Abstract
Study Objectives:
To estimate the prevalence and health correlates of insomnia symptoms and their association with comorbid mental disorders in a nationally representative sample of adolescents in the United States.
Design:
National representative cross-sectional study.
Setting:
Population-based sample from the US adolescents.
Measurements and Results:
A total of 6,483 individuals aged between 13–18 y in the National Comorbidity Survey-Adolescent Supplement (NCS-A) with both individual and parental reports of mental health were included in this study. Participants were classified with insomnia symptoms if they reported difficulty initiating sleep, difficulty maintaining sleep, and/or early morning awakening, nearly every day for at least 2 w in the past year. Nearly one-third of adolescents reported insomnia symptoms for at least 2 w during the previous year. Hispanic and black youth were significantly more likely to report insomnia symptoms (42.0% and 41.3%, respectively) than non-Hispanic white youth (30.4%). Adolescents with insomnia symptoms were at a higher risk for all classes of mental disorders {odds ratio [OR] (95% confidence interval [CI]: 3.4 (2.9–4.0)} including mood, anxiety, behavioral, substance use, and eating disorders, suicidality [OR (95% CI): 2.63 (1.34–5.16)], poor perceived mental health [OR (95% CI): 2.01 (1.02–3.96)], chronic medical conditions [OR (95% CI): 1.94 (1.55–2.43)], smoking [OR (95% CI: 2.60 (1.00–6.72)], and obesity [OR (95% CI: 1.46 (1.10–1.93)] than those without insomnia symptoms. Adolescents with insomnia symptoms and comorbid mental disorders manifested even greater rates of these indicators of negative health behaviors and disorders than those with mental disorders alone (P < 0.05).
Conclusions:
Insomnia symptoms are reported by one-third of adolescents in the general population. Insomnia symptoms, even in the absence of concomitant depression or other mental disorders, are associated with serious health conditions, risk factors, and suicidality. Comorbid mental disorders potentiate the effect of insomnia symptoms on both physical and mental health. Further evaluation of the causes and effective interventions to reduce insomnia symptoms may have a significant effect on public health.
Citation:
Blank M, Zhang J, Lamers F, Taylor AD, Hickie IB, Merikangas KR. Health correlates of insomnia symptoms and comorbid mental disorders in a nationally representative sample of US adolescents. SLEEP 2015;38(2):197–204.
Keywords: adolescent, chronic medical conditions, insomnia, mental disorders, suicidality
INTRODUCTION
The high prevalence, persistence, and pervasive health consequences of sleep problems in the general population1–3 highlight the importance of early detection and intervention of insomnia. Prevalence estimates of insomnia symptoms in adolescents in the United States range from 3.4–34.6% depending on the definition and method of assessment of insomnia or insomnia symptoms.4–7 Insomnia is more common among females than males, and increases with age5,8 and across ethnic subgroups.4 Insomnia symptoms are often persistent in youth, with about 21–60% of youth reporting chronic symptoms across a follow-up period of 1–4 y.4,8–10 Persistence tends to be more common with increased age, female sex, and comorbid depressive symptoms.
The three major symptoms of insomnia, including difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening,11 tend to co-occur both cross-sectionally and over time.12 However, the persistence of the three subtypes of insomnia symptoms and their effect on the chronicity of insomnia has not been explored in adolescents from the general community.
Similar to adults with insomnia, adolescents with insomnia symptoms are at higher risk for numerous negative outcomes, including poor health perception and suicidality,13–17 several chronic medical conditions,18,19 and negative health behaviors such as smoking.8 Even after adjustment for insomnia symptoms as a criterion for some mental disorders,20 there is substantial comorbidity between insomnia symptoms with major depression,18 anxiety disorders,18 attention-deficit/hyperactivity disorder (ADHD),21 and substance abuse.19 To date, there are no studies of the magnitude of insomnia symptoms that simultaneously account for the potent association between insomnia the full range of mental disorders in a general population sample of US adolescents.
The goals of the current study are:
To describe the prevalence of insomnia symptoms in a nationally representative sample of US adolescents and its demographic correlates;
To identify comorbid mental disorders associated with insomnia symptoms;
To evaluate the effect of insomnia symptoms with and without concomitant mental disorders in US youth.
METHODS
Sample and Procedure
The National Comorbidity Survey-Adolescent Supplement (NCS-A) is a nationally representative, face-to-face survey of adolescents age 13–18 y in the continental United States. Details about the design, sampling, and measures have been published elsewhere.22–24 In brief, the NCS-A was based on both household and school samples that were weighted to the general census for youths age 13–18 y. This report includes the subsample of youth on which parent informants provided information on their physical and mental health. This paper is based on the sample of 6,483 adolescents with direct household interviews and parent reports on their behavior and physical and mental health. The response rate for the primary data on insomnia based on adolescent interviews was 82.9%. Complete parent reports were obtained from 48.3% of the sample. Sociodemographic variables in the NCS-A included age, sex, and race/ethnicity.
