Abstract
Objective The association between directly observed mother–adolescent weight-related communication quality and adolescent percent overweight within the context of an adolescent weight control study was examined. Methods As part of a larger study examining the impact of a behavioral weight control intervention that included attention to parent–adolescent communication (Standard Behavioral Treatment + Enhanced Parenting, SBT + EP) compared with an efficacious Standard Behavioral Treatment (SBT), 38 mother–adolescent dyads participated in a weight-related videotaped discussion. Discussions were taped and collected pre- and postintervention. Results No significant differences emerged in the quality of mother–adolescent communication between SBT (n = 19) and SBT + EP (n = 19) participants, nor was baseline mother–adolescent communication quality associated with adolescents’ weight loss in either condition. However, a decline in communication quality was associated with better outcomes for adolescents participating in the SBT group. Conclusions This study provides preliminary evidence that a change in mother–adolescent communication is associated with successful weight loss among adolescents.
Keywords: adolescents, parent-adolescent communication, weight management
Rates of pediatric obesity have increased significantly in the past 30 years, and obesity is now identified as a leading cause of preventable deaths (Ogden, Carroll, Kit, & Flegal, 2012). Adolescent obesity is particularly concerning, as rates have increased markedly during the past decade. In fact, The National Health and Nutrition Examination Survey reported an increase in percentage of overweight adolescents from 14.8% in 1999–2000 to >18% in 2009–2010 (Ogden et al., 2012). These alarming trends highlight the need to understand factors that may contribute to adolescent obesity and that may serve as important targets for intervention.
Numerous studies have examined a variety of determinants of adolescent obesity, including heritability, environmental context, and family factors. Within the realm of family factors, high parental body mass index (BMI), poor family functioning, low family cohesion, and high conflict are all associated with elevated child BMI and worse weight-related health behaviors (Berge, Wall, Larson, Loth, & Neumark-Sztainer, 2013; Gundersen, Mahatmya, Garasky, & Lohman, 2011; Zeller et al., 2007). Specific parenting practices that have been linked to children’s weight management behaviors are parental modeling of healthy weight control practices (exercise and health eating) and provision of healthy options in the home (Golan & Weizman, 2001; Orlet Fisher, Mitchell, Wright, & Birch, 2002). Beyond these practices, Kitzman and Beech (2011) have highlighted parent–child communication as an important variable to consider related to adolescent weight. Specifically, an adversarial parent–teen relationship that is characterized by high levels of criticism and conflict may influence an adolescent’s motivation to engage in and adhere to healthy weight management practices. Adolescents’ perception of poor parental communication and caring also has been associated with unhealthy weight control behaviors (Ackard, Neumark-Sztainer, Story, & Perry, 2006) and weight-related teasing by family members, parents in particular, is reported by a striking percentage of overweight girls (47%) and boys (34%) (Neumark-Sztainer et al., 2002). Examination of directly observed mealtime behaviors and communication has shown that parents of overweight children demonstrate less support (Moens, Braet, & Soetens, 2007) and more weight-related critique than parents of normal-weight peers (Hilbert, Tuschen-Caffier, & Czaja, 2010). These studies indicate that higher levels of family conflict and more negative parent communication are occurring in families of adolescents who are overweight, which is in turn associated with adolescents’ unhealthy weight-related behaviors.
We propose that parent–child communication may be particularly salient for adolescent adoption of healthy weight management strategies based on pediatric psychology research showing the direct influence of improved parent–child communication on other health behaviors (e.g., diabetes management, substance use, and sexual risk). Specifically, Wysocki et al. (2008) demonstrated that among a sample of adolescents with diabetes, improved family communication was associated with improved glycemic control and adherence to diabetes management regimens for those participating in a behavioral family systems therapy intervention. Furthermore, improvements in parent–child communication have consistently demonstrated an impact on reductions in adolescent substance use (Stanton et al., 2004) and adoption of safer sexual practices (i.e., greater condom use (DiClemente et al., 2001)) Two possible mechanisms by which parent–adolescent communication is thought to influence adolescent weight control behaviors are through (1) parental assistance in problem-solving and (2) parents conveying parental values about health dietary choices and exercise behaviors (Kitzmann & Beech, 2011). Although more positive parent–adolescent communication is associated with teen adoption of behaviors that are consistent with parental values (Patrick, Hennessy, McSpadden, & Oh, 2013), no one has directly examined the role of parental assistance in problem-solving and its association with adolescent engagement in healthy weight control behaviors. More research is clearly needed to better understand how parent–child communication may impact adolescents’ success within a weight-control intervention.
Although parents are thought to play an important role in the development of adolescent weight-related behaviors, few parenting interventions have successfully integrated parents as allies to adolescents’ weight reduction attempts. For example, one study documented superior outcomes when adolescents and parents were included (but seen in separate groups) in the intervention (Brownell, Kelman, & Stunkard, 1983), while two other studies showed comparable outcomes regardless of whether the adolescent was treated alone or with a parent (Coates, Killen, & Slinkard, 1982; Wadden et al., 1990). A recent study by Steele et al. (2012) found that both brief family intervention and a family-based behavioral treatment were effective in reducing zBMI (Body Mass Index) among a sample of younger children, but not adolescents. Across these adolescent studies, parents have been targeted to serve in supportive roles, whereas among those in younger children, parents have been targeted for weight loss along with their children. These competing results suggest that the parent–adolescent dynamic related to weight control is complex and more research is needed to understand what parental behaviors may be helpful and/or harmful to teens’ weight loss endeavors.
