physicians presume that early follow-up with the PCP represents an opportunity to address problems that may emerge during the care transition from inpatient to outpatient settings. Early PCP follow-up after admission for high-risk medical conditions, such as heart failure or pneumonia, has been demonstrated1,2 to lower the risk of hospital readmission, helping to validate this practice.
However, the value added by a PCP visit after surgical discharge has been debated for several reasons. First, PCPs may believe that a visit after surgical discharge is unnecessary because issues arising soon after surgery are likely related to the operation and would be best addressed by the surgical team. Second, elderly patients, often debilitated following major surgery, may not be willing to make additional office visits or will not be adherent to them, especially if the visits seem unlikely to add value.3 Finally, in a health care environment increasingly focused on efficiency, more than 6.9 million major cardiovascular operations are performed annually, translating into increasing costs associated with scheduling routine PCP follow-up visits.4
Patients undergoing open thoracic aortic aneurysm (TAA) repair have one of the highest documented readmission rates of any major cardiovascular operation commonly performed among Medicare beneficiaries.5 Accordingly, these procedures have been selected as a potential target for nonreimbursement for readmissions. Within this high-risk population, we examined whether early PCP follow-up visits in addition to surgical follow-up was associated with lower rates of readmission. We examined this question among individual patients undergoing open TAA repair, as well as across hospital referral regions, for patients with and without complications sustained during their index surgical admission. In addition, a control group consisting of patients undergoing uncomplicated elective ventral hernia repair (VHR) was used to compare the benefit of early PCP follow-up among patients undergoing a common lower-risk surgical procedure.
Methods
Data Sources and Study Population
We used the Centers for Medicare & Medicaid Services Medicare Provider Analysis and Review database to study patients undergoing open TAA repair and open VHR between January 1, 2003, and November 30, 2010. International Classification of Diseases, Ninth Revision procedure codes were used to identify patients who underwent open repair of nonruptured open TAA repair as well as open VHR from the Part A Medicare claims data set. In addition to procedural codes for open TAA repair and VHR, each patient was required to have a diagnosis code for TAA and nonobstructed/nongangrenous ventral hernia.
Because our analysis was focused on readmission, patients who underwent surgery were excluded from analysis if they died during their index admission or if they were discharged home with hospice care. To evaluate outpatient visits, Part B Medicare claims were linked to inpatient denominator files for patients undergoing open TAA repair and VHR from January 1, 2003, to November 30, 2010. Part B claims for evaluation and management services were used to examine outpatient visits with PCPs following discharge from the index hospitalization and were captured using Current Procedural Terminology codes 99201 through 99205, 99211 through 99215, 99241 through 99245, 99301 through 99303, 99311 through 99313, 99321 through 99345, and 99347 through 99350. The final date for 30-day patient follow-up was December 30, 2010. Our study protocol was approved by the Dartmouth Institutional Review Board.
Defining the Exposure Variable
Our main exposure variable was patient evaluation by a PCP within 30 days of hospital discharge after elective open TAA repair and VHR. A PCP was defined as a health care worker who was not a member of the surgical team, which included primary care physicians as well as nurse practitioners and/or physician assistants. The PCP visit needed to occur before the date of any readmission. We included all evaluations by PCPs that were performed in an outpatient clinic setting as well as within the patient’s home.
Main Outcome Measure
The primary outcome for the study was 30-day readmission following discharge after surgery. Readmission was defined as a readmission to any hospital within 30 days of discharge from the index hospitalization for the open TAA repair or VHR procedure. Only the first readmission during the first 30 days postoperatively was examined. Transfers to and from another hospital and admissions for rehabilitation were not counted as readmissions.
Prior work5,6 has established that patients who have undergone open TAA repair or VHR and developed complications during their surgical admission are at higher risk for readmission after surgery. Therefore, analysis of our primary outcome was stratified across patients who had and those who had not experienced any major complication during their index hospitalization. Following open TAA repair, major peri-operative complications were defined as renal failure, cardio-pulmonary failure, major gastrointestinal complication, spinal cord ischemia, and stroke or major cerebrovascular complication. Major perioperative-related complications following VHR were defined as gastrointestinal injury, accidental laceration, or cardiopulmonary failure.
