Abstract
The Institute of Medicine and the National Research Council have issued new guidelines for gestational weight gain as well as recommendations for action and research that call for “a radical change in the care provided to women of childbearing age.” For the first time, these guidelines consider the outcomes of both mother and child during and after delivery and the trade-offs between them. The recommendations call for women to begin pregnancy at a healthy weight and to gain within the guidelines, a goal not previously achieved. They also call for individualized preconceptional, prenatal, and postpartum care to help women attain a healthy weight, gain within the guidelines, and return to a healthy weight. Scientific evidence was inadequate to provide specific guidelines by obesity class or to support a public health recommendation to reduce the guidelines below 5–9 kg (11–20 lb) for obese women.
Since the Institute of Medicine (IOM) issued the 1990 guidelines1 for gestational weight gain, the proportion of overweight or obese (body mass index [BMI] 25.0 kg/m2 or more) women of reproductive age has increased from 37%2 to 59.5% in 2007–2008,3 Although gaining within the 1990 IOM gestational weight gain guidelines1 is associated with minimal postpartum weight retention,4 concern has been expressed that these guidelines contributed to the rise in obesity among women of reproductive age.5 The more likely contributor to our obesity epidemic is excessive gestational weight gain; in fact, 38% of normal weight, 63% of overweight, and 46% of obese women gained more than recommended.4 This emphasizes the importance of preventing the development of obesity among women who are normal weight or overweight as well as minimizing maternal and fetal risks among obese women. In this commentary, we discuss the novel features of the 2009 report from the IOM and National Research Council that reexamined the gestational weight gain guidelines and highlight aspects of it that address the recommendation for obese women.
The 2009 report, “Weight Gain During Pregnancy: Reexamining the Guideline,”4 was developed from several important perspectives. First, the multidisciplinary expert committee that wrote the report sought recommendations that would balance risks of high and low gestational weight gain while respecting the principle of “first, do no harm.” Second, the committee was required to base its recommendations on published scientific evidence, which is particularly limited for obese women, and to develop a consensus based on scientific evidence. These approaches often lead to conservative recommendations. Third, the charge to the committee was to examine the role of gestational weight gain within prepregnancy BMI categories. In this conceptualization, recommendations for gestational weight gain have the potential to modify the consequences of this exposure but cannot address the excess weight that many women have at conception.
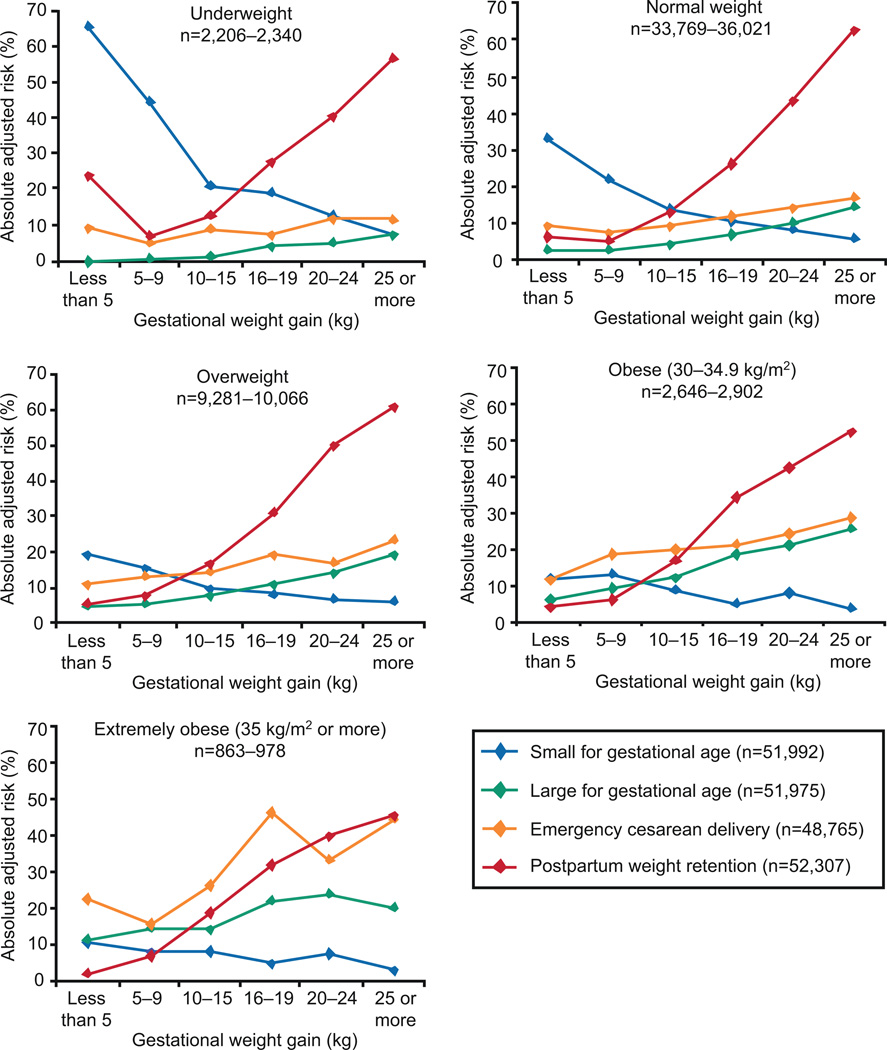
