Abstract
The interface between the intestinal lumen and the mucosa is the location where the majority of ingested immunogenic particles face the scrutiny of the vast gastrointestinal immune system. Upon regular physiological conditions, the intestinal micro-flora and the epithelial barrier are well prepared to process daily a huge amount of food-derived antigens and non-immunogenic particles. Similarly, they are ready to prevent environmental toxins and microbial antigens to penetrate further and interact with the mucosal-associated immune system. These functions promote the development of proper immune responses and oral tolerance and prevent disease and inflammation. Brain-gut axis structures participate in the processing and execution of response signals to external and internal stimuli. The brain-gut axis integrates local and distant regulatory networks and super-systems that serve key housekeeping physiological functions including the balanced functioning of the intestinal barrier. Disturbance of the brain-gut axis may induce intestinal barrier dysfunction, increasing the risk of uncontrolled immunological reactions, which may indeed trigger transient mucosal inflammation and gut disease. There is a large body of evidence indicating that stress, through the brain-gut axis, may cause intestinal barrier dysfunction, mainly via the systemic and peripheral release of corticotropin-releasing factor. In this review, we describe the role of stress and corticotropin-releasing factor in the regulation of gastrointestinal permeability, and discuss the link to both health and pathological conditions.
Keywords: Corticotropin-releasing factor, Inflammation, Permeability, Stress
Official abbreviations according to UPHARM guideline were used in this review series.
CRF, corticotrophin-releasing factor
CRF1, corticotrophin-releasing factor receptor 1
CRF2, corticotrophin-releasing factor receptor 2
Introduction
The epithelium that lines our digestive tract harbors 100 trillion bacteria1 and mediates our relationship to the world outside. Our intestine is constantly exposed to a wide variety of immunogenic particles and microorganism-derived antigens. Its surface area is large enough to process over 50 tons of food in a lifetime. Intestinal and microbial components are strongly linked to each other and represent the most important barrier to limit luminal antigens from travelling across and reach the mucosal-associated immune system. They also play a critical role in training and modulating our immune system, helping it to distinguish between friend and foe.2,3 The absence of constructive engagement between microbes and intestinal mucosa may render epithelial barrier more permeable, allowing it to be breached. When this happens, resident cells become over-activated, and a cascade of pro-inflammatory signals is initiated.4,5 Altered intestinal permeability has large implications for human health, being involved in the origin and development of many digestive and non-digestive diseases. However, up to date, it is not clear whether intestinal barrier dysfunction is a primary event, an epiphenomenon or a consequence in the pathogenesis of these disorders.
The regulation of intestinal permeability involves terminals from ascending and descending pathways from the autonomic nervous system and the central nervous system, the hypothalamic pituitary-adrenal axis, and the enteric nervous system as well. The vast and versatile array of bidirectional and integrative communications between the brain and the gut allows the brain to respond to internal and external signals and, in return, to modify the autonomic and enteric nervous systems to keep intestinal permeability tight.
Physical and psychological stresses represent convincing evidence of the influence of the brain-gut axis on the intestinal barrier function. In fact, stress has been associated with reactivation of inflammatory and functional gastrointestinal disorders mainly through disruption of the intestinal barrier6 in both human and animal models. The stress response is vehiculated via 2 main systems: the sympatho-adrenomedullary system and the hypothalamic pituitary-adrenal axis. Stress stimulates the parvocellular neurons in the paraventricular nucleus of the hypothalamus to secrete corticotropin-releasing factor (CRF), and arginine vasopressin. CRF promotes the synthesis and release of adenocortico-tropic hormone in the anterior pituitary. The adenocorticotropic hormone, in turn, activates the adrenal cortex to induce a temporary rise in blood levels of cortisol and corticosterone7 and also the release of catecholamines by the adrenal medulla. It has been believed for a long time that central secretion of CRF was the main and unique mediator of the majority of the endocrine, behavioral and gastrointestinal changes induced by stress.8 However, we will show that peripheral release of CRF also plays a key role in the regulation of gastrointestinal permeability, and discuss the link to both health and pathological conditions.
Intestinal Permeability
The intestinal mucosal barrier includes several consecutive layers, from the outermost microbiota, through the external mucus, the epithelium, and down to the innermost lamina propria.9 The epithelial layer is described as a continuous polarized monolayer of columnar cells that separates the intestinal lumen from the internal milieu. Aside from epithelial cells, a variety of different cell types are also intermingled with enterocytes, including goblet cells, Paneth cells, enteroendocrine cells, and M cells. Within the lamina propria we can find blood and lymph vessels, and a plethora of distinct immune cells such as plasma cells, lymphocytes, macrophages, eosinophils, mast cells, dendritic cells, and a significant number of intrinsic and extrinsic nerve terminals.10 All of these components are exquisitely reactive and adaptive and display critical effector and modulatory functions. These functions are relevant for the control of inflammation, absorption and secretion, transport of macromolecules, and metabolic processes.11 Moreover, most of the cellular components have been shown to express receptors for CRF.12,13 But the job of the intestinal barrier now appears to be far more nuanced and complex as it communicates multidirectionally with the immune system and the microbes. Communication is developed through the release of an extensive array of chemical mediators, namely neuropeptides, neurohormones, neurotransmitters, cytokines, chemokines, growth factors, and other regulatory molecules.14,15
Enterocytes are tightly bonded to each other sealing the para-cellular space through the apical junctional complex, composed of tight junctions (TJs), adherens junctions, and desmosomes.16 The transmembrane TJ proteins occludin and claudins form complex protein systems, which interact with zonula occludens proteins that bind to the actin cytoskeleton. When actin contracts, it leads to increased permeability to electrolytes and small molecules.17 The paracellular space is not fully impermeable to molecules and antigens, allowing a controlled amount of small particles (less than 400 daltons) to penetrate across to reach the lamina propria,9 a phenomenon that plays a key role in the induction of immune tolerance. This passage of molecules also takes place through the transcellular pathway via endocytosis or exocytosis.18 Disruption of the intestinal barrier leads to uncontrolled flux of luminal antigens and possibly microbes across the epithelium, which may trigger immune activation and sepsis, and also lead to the development of chronic inflammation in the gut.6,19,20 Therefore, the tight regulation of intestinal permeability emerges as a central mechanism to prevent inflammatory diseases. Numerous pathogens and toxins, hormones and neurotransmitters, and gastrointestinal and non-gastrointestinal diseases have been associated with an augmented intestinal permeability.21 Among them, stress hormones and neurotransmitters have been consistently shown to modulate ion and water secretion, intestinal permeability, mucus secretion, and also intestinal flora.22–25
Stress-induced Intestinal Barrier Dysfunction: Role of Corticotropin-releasing Factor and Related Peptides
Stress represents a threat to the internal homeostasis that initiates a systemic coordinated response driven by the autonomic, endocrine, and immune systems to maintain stability. CRF and other members of the CRF signaling family, including urocortin (Ucn) 1, Ucn2, and Ucn3, are the best known and most important neuroendocrine mediators of the stress response.26,27 Central release of CRF and urocortins mediates autonomic, hormonal, and behavioural responses to stress and at the gastrointestinal tract, stimulates the enteric nervous system to modulate gastrointestinal motility and secretion.28–30 In addition, immune cells, regional sensory and sympathetic nerves, enterochromaffin cells, and enteric cells release CRF and urocortins within the gastrointestinal tract28 to modulate mucosal function and gastrointestinal motility.29
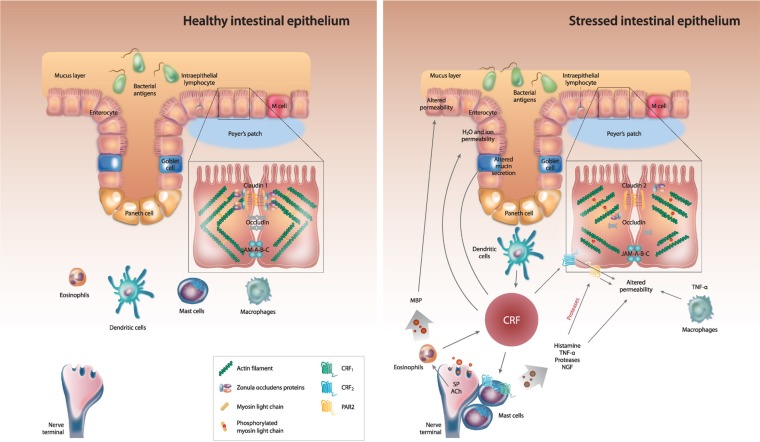
Different type of stress, acute or chronic, physical or psychological, have been shown to influence properties of the intestinal barrier function, including ion and water secretion, intestinal permeability, mucus secretion, and also intestinal flora in both human and animal models.6,31–35 Similarly, both central and peripheral administration of exogenous CRF have been shown to mimic the effects of acute stress in the gastrointestinal tract inducing mucin release,36 and increasing ion and water secretion and intestinal permeability.37,38 Figure summarizes the main effects of stress on the intestinal barrier and the role of CRF in gastrointestinal permeability.
Mucus Production and Release
The intestinal mucosal surface is covered by a layer of mucus gel containing antibacterial peptides and digestive enzymes.39,40 Mucus protects the epithelial lining from adhesion and invasion by attacking microorganisms, and other antigens present in the intestinal lumen.41 Mucus is produced by goblet cells, which express the CRF receptor 1 (CRF1).42 Stress has been shown to increase mucin release in colonic explants from rats submitted to immobilization, and to enhance rat mast cell protease II and prostaglandin E2 secretion. Intravenous or intracerebral injection of CRF in non-stressed rats reproduced stress-associated changes whereas administration of the CRF antagonist α-helical-CRF9–41 or the mast cell stabilizer lodoxamide inhibited them.36 In addition, those changes were abolished in mast-cell deficient mice, highlighting the key role of the CRF-mast cell axis in stress-mediated mucin release.43 On the contrary, rats submitted to chronic stress display mucus depletion and reduced number of goblet cells in the distal colon in association with increased bacterial adhesion and penetration into enterocytes,44,45 what could represent a step towards intestinal barrier dysfunction.