Primary Care Use by Hospital Referral Region
To examine the usefulness of primary care access at population-based levels, regional primary care use measures were identified from the Dartmouth Atlas of Healthcare across the 307 nationwide Hospital Referral Regions (HRRs).7 Primary care use was defined as the percentage of Medicare beneficiaries in each HRR who had at least one ambulatory visit to a primary care provider per calendar year between 2003 and 2007. Regional primary care use data for all nationwide HRRs were then linked to patient-level data from the Medicare Provider Analysis and Review Part A claims data set using unique Centers for Medicare & Medicaid Services hospital identifiers (Figure 1).
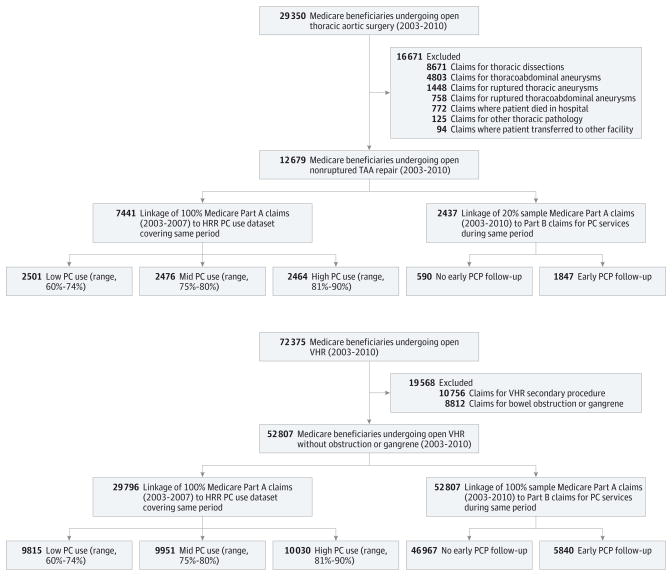
Figure 1. Selection of Patient Cohort Undergoing Open Thoracic Aortic Aneurysm (TAA) Repair and Ventral Hernia Repair (VHR).
Data set linkage to determine primary care provider (PCP) utilization shown. HRR indicates hospital referral region; PC, primary care.
Statistical Analysis
For patient-level PCP visit analyses, a 20% sample of Medicare beneficiaries from the entire open TAA repair cohort was available, whereas a 100% sample of Part B claims was used for VHR and the regional-level analyses (Figure 1). We started by using unadjusted analyses to compare the rates of readmission between patients who were and those who were not seen by a PCP within 30 days following discharge. Crude analyses of patient variables and outcome measures were performed using χ2 tests for categorical variables, unpaired, 2-tailed t tests for continuous variables that were normally distributed, and Wilcoxon signed-rank tests for nonnormally distributed data. We then conducted stratified analyses to examine the effect of major complications on readmission. Potential interactions (effect modifiers) between variables were explored using both stratification techniques and multivariate analysis. In addition, we conducted a sensitivity analysis to investigate whether readmission rates varied by whether PCP follow-up occurred less than or equal to 14 days or greater than 14 days later.
In our regional analyses, we compared readmission rates across nationwide HRRs.8 Our numerator for these calculations was the number of patients readmitted after open TAA repair and VHR, and the denominator was the number of patients undergoing each procedure. We divided all regions into terciles of primary care use and compared regional readmission rates across the terciles of primary care use. To examine the effect of individual patient-level covariates within these regional strata, we conducted stratified analyses based on patient-level probabilities of readmission. Readmission probability scores were calculated based on variables associated with readmission probability scores (log [ρ/(1 − ρ)]) and then used to match patients within models. Patients were matched using nearest-neighbor matching techniques, based on having a low, medium, or high probability for readmission.
Risk-adjusted logistic regression models were constructed to estimate the association between patient- and regional-level primary care use with subsequent risk of readmission. These models controlled for baseline patient demographic variables for age (continuous and categorical variables), sex, race, urgency of admission (elective, urgent, or emergent), and comorbidity score using the Charlson comorbidity index. In addition, regression models and stratified analyses were designed to control for whether patients experienced a major postoperative complication. These models accounted for clustering of patient-level outcomes within hospitals and within hospital referral regions.
P < .05 (2-sided) was considered to be significant for all statistical tests and models, and Bonferroni correction was used to control for multiple comparisons.9 Stata, version 11.0 (Stata-Corp), statistical software was used for all analyses.
