Abstract
Study Objectives:
To compare treatment effects when patients with insomnia and depression receive treatment for either insomnia or depression.
Design:
A 9-w randomized controlled trial with 6- and 12-mo follow-up.
Setting:
Internet Psychiatry Clinic, Stockholm, Sweden.
Participants:
Forty-three adults in whom comorbid insomnia and depression were diagnosed, recruited via media and assessed by psychiatrists.
Interventions:
Guided Internet-delivered cognitive behavior therapy (ICBT) for either insomnia or depression.
Measurements and Results:
Primary outcome measures were symptom self-rating scales (Insomnia Severity Index [ISI] and the Montgomery Åsberg Depression Rating Scale [MADRS-S]), assessed before and after treatment with follow-up after 6 and 12 mo. The participants' use of sleep medication and need for further treatment after completion of ICBT was also investigated. The insomnia treatment was more effective than the depression treatment in reducing insomnia severity during treatment (P = 0.05), and equally effective in reducing depression severity. Group differences in insomnia severity were maintained during the 12-mo follow-up period. Post treatment, participants receiving treatment for insomnia had significantly less self-rated need for further insomnia treatment (P < 0.001) and used less sleep medication (P < 0.05) than participants receiving treatment for depression. The need for depression treatment was similar in both groups.
Conclusions:
In this study, Internet-delivered treatment with cognitive behavior therapy (ICBT) for insomnia was more effective than ICBT for depression for patients with both diagnoses. This indicates, in line with previous research, that insomnia when comorbid with depression is not merely a symptom of depression, but needs specific treatment.
Trial Registration:
The trial was registered at Clinicaltrials.gov, registration ID: NCT01256099.
Citation:
Blom K, Jernelöv S, Kraepelien M, Bergdahl MO, Jungmarker K, Ankartjärn L, Lindefors N, Kaldo V. Internet treatment addressing either insomnia or depression, for patients with both diagnoses: a randomized trial. SLEEP 2015;38(2):267–277.
Keywords: CBT, comorbidity, depression, insomnia, Internet, psychological treatment, psychotherapy
INTRODUCTION
Insomnia and depression are severe public health problems, affecting large proportions of the population. Comorbidity between insomnia and depression is a common phenomenon,1–5 with serious adverse implications for the individual and for society.6–10 There are pharmacological and psychological evidence-based treatments for both depression and insomnia. For insomnia, pharmacological treatment is only recommended for short-term use. Psychological treatment in the form of cognitive behavioral therapy (CBT) has strong evidence both for insomnia11,12 and depression13 with sustained improvements. Self-help-CBT with therapist support, including therapist-guided Internet-delivered CBT (ICBT), has been found effective for a wide range of psychiatric conditions, including insomnia and depression.14–24
When patients present with both depression and insomnia, treatment is often given for the depression only, whereas sleeping problems may be inadequately treated—or are just expected to subside along with other depression symptoms. The British National Institute for Health and Clinical Excellence (NICE) guidelines for treatment of depression mention sleeping problems as a symptom and recommend sleep hygiene as an intervention, but do not discuss insomnia as a differential diagnosis requiring evidence-based treatment. In summary, sleeping problems seem to be viewed as one of many symptoms of depression. But is this really the case?
Research looking into this issue indicates that the answer is no; many studies find that insomnia generally precedes or is concomitant rather than subsequent to depression.1,4,25–27 More importantly, treatment for depression does not seem to provide sufficient remedy for patients' coexisting insomnia.28 Furthermore, there is some evidence that persistence of insomnia is related to incomplete remission of depression29 and that residual insomnia predicts future depressive episodes.30 A pilot study by Manber and colleagues31 which included patients with comorbid depression and insomnia, compared a combined treatment (anti-depressants plus CBT for insomnia) to antidepressants only. The combined treatment had better results both for depression (remission rate 61.5% versus 33.3%) and insomnia (remission rate 50% versus 7%). Another study, comparing treatment with only antidepressants to treatment with both antidepressants and sleep medication, showed similar results.32 To our knowledge, there is no previous report of a randomized controlled trial where patients with this comorbidity received insomnia treatment only.
We aim to further challenge the traditional view of insomnia being secondary to depression. A way to do this is to compare how patients with both conditions respond to either insomnia treatment only or depression treatment only. Previous studies show that many different types of treatment have positive effects on depression, as long as they are credible and delivered with good quality33,34; i.e., the mechanism of action does not seem very specific. Along with the fact that improved sleep reduces depression severity,35–37 this suggests that insomnia treatment might be as effective as depression treatment for reducing depressive symptoms in patients who also suffer from insomnia. CBT for insomnia, however, is shown to have rather specific mechanisms of action,31,38 indicating that insomnia is, most likely, not affected by treatment for depression.
We therefore hypothesized that overall, the insomnia treatment would be more beneficial than the depression treatment for these comorbid conditions. More specifically, we expected the treatment effects on depression severity to be similar for both treatments, whereas the effects on the insomnia severity were expected to be larger for the patients receiving insomnia treatment. We also expected participants receiving depression treatment to express more need for further treatment after completion of the trial, as a result of the depression treatment being overall less effective than the insomnia treatment. The aim of this study was to test these hypotheses in a randomized controlled trial.
METHODS
Participants and Recruitment
This study was open to adults in Stockholm County, Sweden, presenting with both insomnia and major depression. Participants were recruited via ads in daily newspapers, the Internet Psychiatry Clinic's website, and through information to primary care staff.
Inclusion criteria were:
a) 18 y or older
b) Insomnia diagnosis according to the research criteria from the American Academy of Sleep Medicine,39 with more than 10 points on Insomnia Severity Index (ISI).40 Because none of the participants had less than 3 mo with insomnia, these criteria correspond to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)-criteria.41
c) Major depression diagnosis (DSM-IV-TR42)
-
d) Ability to read and write in Swedish.
Exclusion criteria were:
e) Other comorbid sleep disorders urgently requiring other treatment (sleep apnea or narcolepsy)
f) Ongoing alcohol or drug abuse
g) Change in antidepressant medication within the past 2 mo
h) Comorbid disorders directly contraindicative of essential interventions in insomnia treatment (e.g., bipolar disorder)
i) Night-shift work
Other comorbidities were allowed. Sleep medicine use was unrestricted. Inclusion was made in three steps: Web-based screening including consent, telephone interviews, and live assessment at the clinic. Diagnosis of insomnia and depression were made based on Internet screening and telephone interviews, whereas the live assessment focused on confirming the depression diagnosis and doing an overall psychiatric and medical assessment.
The recruitment and screening was a joint procedure for two studies, one of which targeted applicants with insomnia but without depression. Hence, 149 of the screened applicants were excluded from the study presented here and included in the insomnia-only study. The Web-based screening instruments consisted of ISI, the self-report version of the Montgomery Åsberg Depression Rating Scale (MADRS-S),43,44 Alcohol Use Disorders Identification Test (AUDIT),45 and the Drug Use Disorders Identification Test (DUDIT).46 AUDIT and DUDIT were used as input to the assessment of alcohol and drug abuse. The participants also provided contact information and background data (e.g. age, occupation, education).
The telephone interviews lasted 30–45 min and assessed insomnia and depression diagnosis according to the aforementioned criteria. The interview consisted of questions on: sociodemographic data; sleeping problems; the depression section from Structured Clinical Interview for DSM-IV, SCID47; insomnia and depression history; other illnesses; other factors that were perceived by the participant to affect sleep; and the participant's motivation and ability to take part in the study. Insomnia diagnosis was made according to the research criteria, based on information from the ISI questions (to assess sleep patterns and satisfaction with sleep), questions about daytime functioning (Epworth Sleepiness Scale [ESS]48) and a question about adequate opportunity and circumstance for sleep. Depression diagnosis was assessed using the SCID interview.