Ion and Water Secretion
Ion and water secretions also help to prevent the adhesion of pathogens and noxious substances to the mucosal surface, and dilute and flush out them down the gut to minimize their penetration to the lamina propria. Convergent evidences from studies in animal models indicate that both water and ion secretions increase in the intestinal tract in response to acute and chronic stress24,46 and in response to peripheral administration of CRF47 whereas selective CRF1 receptor agonists prevent this response to stress.48,49 Increased baseline short-circuit current (Isc), indicative of enhanced anion secretion, was found in the jejunum of Wistar-Kyoto rats submitted to restraint stress or cold restraint stress when compared to non-stressed rats. This increase in Isc was mediated by chloride anion secretion because replacement of the buffer by chloride free solution normalized Isc values.50 Later, Santos et al37,51 reproduced the results using a model of repetitive exposure to water avoidance stress (WAS) and found that peripheral CRF reproduced stress-induced rat jejunal and colonic epithelial barrier dysfunction via cholinergic and adrenergic nerves, and mast cells. More recently, long-term crowding exposure, a model of psychosocial stress, has been shown to increase baseline Isc in both the jejunum and the colon compared to non-stressed animals.52 Interestingly, colonic tissues from stressed rats exhibited a reduced Isc response to the addition of cholinergic agonists and CRF, suggesting an impaired secretory response to incoming stressful stimuli. Mitochondrial activity was disturbed throughout the intestine, although mitochondrial response to CRF was preserved. These changes were associated with an increased expression of CRF1 receptor in the colon of stressed rats and colonic hyperalgesia.53 Several other studies using various stress models have reproduced the elevation of Isc in the colon and ileum of rodents and showed the involvement of CRF receptors.24,33,45,50,54–56
Both the acute intraperitoneal administration of CRF and chronic peripheral administration of CRF, the selective CRF1 receptor agonist stressin-1 and the selective CRF2 receptor ligand, Ucn3, increase the basal rat colonic Isc.33,57 Therefore, a role for both CRF receptor subtypes in this alteration is suggested, although the response is not reduced by the selective CRF2 receptor antagonist antisauvagine.57 Furthermore, elevated baseline Isc has been also observed in the jejunum of early-weaned pigs, while activation of mast cells and CRF induced elevations in Isc in the pig jejunum mounted in Ussing chambers. This elevation in Isc was inhibited using mast cell protease inhibitors.58 Experiments using selective CRF receptor antagonists reveal that CRF1 receptor activation mediates barrier dysfunction and hypersecretion in the porcine intestine in response to early life stress.58
Apart from ex vivo and in vivo studies, convincing evidence for a direct effect of CRF peptides on intestinal epithelial secretory response comes from in vitro work showing a consistent increase in Isc induced by CRF in the rat colon.33,37,59 Interestingly, maximal Isc increments were obtained with sauvagine, a CRF agonist with high affinity to both CRF receptors, at doses 200–1000 fold lower than CRF, suggesting a predominant CRF2 receptor effect.59 In addition, the effect of peripheral CRF on Isc increase in rat colonic tissue implicates mast cells, and nicotinic and muscarinic receptors, as established by the pharmacological blockade of specific receptors and the use of mast cell deficient rats.37,57 Other studies performed in the guinea-pig support the ample distribution of CRF1 receptor, but not CRF2 receptor throughout the myenteric and submucosal plexuses of the gastrointestinal tract.60 However, all CRF and Ucn1, Ucn2, and Ucn3 were able to increase the excitability of neurons from the enteric nervous system in vitro.61
Experimental studies in humans reveal that acute physical or psychological stress modulate the intestinal barrier. More than 20 years ago, Barclay and Turnberg et al,62,63 using segmental perfusion techniques in the human jejunum, showed that acute stress reduced net water absorption or increased secretion, supporting the role of the central and the autonomic nervous system in the control of intestinal function. In particular, a reduction in water absorption coupled with net sodium/chloride secretion was observed in healthy subjects subjected to psychological stress induced by dichotomous listening.62,63 Later, Santos et al64 showed that cold pain stress increased jejunal water secretion in healthy subjects and in patients with food allergy. These observations have been confirmed and extended recently: using the cold press-or test. The increase in intestinal water secretion during cold pain stress was higher in healthy female volunteers with lower background stress levels, yet blunted in those with elevated background stress.65 These results suggest that chronic life stress could lead to the loss of regulatory mechanisms in healthy individuals, as previously described in the jejunum of chronic stressed rats after neural stimulation.50 CRF1 receptor is expressed throughout the gastrointestinal tract in healthy subjects, and located in the lamina propria, mostly in macrophages, epithelial cells and enteric neurons, with the highest levels in the ileum and rectum and the lowest level in the colon.66 CRF2 receptors are located in the lamina propria and in the epithelial cells of the distal/sigmoid biopsy samples in healthy subjects.67 In contrast to animal studies, the addition of CRF to human colonic biopsies from healthy individuals mounted in Ussing chambers did not show any effect on Isc.68
Permeability
Numerous studies demonstrate the enhancement of intestinal permeability by acute and chronic stressors. In rodents, acute or subchronic stressors, including restraint stress, cold restraint stress, WAS, mild noise stress, and mixed restraint and acoustic stress, increased tissue conductance, and the fluxes of 3H mannitol,51 Cr-labeled EDTA, horseradish peroxidase, in the jejunum, ileum, and colon.32,50,54,69–72 These results indicate the ability of stress to modulate paracellular and transcellular transport of ions, and small and large macromolecules. Multiple mechanisms have been invocated to explain stress-mediated transport abnormalities. The list includes acetylcholine release, histamine, glucagon-like peptide-2, myosin light chain kinase, cytokines such as interferon-γ, interleukin (IL)-4 and IL-13, and mast cell activation, among the most relevant.32,61,71,73–75 Moreover, increased intestinal permeability, measured by lactulose, mannitol and sucralose ratios, was found in rats’ small intestine, following acute swimming stress.23 This increase was glucocorticoid-mediated because adrenalectomy and pharmacologic blockade of glucocorticoid receptors inhibited the response, and dexamethasone increased gastrointestinal permeability in control rats.23
Similarly, rats models of chronic stress (maternal deprivation,55,77–79 WAS,45 and crowding stress52) also show increased ionic permeability, and macromolecular permeability throughout the intestine. The increase was mediated partly by mechanisms including, muscarinic and nicotinic pathways, activation and number of mast cells and the release of nerve growth factor.79 Stress-induced enhancement of colonic permeability was mimicked by exogenous administration of CRF,33 and abolished by pretreatment with the peripheral administration of the non-selective CRF antagonists astressin or α-helical CRF9–41.37,55,80 Likely, the selective CRF1 receptor agonist, cortagine,48 the selective CRF1 receptor antagonist, SSR-125543,80 and the selective CRF2 receptor antagonist, antisauvagine-30,78 reduced the response, supporting the participation of both CRF receptors in the modulation of colonic permeability.
More recently, studies in several cultured epithelial cell lines, including intestinal human HT-29 cells, showed that CRF induced the upregulation of the endotoxin receptor, toll-like receptor 4 (TLR4), and that pretreatment with the CRF2 receptor antagonist, antalarmin, abrogated the response. The concomitant presence of CRF and lipopolysaccharide increased permeability to horseradish peroxidase and decreased transepithelial resistance. This effect was abolished by the CRF2 receptor antagonist, astressin2-B, and was mediated through the upregulation of claudin-2. Similarly, the expression of TLR4 and claudin-2 increased in the small and large intestine of pregnant mice submitted to 10 days of WAS, as was enhanced the permeability to horseradish peroxidase, and the effect abolished by α-helical CRF9–4181 and anti-claudin antibodies. Interestingly, rats submitted to WAS for 10 days, showed higher sensitization to orally-delivered horse-radish peroxidase, as shown by enhanced intestinal permeability upon antigen re-exposure. This effect was prevented by CRF blockade with by α-helical CRF9–41.82
Another line of evidence in animal models highlights the relevance of stress-CRF-mast cell axis in the regulation of intestinal permeability. Elevation of intestinal permeability, in response to restraint stress or intraperitoneal administration of CRF, was reduced or abolished after pretreatment with doxantrazole.59 Similarly, pharmacological inhibition of mast cell activation has been shown to inhibit stress-induced increased intestinal permeability in different animal models.37,58,59,83 Stress/CRF-induced changes in the rat intestinal permeability were also significantly reduced in tissues from mast-cell deficient rats.45,51,59,84 Teitelbaum et al57 also found CRF to cause mast cell hyperplasia and abnormal bacterial attachment and/or penetration into the rat mucosa except in mast-cell deficient rats. The authors revealed that stimulation of CRF1 receptor induced an elevated secretory state, while CRF2 receptor stimulation was associated with permeability dysfunction.57 Although it is clear that mast cell activation disrupts intestinal barrier and increases intestinal permeability, the ultimate mechanisms remain to be elucidated. In this sense, several mast cell mediators have been involved. Tumor necrosis factor-α (TNF-α) has been shown to increase intestinal permeability through nuclear factor-kappa B activation in association with nuclear factor-kappa B-dependent downregulation of zona occludens protein-1 expression and alteration in junctional localization in Caco-2 cells,85 and through myosin light chain kinase phosphorylation.86 More recently, using a porcine ex vivo intestinal model, Overman et al87 found that CRF increased intestinal paracellular permeability via mast cell dependent release of TNF-α and proteases. On the other hand, the tryptase released by mast cells upon activation has been shown to induce TJs disassembly through the activation of proteinase-activated receptor-2 of the epithelial cells.88–90 These receptors can modulate enteric neurotransmission, secretion, motility, epithelial permeability, and visceral sensitivity, and are also known to regulate intestinal inflammation.91 Anatomical contacts between mast cells and enteric nerve fibers have been demonstrated in the human gastrointestinal mucosa and inflammation multiplies these contacts.92,93 Mast cells communicate, bidirectionally, with both the enteric, autonomic and central nervous system through mast cell mediators and neuropeptides.94 In fact, human mast cells synthesize and secrete both CRF and Ucn in response to immunoglobulin E receptor activation.95 Mast cells also express CRF receptors, whose activation leads to the release of cytokines and other pro-inflammatory mediators. CRF enhances the trans-cellular uptake of macromolecules in the human colonic mucosa in vitro, via CRF receptor subtypes CRF1 and CRF2 expressed on subepithelial mast cells.58 CRF1 and CRF2 receptors have been described in human umbilical cord blood-derived mast cells, while only CRF1 receptor has been found in the human leukemic mast cell HMC-1 line. CRF stimulation induces the secretion of vascular endothelial growth factor without tryptase, histamine, IL-6, IL-8, or TNF-α release through CRF1 receptor.96 More recently, acute stress- induced bladder vascular permeability and vascular endothelial growth factor release have been shown to be dependent on CRF2 receptor.97
It is important to note here the ability of eosinophils to alter intestinal permeability and the mechanisms and mediators involved.98 Barrier function has been shown to be affected by eosinophil-derived major basic protein (MBP) through downregulation of occludin in a mast cell independent fashion.98 The neuropeptide substance P (SP) has been found to induce the release of vasoactive mediators from mast cells, macrophages, and T cells, contributing to chloride secretion, enhanced intestinal permeability, and vascular leakiness.99,100 SP increases the expression of CRF1 receptor in mast cells, and in turn, CRF induces the expression of the specific receptor neurokinin (NK)-1.101 More recently, psychological stress, through SP release, mediated stress-induced CRF expression in mice eosinophils and eosinophil-derived CRF was responsible for mast cell activation and epithelial barrier dysfunction. In this work, a cell line of eosinophils was treated with a number of stress mediators, but only SP induced CRF release via NK-1 and NK-2. Moreover, priming of eosinophils with SP resulted in mast cell activation through eosinophil-derived CRF that in turn induced intestinal barrier dysfunction.102 Wallon et al83 examined non-inflamed colonic mucosal biopses from patients with ulcerative colitis and found that eosinophils displayed immunoreactivity to CRF. In addition, in co-culture studies, carbachol activation of eosinophils induced CRF release and subsequent activation of mast cells, which increased permeability of epithelial cells to macromolecules.83 Similar to mast cells, eosinophils have also been shown to localize close to airway nerve terminals in patients with asthma as well as in animal models of bronchial hyperreactivity.103,104 This proximity to nerve terminals is described in certain digestive disorders,105,106 providing the anatomical substrate to understand the relevance of the mast cell-eosinophil-stress/CRF axis in the regulation of epithelial permeability and the initiation of immune and inflammatory diseases.
Stress-induced increase in gut paracellular permeability has also been shown to depend on CRF1 receptor-mediated mast cell release of nerve growth factor (NGF). Maternal deprivation has been shown to enhance colon permeability in association with elevated NGF expression.76 A subsequent study from the same group showed that CRF, acting through its receptor CRF1 receptor, stimulated NGF release from mast cells, which in turn increased gut paracellular permeability.80 Dendritic cells are relevant for the regulation of intestinal immune function and permeability through CRF production, a process augmented by commensal bacteria.107 Similarly, CRF1 and CRF2 receptor agonists exert a biphasic effect on macrophages. During the early stages of the inflammatory response, they suppress TNF-α release via induction of cyclooxygenase-2/prostaglandin E2 while later on they induce TNF-α transcription.108 Unfortunately, the role of CRF-mediated activation of macrophages and dendritic cells in stress-related intestinal barrier dysfunction is largely ignored.
Vanuytsel et al38 have recently shown that, both psychological stress (public speech) and a single intravenous bolus of CRF (100 μg) increased small intestinal permeability in healthy humans, measured by the lactulose/mannitol ratio. Two weeks pretreatment with 800 mg/day of the mast cell stabilizer, disodium cromoglycate, blocked the effect of both stress and CRF, invoking the participation of the CRF-mast cell axis in this response.38 We have also observed in healthy volunteers that cold pain stress enhanced both the blood-to-lumen albumin65 ratio and the blood-to-lumen mannitol and xylose permeability.109 This response was mainly observed in females with higher background stress levels, suggesting an impaired epithelial response to incoming stressful stimuli in this group. In addition, acute cold stress was shown to induce a significant release of α-defensin in the jejunum in this study, supporting the possibility that stress might affect this protective pathway in the gut, as have been shown in the skin.110 Furthermore, we have also found that cold stress evoked a differential gender-determined increase in human intestinal macromolecular permeability.111 This enhanced permeability could lead to excessive uptake of luminal antigens and bacterial products that may initiate an inflammatory response in the mucosa.112 Other studies showing the effect of stress and CRF on intestinal and extra-intestinal permeability are shown in Tables 1 and 2, respectively.
Table 1.