Results
Patient Characteristics
We identified 12 679 patients who underwent open TAA repair and 52 807 patients who underwent VHR between 2003 and 2010 (Figure 1). The characteristics of the patients, stratified by PCP follow-up, are reported in Table 1. Among the 20% sample of our entire open TAA repair cohort (2437 available for analysis), we found that 1847 patients (75.8%) had PCP follow-up within 30 days after discharge, whereas 5840 (11.1%) patients had early PCP follow-up after VHR. Follow-up occurred a median of 12 days following discharge for open TAA repair and a median of 11 days for VHR. Compared with patients without 30-day follow-up, patients who attended a follow-up visit with a PCP were less likely to have experienced a renal or pulmonary complication after open TAA repair but more likely to have a bowel injury complication after VHR (Table 1).
Table 1.
Characteristics of Patient Populations Undergoing Open TAA Repair and VHRa
| Characteristic | Early PCP Follow-up
|
Level of Primary Care Use in HRRs
|
|||||
|---|---|---|---|---|---|---|---|
| No | Yes | P Value | Low | Medium | High | P Value | |
| Open TAA Repair | |||||||
|
| |||||||
| No. of patients | 590 | 1847 | 2501 | 2476 | 2464 | ||
|
| |||||||
| Age, No. (%), y | |||||||
|
| |||||||
| 65–69 | 136 (23.0) | 503 (27.2) | .13 | 575 (23.0) | 643 (26.0) | 641 (26.0) | <.002 |
|
|
|
||||||
| 70–79 | 363 (61.5) | 1065 (57.7) | 1501 (60.0) | 1486 (60.0) | 1503 (61.0) | ||
|
|
|
||||||
| ≥80 | 91 (15.4) | 279 (15.1) | 425 (17.0) | 347 (14.0) | 320 (13.0) | ||
|
| |||||||
| Male sex, No. (%) | 296 (50.2) | 1085 (58.7) | <.001 | 1100 (44.0) | 1065 (43.0) | 1084 (44.0) | .62 |
|
| |||||||
| Black race, No. (%) | 39 (6.6) | 53 (2.7) | <.001 | 125 (5.0) | 74 (3.0) | 99 (4.0) | .003 |
|
| |||||||
| Charlson comorbidity index score, No. (%) | |||||||
|
| |||||||
| <1 | 460 (78.0) | 1515 (82.0) | .06 | 1976 (79.0) | 2006 (81.0) | 1996 (81.0) | .22 |
|
|
|
||||||
| 1–2 | 36 (6.1) | 110 (6.0) | 175 (7.0) | 148 (6.0) | 148 (6.0) | ||
|
|
|
||||||
| >2 | 94 (15.9) | 222 (12.0) | 350 (14.0) | 322 (13.0) | 320 (13.0) | ||
|
| |||||||
| Hospital LOS, mean (SD) | 14.2 (16.1) | 10.4 (7.2) | <.001 | 9.4 (8.3) | 8.3 (6.1) | 8.1 (7.4) | .09 |
|
| |||||||
| Complications, No. (%) | |||||||
|
| |||||||
| Renal failure | 62 (10.5) | 118 (6.4) | <.001 | 200 (8.0) | 149 (6.0) | 172 (7.0) | .03 |
|
| |||||||
| Pulmonary failure | 214 (36.3) | 511 (27.7) | <.001 | 725 (29.0) | 693 (28.0) | 517 (21.0) | <.001 |
|
| |||||||
| Spinal cord ischemia | 5 (0.8) | 8 (0.4) | .23 | 18 (0.7) | 10 (0.4) | 15 (0.6) | .54 |
|
| |||||||
| Cerebrovascular event | 38 (6.4) | 88 (4.8) | .11 | 150 (6.0) | 149 (6.0) | 123 (5.0) | .91 |
|
| |||||||
| Open VHR | |||||||
|
| |||||||
| No. of patients | 46 967 | 5840 | 9815 | 9951 | 10 030 | ||
|
| |||||||
| Age, No. (%), y | |||||||
|
| |||||||
| 65–69 | 11 375 (32.0) | 1246 (28.4) | .04 | 2284 (30.0) | 2248 (29.5) | 2409 (31.7) | .02 |
|
|
|
||||||
| 70–79 | 17 934 (50.5) | 2256 (51.8) | 3879 (50.8) | 3964 (52.0) | 3898 (51.3) | ||
|
|
|
||||||
| ≥80 | 6219 (17.5) | 871 (20.2) | 1480 (19.4) | 1404 (18.4) | 1296 (17.0) | ||
|
| |||||||
| Male sex, No. (%) | 27885 (59.4) | 3492 (59.8) | .53 | 5827 (59.4) | 5888 (59.2) | 5940 (59.0) | .96 |