Given the relevance of parental communication to adolescent weight control and the mixed findings related to parental involvement in healthy adolescent and weight control, our team developed a 16-week adolescent behavioral weight control (BWC) intervention that explicitly targeted parent–adolescent communication (Standard Behavioral Treatment + Enhanced Parenting, SBT + EP; see Methods). The SBT + EP intervention differs from prior interventions involving families in that it explicitly targeted “unhealthy” patterns of communication (e.g., criticism and negative comments) that have been associated with overweight and unhealthy weight-related behaviors (Ackard et al., 2006; Moens et al., 2007), parent weight control behaviors including weekly weigh-ins and completion of food journals, and increasing supportive communication behaviors (e.g., warmth and directness). The SBT + EP intervention was compared with an efficacious Standard Behavioral Treatment (SBT; see Methods). Analyses revealed a significant decrease in adolescent BMI for both conditions at the end of the 16-week treatment study, though no significant differences in adolescent weight loss emerged between conditions (blinded citation). Secondary analyses examining the impact of the intervention on weight-related communication revealed that adolescents in the SBT condition self-reported less maternal negative commentary at the end of the intervention relative to adolescents in the SBT + EP group. This finding was in contrast to what was expected; therefore, we chose to examine the directly observed communication to better understand how changes in parent–adolescent communication may be associated with changes in adolescent weight in the context of two active weight management interventions.
Prior studies have included observational data as a means to shed light on complicated patterns of parent–adolescent interactions and behavior change (Kerig & Lindahl, 2000). For the current study, we chose to examine observational data within the context of a BWC intervention for two primary reasons. First, only a handful of studies have examined direct communication within the context of weight-related behavior and no known studies have employed observational methods to objectively examine and assess quality of parent–adolescent communication within a weight control study. Second, while self-report measures are important to understanding these processes, they can be limited by attribution biases, selective attention, social desirability, and ineffective reporting on communication patterns, which occur over extended time or situations (Bradbury & Fincham, 1990; Noller & Callan, 1990; Noller & Feeney, 2003). Observational methods, while more time-consuming and expensive, allow for assessment of actual behavior, as opposed to participants’ perceptions of behavior, and thus may reveal differing patterns of associations (Noller & Feeney, 2003). Given these gaps in the study of adolescent obesity, observational research with adolescents may provide the field with greater insight into the role of parent–adolescent communication for this high-risk population.
Aims and Hypotheses
The current study examined the association between directly observed mother–adolescent weight-related communication quality and adolescent percent overweight within the context of an adolescent weight control intervention. Three primary questions were explored: (1) Did mother–adolescent dyads randomized to SBT + EP show greater improvement in observed mother–adolescent communication from pre- to postintervention relative to those in the SBT condition?; (2) Did higher baseline mother–adolescent communication predict greater reduction in adolescent percent overweight?; and (3) Were positive changes in mother–adolescent communication over the study period associated with a reduction in percent overweight?
We hypothesized that the SBT + EP condition would show greater gains in mother–adolescent communication quality from pre- to postintervention. Furthermore, based on prior studies showing the role of positive family functioning and lower family conflict in adolescent response to BWC interventions (Germann, Kirschenbaum, & Rich, 2007; White et al., 2004) we predicted that more positive mother–adolescent baseline communication would be associated with a greater reduction in adolescent percent overweight. Finally, we expected that improvements in communication would be associated with a reduction in adolescent percent overweight post intervention.
Methods
Participants
Adolescents aged 13–17 years were recruited from area pediatricians, family physicians, and through newspaper advertisements. Interested adolescents and parents were screened using a brief telephone interview to determine preliminary eligibility. Inclusion criteria for the adolescent were (1) BMI ≥ 95th percentile and absolute BMI ≤ 38; (2) at least one involved caregiver available to participate in the treatment protocol; and (3) both the adolescent and caregiver spoke English. Adolescents were excluded if they (1) were involved in another weight loss program; (2) had a medical condition that would interfere with the prescribed dietary plan or participation in physical activity; or (3) were in treatment for, or diagnosed with, a major psychiatric disorder, including an eating disorder or significant developmental delay, at the time of screening. Eligible participants attended an informational meeting where study details were reviewed and adolescents’ anthropometric data were obtained. Interested and eligible families were scheduled for an initial evaluation. Ineligible or uninterested adolescents were referred back to their primary care physician, to an area nutritionist, or a mental health provider, as appropriate. Parental consent and adolescent assent for study participation were obtained before beginning the initial evaluation. Of the 241 families who completed a phone screening, 49 families met study inclusion criteria and were available to be randomized to one of the two treatment groups. Of those, 38 mother–adolescent dyads had complete baseline and postintervention videotaped observations (88%). Of the 11 dyads excluded from analyses, 4 had either baseline or postintervention videotapes that were unable to be coded owing to taping glitches (e.g., no sound, could only see one member of the dyad, etc.), 2 were missing baseline videotapes, and 5 did not return for the postintervention evaluation.
Procedures
Before randomization, adolescents were asked to complete a 1-week “adherence trial” during which they were asked to record all dietary intake to provide a behavioral measure of treatment readiness. Families were randomized if the adolescent completed diet records for 5 of the 7 days. An urn randomization procedure (Stout, 1994), stratifying by gender and relative degree of obesity (high vs. low determined by median split of the sample), was used to assign adolescents to an intervention group. Adolescents and parents completed assessments separately at baseline and at the end of the 16-week treatment. Posttreatment follow-ups were conducted either the same day as the final session or within 2 weeks for those who did not attend the last session. All study procedures were approved by the institutional review board.