Most importantly, the 2009 report broke new scientific ground because its recommendations were based on the outcomes of both the mother and child.4 The trade-offs between them were reconciled to the extent permitted by available data, which included a systematic evidence-based review on the outcomes of gestational weight gain6 as well as invited presentations and commissioned reports. In the available data, the outcomes for mothers most plausibly related to gestational weight gain were cesarean delivery and postpartum weight retention; the outcomes for offspring were preterm birth, extremes of birth weight (expressed as small- or large-for-gestational age), and childhood obesity. The committee evaluated studies in which all these outcomes were studied simultaneously across the range of gestational weight gain (Fig. 1) as well as less comprehensive studies. To project the possible importance of these outcomes over the mother’s or child’s lifetime, a quantitative risk analysis was commissioned.4
Fig. 1.
Gestational weight gain–specific absolute risks for small for gestational age, large for gestational age, emergency cesarean delivery, and postpartum weight retention within each body mass index group. Note: Absolute risks are derived from odds ratios. Risk for a primiparous woman, age 25–29 years, height 1.60–1.69 m, nonsmoker, no alcohol consumption, high social status, no exercise, 280 days of gestation; for postpartum weight retention, breastfeeding less than 14 weeks. Modified with permission from Nohr EA. Appendix G. In: Institute of Medicine/National Research Council (Committee to Reexamine IOM Pregnancy Weight Guidelines, Food and Nutrition Board and Board on Children, Youth, and Families). Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press; 2009. National Academy of Sciences, courtesy of the National Academies Press, Washington, DC. Rasmussen. New Gestational Weight Gain Recommendations. Obstet Gynecol 2010.
2009 Institute of Medicine and National Research Council Guidelines
Although the 2009 gestational weight gain guidelines (Table 1) reinforce those released in 1990, there are several salient differences. First, the BMI categories were changed to those commonly used for other adult health outcomes. Second, a closed gestational weight gain range is provided for obese women, which is based on data primarily from women with BMI values of 30–34.9. Third, the committee found no justification for continuing to include modified recommendations for short, young, or black women. Most important, however, the committee made specific action recommendations that—if fully implemented—would “represent a radical change in the care provided to women of childbearing age.”4 The committee noted that, “These services may need to continue into the postpartum period to give women the maximum support to return to their prepregnant weight within the first year and, thus, to have a better chance of returning to a normal BMI value at the time of a subsequent conception.”4
Table 1.