Studies Showing the Effect of Stress/Corticotropin-releasing Factor on Intestinal Permeability
| Author | Permeability assessment methods | Stress model | Results |
|---|---|---|---|
| Santos et al,37 1999 | Ussing chambers measuring conductance (G), short-current circuit (Isc) and horseradish peroxidase (HRP) flux in rat colon | Restraint stress and corticotrophin-releasing factor (CRF) administration | Restraint stress increased colonic ion secretion and permeability to ions, bacterial peptide peptide N-formyl-methionyl-leucyl-phenylalanine (fMLP), and HRP. These changes were prevented by alpha-helical CRF9–41 and mimicked by CRF administration. Pre-treatment with hexamethonium, bretylium and doxantrazole also prevented CRF-induced changes in ion secretion and G. |
| Saunders et al,33 2002 | Ussing chambers measuring G, and HRP flux in rat colon | Cold-restraint and water avoidance stress (WAS), and CRF administration | Cold-restraint stress, and WAS significantly elevated G and HRP flux. CRF mimicked the stress responses. Alpha-helical CRF9–41 inhibited the stress-induced abnormalities. |
| Guilarte et al,164 2004 | Albumin release to the intestinal lumen in healthy volunteers and irritable bowel syndrome | CRF administration | CRF induced a significant increase in albumin release to the intestinal lumen. |
| Gareau et al,180 2006 | Ussing chambers measuring G, and Isc in rat colon | Neonatal maternal separation. | Neonatal maternal separation stress increased plasmatic corticosterone, enhanced ion secretion, macromolecular permeability, bacteria adhering, and penetration into the colonic epithelium. Alpha-helical CRF9–41 reversed stress-induced effects. |
| Yang et al,82 2006 | Ussing chambers measuring G, Isc and HRP flux in rat jejunum | WAS and oral HRP sensitization | Antigen challenge induced a rapid ion secretory response and an increase in G only in rats submitted to WAS. These effects were reversed by alpha-helical CRF9–41. |
| Gareau et al,78 2007 | Ussing chambers measuring HRP flux in rat colon | Neonatal maternal separation | Neonatal maternal separation stress increased HRP flux. The enhanced flux was inhibited by atropine and hexamethonium. Alpha-helical CRF9–41 and antisauvagine-30 inhibited stress-induced increase in HRP flux. |
| Santos et al,59 2008 | Ussing chambers measuring Isc and HRP flux in rat colon | CRF and sauvagine exposure | Sauvagine and CRF induced a dose-dependent increase in Isc and HRP flux and an enhancement in protease II pre-treatment with astressin, and doxantrozole inhibited this response. Mast-cell deficient mice displayed a reduced epithelial response to stress peptides. |
| Teitelbaum et al,57 2008 | Ussing chambers measuring G, Isc and HRP flux in rat colon | CRF administration | Chronic CRF administration increased Isc, G, and HRP flux, but not in mast-cell deficient rats. CRF administration induced mast cell hyperplasia and abnormal bacterial attachment into the mucosa that was absent in mast-cell deficient rats. |
| Alonso et al,65 2008 | Albumin release to the intestinal lumen in healthy volunteers | Cold Pain Stress | Cold pain stress induced a significant increase in albumin release to the intestinal lumen. |
| Wallon et al,68 2008 | Ussing chambers measuring Isc, HRP flux, 51Cr-EDTA, and transepithelial resistance (TER) in human colon | CRF administration | CRF increased permeability to HRP. The increased permeability to HRP was abolished by alpha-helical CRF9–41, and lodoxamide pre-treatment. |
| Larauche et al,48 2009 | Evans blue extravasation in rat colon | Cortagine administration | Cortagine induced a significantly increased intestinal permeability. Astressin-B abolished the cortagine-induced increase in intestinal permeability. |
| Zheng et al,102 2009 | Ussing chambers measuring Isc, HRP flux, and TER in mouse jejunum | Restraint stress and substance P (SP) exposure | SP stimulation induced a significant increase in Isc and HRP flux in stressed mice. Those changes were lower in mast cell-deficient mice. Alpha-helical CRF9–41, inhibited SP-induced intestinal barrier dysfunction. |
| Smith et al,58 2010 | Ussing chambers measuring Isc, 3H mannitol flux, 14C inulin flux, and TER in pig jejunum and colon | Early weaning | Early weaning reduced jejunal TER and enhanced Isc and mucosal-to-serosal flux of 3H mannitol and 14C inulin in association with increased lamina propria mast cell density. Sodium cromoglycolate ameliorated barrier dysfunction and hypersecretion in early-weaned pigs. C48/80 and CRF exposure increased Isc and induced intestinal barrier dysfunction that were inhibited with mast cell protease inhibitors. |
| Keita et al,181 2010 | Ussing chambers measuring G, Isc, HRP flux, 51Cr-EDTA, and Escherichia coli K-12 flux in rat follicle-associated epithelium (FAE) and villus epithelium (VE) from rat ileum | WAS | WAS increased G, Isc, HRP and E. Coli uptake in FAE and VE. SP increased bacterial and 51Cr-EDTA intestinal permeability. These results were mimicked by CRF and carbachol and reduced by doxantrazole, CRF receptor antagonist and atropine. |
| Wallon et al,83 2011 | Ussing chambers measuring Isc, HRP flux, 51Cr-EDTA, fluorescein isothiocyanate (FITC)-Dextran 4000, and TER in non inflamed human colon biopsies from ulcerative colitis patients | None | HRP flux, TER, and Isc were increased in mucosa from patients with UC. Alpha-helical CRF9–41, atropine and lodoxamide reversed the increase in intestinal permeability. |
| Alonso et al,111 2012 | Albumin release to the intestinal lumen in healthy volunteers | Cold Pain Stress | Cold pain stress induced a significant increase in albumin release to the intestinal lumen. |
| Ait-Belgnaoui et al,182 2012 | Ussing chambers measuring FITC-Dextran flux in rat colon | Partial restraint stress | Stress increased plasma ACTH and corticosterone, and hypothalamic CRF and enhanced colonic paracellular permeability. Probiotic treatment prevented stress-induced increased intestinal permeability. |
| Overman et al,87 2012 | Ussing chambers measuring FITC-Dextran flux in porcine ileum | CRF exposure | CRF increased paracellular FITC-Dextran flux. Pre-treatment with astressin-B, sodium cromolyn, anti-TNF-α antibodies, protease inhibitors, and tetrodotoxin inhibited CRF-mediated intestinal barrier dysfunction. |
| Vicario et al,53 2012 | Ussing chambers measuring G and Isc in rat colon | Crowding stress and CRF administration | Crowding stress significantly increased G and Isc and CRFR1 in the rat colon. CRF administration mimicked stress-induced epithelial dysfunction. |
| Hill LT et al,183 2013 | Lactulose-mannitol urinary excretion test in shocked patients undergoing small bowel resection during emergency laparotomy and patients undergoing elective hepatobiliary surgery | Shock and abdominal surgery | Shock was associated with increased intestinal permeability. Plasma CRF was significantly increased in the shocked patients. |
| Yu et al,81 2013 | HRP flux and TER in HT-29, T84, MDCK, and Caco2 monolayers Ussing chambers measuring G, Isc, and HRP flux in mouse colon | CRF exposure and WAS | WAS increased G and Isc and HRP flux, and this increase was higher after LPS stimulation. This response was abolished by pre-treatment with anti-claudin 2 (Cldn2) antibodies. Stress also increased the expression of Cldn2 and toll-like receptor-4 (TLR4) in mouse epithelium. Exposure to CRF induced Cldn2 and TLR4 expression in intestinal epithelial cells. |
| Vanuytsel et al,38 2014 | Lactulose-mannitol urinary excretion test in healthy volunteers | Indomethacin administration, public speech, CRF administration, and electroshock anticipation | Public speech and CRF administration increased intestinal permeability and salivary cortisol. Increased permeability after public speech was only present in subjects with a significant elevation of cortisol. Pre-treatment with disodium cromoglycate inhibited stress and CRF-induced increased intestinal permeability. |
Table 2.
Studies Showing the Effect of Stress/Corticotropin-releasing Factor on Extraintestinal Permeability
| Author | Permeability assessment methods | Stress model | Results |
|---|---|---|---|
| Wei et al,184 1986 | Evans blue extravasation in rat paw | Antidromic stimulation of the saphenous nerve in innervated rat paw | Corticotropin-releasing factor (CRF) inhibited neurogenic plasma extravasation in the innervated rat paw. This effect was independent of the hypothalamus or the adrenal gland. |
| Wei and Kiang,185 1987 | Evans-blue extravasation in rat trachea | Antidromic stimulation of the right vagus or exposure to dilute formalin vapors | CRF inhibited tracheal plasma protein extravasation. |
| Kiang et al,186 1987 | Evans-blue extravasation in rat paw | Immersion of rat’s paw in 48°C or 58°C water | CRF inhibited thermal injury-induced pasma extravasation and edema. |
| Wei et al,187 1988 | Fluid displacement method in rat paw | Immersion of anesthetized rat paw in 58°C water | CRF inhibited the progressive development of swelling, and reduced edema, epidermal necrosis and the disruption of tissue architecture produced by thermal injury. CRF effects were reverted by alpha-helical CRF9–41. |
| Tian and Wei,188 1989 | Changes in skin weight and Evans blue extravasation in rat paw | Anesthetized rat paw immersion in 12 N hydrochloric, 18 N sulfuric, or 14 N hydrofluoric acids | CRF reduced the skin acid-induced skin injury. |
| Wei and Kiang,189 1989 | Evans blue extravasation in rat paw | Anesthetized rat paw immersion in 48°C or 58°C and antidromic stimulation of the saphenous nerve | Sauvagine and CRF inhibited plasma extravasation induced by thermal and neurogenic injury. |
| Serda and Wei,190 1991 | Evans blue and Monastral extravasation in rat paw | Anesthetized rat paw immersion in 22% NaCl solution maintained at −20 ± 0.5°C. | CRF inhibited the acute inflammatory response of rat paw skin to cold injury. The anti-inflammatory effects of CRF were blocked by alpha-helical CRF9–41. |
| Wei and Gao,191 1991 | Monastral blue extravasation in rat paw | Mechanical injury to muscle produced by a midline surgical incision in the rectus abdominis or freeze injury to the cortex produced by applying a cold probe (−50°C) to the skull | CRF inhibited the leakage of small blood vessel due to muscle and brain injury. |
| Gao et al,192 1991 | Monastral blue extravasation in rat skin, muscle, trachea and esophagus | Substance P (SP) administration | SP induces plasma protein leakage in skin, muscle, trachea and esophagus. This effect was reverted by the treatment with CRF. |
| Kelley et al,193 1994 | Measurement of lung wet-to-dry ratios to asses mice pulmonary vascular leak | Lipopolysaccharide (LPS) administration | Pulmonary vascular leak, and leukocyte infiltration were significantly depressed by CRF treatment. |
| Yoshihara et al,194 1995 | Evans blue extravasation in Guinea pig trachea and main bronchi | Antigen challenge through inhalation of 5% ovalbumin in the presence of phosphoramidon | CRF reduced ovalbumin-induced plasma extravasation in guinea pig airways by inhibiting the release of tachykinins from primary sensory nerves. |
| Whitney et al,195 1997 | Comparison of rat preischemic amputated limb weight with weight after ischemia and reperfusion | Hind limb replantation | CRF inhibited the gain of weight by ischemia-reperfusion and alpha-helical CRF9–41 administration partially reversed this effect. |
| Theoharide et al,196 1998 | Evans blue vascular extravasation in the rat skin | CRF administration | CRF induced mast cell degranulation and increased capillary permeability, and the antalarmin blocked this effect. |
| Whitney et al,197 1998 | Comparision of rat pedicled hind limb weight with ischemic pedicled hind limb weight | Pedicled hind limb | CRF administration decreased limb weight gain. |
| Singh et al,198 1999 | Evans blue vascular extravasation in rat skin | Urocortin (Ucn) administration | Ucn induced rat skin mast cell degranulation and increased vascular permeability. Alpha-helical CRF9–41, antalarmin and astressin reverted this effect. |
| Rapallino et al,199 2001 | Ionic permeability of rabbit vestibular Deiters neurons membrane | Rotation platform | CRF blocked basal chloride permeation across the Deiters’ membranes and this effect was partially reversed by alpha-helical CRF9–41. |
| Esposito et al,200 2002 | 99Tc gluceptate extravasation in rat brain | Restraint stress | Acute stress and CRF paraventricular nucleus injection increased blood-brain-barrier 99Tc gluceptate extravasation. Antalarmin and cromolyn inhibited this effect. |
| Hendryk et al,201 2002 | Evans blue vascular extravasation in rat brain | Closing of both internal carotid arteries | CRF decreased the endothelial damage in the acute phase of the ischemia. |
| Huang et al,202 2002 | 99Tc gluceptate extravasation in mice skin and knee joints | Restraint stress | Vascular permeability to 99Tc, as well as local CRF levels, were increased by stress, but not in mast-cell deficient mice. |
| Lytinas et al,203 2003 | 99Tc gluceptate and Evans blue extravasation in rat skin | Restraint stress | Acute stress increased skin CRF and vascular permeability. These effects were inhibited by histamine-1 receptor antagonists. |
| Donelan et al,204 2006 | Evans blue extravasation in mice skin | CRF administration | CRF increased vascular permeability. The neurotensin blocker (SR48692) inhibited CRF effects. CRF-induced increased vascular permeability was absent in mast cell deficient mice. |
| Wu et al,205 2006 | Evans blue extravasation in the rat lung | Ucn aerosol inhalation | Ucn inhalation increased lung vascular permeability. Enhanced pulmonary vascular permeability induced by Ucn was markedly inhibited by pretreatment with cromolyn, and azelastine. |
| Cureton et al,206 2009 | Measurement o hydraulic and macromolecule permeability in rat mesenteric venules | LPS-induced systemic inflammation | LPS and Ucn incremented hydraulic permeability. CRF2 receptor blockade decreased the LPS-induced increase in hydraulic permeability. |
| Boucher et al,97 2010 | Evans blue extravasation in mice bladder | Restraint stress | Acute stress increased bladder vascular permeability. CRF2 receptor and astressin2-B inhibited this effect. |
| Song et al,207 2013 | Transepithelial resistance (TER) and permeability to horseradish peroxidase (HRP) in human endothelial cell monolayers (Hmvec) | CRF treatment | Exposure to CRF induced TNF-alpha release by CD14 effector cells, decreased TER and increased permeability to HRP in co-cultured Hmvec monolayers. |
| Wan et al,208 2013 | Crystal violet, FITC-Dextran and resistance in human umbilical vein endothelial cells (HUVEC) | Lipopolysaccharide treatment | Pretreatment of HUVECs with urocortin increased LPS-induced endothelial permeability by regulating the cadherin-catenin complex via CRF2 receptor. |
Clinical Consequences of Stress/ Corticotropin-releasing Factor-mediated Dysregulation of Gastrointestinal Permeability
The growing acknowledgment of the scientific community to the role of intestinal permeability in keeping health and well-being and its relation to the origin of digestive and extradigestive disorders is becoming more and more universal for clinicians. Increased permeability and breakdown of intestinal barrier have been implicated in the origin of gastrointestinal and liver disorders, including celiac disease,113 inflammatory bowel disease,114–118 food allergy,119 acute pancreatitis,120 irritable bowel syndrome (IBS),121,122 functional dyspepsia,123 infectious diarrheal syndromes,124 primary biliary cirrhosis, and primary sclerosing cholangitis,125 liver cirrhosis,126 alcoholic liver disease,127 liver encephalopathy,128 and gastroesophageal reflux disease,129–131 among others. However, whether enhanced gut permeability is an early manifestation of disease, a central step in disease pathogenesis, or a simple epiphenomenon, and its relationship with life stress in the clinical setting, remains to be elucidated. A few examples can illustrate this controversy.