Interventions
Both interventions included 16 weekly 1-hr sessions conducted in a group format. Treatment was delivered by a combination of PhD-level psychologists (including study investigators), advanced clinical psychology graduate students, and bachelor’s level research assistants, with two facilitators per group. A nutritionist was present during five of the meetings to provide information, give individualized feedback on diet records, and offer meal planning. Teen and parent attendance rates were not significantly different across conditions. SBT adolescents completed a mean of 12.9 sessions (80.5%) and SBT + EP adolescents completed a mean of 10.7 sessions (66.8%; t(34.4) = 2.01, p = .052). Parents randomized to the SBT condition attended an average of 2.31 of 3 sessions (76.9%) and parents randomized to the SBT + EP condition attended an average of 10.6 of 16 sessions (66.3%; t(47) = 1.33, p = .19).
Standard Behavioral Treatment
The SBT intervention was modeled after a previously validated adolescent BWC intervention (blinded citation). Treatment components included diet, exercise, behavior modification, and cognitive restructuring. Physical activity was increased incrementally to 60 min/day on most days of the week. Before each group meeting, teens were weighed and their diet records were reviewed by a group leader. Three parent meetings were conducted over the course of the 16 sessions to orient parents to general weight control strategies (session 1), answer questions regarding their teen’s progress (session 8), and review adolescent progress and continuing goals for the end of treatment (session 16).
Standard Behavioral Treatment With Enhanced Parent Involvement
In addition to receiving the SBT intervention, the SBT + EP condition offered enhanced parent involvement through an emphasis on parental modeling of healthy weight-control strategies and improved parent–adolescent communication about weight-related behaviors. Parents and teens attended separate, but simultaneous, sessions. Session content for parents paralleled information provided to adolescents. Similar to teens, parent weight and self-monitoring efforts were reviewed with a group leader before each session.
Parents and adolescents assigned to this condition also received education and participated in joint activities to support effective communication in the context of adolescent–parent interactions related to weight control. The communication didactics and skill-building activities were woven throughout the 16 weekly sessions and accounted for approximately 25% of intervention time. Specific content for the communication intervention was adapted from an HIV risk reduction intervention (Donenberg et al., 2012) and modified to apply to topics of BWC, diet, and physical activity, and further tailored through our earlier pilot work. In vivo communication activities emphasized active listening, assertive communication, and affect management focusing on weight-related discussions (citation not included for blinding).
Observational Coding
To identify a topic for the videotaped parent–adolescent discussion, parents and teens each completed the Family Interactions Topics questionnaire at baseline and the end of the 16-week intervention. The Family Interactions Topics measure was adapted from the Potential Parent–Child Problems measure (Donenberg & Weisz, 1997) and lists weight-related topics that lead to parent–adolescent conflict. Parents and adolescents independently indicated the amount of conflict evoked by a list of 16 situations (e.g., amount of food that teen eats between meals; refusing to participate in physical activity) on a scale of 0 = no conflict to 6 = much conflict. Consistent with prior research (Christensen & Margolin, 1988; Marshall, Longwell, Goldstein, & Swanson, 1990) the item rated most conflictual by both people with the least discrepancy between the two respondents was chosen as the topic for the weight-related discussion task.
Videotaping was directed by a trained research assistant and conducted pre- and postintervention in private rooms at the study site. Before videotaping, parent–teen dyads were instructed “You both identified some things that cause disagreements between the two of you on this sheet you completed. After looking through your responses, I’ve chosen a topic that you both said you disagree about that most. The topic you both identified is _________. I would like you both to take the next 5 minutes to discuss the issue with each other. Please use the full 5 minutes to discuss the topic and I will let you know when the 5 min are up.” Dual microphones were used to improve the sound quality of videotaped interactions. After video setup was completed and instructions were delivered to the dyad, the research assistant left the room, pressed “record” on the camera, and placed a labeled sign in front of the camera to record subject ID number and time point for each interaction. Although each dyad was aware that the discussion would last 5 min, the research assistant was responsible for prompting dyads to begin and end the discussion.
Discussions that lasted longer than 5 min were truncated so that only the first 5 min of each discussion were viewed by the trained coder. Videos were also stripped of participant ID, time point, and any statements that could potentially unblind coders to the intervention condition or time point. Each 5-min videotaped interaction required approximately 30 min to code.
Two previously trained Bachelor-level coders received approximately 100 hr of training from study investigators at the primary investigation site on a study using the observational system (Hadley et al., 2013). Coders were given an overview of the study design and sample, and inter-rater reliability was checked after the first 5, 10, and 20 videotapes were coded to assure adequate inter-rater reliability.
Trained coders watched each videotaped interaction approximately five times. First, coders simply observed the interaction in its entirety without using any of the codes. Coders then selected an individual in the dyad to code by flipping a coin (heads = mother, tails = teen). Ratings were assigned in accordance with the coding system (see below).
Measures
Basic demographic variables (age, gender, race, ethnicity, mother age, and education) were collected at baseline.