|
| |||||||
| Black race, No. (%) | 2787 (5.9) | 336 (5.8) | .58 | 579 (6.0) | 571 (5.7) | 560 (5.6) | .63 |
|
| |||||||
| Charlson comorbidity index score, No. (%) | |||||||
|
| |||||||
| <1 | 26 840 (57.1) | 3110 (53.3) | <.001 | 5740 (58.5) | 5532 (55.6) | 5639 (56.2) | .02 |
|
|
|
||||||
| 1–2 | 14 709 (31.3) | 1925 (33.0) | 3022 (30.8) | 3184 (32.0) | 3143 (31.3) | ||
|
|
|
||||||
| >2 | 5418 (11.5) | 805 (13.8) | 1053 (10.7) | 1235 (12.4) | 1248 (12.4) | ||
|
| |||||||
| Hospital LOS, mean (SD) | 3.4 (2.9) | 3.9 (3.0) | <.001 | 3.3 (3.1) | 3.4 (2.9) | 3.5 (2.9) | .02 |
|
| |||||||
| Complications, No. (%) | |||||||
|
| |||||||
| Bowel injury | 2624 (5.3) | 367 (6.3) | .02 | 457 (4.6) | 549 (5.5) | 622 (6.2) | <.001 |
|
| |||||||
| Cardiopulmonary | 1027 (2.2) | 197 (3.4) | .04 | 285 (2.9) | 295 (3.0) | 277 (2.8) | .68 |
Abbreviations: HRRs, Hospital Referral Regions; LOS, length of stay; TAA, thoracic aortic aneurysm; VHR, ventral hernia repair.
Denominators vary for some characteristics based on data available.
The characteristics of patients undergoing open TAA repair and VHR, stratified by regional levels of primary care use, are also reported in Table 1. Patients who underwent either open TAA repair or VHR in regions with low primary care use were significantly older (P < .05) compared with those in regions with higher use. Patients undergoing open TAA repair in regions with low primary care use had higher rates of renal and pulmonary postoperative complications. In comparison, patients undergoing VHR in regions with low primary care use had shorter lengths of stay and a lower rate of bowel injury complications.
Readmission Rate by PCP Follow-up
Among patients with Part B claims available for analysis, a total of 538 (22.1%) patients who underwent open TAA repair and 4927 (9.3%) patients who underwent VHR were readmitted within 30 days after surgery. Readmissions occurred a mean (SD) of 11.0 (7.9) days after discharge, and patients spent 6.3 (7.8) days in the hospital once readmitted. Compared with patients who had no early follow-up care, patients who visited a PCP within 30 days were significantly less likely to be readmitted following open TAA repair (19.7% vs 28.0%; P < .001), whereas there was no benefit associated with early PCP follow-up for patients undergoing VHR (9.4% vs 9.3%; P = .77).
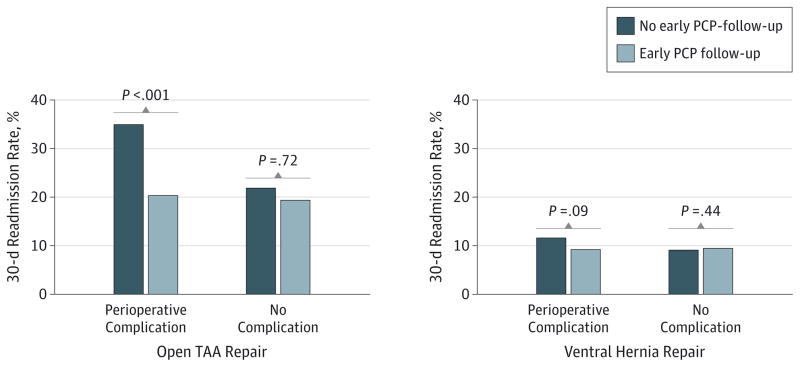
For patients undergoing open TAA repair, the presence of a postoperative complication significantly modified the association between PCP follow-up and 30-day readmission (Figure 2). Patients who had experienced any major postoperative complication following open TAA repair received a significantly greater benefit from early PCP follow-up on risk of readmission (20.4% with follow-up vs 35.0% without follow-up; P < .001) compared with patients who experienced an uncomplicated postoperative hospital course (19.4% with follow-up vs 21.9% without follow-up; P = .31). In comparison, the presence of a complication did not significantly change the association between PCP follow-up and readmission for patients undergoing VHR repair (Figure 2). These associations were sustained regardless of PCP follow-up before or after 14 days.
