Abstract
This study examined service receipt and unmet service needs among youth with autism spectrum disorders (ASD) in their last year of high school, as well as the youth (intellectual disability, race/ethnicity, autism severity, comorbid psychiatric diagnoses, behavior problems, adaptive behavior) and family (income, parental health, parental depressive symptoms, parental anxiety) correlates of service access. Thirty-nine families of youth with ASD participated. Data were collected via parental interview/questionnaire and youth psychological evaluation. Results suggested that this sample was underserved relative to a nationally-representative cohort. Those with a comorbid psychiatric diagnosis and lower levels of adaptive behavior received more services. Greater unmet needs were reported for youth who were racial/ethnic minorities, who had more behavior problems, and whose parents had greater anxiety.
Keywords: autism spectrum disorder, transition to adulthood, services, comorbid psychiatric disorders, family
With the rising prevalence of autism spectrum disorder (ASD) diagnoses over the past two decades (Gurney et al. 2003), most recently estimated at 1 in 68 children (Centers for Disease Control and Prevention 2014), increasing numbers of these youth exit high school with each passing year. But the transition to adulthood is especially difficult for youth with ASD. These individuals often require assistance in employment and activities of daily living in adulthood (Ballaban-Gil et al. 1996; Billstedt et al. 2005; Eaves and Ho 2008; Howlin et al. 2004; Taylor and Seltzer 2012); however, they are more likely than those with other disabilities to receive no formal services after leaving high school (Shattuck et al. 2011). At least partially as a result, rates of disengagement from paid employment or postsecondary education are especially high (Shattuck et al. 2012; Taylor and Seltzer 2011b), and earlier improvements in the autism behavioral phenotype and the mother-child relationship slow or even stop after high school exit (Taylor and Seltzer 2010, 2011a).
Perhaps because of the accumulating evidence for the importance of early treatments in improving outcomes (Dawson 2008), as well as the high public costs of ASD (Ganz 2007; Cidav et al. 2013; Mandell et al. 2006), a growing body of research has focused on frequency and correlates of service access for children and youth with ASD. Cohorts in most of these studies include a fairly broad age range, often ranging from early childhood through young adulthood (Factor et al. 1990; Green et al. 2006; White et al. 2007; Wei et al. 2013; Liptak et al. 2008; Cidav et al. 2013; Goin-Kochel et al. 2007); the present study takes an alternative approach, by focusing on patterns and correlates of service access for youth with ASD during a critical point in the life course. Specifically, we examined service access when youth with ASD were in their last year of high school.
We focused on service access at this time for two important reasons: first, this is the last year when formal services are federally mandated by the Individuals with Disabilities Education Act (IDEA). Although IDEA specifies age 16 as the time to begin transition planning, research suggests that many schools do not meet the delineated timelines for transition services and supports (Landmark and Zhang 2013). Thus, schools may wait as late as the last year of high school to implement these vital services/supports, making this time point important in determining which types of services youth with ASD are receiving, as well as their unmet service needs. Further, although IDEA ensures that youth with ASD have access to formal services until they exit the secondary school system (with a requirement to exit by age 22), there is no such mandate for formal services after high school exit. This results in an under-funded adult service system, with many adults with ASD receiving inadequate or no services and supports (Howlin 2005; Shattuck et al. 2011). Services received during the last year of high school are likely critical in setting up youth for successful post-school outcomes (Landmark and Zhang 2013), and youth with ASD who are underserved at this time may be at particular risk for a poor transition to adulthood.
Second, it may be that youth with ASD who are preparing to exit high school and transition into adult life require a distinct set of services relative to earlier years. To date, no study has focused on service receipt or unmet service needs during the last year of high school; in the present study, we examined service access, barriers to service receipt, and youth and family correlates of service access for youth with ASD during this critical time.
Correlates of service receipt
A limited number of youth and family correlates of service receipt among individuals with ASD have been identified in the extant literature. In terms of youth/child characteristics, one of the most consistent factors associated with disparities in service access is race/ethnicity. Individuals with ASD who are racial/ethnic minorities tend to get an ASD diagnosis later (Mandell et al. 2002), and receive fewer services in childhood (Thomas et al. 2007; Liptak et al. 2008) and in adulthood (Shattuck et al. 2011). Further, disparities in service access for youth who are racial/ethnic minorities do not seem to be accounted for by poverty (Liptak et al. 2008). Thus, in the present study, we expected that racial/ethnic minority status would be correlated with disparities in service access.
Further, relative to “higher functioning” children and youth with ASD, those who are “lower functioning” across a number of domains tend to receive more services, likely reflecting greater service needs for these individuals. Specifically, studies have found that children and youth with more communication deficits (Wei et al. 2013; White et al. 2007), greater autism severity (White et al. 2007; Green et al. 2006), fewer social skills (Narendorf et al. 2011), and greater intellectual impairment (Shattuck et al. 2011) receive more services relative to youth who exhibit fewer impairments in each of these domains. In many of these studies (e.g., Green et al. 2006; Narendorf et al. 2011; Shattuck et al. 2011), level of functioning is measured generally, making specific conclusions about the domains of functioning related to service access or unmet service needs difficult. In the present study, we examined specific aspects of functioning, including adaptive behavior, autism symptom severity, and comorbid intellectual disability diagnosis, during this important period prior to high school exit.
Although psychiatric comorbidities in youth with ASD are quite common (prevalence estimated 70%, Simonoff, Pickles, Charman et al., 2008), the influences of comorbid mental health diagnoses or related problem behaviors on service receipt and unmet needs have not yet been examined. However, youth who have a diagnosed comorbid psychiatric disorder are likely to be accessing mental health services, and thus may be receiving more services in general. Therefore, we chose to include both comorbid psychiatric diagnoses and behavior problems as possible correlates of service access.
Family factors have also been examined as correlates of service access, with mixed results. For example, studies have suggested that parents who are in worse physical and mental health report more difficulty accessing services as well as greater unmet service needs (Krauss et al. 2003; Hare et al. 2004; Cadman et al. 2012). The opposite finding has been reported for parental stress, with higher levels of stress related to greater service receipt (Factor et al. 1990; Thomas et al. 2007). Note, however, that behavior problems exhibited by the son/daughter with ASD is one of the most consistent predictors of parental stress and distress (Hastings 2003; Hastings and Brown 2002; Tomanik et al. 2004; Lounds et al. 2007), and Factor and colleagues (Factor et al. 1990) found greater service use among families who had children with more difficult child characteristics. Thus, the relations between parenting stress and greater service receipt might be a spurious result of having a more difficult child.
Similarly, research on the relation between parental socioeconomic status and service access among individuals with ASD has been mixed, with some studies finding that families with lower incomes tend to have a greater difficulty accessing services (Thomas et al. 2007; Liptak et al. 2008; Shattuck et al. 2012), and others finding no such association (Krauss et al. 2003; Narendorf et al. 2011; Wei et al. 2013; Hare et al. 2004). It may be that the mandate for services in IDEA “levels the playing field,” minimizing the impact of family socioeconomic status on the availability of formal services during the school years (Taylor and Seltzer 2010). Given that there is some evidence for an association of family functioning and socioeconomic status with service receipt, we included them as correlates of service access in the present study.