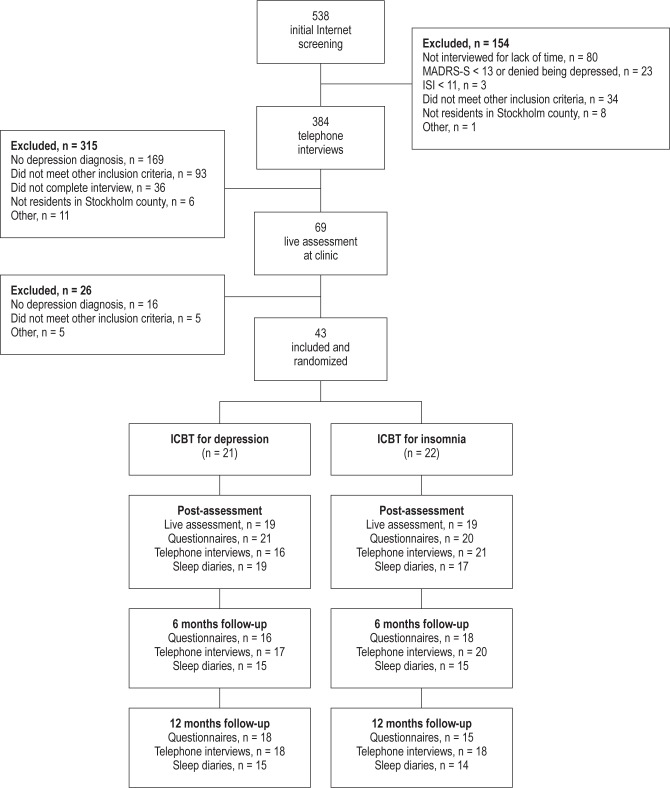
The Internet screening procedure was completed by 538 individuals. Three hundred eighty-four individuals (of whom 149 were included in the parallel study of insomnia only) were interviewed by phone and 69 of these, who met criteria, were then assessed at the clinic by resident physicians, supervised by board certified psychiatrists. The assessment included taking and evaluating the medical history, doing the Mini-International Neuropsychiatric Interview,49 and a cross-checking against inclusion criteria. Of the 69 individuals assessed by a physician, 43 were included and randomized into two treatment groups, ICBT for insomnia (ICBT-i) or ICBT for depression (ICBT-d) (Figure 1). The inclusion period was 8 mo and participants were included in four cohorts.
Figure 1.
Participant flow and reasons for exclusion. ICBT, therapist guided Internet-delivered cognitive behavioral therapy; ISI, Insomnia Severity Index; MADRS-S, Montgomery Åsberg Depression Rating Scale – Self rating; Post, after treatment.
The study protocol was approved by the regional ethics review board in Stockholm, Sweden.
Outcome Measures
Primary Measures
Insomnia and Depression Severity. Because neither depression nor insomnia was regarded as secondary to the other, two primary outcome measures were used: insomnia severity (ISI) and depression severity (MADRS-S). The psychometric properties of ISI are adequate and it is sensitive to change,50 also when Web-based.51 MADRS-S is a much-used, validated instrument for measuring and detecting changes in the severity of depression. The reason for using ISI and not sleep diary data as the primary insomnia measure in this study was that there is no equivalent to a sleep diary for measuring depression. To avoid a measurement confound, we therefore used retrospective self-report questionnaires (ISI and MADRS-S) covering the same time period for both primary outcomes.
We know from previous ICBT studies that it can be difficult to obtain self-rated data from all participants posttreatment.52 In accordance with the suggestion from Hedman and colleagues,52 we therefore acquired self-rated data over the phone at all assessment points to use as a basis for imputing expected missing Internet-rated postdata and follow-up data for ISI and MADR-S. In order to shorten the interview, MADRS-S was replaced by the questions on depression from the Hospital Anxiety and Depression Scale (HADS)53 (items 2, 4, 8 and 10) in the phone interview. ISI was shortened for the same reason, and included only the five diagnosis-related questions (1a-c, 2 and 3). The ISI and HADS questions were asked exactly as in the original versions and the alternative answers were read to the participant, who then chose one answer. See the Statistical Analyses section for more on this imputation method.
Secondary Measures
Sleep Diary. A sleep diary was used for one week at all assessment points. The main reason for choosing one week instead of the recommended two weeks was to reduce the risk that keeping a sleep diary would increase the patients' attention on sleep rather than depression and hence act as a general intervention or placebo, inflating the effects of both interventions on insomnia symptoms. Another reason was to increase compliance to the assessment procedure by reducing patients' burden. Each participant registered bedtime, time of falling asleep, night- time awakenings, time of waking up, and time of getting out of bed. Also, subjective sleep quality was rated daily on a five-point scale from very poor to very good. From these data sleep efficiency (SE), sleep onset latency (SOL), total sleep time (TST), and sleep quality (SQ) were calculated.
Need for Further Treatment. Considering that all participants had two diagnoses but were only treated for one of them, we wanted to find out whether the participants' subjective need for more treatment differed between the groups. A secondary outcome measure was therefore the participants' posttreatment wish for more treatment, and their intention to seek such treatment. All participants were asked four questions: (1) Do you want more treatment for insomnia? (2) Do you want more treatment for depression? (3) Do you intend to seek more insomnia treatment? and (4) Do you intend to seek more depression treatment? The answers were graded on a 0- to 3-point scale where 0 = No, 1 = I'm uncertain, but I don't think so, 2 = I'm uncertain, but I think so, and 3 = Yes.
Remission From Insomnia and Depression. Remission from insomnia and depression was assessed using the same criteria as in pretreatment assessment. Participants were classified as either having the diagnoses or not. This was only done post-treatment, when participants met a psychiatrist for a face-to-face assessment. For each follow-up measurement, we also used the remission criteria ISI < 8 for insomnia54 and MADRSS < 13 for depression.55
Adherence, Client Satisfaction, and Adverse Events. To assess adherence we asked the participants questions about what treatment components they had used. The questions were asked in Web-based questionnaires and in a posttreatment telephone interview. Participants' satisfaction with treatment was assessed using Client Satisfaction Questionnaire (CSQ-8).56 The technical platform allows for gathering of good quality statistics about module completion, therapists' time spent online per participant, number of times participants' logged in to the treatment, and number of messages sent and received. Adverse events were assessed in the telephone interviews posttreatment with the question “Did the treatment have any negative consequences?” if answered with yes, participants were asked to expand upon this.
Randomization and Assessment Points
In this randomized controlled trial, treatments were provided in two arms, ICBT-i or ICBT-d. The participants (n = 43) were randomized by an assistant not otherwise involved in the study, using www.random.org. Outcome measures were assessed before and after treatment, and at 6 and 12 mo after treatment. Adverse events were assessed in the telephone interviews posttreatment. Telephone assessors were final year students of clinical psychology at master level. For practical reasons, physicians and telephone assessors were not blind to treatment condition. The physicians doing assessments were regular staff at the clinic and had no other involvement in the study.
Interventions
Both treatments lasted nine weeks and were based on well-established CBT techniques for insomnia and depression, respectively. The treatments were delivered on the same technical platform. ICBT is built up by modules, accessed on a secure website that only the participant and their therapist can access. A module consists of text to read, questions to answer on theory, behavioral assignments (e.g. activity scheduling and sleep restriction), work sheets and for the ICBT-i group a sleep diary to be filled out throughout the treatment.
The participants should complete on average one module per week. Each module ends with the participant sending in a home-work report via a secure messaging system. The therapist receives the message, then reviews answers, work sheets and sleep diary (ICBT-i only), gives written feedback within 24 h on weekdays and finally gives the participant access to the next module. The participants also have the possibility to send messages with questions to their therapist, and these messages are answered within 24 h on weekdays. When answering, the therapist may not convey any information or give advice that is outside the scope of the manual.