2009 Institute of Medicine and National Research Council Recommendations for Total and Rate of Weight Gain During Pregnancy, by Prepregnancy Body Mass Index
| Rates of Weight Gain* |
||||
|---|---|---|---|---|
| Prepregnancy BMI (kg/m2) |
Total Weight Gain |
Second and Third Trimesters |
||
| Range (kg) | Range (lb) | Mean (Range) (kg/wk) | Mean (Range) (lb/wk) | |
| Underweight (less than 18.5) | 12.5–18.0 | 28.0–40.0 | 0.51 (0.44–0.58) | 1.0 (1.0–1.3) |
| Normal weight (18.5–24.9) | 11.5–16.0 | 25.0–35.0 | 0.42 (0.35–0.50) | 1.0 (0.8–1.0) |
| Overweight (25.0–29.9) | 7.0–11.5 | 15.0–25.0 | 0.28 (0.23–0.33) | 0.6 (0.5–0.7) |
| Obese (30.0 or higher) | 5.0–9.0 | 11.0–20.0 | 0.22 (0.17–0.27) | 0.5 (0.4–0.6) |
BMI, body mass index.
Calculations include a total first-trimester gain of 2 kg (1–3 kg) for all except obese women, who should gain 1.5 kg (0.5–2.0 kg).
Data from Institute of Medicine/National Research Council (Committee to Reexamine IOM Pregnancy Weight Guidelines, Food and Nutrition Board and Board on Children, Youth, and Families). Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press, 2009.
To prevent more women from developing obesity, the committee recommended that action be taken before, during, and after pregnancy. Preconceptionally, overweight women should receive individual counseling to improve diet quality, increase physical activity, and normalize weight. During pregnancy, all women should be encouraged to gain within the new guidelines. The recommended weight gain ranges are those most consistently associated with good outcomes, including reduced postpartum weight retention. Clinicians are encouraged to use weight gain grids to plot weight gain at each prenatal visit. These charts can form the basis for a discussion of gestational weight gain goals and progress toward these goals, and provide an opportunity for individual counseling, given by the clinician or by referral to an appropriate professional, on diet and physical activity. Breastfeeding is recommended to optimize infant health and to assist the mother in normalizing her weight. Postpartum, women should be assisted in achieving and maintaining a healthy weight to increase the likelihood of good outcomes in subsequent pregnancies.
2009 Institute of Medicine and National Research Council Guidelines for Obese Women
For obese women, the committee supported weight loss before pregnancy to improve menstrual functioning, ovulation, and metabolic profile and reduce infertility.7,8 The American College of Obstetricians and Gynecologists recommends that obese women lose weight before and not during pregnancy.9 Among morbidly obese women, bariatric surgery before conception may improve birth outcomes.4
Perhaps the most controversial element of the 2009 IOM and National Research Council report is the guideline for obese women because it is neither lower nor specific for the several obesity classes. Data did not support a lower limit and were insufficient to provide this level of specificity. The committee evaluated data that demonstrated good clinical outcomes among obese and extremely obese women who gain below the amount (approximately 7.5–8.5 kg) required to meet the obligatory maternal tissue accretion during pregnancy and products of conception. Some obese and extremely obese women gain less than lighter women and may even lose weight during pregnancy.10,11 However, only limited data are available on the short- and long-term consequences for the offspring that would support low gestational weight gain or weight loss during gestation. Evidence was not available for the committee to assess whether, when pregnant women lose weight or gain little, the usual pregnancy-induced physiologic, metabolic, and endocrine changes will occur or whether changes that may have adverse consequences for fetal growth and development will occur instead. Such weight changes would mean mobilization of maternal adipose tissue and, possibly, protein stores, but the extent and consequences of these possibilities are unknown.
Dietary patterns, eating behaviors, and physical activity patterns leading to low gestational weight gain or weight loss have not been studied, but expected changes in fuel homeostasis can be deduced from studies conducted in pregnant women subjected to prolonged fasting. Ketonemia; increased free fatty acids; lowered plasma glucose, insulin, and gluconeogenic amino acids; ketonuria, and increased urinary nitrogen excretion were observed.12,13
It is unknown whether intentional prolonged fasting is common in pregnancy, but just skipping breakfast after overnight sleeping can result in a 12- to 18-hour fast. A substantial proportion of pregnant women with normal glucose tolerance have elevated blood ketone concentrations at some time during gestation.14 As a result of caloric insufficiency, low gestational weight gain or weight loss may induce maternal hormonal and metabolic responses that may, in turn, have consequences for the neurologic development of the child. However, research is mixed on whether biomarkers of metabolic fuel alternations are associated with the child’s intellectual development.4
The committee’s review showed that there was insufficient evidence to recommend low gains or weight loss. Women in obesity classes II and III may, without intervention, gain little during pregnancy and may manage their pattern of dietary intake to avoid ketonemia. However, there is no evidence to determine whether a public health guideline for very low weight gain during pregnancy among women in obesity classes II and III would be managed well enough to avoid ketonemia or other potential adverse outcomes.4 More research on this subject is needed.