The present study
The present study addresses an important gap in the literature by focusing on frequencies and correlates of service access for youth with ASD who are in their last year of high school and thus preparing to transition to adulthood. In contrast to most previous studies, we not only examined the number of services that youth with ASD were receiving, but also the number of unmet service needs reported by their parents. Note that these two variables are not necessarily the inverse of each other; some youth and their families may be receiving a low number of services but may also have low service needs. Thus, focusing on both service receipt and unmet needs addresses two separate aspects of service access.
Further, we compared our rates of service receipt and unmet needs to a nationally representative sample of youth with ASD in high school – the National Longitudinal Transition Study-2 (NLTS2; Newman et al. 2011). The NLTS2 is a large scale, 10-year study of youth receiving special education services in the United States. Findings regarding youth with disabilities from the NLTS2 (including those with ASD) can be generalized to all youth receiving special education services in the United States. This comparison serves two purposes: 1) it allows us to consider whether service receipt in this mid-South/Midwest cohort is similar to a nationally-representative sample; and 2) it allows us to compare whether service access when youth with ASD are ages 13-16 (the NLTS2 cohort) is similar to service access when youth with ASD are in their last year of high school (the present cohort).
The present study also extends the research on service receipt during the transition years by utilizing an extremely well-characterized sample of youth with ASD. Although cohorts drawn from the NLTS2 or administrative databases (which have provided most of our information on service access during the transition to adulthood) have very large sample sizes, they provide little detail on the specific behavioral and phenotypic characteristics of their ASD cohorts. The present study complements this work by using gold-standard autism diagnostic instruments and well-validated measures of individual and family functioning, in order to examine specific youth and family factors that are associated with service access when youth with ASD are in their last year of high school.
Two research questions were examined in the present study. First, we focused on the patterns of service access among youth with ASD in their last year of high school, including descriptive information about service access, unmet service needs, barriers to service access, as well as how this information compares to the NLTS2. Second, in order to identify those youth most likely to be underserved during their last year of high school, we examined youth (intellectual disability, race/ethnicity, autism symptom severity, comorbid psychiatric disorders, behavior problems, adaptive behavior) and family (income, parental health, parental depressive symptoms, parental anxiety) correlates of service receipt and unmet service needs.
Methods
Participants and Design
The present study included 39 families of youth with ASD who were in their last year of high school. The inclusion criteria were that the son or daughter with ASD was currently within 12 months of high school exit, had received an ASD diagnosis (autistic disorder, Asperger disorder, or pervasive developmental disorder- not otherwise specified) from an educational or health professional, was willing to participate in the study with a responding parent, and the family was able to travel to one of the project sites (large academic medical centers in the mid-South and Midwest). Participants were recruited through a number of venues, including local clinics and other autism-related research studies, as well as local support groups, service providers, and autism organizations. Families received information about the study through these venues; those who were interested contacted a study coordinator and were subsequently screened and enrolled. ASD diagnoses were confirmed through in-person assessments by clinicians with expertise in ASD diagnosis using gold-standard procedures, namely, a combination of scores from the Autism Diagnostic Observation Schedule (ADOS: Lord et al., 1989) administered to the youth and the Autism Diagnostic Interview-Revised (ADI-R; Rutter, LeCouteur, & Lord, 2003) administered to the responding parent, along with clinician judgment. All clinicians had achieved external research reliability in both the ADOS and the ADI-R. Data were collected through parental interview and self-administered questionnaire, and a psychological assessment of the youth with ASD.
The youth with ASD included in this analysis averaged 18.7 years of age (SD = 1.3), with a range from 17.2 to 22.0 (note that because of IDEA, youth with ASD can stay in school until they are 22 years of age, although many of them choose to exit high school with their peers). Over three-fourths (79.5%) of the youth were male and the majority were white non-Hispanic (89.7%). The youth with ASD exhibited tremendous heterogeneity in intellectual functioning, with IQ scores ranging from 40 to 137. Approximately 30% (30.8%) of the youth had IQ scores of 100 or above, suggesting average or above average intellectual functioning. Using well-accepted IQ and adaptive behavior criteria (American Association on Intellectual and Developmental Disabilities 2010), 30.8% had a comorbid intellectual disability. All but one of the youth were living with the responding parent at this time (during their last year of high school), with the remaining youth living in an apartment with around-the-clock supervision.
Approximately one-half (51.3%) of the youth with ASD had been diagnosed with a comorbid psychiatric disorder; with 30.8% diagnosed with two or more comorbid disorders. The most common disorders were anxiety disorder (28.2%), major depressive disorder (25.6%), and obsessive compulsive disorder (25.6%). The majority of youth (61.5%) were taking at least one prescription medication, and 28.3% were taking 4 or more medications (range from 0 to 8).
The parent sample was composed of 35 mothers and 4 fathers. The participating parent ranged from 38.3 years to 59.2 years of age (M = 49.3, SD = 5.0). This was a well-educated and well-resourced sample on average, with over 70% (71.9%) of the responding parents having attained a postsecondary degree (Associate's or Bachelor's degree), and 30.8% earning a post-bachelor's degree. The median household income was between $80,000 and $90,000, although one-quarter of the sample (25.6%) had annual household incomes below $40,000. Two-thirds of parents were married (n = 26 or 66.7%), with all but three (n = 23 or 59.0%) married to the other biological parent of the youth with ASD.
Measures
Service Access
Using a list of services derived from the NLTS2, parents reported on the availability of each of 16 services (e.g., speech/language services, psychological/mental health services or counseling, transportation services; full list of services is provided in Table 1). Similar to the NLTS2, parents reported whether each service was received in the past twelve months. If parents reported that the service was not received, we asked whether that service was needed. The sum of services received was calculated as our measure of number of services. The sum of services needed but not received by the son or daughter was calculated as our measure of unmet service needs (possible range from 0 to 16 for each). Note that the NLTS2 did not ask whether each service was needed, but instead asked parents whether the son/daughter was getting all of his/her service needs met.
Table 1.
