Abstract
Study Objective:
Short sleep has been linked to increased risk for type 2 diabetes and incident cardiovascular disease and acute sleep restriction impairs insulin-mediated glucose disposal. Here, we examined whether indices of glucose metabolism vary with naturally occurring differences in sleep duration.
Design and Measures:
Subjects were midlife, nondiabetic community volunteers (N = 224; mean age 44.5 ± 6.6 y [range: 30–54]; 52% female; 89% white). Laboratory measures of insulin sensitivity (Si) and acute secretion (AIRg), glucose effectiveness (Sg), and disposition index (Di) were obtained from a 180-min, intravenous glucose tolerance test.
Results:
Shorter self-reported sleep duration (in hours) was associated with lower Si (P = 0.043), although an interaction of sleep duration with participant race (β = −0.81, P = 0.002) showed this association significant only in whites. Moreover, sex-stratified analyses revealed that shorter sleep duration predicted lower Si in white men (β = 0.29, P = 0.003) but not in white women (P = 0.22). Findings were similar for AIRg. The relationship between sleep duration and AIRg was moderated by race as well as sex, such that shorter sleep duration associated with greater insulin release only in white men (β = −0.28, P = 0.004). Sleep duration was unrelated to Sg and Di (P's > 0.05).
Conclusions:
Our findings suggest that shorter sleep duration may impair insulin sensitivity and beta-cell function in nondiabetic white men, possibly contributing to later type 2 diabetes and cardiovascular disease.
Citation:
Wong PM, Manuck SB, DiNardo MM, Korytkowski M, Muldoon MF. Shorter sleep duration is associated with decreased insulin sensitivity in healthy white men. SLEEP 2015;38(2):223–231.
Keywords: glucose metabolism, insulin sensitivity, minimal model, sex differences, sleep duration
INTRODUCTION
Chronic sleep restriction has become increasingly prevalent in modern society.1–3 Accumulating evidence from both cross-sectional and prospective studies associates short sleep with increased risk for obesity, the metabolic syndrome, type 2 diabetes, and incident cardiovascular disease.4–10 A possible pathway linking short sleep to increased disease risk involves the role of sleep in regulating glucose metabolism. Although mechanisms remain elusive, aspects of sleep appear to affect normal glucose homeostasis, such that reductions in sleep quality and duration impair both glucose utilization and glucose tolerance.1,11–15
Shorter sleep duration associates with insulin resistance across various patient samples, including children and adults with obesity and type 2 diabetes.16,17 In addition, experimental studies in healthy adults have shown that partial sleep restriction, generally of 4–5 h sleep/night over periods ranging 1 to 14 nights, rapidly reduces glucose tolerance and insulin sensitivity.11–15 Consistent with these findings, one community-based study showed shorter sleep duration among healthy adolescents was associated with elevated insulin resistance,18 although a similar association has not been reported in community-sampled, nondiabetic adults.19,20 Unlike these population studies that measure average sleep duration, sleep restriction in experimental studies is both acute and artificially induced, which may contribute in part to the conflicting results. Hence, further study is warranted to examine whether detrimental effects of sleep loss in the laboratory setting similarly manifest in free-living, healthy adults who experience habitual, naturally occurring sleep restriction.
That the effects of curtailed sleep on glucose metabolism in experimental investigations have not been shown to generalize to naturally occurring variation in sleep duration among similarly healthy adults may possibly be because of differences in their assessment of glucose metabolism. Robust measures of insulin sensitivity, such as the minimal model analysis of frequently sampled intravenous glucose tolerance test (IVGTT), are routinely employed in restricted-sleep protocols, whereas nonexperimental studies typically rely on the homeostatic model assessment of insulin resistance (HOMA-IR) which is derived from single measurements of plasma glucose and insulin level.21 Relative to gold-standard laboratory measures, however, HOMA-IR shows low sensitivity in differentiating beta-cell deficits from insulin resistance.21 In contrast, the IVGTT with minimal model analysis quantifies pancreatic response to artificially induced hyperglycemia and subsequent glucose disposal over hours and provides valid estimates of both insulin sensitivity and acute insulin response to glucose.22–26 To date, there is a lack of cross-sectional studies that have examined the relationship between sleep duration and assessment of glucose metabolism by IVGTT.
Finally, studies of sleep dynamics in free-living populations may be complicated by correlated variation in health behaviors or physical characteristics such as obesity. For instance, exercise habits, diet, and increased adiposity have all been linked to short sleep duration, as well as decreased insulin sensitivity and heightened risk for type 2 diabetes.27,28 Thus, it is important to examine whether these characteristics also contribute to any relationship between sleep duration and glucose metabolism in a community sample.
In a previous report, we found that self-reported short sleep was associated with presence of the metabolic syndrome in a community sample of healthy, midlife adults.5 Here, we evaluate the relationships between sleep duration and IVGTT-derived indices of glucose metabolism in a nondiabetic subset of the same sample. In addition, we examine whether demographic characteristics such as age, race, and sex moderate the effect of sleep duration on glucose metabolism. Last, exploratory analyses are included to assess whether caloric intake, average physical activity, and central adiposity may confound any relationship between habitual sleep curtailment and glucose metabolism.
DESIGN AND MEASURES
Subjects
Subjects were participants in the University of Pittsburgh's Adult Health and Behavior (AHAB) project, which provides a registry of behavioral and biological measurements collected over multiple laboratory sessions on midlife adults recruited from Allegheny County, Pennsylvania, via mass-mail solicitation. Data in the current study are based on a subset of non-diabetic AHAB participants who were recruited to complete an additional laboratory glucose tolerance test. All subjects were fluent English-speaking community volunteers aged 30 to 54 y. Participants were excluded from the study if they reported a clinical history of atherosclerotic cardiovascular disease, chronic kidney or liver disease, major neurological disorders, schizophrenia or other psychotic illnesses, or cancer treatment within the preceding year. Participants were also excluded if they reported current pregnancy or current use of insulin, glucocorticoid, antiarrhythmic, psychotropic, or prescription weight-loss medications. The University of Pittsburgh Institutional Review Board approved the protocol, and subjects gave informed consent.
Intravenous Glucose Tolerance Test
Subjects began the 3-h IVGTT between 07:00–09:00 following a 10-h overnight fast. Two intravenous (IV) catheters, one on each arm, were placed 20 min prior to a glucose infusion. Participants rested during these 20 min and then glucose (0.3 g/kg) was administered intravenously as a 50% dextrose solution over 1–2 min. Twenty minutes after the glucose infusion, a small dose of regular insulin (0.03 or 0.02 units/kg) was administered intravenously to facilitate the measurement of insulin sensitivity. Thirteen blood samples (4 mL each) were collected at the following times, expressed as minutes in relation to the glucose infusion: −5, 2, 4, 8, 19, 22, 30, 40, 50, 70, 100, 150, and 180, for a total volume of 48 mL. Serum glucose and insulin were measured in each sample. Blood glucose readings were also determined at bedside at 50, 100, and 180 min to monitor for hypoglycemia.