Anthropometrics
Adolescent height and weight were obtained on a balance beam and stadiometer, respectively. Adolescents were measured in hospital gowns with underclothing and no shoes. Weight and height were collected at baseline and end of treatment and were used to calculate BMI (kg/m2) and percent overweight. Percent overweight is standardized for weight and gender and provides a value relative to the 50th percentile BMI for the appropriate age and gender, where positive values indicate being over the 50th percentile and negative values indicate being under the 50th percentile (BMI—BMI at 50th percentile BMI)/by 50th percentile BMI × 100). Percent overweight has demonstrated some advantage with regard to sensitivity to changes in weight as compared with BMI and zBMI in OW/OB youth (Cole, Faith, Pietrobelli, & Heo, 2005; Epstein, Paluch, Roemmich, & Beecher, 2007).
Negative Maternal Commentary
Adolescents completed the 5-item Negative Maternal Commentary subscale of the Family Experiences Related to Food Questionnaire (Kluck, 2008) at baseline and immediately postintervention. This subscale assesses teens’ perceived frequency of negative comments made about their weight and appearance by their mother. Items are rated on a 5-point scale from 1 = Never to 5 = All the time and summed for a total score, with higher scores indicating more perceived problematic family experiences. Internal consistency for this subscale was .72 in the present study. This measure was used to establish convergent validity of the coded communication interactions.
Dietary Choices
Caregivers completed the Dietary Choices subscale of the Weight Control Strategies Scale (Pinto, Fava, Raynor, LaRose, & Wing, 2013) at baseline and postintervention. Items are rated on a scale from 0 = Never to 4 = Always and summed for a total score, with higher scores indicating more frequent selection of dietary choices associated with weight loss. Internal consistency for this subscale was .89 in the present study. This measure was used to establish divergent validity of the coded communication interactions.
Communication Coding
The Dyadic Observed Communication Scale (DOCS) was used to code communication between adolescent and caregiver participants (Hadley et al., 2013). The DOCS is a reliable and valid observational method of assessing both verbal and nonverbal communication behaviors among parent–child dyads. The DOCS includes separate codes for four types of parent and adolescent behaviors (i.e., I-statements, Negative Vocalizations, Positive Vocalizations, and Body Language) and one global code of Parent–Adolescent Communication. Given the small sample and the goal of capturing parent–teen interactions broadly, only the Parent–Adolescent Communication domain was used in this study. This domain is highly correlated with the other DOCS’ domain codes (Hadley et al., 2013).
Mother–Adolescent Communication is a global rating that measures the overall quality of the dyadic communication. Each dyad was scored on five dimensions: (1) Tone (e.g., warmth vs. hostility), with scores ranging from 0 to 2, with higher scores indicating warmer communication; (2) Process (e.g., problem-solving, collaboration, and perspective taking), with scores ranging from 0 to 2, with higher scores indicating better problem-solving, collaboration, and perspective taking; (3) Clarity (e.g., direct communication vs. “beating around the bush”), with scores ranging from 0 to 2, with higher scores indicating more direct communication; (4) Time (e.g., degree of give and take), with scores ranging from 0 to 2, with higher scores indicating a higher degree of give and take in communication; and (5) Power, with a binary score of 0 or 1. Mothers who were clearly “in control” were given a point for power relative to those mothers who displayed more passive parenting styles (e.g., wavering on rule setting). Each dimension of mother–adolescent communication was rated separately and summed to create the overall Mother–Adolescent Communication variable. We examined the combined score given the small sample size, which limits our power to detect changes in scores with limited variability (e.g., range of 0–2). Total scores ranged from 1 to 9 per mother–teen dyad, with higher scores indicating better communication.
Inter-rater reliability using Intraclass Correlation Coefficients was .78 for Mother–Adolescent Communication at baseline and .81 for posttreatment. Coefficients >.60 are considered acceptable (Florsheim, Tolan, & Gorman-Smith, 1996). Mother–Adolescent Communication at baseline was positively correlated with the Negative Maternal Commentary Scale, suggesting convergent validity (r = .33), and unrelated to the Dietary Choices Subscale (r = .04), indicating discriminant validity.
Results
Baseline Comparisons
Baseline characteristics for the current study sample (n = 38) are presented in Table I. Chi-square and t-tests were used to examine differences in demographic variables between treatment groups at baseline (see Table I). There were no significant differences between the two conditions on any of the measured demographics at baseline; therefore, these were not controlled for in any of the remaining analyses.
Table I.