Assessment of Insomnia Symptoms
Three subtypes of insomnia symptoms specified in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), including difficulty initiating sleep (DIS), difficulty maintaining sleep (DMS), and early morning awakening (EMA), were assessed in the Sleep Module of the NCS-A. The participants were asked whether they had a time lasting for 2 w or longer in the past 12 mo when they had any of the following problems with their sleep: (1) problems getting to sleep (DIS)—taking a long time to fall asleep nearly every night; (2) problems staying asleep (DMS)—waking up nearly every night and taking a long time to get back to sleep; or (3) problems waking too early (EMA)—waking up nearly every morning much earlier than wanted. In addition, the duration of these insomnia symptoms based on the number of weeks during the past year was assessed. We also examined each of the three types of insomnia symptoms by duration: less than 4 w; 4–11 w; and greater than or equal to 12 w.
Assessment of Mental Disorders
As described in previous publications, mental disorders were defined by DSM-IV criteria based on a modification of the fully structured World Health Organization Composite International Diagnostic Interview. For this report, we examine disorders that were present during the past 12 mo.22,23 Behavior disorders, including ADHD, conduct disorder, and oppositional defiant disorder, were based on parent report whreas all other mental disorders were ascertained through direct interview with the adolescent according to conventions for informant validity in adolescents.24 In these analyses, we evaluate the major classes of mental disorders including mood disorders (major depression, dysthymia, mania, and hypo-mania); anxiety disorders (separation anxiety, panic, phobias, generalized anxiety, posttraumatic stress disorder); behavior disorders (attention deficit disorder, conduct disorder or oppositional defiant disorder; substance use disorders (drug or alcohol abuse or dependence); and eating disorders (binge eating, bulimia).
Assessment of Physical Conditions, Suicidality, Injury, Substance Use, and Perceived Health
The diagnostic interview also included modules on injuries, health, services, and chronic health conditions over the past 12 mo. For chronic health conditions, participants were asked for a lifetime history of a series of physical conditions on a checklist by the interviewer, and, if so, whether they still had or received treatment for these problems at any time during the past 12 mo. A total of 14 common chronic medical conditions were assessed in the NCS-A study. Because of the limited number of cases (n < 50), human immunodeficiency virus infection, diabetes, cancer, and herpes were not included in the analyses. Participants who endorsed insomnia symptoms during the past 12 mo were considered as cases whereas the others were considered as controls.
Because of the possible sensitivity to questions relating to suicidal ideation, plans, and attempts, literate adolescents were not asked these questions directly, but rather read the questions and responded to them separately. For those participants who were illiterate, the suicidality questions were asked in the face-to-face interview. Suicidality was defined as any suicidal thought, plan or attempt. All variables for physical conditions, suicidality, injury, substance use, and perceived health were dichotomous.
Determination of Obesity
Body mass index (BMI, kg/m2) was calculated from the self-reported weight and height. BMI was transformed into BMI z score according to the 2000 Centers for Disease Control and Prevention growth charts for the United States. Participants with a BMI z score above the 95th percentile were considered obese.
Statistical Analysis
Package for the Social Sciences (SPSS) 19.0 for Windows (SPSS Inc, Chicago, IL, USA) was used for statistical analyses, and all analyses accounted for clustering, weighting, and stratification of complex sampling design features to accurately calculate point estimates and standard errors. Descriptive statistics were given as means ± standard errors and frequencies (percentages) where appropriate. The associations between any insomnia symptoms (Yes vs. No)/insomnia symptoms with and without mental disorders (four groups: no insomnia symptoms and no mental disorders, insomnia symptoms only, mental disorder only, and insomnia symptoms + mental disorders) and sociodemographic characteristics were tested by chi-square tests. The associations across insomnia symptoms with and without comorbid mental disorders and negative consequences were tested by chi-square tests and logistic regression. Logistic regression was used to determine the odds ratios (ORs) and 95% confidence intervals (CIs) for the associations of insomnia symptoms with and without co-morbid mental disorders (independent variable) and negative consequences (dependent variables) as assessed in the current study. P values of less than 0.05 were considered statistically significant.
RESULTS
Distribution of Insomnia Symptoms with and without Comorbid Mental Disorders and its Sociodemographic Correlates
Table 1 presents the weighted prevalence rates of insomnia symptoms by sociodemographic correlates. Participants with any insomnia symptoms were, in general, more likely to be female, and either Hispanic or black. Similar trends were also found among those with comorbid mental disorders and insomnia. Insomnia symptoms alone (without comorbid mental disorders) were most prevalent in adolescents of non-Hispanic black origin, with equivalent proportions of males and females.
Table 1.
Sociodemographic characteristics of insomnia symptoms in US adolescents (n = 6,483).