Interestingly, life events may favor the clinical appearance of celiac disease,132 and cellular stress, through MHC class I chain related genes A and B and endoplasmic reticulum stress pathways, is linked to the disregulation of mucosal homeostasis.133,134 Early in the 80s, celiac patients were shown to display increased intestinal permeability that normalized after several months on a gluten-free diet.113 More precise in vitro investigations revealed that although strict gluten withdrawal restored intestinal histology, a subjacent defect in mucosal permeability, measured by cellobiose/mannitol ratio, was transiently induced by short exposure to gluten, suggesting that increased intestinal permeability in celiac disease could be a primary defect.135 Recently, this defect in intestinal permeability has been related to altered expression of TJ genes related to permeability, polarity, and cell proliferation in active celiac disease,136 partly through the activation of the zonulin pathway in a MyD88-dependent fashion.137,138 Again, the majority of genes returned to normal after 2 years of gluten eviction with the exception of PPP2R3A, possibly indicating a constitutive defect in these patients.136 Moreover, unlike celiac disease, gluten sensitivity is not associated with increased intestinal permeability.139
Increased intestinal permeability has also been described in patients with inflammatory bowel disease. Enhanced intestinal permeability in this population is considered an initial event because it is increased in first-degree relatives of Crohn’s disease patients.140,141 Several observations link clinical relapses to the increase in intestinal permeability142,143 and to life stress,144,145 partly through mast cell activation146 and the release of CRF from eosinophils83 and neighboring nerves.68 Moreover, inflammatory bowel disease patients show associations with genes involved in the regulation of intestinal barrier and various alterations of the transmembrane and intracytoplasmic proteins.147,148 In addition, increased CRF1 receptor66 and Ucn expression, but decreased CRF2 receptor67 expression have been shown in the colonic mucosa of active ulcerative colitis patients.149,150
Accumulating evidence also indicates that IBS is linked to abnormal intestinal permeability,151–153 CRF release and life stress154–157 in close association with low-grade mucosal inflammation and immune activation.158 Several groups have provided preliminary evidence linking clinical manifestations of IBS to structural abnormalities of the apical junctional complex in both the small159,160 and large bowel mucosa.81,161–163 Furthermore, unpublished observations from our group indicate that a single intravenous bolus of CRF (100 μg) increased intestinal permeability, measured as the blood-to-lumen albumin ratio, in healthy subjects and in IBS patients through mast cell activation.164
In the same line, increased intestinal permeability and stress/CRF axis have also been involved in the pathophysiology of food allergy, as these patients display an enhancement of intestinal permeability even in the absence of food allergens165 and stress facilitates sensitization to luminal antigens.82 In fact, patients following immunosuppressive treatment have been shown to develop new-onset food allergies that may be related to the increase in intestinal permeability induced by treatment.166
Many other stress-related conditions such as severe burn,167,168 hemorragic shock,169 chronic kidney disease,170 type 1 diabetes and the metabolic syndrome,171,172 neuropsychiatric disorders,173 autism,174 autoimmune thyroiditis,175 IgA nephropathy,176 patients with primary immunodeficiencies,177 and sepsis178 have been associated with increased intestinal permeability.
Conclusion
The ability of stress and peripheral CRF to affect intestinal epithelial function and, particularly, intestinal permeability, is well documented in human and several animal species. Interestingly, apart from the direct effects on the enterocytes, the stress-induced increase of intestinal permeability is mediated via recruitment and activation of mast cells, eosinophils, macrophages and other mononuclear cells, and implicates both CRFR1 and CRF2 receptors.28
There is abundant literature supporting the link between life stress and the origin and clinical course of several human disorders,179 however, the ultimate clinical relevance of stress-CRF-mediated dysregulation of gastrointestinal permeability, remains at present mostly intuitive, with few exceptions. More work in this area is needed to confirm the findings. In this sense, studies with CRF and related peptides and the development of new antagonists for human use, will offer the opportunity to test this hypoyhesis.
Figure.
Corticotropin-releasing factor actions on gastrointestinal permeability under stress conditions. JAM-A-B-C, junctional adhesion molecule A-B-C; SP, substance P; ACh, acetylcholine; MBP, major basic protein; CRF, corticotropin- releasing factor; CRF1, CRF receptor 1; CRF2, CRF receptor 2; PAR2, protease activated receptor 2.
Acknowledgments
We are grateful to Maite Casado for her helpful contribution to the figure design.
Footnotes
Financial support: This work supported in part by the Fondo de Investigación Sanitaria and Ciberehd, Instituto Carlos III, Subdirección General de Investigación Sanitaria, Ministerio de Ciencia e Innovación and Programa de Especialización e Infraestructuras Internacionales 2012 (EIC-EMBL-2011-0070, Bruno K Rodiño-Janeiro; PI12/00314, Carmen Alonso-Cotoner; CM08/00229, Beatriz Lobo; CM10/00155, Marc Pigrau; CP10/00502, PI13/00935 and The Rome Foundation Award 2013, María Vicario; PI11/00716 & CB06/04/0021, Javier Santos).
Conflicts of interest: None.
ORCID: Bruno K Rodiño-Janeiro, http://orcid.org/0000-0002-0633-6774; Carmen Alonso-Cotoner, http://orcid.org/0000-0002-3483-2919; Marc Pigrau, http://orcid.org/0000-0001-6801-3017; Beatriz Lobo, http://orcid.org/0000-0003-3391-7125; María Vicario, http://orcid.org/0000-0001-9622-3185; Javier Santos, http://orcid.org/0000-0002-4798-5033.
References
- 1.Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915–1920. doi: 10.1126/science.1104816. [DOI] [PubMed] [Google Scholar]
- 2.Wells JM, Rossi O, Meijerink M, van Baarlen P. Epithelial crosstalk at the microbiota-mucosal interface. Proc Natl Acad Sci USA. 2011;108(suppl 1):4607–4614. doi: 10.1073/pnas.1000092107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hooper LV, Macpherson AJ. Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol. 2010;10:159–169. doi: 10.1038/nri2710. [DOI] [PubMed] [Google Scholar]
- 4.Caricilli AM, Castoldi A, Câmara NOS. Intestinal barrier: a gentlemen’s agreement between microbiota and immunity. World J Gastrointest Pathophysiol. 2014;5:18–32. doi: 10.4291/wjgp.v5.i1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mazmanian SK, Round JL, Kasper DL. A microbial symbiosis factor prevents intestinal inflammatory disease. Nature. 2008;453:620–625. doi: 10.1038/nature07008. [DOI] [PubMed] [Google Scholar]
- 6.Söderholm JD, Perdue MH. Stress and gastrointestinal tract. II. Stress and intestinal barrier function. Am J Physiol Gastrointest Liver Physiol. 2001;280:G7–G13. doi: 10.1152/ajpgi.2001.280.1.G7. [DOI] [PubMed] [Google Scholar]
- 7.Cicchetti D, Cohen DJ, editors. Developmental psychopathology. 2nd ed. Hoboken: John Wiley & Sons; 2006. [Google Scholar]
- 8.Mawdsley JE, Rampton DS. Psychological stress in IBD: new insights into pathogenic and therapeutic implications. Gut. 2005;54:1481–1491. doi: 10.1136/gut.2005.064261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner JR. Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009;9:799–809. doi: 10.1038/nri2653. [DOI] [PubMed] [Google Scholar]
- 10.Kato LM, Kawamoto S, Maruya M, Fagarasan S. The role of the adaptive immune system in regulation of gut microbiota. Immunol Rev. 2014;260:67–75. doi: 10.1111/imr.12185. [DOI] [PubMed] [Google Scholar]
- 11.Wood JD. Neuropathophysiology of functional gastrointestinal disorders. World J Gastroenterol. 2007;13:1313–1332. doi: 10.3748/wjg.v13.i9.1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donelan J, Marchand JE, Kempuraj D, Papadopoulou N, Papaliodis D, Theoharides TC. Perifollicular and perivascular mouse skin mast cells express corticotropin-releasing hormone receptor. J Invest Dermatol. 2006;126:929–932. doi: 10.1038/sj.jid.5700153. [DOI] [PubMed] [Google Scholar]
- 13.Larauche M, Kiank C, Tache Y. Corticotropin releasing factor signaling in colon and ileum: regulation by stress and pathophysiological implications. J Physiol Pharmacol. 2009;60(suppl 7):33–46. [PMC free article] [PubMed] [Google Scholar]
- 14.Sansonetti PJ. War and peace at mucosal surfaces. Nat Rev Immunol. 2004;4:953–964. doi: 10.1038/nri1499. [DOI] [PubMed] [Google Scholar]
- 15.Brostoff J, Challacombe SJ. Food Allergy & Intolerance. London: Saunders (WB) Co Ltd (Elsevier Health Sciences); 2002. [Google Scholar]
- 16.Pastorelli L, De Salvo C, Mercado JR, Vecchi M, Pizarro TT. Central role of the gut epithelial barrier in the pathogenesis of chronic intestinal inflammation: lessons learned from animal models and human genetics. Front Immunol. 2013;4:280. doi: 10.3389/fimmu.2013.00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nusrat A, Turner JR, Madara JL. Molecular physiology and pathophysiology of tight junctions. IV. Regulation of tight junctions by extracellular stimuli: nutrients, cytokines, and immune cells. Am J Physiol Gastrointest Liver Physiol. 2000;279:G851–G857. doi: 10.1152/ajpgi.2000.279.5.G851. [DOI] [PubMed] [Google Scholar]
- 18.Ménard S, Cerf-Bensussan N, Heyman M. Multiple facets of intestinal permeability and epithelial handling of dietary antigens. Mucosal Immunol. 2010;3:247–259. doi: 10.1038/mi.2010.5. [DOI] [PubMed] [Google Scholar]
- 19.Chen HQ, Yang J, Zhang M. Lactobacillus plantarum ameliorates colonic epithelial barrier dysfunction by modulating the apical junctional complex and PepT1 in IL-10 knockout mice. Am J Physiol Gastrointest Liver Physiol. 2010;299:G1287–G1297. doi: 10.1152/ajpgi.00196.2010. [DOI] [PubMed] [Google Scholar]
- 20.Su L, Shen L, Clayburgh DR. Targeted epithelial tight junction dysfunction causes immune activation and contributes to development of experimental colitis. Gastroenterology. 2009;136:551–563. doi: 10.1053/j.gastro.2008.10.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alonso C, Vicario M, Pigrau M, Lobo B, Santos J. Intestinal barrier function and the brain-gut axis. Adv Exp Med Biol. 2014;817:73–113. doi: 10.1007/978-1-4939-0897-4_4. [DOI] [PubMed] [Google Scholar]
- 22.Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62:591–599. [PubMed] [Google Scholar]
- 23.Lambert GP. Stress-induced gastrointestinal barrier dysfunction and its inflammatory effects. J Anim Sci. 2009;87:E101–E108. doi: 10.2527/jas.2008-1339. [DOI] [PubMed] [Google Scholar]
- 24.Gareau MG, Silva MA, Perdue MH. Pathophysiological mechanisms of stress-induced intestinal damage. Curr Mol Med. 2008;8:274–281. doi: 10.2174/156652408784533760. [DOI] [PubMed] [Google Scholar]
- 25.Hart A, Kamm MA. Review article: mechanisms of initiation and perpetuation of gut inflammation by stress. Aliment Pharmacol Ther. 2002;16:2017–2028. doi: 10.1046/j.1365-2036.2002.01359.x. [DOI] [PubMed] [Google Scholar]
- 26.Hauger RL, Grigoriadis DE, Dallman MF, Plotsky PM, Vale WW, Dautzenberg FM. International Union of Pharmacology. XXXVI. Current status of the nomenclature for receptors for corticotropin-releasing factor and their ligands. Pharmacol Rev. 2003;55:21–26. doi: 10.1124/pr.55.1.3. [DOI] [PubMed] [Google Scholar]