Figure 2. Thirty-Day Readmission Rates Following Open Thoracic Aortic Aneurysm (TAA) Repair and Ventral Hernia Repair.
Early primary care provider (PCP) follow-up significantly reduced 30-day readmission following open TAA repair if a postoperative complication occurred. In comparison, early PCP follow-up was not associated with a significant difference in readmission rates among patients undergoing ventral hernia repair, whether or not a complication occurred.
The association between 30-day primary care follow-up and readmission for patients undergoing open TAA repair and VHR were confirmed in risk-adjusted logistic regression models accounting for patient comorbidities and stratified by whether perioperative complications occurred (Table 2). In the open TAA repair models, early PCP follow-up when a complication occurred was associated with a 47% decrease (odds ratio [OR], 0.53; 95% CI, 0.37–0.75; P < .001) in the likelihood of being readmitted within 30 days (Table 2). In comparison, early PCP follow-up did not significantly reduce the risk of readmission among VHR patients with or without perioperative complications (Table 2).
Table 2.
Risk-Adjusted Odds of 30-Day Readmission Following Open TAA Repair and VHR
| Characteristic | Postoperative Complicationa
|
No Complicationa
|
||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Open TAA Repair | ||||
|
| ||||
| Early PCP follow-up | 0.53 (0.37–0.75) | <.001 | 0.97 (0.69–1.37) | .87 |
|
| ||||
| Length of hospital stay, d | ||||
|
| ||||
| <9 | 1 [Reference] | 1 [Reference] | ||
|
| ||||
| ≥9 | 1.16 (0.84–1.60) | .36 | 0.83 (0.62–1.11) | .20 |
|
| ||||
| Age, y | ||||
|
| ||||
| 65–69 | 1 [Reference] | 1 [Reference] | ||
|
| ||||
| 70–79 | 1.06 (0.73–1.53) | .77 | 0.98 (0.70–1.36) | .88 |
|
| ||||
| ≥80 | 1.34 (0.81–2.23) | .25 | 0.98 (0.58–1.66) | .93 |
|
| ||||
| Black race | 1.47 (0.62–3.51) | .39 | 1.40 (0.69–2.84) | .35 |
|
| ||||
| Male sex | 1.10 (0.76–1.60) | .61 | 0.70 (0.53–0.93) | .01 |
|
| ||||
| Charlson comorbidity index score | ||||
|
| ||||
| <1 | 1 [Reference] | 1 [Reference] | ||
|
| ||||
| 1–2 | 1.41 (0.80–2.51) | .24 | 1.30 (0.72–2.02) | .34 |
|
| ||||
| >2 | 1.62 (1.12–2.35) | .01 | 1.36 (0.84–2.57) | .23 |
|
| ||||
| Open VHR | ||||
|
| ||||
| Early PCP follow-up | 0.74 (0.52–1.06) | .10 | 1.05 (0.93–1.18) | .43 |
|
| ||||
| Length of hospital stay, d | ||||
|
| ||||
| <3 | 1 [Reference] | 1 [Reference] | ||
|
| ||||
| ≥3 | 1.08 (0.84–1.40) | .54 | 1.58 (1.46–1.71) | <.001 |
|
| ||||
| Age, y | ||||
|
| ||||
| 65–69 | 1 [Reference] | 1 [Reference] | ||
|
| ||||
| 70–79 | 1.03 (0.81–1.31) | .80 | 0.99 (0.91–1.08) | .78 |
|
| ||||
| ≥80 | 1.05 (0.76–1.44) | .77 | 1.07 (0.96–1.19) | .22 |
|
| ||||
| Black race | 1.61 (1.03–2.50) | .04 | 1.35 (1.14–1.60) | <.001 |
|
| ||||
| Male sex | 1.15 (0.92–1.44) | .23 | 0.96 (0.87–1.03) | .27 |
|
| ||||
| Charlson comorbidity index score | ||||
|
| ||||
| <1 | 1 [Reference] | 1 [Reference] | ||
|
| ||||
| 1–2 | 1.23 (0.97–1.54) | .08 | 1.32 (1.21–1.44) | <.001 |
|
| ||||
| >2 | 1.28 (0.90–1.81) | .16 | 1.68 (1.50–1.89) | <.001 |
Abbreviations: OR, odds ratio; PCP, primary care provider; TAA, thoracic aortic aneurysm; VHR, ventral hernia repair.