The therapist also has access to data from weekly symptom severity assessments with ISI and MADRS-S, which allows monitoring of the participant's progress. The system flags the therapist if a participant scores 4 or more points on the suicide ideation item in MADRS-S (item 9), implying that the participant has thoughts about suicide. The therapist then follows the standard procedure at the Internet Psychiatry Clinic for assessment of suicidal ideation. If the participant is inactive for 7 days, the therapist sends a mobile phone text message encouraging the participant to get in touch and continue treatment.
The depression treatment (ICBT-d) has been tried and found efficacious in its original format in a previous study,21 which had a recommended treatment period of eight weeks, and an average treatment period of ten weeks. It is used since 2007 in regular psychiatric care at the Internet Psychiatry Clinic within the Stockholm County public health, Sweden, with a large with-in group effect size of Cohen's d (99% confidence interval) = 1.27 (1.14–1.39).57 The treatment period in regular care is twelve weeks to allow for vacations, illnesses, and such. In the current study, the module about sleeping problems (1 of 10 modules) included in the original depression treatment was removed, which was unavoidable in order not to interfere with the design of the study. Other than this it is the exact same treatment. The modules in the ICBT-d were thus: education on depression and CBT; behavioral activation 1 (increase positively reinforced activity); behavioral activation 2 (handle negatively reinforced and punished activity); registering negative thoughts; reappraisal of negative thoughts; handling anxiety and worry; continued work; summary of the treatment; planning ahead. The treatment and therapist support focuses on behavioral activation, which is part of homework assignments throughout the treatment, and on reappraisal of negative thoughts.
The insomnia treatment (ICBT-i) consisted of eight modules with the educational text delivered in a book that was sent to the participants. The efficacy of the manual has been tried in a randomized controlled trial with good results.16 The Internet part of the modules consisted of the sleep diary, reading instructions for the book, summary of the text, weekly assignments, work sheets and communication with the therapist. The ICBT-i modules were: introduction and facts about sleep; introduction to CBT for insomnia and sleep hygiene; education on sleep medicine and how to quit; sleep restriction and stimulus control; stress management; managing fatigue; handling negative thoughts about sleep; and planning ahead. The main focus during treatment, both in the modules and therapist support, was on sleep restriction and stimulus control.
Therapists Training and Adherence
Therapists (n = 6) were final-year students of clinical psychology at master level, with theoretical and practical training in CBT, including at least 18 mo of providing supervised face-to-face CBT to patients. They were trained in the treatment manuals and Internet treatment procedure, and then supervised weekly by a licensed clinical psychologist with CBT and insomnia/depression treatment expertise involved in the study (KB). Supervision was also available at request between weekly sessions. The supervising psychologist made sure therapists adhered to the protocol through the weekly supervision and by checking the written communication between a participant and the therapist, approximately five checks per therapist at different time points during the treatment.
Statistical Analyses
Both t test and χ2 associations were used to compare baseline data. All primary outcome analyses were done on an intent-to-treat basis, i.e., including treatment dropouts. Missing data for the self-rated primary outcome measures were replaced with self-rated data acquired by the telephone interview, when available. Because Internet data and telephone data are not directly interchangeable, a linear regression formula was used to impute missing Internet values (ISI and MADRS-S) from telephone values (partial ISI and HADS). The regression formulas, one for ISI and one for MADRS-S, were calculated by using post- and follow-up data from 168 participants in this and the parallel insomnia study where the telephone measure (independent variable) and the Internet measure (dependent variable) had been scored within one week. These measures were highly correlated (r = 0.83, P < 0.0001 for ISI and r = 0.75, P < 0.0001 for MADRSS/HADS). The interview version of ISI (items 1a-c, 2, and 3) had a Cronbach α of 0.83 and the four-item HADS-depression (items 2, 4, 8, and 10) had a Cronbach α of 0.74. Secondary outcome measures were calculated using available postdata.
Hierarchical linear mixed-effect modeling was used to perform significance tests for primary outcome data and sleep diary data. This statistical method is an intent-to-treat analysis and is superior to other methods in handling missing data.58 Full maximum likelihood estimation was used to fit the model. The models best fitted to data consisted of two timepieces with linear changes—pretreatment to posttreatment (timepiece1) and post-treatment to 6-mo (FU6) and 12-mo follow-up (FU12) (time-piece2). In order to test the overall group difference during the whole follow-up period, we tested an initial model, where the interaction between group and time during timepiece2 was not included. Subsequently, to find the final model, the interaction effect in timepiece2 was added to test if it increased the overall model fit. Baseline variables showing a simple correlation to either missingness, outcome, or both were included as possible covariates in order to test if they significantly improved model fit.
For effect sizes Cohen's d with pooled standard deviations were calculated using observed data. Because the MADRS-S includes an item about sleeping problems, a sensitivity analysis was carried out for MADRS-S with and without this item.
The secondary measure “need for further treatment”, only assessed posttreatment, was analyzed with independent t tests, as were adherence data. We used the Fischer exact test to test for differences between groups regarding remission from diagnoses and use of medication pretreatment and posttreatment.
A power analysis with 80% power indicated a sample size of 100 participants was needed, assuming the effect size d = 0.5 (α = 0.05). Statistical analyses were made using SPSS version 21 (IBM Inc., Armonk, NY, USA).
RESULTS
Baseline Characteristics
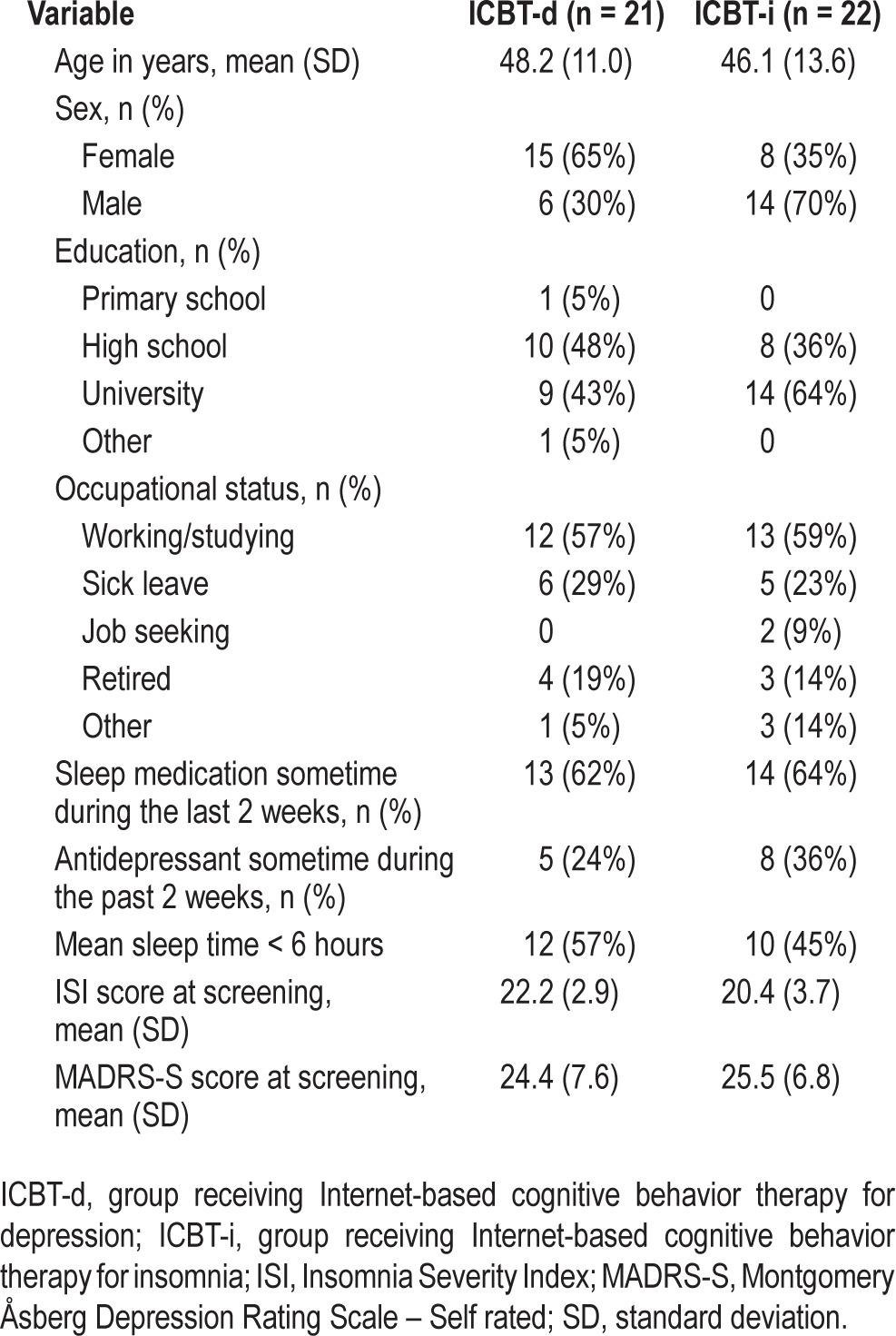
The two groups had no significant differences on any of the outcome measures before treatment. Baseline demographics (Table 1) showed no significant differences between groups except for sex; there were significantly more men in the ICBT-i group (χ2 = 5.31, P < 0.05).