- 27.Fekete EM, Zorrilla EP. Physiology, pharmacology, and therapeutic relevance of urocortins in mammals: ancient CRF paralogs. Front Neuroendocrinol. 2007;28:1–27. doi: 10.1016/j.yfrne.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiank C, Taché Y, Larauche M. Stress-related modulation of inflammation in experimental models of bowel disease and post-infectious irritable bowel syndrome: role of corticotropin-releasing factor receptors. Brain Behav Immun. 2010;24:41–48. doi: 10.1016/j.bbi.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.la Fleur SE, Wick EC, Idumalla PS, Grady EF, Bhargava A. Role of peripheral corticotropin-releasing factor and urocortin II in intestinal inflammation and motility in terminal ileum. Proc Natl Acad Sci USA. 2005;102:7647–7652. doi: 10.1073/pnas.0408531102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kokkotou E, Torres D, Moss AC, et al. Corticotropin-releasing hormone receptor 2-deficient mice have reduced intestinal inflammatory responses. J Immunol. 2006;177:3355–3361. doi: 10.4049/jimmunol.177.5.3355. [DOI] [PubMed] [Google Scholar]
- 31.Meddings JB, Swain MG. Environmental stress-induced gastrointestinal permeability is mediated by endogenous glucocorticoids in the rat. Gastroenterology. 2000;119:1019–1028. doi: 10.1053/gast.2000.18152. [DOI] [PubMed] [Google Scholar]
- 32.Kiliaan AJ, Saunders PR, Bijlsma PB, et al. Stress stimulates transepithelial macromolecular uptake in rat jejunum. Am J Physiol. 1998;275:G1037–G1044. doi: 10.1152/ajpgi.1998.275.5.G1037. [DOI] [PubMed] [Google Scholar]
- 33.Saunders PR, Santos J, Hanssen NP, Yates D, Groot JA, Perdue MH. Physical and psychological stress in rats enhances colonic epithelial permeability via peripheral CRH. Dig Dis Sci. 2002;47:208–215. doi: 10.1023/A:1013204612762. [DOI] [PubMed] [Google Scholar]
- 34.Liźko NN, Silov VM, Syrych GD. [Events in he development of dysbacteriosis of the intestines in man under extreme conditions] Nahrung. 1984;28:599–605. doi: 10.1002/food.19840280604. [German] [DOI] [PubMed] [Google Scholar]
- 35.Lyte M, Ernst S. Catecholamine induced growth of gram negative bacteria. Life Sci. 1992;50:203–212. doi: 10.1016/0024-3205(92)90273-R. [DOI] [PubMed] [Google Scholar]
- 36.Castagliuolo I, Lamont JT, Qiu B, et al. Acute stress causes mucin release from rat colon: role of corticotropin releasing factor and mast cells. Am J Physiol. 1996;271(5 Pt 1):G884–G892. doi: 10.1152/ajpgi.1996.271.5.G884. [DOI] [PubMed] [Google Scholar]
- 37.Santos J, Saunders PR, Hanssen NP, et al. Corticotropin-releasing hormone mimics stress-induced colonic epithelial pathophysiology in the rat. Am J Physiol. 1999;277(2 Pt 1):G391–G399. doi: 10.1152/ajpgi.1999.277.2.G391. [DOI] [PubMed] [Google Scholar]
- 38.Vanuytsel T, van Wanrooy S, Vanheel H, et al. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut. 2014;63:1293–1299. doi: 10.1136/gutjnl-2013-305690. [DOI] [PubMed] [Google Scholar]
- 39.Farhadi A, Banan A, Fields J, Keshavarzian A. Intestinal barrier: an interface between health and disease. J Gastroenterol Hepatol. 2003;18:479–497. doi: 10.1046/j.1440-1746.2003.03032.x. [DOI] [PubMed] [Google Scholar]
- 40.Liévin-Le Moal V, Servin AL. The front line of enteric host defense against unwelcome intrusion of harmful microorganisms: mucins, antimicrobial peptides, and microbiota. Clin Microbiol Rev. 2006;19:315–337. doi: 10.1128/CMR.19.2.315-337.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gibson P, Rosella O, Nov R, Young G. Colonic epithelium is diffusely abnormal in ulcerative colitis and colorectal cancer. Gut. 1995;36:857–863. doi: 10.1136/gut.36.6.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chatzaki E, Crowe PD, Wang L, Million M, Taché Y, Grigoriadis DE. CRF receptor type 1 and 2 expression and anatomical distribution in the rat colon. J Neurochem. 2004;90:309–316. doi: 10.1111/j.1471-4159.2004.02490.x. [DOI] [PubMed] [Google Scholar]
- 43.Castagliuolo I, Wershil BK, Karalis K, Pasha A, Nikulasson ST, Pothoulakis C. Colonic mucin release in response to immobilization stress is mast cell dependent. Am J Physiol. 1998;274(6 Pt 1):G1094–G1100. doi: 10.1152/ajpgi.1998.274.6.G1094. [DOI] [PubMed] [Google Scholar]
- 44.Pfeiffer CJ, Qiu B, Lam SK. Reduction of colonic mucus by repeated short-term stress enhances experimental colitis in rats. J Physiol Paris. 2001;95:81–87. doi: 10.1016/S0928-4257(01)00012-2. [DOI] [PubMed] [Google Scholar]
- 45.Söderholm JD, Yang PC, Ceponis P, et al. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123:1099–1108. doi: 10.1053/gast.2002.36019. [DOI] [PubMed] [Google Scholar]
- 46.Hirata T, Keto Y, Nakata M, et al. Effects of serotonin 5-HT3 receptor antagonists on stress-induced colonic hyperalgesia and diarrhoea in rats: a comparative study with opioid receptor agonists, a muscarinic receptor antagonist and a synthetic polymer. Neurogastroenterol Motil. 2008;20:557–565. doi: 10.1111/j.1365-2982.2007.01069.x. [DOI] [PubMed] [Google Scholar]
- 47.Saunders PR, Maillot C, Million M, Taché Y. Peripheral corticotropin-releasing factor induces diarrhea in rats: role of CRF1 receptor in fecal watery excretion. Eur J Pharmacol. 2002;435:231–235. doi: 10.1016/S0014-2999(01)01574-6. [DOI] [PubMed] [Google Scholar]
- 48.Larauche M, Gourcerol G, Wang L, et al. Cortagine, a CRF1 agonist, induces stresslike alterations of colonic function and visceral hypersensitivity in rodents primarily through peripheral pathways. Am J Physiol Gastrointest Liver Physiol. 2009;297:G215–G227. doi: 10.1152/ajpgi.00072.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuan PQ, Million M, Wu SV, Rivier J, Taché Y. Peripheral corticotropin releasing factor (CRF) and a novel CRF1 receptor agonist, stressin1-A activate CRF1 receptor expressing cholinergic and nitrergic myenteric neurons selectively in the colon of conscious rats. Neurogastroenterol Motil. 2007;19:923–936. doi: 10.1111/j.1365-2982.2007.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saunders PR, Kosecka U, McKay DM, Perdue MH. Acute stressors stimulate ion secretion and increase epithelial permeability in rat intestine. Am J Physiol. 1994;267(5 Pt 1):G794–G799. doi: 10.1152/ajpgi.1994.267.5.G794. [DOI] [PubMed] [Google Scholar]
- 51.Santos J, Benjamin M, Yang PC, Prior T, Perdue MH. Chronic stress impairs rat growth and jejunal epithelial barrier function: role of mast cells. Am J Physiol Gastrointest Liver Physiol. 2000;278:G847–G854. doi: 10.1152/ajpgi.2000.278.6.G847. [DOI] [PubMed] [Google Scholar]
- 52.Vicario M, Guilarte M, Alonso C, et al. Chronological assessment of mast cell-mediated gut dysfunction and mucosal inflammation in a rat model of chronic psychosocial stress. Brain Behav Immun. 2010;24:1166–1175. doi: 10.1016/j.bbi.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 53.Vicario M, Alonso C, Guilarte M, et al. Chronic psychosocial stress induces reversible mitochondrial damage and corticotropin-releasing factor receptor type-1 upregulation in the rat intestine and IBS-like gut dysfunction. Psychoneuroendocrinology. 2012;37:65–77. doi: 10.1016/j.psyneuen.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 54.Cameron HL, Perdue MH. Stress impairs murine intestinal barrier function: improvement by glucagon-like peptide-2. J Pharmacol Exp Ther. 2005;314:214–220. doi: 10.1124/jpet.105.085373. [DOI] [PubMed] [Google Scholar]
- 55.Söderholm JD, Yates DA, Gareau MG, Yang PC, MacQueen G, Perdue MH. Neonatal maternal separation predisposes adult rats to colonic barrier dysfunction in response to mild stress. Am J Physiol Gastrointest Liver Physiol. 2002;283:G1257–G1263. doi: 10.1152/ajpgi.00314.2002. [DOI] [PubMed] [Google Scholar]
- 56.Zareie M, Johnson-Henry K, Jury J, et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut. 2006;55:1553–1560. doi: 10.1136/gut.2005.080739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Teitelbaum AA, Gareau MG, Jury J, Yang PC, Perdue MH. Chronic peripheral administration of corticotropin-releasing factor causes colonic barrier dysfunction similar to psychological stress. Am J Physiol Gastrointest Liver Physiol. 2008;295:G452–G459. doi: 10.1152/ajpgi.90210.2008. [DOI] [PubMed] [Google Scholar]
- 58.Smith F, Clark JE, Overman BL, et al. Early weaning stress impairs development of mucosal barrier function in the porcine intestine. Am J Physiol Gastrointest Liver Physiol. 2010;298:G352–G363. doi: 10.1152/ajpgi.00081.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Santos J, Yates D, Guilarte M, Vicario M, Alonso C, Perdue MH. Stress neuropeptides evoke epithelial responses via mast cell activation in the rat colon. Psychoneuroendocrinology. 2008;33:1248–1256. doi: 10.1016/j.psyneuen.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 60.Liu S, Gao X, Gao N, et al. Expression of type 1 corticotropin-releasing factor receptor in the guinea pig enteric nervous system. J Comp Neurol. 2005;481:284–298. doi: 10.1002/cne.20370. [DOI] [PubMed] [Google Scholar]
- 61.Liu S, Ren W, Qu MH, et al. Differential actions of urocortins on neurons of the myenteric division of the enteric nervous system in guinea pig distal colon. Br J Pharmacol. 2010;159:222–236. doi: 10.1111/j.1476-5381.2009.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barclay GR, Turnberg LA. Effect of psychological stress on salt and water transport in the human jejunum. Gastroenterology. 1987;93:91–97. doi: 10.1016/0016-5085(87)90319-2. [DOI] [PubMed] [Google Scholar]
- 63.Barclay GR, Turnberg LA. Effect of cold-induced pain on salt and water transport in the human jejunum. Gastroenterology. 1988;94:994–998. doi: 10.1016/0016-5085(88)90558-6. [DOI] [PubMed] [Google Scholar]
- 64.Santos J, Bayarri C, Saperas E, et al. Characterisation of immune mediator release during the immediate response to segmental mucosal challenge in the jejunum of patients with food allergy. Gut. 1999;45:553–558. doi: 10.1136/gut.45.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alonso C, Guilarte M, Vicario M, et al. Maladaptive intestinal epithelial responses to life stress may predispose healthy women to gut mucosal inflammation. Gastroenterology. 2008;135:163–172. e1. doi: 10.1053/j.gastro.2008.03.036. [DOI] [PubMed] [Google Scholar]
- 66.Yuan PQ, Wu SV, Elliott J, et al. Expression of corticotropin releasing factor receptor type 1 (CRF1) in the human gastrointestinal tract and upregulation in the colonic mucosa in patients with ulcerative colitis. Peptides. 2012;38:62–69. doi: 10.1016/j.peptides.2012.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chatzaki E, Anton PA, Million M, et al. Corticotropin-releasing factor receptor subtype 2 in human colonic mucosa: down-regulation in ulcerative colitis. World J Gastroenterol. 2013;19:1416–1423. doi: 10.3748/wjg.v19.i9.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wallon C, Yang PC, Keita AV, et al. Corticotropin-releasing hormone (CRH) regulates macromolecular permeability via mast cells in normal human colonic biopsies in vitro. Gut. 2008;57:50–58. doi: 10.1136/gut.2006.117549. [DOI] [PubMed] [Google Scholar]
- 69.Bijlsma PB, van Raaij MT, Dobbe CJ, et al. Subchronic mild noise stress increases HRP permeability in rat small intestine in vitro. Physiol Behav. 2001;73:43–49. doi: 10.1016/S0031-9384(01)00424-3. [DOI] [PubMed] [Google Scholar]
- 70.Demaude J, Salvador-Cartier C, Fioramonti J, Ferrier L, Bueno L. Phenotypic changes in colonocytes following acute stress or activation of mast cells in mice: implications for delayed epithelial barrier dysfunction. Gut. 2006;55:655–661. doi: 10.1136/gut.2005.078675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saunders PR, Hanssen NP, Perdue MH. Cholinergic nerves mediate stress-induced intestinal transport abnormalities in Wistar-Kyoto rats. Am J Physiol. 1997;273(2 Pt 1):G486–G490. doi: 10.1152/ajpgi.1997.273.2.G486. [DOI] [PubMed] [Google Scholar]