Services received by youth with ASD in their last year of high school
| Service | Receiving Service in Present Sample | Not Receiving Service in Present Sample | Receiving Service in NLTS2 | |
|---|---|---|---|---|
| Service Needed but Not Received | Service Not Needed | |||
| 1. Psychological/Mental Health Services or Counseling | 43.6% | 15.4% | 41.0% | 46.2% |
| 2. Speech Language Therapy or Communication Services | 35.9% | 10.3% | 53.8% | 74.6% |
| 3. Career Counseling or Vocational/Job Skills Training | 33.3% | 35.9% | 30.8% | 20.6% |
| 4. Personal Assistant or in-home/in-classroom aide | 33.3% | 2.6% | 64.1% | 53.9% |
| 5. Medical services or diagnosis/evaluation related to special needs | 30.8% | 10.3% | 59.0% | 46.9% |
| 6. Occupational/Life Skills Therapy or Training | 25.6% | 30.8% | 43.6% | 49.0% |
| 7. Tutor | 25.6% | 15.4% | 59.0% | 14.3% |
| 8. Transportation Services | 20.5% | 7.7% | 71.8% | 54.6% |
| 9. Social Work Services | 15.4% | 15.4% | 69.2% | 27.7% |
| 10. Assistive Technology Services/Devices | 10.3% | 10.3% | 79.5% | 15.7% |
| 11. Respite Care | 10.3% | 5.1% | 84.6% | 19.6% |
| 12. Reader or Interpreter | 10.3% | 0% | 89.7% | 6.1% |
| 13. Physical Therapy | 5.1% | 0% | 94.9% | 17.3% |
| 14. Orientation and Mobility Services | 0% | 2.6% | 97.4% | 4.8% |
| 15. Audiology Services | 0% | 7.7% | 92.3% | 2.5% |
| 16. Other Services | 5.1% | 15.4% | 79.5% | 4.7% |
Note. Services are organized by how commonly they are received in the present sample. Rates of service receipt in the NLTS2 were derived from data tables provided on the project website (United States Department of Education, National Center for Special Education Research 2014).
In addition, parents were asked questions from the NLTS2 about barriers in accessing services (e.g., costs of services, language problems, services not being available; full list of possible problems is provided in Table 2). Parents were asked to place a check-mark by each barrier that has been a problem for them in getting or dealing with services. In consultation with families and experts, we added two additional problems to the list provided by the NLTS2; 1) doctor or specialist doesn't accept insurance type; and 2) physical accessibility of services.
Table 2.
Barriers to Receiving Services Reported by Parents
| Percent Endorsed in Present Sample | Percent Endorsed in NLTS-2 | |
|---|---|---|
| 1. Cost of Services | 38.5% | 33.9% |
| 2. Where Services are Provided | 33.3% | 32.7% |
| 3. Doctor/Specialist does not Accept Insurance | 33.3% | Not Asked |
| 4. Services not Available | 25.6% | 49.3% |
| 5. Scheduling Conflicts | 23.1% | 29.5% |
| 6. Son/Daughter not Eligible | 23.1% | 33.2% |
| 7. Getting Information about Services | 20.5% | 40.4% |
| 8. Transportation | 17.9% | 18.9% |
| 9. Poor Service Quality | 15.4% | 34.6% |
| 10. Lack of Time for Services | 12.8% | 26.3% |
| 11. Language Barrier | 2.6% | 14.3% |
| 12. Physical Accessibility | 2.6% | Not Asked |
Note. Barriers are organized by how commonly they are received in the present sample. Rates of barriers in the NLTS2 were derived from data tables provided on the project website (United States Department of Education, National Center for Special Education Research 2014).
Youth Characteristics
Intellectual disability
Comorbid intellectual disability status (0 = no intellectual disability, 1 = intellectual disability) was determined using standardized IQ and adaptive behavior assessments. Standardized IQ was obtained by administering the Stanford-Binet Intelligence Scale (Roid 2003) to youth with ASD during the psychological assessment. The Stanford-Binet is a commonly used intelligence scale with strong psychometric properties and both verbal and nonverbal sections. Adaptive behavior was assessed by administering the Vineland Adaptive Behavior Scales-Second Edition (Sparrow et al. 2005) to parents. Individuals with standard scores of 70 or below on both IQ and adaptive behavior measures were classified as having an intellectual disability, consistent with diagnostic guidelines (Luckasson et al. 2002). For cases where the individual with ASD scored above 70 on either measure, determination of intellectual disability status was made by clinicians.
Race/ethnicity
We collected the race/ethnicity of the youth with ASD, coded into 1 = white/non-Hispanic; 0 = other race/ethnicity. Although there were few participants who were racial/ethnic minorities in this sample, we included this variable given the prominence of racial/ethnicity disparities in other studies of service receipt in ASD (Thomas et al. 2007; Shattuck et al. 2011; Liptak et al. 2008; Mandell et al. 2002).
Autism symptom severity
Autism symptom severity was measured using the Social Responsiveness Scale (SRS; Constantino and Gruber 2005), a 65-item parent-report measure. The SRS measures dimensions of interpersonal behavior, communication, and repetitive/stereotypic behavior that are characteristic of ASD. Parents are asked to respond on a Likert-scale to items in terms of how best they describe their son/daughter's behaviors over the last 6 months, ranging from 1 = not true to 4 = almost always true. Item scores are combined to form five subscale scores (social awareness, social cognition, social communication, social motivation, autistic mannerisms) and an overall severity score. The SRS has demonstrated adequate reliability and validity in ASD samples (Constantino and Gruber 2005). Overall severity scores were used in the present analyses, with higher scores indicating greater symptom severity.
Comorbid psychiatric diagnoses
Current comorbid psychiatric diagnoses (1 = youth has a comorbid psychiatric diagnosis, 0 = youth does not have a comorbid psychiatric diagnosis) were determined using the psychiatric disorder section of the Rochester Health Status Survey (Davidson et al. 2008), a medical survey designed for individuals with disabilities. Parents were given a checklist of 12 possible psychiatric diagnoses (schizophrenia, other psychosis, bipolar disorder, depression, anxiety disorder, obsessive-compulsive disorder, post-traumatic stress disorder, personality disorder, alcohol/substance abuse, eating disorder, self-injury, other psychiatric disorder), and asked to indicate if their son or daughter currently has this condition, as diagnosed by a medical provider. Information collected about each diagnosis was combined to indicate whether the youth had any current comorbid psychiatric diagnoses.
Behavior problems
The Adult Behavior Checklist (ABCL; Achenbach and Rescorla 2003), a parent-report scale, was used to measure behavior problems among the youth with ASD. In the ABCL, parents are asked to rate the frequency of each of 126 problem behaviors on a 3-point Likert scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true). Scores are summed and converted to T-scores (M = 50, SD = 10) to form eight syndrome scales: Anxious/Depressed, Withdrawn, Somatic Complaints, Thought Problems, Attention Problems, Aggressive Behavior, Rule-Breaking Behavior, and Intrusiveness. Syndrome scales are combined to yield the Internalizing Problems, Externalizing Problems, and Total Problems composite scores. The ABCL has been validated for individuals ages 18-59; although about one-third of our participants were 17 years of age at data collection, we chose to administer the ABCL uniformly to ensure comparability across the entire sample. The manual for the ABCL reports adequate reliability and validity for scale and composite scores (Achenbach and Rescorla 2003). The ABCL has been validated in adults with intellectual disabilities (Tenneij and Koot 2007), and is commonly used in studies of adults with ASD (e.g., Anderson et al. 2011; Baker et al. 2012; Sachse et al. 2013; Visser et al. 2014). Total Problems T-scores were used in these analyses, with higher scores indicating more behavior problems.
Adaptive behavior
Adaptive behavior was assessed by the Vineland Adaptive Behavior Scales-Second Edition (Sparrow et al. 2005), a well-validated parent interview that assesses social, communication, daily living, and motor skills. It provides standard scores for these domains as well as an overall adaptive behavior composite (M=100, SD=15). The total Adaptive Behavior Composite was used in the present analyses, with higher scores indicating higher levels of adaptive behavior.