The data were evaluated for extreme or discrepant values prior to analysis. The resulting glucose and insulin levels were analyzed using the minimal model (Minmod Millennium Version 5.18) to determine four output variables of interest: Insulin sensitivity (Si) was calculated through an algorithm in Minmod that estimates the effect of the insulin dose in accelerating glucose uptake. The detailed mathematical equation for Si has been described previously.22,29 Noninsulin-mediated glucose removal (Sg), or glucose effectiveness, was quantified as the disappearance rate of glucose at the basal insulin level.22 The acute insulin response to glucose (AIRg), a measure of pancreatic beta-cell secretion, was calculated as the mean insulin concentration during the initial 10 min after the glucose infusion minus the mean basal insulin concentration.23 Finally, the disposition index (Di) was calculated as Si × AIRg and represents an index of beta-cell function that takes into account insulin sensitivity and the curvilinear relationship between Si and AIRg.
The IVGTT with minimal model analysis provides a valid measure of Si that is significantly correlated with results from the glucose clamp test, especially when used to assess non-diabetic individuals (r's = 0.53–0.89).23,30,31 Likewise, AIRg demonstrates reasonable validity (r = 0.75) compared to that measured from the hyperglycemic clamp.23 The current study utilized a validated reduced sample IVGTT protocol that was designed to lessen the number of samples required in the original IVGTT.26,29 Steil and colleagues demonstrated that in comparison with the full 22 sample IVGTT, a reduced sample IVGTT provides highly correlated measures of insulin sensitivity (Si; r = 0.95) and noninsulin mediated glucose removal (Sg; r = 0.85).26
Subsequent examination showed no effect of insulin units administered (0.03 versus 0.02 units/kg) on Si or Di (P's > 0.15).
Self-Reported Sleep Assessment
As described previously,5 self-reported sleep duration was obtained from administration of the Stanford Five-City Physical Activity Interview.32 Participants were asked to report the number of hours per night they had slept over the past 7 days and were asked separately about sleep duration on weeknights (Sunday-Thursday) and weekend nights (Friday and Saturday). Consistent with other studies of sleep duration and cardiometabolic risk,19,33 weekly average sleep duration was calculated as the weighted average of reported weeknight and weekend night durations: [((5 × weekday sleep duration) + (2 × weekend sleep duration))/7]. Sleep duration was entered as a continuous variable in all analyses.
Subject Demographics and Health Characteristics
Various participant demographics were assessed as potential moderators of the relationship between sleep duration and insulin sensitivity. Age, sex, race (non-Hispanic Caucasian, African American), and educational attainment were gathered via self-report.
Physical activity was measured using the Paffenbarger physical activity questionnaire.34 The questionnaire asks about activities in the past year defined as the daily distance walked, pace of walking, flights of stairs climbed, and the type, duration and frequency of exercise, sports, and other recreational activities. From reported activities, weekly total energy expenditures (total kilocalories) are estimated. The Paffenbarger questionnaire has adequate test-retest reliability (r = 0.72) and validity in comparison with other physical activity surveys,35 and also predicts risk for all-cause mortality.36
Dietary consumption was assessed by electronic interview. Two unannounced 24-h dietary telephone recalls (TRs) were administered and information was scored using the Nutrition Data System for Research software version 4.06, (released May 2003) developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN.37 The Obesity and Nutrition Research Center at the University of Pittsburgh provided training and technical support. The TR has been used extensively to estimate dietary intake in diverse samples.38,39 Given the unannounced aspect of the interviews, the TRs are favored over diary records because there is less likelihood that instrumentation would affect food consumption.40,41
Measurements were obtained of the participant's height, weight, and waist circumference (at the umbilicus). Blood pressure was calculated as the mean of two consecutive readings obtained in the right arm, in a seated position, and following 10 min rest. Study staff also collected a venous blood sample, medication usage, and health status at the time of data collection.
Glucose and insulin concentrations were measured at the Heinz Nutrition Laboratory, University of Pittsburgh Graduate School of Public Health, which has met criteria of the Centers for Disease Control and Prevention—National Heart, Lung, and Blood Institute Lipid Standardization Program since 1982. Concentration of serum glucose was quantified by an enzymatic method in a procedure similar to that described by Bondar and Mead,42 and the coupled enzyme reactions catalyzed by hexokinase and glocse-6-phosphate dehydrogenase was used. The coefficient of variation (CV) between runs was 2.0%. The intra-assay CV was 1.6%.
Serum insulin was measured with a radioimmunoassay procedure developed by Linco Research, Inc. Cross-reactivity of the antibody with human proinsulin is less than 0.2%. The CV between runs was 8.2 ± 0.7%. The intra-assay CV was 7.0%.
Statistical Analysis
Data were analyzed with the SPSS v20 software package (Version 20.0., IBM Corporation, Armonk, NY). Because of a positive skew in the distributions of Si, AIRg, and Di, the distributions were normalized by log transformation (x' = lg10(x)). Sleep duration as well as Sg were entered as untransformed variables in the analyses. Correlational values (r's) reported are based on bivariate correlations unless indicated otherwise.
Multiple hierarchical linear regression analyses were used to test the effect of sleep duration on IVGTT-derived indices. The primary model examined the effect of sleep duration on Si, AIRg, Sg, and Di after controlling for age, race, and sex. Subsequently, three separate models examined whether age, race, and/or sex modified the effect of sleep duration. In addition, the sample was stratified by demographic variables for additional analyses (e.g., effect of sleep duration among white males). A supplementary logistic regression analysis was also conducted to examine if shorter sleep duration, entered as a continuous variable, predicted to relatively impaired insulin sensitivity in white men. Similar to previous reports on healthy adults, impaired insulin sensitivity was defined as the lower quartile of the sample distribution of Si values.43,44 In this model, a dichotomous outcome variable was implemented such that white male participants were categorized as either meeting criteria for relatively impaired Si (< 25th percentile) or not (> 25th percentile). Last, a linear regression model was conducted to examine the effect of sleep duration specifically in white men, after controlling for waist circumference, physical activity, and caloric intake. A detailed outline of the specific covariates and predictor variables entered per regression model are described in the results in the next paragraph. A P value of 0.05 was used as the threshold for statistical significance.