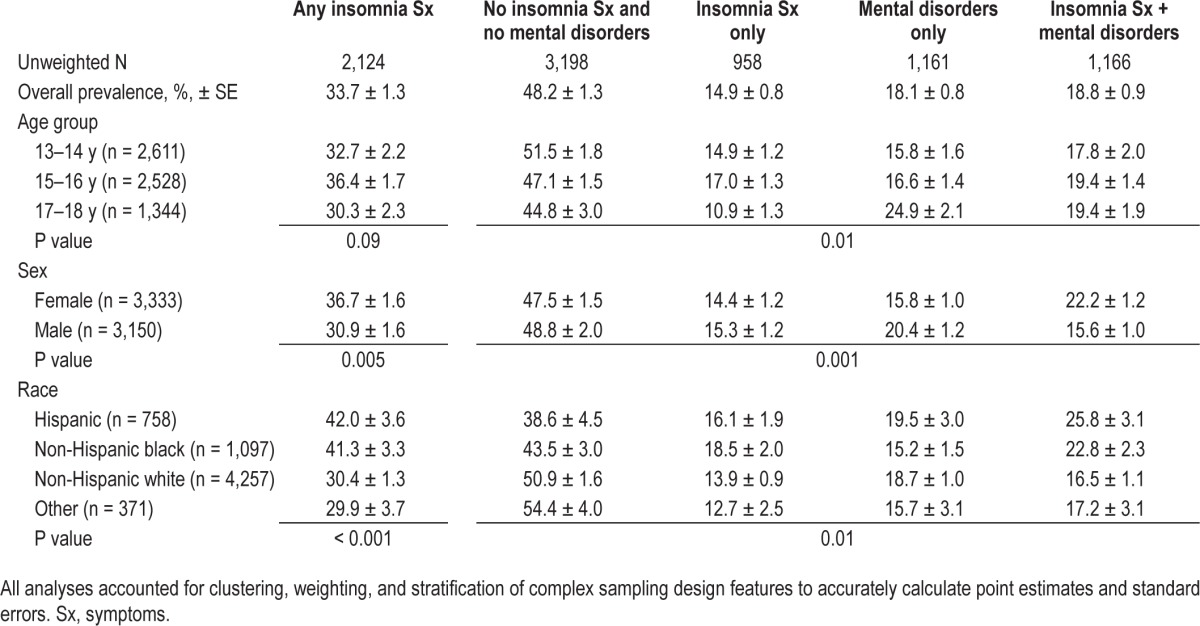
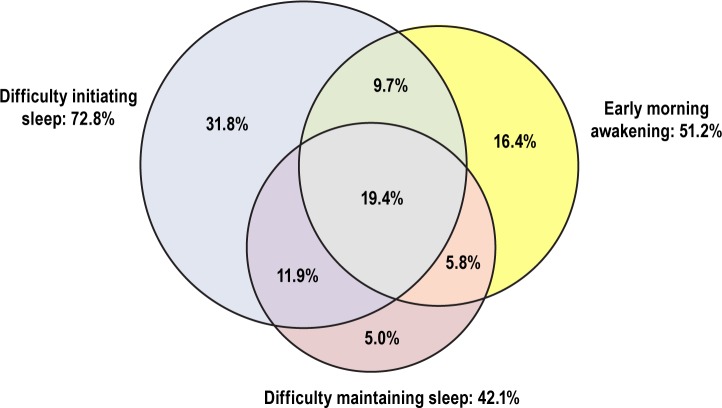
Figure 1 shows the proportions of each of the insomnia symptoms and their combinations among adolescents with insomnia. Among those with any insomnia symptoms (n = 2,124), 72.8% had DIS, 51.3% had EMA, and 42.1% had DMS. In terms of the number of insomnia symptoms, 53.2% had only one symptom, 27.4% had two symptoms, and 19.4% had all three insomnia symptoms (Table S1, supplemental material). DIS was the most common symptom that occurred alone (31.8%), whereas EMA alone was much less frequent (16.4%) and DMS nearly always co-occurred with the other two symptoms (95%). Whereas females had greater rates of DIS and DMS, there was no sex difference in EMA (Table S1).
Figure 1.
Distribution (percentage) of insomnia symptoms among adolescents with insomnia (n = 2,124; percentage of participants with insomnia who report DIS, DMS, and/or EMA).
Associations between any Insomnia Symptoms and Mental Disorders
Table 2 presents the associations between classes of mental disorders among those with and without insomnia symptoms. The prevalence of all of the classes of mental disorders was greater among youth with any insomnia symptoms compared to those without any insomnia symptoms. The highest prevalence rates of comorbid mental disorders were seen for anxiety disorders (33.4%), followed by behavior disorders (23.9%) and mood disorders (20.7%). Both the crude ORs and the sociodemographic factor-adjusted ORs comparing those with and without insomnia symptoms were significantly elevated for all disorder classes. The adjusted OR between insomnia symptoms and specific mental disorders ranged from 1.88 to 7.85 with a median of 4.09 and an interquartile range of 2.70–5.43.