Family Factors
Family income
Parents were also asked about their family's income in the previous year, coded from 1 = less than $10,000 to 14 = over $160,000.
Parental health
Parents reported their own health at the present time on a 4-point scale ranging from 1 = poor to 4 = excellent. Self-rated health has been shown to be related to both morbidity and mortality across a variety of populations (including 12 different nationalities), even after controlling for known risk factors like socio-demographics, chronic health conditions, and health practices (Idler and Benyamini 1997).
Parental depressive symptoms
Parental depressive symptoms were assessed by the Center for Epidemiological Studies – Depression Scale (Radloff 1977). The measure has been used extensively in adult samples (Radloff 1991; Gatz and Hurwicz 1990). For each of 20 depressive symptoms, the respondent is asked to indicate how many days in the past week the symptom was experienced (0 = never to 3 = 5 to 7 days). Scores can range from 0 to 60, with a high score reflective of a greater intensity of depressive symptoms (α in this sample = .91).
Parental anxiety
The Anxiety subscale of the Profile of Mood States (McNair et al. 1981) was used to measure parental anxiety. This subscale measures the frequency of nine anxiety symptoms in the last week, such as feeling tense, shaky, or on edge (0 = not at all to 4 = extremely). Total scores range from 0 to 36, with higher scores indicating more anxiety (α in this sample = .93). The Profile of Mood States has been shown to have strong construct validity in past research (Gibson 1997).
Data Analysis
In order to address our first research question (patterns of service access), we examined means to determine the average number of services received by youth with ASD in their last year of high school, as well as the average number of unmet service needs. We examined the percentages of youth who were receiving each type of service, as well as the percentage who were reported as needing that service but not currently receiving it. We also examined the percentage of parents who reported each of 12 possible barriers to receiving services. In order to understand the representativeness of our sample, we compared their rates of service receipt and reported barriers to data collected from families of a nationally-representative sample of youth with ASD in high school, the NLTS2 (Newman et al. 2011).
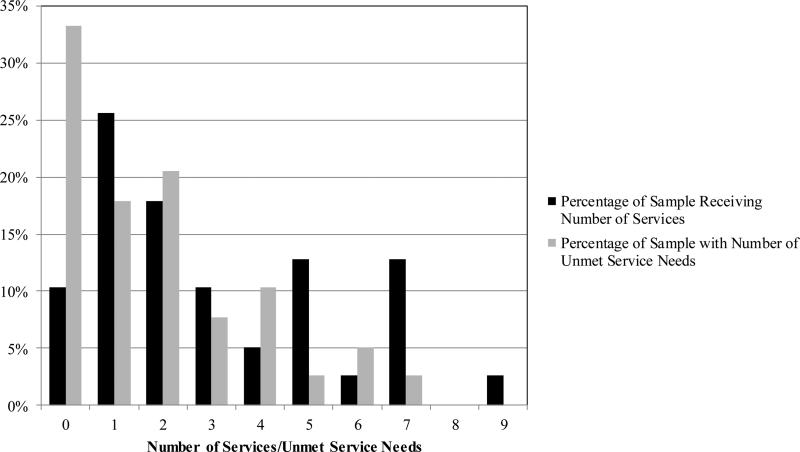
We next examined the youth (intellectual disability, race/ethnicity, autism symptom severity, comorbid psychiatric diagnoses, behavior problems, adaptive behavior) and family (income, parental health, parental depressive symptoms, parental anxiety) factors that were related to the number of services that youth with ASD received and their number of unmet service needs. Because the distributions of number of services and unmet service needs were not normal (see Figure 1), we used non-parametric statistics in all analyses. First, we examined the bivariate relations between study variables using Spearman Rho correlations. Then we used two ordinal regression equations to examine which of the youth and family variables predicted (1) number of services and (2) unmet service needs. Although it would have been preferable to include all of the possible independent variables in the regression equations, our relatively small sample size did not afford the statistical power. Therefore, we only included the youth and family characteristics in the regression equations if they had significant bivariate relations with the respective dependent variable (i.e., number of services or unmet service needs).
Figure 1.
Distribution of Number of Services and Unmet Service Needs.
Results
Descriptive Information on Service Access
Figure 1 depicts the distribution of the number of services received by youth with ASD in their last year of high school, as well as the number of services that were needed but not being received (unmet service needs). On average, youth were receiving approximately 3 services (M = 3.05, SD = 2.46), with a range from 0 to 9. The majority of youth (89.7%) were receiving at least one service at this time. As can be seen in Table 1, the most frequently accessed services were psychological/mental health services (43.6%), followed by speech language services (35.9%), career counseling/job skills training (33.3%), in-home/in-classroom aide (33.3%), and medical services related to special needs (30.8%). The remaining services were received by 25% or fewer of the sample.
When comparing rates of service receipt using data on youth with ASD from the NLTS2, youth with ASD in the present sample were less likely to be receiving 12 of the 15 measured services (see Table 1). The greatest disparities in service receipt between samples was for speech language therapy (74.6% in the NLTS2 vs. 35.9% in the present sample), in-home/in-classroom aide (53.9% vs. 33.3%), occupational/life skills (49.0% vs. 25.6%), and transportation services (54.6% vs. 20.5%). Thus, youth with ASD in the present sample were underserved compared to a nationally-representative cohort.
Disparities in service receipt in the present sample did not appear to be related to less need for services. The average number of unmet service needs was 1.85 (SD = 1.94), with a range from 0 to 7 (see Figure 1). Perhaps more importantly, two-thirds of the sample reported having at least one unmet service need, with nearly 30% (28.3%) reporting 3 or more unmet needs. In contrast, fewer than one-half of families in the NLTS2 (42.6%) reported that they were not getting their service needs met. As presented in Table 1, the most common unmet service needs in this sample were career counseling/job skills training and occupational/life skills training, which likely reflect parents’ concerns about preparing their son or daughter for exiting high school over the next year.
Barriers to receiving services, both in the present sample and in the NLTS2, are presented in Table 2. The three most common barriers endorsed by parents in the present sample were that the services cost too much, they weren't provided in a geographic area that was convenient/accessible, and the doctor/specialist did not accept their insurance type. In contrast, in the NLTS2, the most common barriers were that the services were not available and difficulties getting information about services (both endorsed by nearly twice as many parents as in the present sample).
In sum, parents of youth with ASD in their last year of high school (in the present sample) were receiving fewer services with higher numbers of unmet service needs, relative to a nationally-representative sample of youth with ASD in high school (the NLTS2). Barriers to accessing services differed between samples – in our sample, families were less likely to report service unavailability or inadequate information as barriers, but instead reported that cost and geographic location of services were the major barriers to service receipt.