RESULTS
Subject Characteristics
A total of 308 participants were originally recruited for this study. A total of 65 participants were excluded because of: missing physical activity and/or food intake data (n = 13), missing sleep data (n = 1), incomplete laboratory sessions (n = 33), symptomatic hypoglycemia during the IVGTT (n = 14), error during the laboratory procedure (n = 1; the participant was noted to have received insulin prior to the IVGTT), indication of diabetes as determined from glucose level (fasting glucose of 131 mg/dL; n = 1), and biologically implausible IVGTT outcomes (n = 2; AIRg = −64.95; Si = 109.46). Thus, the final sample consisted of 244 participants.
Table 1 reports the mean IVGTT outcomes stratified by sex. Partial correlations controlling for age, race, and sex revealed that Si and AIRg were each correlated with average physical activity, calories consumed, and waist circumference and Sg was correlated with average physical activity and waist circumference (P's < 0.05; Table 1). Characteristics of the sample, stratified by sex, are shown in Table 2. Fifty-five percent of the sample was overweight or obese, as defined by a body mass index (BMI; kg/m2) of 25 or greater (sample range: 14.0–37.6).
Table 1.
Summary of intravenous glucose tolerance test-derived parameters of glucose metabolism by sex and correlations with health behaviors and central adiposity.
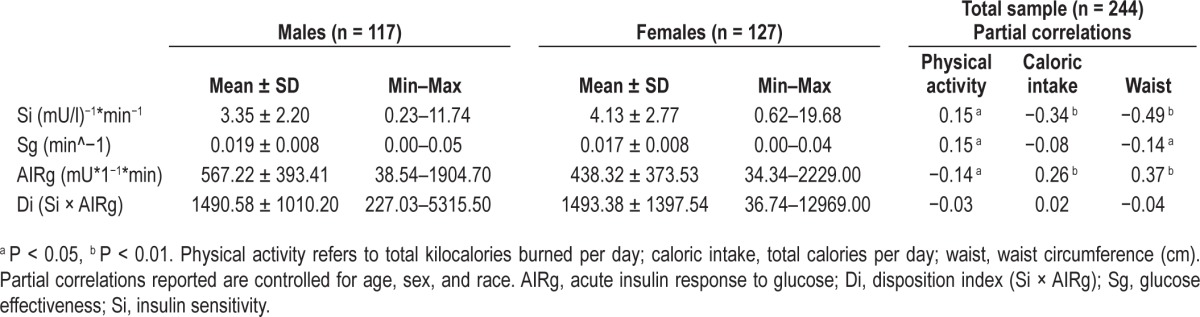
Table 2.
Participant characteristics by sex.
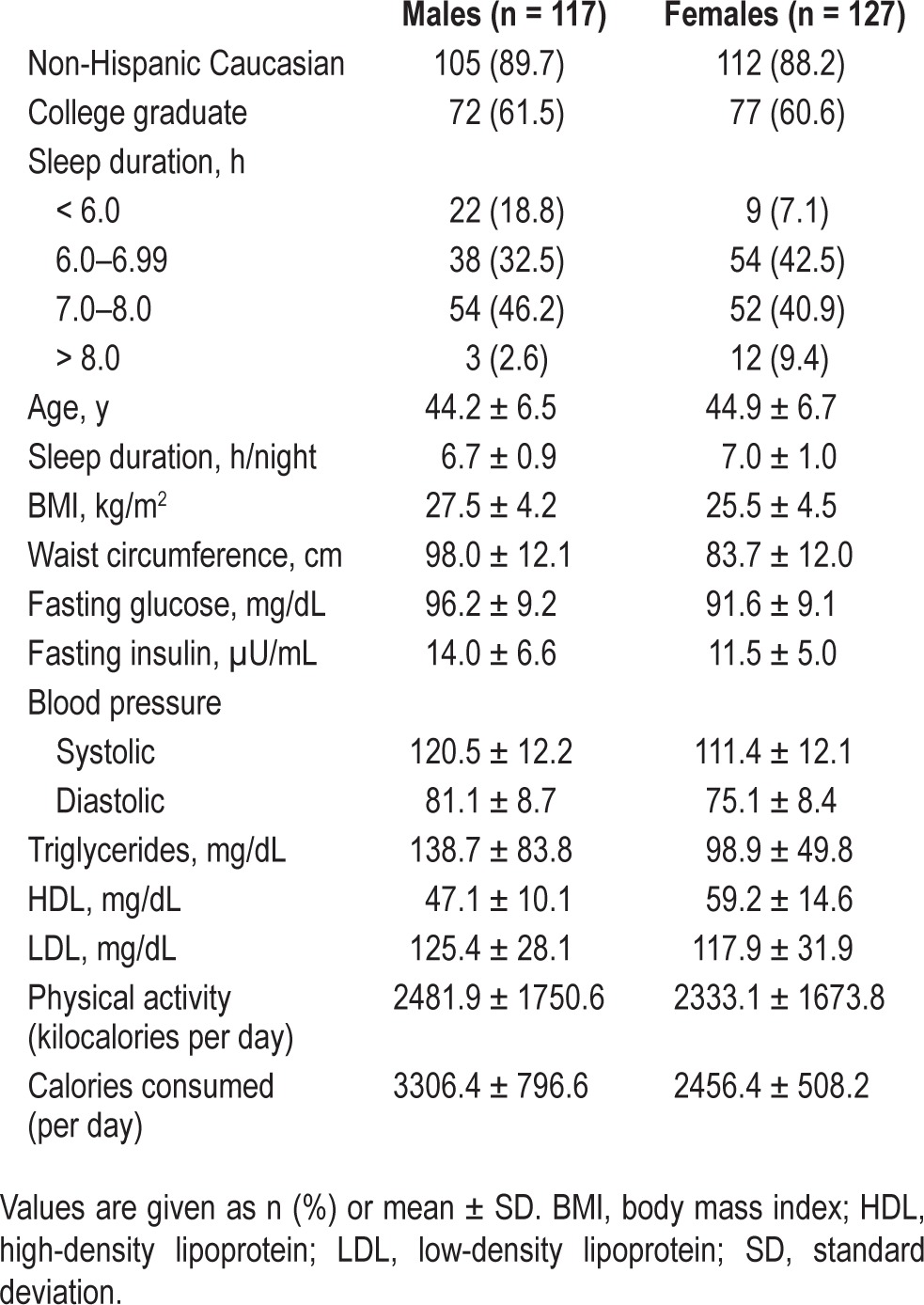
Sleep duration was normally distributed, with 12.7% of the sample reporting a weekly average of less than 6 h/night (Table 2). Average sleep duration differed by race, such that African American participants reported sleeping less than white participants (6.41 ± 0.87 h, 6.89 ± 0.96 h, respectively). In addition, no African American participants reported sleeping greater than 8 h/night. Women reported a longer average sleep duration (6.98 ± 0.96 h) than men (6.67 ± 0.93 h, P = 0.013), and also had lower fasting glucose and insulin levels (P's ≤ 0.001). These values are comparable to the larger AHAB sample described in our previous report on the association between sleep duration and the metabolic syndrome.5
Insulin Sensitivity
Table 3 reports the results from each hierarchical linear regression model conducted. As shown in Model 1, after controlling for participant demographics in the total sample, shorter sleep duration (in h) was associated with lower Si (β = 0.13, P = 0.043). There was a moderate correlation between Si and AIRg (r = −0.50). Further tests were conducted to examine whether the relationship between sleep duration and Si was curvilinear, but the addition of cubic and quadratic sleep duration terms did not improve either of the analyses (P's > 0.05).