Descriptive Data (Mean [SD] or Frequency [%]) for Participants by Treatment Group
| Overall |
SBT |
SBT + EP |
|||||
|---|---|---|---|---|---|---|---|
| Variable | M (SD) | N (%) | M (SD) | N (%) | M (SD) | N (%) | p |
| Adolescents | |||||||
| Age | 15.1 (1.3) | – | 14.9 (1.2) | – | 15.2 (1.4) | – | 0.51 |
| Female | – | 29 (76.3) | – | 13 (68.1) | – | 16 (84.2) | 0.25 |
| Ethnicity | 1.00 | ||||||
| Latino | – | 6 (15.7) | – | 3 (15.8) | – | 3 (15.8) | |
| Non-Latino | – | 32 (84.3) | 16 (84.2) | – | 16 (84.2) | ||
| Race | – | 0.26 | |||||
| Caucasian | – | 24 (63.4) | – | 15 (78.9) | – | 9 (47.4) | |
| African American | – | 4 (10.5) | – | 2 (10.5) | – | 2 (10.5) | |
| Asian American | – | 1 (2.6) | – | 0 (0.0) | – | 1 (5.3) | |
| Native American | – | 2 (5.2) | – | 1 (5.3) | – | 1 (5.3) | |
| Biracial | – | 3 (7.8) | – | 0 (0.0) | – | 3 (15.8) | |
| Other | – | 4 (10.5) | – | 1 (5.3) | – | 3 (15.8) | |
| BMI at baseline | 32.3 (3.5) | – | 31.6 (2.7) | – | 32.9 (4.1) | – | 0.23 |
| BMI at 16 weeks | 31.1 (3.8) | – | 30.2 (3.6) | – | 32.0 (3.8) | – | 0.13 |
| % Overweight baseline | 62.2 (17.4) | 59.7 (13.2) | 64.8 (20.8) | 0.37 | |||
| % Overweight 16 weeks | 57.2 (18.4) | 53.3 (15.6) | 61.1 (20.5) | 0.19 | |||
| Mothers | |||||||
| Age | 45.9 (7.3) | – | 46.1 (7.2) | – | 45.8 (7.6) | – | 0.91 |
| BMI at baseline | 30.4 (5.4) | 32.1 (5.6) | 28.9 (4.7) | 0.06 | |||
| BMI at 16 weeks | 30.1 (5.6) | 32.1 (5.5) | 28.7 (5.1) | 0.06 | |||
| Education | 0.21 | ||||||
| Some high school | – | 7 (18.4) | – | 5 (26.3) | – | 2 (10.5) | |
| College or more | – | 31 (81.6) | – | 14 (73.7) | – | 17 (89.5) | |
| Parent–adolescent communication | |||||||
| Baseline | 5.7 (1.9) | – | 5.8 (1.9) | – | 5.5 (2.1) | – | 0.62 |
| Postintervention | 5.6 (1.8) | – | 5.8 (1.8) | – | 5.5 (1.9) | – | 0.61 |
Mother–Adolescent Communication and Adolescent BMI
1. Did Mother-Adolescent Dyads Randomized to the SBT + EP Intervention Show Greater Improvement in Mother–Adolescent Communication From Pre- to Postintervention?
The Mother–Adolescent Communication score was categorized into the following groupings at baseline and postintervention: poor communication (score = 1–3), average communication (score = 4–6), and high communication (score = 7–9). Dyads were then classified into one of three categories based on their change in category from baseline to postintervention (i.e., improved, maintained, or declined). For example, dyads that moved from the poor to average communication category were categorized as “improved,” whereas those who moved from high to average communication were labeled as “declined.” A chi-square test of independence was calculated to examine communication change (i.e., improved, maintained, declined) by treatment group (SBT, SBT + EP). No significant differences emerged between the SBT (N = 19) and SBT + EP (N = 19) treatment groups related to Mother–Adolescent communication, χ2(2, N = 38) = .19, p = .91. Cramer’s V (the square root of chi-square/sample size × degrees of freedom; (Gravetter & Wallnau, 2004)) was calculated to determine effect size. This calculation generated a v = .07 which equates to a small effect size.
2. Does Higher Baseline Mother–Adolescent Communication Quality Predict Greater Reduction in Adolescent Percent Overweight?
An analysis of covariance (ANCOVA) was calculated to examine differences in percent overweight at posttreatment, controlling for baseline percent overweight, among baseline Mother–Adolescent Communication categories (i.e., low, average, high). Baseline Mother–Adolescent Communication category was not associated with percent overweight at posttreatment, F(2, 34) = 0.06, p = .95. The effect size for this outcome was generated using partial eta squared (the sum of squares between divided by the sum of squares total plus sum or squares error) and was small, = .00 (Cohen, 1988).
3. Were Positive Changes in Mother Adolescent Communication Quality Over the Study Period Associated With A Reduction in Adolescent Percent Overweight?
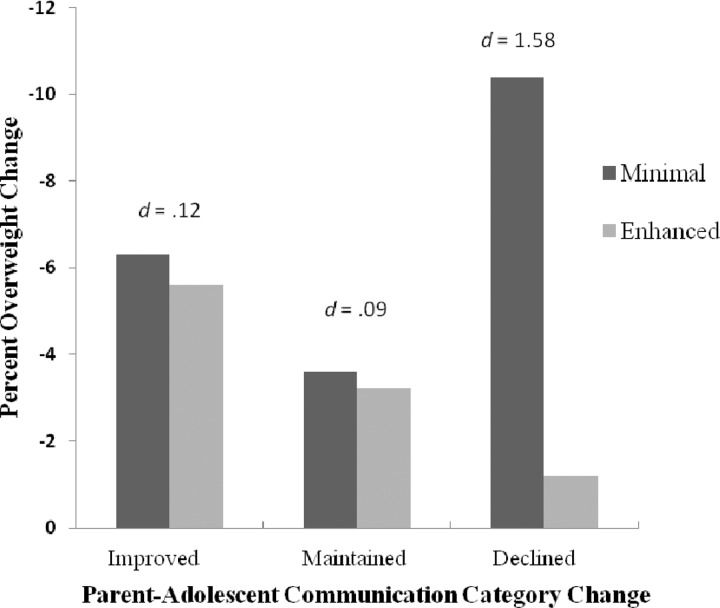
An ANCOVA, controlling for baseline percent overweight, was conducted to examine two questions: (1) if change in Mother–Adolescent Communication category (i.e., improved, maintained, declined) from pre- to posttreatment was associated with adolescent weight loss and (2) if treatment group (i.e., SBT, SBT + EP) moderated the effect of category change on adolescent percent overweight. Results revealed no main effect of communication category change, F(2, 32) = 1.05, p = .36, treatment group, F(1, 32) = 4.01, p = .05, or category change by treatment group, F(2, 32) = 2.41, p = .10. Although not statistically significant, there was a large effect size for the category change by treatment group. Effect sizes were calculated to compare the impact of treatment condition on percent overweight within each level of category change (i.e., improved, maintained, and declined). Using Cohen’s (1988) guidelines for interpreting Cohen’s d effect sizes (0.2 = small, 0.5 = medium, and ≥0.8 = large), when comparing the minimal and enhanced groups a large effect size emerged between the “declined” category (d = 1.58), small for “maintained” (d = 0.09), and small for “improved” (d = 0.12; See Figure 1).