Youth and Family Correlates of Service Access
The second research question focused on the youth and family correlates of service receipt and unmet service needs. Table 3 presents the bivariate relations between study variables. Interestingly, there was only a moderate correlation between the number of services that youth were receiving and the number of unmet service needs. That is, parents of youth who were getting fewer services were not necessarily reporting a higher number of unmet needs. Several youth variables were associated with the number of services received. Specifically, youth with ASD received more services if their autism symptoms were more severe (marginal), if they had a comorbid psychiatric diagnosis, and if they had lower levels of adaptive behavior. There was a marginally significant association between higher levels of maternal depressive symptoms and greater service receipt. More unmet service needs were associated with racial/ethnic minority status, greater severity of autism symptoms (marginal), as well more behavior problems and lower levels of adaptive behavior. A number of the family factors were also marginally or significantly associated with unmet service needs; families who had lower incomes and families in which the responding parent was in worse health and had higher levels of anxiety reported more unmet service needs.
Table 3.
Spearman Rho Correlations between Study Variables
| Number of Services |
Unmet needs |
Intellectual Disability |
White/ non- Hispanic |
Autism Symptom Severity |
Psychiatric Dx |
Behavior Problems |
Adaptive Behavior |
Family Income |
Parental Health |
Parental Depression |
Parental Anxiety |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Services | - - - | .21 | .18 | −.10 | .30† | .41** | .04 | −.39* | −.01 | −.23 | .31† | .25 |
| Unmet Service Needs | - - - | −.02 | −.45** | .29† | .10 | .41* | −.33* | −.29† | −.28† | .22 | .36* | |
| Youth Characteristics | ||||||||||||
| Intellectual Disability (1 = yes) | - - - | .04 | .25 | .12 | .14 | −.60** | −.07 | −.09 | −.01 | −.02 | ||
| White/non-Hispanic (1 = yes) | - - - | .14 | .11 | .04 | .17 | .37* | .36* | −.17 | −.19 | |||
| Autism Symptom Severity | - - - | .29† | .60** | −.48** | −.23 | −.15 | .39* | .24 | ||||
| Comorbid Psychiatric Dx (1 = yes) | - - - | .32* | −.24 | .02 | −.43* | .35* | .25 | |||||
| Behavior Problems Total | - - - | −.21 | −.26 | −.27† | .52** | .42** | ||||||
| Adaptive Behavior | - - - | .14 | .37* | −.07 | −.00 | |||||||
| Family Factors | ||||||||||||
| Family Income | - - - | .20 | −.30† | −.31† | ||||||||
| Parental Health | - - - | −.26 | −.14 | |||||||||
| Parental Depression | - - - | .82** | ||||||||||
| Parental Anxiety | - - - |
p < .10
p < .05
p < .01
Table 4 presents the results of the ordinal regression analyses examining which youth and family factors independently predicted number of services and unmet service needs. Both individual characteristics that had statistically significant bivariate correlations with number of services remained statistically significant when entered simultaneously into the regression model (top of Table 4). That is, youth who had a comorbid psychiatric diagnosis and those who had lower levels of adaptive behavior were receiving more services. Youth with a comorbid psychiatric diagnosis, on average, were receiving approximately two more services relative to youth without a comorbid diagnosis (4.19 vs. 2.26). Similarly, youth with adaptive behavior scores of less than 70 were receiving approximately 1.5 more services than youth with scores of 70 or above (3.48 services vs. 2.08 services)
Table 4.
Ordinal Regression Equations Predicting Number of Services and Unmet Service Needs
| Independent Variable | Estimate | SE | Wald χ2 |
|---|---|---|---|
| Number of Services | |||
| Co-morbid Psychiatric Diagnosis | 1.56 | .63 | 6.15* |
| Adaptive Behavior | −.06 | .02 | 6.60* |
| Number of Unmet Service Needs | |||
| White/non-Hispanic | −3.14 | 1.21 | 6.74** |
| Behavior Problems | .13 | .05 | 6.42* |
| Adaptive Behavior | −.04 | .02 | 2.50 |
| Parental Anxiety | .11 | .05 | 5.21* |
p < .05
p < .01
In the regression equation predicting unmet service needs, racial/ethnic minority status, more behavior problems and higher levels of parental anxiety independently predicted more unmet service needs (bottom of Table 4). Youth who were racial/ethnic minorities, on average, had 3 more unmet needs relative to youth who were White/non-Hispanic (4.75 vs. 1.51). When grouping behavior problems T-scores into average (T-scores of 50-64), borderline (T-scores of 65-69), and clinical behavior problems (T-scores ≥ 70; Achenbach and Rescorla 2003), 30.8% of youth with at least one unmet service need had behavior problems in the clinical range, compared to only 7.7% of youth with no unmet service needs. Further, parents of youth with at least one unmet need had anxiety scores that were approximately twice as high as parents of youth with no needs (10.65 vs. 5.85).
Thus, greater service receipt appeared to be related to greater functional needs (i.e., lower adaptive behavior) and the presence of a diagnosed comorbid mental health diagnosis in the youth with ASD, whereas youth with more unmet service needs tended to be racial/ethnic minorities, have greater behavioral needs (i.e., more behavior problems), and parents who were more anxious.
Follow-up Analyses
Because psychological/mental health services were included in our services count variable, we hypothesized that this type of service could account for greater service receipt among youth with ASD with a comorbid psychiatric diagnosis, relative to those without a comorbid diagnosis. Thus, we calculated another variable that counted the number of services excluding mental health services, and examined whether youth with ASD with a comorbid psychiatric diagnosis continued to receive more services. Having a comorbid diagnosis remained a significant predictor of the number of services received, B=1.38, SE=.62, Wald χ2 (1) = 4.99, p < .05. Even excluding mental health services, youth with ASD with a comorbid psychiatric diagnosis were receiving an average of 1.4 more services relative to youth without a comorbid diagnosis (3.63 vs. 1.91).
Discussion
Results from our cohort suggest that youth with ASD in their last year of high school are underserved relative to a nationally-representative sample of high-school aged students with ASD; these youth were less likely to be receiving 12 out of 15 services relative to the younger NLTS2 cohort. As suggested by Mandell and colleagues (Cidav et al. 2013), it may be that youth begin “aging out” of services as they approach their last few years of eligibility under IDEA. One striking example is speech/language therapy, which was received by only 36% of youth in this sample relative to 75% of youth in the NLTS2. Interestingly, however, for the services in which we observed the greatest disparities in the present cohort (speech/language therapy, in-home/in-classroom aide, transportation services), families reported fairly low levels of unmet need. Instead, high need was reported for more transition-focused services such as career/vocational training and occupational/life skills training. Thus, it seems likely that the types of services valued and pursued by parents may shift as the transition out of high school and into the adult service system looms closer.
Upon closer inspection, it appeared that relative to youth who have ASD and an intellectual disability (ID), those with ASD without ID might be particularly underserved in vocational and occupational/life skills training (results available from first author). Compared to those with ID, youth without ID were about one-half as likely to be receiving career/vocational training through the school system, and one-fourth as likely to be receiving occupational/life skills training through schools. Perhaps most worrisome, of those who were not receiving vocational training, parents of youth with ASD without ID were almost 2.5 times more likely than parents of youth with ID to report that this type of training is needed (63.2% vs. 28.6%). This suggests that vocational training is valued by parents of higher functioning youth with ASD, who often receive exclusively academic instruction in high school. Given that youth with ASD without ID are more likely than those with ID to have no vocational activities after high school exit (Taylor & Seltzer, 2011b), targeting vocational/job skills or life skills training toward these individuals might improve employment outcomes in adulthood.