Table 3.
Hierarchical regression analyses examining the effect of sleep duration on insulin sensitivity and acute insulin response to glucose.
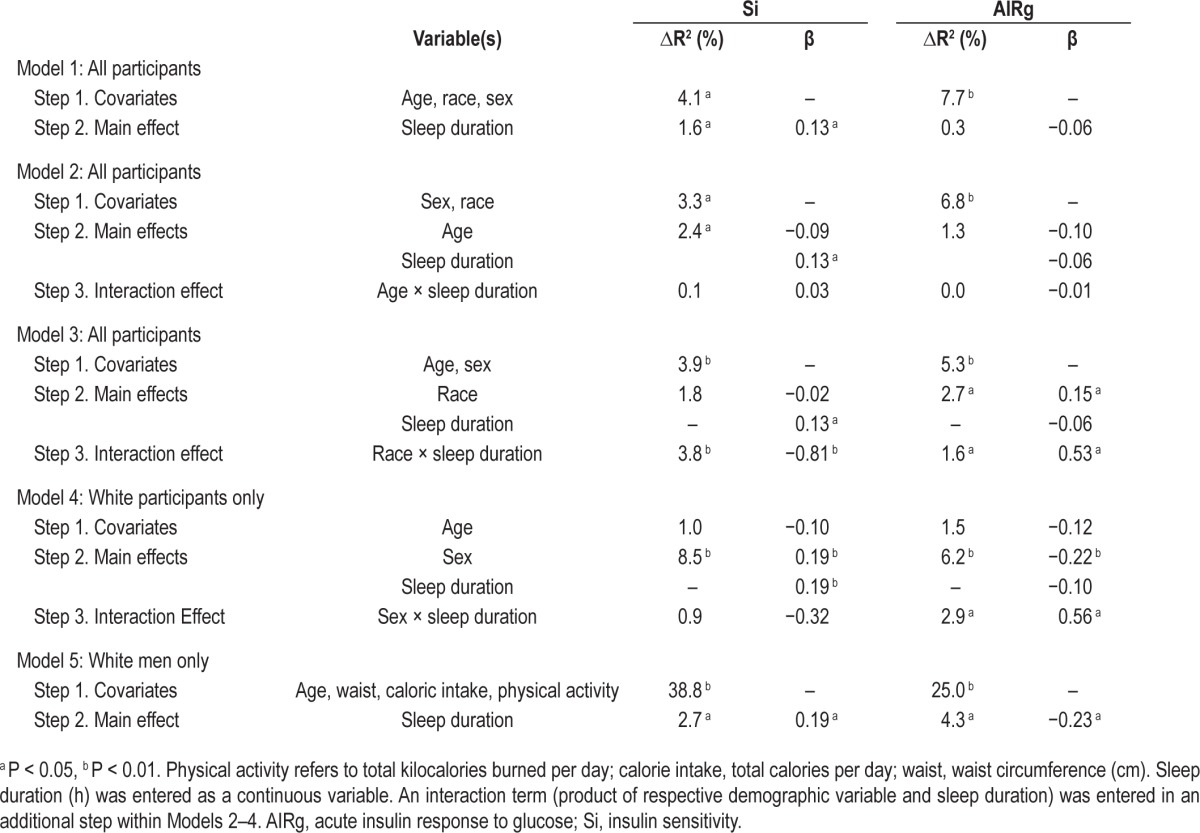
In testing next for potential interactions with demographic factors, age did not modify the effect of sleep duration on Si (Table 3, Model 2; P > 0.05). Participant race, however, interacted with sleep duration (Table 3, Model 3; β = −0.81, P = 0.002). Examining the simple slopes revealed that sleep duration covaried positively with Si among white participants (β = 0.04, P = 0.004) but inversely in African Americans (β = −0.11, P = 0.02). The small number of African Americans precluded further analyses within that subset of participants. Given the difference between races, the following sex and sleep duration interaction effect was investigated in white participants only.
In the total sample, women had greater Si than men (P = 0.017). Sex did not significantly moderate the relationship between sleep duration and Si in white participants (P > 0.05). However, sexstratified analyses revealed that shorter sleep duration associated with lower Si in white men (β = 0.29, P = 0.003; Figure 1) and not in white women (P = 0.22). For illustrative purposes, Figure 2 shows the proportion of white men with relatively impaired insulin sensitivity when divided into sleep duration categories. A logistic regression controlling for age revealed that each hour decrease in sleep duration was associated with a 50.4% higher odds of falling within the lower quartile of Si values (confidence interval: 0.30–0.84, P = 0.008). Sleep duration was not predictive of the dichotomous Si value in white women (P > 0.05).
Figure 1.