Table 1.
Patient characteristics at baseline.
Missing Data and Model Fit
Attrition at posttreatment assessment for primary outcome measures was low: 2% and 4% for ISI and MADRS-S, respectively, after imputation of telephone data from one participant, i.e., after imputation, data were missing from one participant for ISI and two participants (one per group) for MADRS-S. At 6 and 12 mo, attrition was 7% and 9%, respectively (after imputation). Data from telephone interviews were imputed for five and seven participants, respectively, for the 6- and 12-mo assessments. After this imputation, data were still missing for three participants at FU6 (one in ICBT-i, two in ICBT-d) and four at FU12 (two per group). Sleep diary measures were harder to obtain despite great efforts via telephone, text messages, and written letters to encourage participants to provide data: at post-assessment 16% was missing, at 6 and 12 mo follow-up 33% and 35%, respectively. Given the quantity of missing sleep diary data at 6 and 12 mo follow-up, and the relatively small sample size, sleep diary data was only used for prestatistics to poststatistics. Data regarding need for further treatment were obtained from Internet questionnaires. Here attrition was low, 7%. Five participants, 11%, did not attend the posttreatment face-to-face assessment (see flow chart, Figure 1).
For each outcome measure the best modification of the basic mixed model with two timepieces was evaluated. Somewhat unexpectedly, we found that the changes during timepiece2 (i.e. from posttreatment to FU12) were very similar for both groups, for both ISI and MADRS-S. As a consequence, adding the interaction parameter for timepiece2 did not significantly add to the model fit and was therefore not included in the final model. In the final model for ISI the intercept was set to random and the fixed effects included time for timepiece1, time for timepiece2, group, and group × time for timepiece1, and the following baseline covariates were included: ISI, sleep quality, and educational level. The same was found for MADRS-S, except that the baseline covariates were MADRS-S and occupational status. For the sleep diary analysis only timepiece1 was used (predatapostdata) because of the high levels of missing data at FU6 and FU12, but the model was otherwise very similar to the aforementioned model.
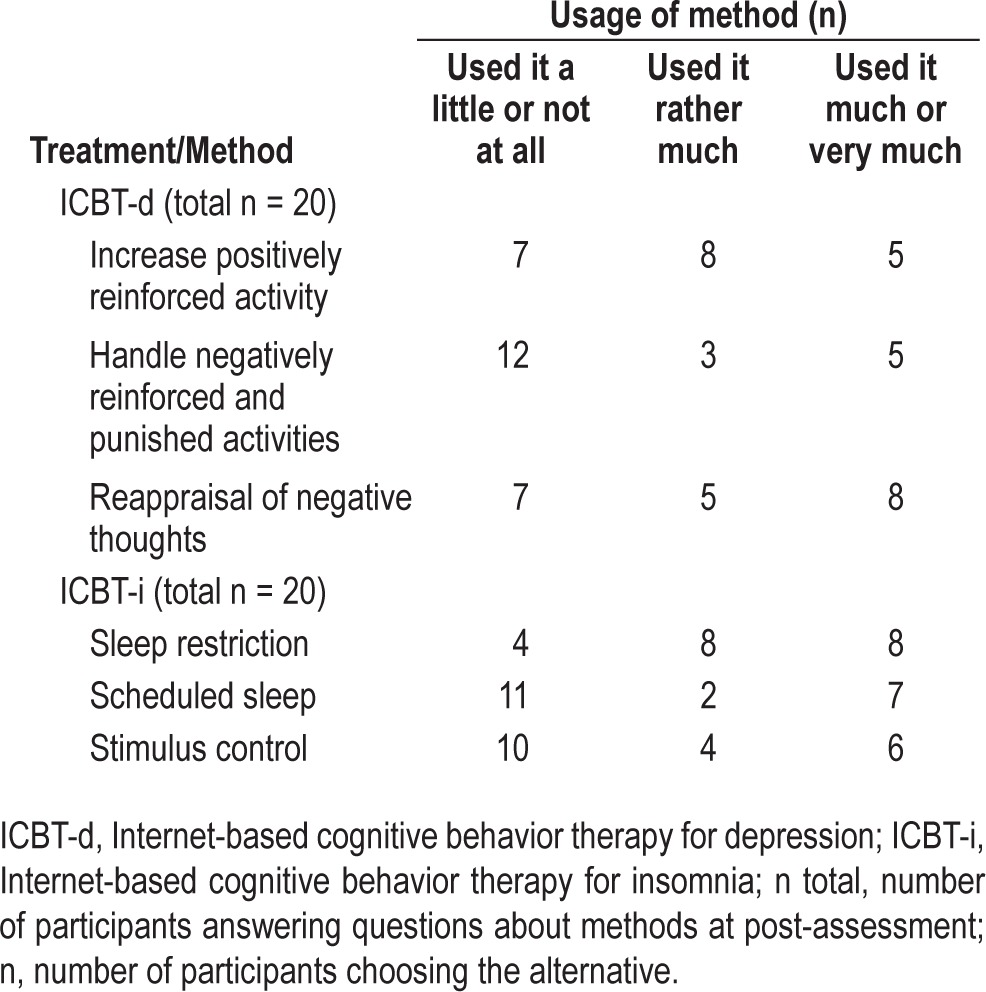
Treatment Adherence
Two participants (both in the ICBT-i group) dropped out of treatment immediately after start and have not read or completed any modules. Postdata were obtained and included in the analysis for both these participants, 6 and 12 mo follow-up data was obtained and included for one of them. There was no significant difference between the groups regarding number of modules completed. The ICBT-i group completed 82% (standard deviation [SD] 27%) and the ICBT-d group 93% (SD 16%) of the modules. At the post-assessment, participants were asked how much they had used the main treatment components, results are presented in Table 2. No significance tests were made to compare these since the treatments had different main components.
Table 2.
Usage of main treatment components, self-rated posttreatment.
The groups were then compared on a range of more general adherence measures, and t tests found no significant differences (P = 0.15–0.96) regarding: number of times participants were logged in (ICBT-d: mean = 77 [56], ICBT-i: mean = 78 [42]); number of messages sent to therapist (ICBT-d: mean = 15 [9], ICBT-i: mean = 20 [11]); number of messages received from therapist (ICBT-d: mean = 15 [7], ICBT-i: mean = 17 [7]); total therapist time (min) spent per participant (ICBT-d: mean = 89 [53], ICBT-i: mean = 116 [72]). Client satisfaction, measured posttreatment with Client Satisfaction Questionnaire-8 (CSQ-8), showed similar treatment satisfaction between groups (ICBT-d: mean = 22.6 [4.4], ICBT-i: mean = 23.1 [4.8]).