Alternatively, differences in service access between the present cohort and the NLTS might reflect geographic disparities in service access. The state of Tennessee, where the majority of the sample is located, consistently falls among the states with the smallest expenditures on both education and special education per pupil (U.S. Census Bureau 2012; Parrish et al. 2004). If indeed the disparities in service access in the present cohort are a result of geography, then our findings are even more alarming as this cohort overall was socioeconomically advantaged. Although we did not find a relation between parental income and service access in our sample, other studies of school-aged youth have found that parents who have more economic resources have greater access to needed services for their son/daughter with ASD (Thomas et al. 2007; Liptak et al. 2008). Future research that separates out geographic differences in service access from age-related differences is needed to determine whether age and/or geography play a more important role in disparities in service access among adolescents with ASD.
As expected, the correlation between the number of services that youth with ASD were receiving and their number of unmet service needs was relatively low, suggesting that youth who are receiving few services may not necessarily need more of them, or alternatively, that youth who are receiving many services may not necessarily have all of their service needs met. Further, the youth and family factors that were correlated with the number of services were substantially different from those that were correlated with unmet needs. This provides evidence for the importance of considering both aspects of service access when trying to best understand how to meet the needs of youth with ASD who are transitioning to adulthood.
Interestingly, the presence of a comorbid psychiatric diagnosis was related to receiving a greater number of services, but higher behavior problem scores were related to more unmet service needs. Although higher levels of behavior problems might be expected to co-occur with comorbid psychiatric diagnoses, the correlation between these two variables was only moderate in the present cohort. This may be because the majority of youth who had a comorbid psychiatric diagnosis were being treated by prescription medication (81.2%), compared to 47.8% of youth without a comorbid diagnosis. Thus, treating the comorbid disorders should lessen the behavior problems that youth exhibit, disentangling this relationship. Our findings suggest that regardless of whether there is a diagnosed comorbid psychiatric disorder, parents would like further services and supports during the transition years to treat their son/daughter's problem behaviors. If youth with ASD and high level of behavior problems are underserved while under the mandate of IDEA, they may be at particularly high risk after high school exit. Our prior studies have found that high levels of behavior problems are associated with poor vocational outcomes in adulthood, suggesting that this is indeed the case (Taylor and Mailick 2014; Taylor and Seltzer 2011b, 2012).
Our finding that having a diagnosed comorbid psychiatric disorder predicted greater service use, although novel, was not surprising given that mental health services was one of the types of services included in the overall count. However, follow-up analyses suggested that relative to youth without a comorbid disorder, these youth received additional services net of mental health services. Thus, effectively treating comorbid psychiatric problems during the transition years might alleviate the services needed by youth in other domains as well. Given the high public costs of ASD (Ganz 2007; Cidav et al. 2013; Mandell et al. 2006), future investigation into whether effectively treating mental health problems in these youth results in reduction in service needs and associated costs is highly significant.
Consistent with previous research (Cadman et al. 2012; Hare et al. 2004), we found that poor parental mental health was related to unmet needs for youth with ASD. Specifically, our findings suggested that parents with higher levels of anxiety had sons/daughters with ASD who had more unmet service needs. Perhaps most importantly, this is the first study to find that the relation between parental mental health and unmet service needs remained statistically significant after controlling for the behavior problems of the youth with ASD (which is one of the most consistent correlates of parental mental health; Hastings 2003; Hastings and Brown 2002; Tomanik et al. 2004; Lounds et al. 2007). Because this is a cross-sectional study, it is impossible to determine the direction of effects between these variables; it may be that having a high number of unmet service needs leads to high levels of anxiety among parents of transitioning youth. Alternatively, it could be that parents who exhibit high levels of anxiety are less effective in procuring needed services for their son/daughter with ASD. If this is the case, we might expect the impact of parental mental health on service receipt to be even more pronounced after high school exit, when services are no longer mandated, leaving parents with the responsibility for finding, coordinating, and maintaining services. Longitudinal studies are needed to disentangle the direction of effects between parental mental health and son/daughter service access, as the results have important implications for intervention. Particularly if parental anxiety does indeed lead to less effectiveness in procuring needed services, then new, family-focused targets for potential interventions might be appropriate to increase service access for youth with ASD.
Also consistent with some extant studies (Thomas et al. 2007; Shattuck et al. 2011; Liptak et al. 2008), youth with ASD who were racial/ethnic minorities averaged 3 more unmet service needs relative to youth who were white/non-Hispanic. Although conclusions must be drawn with great caution, given the small number of racial/ethnic minority families in our cohort, results suggest that these families are being underserved while youth with ASD are still under the umbrella of IDEA. As suggested by Shattuck and colleagues (Shattuck et al. 2011), disparities in service access might be magnified even further after high school exit, placing these young adults with ASD at extraordinarily high risk for unemployment and poor adult outcomes.
There are a number of limitations to the present study that are important to note. First, this was a small, non-representative sample who lived in two specific geographic regions. Not only did the small sample preclude our ability to conduct further statistical analyses (due to lack of power), but it is unclear to what extent results from this sample will generalize to other samples of youth with ASD in their last year of high school. Our recruitment methods and study procedures also likely affect generalizability; many participants in the present study were recruited through other autism-related studies or mailing lists from autism organizations, and may be better-connected and more likely to be receiving services than families in the general population. Further, participants were required to travel to the project site to participate in the research, and thus families who are more socioeconomically disadvantaged are likely under-represented in the sample. If families in the present cohort are indeed better served and more economically advantaged than the population of families of youth with ASD in our geographic areas, then our finding that youth with ASD are underserved in their last year of high school is even more alarming, as we may be underestimating the true amount of need. Larger-scale studies are needed to determine to what extent the disparities in service access noted in this sample are due to geography or to stage of the life course (youth in their last year of high school as opposed to earlier in their high school career).
Second, the majority of measures included in this study were collected via parental self-report. Although this allowed us to collect data from parents of youth with a wide range of functioning, it is possible that the shared method variance may be accounting for some of our findings. On a related note, we did not have access to the youths’ Individualized Education Plans (IEPs), which would detail the services prescribed by the school system (though not the quality or appropriateness of the services). It is possible that youth in this sample were receiving more services through schools than parents were aware. Future research should consider multiple reports of service access, as they provide complementary information.
Finally, because this was a cross-sectional study, there were important questions that we were not able to examine. First, we were unable to explore directionality of the observed relations. This was particularly relevant for the relations between unmet service needs, behavior problems, and parental anxiety. Do youth with more behavior problems have increasing difficulty accessing services? Or does difficulty accessing needed services lead to an increase in behavior problems? Similarly, do parents have more anxiety because their son/daughter is not getting his/her service needs met? Or are parents with high levels of anxiety less effective in procuring needed services for their son or daughter? Longitudinal studies are needed to separate out the directionality of these relations, which has important implications for intervention. Second, it is unclear to what extent disparities in service access while youth with ASD are in high school leads to problematic outcomes in adulthood. Although it is reasonable to expect that disparities in service access will be magnified after youth leave the protective umbrella of IDEA and enter the adult service system, this needs to be tested with longitudinal studies that follow youth with ASD from before to after high school exit.