Includes major postoperative complications such as renal failure, pulmonary failure, spinal cord ischemia, cerebrovascular event, and gastrointestinal injury or ischemia for patients undergoing open TAA repair; and bowel injury, cardiopulmonary failure, and accidental laceration for patients undergoing VHR.
Readmission Rates by Regional Primary Care Use Tercile
To further explore the association between outpatient primary care follow-up with risk of readmission following open TAA repair and VHR, we assessed the variation in primary care use within 307 nationwide HRRs. A total of 7441 beneficiaries underwent open TAA repair and 29 796 beneficiaries underwent VHR between 2003 and 2007 and had their claims data linked to rates of primary care use at the HRR level for the corresponding years. As displayed in Figure 1, patients were then stratified into 3 equally sized groups based on regional rates of primary care use, classified as low (range, 60%–74%), medium (range, 75%–80%), and high (range, 81%–90%).
After stratifying patients by regional level of primary care use, we found that open TAA repair undertaken in regions with high primary care use was associated with a significant reduction in 30-day readmission compared with regions with low primary care use (19.6% vs 23.3%; P = .04). Moreover, readmission following open TAA repair was significantly lower in regions with high vs low primary care utilization when a complication occurred (20.6% vs 25.5%; P = .03), but was not significantly lower when patients had an uncomplicated hospital course 19.1% vs 22.0%; P = .12). In comparison, we found no significant difference in readmission rates among patients undergoing open VHR in regions with high vs low primary care use (9.2% vs 9.1; P = .18), regardless of whether a perioperative complication occurred.
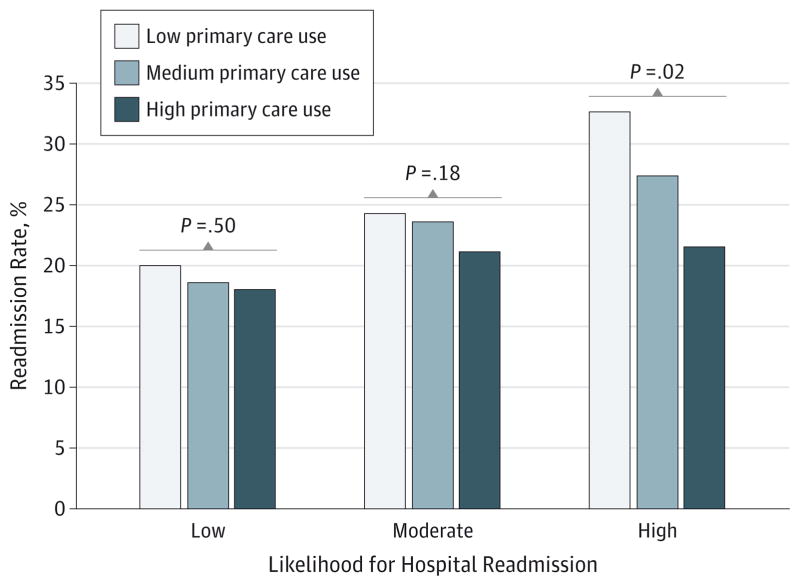
The results of the region comparisons were confirmed in logistic regression models that controlled for patient demographics and complications. Adjusted models demonstrated an 18% lower likelihood of readmission (OR, 0.82; 95% CI, 0.71–0.96; P = .02) when open TAA repair was undertaken in regions with high compared with low primary care use, whereas no significant difference in readmission risk was found when VHR was undertaken in regions with high vs low primary care use (OR, 1.0; 95% CI, 0.91–1.10; P = .92). Furthermore, readmission rates following open TAA repair varied across patient strata categorized as being at low, medium, or high risk for readmission using risk scores. Among patients classified as being at low or medium risk for readmission, there was no significant difference between readmission rates following open TAA repair in regions with low vs high primary care use (Figure 3). However, patients estimated to be at high risk for readmission following open TAA repair had a significant reduction in readmission rates (21.5% high vs 32.6% low; P = .02) when procedures were undertaken in regions with high vs low primary care use.
Figure 3. Thirty-Day Readmission Rates Among Patients at Low, Moderate, and High Risk for Readmission Following Open Thoracic Aortic Aneurysm Repair.
Patients determined to be at the highest risk for readmission following open thoracic aortic aneurysm repair achieved the greatest benefit from having their procedure performed in a region with high primary care use.