Primary Outcome Measures
Both groups improved significantly on both measures from pre-assessment to post-assessment (P ≤ 0.002). Improvements were still significant and slightly increased at 6- and 12-mo follow-up. The mixed-model analysis showed a significant interaction effect of group and time for ISI pre-assessment to post-assessment (ISI; F = 3.82, df = 124, P = 0.05) to the advantage of ICBT-i. From post-assessment to FU12, the difference between groups was maintained and significant (P = 0.04) (Figure 2 and Table 3). There was no significant interaction effect from pre-assessment to post-assessment for MADRSS, and neither was there a significant difference between the groups during the follow-up period.
Figure 2.
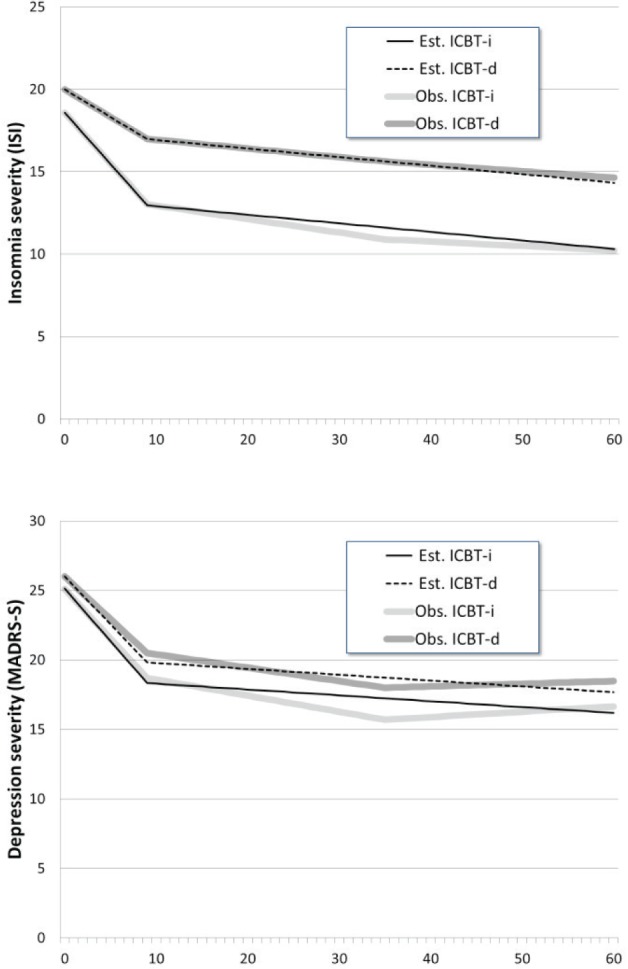
Change in insomnia and depression severity; comparison between treatments, estimated and observed means. ISI, Insomnia Severity Index, mean values; MADRS-S, Montgomery Åsberg Depression Rating Scale – Self rating, mean values; X-axis, number of weeks, posttreatment at 9 w, 6- and 12-mo follow-up at 35 and 61 w, respectively; ICBT-i, group receiving Internet-based cognitive behavior therapy for insomnia; ICBT-d, group receiving Internet-based cognitive behavior therapy for depression.
Table 3.
Means, standard deviations, and effect sizes (Cohen's d) of primary outcome measures and sleep diary data, observed data.
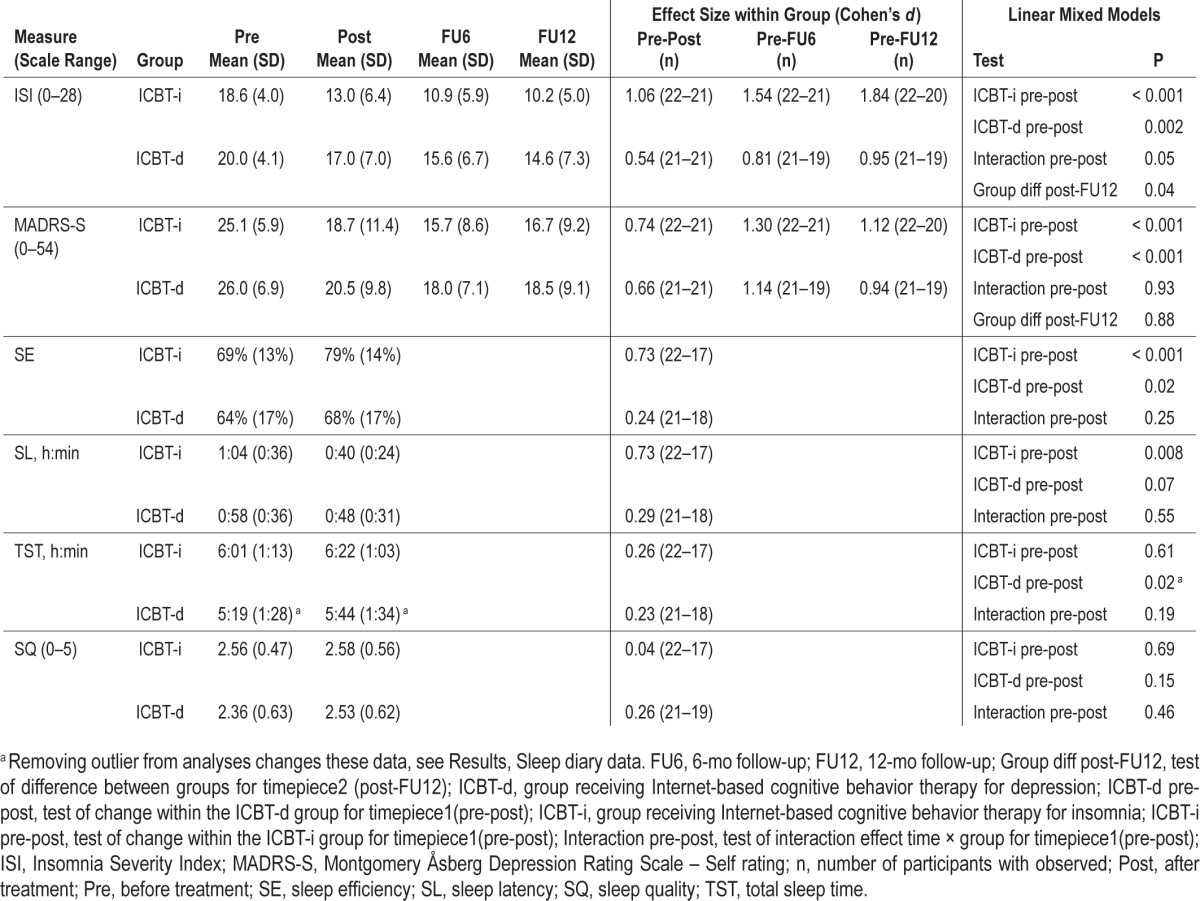
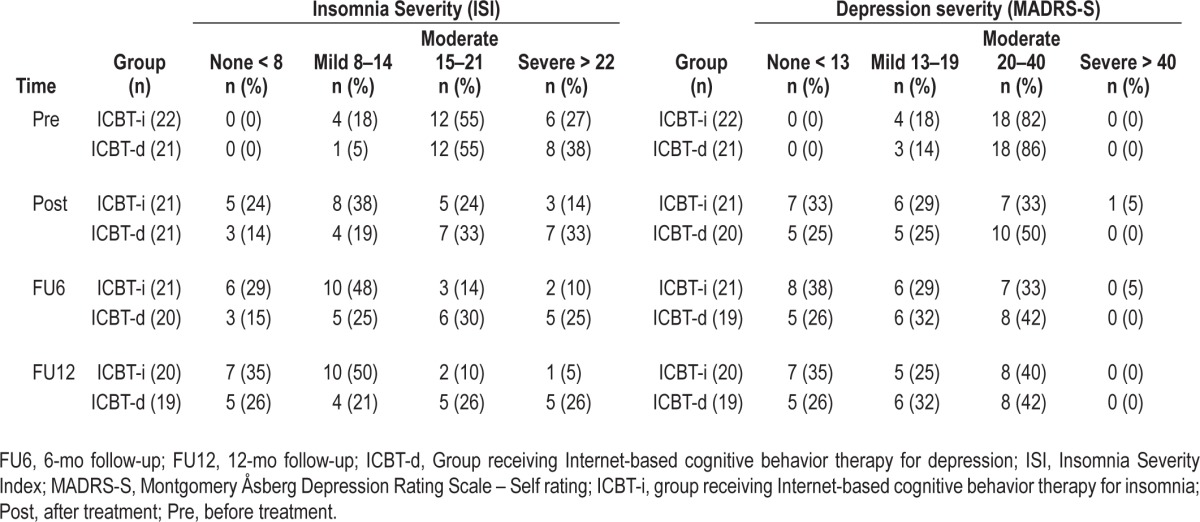
Within-group effect sizes across assessment points were moderate to very large for ICBT-i, and moderate to large for ICBT-d (Table 3). The sensitivity analysis done of MADRS-S without the sleep item showed that this item did not affect the results. Scores for ISI and MADRS-S divided into groups reflecting symptom severity54,55 at all timepoints can be seen in Table 4.