Table 2.
Prevalence of mental disorders in adolescents with and without insomnia symptoms (n = 6,483).
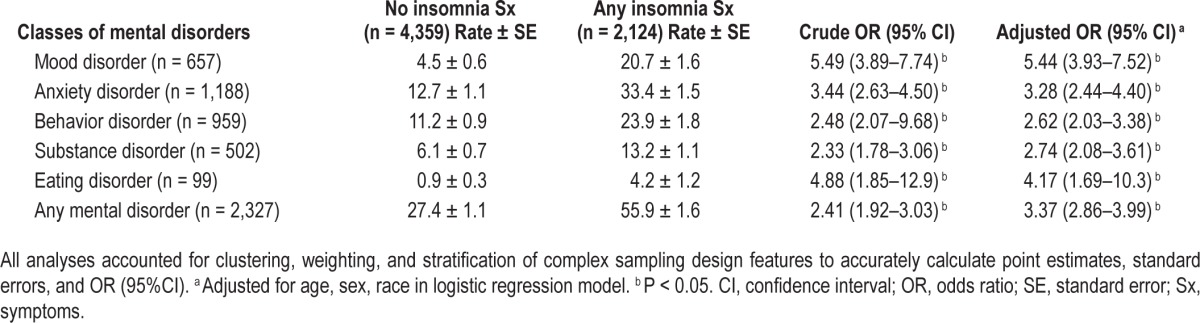
Figure 2 shows the duration of insomnia symptoms during the past year by the number of symptoms and comorbid mental disorders. There was a direct association between the number of symptoms of insomnia and duration; those with one symptom tended to have duration less than 4 w (acute insomnia), whereas those with three symptoms tended to duration greater than 12 w (persistent insomnia) (Figure 2A). Similarly, participants with mental disorders tended to have higher rates of persistent insomnia symptoms (42.0%) compared to those without mental disorders (31.0%) (Figure 2B).
Figure 2.
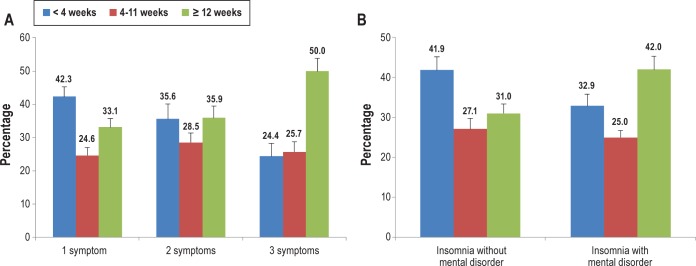
Duration of insomnia in weeks by number of insomnia symptoms (A) and comorbid mental disorders (B) among youth with insomnia symptoms (n = 2,124).
Negative Health Correlates of Insomnia Symptoms
Table 3 shows the rates and associations of behavioral and health conditions with insomnia symptoms stratified by the presence or absence of comorbid mental disorders. In general, when compared with controls who had neither insomnia symptoms nor mental disorders, participants with comorbid mental disorders had the highest rates of negative health correlates, followed by participants with mental disorders alone, and then by participants with insomnia alone. Specifically, adolescents with insomnia symptoms alone had a statistically significant increased risk of suicidality (OR: 2.63, 95% CI: 1.34–5.16), poorer perceived mental health (OR: 2.01, 95% CI: 1.02–3.96), and a trend toward increased tobacco use (OR: 2.60, 95% CI: 1.00–6.72), but did not show significantly increased rates of injuries or poor perceived physical health. When compared to those with mental disorders alone, those with comorbid insomnia symptoms had significantly greater rates of suicidal ideation and behavior, and poorer perceived physical and mental health (P < 0.05) (Table 3).
Table 3.
Correlates of insomnia symptoms by presence or absence of mental disorders (n = 6,483).