Figure 1.
Changes in adolescent percent overweight by Mother–Adolescent Communication category change and treatment condition. Note. Communication Change defined as (1) Improved: Communication ratings increased a category from pre- to postintervention; (2) Declined: Communication categories decreased a category from pre- to postintervention; (3) Maintained: Communication categories stayed the same from pre- to postintervention. d = Cohen’s d effect sizes where 0.2 = small, 0.5 = medium, and 0.8 = large.
To better understand this pattern of change within the “improved” and “declined” communication groups, we visually inspected the frequencies for each of the domains of Mother–Adolescent Communication (i.e., Tone, Clarity, Time, Power, and Process). Inspection of these domains revealed the following patterns for the “declined” group: 80% decreased in Tone, 67% decreased in Clarity, 55% decreased in Process, 33% decreased in Power, and 22% decreased in Time. For the “improved” group, 77% increased in Tone, 46% increased in Clarity, 31% increased in Time, 8% increased in Process, and 8% increased in Power.
Discussion
This was the first study to examine directly observed communication among mother–adolescent dyads within the context of an adolescent weight management intervention. The DOCS coding system was found to be a valid and reliable coding system within the context of mother–adolescent weight-related discussions. Findings indicated that the SBT + EP intervention did not demonstrate a significant improvement in communication relative to the comparison condition, that baseline communication was not predictive of response to the intervention, and finally, that change in communication quality was associated with a decrease in adolescent percent overweight over the intervention study period.
Counter to our prediction, but consistent with the previous study examining self-report of communication (blinded citation), findings indicate that dyads randomized to the SBT + EP condition did not demonstrate an improvement in communication relative to those dyads randomized to the SBT condition. Notably, the study did not explicitly recruit dyads with impaired patterns of communication, resulting in a total of only six (15.8%) dyads that were categorized as having “poor” quality communication at baseline. This limited sample size may have impacted our ability to demonstrate improvements in communication. Alternatively, among dyads randomized to the SBT condition, mothers received three sessions focused on awareness of weight management strategies, adolescent progress updates, and goal setting. These three sessions may have provided mothers with sufficient tools to support the teens in their weight loss efforts without the need to address poor communication. Future studies examining the role of parent–adolescent communication within adolescent weight-related behaviors should consider explicitly targeting dyads or families with impaired communication.
Contrary to our hypothesis and prior studies demonstrating that positive family dynamics are associated with better response to weight loss interventions (Germann etal., 2007; White et al., 2004), baseline levels of communication about weight were unrelated to intervention impact on adolescent weight loss. Notably, neither poor nor high communication quality at baseline was associated with adolescent weight loss. This is unexpected given findings in pediatric psychology identifying positive family functioning as a resilience factor in the context of youths’ chronic illness (Drotar, 1997; Kazak, 1989). In terms of poor communication, other buffering factors, such as healthy food options in the home and peer support for healthier dietary behaviors, may have been present and served to ameliorate the impact of negative mother–child communication on adolescents’ attempts to change their weight-related behaviors. Similarly, the impact of positive communication may have been attenuated by negative family dynamics outside of the mother–child relationship. For example, marital discord or family chaos related to unemployment may have undermined the positive influence of higher quality communication within the mother–adolescent dyad. Unfortunately, these constructs were not examined within the current study, but may be important indices to examine as potential moderators of intervention impact. It is clear that more research is needed to fully understand how mother–adolescent communication impacts adolescent weight loss.
Finally, although the SBT + EP intervention was not successful in significantly changing communication as compared with the SBT intervention, changes in Mother–Adolescent Communication overall were associated with a reduction in adolescent percent overweight. The results suggest that movement in mother–adolescent communication quality may be more important to weight loss than initial communication quality. Unexpectedly, the largest difference between treatment conditions on reduction in percent overweight was found within the “declined” communication category. One potential interpretation of this finding is that frequency of negative communication may be more harmful within the context of interventions that more actively involve family members than if the adolescent takes sole responsibility for his/her weight loss efforts with minimal parent involvement. Alternatively, these declines in communication could be wholly attributed to adolescent withdrawal from these conversations as they become more independent in their efforts to manage their weight-related behaviors. Finally, it is possible that the higher maternal BMI seen among those in the minimal group negatively influenced the tone of the communication and concerns expressed by parents who themselves struggled with their own weight management and created a stronger sense of urgency toward changing their teens behavior especially within the context of a weight management intervention. All of these interpretations must be cautiously considered given that changes in communication and changes in percent overweight are measured concurrently and therefore direction of influence cannot be ascertained. Future research should consider examining these patterns over time to determine the influence of mother–adolescent communication on adolescent’s response to weight control interventions.