Table 4.
Scores per group and symptom severity for Insomnia Severity Index and Montgomery Åsberg Depression Rating Scale – Self rating, observed data.
Secondary Outcome Measures
Sleep Diary Data
Because of high attrition for sleep diaries at follow-up assessments, these data were only analyzed from pre-assessment to post-assessment. No significant interactions between groups were found for sleep diary data (Table 3). However, there were some significant within-groups effects. The ICBT-i group increased their mean sleep efficiency from 69% to 79% (P < 0.001) and the ICBT-d group from 64% to 68% (P = 0.02). The ICBT-i group also decreased their mean sleep latency with 24 min (P < 0.008) whereas the ICBT-d group increased their TST with 22 min (P = 0.02). One outlier was found in the ICBT-d with an increased total sleep time of 6.1 h. This participant already used zolpidem, and started to use mirtazapine, an antidepressant with documented sedative effects,59 during the treatment period. An analysis without this outlier rendered the TST-increase (now 5 min) non-significant. The other sleep data showed no changes in significance levels when removing the outlier.
Need for Further Treatment
At post-assessment 80% in the ICBT-d group wanted further treatment for insomnia (i.e., had 2 or 3 points on the scale (0–3) for this item) compared to 40% in the ICBT-i group. This difference was significant (t = −4.55, df = 38, P < 0.001). The proportion of the ICBT-d group who intended to seek insomnia treatment was also significantly higher, 75% versus 30% in the ICBT-i group (t = −2.99, df = 38, P < 0.005). There was no significant difference between the groups regarding their wish for (81% for ICBT-d versus 68% for ICBT-i), or intention to seek more treatment (52% versus 68%) for depression.
Insomnia and Depression Diagnoses and Remission
There was a significant difference between groups regarding remission from insomnia after treatment according to the psychiatrist assessment (using the same criteria as in pretreatment assessment) in favor of the ICBT-i group (P < 0.05). In the ICBT-i group 57% (12 of 21) no longer had insomnia, compared to 19% (3 of 16) in the ICBT-d group. There was no significant difference between groups regarding remission from depression. Posttreatment, 37% (7 of 19) were in remission from depression in the ICBT-i group and 21% (4 of 19) in the ICBT-d group. Using intent-to- treat data (assuming missing patients are not in remission) does not change significance levels. Using remission criteria for ISI (< 8) and MADRS-S (< 13) there was no significant difference between groups regarding remission from diagnoses at any assessment point (see Table 4).
Use of Other Treatments
Significantly more participants in the ICBT-i group discontinued or reduced their sleep medication use during the treatment period compared to the ICBT-d group (12 of 13 versus 6 of 12 users, P < 0.05). One participant in the ICBT-i group increased their use of antidepressants during the treatment period, whereas one person in the ICBT-d group started and one stopped using antidepressants.
From posttreatment to 12 mo follow-up, two participants in the ICBT-d group received another treatment for depression and two for insomnia; all reported no help was gained. One person in the ICBT-i group received another treatment for insomnia (no improvement) and two participants received another treatment for depression; one reported improvements.
Adverse Events
At the posttreatment telephone interview, four participants per group reported having experienced negative consequences from treatment. In the ICBT-i group two persons complained of getting tired from doing sleep restriction, one was discontent with unwanted changes of habits (e.g., not being allowed to watch TV in bed) and two persons noticed other problems in life more when the insomnia and depression improved. In the ICBT-d group two participants had experienced stress from filling out the weekly activity plan, one was stressed from the amount of text to be read, and one had experienced a lack of time.
DISCUSSION
Our main finding is that insomnia treatment was significantly more effective than depression treatment regarding insomnia severity, and equally effective in reducing depression, for patients in whom both conditions were diagnosed. This advantage for the insomnia treatment was further strengthened by higher remission rates according to the live assessment of diagnoses posttreatment (but not according to remission criteria for ISI), larger decrease in use of sleep medication, and that after treatment, the ICBT-d group wanted more additional treatment for insomnia than the ICBT-i group. There was no difference between groups in their wish for additional depression treatment. Although this study has a different design, these findings are in line with the studies by Manber and colleagues31 as well as Fava and colleagues,32 where adding insomnia treatment to depression treatment improves outcome for both conditions.
There are several possible explanations why the insomnia treatment yielded better results than the depression treatment. Previous studies suggest unspecific mechanisms of action in treatment of depression, which could explain why the insomnia treatment resulted in reduced depression severity even though depression was not specifically targeted. Insomnia treatment, however, seems to be mediated by more specific mechanisms of action, which may explain the insomnia treatment's superior results for alleviating insomnia. Another explanation could be that when both conditions are present, depression is more often caused or maintained by insomnia than vice versa, which suggests that treating insomnia might reduce depression. This notion is supported by Chang et al.25 and Buysse et al.,4 who showed that insomnia often precedes depression. At a slightly different angle, Staner60 discusses several possible mechanisms of how insomnia could cause depression: the effects of sleep deprivation on the endocrine system; the initiation of worrying and rumination while trying to fall asleep; diminished capacity to cope with social and interpersonal challenges; learned helplessness; and the use of hypnotic drugs or tranquilizers. Researchers in Norway61 showed that the use of hypnotics (benzodiazepines) was related to subsequent development of depression and anxiety. Hence, it is possible that the discontinuation or tapering of sleep medication, which was more frequent in the ICBT-i group, may partly explain the results. Antidepressant use was stable for 2 mo before treatment, and did not differ significantly between groups. Still, the ICBT-i-group may have had a slight advantage over the ICBT-d-group in that eight participants (versus five in the ICBT-d-group) were stable on antidepressants at baseline, which might have affected symptom severity outcomes positively. Also, less time spent in bed (because of sleep restriction or scheduled sleep) could be a mechanism for change of depression severity in the ICBT-i group, thanks to increased daytime activity. In a corresponding manner, increased daytime activity and daylight, which is part of the depression treatment manual, is likely to positively affect sleep.
SE improved more for the ICBT-i group than the ICBT-d group (but not significantly so), and sleep latency decreased for the ICBT-i group, in line with the hypothesis. This improvement is probably an effect of using the sleep restriction technique, supporting the notion that insomnia treatment has specific mechanisms of action. TST increased significantly for the ICBT-d group but not for the ICBT-i group, which is an unexpected finding. Removing an outlier from the analyses did, however, change the average TST-increase for ICBT-d from 22 to 5 min and rendered the increase nonsignificant, but did not alter any other sleep diary findings. No other significant differences between the treatments were seen in sleep diary data, possibly in part because of the small sample and relatively high attrition rate, since sleep diary changes tend to be smaller than subjective ratings of insomnia.15 Another reason for the small changes in sleep diary data could be the participants' high symptom levels, which may have affected outcome on the whole (discussed in the next paragraph).