Although there are limitations to this data, this is the first study to our knowledge that provides a detailed examination of service access for youth with ASD at a critical point in the lifespan – during their last year of high school. This study is also unique relative to most research on service access for transition-aged youth with ASD by utilizing a carefully phenotyped sample with detailed, well-validated measures across a range of youth and family factors. Our findings suggest that these youth are underserved, even in comparison to their younger, high-school aged peers, and have specific needs in areas such as vocational and life skills training. That vocational and life skills training needs are not met is of concern, as these types of services are likely to be very important in promoting post-school independence. Youth who were particularly underserved in our sample – those who were racial/ethnic minorities, who had high levels of behavior problems, and who had parents with high levels of anxiety – might be at greatest risk for a poor transition to adulthood and warrant future research with larger, longitudinal samples to understand their transition outcomes.
Acknowledgments
This project was supported by the National Institute of Mental Health (K01 MH92598, J.L. Taylor, PI) and the National Center for Advancing Translational Sciences (CTSA award UL1TR000445). Core support was provided by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P30 HD15052, E.M. Dykens, PI). The contents of this project are solely the responsibility of the authors and do not necessarily represent official views of the National Institutes of Health. We are grateful to the families who participated in this research, to Dr. Amie Duncan for her assistance in data collection, as well as to Dr. Leann Smith for providing feedback on an earlier version of the manuscript.
Contributor Information
Julie Lounds Taylor, Vanderbilt Kennedy Center; Department of Pediatrics, Vanderbilt University School of Medicine and the Monroe Carell Jr. Children's Hospital at Vanderbilt; Nashville, TN, USA..
Natalie A. Henninger, Vanderbilt Kennedy Center, Vanderbilt University, Nashville, TN, USA.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms & Profiles. University of Vermont, Reserach Center for Children, Youth, & Families; Burlington, VT: 2003. [Google Scholar]
- American Association on Intellectual and Developmental Disabilities . Intellectual disability : definition, classification, and systems of supports. 11th ed. American Association on Intellectual and Developmental Disabilities; Washington, DC: 2010. [Google Scholar]
- Anderson DD, Maye MP, Lord C. Changes in Maladaptive Behaviors From Midchildhood to Young Adulthood in Autism Spectrum Disorder. American Journal on Intellectual and Developmental Disabilities. 2011;116(5):381–397. doi: 10.1352/1944-7558-116.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Seltzer MM, Greenberg JS. Behaviour problems, maternal internalising symptoms and family relations in families of adolescents and adults with fragile X syndrome. Journal of Intellectual Disability Research. 2012;56(10):984–995. doi: 10.1111/j.1365-2788.2012.01580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballaban-Gil K, Rapin l., Tuchman T, Shinnar S. Longitudinal examination of the behavioral, language, and social changes in a population of adolescent and young adults with autistic disorder. Pediatric Neurology. 1996;15(3):217–223. doi: 10.1016/s0887-8994(96)00219-6. [DOI] [PubMed] [Google Scholar]
- Billstedt E, Gillberg C, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders. 2005;35(3):351–360. doi: 10.1007/s10803-005-3302-5. [DOI] [PubMed] [Google Scholar]
- Cadman T, Eklund H, Howley D, Hayward H, Clarke H, Findon J, et al. Caregiver burden as people with autism spectrum disorder and attention-deficit/hyperactivity disorder transition into adolescence and adulthood in the United Kingdom. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(9):879–888. doi: 10.1016/j.jaac.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Prevalence of autism spectrum disorder among children aged 8 years - Autism and Developmetnal Disabilities Monitoring Network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report Surveillance Summary. 2014;63(SS02):1–21. [PubMed] [Google Scholar]
- Cidav Z, Lawer L, Marcus SC, Mandell DS. Age-Related Variation in Health Service Use and Associated Expenditures Among Children with Autism. Journal of Autism and Developmental Disorders. 2013;43(4):924–931. doi: 10.1007/s10803-012-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale (SRS) manual. Western Psychological Services; Los Angeles, CA: 2005. [Google Scholar]
- Davidson PW, Henderson CM, Janicki MP, Robinson LM, Bishop KM, Wells A, et al. Ascertaining Health-Related Information on Adults With Intellectual Disabilities: Development and Field Testing of the Rochester Health Status Survey. Journal of Policy and Practice in Intellectual Disabilities. 2008;5(1):12–23. [Google Scholar]
- Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology. 2008;20(3):775–803. doi: 10.1017/S0954579408000370. [DOI] [PubMed] [Google Scholar]
- Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38(4):739–747. doi: 10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- Factor DC, Perry A, Freeman N. Stress, Social Support, and Respite Care Use in Families with Autistic Children - Brief Report. Journal of Autism and Developmental Disorders. 1990;20(1):139–146. doi: 10.1007/BF02206863. [DOI] [PubMed] [Google Scholar]
- Ganz ML. The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics & Adolescent Medicine. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- Gatz M, Hurwicz ML. Are old people more depressed? Cross-sectional data on Center for Epidemiological Studies Depression Scale factors. Psychology and Aging. 1990;5(2):284–290. doi: 10.1037//0882-7974.5.2.284. [DOI] [PubMed] [Google Scholar]
- Gibson SJ. The measurement of mood states in older adults. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1997;52B(4):167–174. doi: 10.1093/geronb/52b.4.p167. [DOI] [PubMed] [Google Scholar]
- Goin-Kochel RP, Myers BJ, Mackintosh VH. Parental reports on the use of treatments and therapies for children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2007;1(3):195–209. [Google Scholar]
- Green VA, Pituch KA, Itchon J, Choi A, O'Reilly M, Sigafoos J. Internet survey of treatments used by parents of children with autism. Research in Developmental Disabilities. 2006;27(1):70–84. doi: 10.1016/j.ridd.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Gurney JG, Fritz MS, Ness KK, Sievers P, Newschaffer CJ, Shapiro EG. Analysis of prevalence trends of autism spectrum disorder in Minnesota. Archives of Pediatrics and Adolescent Medicine. 2003;157(7):622–627. doi: 10.1001/archpedi.157.7.622. [DOI] [PubMed] [Google Scholar]
- Hare, Pratt, Burton, Bromley, Emerson The health and social care needs of family carers supporting adults with autistic spectrum disorders. Autism. 2004;8(4):425–444. doi: 10.1177/1362361304047225. [DOI] [PubMed] [Google Scholar]