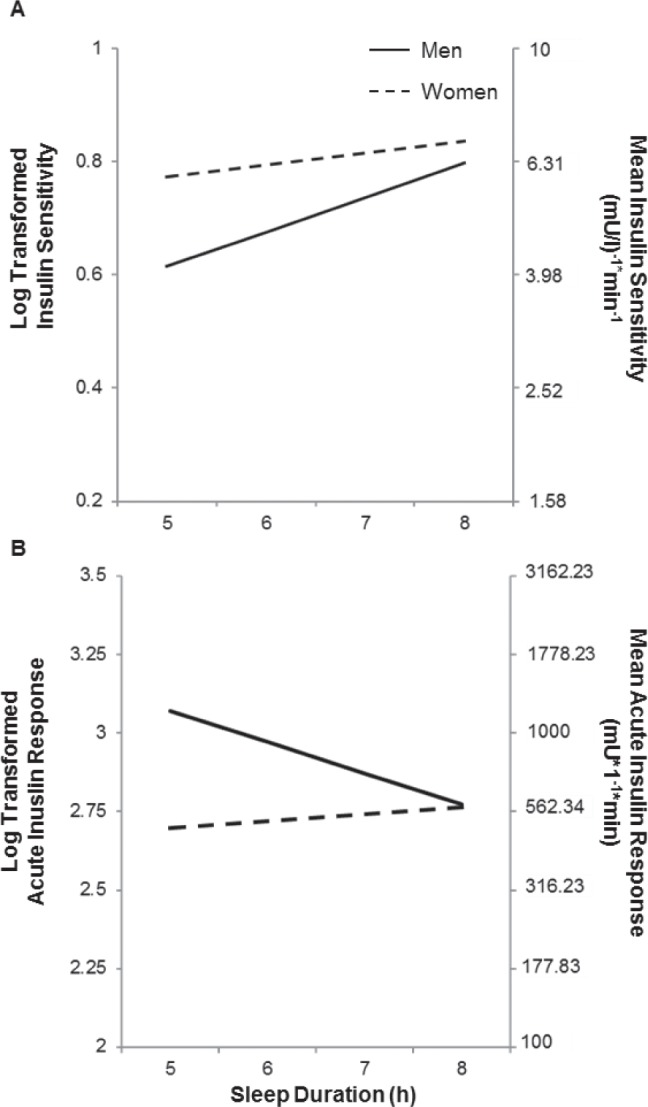
Association between sleep duration and indices of glucose metabolism obtained from IVGTT in White participants. IVGTT results were calculated with the Minmod Millenium software. Sleep duration was associated with (A) insulin sensitivity (Si), and (B) acute beta-cell insulin secretory response (AIRg) levels in White males but not in White females.
Figure 2.
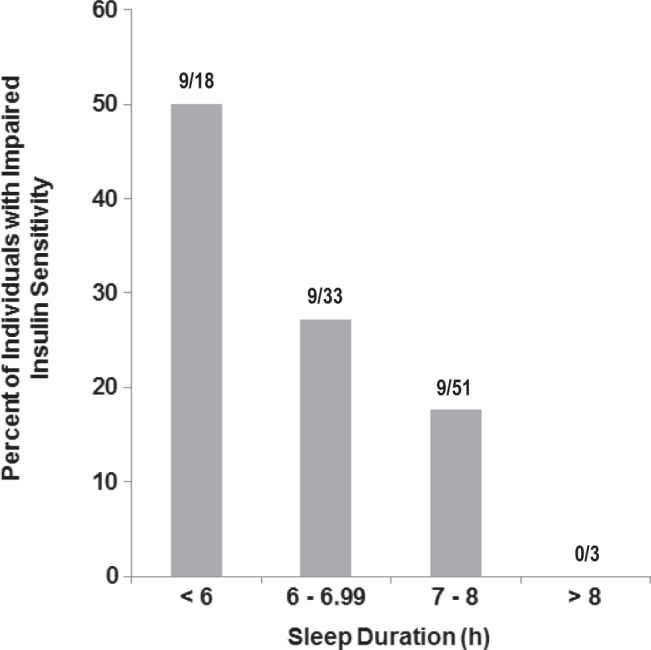
Proportion of white men in each sleep duration category with impaired insulin sensitivity (Si). Presence of impaired Si is defined as Si value < 25th percentile in sample distribution.
Last, a sex-specific analysis revealed that in white men, increased waist circumference significantly associated with decreased Si (β = −0.65, P < 0.001) but the health behaviors were unrelated (P's > 0.05). Sleep duration continued to covary positively with Si after controlling for waist circumference as well as health behaviors (Table 3, Model 5; β = 0.19, P = 0.033).
Acute Insulin Response to Glucose
In the total sample, sleep duration was not associated with AIRg (Table 3, Model 1, P = 0.356). The addition of cubic and quadratic sleep duration terms in the model were not significant and did not reveal a curvilinear relationship between sleep duration and AIRg (P's > 0.05).
As reported in Table 3, age did not modify the effect of sleep duration on AIRg (P > 0.05). In contrast, race interacted with sleep duration (Model 3; β = 0.53, P = 0.038), although simple slope analyses did not reveal significant effects of sleep duration on AIRg in either white or African American participants.
Parallel to Model 4 of the Si analysis, the interaction of sex and sleep duration was investigated in white participants only. In the total sample, women had lower AIRg relative to men (P = 0.009). Among white participants, sex moderated the effect of sleep duration on AIRg (Table 3, Model 4; β = 0.56, P = 0.010). As illustrated in Figure 1, shorter sleep duration was associated with higher AIRg in white men (β = −0.10, P = 0.004) but not in white women (P = 0.49). Specifically in white men, waist circumference was positively associated with AIRg (Model 5, β = 0.42, P = 0.001), whereas the health behaviors were unrelated (P's > 0.05). In this model, sleep duration continued to covary inversely with AIRg after controlling for waist circumference and health behaviors (β = −0.23, P = 0.015).
Sg and Di
Sg was correlated with Si (r = 0.38, P < 0.001) but not AIRg (P > 0.05). Di was correlated with each of the three IVGTT outcome variables (Si: r = 0.33, AIRg: r = 0.65, Sg: r = 0.30; P's < 0.001). A model controlling for age, sex, and race revealed that sleep duration was not related to either Sg (β = 0.08, P = 0.200) or Di (β = 0.07, P = 0.289).
CONCLUSIONS
The primary aim of this study was to examine whether self-reported sleep duration associates with indices of glucose metabolism based on the IVGTT–derived measures of insulin secretion and sensitivity in a nondiabetic community sample. The results reveal that habitual sleep restriction is linked to reduced insulin sensitivity in a linear relationship, specifically in white men. This association was absent in white women. The relationship between sleep duration and insulin sensitivity persists with adjustment for central adiposity, caloric intake, and physical activity. To our knowledge, this is the first study to extend findings of experimentally curtailed sleep on insulin sensitivity, assessed by IVGTT, to natural variation in sleep duration in nondiabetic adults.
The acute insulin response to glucose was inversely related to sleep duration in white men. Shorter sleep was associated with greater insulin secretion from pancreatic beta-cells in response to intravenous glucose administration during the IVGTT, which may indicate a compensatory response to the low insulin sensitivity in participants with habitually short sleep. This is also supported by the absence of an association between sleep duration and the disposition index. A parallel decrease in both insulin sensitivity and secretion results in a reduced disposition index, the latter of which is a predictor of type 2 diabetes development as well as the worsening of metabolic functioning prediabetes and post-diabetes diagnosis.45 Our finding that both the beta-cell response and disposition index remain unimpaired is congruent with observations that in nondiabetic individuals, insulin secretion rises to compensate for decreasing insulin sensitivity.29 A longitudinal study has shown that the inability of beta-cell insulin secretion to rise along with deteriorating insulin sensitivity distinguishes whether an individual maintains normal glucose tolerance or progresses toward type 2 diabetes.45 In addition, the current study did not reveal an effect of sleep duration on glucose effectiveness. This observation, however, is consistent with previous evidence that noninsulin-mediated glucose uptake remains intact among nondiabetic individuals.46 Prospective studies are needed to evaluate the extent to which habitual sleep restriction may contribute to the eventual impairment of the pancreatic beta-cell response, glucose effectiveness, an elevated disposition index, and incident type 2 diabetes.