In terms of strengths, the current study includes an ethnically and racially diverse sample (40% reported an ethnic or racial minority background), the use of observational methods among a sample of mother–adolescent dyads, and the examination of observational data within the context of an adolescent weight-loss study. Despite these significant strengths, weaknesses include a small sample size, which limited our ability to examine the individual components of the overall Mother–Adolescent Communication code (e.g., Tone, Clarity) and their relationship to change in adolescent percent overweight, and a relatively brief follow-up period. Additionally, since fathers were not included in the current study, our conclusions are limited to maternal–adolescent communication and do not account for communication between fathers and adolescents.
In conclusion, the current study provides new insights into the association between mother–adolescent communication quality and adolescent weight reduction within the context of a weight management intervention. These preliminary findings suggest that clinicians working with adolescents attempting to lose weight should assess the dyadic communication. When communication is poor, clinicians should consider minimizing parental treatment involvement to decrease the potential impact of negative dyadic communication patterns on adolescents’ motivation toward weight loss. Alternatively, it may be important to specifically address and bolster positive mother–adolescent communication with an emphasis on increasing warmth (e.g., Tone) and directness (e.g., Clarity) during weight-related discussions before facilitating adolescents’ weight-loss attempts. Future research should attempt to examine these findings with a larger sample that will be adequately powered to examine changes in communication components (e.g., tone, clarity) and also include fathers. A clearer understanding of the nuances in parent–adolescent communication behaviors will provide more specific targets for working with parents and adolescents attempting to lose weight.
Funding
NIH grant R03 HD060137 (PI: E.J.).
Conflicts of interest: None declared.
References
- Ackard D M, Neumark-Sztainer D, Story M, Perry C. Parent–child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine. 2006;30:59–66. doi: 10.1016/j.amepre.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Berge J M, Wall M, Larson N, Loth K A, Neumark-Sztainer D. Family functioning: Associations with weight status, eating behaviors, and physical activity in adolescents. Journal of Adolescent Health. 2013;52:351–357. doi: 10.1016/j.jadohealth.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury T, Fincham F. Attributions in marriage: Review and critique. Psychological Bulletin. 1990;107:3–33. doi: 10.1037/0033-2909.107.1.3. doi:10.1037/0033-2909.107.1.3. [DOI] [PubMed] [Google Scholar]
- Brownell K D, Kelman J H, Stunkard A J. Treatment of obese children with and without their mothers: Changes in weight and blood pressure. Pediatrics. 1983;71:515–523. [PubMed] [Google Scholar]
- Christensen A, Margolin G, editors. Conflict and alliance in distressed and nondistressed families. Oxford: Oxford University Press; 1988. [Google Scholar]
- Coates T J, Killen J D, Slinkard L A. Parent participation in a treatment program for overweight adolescents. International Journal of Eating Disorders. 1982;1:37–48. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Cole T J, Faith M, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? European Journal of Clinical Nutrition. 2005;59:419–425. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- DiClemente R, Wingood G, Crosby R, Cobb B, Harrington K, Davies S. Parent-adolescent communication and sexual risk behaviors among African American adolescent females. Journal of Pediatrics. 2001;139:407–412. doi: 10.1067/mpd.2001.117075. [DOI] [PubMed] [Google Scholar]
- Donenberg G, Brown L, Hadley W, Kapungu C, Lescano C, DiClemente R, Style P. Family-based HIV-prevention for Adolescents with Psychiatric Disorders. In: Pequegnat W, Bell C, editors. Families and HIV/AIDS. New York, NY: Springer Press; 2012. pp. 261–278. [Google Scholar]
- Donenberg G, Weisz J. Experimental task and speaker effects on parent-child interactions of aggressive and depressed/anxious children. Journal of Abnormal Child Psychology. 1997;25:367–387. doi: 10.1023/a:1025733023979. [DOI] [PubMed] [Google Scholar]
- Drotar D. Relating parent and family functioning to the psychological adjustment of children with chronic health conditions: What have we learned? What do we need to know? Journal of Pediatric Psychology. 1997;22:149–165. doi: 10.1093/jpepsy/22.2.149. [DOI] [PubMed] [Google Scholar]
- Epstein L H, Paluch R A, Roemmich J N, Beecher M D. Family-based obesity treatment, then and now: Twenty-five years of pediatric obesity treatment. Health Psychology. 2007;26:381–391. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florsheim P, Tolan P, Gorman-Smith D. Family processes and risk for externalizing behavior problems among African American and Hispanic boys. Journal of Consulting and Clinical Psychology. 1996;64:1222–1230. doi: 10.1037//0022-006x.64.6.1222. doi:10.1037/0022-006x.64.6.1222. [DOI] [PubMed] [Google Scholar]
- Germann J N, Kirschenbaum D S, Rich B H. Child and parental self-monitoring as determinants of success in the treatment of morbid obesity in low-income minority children. Journal of Pediatric Psychology. 2007;32:111–121. doi: 10.1093/jpepsy/jsl007. [DOI] [PubMed] [Google Scholar]
- Golan M, Weizman A. Familial approach to the treatment of childhood obesity: Conceptual model. Journal of nutrition education. 2001;33:102–107. doi: 10.1016/s1499-4046(06)60173-5. [DOI] [PubMed] [Google Scholar]