- Hastings RP. Child behavior problems and partner mental health as correlates of stress in mothers and fathers of children with autism. Journal of Intellectual Disability Research. 2003;47(4):231–237. doi: 10.1046/j.1365-2788.2003.00485.x. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Brown T. Behavior problems of children with autism, parental self-efficacy, and mental health. American Journal on Mental Retardation. 2002;107(3):222–232. doi: 10.1352/0895-8017(2002)107<0222:BPOCWA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Howlin P. Outcomes in autism spectrum disorders. In: Volkmar FR, Paul R, Klin A, Cohen D, editors. Handbook of autism and pervasive developmental disorders. 3rd ed. Vol. 1. John Wiley & Sons, Inc.; Hoboken, NJ: 2005. pp. 201–220. [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Krauss MW, Gulley S, Sciega JM, Wells N. Access to specialty medical care for children with mental retardation, autism, and other special health care needs. Mental Retardation. 2003;41(5):329–339. doi: 10.1352/0047-6765(2003)41<329:ATSMCF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Landmark LJ, Zhang D. Compliance and Practices in Transition Planning: A Review of Individualized Education Program Documents. Remedial and Special Education. 2013;34(2):113–125. [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, et al. Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children's Health. Journal of developmental and behavioral pediatrics. 2008;29(3):152–160. doi: 10.1097/DBP.0b013e318165c7a0. [DOI] [PubMed] [Google Scholar]
- Lounds JJ, Seltzer MM, Greenberg JS, Shattuck PT. Transition and change in adolescents and young adults with autism: Longitudinal effects on maternal well-being. American Journal on Mental Retardation. 2007;112(6):401–417. doi: 10.1352/0895-8017(2007)112[401:TACIAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Luckasson R, Borthwick-Duffy S, Buntinx WHE, Coulter DL, Craig EM, Reeve A, et al. Mental retardation: Definition, classification, and systems of supports. 10th ed. American Association on Mental Retardation; Washington, DC: 2002. [Google Scholar]
- Mandell DS, Cao J, Ittenbach R, Pinto-Martin JA. Medicaid expenditures for children with autistic spectrum disorders: 1994-1999. Journal of Autism and Developmental Disorders. 2006;36(4):475–485. doi: 10.1007/s10803-006-0088-z. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Listerud J, Levy SE, Pinto-Martin JA. Race differences in the age at diagnosis among medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(12):1447–1453. doi: 10.1097/00004583-200212000-00016. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Profile of Mood States (POMS) Manual. Educational and Industrial Testing Service; San Diego, CA: 1981. [Google Scholar]
- Narendorf SC, Shattuck PT, Sterzing PR. Mental Health Service Use Among Adolescents With an Autism Spectrum Disorder. Psychiatric Services. 2011;62(8):975–978. doi: 10.1176/appi.ps.62.8.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman L, Wagner M, Huang T, Shaver D, Knokey A-M, Yu J, et al. Secondary school programs and performance of students with disabilities: A special topic report of findings from the National Longitudinal Transition Study-2 (NLTS2) (NCSER 2012-3000) U.S. Department of Education; National Center for Special Education Research; SRI International; Washington, DC: Menlo Par, CA: 2011. [Google Scholar]
- Parrish T, Harr J, Wolman J, Anthony J, Merickel A, Esra P. Part II: Special Education Revenues and Expenditures. Center for Special Education Finance, American Institutes for Research; Palo Alto, CA: 2004. State Special Education Financy Systems, 1999-2000. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS. The Use of the Center for Epidemiologic Studies Depression Scale in Adolescents and Young-Adults. Journal of Youth and Adolescence. 1991;20(2):149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Roid GH. Stanford-Binet Intelligence Scales. Fifth Edition. Riverside Publishing; Itasca, IL: 2003. [Google Scholar]
- Sachse M, Schlitt S, Hainz D, Ciaramidaro A, Schirman S, Walter H, Poustka F, Bolte S, Freitag CM. Executive and visuo-motor function in adolescents and adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43(5):1222–1235. doi: 10.1007/s10803-012-1668-8. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary Education and Employment Among Youth With an Autism Spectrum Disorder. Pediatrics. 2012;129(6):1042–1049. doi: 10.1542/peds.2011-2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck PT, Wagner M, Narendorf S, Sterzing P, Hensley M. Post-High School Service Use Among Young Adults With an Autism Spectrum Disorder. Archives of Pediatrics & Adolescent Medicine. 2011;165(2):141–146. doi: 10.1001/archpediatrics.2010.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sparrow SD, Cicchetti DV, Balla DA. Vineland-II Adaptive Behavior Scales: Survey Forms Manual. AGS Publishing; Circle Pines, MN: 2005. [Google Scholar]
- Taylor JL, Mailick MR. A longitudinal examination of 10-year change in vocational and educational activities for adults With autism spectrum disorders. Developmental Psychology. 2014;50(3):699–708. doi: 10.1037/a0034297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Change in the autism phenotype during the transition to adulthood. Journal of Autism and Developmental Disorders. 2010;40(12):1431–1446. doi: 10.1007/s10803-010-1005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Changes in the mother-child relationship during the transition to adulthood for youth with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2011a;41(10):1397–1410. doi: 10.1007/s10803-010-1166-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Employment and post-secondary education activities for young adults with autism spectrum disorders during the transition to adulthood. Journal of Autism and Developmental Disorders. 2011b;41(5):566–574. doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Developing a vocational index for adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42(12):2669–2679. doi: 10.1007/s10803-012-1524-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenneij NH, Koot HM. A preliminary investigation into the utility of the Adult Behavioral Checklist in the assessment of psychopathology in people with low IQ. Journal of Applied Research in Intellectual Disabilities. 2007;20(5):391–400. [Google Scholar]
- Thomas KC, Ellis AR, McLaurin C, Daniels J, Morrissey JP. Access to care for autism-related services. Journal of Autism and Developmental Disorders. 2007;37(10):1902–1912. doi: 10.1007/s10803-006-0323-7. [DOI] [PubMed] [Google Scholar]
- Tomanik S, Harris GE, Hawkins J. The relationship between behaviours exhibited by children with autism and maternal stress. Journal of Intellectual & Developmental Disability. 2004;29(1):16–26. [Google Scholar]
- U.S. Census Bureau . Public Education Finances, 2010, G10-ASPEF. U.S. Government Printing Office; Washington, DC: 2012. [Google Scholar]
- United States Department of Education, National Center for Special Education Research [March 21 2014];National Longitudinal Transition Study-2: Data Tables. 2014 http://www.nlts2.org/data_tables/index.html.
- Visser EM, Berger HJC, Prins JB, Van Schrojenstein Lantman-De Valk HMJ, Teunisse JP. Shifting impairment and aggression in intellectual disability and Autism Spectrum Disorder. Research in Developmental Disabilities. 2014;35(9):2137–2147. doi: 10.1016/j.ridd.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Wei X, Wagner M, Christiano ERA, Shattuck P, Yu JW. Special Education Services Received by Students With Autism Spectrum Disorders From Preschool Through High School. The Journal of Special Education. 2013 doi: 10.1177/0022466913483576. doi:10.1177/0022466913483576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Scahill L, Klin A, Koenig K, Volkmar FR. Educational placements and service use patterns of individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37(8):1403–1412. doi: 10.1007/s10803-006-0281-0. [DOI] [PubMed] [Google Scholar]