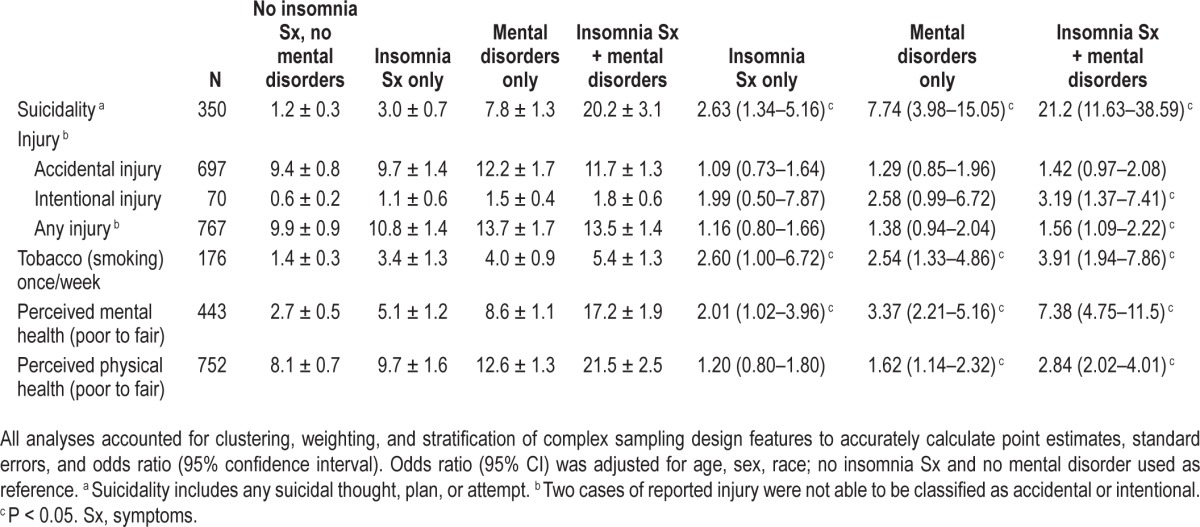
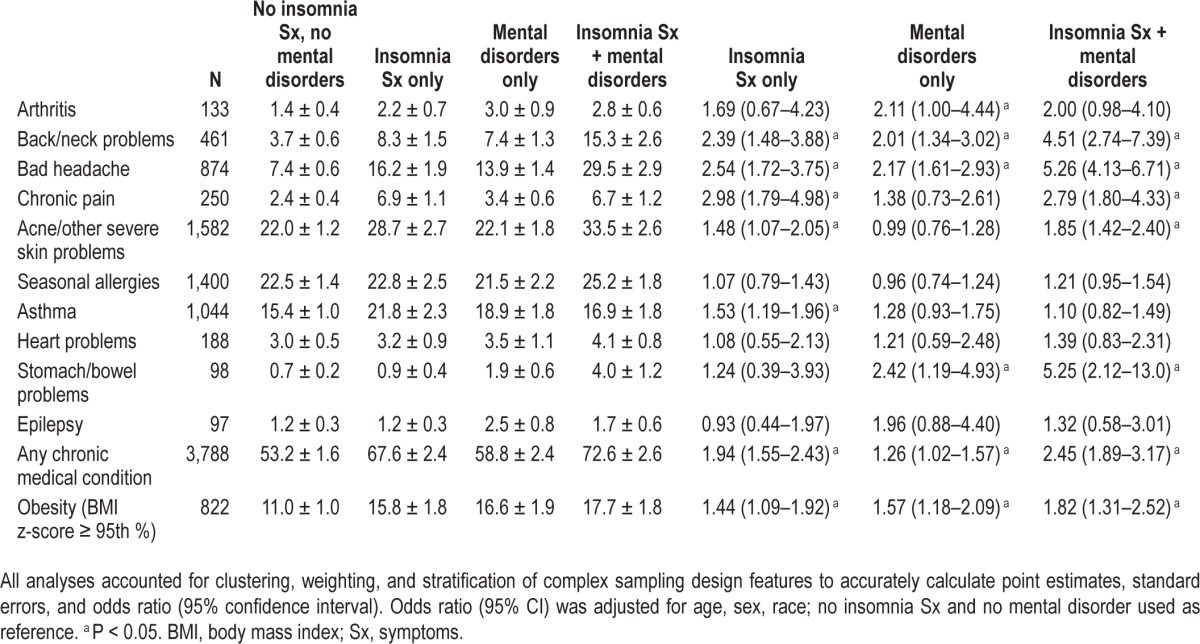
Table 4 shows the rates and associations of chronic medical conditions with insomnia symptoms and mental disorders. Those with insomnia symptoms alone had an increased risk of several chronic medical conditions, most notably, pain-related disorders (arthritis, back and neck problems, bad headaches, and any other chronic pain). In addition, when compared with controls, adolescents with insomnia symptoms alone also had greater rates of acne or other severe skin problems (OR 1.48, 95% CI: 1.07–2.05), asthma (OR 1.53, 95% CI: 1.19–1.96), greater rates of obesity (defined as BMI z score greater than the 95th percentile) (OR 1.46, 95% CI: 1.10–1.93) and any chronic medical condition (OR 1.94, 95% CI: 1.55–2.43, Table 3). Rates of these conditions were further increased in the comorbid insomnia symptoms group compared with those with mental disorders alone (P < 0.05) (Table 4).
Table 4.
Prevalence and association of physical disorders with insomnia symptoms by presence or absence of mental disorders (n = 6,483).