Discussion
Hospital readmissions for high-risk medical and surgical patients are common, and these events impose a significant economic effect on our health care system. Our study demonstrates that early follow-up with a PCP after high-risk surgery, such as open TAA repair, especially among patients who have a complicated hospital course, is associated with a lower risk of hospital readmission. Furthermore, we show that regional- and patient-level use of primary care services among Medicare beneficiaries is similarly correlated with the risk of 30-day readmission following open TAA repair. In comparison, our data indicate that early PCP follow-up after a lower-risk surgery, such as VHR, does not reduce the risk of readmission. These findings suggest that ensuring access to primary care follow-up for high-risk surgical patients and coordinating outpatient services during transitions of care may be an effective strategy to limit readmissions.
The transition from inpatient to outpatient care is a critical stage for patients hospitalized with a wide range of complex medical and surgical conditions. Transitional care includes many critical processes, such as communication between inpatient and outpatient providers, reconciliation of medications, coordinating outpatient services, and ensuring that patients follow up with appropriate PCPs.10 Deficits in communication and/or the transfer of information between hospital physicians and outpatient PCPs is estimated to affect the quality of care and outcomes in more than 25% of discharged patients.11 As such, the Patient Protection and Affordable Care Act of 201012 established a variety of transition care programs to improve quality among vulnerable patients.10 Improving the components of transitional care can significantly reduce readmission rates among patients with high-risk medical conditions.13 This includes high-risk medical patients randomized to comprehensive hospital discharge programs, which have been shown14,15 to significantly reduce readmissions among those receiving coordinated follow-up appointments and medicine reconciliation. Finally, it was shown1 that among patients hospitalized for heart failure complications, early follow-up with outpatient PCPs after discharge significantly reduced 30-day readmissions.
In terms of preventing readmission, it remains unknown whether the benefits associated with outpatient follow-up after high-risk medical discharge extend to patients undergoing high-risk surgical procedures. Presuming that these benefits would extend to patients with aortic aneurysm disease has face validity because many clinical characteristics are shared by these patients, including chronic obstructive pulmonary disease, diabetes mellitus, stroke, renal insufficiency, and congestive heart failure. These conditions are common in both high-risk populations, are all independently associated with an increased risk of readmission, and may be exacerbated by surgical stress during the perioperative period.16 In comparison, patients undergoing lower-risk surgery experience less physiological stress during the peri-operative period, which may reduce the likelihood that coexisting medical conditions will be exacerbated during the recovery period.17
We hypothesize that for patients undergoing high-risk surgery, follow-up with PCPs is a means by which complications or errors in discharge planning can be recognized before they escalate into larger problems. For example, a minor surgical site infection could be diagnosed and treated early with antibiotics, or treatment with a critical medication that was omitted from the discharge instructions could be restarted before the patient experienced an adverse clinical event. As our data show, most primary care follow-up occurred within 2 weeks after hospital discharge, allowing the opportunity for PCPs to implement these types of prophylactic measures in a clinic setting and avoid a preventable readmission.
It remains to be determined how triage should be conducted to select outpatient primary care services for surgical patients. As health care policy migrates toward capitated services, the relevant issue to address is whether all high-risk patients should be directed to primary care follow-up or whether there should be a targeted approach limited to patients most likely to benefit from primary care follow-up. Our study suggests that a good starting point is identifying patients undergoing surgical procedures associated with a high risk of readmission and focusing on those experiencing major complications during the postoperative course. Systems that identify and risk-stratify patients based on events during their postoperative hospital course can be used to ensure that individuals at high risk for readmission are targeted for primary care follow-up. This practice could be integrated as part of a coordinated transition care program using electronic health records, which have been shown13 to be effective for preventing readmissions among high-risk medical patients. As the mandate to reduce health care costs and improve the quality of care for surgical patients is upon us, transitional care programs, such as the ones described here, may prove to be effective in reducing readmission rates.
Our study has several limitations. First, primary care use was determined retrospectively from claims and our data were observational. Differences in outcomes between primary care use groups may be confounded by unmeasured socioeconomic variables and other factors that can influence access to care. However, Medicare beneficiaries are provided similar health care benefits, and use of outpatient services is determined by providers and health care referral networks. Second, although the use of 100% denominator Medicare claims was a reliable data set for longitudinal assessment of readmissions rates, it is not possible to accurately ascertain the cause of postsurgical readmissions from administrative data. It will be important to determine the causes of readmissions, such as infectious or cardiopulmonary complications, to plan future quality improvement initiatives. Third, the precise temporal association and mechanism by which visiting a PCP lowers the risk of readmissions remains undefined. Addressing this question, however, will likely delineate the processes of care that are important in avoiding readmission of surgical patients. Finally, although open TAA repair and VHR were used as examples of high- and low-risk surgical procedures, respectively, these procedures may not adequately reflect the effect of early PCP follow-up care on readmission risks for other surgical patients. It will be important to evaluate the role of early PCP follow-up in transitions of care for other common surgical conditions.