- 72.Kuge T, Greenwood-Van Meerveld B, Sokabe M. Stress-induced breakdown of intestinal barrier function in the rat: reversal by wood creosote. Life Sci. 2006;79:913–918. doi: 10.1016/j.lfs.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 73.Ferrier L, Mazelin L, Cenac N, et al. Stress-induced disruption of colonic epithelial barrier: role of interferon-gamma and myosin light chain kinase in mice. Gastroenterology. 2003;125:795–804. doi: 10.1016/S0016-5085(03)01057-6. [DOI] [PubMed] [Google Scholar]
- 74.Weber CR, Raleigh DR, Su L, et al. Epithelial myosin light chain kinase activation induces mucosal interleukin-13 expression to alter tight junction ion selectivity. J Biol Chem. 2010;285:12037–12046. doi: 10.1074/jbc.M109.064808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Santos J, Perdue MH. Stress and neuroimmune regulation of gut mucosal function. Gut. 2000;47(suppl 4):iv49–iv51. doi: 10.1136/gut.47.suppl_4.iv49. discussion iv52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Barreau F, Cartier C, Ferrier L, Fioramonti J, Bueno L. Nerve growth factor mediates alterations of colonic sensitivity and mucosal barrier induced by neonatal stress in rats. Gastroenterology. 2004;127:524–534. doi: 10.1053/j.gastro.2004.05.019. [DOI] [PubMed] [Google Scholar]
- 77.Barreau F, Ferrier L, Fioramonti J, Bueno L. Neonatal maternal deprivation triggers long term alterations in colonic epithelial barrier and mucosal immunity in rats. Gut. 2004;53:501–506. doi: 10.1136/gut.2003.024174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gareau MG, Jury J, Perdue MH. Neonatal maternal separation of rat pups results in abnormal cholinergic regulation of epithelial permeability. Am J Physiol Gastrointest Liver Physiol. 2007;293:G198–G203. doi: 10.1152/ajpgi.00392.2006. [DOI] [PubMed] [Google Scholar]
- 79.Kim YS, Lee MY, Ryu HS, et al. Regional differences in chronic stress-induced alterations in mast cell and protease-activated receptor-2-positive cell numbers in the colon of Ws/Ws Rats. J Neurogastroenterol Motil. 2014;20:54–63. doi: 10.5056/jnm.2014.20.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Barreau F, Cartier C, Leveque M, et al. Pathways involved in gut mucosal barrier dysfunction induced in adult rats by maternal deprivation: corticotrophin-releasing factor and nerve growth factor interplay. J Physiol. 2007;580(Pt 1):347–356. doi: 10.1113/jphysiol.2006.120907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yu Y, Liu Z-Q, Liu X-Y, et al. Stress-derived corticotropin releasing factor breaches epithelial endotoxin tolerance. PloS One. 2013;8:e65760. doi: 10.1371/journal.pone.0065760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yang PC, Jury J, Söderholm JD, Sherman PM, McKay DM, Perdue MH. Chronic psychological stress in rats induces intestinal sensitization to luminal antigens. Am J Pathol. 2006;168:104–114. doi: 10.2353/ajpath.2006.050575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wallon C, Persborn M, Jönsson M, et al. Eosinophils express muscarinic receptors and corticotropin-releasing factor to disrupt the mucosal barrier in ulcerative colitis. Gastroenterology. 2011;140:1597–1607. doi: 10.1053/j.gastro.2011.01.042. [DOI] [PubMed] [Google Scholar]
- 84.Santos J, Yang PC, Söderholm JD, Benjamin M, Perdue MH. Role of mast cells in chronic stress induced colonic epithelial barrier dysfunction in the rat. Gut. 2001;48:630–636. doi: 10.1136/gut.48.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ma TY, Iwamoto GK, Hoa NT, et al. TNF-alpha-induced increase in intestinal epithelial tight junction permeability requires NF-kappa B activation. Am J Physiol Gastrointest Liver Physiol. 2004;286:G367–G376. doi: 10.1152/ajpgi.00173.2003. [DOI] [PubMed] [Google Scholar]
- 86.Zolotarevsky Y, Hecht G, Koutsouris A, et al. A membrane-permeant peptide that inhibits MLC kinase restores barrier function in in vitro models of intestinal disease. Gastroenterology. 2002;123:163–172. doi: 10.1053/gast.2002.34235. [DOI] [PubMed] [Google Scholar]
- 87.Overman EL, Rivier JE, Moeser AJ. CRF induces intestinal epithelial barrier injury via the release of mast cell proteases and TNF-α. PloS One. 2012;7:e39935. doi: 10.1371/journal.pone.0039935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jacob C, Yang PC, Darmoul D, et al. Mast cell tryptase controls paracellular permeability of the intestine. Role of protease-activated receptor 2 and beta-arrestins. J Biol Chem. 2005;280:31936–31948. doi: 10.1074/jbc.M506338200. [DOI] [PubMed] [Google Scholar]
- 89.Gebhardt T, Gerhard R, Bedoui S, et al. Beta2-adrenoceptor-mediated suppression of human intestinal mast cell functions is caused by disruption of filamentous actin dynamics. Eur J Immunol. 2005;35:1124–1132. doi: 10.1002/eji.200425869. [DOI] [PubMed] [Google Scholar]
- 90.Goldblum SE, Rai U, Tripathi A, et al. The active Zot domain (aa 288–293) increases ZO-1 and myosin 1C serine/threonine phosphorylation, alters interaction between ZO-1 and its binding partners, and induces tight junction disassembly through proteinase activated receptor 2 activation. FASEB J. 2011;25:144–158. doi: 10.1096/fj.10-158972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vergnolle N. Clinical relevance of proteinase activated receptors (pars) in the gut. Gut. 2005;54:867–874. doi: 10.1136/gut.2004.048876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stead RH, Dixon MF, Bramwell NH, Riddell RH, Bienenstock J. Mast cells are closely apposed to nerves in the human gastrointestinal mucosa. Gastroenterology. 1989;97:575–585. doi: 10.1016/0016-5085(89)90627-6. [DOI] [PubMed] [Google Scholar]
- 93.Barbara G, Stanghellini V, De Giorgio R, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693–702. doi: 10.1053/j.gastro.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 94.Buhner S, Schemann M. Mast cell-nerve axis with a focus on the human gut. Biochim Biophys Acta. 2012;1822:85–92. doi: 10.1016/j.bbadis.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 95.Kempuraj D, Papadopoulou NG, Lytinas M, et al. Corticotropin-releasing hormone and its structurally related urocortin are synthesized and secreted by human mast cells. Endocrinology. 2004;145:43–48. doi: 10.1210/en.2003-0805. [DOI] [PubMed] [Google Scholar]
- 96.Cao J, Papadopoulou N, Kempuraj D, et al. Human mast cells express corticotropin-releasing hormone (CRH) receptors and CRH leads to selective secretion of vascular endothelial growth factor. J Immunol. 2005;174:7665–7675. doi: 10.4049/jimmunol.174.12.7665. [DOI] [PubMed] [Google Scholar]
- 97.Boucher W, Kempuraj D, Michaelian M, Theoharides TC. Corticotropin-releasing hormone-receptor 2 is required for acute stress-induced bladder vascular permeability and release of vascular endothelial growth factor. BJU Int. 2010;106:1394–1399. doi: 10.1111/j.1464-410X.2010.09237.x. [DOI] [PubMed] [Google Scholar]
- 98.Furuta GT, Nieuwenhuis EES, Karhausen J, et al. Eosinophils alter colonic epithelial barrier function: role for major basic protein. Am J Physiol Gastrointest Liver Physiol. 2005;289:G890–G897. doi: 10.1152/ajpgi.00015.2005. [DOI] [PubMed] [Google Scholar]
- 99.Koon HW, Pothoulakis C. Immunomodulatory properties of substance P: the gastrointestinal system as a model. Ann N Y Acad Sci. 2006;1088:23–40. doi: 10.1196/annals.1366.024. [DOI] [PubMed] [Google Scholar]
- 100.Wang L, Stanisz AM, Wershil BK, Galli SJ, Perdue MH. Substance P induces ion secretion in mouse small intestine through effects on enteric nerves and mast cells. Am J Physiol. 1995;269(1 Pt 1):G85–G92. doi: 10.1152/ajpgi.1995.269.1.G85. [DOI] [PubMed] [Google Scholar]
- 101.Asadi S, Alysandratos KD, Angelidou A, et al. Substance P (SP) induces expression of functional corticotropin-releasing hormone receptor-1 (CRHR-1) in human mast cells. J Invest Dermatol. 2012;132:324–329. doi: 10.1038/jid.2011.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zheng PY, Feng BS, Oluwole C, et al. Psychological stress induces eosinophils to produce corticotrophin releasing hormone in the intestine. Gut. 2009;58:1473–1479. doi: 10.1136/gut.2009.181701. [DOI] [PubMed] [Google Scholar]
- 103.Thornton MA, Akasheh N, Walsh MT, et al. Eosinophil recruitment to nasal nerves after allergen challenge in allergic rhinitis. Clin Immunol. 2013;147:50–57. doi: 10.1016/j.clim.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 104.Kingham PJ, Costello RW, McLean WG. Eosinophil and airway nerve interactions. Pulm Pharmacol Ther. 2003;16:9–13. doi: 10.1016/S1094-5539(02)00093-7. [DOI] [PubMed] [Google Scholar]
- 105.O’Brien LM, Fitzpatrick E, Baird AW, Campion DP. Eosinophil-nerve interactions and neuronal plasticity in rat gut associated lymphoid tissue (GALT) in response to enteric parasitism. J Neuroimmunol. 2008;197:1–9. doi: 10.1016/j.jneuroim.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 106.Bischoff SC, Gebhardt T. Role of mast cells and eosinophils in neuroimmune interactions regulating mucosal inflammation in inflammatory bowel disease. Adv Exp Med Biol. 2006;579:177–208. doi: 10.1007/0-387-33778-4_12. [DOI] [PubMed] [Google Scholar]
- 107.Hojo M, Ohkusa T, Tomeoku H, et al. Corticotropin-releasing factor secretion from dendritic cells stimulated by commensal bacteria. World J Gastroenterol. 2011;17:4017–4022. doi: 10.3748/wjg.v17.i35.4017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tsatsanis C, Androulidaki A, Dermitzaki E, Gravanis A, Margioris AN. Corticotropin releasing factor receptor 1 (CRF1) and CRF2 agonists exert an anti-inflammatory effect during the early phase of inflammation suppressing LPS-induced TNF-alpha release from macrophages via induction of COX-2 and PGE2. J Cell Physiol. 2007;210:774–783. doi: 10.1002/jcp.20900. [DOI] [PubMed] [Google Scholar]
- 109.Rezzi S, Martin FP, Alonso C, et al. Metabotyping of biofluids reveals stress-based differences in gut permeability in healthy individuals. J Proteome Res. 2009;8:4799–4809. doi: 10.1021/pr900525w. [DOI] [PubMed] [Google Scholar]
- 110.Aberg KM, Radek KA, Choi EH, et al. Psychological stress down-regulates epidermal antimicrobial peptide expression and increases severity of cutaneous infections in mice. J Clin Invest. 2007;117:3339–3349. doi: 10.1172/JCI31726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Alonso C, Guilarte M, Vicario M, et al. Acute experimental stress evokes a differential gender-determined increase in human intestinal macromolecular permeability. Neurogastroenterol Motil. 2012;24:740–746. e348–349. doi: 10.1111/j.1365-2982.2012.01928.x. [DOI] [PubMed] [Google Scholar]
- 112.Ando T, Rivier J, Yanaihara H, Arimura A. Peripheral corticotropin-releasing factor mediates the elevation of plasma IL-6 by immobilization stress in rats. Am J Physiol. 1998;275(5 Pt 2):R1461–R1467. doi: 10.1152/ajpregu.1998.275.5.R1461. [DOI] [PubMed] [Google Scholar]
- 113.Bjarnason I, Peters TJ. In vitro determination of small intestinal permeability: demonstration of a persistent defect in patients with coeliac disease. Gut. 1984;25:145–150. doi: 10.1136/gut.25.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sartor RB. Mechanisms of disease: pathogenesis of Crohn’s disease and ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol. 2006;3:390–407. doi: 10.1038/ncpgasthep0528. [DOI] [PubMed] [Google Scholar]
- 115.Clavel T, Haller D. Bacteria- and host-derived mechanisms to control intestinal epithelial cell homeostasis: implications for chronic inflammation. Inflamm Bowel Dis. 2007;13:1153–1164. doi: 10.1002/ibd.20174. [DOI] [PubMed] [Google Scholar]