Across all timepoints, both treatments had moderate to large within-group effect sizes, comparable to previous studies on CBT and ICBT for depression and insomnia, respectively.12,13,15–17,21 The only exception was the postmeasure on depression symptoms for the depression treatment (ICBT-d), showing a smaller effect compared to the original study21 and when the treatment has been used in regular care.57 This might be explained by the fact that the sleep module included in the original treatment was removed in the current study in order not to provide explicit insomnia treatment to the ICBT-d group and confound the design of the study. Another explanation could be that the treatment was only nine weeks long, as compared to eight to ten weeks in the original study and twelve weeks in regular care. Paired with the fact that the participants in this study had more severe depression, nine weeks may not have been enough time for the treatment to produce full effect. However, at the 6-mo follow-up, the effect size of MADRS-S was large even though no treatment was added after the nine weeks. This might indicate that the treatment was indeed adequate, but that full treatment effect did not show until later. The participants in both treatment conditions had access to all treatment material for 6 mo after treatment (except therapist contact), which means they could repeat and complete treatment work at their own discretion. This might affect long term outcomes. Still, it would be preferable that this study's design was repeated comparing insomnia treatment to a depression treatment that was validated for the exact same length as the insomnia treatment and, most importantly, without a sleep module.
Even though the effect sizes for both measures (ISI and MADRS-S) were large at the 6- and 12-mo follow-up, it is of interest that for both measurements, the symptom severity mean scores stayed fairly high at the follow-up assessments. For the most improved group, ICBT-i, the mean ISI-score at 12-mo follow-up ended up above the diagnosis cutoff for insomnia, indicating that patients on average still had a mild insomnia. For depression, the mean MADRS-S score ended up leaving most participants with a mild depression at 12-mo follow-up. Furthermore, remission rates according to criteria for ISI (< 8 points) and MADRS-S (< 13 points) were relatively low for both groups (Table 4), and sleep diary data show less than satisfactory results. Compared to the other self-help studies previously mentioned, these patients had more severe insomnia and depression both before and after treatment. There was also a relatively large number of participants in both groups with an average of less than 6 h of sleep pretreatment (see Table 1), something that previous studies by Vgontzas et al.62 have shown could be a more afflicted group with more sleep related health issues than individuals with insomnia with longer total sleep time. This could indicate that comorbidity between insomnia and depression implies a heavier symptom burden than insomnia or depression only. We therefore suggest further research, looking into more effective treatments for this patient group. To follow up on the aforementioned studies by Manber et al.31 and Fava et al.,32 it seems relevant to study combined CBT for insomnia and depression.
This study uses Internet-based treatment, which implies that generalizability to other forms of CBT is limited. The findings could be limited to a population of patients willing and able to self-refer to and engage in an Internet-based guided self-help treatment. However, in previous studies,63–65 ICBT has been shown to be equivalent to individual and group therapy. It is therefore not entirely farfetched to hypothesize that similar results regarding the relationship between insomnia and depression treatment (if not the actual treatment effects per se) might be found if this study was repeated using group or individual therapy. This hypothesis would need to be tested in a future trial.
The most obvious limitation to this study is the small sample size, making the statistical analyses underpowered. The study needs to be replicated with more subjects and preferably with the use of traditional CBT administration formats (individual or group), in order to strengthen or disprove the conclusions. Also, it would be preferable to assess sleep using two weeks of sleep diary according to recommendations by Buysse and colleagues.66 Another limitation is that the manual text in the insomnia treatment was delivered in the form of a book, whereas the text in the depression treatment was presented on the Internet site. Even though all other material, i.e., reading instructions, exercises, worksheets, homework assignments, and communication with the psychologist was delivered online in both treatments, this difference might have affected the outcome. A fourth limitation is that the study did not have blind assessors. However, the primary outcome measures in this study are self-rating scales, where assessors have no effect. Also, the involved physicians did not have anything invested in the study, nor were they involved in any other part of the study than the assessment.
A strength of this study is the innovative design, where only one of two diagnoses is targeted, to explore what effects this has on both problem areas. Also, the highly structured and standardized format of ICBT makes it an ideal treatment form when comparing interventions with different contents: the risk for content diffusion and low adherence to the treatment protocol is diminished as compared to individual or group therapy, where a therapist to a much larger extent determines the treatment content that is conveyed. The therapists in this study had university level training and experience in CBT and were supervised by the same senior psychologist. These factors minimize the risk for so called therapist drift, i.e., that the therapist along the way changes the content of the treatment. Other strengths are the thorough assessment procedures and that few data were lost.
CONCLUSION
This randomized controlled trial indicates that CBT for insomnia is an important treatment for patients suffering from both insomnia and depression. The results support the notion that insomnia, when comorbid with depression, is not merely a symptom of or secondary to depression, but that both problems need to be addressed with evidence-based treatments. Given the high levels of insomnia and depression severity, this burdened patient group deserves special attention.
DISCLOSURE STATEMENT
This was not an industry supported study. This project was funded by the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet, Söderström-Königska Foundation, KI funds and AFA Sickness Insurance Research Fund. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Thanks to Monica Hellberg for administrative assistance, to Maria Brodin, Lovisa Egnell, Jennie Eriksson, Mia Eriksson, Anna Etzler, Karin Frankel, Astrid Jonsell and Michele Storm for assessments and therapist work, and to the physicians at the Internet Psychiatry Clinic for diagnostic assessments, especially Christian Rück who managed the team and helped with recruitment. Thanks to Brjánn Ljótsson for statistical consultation, system development and support and Per Carlbring for help with recruitment.
Footnotes
A commentary on this article appears in this issue on page 177.