Conclusions
Routine follow-up with a PCP after high-risk surgery was associated with a lower likelihood of 30-day readmission, particularly among patients with a complicated postoperative course. This association was evident both in patient-and regional-level assessment of primary care integration in the discharge process, and patients at the highest risk for readmission appear to receive the greatest benefit from early outpatient primary care services. Low-risk surgical patients, however, may not receive a benefit from this routine practice. Ensuring primary care follow-up for high-risk surgical patients may be an effective, low-cost mechanism to limit readmissions.0
Acknowledgments
Funding/Support: Dr Goodney is supported by Career Development Award K08 HL05676 from the National Heart, Lung, and Blood Institute and a Society of Vascular Surgery Foundation award. Dr Goodman is supported in part by the Robert Wood Johnson Foundation.
Role of the Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: None reported.
Author Contributions: Dr Brooke had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Brooke, Stone, Cronenwett, Goodney.
Acquisition, analysis, or interpretation of data: Brooke, Stone, Nolan, DeMartino, MacKenzie, Goodman.
Drafting of the manuscript: Brooke, Goodney.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Brooke, Nolan, DeMartino, MacKenzie, Goodney.
Obtained funding: Goodney.
Administrative, technical, or material support: Stone, Goodman.
Study supervision: Stone, Cronenwett, DeMartino.
References
- 1.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 2.Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: examining the effects of timing of primary care provider follow-up. J Hosp Med. 2010;5(7):392–397. doi: 10.1002/jhm.666. [DOI] [PubMed] [Google Scholar]
- 3.Leduc N, Tannenbaum TN, Bergman H, Champagne F, Clarfield AM, Kogan S. Compliance of frail elderly with health services prescribed at discharge from an acute-care geriatric ward. Med Care. 1998;36(6):904–914. doi: 10.1097/00005650-199806000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;(29):1–20. 24. [PubMed] [Google Scholar]
- 5.Brooke BS, Goodney PP, Powell RJ, et al. Early discharge does not increase readmission or mortality after high-risk vascular surgery. J Vasc Surg. 2013;57(3):734–740. doi: 10.1016/j.jvs.2012.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T. Nationwide analysis of prolonged hospital stay and readmission after elective ventral hernia repair. Dan Med Bull. 2011;58(10):A4322. [PubMed] [Google Scholar]
- 7.Goodman DC, Brownlee S, Chang C-H, Fisher ES. Regional and Racial Variation in Primary Care and the Quality of Care among Medicare Beneficiaries. Lebanon, New Hampshire: Dartmouth Institute for Healthcare Policy and Clinical Practice; 2010. [PubMed] [Google Scholar]
- 8.Bauer H. Cimetidine in the preoperative treatment of acute bleeding gastroduodenal lesions [in German] MMW Munch Med Wochenschr. 1979;121(34):1085–1088. [PubMed] [Google Scholar]
- 9.Pocock SJ, Geller NL, Tsiatis AA. The analysis of multiple endpoints in clinical trials. Biometrics. 1987;43(3):487–498. [PubMed] [Google Scholar]
- 10.Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The care span: the importance of transitional care in achieving health reform. Health Aff (Millwood) 2011;30(4):746–754. doi: 10.1377/hlthaff.2011.0041. [DOI] [PubMed] [Google Scholar]
- 11.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 12.Patient Protection and Affordable Care Act: preexisting condition exclusions, lifetime and annual limits, rescissions, and patient protections: interim final rules with request for comments. Fed Regist. 2010;75(13):37187–37241. [PubMed] [Google Scholar]
- 13.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 14.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 16.Greenwald JL, Jack BW. Preventing the preventable: reducing rehospitalizations through coordinated, patient-centered discharge processes. Prof Case Manag. 2009;14(3):135–140. doi: 10.1097/NCM.0b013e318198d4e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veenhof AA, Vlug MS, van der Pas MH, et al. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg. 2012;255(2):216–221. doi: 10.1097/SLA.0b013e31824336e2. [DOI] [PubMed] [Google Scholar]