DISCUSSION
Summary of Findings
This is the first study of a nationally representative sample of US youth that examines the prevalence, duration, and health and behavioral correlates of insomnia symptoms alone and in combination with mental disorders. We show that (1) insomnia symptoms are highly prevalent in the general population of US adolescents; (2) duration of insomnia symptoms increases as a function of the number of symptoms and presence of comorbid mental disorders; (3) insomnia symptoms alone are associated with pervasive negative health conditions including comorbid chronic medical conditions, suicidality, tobacco use, obesity, and poorer perceived mental health; and (4) adolescents with insomnia symptoms comorbid with mental disorders are at even greater risk for several of these negative health problems.
About one-third of US adolescents report that they have suffered from insomnia symptoms during the past 12 mo. Although insomnia symptoms were closely associated with mental disorders, nearly one-half of those with insomnia symptoms did not have comorbid mental disorders within the past 12 mo, indicating the significance of insomnia symptoms as a distinct entity. Females had greater rates of insomnia symptoms than males as shown in previous studies5–7; however, we found that this sex difference was attributable to comorbid mental disorders, particularly anxiety and depression in girls.
There were also greater rates of insomnia symptoms in Hispanics and non-Hispanic blacks, corroborating findings from earlier studies of adults based on self-reports25 as well as others that were based on objective measures of sleep patterns.26 In fact, the latter study demonstrated lower mean sleep duration, lower sleep efficiency, and higher sleep latency among young adult blacks than among their white counterparts, even after controlling for various socioeconomic and demographic factors. By contrast, an earlier community study of adolescents6 in Texas did not demonstrate ethnic differences in insomnia, suggesting that future studies explore this issue in more depth.
Correlates of Insomnia Symptoms
The pervasive comorbidity between insomnia symptoms across all classes of mental disorders highlights the importance of consideration of the full range of emotional, cognitive, and behavioral correlates of insomnia that is not solely associated with depression that has often been the sole focus of previous community based research on insomnia. In fact, insomnia symptoms were much more common among those with anxiety disorders than those with mood disorders.
The increased reporting of suicidal ideation and behavior associated with insomnia symptoms is perhaps the most serious correlate of insomnia symptoms as previously demonstrated in both adolescents13–17 and adults.27,28 However, few of these earlier studies actually controlled for comorbid mental disorders. These findings extend this observation to a community sample of adolescents and demonstrate that insomnia symptoms confer an increased risk of suicidality, even in the absence of comorbid mental disorders.14 The greater severity of insomnia symptoms among those with comorbid mental disorders may explain the additional increase in suicidal risk in this subgroup of youth.29,30 These findings suggest that insomnia symptoms should be considered as a modifiable risk factor for suicidality31 that should be considered independent of concomitant mental disorders. Further studies are warranted to investigate the effect of alleviation of insomnia symptoms, either by medication or cognitive behavioral therapy for insomnia on suicidality.
Recent cross-sectional studies have shown that insomnia symptoms in adolescents are closely associated with smoking and substance misuse. In the current study, we confirmed earlier findings regarding increased risk of tobacco use32–34 in all three subgroups with insomnia symptoms and/or mental disorders when compared with controls. Rates of tobacco use were similar for those with insomnia symptoms only and the mental disorders-only groups, suggesting that insomnia symptoms alone may be an important risk factor and potential target for prevention of smoking in adolescents. Although the stimulant property of tobacco is an obvious potential explanation for this association, the bidirectional influence of smoking on insomnia symptoms suggests that they may have a more complex relationship.8,35
Congruent with previous research, this study demonstrates that sleep problems are associated with poor perceived mental, but not perceived physical health.36–39 Insomnia symptoms and mental disorders seem to contribute equally to poor perceived mental health, and there is an additive effect when insomnia symptoms are comorbid with mental disorders. Although individuals with pure insomnia symptoms did not have poorer perceived physical health, they were still more likely to have chronic medical conditions. As shown in an earlier study,40 insomnia symptoms alone were strongly associated with pain disorders. The relationship of chronic pain and insomnia symptoms has been postulated to be bidirectional.41 Although pain could make it difficult for a person to initiate or maintain sleep, it may also be exacerbated by a lack of sufficient sleep. Dysregulation of mesolimbic dopamine has been suggested as a cause for the co-occurrence of insomnia, pain, and depression42; however, other research does not demonstrate mediation of the relationship between insomnia symptoms and pain by depression.43,44
Clinical Implications
Insomnia symptoms or sleep difficulties are considered as diagnostic indictors of mental disorders.20 Indeed, the current study shows that over half of those with insomnia symptoms also have comorbid mental disorders, thereby demonstrating the close link between sleep problems and mental disorders. However, recent studies have shown that insomnia (symptoms) should also be considered as an independent entity or entities, because of their unique natural history and independent treatment.3,45 Prospective studies support a bi-directional association between insomnia symptoms and depression/anxiety in both adults and adolescents.46,47 In this regard, distinctions between symptom presentation and negative health and behavioral correlates of insomnia symptoms from those of major depression in the current study support the independence of insomnia symptoms from major depression and anxiety disorders. However, insomnia symptoms appear to potentiate the consequences of mental disorders, which indicate that evaluation of insomnia symptoms should be a critical component of the clinical evaluation of mood and other mental disorders in the youth.