The committee concluded that low gain or weight loss during pregnancy is not recommended for obese women because of the potential for irreversible effects on child neurologic development. The risks for small for gestational age (SGA) and preterm births rise with decreasing gestational weight gain in all women.4 SGA is associated with minimal neurologic dysfunction (eg, poor school performance) and is not associated with major handicaps, such as cerebral palsy, unless accompanied by asphyxia at birth.15,16 Preterm SGA is associated with cognitive, neurodevelopmental, or both cognitive and neurodevelopmental impairments, although this relationship may be modified by degree of postnatal catch-up growth and maternal-child interactions.17,18 The committee called for research to address the many unknowns in the pathway from low gestational weight gain or even weight loss during pregnancy to neurologic outcomes in the child.
Since this report was released, interventions to help women gain within the gestational weight gain guidelines by modifying diet, taking on physical activity, or doing both have been published.19 Prenatal intervention programs have often—but not always—helped obese women to limit their gestational weight gain. Further studies with adequate sample sizes are needed that evaluate both the short- and long-term outcomes for women and their children. Only once the efficacy and safety of such interventions have been evaluated can it be determined whether public health recommendations to lower the gestational weight gain guideline for obese women would be appropriate.
CONCLUSIONS
The 2009 IOM and National Research Council–recommended gestational weight gain ranges are those most consistently associated with good maternal and infant outcomes for all women. Individualized preconceptional, prenatal, and postpartum care are needed to support women to gain within the guidelines and attain healthy weight postpartum in our challenging obesogenic environment. The recommendations for action and research in the new guidelines are designed to help women meet these goals.
As clinicians and researchers, we are also challenged by what to do in the face of uncertainty, particularly that related to caring for obese women who become pregnant. Scientific evidence was inadequate to provide specific guidelines by obesity class or to support a public health recommendation to reduce the guidelines below 5–9 kg (11–20 lb) for obese women. Until further research is available, individualized care and good clinical judgment will remain the cornerstones of the obstetric care of obese women.
Acknowledgments
This commentary draws on the Institute of Medicine report, “Weight Gain During Pregnancy: Reexamining the Guidelines” (2009), which was supported in part by the U.S. Department of Health and Human Services and a grant from the March of Dimes Foundation. It was prepared by a committee composed of Claude Bouchard, Matthew Gillman, Fernando Guerra, Paula Johnson, Michael Lu, Elizabeth McAnarney, Rafael Perez-Escamilla, David Savitz, and the authors of this article. Any views not attributed to the report are those of the authors and do not necessarily represent the views of the Institute of Medicine.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Nutrition during pregnancy: part I, weight gain; part II, nutrient supplements. Washington, DC: National Academies Press; 1990. Institute of Medicine (Subcommittees on Nutritional Status and Weight Gain During Pregnancy and Dietary Intake and Nutrient Supplements During Pregnancy, Committee on Nutritional Status During Pregnancy and Lactation, Food and Nutrition Board) [Google Scholar]
- 2.Health, United States, 2005. Hyattsville, MD: U.S. Department of Health and Human Services; 2005. National Center for Health Statistics. [Google Scholar]