- Gravetter F, Wallnau L. Statistics for the behavioral sciences. Seatle, WA: Thomson Wadsworth; 2004. [Google Scholar]
- Gundersen C, Mahatmya D, Garasky S, Lohman B. Linking psychosocial stressors and childhood obesity. Obesity Reviews. 2011;12:e54–e63. doi: 10.1111/j.1467-789X.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- Hadley W, Stewart A, Hunter H L, Affleck K, Donenberg G, DiClemente R, Brown L K. Reliability and Validity of the Dyadic Observed Communication Scale (DOCS) Journal of Child and Family Studies. 2013;22:279–287. doi: 10.1007/s10826-012-9577-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Tuschen-Caffier B, Czaja J. Eating behavior and familial interactions of children with loss of control eating: A laboratory test meal study. The American Journal of Clinical Nutrition. 2010;91:510–518. doi: 10.3945/ajcn.2009.28843. [DOI] [PubMed] [Google Scholar]
- Kazak A E. Families of chronically ill children: A systems and social-ecological model of adaptation and challenge. Journal of Consulting and Clinical Psychology. 1989;57(1):25–30. doi: 10.1037//0022-006x.57.1.25. [DOI] [PubMed] [Google Scholar]
- Kerig P K, Lindahl K M. Family observational coding systems: Resources for systemic research. Philadelphia, PA: Psychology Press; 2000. [Google Scholar]
- Kitzmann K M, Beech B. Family-based interventions for pediatric obesity: Methodological and conceptual challenges from family psychology. Journal of Family Psychology. 2006;20:175–189. doi: 10.1037/0893-3200.20.2.175. [DOI] [PubMed] [Google Scholar]
- Kluck A S. Family factors in the development of disordered eating: Integrating dynamic and behavioral explanations. Eating Behaviors. 2008;9:471–483. doi: 10.1016/j.eatbeh.2008.07.006. [DOI] [PubMed] [Google Scholar]
- Marshall V, Longwell L, Goldstein M, Swanson J. Family factors associated with aggressive symptomatology in boys with attention deficit hyperactivity disorder: A research note. Journal of Child Psychology & Psychiatry & Allied Disciplines. 1990;31:629–636. doi: 10.1111/j.1469-7610.1990.tb00802.x. doi:10.1111/1469-7610.ep11354738. [DOI] [PubMed] [Google Scholar]
- Moens E, Braet C, Soetens B. Observation of family functioning at mealtime: A comparison between families of children with and without overweight. Journal of Pediatric Psychology. 2007;32:52–63. doi: 10.1093/jpepsy/jsl011. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan P J, Mulert S. Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. International Journal of Obesity and Related Metabolic Disorders. 2002;26:123–31. doi: 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- Noller P, Callan V. Adolescents' perceptions of the nature of their communication with parents. Journal of Youth & Adolescence. 1990;19:349–362. doi: 10.1007/BF01537077. [DOI] [PubMed] [Google Scholar]
- Noller P, Feeney J. Handbook of Family Communication. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 2003. Studying family communication: Multiple methods and multiple sources; pp. 31–50. [Google Scholar]
- Ogden C L, Carroll M D, Kit B K, Flegal K M. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010 [comparative study] JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. doi:10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlet Fisher J, Mitchell D C, Wright H S, Birch L L. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. Journal of the American Dietetic Association. 2002;102:58–64. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick H, Hennessy E, McSpadden K, Oh A. Parenting styles and practices in children's obesogenic behaviors: Scientific gaps and future research directions. Childhood Obesity. 2013;9(Suppl 1):S73–S86. doi: 10.1089/chi.2013.0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto A M, Fava J L, Raynor H A, LaRose J G, Wing R R. Development and validation of the weight control strategies scale. Obesity (Silver Spring) 2013;21:2429–2436. doi: 10.1002/oby.20368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton B, Cole M, Galbraith J, Li X, Pendleton S, Cottrel L, Marshall S, Wu Y, Kaljee L. Randomized trial of a parent intervention: Parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics & Adolescent Medicine. 2004;158:947–955. doi: 10.1001/archpedi.158.10.947. [DOI] [PubMed] [Google Scholar]
- Steele R G, Aylward B S, Jensen C D, Cushing C C, Davis A M, Bovaird J A. Comparison of a family-based group intervention for youths with obesity to a brief individual family intervention: A practical clinical trial of positively fit. Journal of Pediatric Psychology. 2012;37:53–63. doi: 10.1093/jpepsy/jsr057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout R. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol Supplement. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Wadden T A, Stunkard A J, Rich L, Rubin C J, Sweidel G, McKinney S. Obesity in black adolescent girls: A controlled clinical trial of treatment by diet, behavior modification, and parental support. Pediatrics. 1990;85:345–352. [PubMed] [Google Scholar]
- White M A, Martin P D, Newton R L, Walden H M, York-Crowe E E, Gordon S T, Ryan D H, Williamson D A. Mediators of weight loss in a family-based intervention presented over the internet. Obesity Research. 2004;12:1050–1059. doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris M A, Buckloh L M, Mertlich D, Lochrie A S, Taylor A, Sadler M, White N H. Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior Therapy. 2008;39:33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Zeller M H, Reiter-Purtill J, Modi A C, Guzwiler J, Vannatta K, Davies W H. A controlled study of critical parent and family factors in the obesigenic environment. Obesity. 2007;15:126–136. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]