- 116.Pearson AD, Eastham EJ, Laker MF, Craft AW, Nelson R. Intestinal permeability in children with Crohn’s disease and coeliac disease. Br Med J (Clin Res Ed) 1982;285:20–21. doi: 10.1136/bmj.285.6334.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bjarnason I, O’Morain C, Levi AJ, Peters TJ. Absorption of 51chromium-labeled ethylenediaminetetraacetate in inflammatory bowel disease. Gastroenterology. 1983;85:318–322. [PubMed] [Google Scholar]
- 118.Heller F, Florian P, Bojarski C, et al. Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterology. 2005;129:550–564. doi: 10.1016/j.gastro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 119.Järvinen KM, Konstantinou GN, Pilapil M, et al. Intestinal permeability in children with food allergy on specific elimination diets. Pediatr Allergy Immunol. 2013;24:589–595. doi: 10.1111/pai.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fishman JE, Levy G, Alli V, Zheng X, Mole DJ, Deitch EA. The intestinal mucus layer is a critical component of the gut barrier that is damaged during acute pancreatitis. Shock. 2014;42:264–270. doi: 10.1097/SHK.0000000000000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Camilleri M, Gorman H. Intestinal permeability and irritable bowel syndrome. Neurogastroenterol Motil. 2007;19:545–552. doi: 10.1111/j.1365-2982.2007.00925.x. [DOI] [PubMed] [Google Scholar]
- 122.Lee H, Park JH, Park DI, et al. Mucosal mast cell count is associated with intestinal permeability in patients with diarrhea predominant irritable bowel syndrome. J Neurogastroenterol Motil. 2013;19:244–250. doi: 10.5056/jnm.2013.19.2.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Vanheel H, Vicario M, Vanuytsel T, et al. Impaired duodenal mucosal integrity and low-grade inflammation in functional dyspepsia. Gut. 2014;63:262–271. doi: 10.1136/gutjnl-2012-303857. [DOI] [PubMed] [Google Scholar]
- 124.Gadewar S, Fasano A. Current concepts in the evaluation, diagnosis and management of acute infectious diarrhea. Curr Opin Pharmacol. 2005;5:559–565. doi: 10.1016/j.coph.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 125.Sakisaka S, Kawaguchi T, Taniguchi E, et al. Alterations in tight junctions differ between primary biliary cirrhosis and primary sclerosing cholangitis. Hepatology. 2001;33:1460–1468. doi: 10.1053/jhep.2001.25086. [DOI] [PubMed] [Google Scholar]
- 126.Pijls KE, Jonkers DM, Elamin EE, Masclee AA, Koek GH. Intestinal epithelial barrier function in liver cirrhosis: an extensive review of the literature. Liver Int. 2013;33:1457–1469. doi: 10.1111/liv.12271. [DOI] [PubMed] [Google Scholar]
- 127.Rao RK, Seth A, Sheth P. Recent advances in alcoholic liver disease I. Role of intestinal permeability and endotoxemia in alcoholic liver disease. Am J Physiol Gastrointest Liver Physiol. 2004;286:G881–G884. doi: 10.1152/ajpgi.00006.2004. [DOI] [PubMed] [Google Scholar]
- 128.Summa KC, Voigt RM, Forsyth CB, et al. Disruption of the circadian clock in mice increases intestinal permeability and promotes alcohol-induced hepatic pathology and inflammation. PloS One. 2013;8:e67102. doi: 10.1371/journal.pone.0067102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Li J, Brackbill RM, Stellman SD, et al. Gastroesophageal reflux symptoms and comorbid asthma and posttraumatic stress disorder following the 9/11 terrorist attacks on World Trade Center in New York City. Am J Gastroenterol. 2011;106:1933–1941. doi: 10.1038/ajg.2011.300. [DOI] [PubMed] [Google Scholar]
- 130.Farré R, Blondeau K, Clement D, et al. Evaluation of oesophageal mucosa integrity by the intraluminal impedance technique. Gut. 2011;60:885–892. doi: 10.1136/gut.2010.233049. [DOI] [PubMed] [Google Scholar]
- 131.Söderholm JD. Stress-related changes in oesophageal permeability: filling the gaps of GORD? Gut. 2007;56:1177–1180. doi: 10.1136/gut.2007.120691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ciacci C, Siniscalchi M, Bucci C, Zingone F, Morra I, Iovino P. Life events and the onset of celiac disease from a patient’s perspective. Nutrients. 2013;5:3388–3398. doi: 10.3390/nu5093388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Allegretti YL, Bondar C, Guzman L, et al. Broad MICA/B expression in the small bowel mucosa: a link between cellular stress and celiac disease. PloS One. 2013;8:e73658. doi: 10.1371/journal.pone.0073658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Caputo I, Secondo A, Lepretti M, et al. Gliadin peptides induce tissue transglutaminase activation and ER-stress through Ca2+ mobilization in Caco-2 cells. PloS One. 2012;7:e45209. doi: 10.1371/journal.pone.0045209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hamilton I, Cobden I, Rothwell J, Axon AT. Intestinal permeability in coeliac disease: the response to gluten withdrawal and single-dose gluten challenge. Gut. 1982;23:202–210. doi: 10.1136/gut.23.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Jauregi-Miguel A, Fernandez-Jimenez N, Irastorza I, Plaza-Izurieta L, Vitoria JC, Bilbao JR. Alteration of tight junction gene expression in celiac disease. J Pediatr Gastroenterol Nutr. 2014;58:762–767. doi: 10.1097/MPG.0000000000000338. [DOI] [PubMed] [Google Scholar]
- 137.Lammers KM, Lu R, Brownley J, et al. Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology. 2008;135:194–204. e3. doi: 10.1053/j.gastro.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wang W, Uzzau S, Goldblum SE, Fasano A. Human zonulin, a potential modulator of intestinal tight junctions. J Cell Sci. 2000;113(Pt 24):4435–4440. doi: 10.1242/jcs.113.24.4435. [DOI] [PubMed] [Google Scholar]
- 139.Sapone A, Lammers KM, Casolaro V, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med. 2011;9:23. doi: 10.1186/1741-7015-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hollander D, Vadheim CM, Brettholz E, Petersen GM, Delahunty T, Rotter JI. Increased intestinal permeability in patients with Crohn’s disease and their relatives. A possible etiologic factor. Ann Intern Med. 1986;105:883–885. doi: 10.7326/0003-4819-105-6-883. [DOI] [PubMed] [Google Scholar]
- 141.Kucharzik T, Walsh SV, Chen J, Parkos CA, Nusrat A. Neutrophil transmigration in inflammatory bowel disease is associated with differential expression of epithelial intercellular junction proteins. Am J Pathol. 2001;159:2001–2009. doi: 10.1016/S0002-9440(10)63051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.D’Incà R, Di Leo V, Corrao G, et al. Intestinal permeability test as a predictor of clinical course in Crohn’s disease. Am J Gastroenterol. 1999;94:2956–2960. doi: 10.1016/S0002-9270(99)00500-6. [DOI] [PubMed] [Google Scholar]
- 143.Arnott ID, Kingstone K, Ghosh S. Abnormal intestinal permeability predicts relapse in inactive Crohn disease. Scand J Gastroenterol. 2000;35:1163–1169. doi: 10.1080/003655200750056637. [DOI] [PubMed] [Google Scholar]
- 144.Singh S, Graff LA, Bernstein CN. Do NSAIDs, antibiotics, infections, or stress trigger flares in IBD? Am J Gastroenterol. 2009;104:1298–1313. doi: 10.1038/ajg.2009.15. [DOI] [PubMed] [Google Scholar]
- 145.Cámara RJ, Ziegler R, Begré S, Schoepfer AM, von Känel R, Swiss Inflammatory Bowel Disease Cohort Study (SIBDCS) group The role of psychological stress in inflammatory bowel disease: quality assessment of methods of 18 prospective studies and suggestions for future research. Digestion. 2009;80:129–139. doi: 10.1159/000226087. [DOI] [PubMed] [Google Scholar]
- 146.Farhadi A, Fields JZ, Keshavarzian A. Mucosal mast cells are pivotal elements in inflammatory bowel disease that connect the dots: stress, intestinal hyperpermeability and inflammation. World J Gastroenterol. 2007;13:3027–3030. doi: 10.3748/wjg.v13.i22.3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Merga Y, Campbell BJ, Rhodes JM. Mucosal barrier, bacteria and inflammatory bowel disease: possibilities for therapy. Dig Dis. 2014;32:475–483. doi: 10.1159/000358156. [DOI] [PubMed] [Google Scholar]
- 148.Fries W, Belvedere A, Vetrano S. Sealing the broken barrier in IBD: intestinal permeability, epithelial cells and junctions. Curr Drug Targets. 2013;14:1460–1470. doi: 10.2174/1389450111314120011. [DOI] [PubMed] [Google Scholar]
- 149.Moss AC, Anton P, Savidge T, et al. Urocortin II mediates pro-inflammatory effects in human colonocytes via corticotropin-releasing hormone receptor 2alpha. Gut. 2007;56:1210–1217. doi: 10.1136/gut.2006.110668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Saruta M, Takahashi K, Suzuki T, Torii A, Kawakami M, Sasano H. Urocortin 1 in colonic mucosa in patients with ulcerative colitis. J Clin Endocrinol Metab. 2004;89:5352–5361. doi: 10.1210/jc.2004-0195. [DOI] [PubMed] [Google Scholar]
- 151.Dunlop SP, Hebden J, Campbell E, et al. Abnormal intestinal permeability in subgroups of diarrhea-predominant irritable bowel syndromes. Am J Gastroenterol. 2006;101:1288–1294. doi: 10.1111/j.1572-0241.2006.00672.x. [DOI] [PubMed] [Google Scholar]
- 152.Mujagic Z, Ludidi S, Keszthelyi D, et al. Small intestinal permeability is increased in diarrhoea predominant IBS, while alterations in gastroduodenal permeability in all IBS subtypes are largely attributable to confounders. Aliment Pharmacol Ther. 2014;40:288–297. doi: 10.1111/apt.12829. [DOI] [PubMed] [Google Scholar]
- 153.Piche T, Barbara G, Aubert P, et al. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut. 2009;58:196–201. doi: 10.1136/gut.2007.140806. [DOI] [PubMed] [Google Scholar]
- 154.Taché Y, Martinez V, Wang L, Million M. CRF1 receptor signaling pathways are involved in stress-related alterations of colonic function and viscerosensitivity: implications for irritable bowel syndrome. Br J Pharmacol. 2004;141:1321–1330. doi: 10.1038/sj.bjp.0705760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Fukudo S. Role of corticotropin-releasing hormone in irritable bowel syndrome and intestinal inflammation. J Gastroenterol. 2007;42(suppl 17):48–51. doi: 10.1007/s00535-006-1942-7. [DOI] [PubMed] [Google Scholar]
- 156.Labus JS, Hubbard CS, Bueller J, et al. Impaired emotional learning and involvement of the corticotropin-releasing factor signaling system in patients with irritable bowel syndrome. Gastroenterology. 2013;145:1253–1261. e1–e3. doi: 10.1053/j.gastro.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut. 1998;43:256–261. doi: 10.1136/gut.43.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.O’Malley D, Quigley EM, Dinan TG, Cryan JF. Do interactions between stress and immune responses lead to symptom exacerbations in irritable bowel syndrome? Brain Behav Immun. 2011;25:1333–1341. doi: 10.1016/j.bbi.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 159.Martínez C, Lobo B, Pigrau M, et al. Diarrhoea-predominant irritable bowel syndrome: an organic disorder with structural abnormalities in the jejunal epithelial barrier. Gut. 2013;62:1160–1168. doi: 10.1136/gutjnl-2012-302093. [DOI] [PubMed] [Google Scholar]
- 160.Martínez C, Vicario M, Ramos L, et al. The jejunum of diarrhea-predominant irritable bowel syndrome shows molecular alterations in the tight junction signaling pathway that are associated with mucosal pathobiology and clinical manifestations. Am J Gastroenterol. 2012;107:736–746. doi: 10.1038/ajg.2011.472. [DOI] [PubMed] [Google Scholar]
- 161.Wilcz-Villega E, McClean S, O’Sullivan M. Reduced E-cadherin expression is associated with abdominal pain and symptom duration in a study of alternating and diarrhea predominant IBS. Neurogastroenterol Motil. 2014;26:316–325. doi: 10.1111/nmo.12262. [DOI] [PubMed] [Google Scholar]
- 162.Bertiaux-Vandaële N, Youmba SB, Belmonte L, et al. The expression and the cellular distribution of the tight junction proteins are altered in irritable bowel syndrome patients with differences according to the disease subtype. Am J Gastroenterol. 2011;106:2165–2173. doi: 10.1038/ajg.2011.257. [DOI] [PubMed] [Google Scholar]