- 3.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 4.Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press; 2009. Institute of Medicine/National Research Council (Committee to Reexamine IOM Pregnancy Weight Guidelines, Food and Nutrition Board and Board on Children, Youth, and Families) [Google Scholar]
- 5.Artal R, Lockwood CJ, Brown HL. Weight gain recommendations in pregnancy and the obesity epidemic. Obstet Gynecol. 2010;115:152–155. doi: 10.1097/AOG.0b013e3181c51908. [DOI] [PubMed] [Google Scholar]
- 6.Viswanathan M, Siega-Riz AM, Moos M-K, et al. Evidence report/technology assessment, number 168 (AHRQ Publication No. 08-E09) Research Triangle Park, NC: RTI International–University of North Carolina Evidence-based Practice Center; 2008. Outcomes of maternal weight gain. [Google Scholar]
- 7.Sarwer DB, Allison KC, Gibbons LM, Markowitz JT, Nelson DB. Pregnancy and obesity: a review and agenda for future research. J Women’s Health (Larchmt) 2006;15:720–733. doi: 10.1089/jwh.2006.15.720. [DOI] [PubMed] [Google Scholar]
- 8.Clark AM, Thornley B, Tomlinson L, Galletley C, Norman RJ. Weight loss in obese infertile women results in improvement in reproductive outcome for all forms of obesity treatment. Hum Reprod. 1998;13:1502–1505. doi: 10.1093/humrep/13.6.1502. [DOI] [PubMed] [Google Scholar]
- 9.Obesity in pregnancy. ACOG Committee Opinion No. 315. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2005;106:671–675. doi: 10.1097/00006250-200509000-00054. [DOI] [PubMed] [Google Scholar]
- 10.Kiel DW, Dodson EA, Artal R, Boehmer TK, Leet TL. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110:752–758. doi: 10.1097/01.AOG.0000278819.17190.87. [DOI] [PubMed] [Google Scholar]
- 11.Bodnar LM, Siega-Riz AM, Simhan HN, Himes KP, Abrams B. Severe obesity, gestational weight gain, and adverse birth outcomes. Am J Clin Nutr. 2010;91:1642–1648. doi: 10.3945/ajcn.2009.29008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Felig P, Lynch V. Starvation in human pregnancy: hypoglycemia, hypoinsulemia, and hyperketonemia. Science. 1970;179:990–992. doi: 10.1126/science.170.3961.990. [DOI] [PubMed] [Google Scholar]
- 13.Felig P. Maternal and fetal fuel homeostatis in human pregnancy. Am J Clin Nutr. 1973;26:998–1005. doi: 10.1093/ajcn/26.9.998. [DOI] [PubMed] [Google Scholar]
- 14.Gin H, Vambergue A, Vasseur C, Rigalleau V, Dufour P, Roques A, et al. Blood ketone monitoring: a comparison between gestational diabetes and non-diabetic pregnant women. Diabetes Metab. 2006;32:592–597. doi: 10.1016/S1262-3636(07)70313-0. [DOI] [PubMed] [Google Scholar]
- 15.Grantham-McGregor S. A review of studies of the effect of severe malnutrition on mental development. J Nutr. 2010;125(8 suppl):2233S–2238S. doi: 10.1093/jn/125.suppl_8.2233S. [DOI] [PubMed] [Google Scholar]
- 16.Goldenberg RL, Hoffman HJ, Cliver SP. Neurodevelopmental outcome of small-for-gestational-age infants. Eur J Clin Nutr. 1998;52(suppl 1):S54–S58. [PubMed] [Google Scholar]
- 17.Casey PH, Whiteside-Mansell L, Barrett K, Bradley RH, Gargus R. Impact of prenatal and/or postnatal growth problems in low birth weight preterm infants on school-age outcomes: an 8-year longitudinal evaluation. Pediatrics. 2006;118:1078–1086. doi: 10.1542/peds.2006-0361. [DOI] [PubMed] [Google Scholar]
- 18.Feldman R, Eidelman AI. Neonatal state organization, neuromaturation, mother-infant interaction, and cognitive development in small-for-gestational-age premature infants. Pediatrics. 2006;118:e869–e878. doi: 10.1542/peds.2005-2040. [DOI] [PubMed] [Google Scholar]
- 19.Rasmussen KM, Catalano PM, Yaktine AL. New guidelines for weight gain during pregnancy: what obstetrician/gynecologists should know. Curr Opin Obstet Gynecol. 2009;21:521–526. doi: 10.1097/GCO.0b013e328332d24e. [DOI] [PMC free article] [PubMed] [Google Scholar]