REFERENCES
- 1.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 2.Arroll B, Fernando A, 3rd, Falloon K, Goodyear-Smith F, Samaranayake C, Warman G. Prevalence of causes of insomnia in primary care: a cross-sectional study. Br J Gen Pract. 2012;62:99–103. doi: 10.3399/bjgp12X625157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soldatos CR. Insomnia in relation to depression and anxiety: epidemiologic considerations. J Psychosom Res. 1994;38:3–8. doi: 10.1016/0022-3999(94)90130-9. [DOI] [PubMed] [Google Scholar]
- 4.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 6.Daley M, Morin CM, LeBlanc M, Gregoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- 7.Leger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63:49–55. doi: 10.1097/00006842-200101000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Morin CM, Gramling SE. Sleep patterns and aging: comparison of older adults with and without insomnia complaints. Psychol Aging. 1989;4:290–4. doi: 10.1037//0882-7974.4.3.290. [DOI] [PubMed] [Google Scholar]
- 9.Wiley JA, Camacho TC. Life-style and future health: evidence from the Alameda County study. Prev Med. 1980;9:1–21. doi: 10.1016/0091-7435(80)90056-0. [DOI] [PubMed] [Google Scholar]
- 10.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 11.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia:update of the recent evidence (1998-2004) Sleep. 2006;29:1398–414. doi: 10.1093/sleep/29.11.1398. [DOI] [PubMed] [Google Scholar]
- 12.Riemann D, Perlis ML. The treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med Rev. 2009;13:205–14. doi: 10.1016/j.smrv.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Hedman E, Ljotsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res. 2012;12:745–64. doi: 10.1586/erp.12.67. [DOI] [PubMed] [Google Scholar]
- 15.van Straten A, Cuijpers P. Self-help therapy for insomnia: a meta-analysis. Sleep Med Rev. 2009;13:61–71. doi: 10.1016/j.smrv.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Jernelov S, Lekander M, Blom K, et al. Efficacy of a behavioral self-help treatment with or without therapist guidance for co-morbid and primary insomnia--a randomized controlled trial. BMC Psychiatry. 2012;12:5. doi: 10.1186/1471-244X-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ritterband LM, Thorndike FP, Gonder-Frederick LA, et al. Efficacy of an Internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009;66:692–8. doi: 10.1001/archgenpsychiatry.2009.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng SK, Dizon J. Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis. Psychother Psychosom. 2012;81:206–16. doi: 10.1159/000335379. [DOI] [PubMed] [Google Scholar]
- 19.Espie CA, Kyle SD, Williams C, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35:769–81. doi: 10.5665/sleep.1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Straten A, Emmelkamp J, de Wit J, et al. Guided Internet-delivered cognitive behavioural treatment for insomnia: a randomized trial. Psychol Med. 2013:1–12. doi: 10.1017/S0033291713002249. [DOI] [PubMed] [Google Scholar]
- 21.Andersson G, Bergstrom J, Hollandare F, Carlbring P, Kaldo V, Ekselius L. Internet-based self-help for depression: randomised controlled trial. Br J Psychiatry. 2005;187:456–61. doi: 10.1192/bjp.187.5.456. [DOI] [PubMed] [Google Scholar]
- 22.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;37:319–28. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 23.Kessler D, Lewis G, Kaur S, et al. Therapist-delivered Internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet. 2009;374:628–34. doi: 10.1016/S0140-6736(09)61257-5. [DOI] [PubMed] [Google Scholar]
- 24.Perini S, Titov N, Andrews G. Clinician-assisted Internet-based treatment is effective for depression: randomized controlled trial. Aust N Z J Psychiatry. 2009;43:571–8. doi: 10.1080/00048670902873722. [DOI] [PubMed] [Google Scholar]
- 25.Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression. The Johns Hopkins Precursors Study. Am J Epidemiol. 1997;146:105–14. doi: 10.1093/oxfordjournals.aje.a009241. [DOI] [PubMed] [Google Scholar]
- 26.Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behav Sleep Med. 2003;1:227–47. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 27.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Carney CE, Segal ZV, Edinger JD, Krystal AD. A comparison of rates of residual insomnia symptoms following pharmacotherapy or cognitive-behavioral therapy for major depressive disorder. J Clin Psychiatry. 2007;68:254–60. doi: 10.4088/jcp.v68n0211. [DOI] [PubMed] [Google Scholar]
- 29.Pigeon WR, Hegel M, Unutzer J, et al. Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep. 2008;31:481–8. doi: 10.1093/sleep/31.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ. Self-reported sleep disturbance as a prodromal symptom in recurrent depression. J Affect Disord. 1997;42:209–12. doi: 10.1016/s0165-0327(96)01411-5. [DOI] [PubMed] [Google Scholar]
- 31.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fava M, McCall WV, Krystal A, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiat. 2006;59:1052–60. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 33.Cuijpers P, Andersson G, Donker T, van Straten A. Psychological treatment of depression: results of a series of meta-analyses. Nord J Psychiatry. 2011;65:354–64. doi: 10.3109/08039488.2011.596570. [DOI] [PubMed] [Google Scholar]
- 34.Barth J, Munder T, Gerger H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLoS Med. 2013;10:e1001454. doi: 10.1371/journal.pmed.1001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riemann D. Does effective management of sleep disorders reduce depressive symptoms and the risk of depression? Drugs. 2009;69(Suppl 2):43–64. doi: 10.2165/11531130-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 36.Morawetz D. Insomnia and depression: which comes first? Sleep Res Online. 2003;5:77–81. [Google Scholar]
- 37.Lancee J, van den Bout J, van Straten A, Spoormaker VI. Baseline depression levels do not affect efficacy of cognitive-behavioral self-help treatment for insomnia. Depress Anxiety. 2013;30:149–56. doi: 10.1002/da.22004. [DOI] [PubMed] [Google Scholar]
- 38.Harvey L, Inglis SJ, Espie CA. Insomniacs' reported use of CBT components and relationship to long-term clinical outcome. Behav Res Ther. 2002;40:75–83. doi: 10.1016/s0005-7967(01)00004-3. [DOI] [PubMed] [Google Scholar]
- 39.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27:1567–96. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 40.Morin CM. New York, NY: Guilford Press; 1993. Insomnia: Psychological Assessment and Management. [Google Scholar]
- 41.American Psychiatric Association. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 42.American Psychiatric Association. Text revision. 4th ed. Washington, DC: American Psychiatric Association; 2002. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 43.Svanborg P, Åsberg M. A new self-rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr Scand. 1994;89:21–8. doi: 10.1111/j.1600-0447.1994.tb01480.x. [DOI] [PubMed] [Google Scholar]
- 44.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 45.Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 46.Berman AH, Bergman H, Palmstierna T, Schlyter F. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur Addict Res. 2005;11:22–31. doi: 10.1159/000081413. [DOI] [PubMed] [Google Scholar]
- 47.First MB, Gibbon M, Spitzer RI, Williams JBW, Benjamin LS. Danderyd: Pilgrim Press; 1999. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (Swedish version) [Google Scholar]
- 48.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 49.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. quiz 4–57. [PubMed] [Google Scholar]
- 50.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 51.Thorndike FP, Ritterband LM, Saylor DK, Magee JC, Gonder-Frederick LA, Morin CM. Validation of the insomnia severity index as a web-based measure. Behav Sleep Med. 2011;9:216–23. doi: 10.1080/15402002.2011.606766. [DOI] [PubMed] [Google Scholar]
- 52.Hedman E, Ljotsson B, Blom K, et al. Telephone versus internet administration of self-report measures of social anxiety, depressive symptoms, and insomnia: psychometric evaluation of a method to reduce the impact of missing data. J Med Internet Res. 2013;15:e229. doi: 10.2196/jmir.2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 54.Morin CM, Espie CA. New York: Springer; 2003. Insomnia: A Clinician's Guide to Assessment and Treatment. [Google Scholar]
- 55.Svanborg P, Ekselius L. Self-assessment of DSM-IV criteria for major depression in psychiatric out- and inpatients. Nord J Psychiatry. 2003;57:291–6. doi: 10.1080/08039480307281. [DOI] [PubMed] [Google Scholar]
- 56.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 57.Hedman E, Ljotsson B, Kaldo V, et al. Effectiveness of Internet-based cognitive behaviour therapy for depression in routine psychiatric care. J Affect Disord. 2014;55:49–58. doi: 10.1016/j.jad.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 58.Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61:310–7. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- 59.Dolder CR, Nelson MH, Iler CA. The effects of mirtazapine on sleep in patients with major depressive disorder. Ann Clin Psychiatry. 2012;24:215–24. [PubMed] [Google Scholar]
- 60.Staner L. Comorbidity of insomnia and depression. Sleep Med Rev. 2010;14:35–46. doi: 10.1016/j.smrv.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 61.Neckelmann D, Mykletun A, Dahl AA. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007;30:873–80. doi: 10.1093/sleep/30.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32:491–7. doi: 10.1093/sleep/32.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hedman E, Andersson G, Ljotsson B, et al. Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: a randomized controlled non-inferiority trial. PLoS One. 2011;6:e18001. doi: 10.1371/journal.pone.0018001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kaldo V, Levin S, Widarsson J, Buhrman M, Larsen HC, Andersson G. Internet versus group cognitive-behavioral treatment of distress associated with tinnitus: a randomized controlled trial. Behav Ther. 2008;39:348–59. doi: 10.1016/j.beth.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 65.Carlbring P, Nilsson-Ihrfelt E, Waara J, et al. Treatment of panic disorder: live therapy vs. self-help via the Internet. Behav Res Ther. 2005;43:1321–33. doi: 10.1016/j.brat.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 66.Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29:1155–73. doi: 10.1093/sleep/29.9.1155. [DOI] [PubMed] [Google Scholar]