We observed that the effect of sleep loss on glucose metabolism is specific to white men. Although some studies have reported that experimentally restricted and fragmented sleep decreased insulin sensitivity in mixed sex samples, these studies were too small for sex-stratified analyses (women n = 2–4).11,12 Our sex-dependent findings parallel some longitudinal studies showing self-reported short sleep to predict increased relative risk for type 2 diabetes in men.6,47 Ayas and colleagues7 found that although short sleep was likewise predictive of diabetes over 10 y in initially healthy women (N = 70,026), this effect was no longer significant after adjustment for BMI at baseline. Our sex-specific finding could be the result of lower power in the subset of women. Although women comprised 52% of our sample, they had relatively longer sleep, lower BMI, higher insulin sensitivity, and lower insulin secretion when compared with the men (P's < 0.05). It is possible that insufficient variability in these characteristics preclude the detection of the hypothesized sleep effect in women. Moreover, sleep disordered breathing is prevalent in the general population, with male sex and obesity identified as risk factors for the disorder.48,49 Mea sures of specific sleep disturbances were not available in the AHAB cohort, and so we were unable to adjust for the presence of sleep disorders (e.g. obstructive sleep apnea) in our analyses. There is evidence that obstructive sleep apnea among men is related to lower insulin sensitivity as well as a higher prevalence of type 2 diabetes.50 Hence, it is possible that our sex-specific findings may be caused in part by the presence of undetected obstructive sleep apnea among the men in our sample. Our sex-specific findings warrant other studies to further investigate whether there is indeed a moderation effect of sex after excluding or controlling for the presence of sleep disorders.
Sleep loss can contribute to insulin resistance either by interfering with nighttime glucose regulation directly or by dys-regulation of appetite with an increased risk for obesity. Past studies have shown that sleep restriction increases self-reported hunger and calorie consumption51–53 and could reduce daytime physical activity caused by fatigue, whereas a lack of exercise and high-fat diet can impair glucose metabolism.27,28 In addi tion, a previous study found that sleep restriction in the presence of high caloric intake and lack of exercise related to high insulin resistance.15 In the current sample, however, physical activity and caloric intake did not correlate with either sleep duration or the indices of glucose metabolism. It is important to note that laboratory-based studies examining the relationship between sleep restriction, glucose metabolism, caloric in-take, and physical activity employ controlled measured such as predetermined food intake and/or monitored, objectively quantified food intake, and enforced sedentary activity.15,52 In contrast, the current study measured physical activity and food intake through the Paffenbarger and Nutrition Data System interview. Although these measures are reliable and valid diary measures,35,40,41 the reliance on subjective recall serves as a limitation. These methodological differences may explain the inconsistent findings regarding the role of physical activity and caloric intake in glucose metabolism.
Given the confounding relationship between waist circumference and sex, the current study included a sex-stratified, exploratory set of analyses to examine whether sleep duration was related to glucose metabolism beyond the effect of adiposity. Previous reports on the associations between waist circumference and health outcomes similarly employed sexstratified analyses to examine the independent effect of waist circumference.54,55 In the current sample, waist circumference and BMI were predictive of insulin sensitivity and secretion in both sexes (P's < 0.001). One study reported reduced sleep duration has been linked to weight gain in women,56 but here shorter sleep duration was related to adiposity only in men. Despite the effect of waist circumference on glucose metabolism in white men, we found that sleep duration continued to associate with insulin sensitivity and secretion after controlling for adiposity measures. That there remained a significant residual effect of sleep duration suggests that additional mechanisms are operating.
Aside from alterations in health behaviors, curtailed sleep has been theorized to affect glucose metabolism via several physiologic pathways. Activation of the hypothalamic-pituitary-adrenal (HPA) axis and autonomic nervous system play important roles in regulating glucose levels during hypoglycemia. Given that sleep restriction has been shown to activate the HPA axis, increase cortisol output, and also raise overnight catecholamine levels,57 alterations in these systems may mediate the link between sleep and glucose tolerance. In addition, slow wave sleep (SWS; the deeper substage of nonrapid eye movement sleep) is temporally associated with decreased brain glucose utilization, decreased sympathetic nervous system activation and increased vagal tone. It has been proposed that reduced SWS may induce increased sympathetic activation and impairments in glucose tolerance but the evidence is mixed.13,58 Last, central and peripheral circadian clocks coordinate the temporal relationships between sleep-wake behaviors, feeding cycles, and metabolic rhythms (i.e., glucose homeostasis). Accumulating evidence suggests that clock disruptions impair glucose metabolism59–61 and may contribute in part to the effect of sleep curtailment.
In our analysis, the effect of sleep duration on insulin sensitivity was different in African Americans, compared to the white participants. The underrepresentation of African Americans in our sample (n = 27), however, prevented us from further exploring or interpreting these findings. Additional studies with more racially diverse samples are needed to examine whether or not habitual sleep curtailment associates with IVGTT-based measures of glucose metabolism across racial groups.
We previously reported a U-shape curvilinear relationship between sleep duration, elevated glucose levels, and risk for the metabolic syndrome in the AHAB sample.5 However, the current subset of AHAB subjects demonstrated a linear relationship between sleep and glucose metabolism. It is possible that with few individuals sleeping greater than 8 h/night (n = 13) the current analyses were unable to detect a curvilinear relationship or that long sleep may be linked to cardiovascular and metabolic diseases via different mechanisms than short sleep. For example, long sleep duration may indicate undiagnosed sleep disordered breathing that in turn drives the relationship between long sleep and poorer health outcome.62,63
It is important to note our study quantified sleep duration based on self-report. Relative to sleep times based on both polysomnography and actigraphy measures, self-reported sleep duration tends to be overestimated and have poor internal validity.46,47 However, an accumulation of data have shown that self-reported sleep duration links to various disease outcomes,5–8 which indicates there is an important relationship between self-reported sleep duration and health risk despite the discrepancy between subjective and objective quantification of the construct. It is possible that self-reported short sleep may indicate other risk factors including subjective sleep debt or poor sleep quality, and that such constructs underlie the link between self-reported sleep duration and disease risk. Our findings warrant further studies to use measures such as actigraphy to examine whether behaviorally defined sleep duration outside of the laboratory setting associates with IVGTT indices or other robust measures of glucose metabolism. The cross-sectional design of our study precludes determination of the directionality between sleep duration and glucose metabolism. Longitudinal studies are warranted to examine whether habitual sleep loss is driving disease risk or vice versa.