Strengths and Limitations
Strengths of this study include the systematic assessment of consequences, sufficient statistical power, face-to-face interviews, and reliable measures of mental disorders and suicidality. However, there are also several limitations in our study. First, the cross-sectional design precludes determination of the link between insomnia symptoms and their consequences. Future interventional studies may shed light on the causal association and the potential reversibility of the consequences after treatment. Second, the diagnostic interview only measured insomnia symptoms rather than assessing full criteria for all of the DSM-IV criteria for insomnia as a sleep disorder. Because the current study used broad definitions for insomnia symptoms, a duration of 2 w in the past 12 mo and absence of requirement of daytime functional impairment, the estimated prevalence of insomnia symptoms might be somewhat inflated. However, because the prevalence rate of insomnia symptoms in the current study is comparable to that of prior studies with full diagnostic criteria,5–7 it is unlikely that our findings are overestimates of the true prevalence. Future analyses are warranted to determine how the duration of insomnia symptoms and the inclusion of daytime functional impairment might influence the negative consequences of insomnia symptoms. Furthermore, although the measures of insomnia symptoms were generated from the three core subtypes of insomnia, their validity has not been tested.
CONCLUSIONS
The current study provides evidence that insomnia symptoms occur frequently in the absence of mental disorders and are associated with substantial chronic health problems and behaviors in US adolescents. Furthermore, when comorbid with mental disorders, insomnia symptoms tend to potentiate their negative health consequences. The association between suicidal ideation and attempts is the most disturbing correlate of insomnia. Further evaluation of the mechanisms for these associations and development of effective interventions should have a significant effect on public health.
DISCLOSURE STATEMENT
This was not an industry supported study. The National Comorbidity Survey-Adolescent Supplement (NCS-A) was supported by the National Institute of Mental Health (U01-MH60220) and (ZIA MH 002808), and the National Institute of Drug Abuse (R01DA016558). The NCS-A was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. This work was supported by the Intramural Research Program of the National Institute of Mental Health. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. government. The authors have indicated no financial conflicts of interest.
SUPPLEMENTAL MATERIAL
Sociodemographic characteristics of insomnia in adolescents by type and number of insomnia symptoms (n = 6,483).
REFERENCES
- 1.Walsh JK, Coulouvrat C, Hajak G, et al. Nighttime insomnia symptoms and perceived health in the America Insomnia Survey (AIS) Sleep. 2011;34:997–1011. doi: 10.5665/SLEEP.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth T, Coulouvrat C, Hajak G, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69:592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 3.Buysse DJ. Chronic insomnia. Am J Psychiatry. 2008;165:678–86. doi: 10.1176/appi.ajp.2008.08010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts RE, Roberts CR, Chan W. Persistence and change in symptoms of insomnia among adolescents. Sleep. 2008;31:177–84. doi: 10.1093/sleep/31.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–56. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 6.Roberts RE, Roberts CR, Chan W. Ethnic differences in symptoms of insomnia among adolescents. Sleep. 2006;29:359–65. doi: 10.1093/sleep/29.3.359. [DOI] [PubMed] [Google Scholar]
- 7.Roberts RE, Lee ES, Hemandez M, Solari AC. Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas. Sleep. 2004;27:751–60. doi: 10.1093/sleep/27.4.751. [DOI] [PubMed] [Google Scholar]
- 8.Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000;106:E23. doi: 10.1542/peds.106.2.e23. [DOI] [PubMed] [Google Scholar]
- 9.Fricke-Oerkermann L, Pluck J, Schredl M, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007;30:1371–7. doi: 10.1093/sleep/30.10.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gregory AM, O'Connor TG. Sleep problems in childhood: a longitudinal study of developmental change and association with behavioral problems. J Am Acad Child Adolesc Psychiatry. 2002;41:964–71. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Sleep Medicine. Diagnostic and coding manual. 2nd edition. Westchester, IL: American Academy of Sleep Medicine; 2005. International classification of sleep disorders. [Google Scholar]
- 12.Hohagen F, Kappler C, Schramm E, Riemann D, Weyerer S, Berger M. Sleep onset insomnia, sleep maintaining insomnia and insomnia with early morning awakening--temporal stability of subtypes in a longitudinal study on general practice attenders. Sleep. 1994;17:551–4. [PubMed] [Google Scholar]
- 13.Choquet M, Menke H. Suicidal thoughts during early adolescence: prevalence, associated troubles and help-seeking behavior. Acta Psychiatr Scand. 1990;81:170–7. doi: 10.1111/j.1600-0447.1990.tb06474.x. [DOI] [PubMed] [Google Scholar]
- 14.Tishler CL, McKenry PC, Morgan KC. Adolescent suicide attempts: some significant factors. Suicide Life Threat Behav. 1981;11:86–92. doi: 10.1111/j.1943-278x.1981.tb00907.x. [DOI] [PubMed] [Google Scholar]