- 163.Piche T. Tight junctions and IBS--the link between epithelial permeability, low-grade inflammation, and symptom generation? Neurogastroenterol Motil. 2014;26:296–302. doi: 10.1111/nmo.12315. [DOI] [PubMed] [Google Scholar]
- 164.Guilarte M, Santos J, Alonso C, et al. Corticotropin-releasing hormone (CRH) triggers jejunal mast cell and eosinophil activation in IBS patients. Gastroenterology. 2004;126(suppl 2):A38. [Google Scholar]
- 165.Ventura MT, Polimeno L, Amoruso AC, et al. Intestinal permeability in patients with adverse reactions to food. Dig Liver Dis. 2006;38:732–736. doi: 10.1016/j.dld.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 166.Ozdemir O, Arrey-Mensah A, Sorensen RU. Development of multiple food allergies in children taking tacrolimus after heart and liver transplantation. Pediatr Transplant. 2006;10:380–383. doi: 10.1111/j.1399-3046.2005.00474.x. [DOI] [PubMed] [Google Scholar]
- 167.Chen C, Wang P, Su Q, Wang S, Wang F. Myosin light chain kinase mediates intestinal barrier disruption following burn injury. PloS One. 2012;7:e34946. doi: 10.1371/journal.pone.0034946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Costantini TW, Peterson CY, Kroll L, et al. Role of p38 MAPK in burn-induced intestinal barrier breakdown. J Surg Res. 2009;156:64–69. doi: 10.1016/j.jss.2009.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Li Y, Guo M, Shen J, et al. Limited fluid resuscitation attenuates lung and intestine injury caused by hemorrhagic shock in rats. J Invest Surg. 2014;27:81–87. doi: 10.3109/08941939.2013.837991. [DOI] [PubMed] [Google Scholar]
- 170.Vaziri ND, Yuan J, Norris K. Role of urea in intestinal barrier dysfunction and disruption of epithelial tight junction in chronic kidney disease. Am J Nephrol. 2013;37:1–6. doi: 10.1159/000345969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Bekkering P, Jafri I, van Overveld FJ, Rijkers GT. The intricate association between gut microbiota and development of type 1, type 2 and type 3 diabetes. Expert Rev Clin Immunol. 2013;9:1031–1041. doi: 10.1586/1744666X.2013.848793. [DOI] [PubMed] [Google Scholar]
- 172.Watts T, Berti I, Sapone A, et al. Role of the intestinal tight junction modulator zonulin in the pathogenesis of type I diabetes in BB diabetic-prone rats. Proc Natl Acad Sci USA. 2005;102:2916–2921. doi: 10.1073/pnas.0500178102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Fetissov SO, Déchelotte P. The new link between gut-brain axis and neuropsychiatric disorders. Curr Opin Clin Nutr Metab Care. 2011;14:477–482. doi: 10.1097/MCO.0b013e32834936e7. [DOI] [PubMed] [Google Scholar]
- 174.Heberling CA, Dhurjati PS, Sasser M. Hypothesis for a systems connectivity model of Autism Spectrum Disorder pathogenesis: links to gut bacteria, oxidative stress, and intestinal permeability. Med Hypotheses. 2013;80:264–270. doi: 10.1016/j.mehy.2012.11.044. [DOI] [PubMed] [Google Scholar]
- 175.Rebuffat SA, Kammoun-Krichen M, Charfeddine I, Ayadi H, Bougacha-Elleuch N, Peraldi-Roux S. IL-1β and TSH disturb thyroid epithelium integrity in autoimmune thyroid diseases. Immunobiology. 2013;218:285–291. doi: 10.1016/j.imbio.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 176.Peng SN, Zeng HH, Fu AX, Chen XW, Zhu QX. Effects of rhein on intestinal epithelial tight junction in IgA nephropathy. World J Gastroenterol. 2013;19:4137–4145. doi: 10.3748/wjg.v19.i26.4137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Giardino G, Cirillo E, Maio F, et al. Gastrointestinal involvement in patients affected with 22q11.2 deletion syndrome. Scand J Gastroenterol. 2014;49:274–279. doi: 10.3109/00365521.2013.855814. [DOI] [PubMed] [Google Scholar]
- 178.Klaus DA, Motal MC, Burger-Klepp U, et al. Increased plasma zonulin in patients with sepsis. Biochem Medica. 2013;23:107–111. doi: 10.11613/BM.2013.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Perlman SE, Friedman S, Galea S, et al. Short-term and medium-term health effects of 9/11. Lancet. 2011;378:925–934. doi: 10.1016/S0140-6736(11)60967-7. [DOI] [PubMed] [Google Scholar]
- 180.Gareau MG, Jury J, Yang PC, MacQueen G, Perdue MH. Neonatal maternal separation causes colonic dysfunction in rat pups including impaired host resistance. Pediatr Res. 2006;59:83–88. doi: 10.1203/01.pdr.0000190577.62426.45. [DOI] [PubMed] [Google Scholar]
- 181.Keita AV, Söderholm JD, Ericson AC. Stress-induced barrier disruption of rat follicle-associated epithelium involves corticotropin-releasing hormone, acetylcholine, substance P, and mast cells. Neurogastroenterol Motil. 2010;22:770–778. e221, e222. doi: 10.1111/j.1365-2982.2010.01471.x. [DOI] [PubMed] [Google Scholar]
- 182.Ait-Belgnaoui A, Durand H, Cartier C, et al. Prevention of gut leakiness by a probiotic treatment leads to attenuated HPA response to an acute psychological stress in rats. Psychoneuroendocrinology. 2012;37:1885–1895. doi: 10.1016/j.psyneuen.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 183.Hill LT, Kidson SH, Michell WL. Corticotropin-releasing factor is present in intestinal tissue of patients with gastrointestinal dysfunction following shock and abdominal surgery. Nutrition. 2013;29:650–654. doi: 10.1016/j.nut.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 184.Wei ET, Kiang JG, Buchan P, Smith TW. Corticotropin-releasing factor inhibits neurogenic plasma extravasation in the rat paw. J Pharmacol Exp Ther. 1986;238:783–787. [PubMed] [Google Scholar]
- 185.Wei ET, Kiang JG. Inhibition of protein exudation from the trachea by corticotropin-releasing factor. Eur J Pharmacol. 1987;140:63–67. doi: 10.1016/0014-2999(87)90634-0. [DOI] [PubMed] [Google Scholar]
- 186.Kiang JG, Wei ET. Corticotropin-releasing factor inhibits thermal injury. J Pharmacol Exp Ther. 1987;243:517–520. [PubMed] [Google Scholar]
- 187.Wei ET, Serda S, Tian JQ. Protective actions of corticotropin-releasing factor on thermal injury to rat pawskin. J Pharmacol Exp Ther. 1988;247:1082–1085. [PubMed] [Google Scholar]
- 188.Tian JQ, Wei ET. Acute inflammatory response of the rat pawskin to acid injury is attenuated by corticotropin-releasing factor. Drug Chem Toxicol. 1989;12:61–66. doi: 10.3109/01480548908999143. [DOI] [PubMed] [Google Scholar]
- 189.Wei ET, Kiang JG. Peptides of the corticoliberin superfamily attenuate thermal and neurogenic inflammation in rat pawskin. Eur J Pharmacol. 1989;168:81–86. doi: 10.1016/0014-2999(89)90635-3. [DOI] [PubMed] [Google Scholar]
- 190.Serda SM, Wei ET. Corticotropin-releasing factor inhibits the acute inflammatory response of rat pawskin to cold injury. Cryobiology. 1991;28:185–190. doi: 10.1016/0011-2240(91)90021-F. [DOI] [PubMed] [Google Scholar]
- 191.Wei ET, Gao GC. Corticotropin-releasing factor: an inhibitor of vascular leakage in rat skeletal muscle and brain cortex after injury. Regul Pept. 1991;33:93–104. doi: 10.1016/0167-0115(91)90205-U. [DOI] [PubMed] [Google Scholar]
- 192.Gao GC, Dashwood MR, Wei ET. Corticotropin-releasing factor inhibition of substance P-induced vascular leakage in rats: possible sites of action. Peptides. 1991;12:639–644. doi: 10.1016/0196-9781(91)90113-4. [DOI] [PubMed] [Google Scholar]
- 193.Kelley DM, Lichtenstein A, Wang J, Taylor AN, Dubinett SM. Corticotropin-releasing factor reduces lipopolysaccharide-induced pulmonary vascular leak. Immunopharmacol Immunotoxicol. 1994;16:139–148. doi: 10.3109/08923979409007086. [DOI] [PubMed] [Google Scholar]
- 194.Yoshihara S, Ricciardolo FL, Geppetti P, et al. Corticotropin-releasing factor inhibits antigen-induced plasma extravasation in airways. Eur J Pharmacol. 1995;280:113–118. doi: 10.1016/0014-2999(95)00187-P. [DOI] [PubMed] [Google Scholar]
- 195.Whitney TM, Wang KK, Sternbach Y, Chaklis-Haley D. Reduction of ischemic reperfusion edema with corticotropin-releasing factor (CRF) in rat hind limb replantation. Ann Plast Surg. 1997;38:416–419. doi: 10.1097/00000637-199704000-00018. discussion 419–420. [DOI] [PubMed] [Google Scholar]
- 196.Theoharides TC, Singh LK, Boucher W, et al. Corticotropin-releasing hormone induces skin mast cell degranulation and increased vascular permeability, a possible explanation for its proinflammatory effects. Endocrinology. 1998;139:403–413. doi: 10.1210/endo.139.1.5660. [DOI] [PubMed] [Google Scholar]
- 197.Whitney TM, Bentz ML, Johnson PC. Reduction of reperfusion injury edema with corticotropin-releasing factor (CRF): a pilot study. Microsurgery. 1998;18:76–78. doi: 10.1002/(SICI)1098-2752(1998)18:2<76::AID-MICR3>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 198.Singh LK, Boucher W, Pang X, et al. Potent mast cell degranulation and vascular permeability triggered by urocortin through activation of corticotropin-releasing hormone receptors. J Pharmacol Exp Ther. 1999;288:1349–1356. [PubMed] [Google Scholar]
- 199.Rapallino MV, Cupello A, Hydén H, Izvarina NL. Modulation by acute stress of chloride permeation across microdissected vestibular neurons membranes: different results in two rabbit strains and CRF involvement. Brain Res. 2001;890:255–260. doi: 10.1016/S0006-8993(00)03175-9. [DOI] [PubMed] [Google Scholar]
- 200.Esposito P, Chandler N, Kandere K, et al. Corticotropin-releasing hormone and brain mast cells regulate blood-brain-barrier permeability induced by acute stress. J Pharmacol Exp Ther. 2002;303:1061–1066. doi: 10.1124/jpet.102.038497. [DOI] [PubMed] [Google Scholar]
- 201.Hendryk S, Jedrzejowska-Szypulka H, Jośko J, Jarzab B, Döhler KD. Influence of the corticotropin releasing hormone (CRH) on the brain-blood barrier permeability in cerebral ischemia in rats. J Physiol Pharmacol. 2002;53:85–94. [PubMed] [Google Scholar]
- 202.Huang M, Berry J, Kandere K, Lytinas M, Karalis K, Theoharides TC. Mast cell deficient W/Wv mice lack stress-induced increase in serum IL-6 levels, as well as in peripheral CRH and vascular permeability, a model of rheumatoid arthritis. Int J Immunopathol Pharmacol. 2002;15:249–254. doi: 10.1177/039463200201500314. [DOI] [PubMed] [Google Scholar]
- 203.Lytinas M, Kempuraj D, Huang M, Boucher W, Esposito P, Theoharides TC. Acute stress results in skin corticotropin-releasing hormone secretion, mast cell activation and vascular permeability, an effect mimicked by intradermal corticotropin-releasing hormone and inhibited by histamine-1 receptor antagonists. Int Arch Allergy Immunol. 2003;130:224–231. doi: 10.1159/000069516. [DOI] [PubMed] [Google Scholar]
- 204.Donelan J, Boucher W, Papadopoulou N, et al. Corticotropin-releasing hormone induces skin vascular permeability through a neurotensin-dependent process. Proc Natl Acad Sci USA. 2006;103:7759–7764. doi: 10.1073/pnas.0602210103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wu Y, Xu Y, Zhou H, Tao J, Li S. Expression of urocortin in rat lung and its effect on pulmonary vascular permeability. J Endocrinol. 2006;189:167–178. doi: 10.1677/joe.1.06607. [DOI] [PubMed] [Google Scholar]
- 206.Cureton EL, Ereso AQ, Victorino GP, et al. Local secretion of urocortin 1 promotes microvascular permeability during lipopolysaccharide-induced inflammation. Endocrinology. 2009;150:5428–5437. doi: 10.1210/en.2009-0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Song JP, Chen X, Yang G, Geng XR. Corticotropin releasing hormone activates CD14+ cells to induce endothelial barrier dysfunction. Cell Biol Int Published. 2013 May 17; doi: 10.1002/cbin.10133. [DOI] [PubMed] [Google Scholar]
- 208.Wan R, Guo R, Chen C, et al. Urocortin increased LPS-induced endothelial permeability by regulating the cadherin-catenin complex via corticotrophin-releasing hormone receptor 2. J Cell Physiol. 2013;228:1295–1303. doi: 10.1002/jcp.24286. [DOI] [PubMed] [Google Scholar]