Finally, the IVGTT used in the current study provides a more robust measure of insulin and glucose dynamics relative to the HOMA-IR method used in previous large, community-sampled studies. The IVGTT is a cost-effective method that has been validated against glucose clamp techniques,23,30,31 but there are several limitations to note. Although the euglycemic clamp is limited in its complex application, it measures the glucose infusion rate under a steady state of induced euglycemia and provides a gold-standard measure of tissue sensitivity to endogenous insulin.64 Unlike HOMA-IR, the IVGTT provides an additional measure of the beta-cell response to glucose but this estimate is limited to the acute, first phase of insulin release.25 Following the acute insulin release, there is a second-phase, gradual release of insulin in the presence of elevated plasma glucose concentration. The hyperglycemic clamp induces a steady state of hyperglycemia which allows quantification of the biphasic beta-cell insulin response.64 In addition, we were unable to estimate glucose tolerance with the abbreviated IVGTT implemented in the current study. The current findings can therefore be confirmed and supplemented with more comprehensive measures of insulin sensitivity and secretion via glucose clamp techniques.
The principal findings along with the limitations of the current study suggest several directions for future research regarding sleep and glucose metabolism. Additional research is needed to evaluate (1) the generalizability of our results to older adults, African-Americans, and populations at risk for the development of diabetes, (2) whether sleep duration quantified by more objective measures of habitual sleep behaviors similarly associates with glucose metabolism, (3) whether sleep duration by influencing insulin sensitivity and beta cell function portends incident diabetes in prospective studies, and (4) whether sleep hygiene interventions favorably affect not just sleep quality and duration but important indices of glucose metabolism. Finally, it is of interest to evaluate the etiology of short sleep (e.g., insomnia, and psychiatric comorbidities) and other dimensions of sleep (e.g., sleep architecture, sleep debt, sleep continuity, and sleep quality) that may be related to alterations in insulin sensitivity, secretion, or both.
DISCLOSURE STATEMENT
This study was supported by NIH Grant P01 HL040962. This study was also supported in part by NIH Grants R01 DK095780, U01 DK057002, 1R01DK096028-01A1, and Sanofi-Aventis. Dr. Korytkowski has received research support from Sanofi-Aventis, administrated through the Office of Research at the University of Pittsburgh. She received an honorarium from the American Association of Clinical Endocrinologists for presentation at a symposium that was funded by SanofiAventis. She also provides consultation services for Regeneron Pharmaceuticals. The other authors have indicated no financial conflicts of interest. The work presented in this manuscript was conducted at the University of Pittsburgh.
ACKNOWLEDGMENTS
The authors thank Dr. Lauren Terhorst of the University of Pittsburgh School of Nursing for her statistical guidance.
REFERENCES
- 1.Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99:2008–19. doi: 10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- 2.Kronholm E, Partonen T, Laatikainen T, et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005: a comparative review and re-analysis of Finnish population samples. J Sleep Res. 2008;17:54–62. doi: 10.1111/j.1365-2869.2008.00627.x. [DOI] [PubMed] [Google Scholar]
- 3.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10:S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–4. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall MH, Muldoon MF, Jennings JR, Buysse DJ, Flory JD, Manuck SB. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep. 2008;31:635–43. doi: 10.1093/sleep/31.5.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29:657–61. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 7.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 8.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32:1484–92. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 9.Chaput JP, Despres JP, Bouchard C, Tremblay A. Association of sleep duration with type 2 diabetes and impaired glucose tolerance. Diabetologia. 2007;50:2298–304. doi: 10.1007/s00125-007-0786-x. [DOI] [PubMed] [Google Scholar]
- 10.Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin. 2007;2:187–97. doi: 10.1016/j.jsmc.2007.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donga E, van Dijk M, van Dijk JG, et al. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010;95:2963–8. doi: 10.1210/jc.2009-2430. [DOI] [PubMed] [Google Scholar]
- 13.Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59:2126–33. doi: 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 15.Nedeltcheva AV, Kessler L, Imperial J, Penev PD. Exposure to recurrent sleep restriction in the setting of high caloric intake and physical inactivity results in increased insulin resistance and reduced glucose tolerance. J Clin Endocrinol Metab. 2009;94:3242–50. doi: 10.1210/jc.2009-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flint J, Kothare SV, Zihlif M, et al. Association between inadequate sleep and insulin resistance in obese children. J Pediatr. 2007;150:364–9. doi: 10.1016/j.jpeds.2006.08.063. [DOI] [PubMed] [Google Scholar]
- 17.Donga E, van Dijk M, van Dijk JG, et al. Partial sleep restriction decreases insulin sensitivity in type 1 diabetes. Diabetes Care. 2010;33:1573–7. doi: 10.2337/dc09-2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin resistance in healthy black and white adolescents. Sleep. 2012;35:1353–8. doi: 10.5665/sleep.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knutson KL, Van Cauter E, Zee P, Liu K, Lauderdale DS. Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: the Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study. Diabetes Care. 2011;34:1171–6. doi: 10.2337/dc10-1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 22.Pacini G, Bergman RN. MINMOD: a computer program to calculate insulin sensitivity and pancreatic responsivity from the frequently sampled intravenous glucose tolerance test. Comput Methods Programs Biomed. 1986;23:113–22. doi: 10.1016/0169-2607(86)90106-9. [DOI] [PubMed] [Google Scholar]
- 23.Korytkowski MT, Berga SL, Horwitz MJ. Comparison of the minimal model and the hyperglycemic clamp for measuring insulin sensitivity and acute insulin response to glucose. Metabolism. 1995;44:1121–5. doi: 10.1016/0026-0495(95)90003-9. [DOI] [PubMed] [Google Scholar]
- 24.Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294:E15–26. doi: 10.1152/ajpendo.00645.2007. [DOI] [PubMed] [Google Scholar]
- 25.Ferrannini E, Mari A. Beta cell function and its relation to insulin action in humans: a critical appraisal. Diabetologia. 2004;47:943–56. doi: 10.1007/s00125-004-1381-z. [DOI] [PubMed] [Google Scholar]