- 15.Bailly D, Bailly-Lambin I, Querleu D, Beuscart R, Collinet C. [Sleep in adolescents and its disorders. A survey in schools] L'Encephale. 2004;30:352–9. doi: 10.1016/s0013-7006(04)95447-4. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychology. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. J Psychosom Res. 2002;53:561–9. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- 18.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 19.Shibley HL, Malcolm RJ, Veatch LM. Adolescents with insomnia and substance abuse: consequences and comorbidities. J Psychiatr Pract. 2008;14:146–53. doi: 10.1097/01.pra.0000320113.30811.46. [DOI] [PubMed] [Google Scholar]
- 20.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gau SS, Chiang HL. Sleep problems and disorders among adolescents with persistent and subthreshold attention-deficit/hyperactivity disorders. Sleep. 2009;32:671–9. doi: 10.1093/sleep/32.5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Avenevoli S, Costello EJ, et al. The National Comorbidity Survey Adolescent Supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry. 2009;48:380–5. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merikangas KR, Avenevoli S, Costello EJ, Koretx D, Kessler RC. The National Comorbidity Survey Adolescent Supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48:367–9. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grills AE, Ollendick TH. Issues in parent-child agreement: the case of structured diagnostic interviews. Clin Child Fam Psychol Rev. 2002;5:57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- 25.Bixler EO, Vgontzas AN, Lin HM, Vela-Bueno A, Kales A. Insomnia in central Pennsylvania. J Psychosom Res. 2002;53:589–92. doi: 10.1016/s0022-3999(02)00450-6. [DOI] [PubMed] [Google Scholar]
- 26.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 27.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43:526–31. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li SX, Lam SP, Yu MW, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71:1440–6. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 29.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35:61–8. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang J, Lam SP, Li SX, et al. Long-term outcomes and predictors of chronic insomnia: a prospective study in Hong Kong Chinese adults. Sleep Med. 2012;13:455–62. doi: 10.1016/j.sleep.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 31.McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. 2013;15:389. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Med. 2009;10:787–96. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug Alcohol Depend. 2001;64:1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 34.Mak KK, Ho SY, Thomas GN, et al. Smoking and sleep disorders in Chinese adolescents. Sleep Med. 2010;11:268–73. doi: 10.1016/j.sleep.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 35.Zhang J, Lam SP, Li SX, Li AM, Lai KY, Wing YK. Longitudinal course and outcome of chronic insomnia in Hong Kong Chinese children: a 5-year follow-up study of a community-based cohort. Sleep. 2011;34:1395–402. doi: 10.5665/SLEEP.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Furihata R, Uchiyama M, Takahashi S, et al. The association between sleep problems and perceived health status: a Japanese nationwide general population survey. Sleep Med. 2012;13:831–7. doi: 10.1016/j.sleep.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 37.Zammit GK, Weiner J, Damato N, Sillup GP, McMillan CA. Quality of life in people with insomnia. Sleep. 1999;22(Suppl 2):S379–85. [PubMed] [Google Scholar]
- 38.Hajak G. Epidemiology of severe insomnia and its consequences in Germany. Eur Arch Psychiatry Clin Neurosci. 2001;251:49–56. doi: 10.1007/s004060170052. [DOI] [PubMed] [Google Scholar]
- 39.Leger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63:49–55. doi: 10.1097/00006842-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Ohayon MM. Relationship between chronic painful physical condition and insomnia. J Psychiatr Res. 2005;39:151–9. doi: 10.1016/j.jpsychires.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 41.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 42.Finan PH, Smith MT. The comorbidity of insomnia, chronic pain, and depression: dopamine as a putative mechanism. Sleep Med Rev. 2013;17:173–83. doi: 10.1016/j.smrv.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lateef T, Swanson S, Cui L, Nelson K, Nakamura E, Merikangas K. Headaches and sleep problems among adults in the United States: findings from the National Comorbidity Survey-Replication study. Cephalalgia. 2011;31:648–53. doi: 10.1177/0333102410390395. [DOI] [PubMed] [Google Scholar]
- 44.Zhang J, Lam SP, Li SX, et al. Insomnia, sleep quality, pain, and somatic symptoms: sex differences and shared genetic components. Pain. 2012;153:666–73. doi: 10.1016/j.pain.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 45.Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379:1129–41. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]
- 46.Luo C, Zhang J, Pan J. One-year course and effects of insomnia in rural Chinese adolescents. Sleep. 2013;36:377–84. doi: 10.5665/sleep.2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jansson-Frojmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64:443–9. doi: 10.1016/j.jpsychores.2007.10.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Sociodemographic characteristics of insomnia in adolescents by type and number of insomnia symptoms (n = 6,483).