- 26.Steil GM, Volund A, Kahn SE, Bergman RN. Reduced sample number for calculation of insulin sensitivity and glucose effectiveness from the minimal model. Suitability for use in population studies. Diabetes. 1993;42:250–6. doi: 10.2337/diab.42.2.250. [DOI] [PubMed] [Google Scholar]
- 27.Bisschop PH, de Metz J, Ackermans MT, et al. Dietary fat content alters insulin-mediated glucose metabolism in healthy men. Am J Clin Nutr. 2001;73:554–9. doi: 10.1093/ajcn/73.3.554. [DOI] [PubMed] [Google Scholar]
- 28.Heath GW, Gavin JR, 3rd, Hinderliter JM, Hagberg JM, Bloomfield SA, Holloszy JO. Effects of exercise and lack of exercise on glucose tolerance and insulin sensitivity. J Appl Physiol. 1983;55:512–7. doi: 10.1152/jappl.1983.55.2.512. [DOI] [PubMed] [Google Scholar]
- 29.Wagenknecht LE, Mayer EJ, Rewers M, et al. The insulin resistance atherosclerosis study (IRAS) objectives, design, and recruitment results. Ann Epidemiol. 1995;5:464–72. doi: 10.1016/1047-2797(95)00062-3. [DOI] [PubMed] [Google Scholar]
- 30.Saad MF, Anderson RL, Laws A, et al. A comparison between the minimal model and the glucose clamp in the assessment of insulin sensitivity across the spectrum of glucose tolerance. Insulin Resistance Atherosclerosis Study. Diabetes. 1994;43:1114–21. doi: 10.2337/diab.43.9.1114. [DOI] [PubMed] [Google Scholar]
- 31.Bergman RN, Prager R, Volund A, Olefsky JM. Equivalence of the insulin sensitivity index in man derived by the minimal model method and the euglycemic glucose clamp. J Clin Invest. 1987;79:790–800. doi: 10.1172/JCI112886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 33.Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch Intern Med. 2006;166:1768–74. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- 34.Paffenbarger RS, Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–75. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 35.Albanes D, Conway JM, Taylor PR, Moe PW, Judd J. Validation and comparison of eight physical activity questionnaires. Epidemiology. 1990;1:65–71. doi: 10.1097/00001648-199001000-00014. [DOI] [PubMed] [Google Scholar]
- 36.Paffenbarger RS, Jr, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328:538–45. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- 37.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. 1988;88:1268–71. [PubMed] [Google Scholar]
- 38.Lyons GK, Woodruff SI, Candelaria JI, Rupp JW, Elder JP. Development of a protocol to assess dietary intake among Hispanics who have low literacy skills in English. J Am Diet Assoc. 1996;96:1276–9. doi: 10.1016/S0002-8223(96)00333-1. [DOI] [PubMed] [Google Scholar]
- 39.Smith CJ, Nelson RG, Hardy SA, Manahan EM, Bennett PH, Knowler WC. Survey of the diet of Pima Indians using quantitative food frequency assessment and 24-hour recall. Diabetic Renal Disease Study. J Am Diet Assoc. 1996;96:778–84. doi: 10.1016/s0002-8223(96)00216-7. [DOI] [PubMed] [Google Scholar]
- 40.Feskanich D, Buzzard IM, Welch BT, et al. Comparison of a computerized and a manual method of food coding for nutrient intake studies. J Am Diet Assoc. 1988;88:1263–7. [PubMed] [Google Scholar]
- 41.Mullenbach V, Kushi LH, Jacobson C, et al. Comparison of 3-day food record and 24-hour recall by telephone for dietary evaluation in adolescents. J Am Diet Assoc. 1992;92:743–5. [PubMed] [Google Scholar]
- 42.Bondar RJ, Mead DC. Evaluation of glucose-6-phosphate dehydrogenase from Leuconostoc mesenteroides in the hexokinase method for determining glucose in serum. Clin Chem. 1974;20:586–90. [PubMed] [Google Scholar]
- 43.Festa A, D'Agostino R, Jr, Howard G, Mykkanen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102:42–7. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 44.Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR) Diabet Med. 1999;16:442–3. doi: 10.1046/j.1464-5491.1999.00059.x. [DOI] [PubMed] [Google Scholar]
- 45.Weyer C, Bogardus C, Mott DM, Pratley RE. The natural history of insulin secretory dysfunction and insulin resistance in the pathogenesis of type 2 diabetes mellitus. J Clin Invest. 1999;104:787–94. doi: 10.1172/JCI7231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bergman RN. Lilly lecture 1989. Toward physiological understanding of glucose tolerance. Minimal-model approach. Diabetes. 1989;38:1512–27. doi: 10.2337/diab.38.12.1512. [DOI] [PubMed] [Google Scholar]
- 47.Mallon L, Broman JE, Hetta J. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28:2762–7. doi: 10.2337/diacare.28.11.2762. [DOI] [PubMed] [Google Scholar]
- 48.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 49.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meslier N, Gagnadoux F, Giraud P, et al. Impaired glucose-insulin metabolism in males with obstructive sleep apnoea syndrome. Eur Respirat J. 2003;22:156–60. doi: 10.1183/09031936.03.00089902. [DOI] [PubMed] [Google Scholar]
- 51.Morselli L, Leproult R, Balbo M, Spiegel K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best practice & research. Clin Endocrinol Metab. 2010;24:687–702. doi: 10.1016/j.beem.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89:126–33. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 54.Bigaard J, Tjonneland A, Thomsen BL, Overvad K, Heitmann BL, Sorensen TI. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Obes Res. 2003;11:895–903. doi: 10.1038/oby.2003.123. [DOI] [PubMed] [Google Scholar]
- 55.Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J. 2004;25:2212–9. doi: 10.1016/j.ehj.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 56.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:947–54. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Balbo M, Leproult R, Van Cauter E. Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. Int J Endocrinol. 2010;2010:759234. doi: 10.1155/2010/759234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105:1044–9. doi: 10.1073/pnas.0706446105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106:4453–8. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Buxton OM, Cain SW, O'Connor SP, et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med. 2012;4:129ra43. doi: 10.1126/scitranslmed.3003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sookoian S, Gemma C, Fernandez Gianotti T, et al. Effects of rotating shift work on biomarkers of metabolic syndrome and inflammation. J Intern Med. 2007;261:285–92. doi: 10.1111/j.1365-2796.2007.01766.x. [DOI] [PubMed] [Google Scholar]
- 62.Alvarez GG, Ayas NT. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19:56–9. doi: 10.1111/j.0889-7204.2004.02422.x. [DOI] [PubMed] [Google Scholar]
- 63.Kripke DF, Ancoli-Israel S, Mason WJ, Kaplan O. Sleep apnea: association with deviant sleep durations and increased mortality. In: Guilleminault C, Partinen M, editors. Obstructive Sleep Apnea Syndrome: Clinical Research and Treatment. New York: Raven Press Ltd; 1990. pp. 9–14. [Google Scholar]
- 64.DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237:E214–23. doi: 10.1152/ajpendo.1979.237.3.E214. [DOI] [PubMed] [Google Scholar]


